Anxiety Disorders and Depression Essay (Critical Writing)
Introduction, description section, feelings section, action plan, reference list.
Human beings become anxious in different situations that are uncertain to them. Depression and anxiety occur at a similar time. Anxiety is caused due to an overwhelming fear of an expected occurrence of an event that is unclear to a person. More than 25 million people globally are affected by anxiety disorders. People feel anxious in moments such as when making important decisions, before facing an interview panel, and before taking tests. Anxiety disorders are normally brained reactions to stress as they alert a person of impending danger. Most people feel sad and low due to disappointments. Feelings normally overwhelm a person leading to depression, especially during sad moments such as losing a loved one or divorce. When people are depressed, they engage in reckless behaviors such as drug abuse that affect them physically and emotionally. However, depression manifests in different forms in both men and women. Research shows that more women are depressed compared to men. This essay reflects on anxiety disorders and depression regarding from a real-life experience extracted from a publication.
“Every year almost 20% of the general population suffers from a common mental disorder, such as depression or an anxiety disorder” (Cuijpers et al. 2016, p.245). I came across a publication by Madison Jo Sieminski available who was diagnosed with depression and anxiety disorders (Madison 2020). She explains how she was first diagnosed with anxiety disorders and depression and how it felt unreal at first. She further says that she developed the need to get a distraction that would keep her busy so that she won’t embrace her situation. In her case, anxiety made her feel that she needed to do more, and everything needed to be perfect.
Madison further said that the struggle with anxiety is that it never seemed to happen, but it happened eventually. She always felt a feeling of darkness and loneliness. She could barely stay awake for more than 30 minutes for many days. Anxiety and depression made her question herself if she was good enough, and this resulted in tears in her eyes due to the burning sensation and overwhelmed emotions. In her own words, she said, “Do I deserve to be here? What is my purpose?” (Madison 2020). Anxiety made her lose confidence in herself and lowered her self-esteem. She could lay in bed most of the time and could not take any meal most of the days.
Madison said that since the sophomore year of high school, all was not well, and she suddenly felt someone in her head telling her to constantly worry and hold back from everything. She could wake up days when she could try a marathon to keep her mind busy. However, she sought help on 1 January 2020, since she felt her mental health was important, and she needed to be strong. She was relieved from her biggest worries, and what she thought was failure turned into a biggest achievement. She realized that her health needed to be her priority. Even after being diagnosed with depression disorders, she wanted to feel normal and have a normal lifestyle like other people.
Madison was happy with her decision to seek medical help even though she had her doubts. She was happy that she finally took that step to see a doctor since she was suffering in silence. She noted that the background of her depression and anxiety disorders was her family. It was kind of genetic since her mom also struggled with depression and anxiety disorders. Her mom was always upset, and this broke her heart. She said it took her years to better herself, but she still had bad days. Madison decided to take the challenge regarding her mother’s experience. Also, Madison said she was struggling to get over depression since her childhood friends committed suicide, and it affected her deeply. She also told the doctor how she often thought of harming herself. The doctor advised her on the different ways she could overcome her situation after discovering she had severe depression and anxiety disorders.
After going through Madison’s story, I was hurt by the fact that he had to go through that for a long time, and something tragic could have happened if she had not resorted to medical help. I felt emotional by the fact that she constantly blamed herself due to her friends who committed suicide, and she decided to accumulate all the pain and worries. The fact that I have heard stories of how people commit suicide due to depression and anxiety disorders made me have a somber mood considering her case. In this case, you will never know what people are going through in their private lives until they decide to open up. We normally assume every person is okay, yet they fight their demons and struggle to look okay. Hence, it won’t cost any person to check up on other people, especially if they suddenly change their social characters.
Madison’s story stood out for me since she had struggled since childhood to deal with depression and anxiety disorders. In her case, she was unable to seek help first even when she knew that she was suffering in silence (Madison 2020). However, most people find it hard to admit they need help regardless of what they are going through, like Madison. People who are depressed cannot work as they lack the motivation to do anything. In my knowledge, depression affects people close to you, including your family and friends. Depression also hurts those who love someone suffering from it. Hence, it is complex to deal with. Madison’s situation stood out for me since her childhood friends committed suicide, and she wished silently she could be with them. Hence, this leads to her constant thoughts of harming herself. Childhood friends at one point can become your family even though you are not related by blood due to the memories you share.
Depression and Anxiety disorders have been common mental health concerns globally for a long time. Depression and anxiety disorders create the impression that social interactions are vague with no meaning. It is argued by Cuijpers (2016, p.245) that people who are depressed normally have personality difficulties as they find it hard to trust people around them, including themselves. In this case, Madison spent most of her time alone, sleeping, and could not find it necessary to hang around other people. Negativity is the order of the day as people depressed find everything around them not interesting.
People who are depressed find it easy to induce negativity in others. Hence, they end up being rejected. Besides, if someone is depressed and is in a relationship, he/she may be the reason for ending the relationship since they would constantly find everything offensive. Research shows that people who are clinically depressed, such as Madison, prefer sad facial expressions to happy facial expressions. Besides, most teenagers in the 21 st century are depressed, and few parents tend to notice that. Also, most teenagers lack parental love and care since their parents are busy with their job routines and have no time to engage their children. Research has shown that suicide is the second cause of death among teenagers aged between 15-24 years due to mental disorders such as suicide and anxiety disorders.
Despite depression being a major concern globally, it can be controlled and contained if specific actions are taken. Any person needs to prioritize their mental health to avoid occurrences of depression and anxiety orders. Emotional responses can be used to gauge if a person is undergoing anxiety and depression. The best efficient way to deal with depression and anxiety is to sensitize people about depression through different media platforms (Cuijpers et al. 2016). A day in a month should be set aside where students in colleges are sensitized on the symptoms of depression and how to cope up with the situation. Some of the basic things to do to avoid anxiety and depression include; talking to someone when you are low, welcoming humor, learning the cause of your anxiety, maintaining a positive attitude, exercising daily, and having enough sleep.
Depression and anxiety disorders are different forms among people, such as irritability and nervousness. Most people are diagnosed with depression as a psychiatric disorder. Technology has been a major catalyst in enabling depression among people as they are exposed to many negative experiences online. Besides, some people are always motivated by actions of other people who seem to have given up due to depression. Many people who develop depression normally have a history of anxiety disorders. Therefore, people with depression need to seek medical attention before they harm themselves or even commit suicide. Also, people need to speak out about what they are going through to either their friends or people they trust. Speaking out enables people to relieve their burden and hence it enhances peace.
Cuijpers, P., Cristea, I.A., Karyotaki, E., Reijnders, M. and Huibers, M.J., 2016. How effective are cognitive behavior therapies for major depression and anxiety disorders? A meta‐analytic update of the evidence . World Psychiatry 15(3), pp. 245-258.
Madison, J. 2020. Open Doors .
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, June 16). Anxiety Disorders and Depression. https://ivypanda.com/essays/anxiety-disorders-and-depression/
"Anxiety Disorders and Depression." IvyPanda , 16 June 2022, ivypanda.com/essays/anxiety-disorders-and-depression/.
IvyPanda . (2022) 'Anxiety Disorders and Depression'. 16 June.
IvyPanda . 2022. "Anxiety Disorders and Depression." June 16, 2022. https://ivypanda.com/essays/anxiety-disorders-and-depression/.
1. IvyPanda . "Anxiety Disorders and Depression." June 16, 2022. https://ivypanda.com/essays/anxiety-disorders-and-depression/.
Bibliography
IvyPanda . "Anxiety Disorders and Depression." June 16, 2022. https://ivypanda.com/essays/anxiety-disorders-and-depression/.
- James Madison’s Leadership Qualities
- Madison PLC: Funding and Management
- James Madison’s Political Theory
- Madison Consultancy Group: Ethics and Conduct Program
- James Madison's Life, Service and Conduct
- James Madison and the United States Constitution
- Constitution and James Madison’s Influence on It
- Concept Care Plan Mapping: Eva Madison
- The United States Supreme Court: Marbury vs. Madison
- Federalist Paper Number 10
- Cerebral Palsy: Epidemiology and Etiology
- Neurological System Disorder of Falling Asleep
- Migraine Headache and Tension Headache Compared
- Neurodevelopmentally at‐Risk Infants
- Migraine Without Aura Treatment Plan

Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
The Critical Relationship Between Anxiety and Depression
- Ned H. Kalin , M.D.
Search for more papers by this author
Anxiety and depressive disorders are among the most common psychiatric illnesses; they are highly comorbid with each other, and together they are considered to belong to the broader category of internalizing disorders. Based on statistics from the Substance Abuse and Mental Health Services Administration, the 12-month prevalence of major depressive disorder in 2017 was estimated to be 7.1% for adults and 13.3% for adolescents ( 1 ). Data for anxiety disorders are less current, but in 2001–2003, their 12-month prevalence was estimated to be 19.1% in adults, and 2001–2004 data estimated that the lifetime prevalence in adolescents was 31.9% ( 2 , 3 ). Both anxiety and depressive disorders are more prevalent in women, with an approximate 2:1 ratio in women compared with men during women’s reproductive years ( 1 , 2 ).
Across all psychiatric disorders, comorbidity is the rule ( 4 ), which is definitely the case for anxiety and depressive disorders, as well as their symptoms. With respect to major depression, a worldwide survey reported that 45.7% of individuals with lifetime major depressive disorder had a lifetime history of one or more anxiety disorder ( 5 ). These disorders also commonly coexist during the same time frame, as 41.6% of individuals with 12-month major depression also had one or more anxiety disorder over the same 12-month period. From the perspective of anxiety disorders, the lifetime comorbidity with depression is estimated to range from 20% to 70% for patients with social anxiety disorder ( 6 ), 50% for patients with panic disorder ( 6 ), 48% for patients with posttraumatic stress disorder (PTSD) ( 7 ), and 43% for patients with generalized anxiety disorder ( 8 ). Data from the well-known Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study demonstrate comorbidity at the symptom level, as 53% of the patients with major depression had significant anxiety and were considered to have an anxious depression ( 9 ).
Anxiety and depressive disorders are moderately heritable (approximately 40%), and evidence suggests shared genetic risk across the internalizing disorders ( 10 ). Among internalizing disorders, the highest level of shared genetic risk appears to be between major depressive disorder and generalized anxiety disorder. Neuroticism is a personality trait or temperamental characteristic that is associated with the development of both anxiety and depression, and the genetic risk for developing neuroticism also appears to be shared with that of the internalizing disorders ( 11 ). Common nongenetic risk factors associated with the development of anxiety and depression include earlier life adversity, such as trauma or neglect, as well as parenting style and current stress exposure. At the level of neural circuits, alterations in prefrontal-limbic pathways that mediate emotion regulatory processes are common to anxiety and depressive disorders ( 12 , 13 ). These findings are consistent with meta-analyses that reveal shared structural and functional brain alterations across various psychiatric illnesses, including anxiety and major depression, in circuits involving emotion regulation ( 13 ), executive function ( 14 ), and cognitive control ( 15 ).
Anxiety disorders and major depression occur during development, with anxiety disorders commonly beginning during preadolescence and early adolescence and major depression tending to emerge during adolescence and early to mid-adulthood ( 16 – 18 ). In relation to the evolution of their comorbidity, studies demonstrate that anxiety disorders generally precede the presentation of major depressive disorder ( 17 ). A European community-based study revealed, beginning at age 15, the developmental relation between comorbid anxiety and major depression by specifically focusing on social phobia (based on DSM-IV criteria) and then asking the question regarding concurrent major depressive disorder ( 18 ). The findings revealed a 19% concurrent comorbidity between these disorders, and in 65% of the cases, social phobia preceded major depressive disorder by at least 2 years. In addition, initial presentation with social phobia was associated with a 5.7-fold increased risk of developing major depressive disorder. These associations between anxiety and depression can be traced back even earlier in life. For example, childhood behavioral inhibition in response to novelty or strangers, or an extreme anxious temperament, is associated with a three- to fourfold increase in the likelihood of developing social anxiety disorder, which in turn is associated with an increased risk to develop major depressive disorder and substance abuse ( 19 ).
It is important to emphasize that the presence of comor‐bid anxiety symptoms and disorders matters in relation to treatment. Across psychiatric disorders, the presence of significant anxiety symptoms generally predicts worse outcomes, and this has been well demonstrated for depression. In the STAR*D study, patients with anxious major depressive disorder were more likely to be severely depressed and to have more suicidal ideation ( 9 ). This is consistent with the study by Kessler and colleagues ( 5 ), in which patients with anxious major depressive disorder, compared with patients with nonanxious major depressive disorder, were found to have more severe role impairment and more suicidal ideation. Data from level 1 of the STAR*D study (citalopram treatment) nicely illustrate the impact of comorbid anxiety symptoms on treatment. Compared with patients with nonanxious major depressive disorder, those 53% of patients with an anxious depression were less likely to remit and also had a greater side effect burden ( 20 ). Other data examining patients with major depressive disorder and comorbid anxiety disorders support the greater difficulty and challenge in treating patients with these comorbidities ( 21 ).
This issue of the Journal presents new findings relevant to the issues discussed above in relation to understanding and treating anxiety and depressive disorders. Drs. Conor Liston and Timothy Spellman, from Weill Cornell Medicine, provide an overview for this issue ( 22 ) that is focused on understanding mechanisms at the neural circuit level that underlie the pathophysiology of depression. Their piece nicely integrates human neuroimaging studies with complementary data from animal models that allow for the manipulation of selective circuits to test hypotheses generated from the human data. Also included in this issue is a review of the data addressing the reemergence of the use of psychedelic drugs in psychiatry, particularly for the treatment of depression, anxiety, and PTSD ( 23 ). This timely piece, authored by Dr. Collin Reiff along with a subgroup from the APA Council of Research, provides the current state of evidence supporting the further exploration of these interventions. Dr. Alan Schatzberg, from Stanford University, contributes an editorial in which he comments on where the field is in relation to clinical trials with psychedelics and to some of the difficulties, such as adequate blinding, in reliably studying the efficacy of these drugs ( 24 ).
In an article by McTeague et al. ( 25 ), the authors use meta-analytic strategies to understand the neural alterations that are related to aberrant emotion processing that are shared across psychiatric disorders. Findings support alterations in the salience, reward, and lateral orbital nonreward networks as common across disorders, including anxiety and depressive disorders. These findings add to the growing body of work that supports the concept that there are common underlying factors across all types of psychopathology that include internalizing, externalizing, and thought disorder dimensions ( 26 ). Dr. Deanna Barch, from Washington University in St. Louis, writes an editorial commenting on these findings and, importantly, discusses criteria that should be met when we consider whether the findings are actually transdiagnostic ( 27 ).
Another article, from Gray and colleagues ( 28 ), addresses whether there is a convergence of findings, specifically in major depression, when examining data from different structural and functional neuroimaging modalities. The authors report that, consistent with what we know about regions involved in emotion processing, the subgenual anterior cingulate cortex, hippocampus, and amygdala were among the regions that showed convergence across multimodal imaging modalities.
In relation to treatment and building on our understanding of neural circuit alterations, Siddiqi et al. ( 29 ) present data suggesting that transcranial magnetic stimulation (TMS) targeting can be linked to symptom-specific treatments. Their findings identify different TMS targets in the left dorsolateral prefrontal cortex that modulate different downstream networks. The modulation of these different networks appears to be associated with a reduction in different types of symptoms. In an editorial, Drs. Sean Nestor and Daniel Blumberger, from the University of Toronto ( 30 ), comment on the novel approach used in this study to link the TMS-related engagement of circuits with symptom improvement. They also provide a perspective on how we can view these and other circuit-based findings in relation to conceptualizing personalized treatment approaches.
Kendler et al. ( 31 ), in this issue, contribute an article that demonstrates the important role of the rearing environment in the risk to develop major depression. Using a unique design from a Swedish sample, the analytic strategy involves comparing outcomes from high-risk full sibships and high-risk half sibships where at least one of the siblings was home reared and one was adopted out of the home. The findings support the importance of the quality of the rearing environment as well as the presence of parental depression in mitigating or enhancing the likelihood of developing major depression. In an accompanying editorial ( 32 ), Dr. Myrna Weissman, from Columbia University, reviews the methods and findings of the Kendler et al. article and also emphasizes the critical significance of the early nurturing environment in relation to general health.
This issue concludes with an intriguing article on anxiety disorders, by Gold and colleagues ( 33 ), that demonstrates neural alterations during extinction recall that differ in children relative to adults. With increasing age, and in relation to fear and safety cues, nonanxious adults demonstrated greater connectivity between the amygdala and the ventromedial prefrontal cortex compared with anxious adults, as the cues were being perceived as safer. In contrast, neural differences between anxious and nonanxious youths were more robust when rating the memory of faces that were associated with threat. Specifically, these differences were observed in the activation of the inferior temporal cortex. In their editorial ( 34 ), Dr. Dylan Gee and Sahana Kribakaran, from Yale University, emphasize the importance of developmental work in relation to understanding anxiety disorders, place these findings into the context of other work, and suggest the possibility that these and other data point to neuroscientifically informed age-specific interventions.
Taken together, the papers in this issue of the Journal present new findings that shed light onto alterations in neural function that underlie major depressive disorder and anxiety disorders. It is important to remember that these disorders are highly comorbid and that their symptoms are frequently not separable. The papers in this issue also provide a developmental perspective emphasizing the importance of early rearing in the risk to develop depression and age-related findings important for understanding threat processing in patients with anxiety disorders. From a treatment perspective, the papers introduce data supporting more selective prefrontal cortical TMS targeting in relation to different symptoms, address the potential and drawbacks for considering the future use of psychedelics in our treatments, and present new ideas supporting age-specific interventions for youths and adults with anxiety disorders.
Disclosures of Editors’ financial relationships appear in the April 2020 issue of the Journal .
1 Substance Abuse and Mental Health Services Administration (SAMHSA): Key substance use and mental health indicators in the United States: results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53). Rockville, Md, Center for Behavioral Health Statistics and Quality, SAMHSA, 2018. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHFFR2017/NSDUHFFR2017.htm Google Scholar
2 Kessler RC, Chiu WT, Demler O, et al. : Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication . Arch Gen Psychiatry 2005 ; 62:617–627, correction, 62:709 Crossref , Medline , Google Scholar
3 Merikangas KR, He JP, Burstein M, et al. : Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) . J Am Acad Child Adolesc Psychiatry 2010 ; 49:980–989 Crossref , Medline , Google Scholar
4 Kessler RC, McGonagle KA, Zhao S, et al. : Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey . Arch Gen Psychiatry 1994 ; 51:8–19 Crossref , Medline , Google Scholar
5 Kessler RC, Sampson NA, Berglund P, et al. : Anxious and non-anxious major depressive disorder in the World Health Organization World Mental Health Surveys . Epidemiol Psychiatr Sci 2015 ; 24:210–226 Crossref , Medline , Google Scholar
6 Dunner DL : Management of anxiety disorders: the added challenge of comorbidity . Depress Anxiety 2001 ; 13:57–71 Crossref , Medline , Google Scholar
7 Kessler RC, Sonnega A, Bromet E, et al. : Posttraumatic stress disorder in the National Comorbidity Survey . Arch Gen Psychiatry 1995 ; 52:1048–1060 Crossref , Medline , Google Scholar
8 Brawman-Mintzer O, Lydiard RB, Emmanuel N, et al. : Psychiatric comorbidity in patients with generalized anxiety disorder . Am J Psychiatry 1993 ; 150:1216–1218 Link , Google Scholar
9 Fava M, Alpert JE, Carmin CN, et al. : Clinical correlates and symptom patterns of anxious depression among patients with major depressive disorder in STAR*D . Psychol Med 2004 ; 34:1299–1308 Crossref , Medline , Google Scholar
10 Hettema JM : What is the genetic relationship between anxiety and depression? Am J Med Genet C Semin Med Genet 2008 ; 148C:140–146 Crossref , Medline , Google Scholar
11 Hettema JM, Neale MC, Myers JM, et al. : A population-based twin study of the relationship between neuroticism and internalizing disorders . Am J Psychiatry 2006 ; 163:857–864 Link , Google Scholar
12 Kovner R, Oler JA, Kalin NH : Cortico-limbic interactions mediate adaptive and maladaptive responses relevant to psychopathology . Am J Psychiatry 2019 ; 176:987–999 Link , Google Scholar
13 Etkin A, Schatzberg AF : Common abnormalities and disorder-specific compensation during implicit regulation of emotional processing in generalized anxiety and major depressive disorders . Am J Psychiatry 2011 ; 168:968–978 Link , Google Scholar
14 Goodkind M, Eickhoff SB, Oathes DJ, et al. : Identification of a common neurobiological substrate for mental illness . JAMA Psychiatry 2015 ; 72:305–315 Crossref , Medline , Google Scholar
15 McTeague LM, Huemer J, Carreon DM, et al. : Identification of common neural circuit disruptions in cognitive control across psychiatric disorders . Am J Psychiatry 2017 ; 174:676–685 Link , Google Scholar
16 Beesdo K, Knappe S, Pine DS : Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V . Psychiatr Clin North Am 2009 ; 32:483–524 Crossref , Medline , Google Scholar
17 Kessler RC, Wang PS : The descriptive epidemiology of commonly occurring mental disorders in the United States . Annu Rev Public Health 2008 ; 29:115–129 Crossref , Medline , Google Scholar
18 Ohayon MM, Schatzberg AF : Social phobia and depression: prevalence and comorbidity . J Psychosom Res 2010 ; 68:235–243 Crossref , Medline , Google Scholar
19 Clauss JA, Blackford JU : Behavioral inhibition and risk for developing social anxiety disorder: a meta-analytic study . J Am Acad Child Adolesc Psychiatry 2012 ; 51:1066–1075 Crossref , Medline , Google Scholar
20 Fava M, Rush AJ, Alpert JE, et al. : Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report . Am J Psychiatry 2008 ; 165:342–351 Link , Google Scholar
21 Dold M, Bartova L, Souery D, et al. : Clinical characteristics and treatment outcomes of patients with major depressive disorder and comorbid anxiety disorders: results from a European multicenter study . J Psychiatr Res 2017 ; 91:1–13 Crossref , Medline , Google Scholar
22 Spellman T, Liston C : Toward circuit mechanisms of pathophysiology in depression . Am J Psychiatry 2020 ; 177:381–390 Link , Google Scholar
23 Reiff CM, Richman EE, Nemeroff CB, et al. : Psychedelics and psychedelic-assisted psychotherapy . Am J Psychiatry 2020 ; 177:391–410 Link , Google Scholar
24 Schatzberg AF : Some comments on psychedelic research (editorial). Am J Psychiatry 2020 ; 177:368–369 Link , Google Scholar
25 McTeague LM, Rosenberg BM, Lopez JW, et al. : Identification of common neural circuit disruptions in emotional processing across psychiatric disorders . Am J Psychiatry 2020 ; 177:411–421 Link , Google Scholar
26 Caspi A, Moffitt TE : All for one and one for all: mental disorders in one dimension . Am J Psychiatry 2018 ; 175:831–844 Link , Google Scholar
27 Barch DM : What does it mean to be transdiagnostic and how would we know? (editorial). Am J Psychiatry 2020 ; 177:370–372 Abstract , Google Scholar
28 Gray JP, Müller VI, Eickhoff SB, et al. : Multimodal abnormalities of brain structure and function in major depressive disorder: a meta-analysis of neuroimaging studies . Am J Psychiatry 2020 ; 177:422–434 Link , Google Scholar
29 Siddiqi SH, Taylor SF, Cooke D, et al. : Distinct symptom-specific treatment targets for circuit-based neuromodulation . Am J Psychiatry 2020 ; 177:435–446 Link , Google Scholar
30 Nestor SM, Blumberger DM : Mapping symptom clusters to circuits: toward personalizing TMS targets to improve treatment outcomes in depression (editorial). Am J Psychiatry 2020 ; 177:373–375 Abstract , Google Scholar
31 Kendler KS, Ohlsson H, Sundquist J, et al. : The rearing environment and risk for major depression: a Swedish national high-risk home-reared and adopted-away co-sibling control study . Am J Psychiatry 2020 ; 177:447–453 Abstract , Google Scholar
32 Weissman MM : Is depression nature or nurture? Yes (editorial). Am J Psychiatry 2020 ; 177:376–377 Abstract , Google Scholar
33 Gold AL, Abend R, Britton JC, et al. : Age differences in the neural correlates of anxiety disorders: an fMRI study of response to learned threat . Am J Psychiatry 2020 ; 177:454–463 Link , Google Scholar
34 Gee DG, Kribakaran S : Developmental differences in neural responding to threat and safety: implications for treating youths with anxiety (editorial). Am J Psychiatry 2020 ; 177:378–380 Abstract , Google Scholar
- Cited by None
- Neuroanatomy
- Neurochemistry
- Neuroendocrinology
- Other Research Areas

Personal Stories
We want to hear your story.
Tell us how mental illness has affected your life.
Share Your Story
Find Your Local NAMI
Call the NAMI Helpline at
800-950-6264
Or text "HelpLine" to 62640
My Depression in My Life
Depression is something that shows itself differently for everyone. There is no one person, or one story, or one experience that can make someone universally understand truly how depression alters the lives of those of us who suffer from it. I can’t make anyone understand how it is for everyone, but I can tell you how it alters my life, and maybe that will help people understand how all-encompassing it really is.
For me there are two main ways that my depression manifests itself when it breaks through the barriers I have set with the help of years of therapy and medication. There is the gut wrenching loneliness and near constant anxiety and then there is the checking out, the feeling nothing at all, the numbness. Sometimes I don’t know which is worse, but I will try to explain both.
The Loneliness and Anxiety:
In some ways I consider this step one of when my depression spikes because it always seems to come first. But I don’t consider it step one in levels of horribleness. Like I said above I really think that both ways my depression hits me are pretty awful and I couldn’t say which is worse.
You know that feeling you have in your gut when you are about to and/or really need to cry. While that is what it is like. All the time. I could be laughing and having a great time with my friends, which I often am because my friends are great, and yet in the back of my mind I feel more alone than ever and I just want to curl up into fetal position and cry. But I never can. I can’t go home and cry and then feel better, because it’s not like there is something to cry about, or really anything to be sad about. And it isn’t really sadness. It is complete solitude. It’s when my brain tells me that I am alone, that I can’t be loved, that no one really wants me around, and worst of all that no one will understand me.
That is worst of all because at the place I am in my life, no matter what I have been through in the past, or what my depression tries to make me believe I know that I can be loved, that I’m not alone and that I am wanted. And I know that because of the hard work I have done to get to that place in my life, and because of some of the amazing people in my life who make sure that I know that they are there for me, that they love me, and that they want to spend time with me.
But the idea that no one will ever truly understand who I am, or any of that. That is a little harder to dissuade myself from believing. Because as much as I can tell people what I went, and still go through and what goes through my mind, who can really understand me other than me. And that isn’t necessarily a bad thing, but the way my depression tells me it, it is a bad thing.
So there I am surrounded by people, very possibly having some of the best experiences of my life, feeling like I need to bawl, completely unable to, and nearly having an anxiety attack because I just want it to end.
And it is here where two things happen. It is here where I wish for and welcome the numbness because I don’t want to feel the all-encompassing loneliness and anxiety. It is also where I think about cutting.
I have not cut myself in three and a half years. And I know that it doesn’t solve my problems. I know that I shouldn’t and I don’t want to. Even when I want to I don’t want to.
But here, when I am feeling the all-encompassing loneliness which is the very last thing that I want to feel, I think about cutting because it lets me feel something else.
The physical act of cutting gives me something to think about and focus on, something other than that loneliness. And when I am not physically cutting, instead of thinking about how lonely I am and how that feeling will never end I think about the next time I can cut, or the most recent time I did.
And Then The Numbness:
I don’t really know how to explain this numbness. It is simply a period of time where I feel literally nothing. I fake happiness/normal emotion around friends, not always very well, and when I am alone I just don’t care about anything.
This is when my grades often fall because I don’t care about anything, including school, and therefore school work.
And then, sometimes I just want to feel something, anything, and so that is when I think about cutting. I think about cutting because it gives me something to feel, something I can control, but still feel.
The numbness comes because I can’t handle what I’m thinking and feeling, because it is too much for me to deal with, so I shut everything off so I don’t have to feel it.
In some ways, cutting transitions me back into feeling. But again, cutting, NOT A SOLUTION, NOT HEALTHY.
And something that I no longer do.
Now, for the past three and a half years, whenever I think of cutting, which I still do. It is still my first thought in either of these situations, I instead do one of the many things that I have come to know to help me cope.
For example, I force myself to spend more time with my friends, because I know that the loneliness will pass and I can talk myself out of feeling lonely when I am not physically alone.
I read/watch anything romantic. I pretend that I am one of the characters, and then I feel what they feel instead of what I am feeling (or preventing myself from feeling).
I belt along to old school Taylor Swift. Because what is more beautiful than a summer romance in a small country town with Chevy trucks and Tim McGraw?
And though my schoolwork does still sometimes fall through the cracks, I always make myself do some work.
Basically I force myself to live my life, because well, it is my life, and I refuse to live it feeling alone when I’m not, and numb when I could be great.
So even though I do feel those things far more often than I would like it is something that I live with, because I have depression.
Because depression is a disease, and I will always have it.
Because my depression is a part of who I am.
And most of all, because I only have one life, and I want to live it. Because even though when my depression spikes it makes me want to not live sometimes, I refuse.
Because I am the author of my own life and I choose to put a semicolon instead of a period at every point that my depression tells me otherwise.
So that is how my depression affects my life. That is how I deal with it. Like it or not I always will.
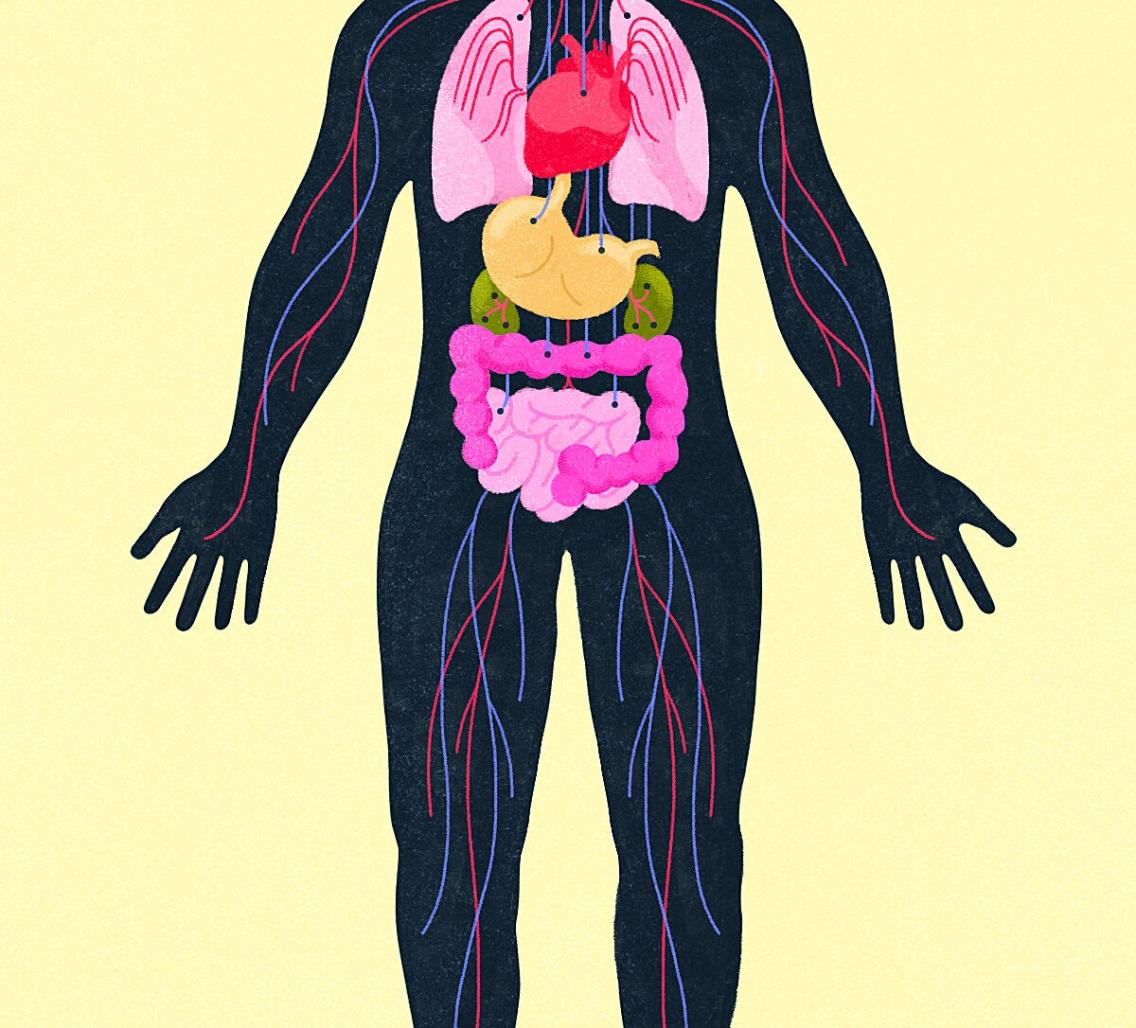
The Devastating Ways Depression and Anxiety Impact the Body
By Jane Brody
It’s no surprise that when a person gets a diagnosis of heart disease, cancer or some other life-limiting or life-threatening physical ailment, they become anxious or depressed. But the reverse can also be true: Undue anxiety or depression can foster the development of a serious physical disease, and even impede the ability to withstand or recover from one. The potential consequences are particularly timely, as the ongoing stress and disruptions of the pandemic continue to take a toll on mental health .
The human organism does not recognize the medical profession’s artificial separation of mental and physical ills. Rather, mind and body form a two-way street. What happens inside a person’s head can have damaging effects throughout the body, as well as the other way around. An untreated mental illness can significantly increase the risk of becoming physically ill, and physical disorders may result in behaviors that make mental conditions worse.
In studies that tracked how patients with breast cancer fared, for example, Dr. David Spiegel and his colleagues at Stanford University School of Medicine showed decades ago that women whose depression was easing lived longer than those whose depression was getting worse. His research and other studies have clearly shown that “the brain is intimately connected to the body and the body to the brain,” Dr. Spiegel said in an interview. “The body tends to react to mental stress as if it was a physical stress.”
Despite such evidence, he and other experts say, chronic emotional distress is too often overlooked by doctors. Commonly, a physician will prescribe a therapy for physical ailments like heart disease or diabetes, only to wonder why some patients get worse instead of better.
Many people are reluctant to seek treatment for emotional ills. Some people with anxiety or depression may fear being stigmatized, even if they recognize they have a serious psychological problem. Many attempt to self-treat their emotional distress by adopting behaviors like drinking too much or abusing drugs, which only adds insult to their pre-existing injury.
And sometimes, family and friends inadvertently reinforce a person’s denial of mental distress by labeling it as “that’s just the way he is” and do nothing to encourage them to seek professional help.
How common are anxiety and depression?
Anxiety disorders affect nearly 20 percent of American adults . That means millions are beset by an overabundance of the fight-or-flight response that primes the body for action. When you’re stressed, the brain responds by prompting the release of cortisol, nature’s built-in alarm system. It evolved to help animals facing physical threats by increasing respiration, raising the heart rate and redirecting blood flow from abdominal organs to muscles that assist in confronting or escaping danger.
These protective actions stem from the neurotransmitters epinephrine and norepinephrine, which stimulate the sympathetic nervous system and put the body on high alert. But when they are invoked too often and indiscriminately, the chronic overstimulation can result in all manner of physical ills, including digestive symptoms like indigestion, cramps, diarrhea or constipation, and an increased risk of heart attack or stroke.
Depression, while less common than chronic anxiety, can have even more devastating effects on physical health. While it’s normal to feel depressed from time to time, more than 6 percent of adults have such persistent feelings of depression that it disrupts personal relationships, interferes with work and play, and impairs their ability to cope with the challenges of daily life. Persistent depression can also exacerbate a person’s perception of pain and increase their chances of developing chronic pain.
“Depression diminishes a person’s capacity to analyze and respond rationally to stress,” Dr. Spiegel said. “They end up on a vicious cycle with limited capacity to get out of a negative mental state.”
Potentially making matters worse, undue anxiety and depression often coexist, leaving people vulnerable to a panoply of physical ailments and an inability to adopt and stick with needed therapy.
A study of 1,204 elderly Korean men and women initially evaluated for depression and anxiety found that two years later, these emotional disorders increased their risk of physical disorders and disability. Anxiety alone was linked with heart disease, depression alone was linked with asthma, and the two together were linked with eyesight problems, persistent cough, asthma, hypertension, heart disease and gastrointestinal problems.
Treatment can counter emotional tolls
Although persistent anxiety and depression are highly treatable with medications, cognitive behavioral therapy and talk therapy, without treatment these conditions tend to get worse. According to Dr. John Frownfelter, treatment for any condition works better when doctors understand “the pressures patients face that affect their behavior and result in clinical harm.”
Dr. Frownfelter is an internist and chief medical officer of a start-up called Jvion. The organization uses artificial intelligence to identify not just medical factors but psychological, social and behavioral ones as well that can impact the effectiveness of treatment on patients’ health. Its aim is to foster more holistic approaches to treatment that address the whole patient, body and mind combined.
The analyses used by Jvion, a Hindi word meaning life-giving, could alert a doctor when underlying depression might be hindering the effectiveness of prescribed treatments for another condition. For example, patients being treated for diabetes who are feeling hopeless may fail to improve because they take their prescribed medication only sporadically and don’t follow a proper diet, Dr. Frownfelter said.
“We often talk about depression as a complication of chronic illness,” Dr. Frownfelter wrote in Medpage Today in July . “But what we don’t talk about enough is how depression can lead to chronic disease. Patients with depression may not have the motivation to exercise regularly or cook healthy meals. Many also have trouble getting adequate sleep.”
Some changes to medical care during the pandemic have greatly increased patient access to depression and anxiety treatment. The expansion of telehealth has enabled patients to access treatment by psychotherapists who may be as far as a continent away.
Patients may also be able to treat themselves without the direct help of a therapist. For example, Dr. Spiegel and his co-workers created an app called Reveri that teaches people self-hypnosis techniques designed to help reduce stress and anxiety, improve sleep, reduce pain and suppress or quit smoking.
Improving sleep is especially helpful, Dr. Spiegel said, because “it enhances a person’s ability to regulate the stress response system and not get stuck in a mental rut.” Data demonstrating the effectiveness of the Reveri app has been collected but not yet published, he said.
Jane Brody is the Personal Health columnist, a position she has held since 1976. She has written more than a dozen books including the best sellers “Jane Brody’s Nutrition Book” and “Jane Brody’s Good Food Book.”
- Share full article
Advertisement
Supported by
Personal Health
The Devastating Ways Depression and Anxiety Impact the Body
Mind and body form a two-way street.

By Jane E. Brody
It’s no surprise that when a person gets a diagnosis of heart disease, cancer or some other life-limiting or life-threatening physical ailment, they become anxious or depressed. But the reverse can also be true: Undue anxiety or depression can foster the development of a serious physical disease, and even impede the ability to withstand or recover from one. The potential consequences are particularly timely, as the ongoing stress and disruptions of the pandemic continue to take a toll on mental health .
The human organism does not recognize the medical profession’s artificial separation of mental and physical ills. Rather, mind and body form a two-way street. What happens inside a person’s head can have damaging effects throughout the body, as well as the other way around. An untreated mental illness can significantly increase the risk of becoming physically ill, and physical disorders may result in behaviors that make mental conditions worse.
In studies that tracked how patients with breast cancer fared, for example, Dr. David Spiegel and his colleagues at Stanford University School of Medicine showed decades ago that women whose depression was easing lived longer than those whose depression was getting worse. His research and other studies have clearly shown that “the brain is intimately connected to the body and the body to the brain,” Dr. Spiegel said in an interview. “The body tends to react to mental stress as if it was a physical stress.”
Despite such evidence, he and other experts say, chronic emotional distress is too often overlooked by doctors. Commonly, a physician will prescribe a therapy for physical ailments like heart disease or diabetes, only to wonder why some patients get worse instead of better.
Many people are reluctant to seek treatment for emotional ills. Some people with anxiety or depression may fear being stigmatized, even if they recognize they have a serious psychological problem. Many attempt to self-treat their emotional distress by adopting behaviors like drinking too much or abusing drugs, which only adds insult to their pre-existing injury.
And sometimes, family and friends inadvertently reinforce a person’s denial of mental distress by labeling it as “that’s just the way he is” and do nothing to encourage them to seek professional help.
How common are anxiety and depression?
Anxiety disorders affect nearly 20 percent of American adults . That means millions are beset by an overabundance of the fight-or-flight response that primes the body for action. When you’re stressed, the brain responds by prompting the release of cortisol, nature’s built-in alarm system. It evolved to help animals facing physical threats by increasing respiration, raising the heart rate and redirecting blood flow from abdominal organs to muscles that assist in confronting or escaping danger.
These protective actions stem from the neurotransmitters epinephrine and norepinephrine, which stimulate the sympathetic nervous system and put the body on high alert. But when they are invoked too often and indiscriminately, the chronic overstimulation can result in all manner of physical ills, including digestive symptoms like indigestion, cramps, diarrhea or constipation, and an increased risk of heart attack or stroke.
Depression, while less common than chronic anxiety, can have even more devastating effects on physical health. While it’s normal to feel depressed from time to time, more than 6 percent of adults have such persistent feelings of depression that it disrupts personal relationships, interferes with work and play, and impairs their ability to cope with the challenges of daily life. Persistent depression can also exacerbate a person’s perception of pain and increase their chances of developing chronic pain.
“Depression diminishes a person’s capacity to analyze and respond rationally to stress,” Dr. Spiegel said. “They end up on a vicious cycle with limited capacity to get out of a negative mental state.”
Potentially making matters worse, undue anxiety and depression often coexist, leaving people vulnerable to a panoply of physical ailments and an inability to adopt and stick with needed therapy.
A study of 1,204 elderly Korean men and women initially evaluated for depression and anxiety found that two years later, these emotional disorders increased their risk of physical disorders and disability. Anxiety alone was linked with heart disease, depression alone was linked with asthma, and the two together were linked with eyesight problems, persistent cough, asthma, hypertension, heart disease and gastrointestinal problems.
Treatment can counter emotional tolls
Although persistent anxiety and depression are highly treatable with medications, cognitive behavioral therapy and talk therapy, without treatment these conditions tend to get worse. According to Dr. John Frownfelter, treatment for any condition works better when doctors understand “the pressures patients face that affect their behavior and result in clinical harm.”
Dr. Frownfelter is an internist and chief medical officer of a start-up called Jvion. The organization uses artificial intelligence to identify not just medical factors but psychological, social and behavioral ones as well that can impact the effectiveness of treatment on patients’ health. Its aim is to foster more holistic approaches to treatment that address the whole patient, body and mind combined.
The analyses used by Jvion, a Hindi word meaning life-giving, could alert a doctor when underlying depression might be hindering the effectiveness of prescribed treatments for another condition. For example, patients being treated for diabetes who are feeling hopeless may fail to improve because they take their prescribed medication only sporadically and don’t follow a proper diet, Dr. Frownfelter said.
“We often talk about depression as a complication of chronic illness,” Dr. Frownfelter wrote in Medpage Today in July . “But what we don’t talk about enough is how depression can lead to chronic disease. Patients with depression may not have the motivation to exercise regularly or cook healthy meals. Many also have trouble getting adequate sleep.”
Some changes to medical care during the pandemic have greatly increased patient access to depression and anxiety treatment. The expansion of telehealth has enabled patients to access treatment by psychotherapists who may be as far as a continent away.
Patients may also be able to treat themselves without the direct help of a therapist. For example, Dr. Spiegel and his co-workers created an app called Reveri that teaches people self-hypnosis techniques designed to help reduce stress and anxiety, improve sleep, reduce pain and suppress or quit smoking.
Improving sleep is especially helpful, Dr. Spiegel said, because “it enhances a person’s ability to regulate the stress response system and not get stuck in a mental rut.” Data demonstrating the effectiveness of the Reveri app has been collected but not yet published, he said.
Jane Brody is the Personal Health columnist, a position she has held since 1976. She has written more than a dozen books including the best sellers “Jane Brody’s Nutrition Book” and “Jane Brody’s Good Food Book.” More about Jane E. Brody
Jane Brody’s Personal Health Advice
After joining the new york times in 1965, she was its personal health columnist from 1976 to 2022. revisit some of her most memorable writing:.
Brody’s first column, on jogging , ran on Nov. 10, 1976. Her last, on Feb. 21. In it, she highlighted the evolution of health advice throughout her career.
Personal Health has often offered useful advice and a refreshing perspective. Declutter? This is why you must . Cup of coffee? Yes, please.
As a columnist, she has never been afraid to try out, and write about, new things — from intermittent fasting to knitting groups .
How do you put into words the pain of losing a spouse of 43 years? It is “nothing like losing a parent,” she wrote of her own experience with grieving .
Need advice on aging? She has explored how to do it gracefully , building muscle strength and knee replacements .
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Anxiety vs. Depression Symptoms and Treatment
Overlapping and distinguishing features of anxiety and depression
:max_bytes(150000):strip_icc():format(webp)/Deborah-R.-Glasofer-PhD-1000-7cac259d94c641a7b388a605ec430842.jpg)
Amy Morin, LCSW, is a psychotherapist and international bestselling author. Her books, including "13 Things Mentally Strong People Don't Do," have been translated into more than 40 languages. Her TEDx talk, "The Secret of Becoming Mentally Strong," is one of the most viewed talks of all time.
:max_bytes(150000):strip_icc():format(webp)/VW-MIND-Amy-2b338105f1ee493f94d7e333e410fa76.jpg)
The terms “anxious” and “depressed” get thrown around a lot in casual conversation—and for good reason. Both are normal emotions to experience, routinely occurring in response to high-stakes or potentially dangerous situations (in the case of anxiety) or disappointing, upsetting circumstances (in the case of depression).
The relationship between these emotions—and their associated clinical conditions, anxiety disorders and mood disorders—is complex and somewhat idiosyncratic.
For one person, anxiety can lead to avoidance and isolation. Isolation can result in a lack of opportunity for pleasurable experiences, which then leads to low mood. For others, the emotions may flow in the opposite direction. Feeling down may zap someone of the energy to do things they typically enjoy, and attempts to re-engage with the world after being out of practice may result in nervousness.
Understanding the distinctions between the two emotions (anxiety vs. depression) and characterizing the severity of the problem can help you to determine how to feel better.
The Relationship Between Anxiety and Depression
Anxiety and depression share a biological basis. Persistent states of anxiety or low mood like those experienced by people with clinical anxiety and mood disorders involve changes in neurotransmitter function. Low serotonin levels are thought to play a role in both, along with other brain chemicals such as dopamine and epinephrine.
While the biological underpinnings of these problems are similar, anxiety and depression are experienced differently. In this way, the two states might be considered two sides of the same coin.
Anxiety and depression can occur sequentially (one in reaction to the other), or they can co-occur. When anxiety and mood problems reach the threshold for clinical diagnosis simultaneously, the specific diagnoses are considered comorbid conditions .
Mental Differences: Anxiety vs. Depression
Anxiety and depression have distinct psychological features. Their mental markers (symptoms or expressions of the condition) are different.
Mental Markers of Anxiety
People with anxiety may:
Worry about the immediate or long-term future
- Have uncontrollable, racing thoughts about something going wrong
- Avoid situations that could cause anxiety so that feelings and thoughts don’t become consuming
- Think about death , in the sense of fearing death due to the perceived danger of physical symptoms or anticipated dangerous outcomes
Depending on the nature of the anxiety, these mental markers can vary. For example, someone with generalized anxiety disorder (GAD) may worry about a variety of topics, events, or activities. A person with social anxiety disorder (SAD) , on the other hand, is more apt to fear negative evaluation or rejection by others and to be apprehensive about meeting new people or other socially challenging situations.
Obsessions are unrealistic thoughts or mental impulses (sometimes with a magical quality) that extend beyond everyday worries. They are the hallmark mental manifestation of anxiety in people with obsessive-compulsive disorder (OCD) .
Simply put, people with anxiety are mentally preoccupied with worry to a degree that is disproportionate with actual risk or reality.
Mental Markers of Depression
People with depression may:
- Be hopeless , assuming that nothing positive will happen in the future for themselves, for others, or for the world
- Believe it is not worth trying to think or feel differently, because of this hopelessness
- Feel worthless , as if who they are or what they do is not valuable
- Think about death due to a persistent belief that life is not worth living or that the individual is a burden on others. In cases of moderate to severe depression, more specific suicidal thoughts can be present.
Have uncontrollable, racing thoughts
Avoid situations that could cause anxiety
Think about death due to perceived danger
Feel hopeless about themselves, others, the world
Believe it is not worth trying
Feel worthless
Think about death due to a persistent belief that life is not worth living
In major depressive disorder (MDD), these types of thoughts are persistent most of the day and more days than not for weeks on end. If a person vacillates between a very low and very high mood state, then a diagnosis of bipolar disorder may apply. For any variant of a mood disorder , the low mood state is likely to be characterized by the type of thinking described above.
If you are having suicidal thoughts, contact the National Suicide Prevention Lifeline at 988 for support and assistance from a trained counselor. If you or a loved one are in immediate danger, call 911.
For more mental health resources, see our National Helpline Database .
Physical Differences: Anxiety vs. Depression
The physical symptoms of both anxiety or depression can be exhausting for the afflicted individual.
Physical Signs of Anxiety
The physical state of anxiety can be conceptualized overall as that of heightened arousal . Specific characteristics include:
- Difficulty concentrating due to state of agitation or racing thoughts
- Difficulty falling or staying asleep due to racing thoughts or other physical symptoms
- Gastrointestinal distress (e.g., nausea, diarrhea, or constipation)
- Increased heart rate, blood pressure, sweating
- Muscle tension
- Shortness of breath
Physical Signs of Depression
Depression is primarily characterized by changes in usual physical processes from baseline, such as:
- Difficulty with concentration, focus, and memory due to ruminative thought processes or other physical symptoms
- Lack of energy
- Loss of appetite or a significant increase in appetite
- Moving or talking more slowly than usual
- Physical achiness without cause
- Sleeping much more or much less than is typical due to ruminative thought processes or low energy
Symptom Severity
It is not unusual to experience brief periods of low mood or anxiety, particularly in response to certain life stressors (for example, loss of a loved one, receiving a diagnosis of a physical illness, starting a new job or school, experiencing financial problems, etc.).
To meet the diagnostic threshold of an anxiety disorder, however, symptoms must be persistent (often for several months) and impairing.
Mood disorders are diagnosed when the associated symptoms occur more often than not for at least a couple of weeks.
To assess the severity of your symptoms:
- Ask yourself some key questions about how much the symptoms are getting in the way of your day-to-day functioning. You might also ask trusted friends and family members if they have noticed changes in you and your behavior, and if so, what those changes are.
- Read about typical presentations of mild, moderate, and severe versions of depression or anxiety.
- Track your psychological and physical symptoms for a week or two to get an accurate representation of fluctuations in mood and anxiety.
Treatment for Anxiety and Depression
Even if you decide that your anxiety or mood problem is a low-grade issue for you, it is still worth working on. Consider how much it is interfering with your life, and in what ways, to determine what kinds of interventions might be helpful.
Self-Help Approaches
If your symptoms are mild, tending to ebb and flow, or if you have had formal treatment previously and are concerned about relapse, self-help interventions can be a reasonable place to start.
These approaches can include self-help books and phone apps that adapt evidence-based psychotherapies or offer a way to practice skills that target a symptom (such as mindfulness meditation for anger or anxiety).
If your symptoms are persistent, are impacting your relationships and ability to fulfill various responsibilities, or are clearly noticeable to others, then more formal treatment is worth considering.
Psychotherapy
For depression and/or anxiety problems, there are several types of talk therapy. In structured psychotherapy, like cognitive behavioral therapy (CBT), the treatment approach for anxiety and depression can vary slightly. For both issues, CBT will teach you how to work with unhelpful thought traps. And, for either problem, CBT is likely to ask that you do more behaviorally.
For anxiety, the goal is to minimize avoidant behavior and to help you disconfirm a feared consequence. For depression, the goal is to help you experience positive emotion, a surge in energy (even if briefly), or another type of pleasant interaction with the world. The theory is that activating behavior, even when—or especially when—your energy or mood is low, can result in some type of positive reward.
In psychodynamic talk therapy , sessions for anxiety and depression may look more alike than different. You will be asked to speak freely about the past and the present in order to become aware of unconscious thoughts and conflicts underlying your symptoms.
Do not despair if you think you are experiencing separate, co-occurring anxiety and mood symptoms. There is an overlap in effective psychotherapies for these problems.
Medications
A group of medications known as selective serotonin reuptake inhibitors (SSRIs) has been shown to be helpful for both anxiety and depression. Other medications that may be used depending on your symptoms include tricyclic antidepressants (TCAs), selective norepinephrine reuptake inhibitors (SNRIs), and anti-anxiety medications.
How to Seek Help
When seeking more formalized help for anxiety or depression, start by speaking with your primary care physician.
You can also research local referrals via national organizations including:
- The Anxiety and Depression Association of America
- The Association for Behavioral and Cognitive Therapies
- The Association for Contextual Behavioral Science
- The American Psychiatric Association
Bear in mind that while effective treatment for anxiety or depression need not be a long-term commitment, it is likely to require regular, ongoing appointments at least in the short term (say, six to 12 months). Therefore, it is critical to find a professional you trust and with whom you feel comfortable speaking about your symptoms.
It is equally important to make sure that you find a clinician that you can afford. Before making the commitment to ongoing care, you may want to meet with a couple of providers to get a feel for their therapeutic styles and their treatment recommendations. You can then use this information to determine which path forward feels best to you.
Watson D, Naragon-Gainey K. Personality, emotions, and the emotional disorders . Clin Psychol Sci . 2014;2(4):422-442. doi:10.1177/2167702614536162
Deakin J. The role of serotonin in depression and anxiety . Eur Psychiatry. 1998;13 Suppl 2:57s-63s. doi:10.1016/S0924-9338(98)80015-1
Otte C, Gold SM, Penninx BW, et al. Major depressive disorder . Nat Rev Dis Primers. 2016;2:16065. doi:10.1038/nrdp.2016.65
Cisler JM, Olatunji BO. Emotion regulation and anxiety disorders . Curr Psychiatry Rep . 2012;14(3):182-187. doi:10.1007/s11920-012-0262-2
Bystritsky A, Khalsa SS, Cameron ME, Schiffman J. Current diagnosis and treatment of anxiety disorders . P T . 2013;38(1):30-57.
David D, Cristea I, Hofmann SG. Why cognitive behavioral therapy is the current gold standard of psychotherapy . Front Psychiatry . 2018;9:4. doi:10.3389/fpsyt.2018.00004
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition . Arlington, VA: American Psychiatric Association, 2013.
By Deborah R. Glasofer, PhD Deborah Glasofer, PhD is a professor of clinical psychology and practitioner of cognitive behavioral therapy.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Anxiety and Depression Overlap: Link Between Comorbid Disorders
- How They Feel
- When Treatment-Resistant
Having depression and anxiety at the same time is somewhat common. Research shows that 60% of people with anxiety will also have symptoms of depression. The rate is the same for those who have depression with symptoms of anxiety.
Anxiety and depression are two distinct conditions that can occur at the same time. This can make symptoms more complex. However, the same treatments can address both problems. They can often improve with psychotherapy (talk therapy), drugs, or both.
This article describes the link between anxiety and depression. It also explains their symptoms, diagnosis, and treatment when they occur at the same time.
MementoJpeg / Getty Images
Anxiety and Depression: An Indirect or Direct Link?
The relationship between anxiety and depression is complex. While depression is typically regarded as a low-energy condition and anxiety a high-energy condition, these disorders and their symptoms commonly occur together. The reason they are often linked is well understood, though several potential factors exist.
Many of the same factors that predispose you to anxiety also make you vulnerable to depression. Both are considered internalizing disorders, problems that are developed and maintained to a great extent within the affected person.
Like other internalizing disorders, anxiety and depression are linked to similar factors that include genetic risk and neuroticism (the tendency toward negative thoughts). They are also associated with several shared nongenetic risk factors such as early trauma and current stress.
Anxiety and depression have many overlapping symptoms because they both involve changes in the function of neurotransmitters like serotonin in your brain. Your symptoms may meet the criteria of both disorders.
The relationship between anxiety and depression may not be a situation in which one causes the other, but the fact that they may be two sides of the same coin. Being depressed can often make you feel worried or anxious. Similarly, having an anxiety attack can make you feel hopeless with depression.
Related Causes/Risk Factors
While the exact causes of comorbid depression and anxiety are not known, the following risk factors increase your chances of having these disorders together:
- Lifetime history of anxiety or depression
- Adversity during childhood
- Poor parenting
- Recent major life events
- Current exposure to stress
- High neuroticism
- Substance use disorders
- Family history
How Anxiety and Depression Symptoms Feel
Symptoms of anxiety and depression can vary by individual. However, both disorders can cause symptoms that can interfere with daily life and interpersonal relationships.
Similarities
Symptoms common in both anxiety and depression include:
- Problems with digestion
- Unintended changes in appetite or weight
- Inability to concentrate or make decisions
- Problems sleeping, either too much or too little
- Feeling constantly restless or irritable
Differences
Worrying is normal in some situations. Anxiety differs from normal worrying because it involves excessive fear that can be debilitating. Symptoms that may be characteristic of anxiety include:
- Constantly feeling wound up or restless
- Ongoing excessive worry about the immediate or long-term future
- Focusing on negative outcomes when decision-making
- Uncontrollable, racing thoughts about something going wrong
- Avoiding situations that could cause worry and anxiety
- Feeling a lack of certainty
The key characteristics of depression involve a persistent feeling of extremely low mood and/or loss of interest in activities you once enjoyed. Symptoms that may be characteristic of depression include:
- Feelings of sadness and persistent low mood
- Lack of interest or enjoyment in life experiences
- Loss of energy or extreme fatigue
- Increase in purposeless physical activities such as hand-wringing that is noticeable to others
- Increase in slowed movements or speech that occur often enough to be noticed by others
- Feelings of worthlessness or guilt
- Emphasis on loss or deprivation
- Thoughts of death or suicide
Help Is Available
If you or someone you know is having suicidal thoughts, call or text 988 to contact the 988 Suicide & Crisis Lifeline and connect with a trained counselor. If you or they are in immediate danger, dial 911 .
For more mental health resources, see our National Helpline Database .
Anxiety, Depression, or Both: How to Diagnose Symptoms
Many symptoms of anxiety and depression overlap, making it harder to determine which disorder is causing the problem. When anxiety and depression occur together, symptoms tend to be more intense and persistent because they work together. This can make your condition harder to diagnose and more complex to treat.
Diagnosing symptoms of a mental health disorder requires a comprehensive evaluation by a mental health provider. This can help ensure you get an accurate diagnosis and treatment.
Symptoms that might indicate that both anxiety and depression exist include:
- Persistent irrational fears or worries
- Physical symptoms like fatigue, headaches , labored breathing , abdominal pain , or rapid heartbeat
- Persistent feelings of worthlessness or sadness
- Problems going to sleep or staying asleep
- Difficulty remembering or concentrating
- Inability to make decisions
- Loss of interest in hobbies or activities
- Constantly feeling tired and cranky
- Panic attacks or a sense of losing inner control
- Inability to live in the moment and relax
Role of Gut Microbiome
Gut microbiome includes all the microorganisms living in your digestive system. It affects your digestive health as well as your overall health.
Research indicates that there is evidence of a link between gut microbes and depression. It is attributed to the gut and brain connection, called the gut-brain axis. Evidence shows that inflammation caused by gut microbes can influence mood in depression.
How to Cope With Comorbid Anxiety and Depression
There is no single treatment appropriate for every case of comorbid (co-occurring) anxiety and depression. Therapies typically include antidepressant drugs and/or a form of psychotherapy. Self-care can help you maintain your progress.
While research indicates that a combination of medication and therapy can provide the best results, your treatment plan may differ. Depending on your symptoms, you may be advised to start your treatment with either one of these therapies.
Self-care includes behaviors that support your physical and mental well-being. It involves actions that can help manage symptoms of anxiety and/or depression and complement therapy and/or medications.
The following strategies are ways to prioritize self-care:
- Establish and maintain a regular exercise routine with a target of 30 minutes daily. Exercising for smaller amounts of time can also make a difference.
- Follow a diet of nutritious meals and adequate hydration. Limit caffeinated beverages, alcohol, and added sugar.
- Maintain proper sleep hygiene , which involves following a daily sleep schedule and other behaviors supporting a good night's sleep.
- Try activities that involve relaxation, meditation, and breathing exercises to relieve stress and reduce feelings linked with anxiety and depression.
- Remain connected with friends or family members you can count on to provide practical help and emotional support if needed.
- Practice gratitude by journaling to remind yourself of the positive things in your life.
- Establish goals and priorities to avoid taking on new tasks and responsibilities that can overwhelm you.
Therapy is regarded as a key part of treatment for symptoms that involve anxiety and/or depression. Your results and the time it takes to achieve them depend on your symptoms and your unique situation.
The following types of therapy are used to treat anxiety and depression:
- Cognitive behavioral therapy (CBT) : This type of psychotherapy is considered the gold standard for treating anxiety and depression, among other mental health conditions.
- CBT is a time-limited and goal-oriented therapy. It focuses on changing negative thought patterns by altering negative behaviors and emotions.
- Interpersonal therapy (IPT) : This type of time-limited psychotherapy helps you see emotions as social signals so you can use them to improve interpersonal challenges. Rather than focusing on your past, IPT focuses on communication and current interpersonal relationships and issues you're having related to them.
- Dialectical behavioral therapy (DBT) : DBT is a modified version of CBT that focuses on healthy ways to live in the moment, regulate emotions, and improve interpersonal relationships. It integrates mindfulness skills, interpersonal effectiveness, distress tolerance, and emotion regulation into treatment.
- Acceptance and commitment therapy (ACT) : ACT is a type of psychotherapy that focuses on mindfulness, remaining in the present, and strategies for behavioral changes. It focuses on helping you become psychologically flexible so you can accept difficult thoughts and emotions while committing to meaningful life activities consistent with your goals and values.
With Medication
Medication for anxiety and/or depression works by increasing the activity of neurotransmitters, like serotonin , dopamine , norepinephrine , and gamma-aminobutyric acid ( GABA ). These are the chemical messengers in your brain that affect mood regulation.
The type of medication you receive depends on your symptoms and other factors regarding your overall condition. The following classes of medications are commonly used:
Selective serotonin reuptake inhibitors (SSRIs) : SSRIs are the first-line treatments preferred for treating depression and many comorbid anxiety disorders. They work by increasing serotonin levels.
SSRIs include:
- Celexa ( citalopram )
- Lexapro ( escitalopram )
- Paxil ( paroxetine )
- Prozac ( fluoxetine )
- Zoloft ( sertraline )
Serotonin-norepinephrine reuptake inhibitors (SNRIs) : SNRIs increase levels of serotonin and norepinephrine. These drugs are also acceptable first-line treatments for comorbid anxiety and depression.
SNRIs include:
- Effexor ( venlafaxine )
- Pristiq ( desvenlafaxine )
- Cymbalta ( duloxetine )
- Savella ( milnacipran ):
- Fetzima ( levomilnacipran ):
Tricyclic antidepressants (TCAs) : TCAs boost levels of serotonin and norepinephrine. TCAs include:
- Elavil ( amitriptyline )
- Pamelor ( nortriptyline )
- Tofranil ( imipramine )
- Norpramin ( desipramine )
- Anafranil ( clomipramine )
Monoamine oxidase inhibitors (MAOIs) : MAOIs were the first class of antidepressants. They are generally regarded as outdated because of their side effects, though they may be appropriate for treatment-resistant depression in its later stages.
MAOIs include:
- Marplan ( isocarboxazid )
- Nardil ( phenelzine )
- Emsam ( selegiline patch)
Treatment-Resistant Depression (With Anxiety)
Treatment-resistant depression (with anxiety) describes depression that hasn't responded to an adequate trial of at least two different antidepressants. Research indicates that the situation is not uncommon. Between 29% and 46% of people with depression show partial or no response to treatments.
Therapies for treatment-resistant depression (with anxiety) involve the following:
- Transcranial magnetic stimulation (TMS) : TMS is a noninvasive treatment that involves placing electromagnets on your head. The magnets send hundreds of thousands of targeted magnetic pulses to stimulate and reset the neurological processes regulating mood.
- Electroconvulsive therapy (ECT) : ECT, previously known as electroshock therapy, is a procedure in which controlled electric currents are passed through your brain while you are under anesthesia. Treatment is usually given two or three times a week for six to 12 weeks, depending on your symptoms and response.
- Ketamine : Ketamine has been used as an anesthetic in surgeries for many years. It is also used off-label for treatment-resistant depression. It works by targeting subsets of neurotransmitters that are different from those affected by traditional antidepressants. Ketamine is delivered by intravenous infusion (directly into your vein) in a procedure that takes up to an hour.
- Spravato (esketamine): Esketamine is a ketamine formulation approved by the Food and Drug Administration (FDA) for depression. Esketamine is more potent than ketamine, so it may produce results with lower doses than ketamine. It is administered as an intranasal spray in monitored treatment sessions over a few weeks.
Feelings of sadness and worry are normal. However, when these types of feelings intrude on your daily life, they may be signs of mental health problems.
Anxiety and depression are two of the most commonly diagnosed mental health problems. While they are two distinct conditions, they often occur at the same time.
When these disorders occur together, treatments are more complex. Symptoms can overlap and often worsen when more than one mental health problem exists. The good news is that treating these comorbid disorders is most effective when they are handled at the same time.
National Association on Mental Illness NAMI. The comorbidity of anxiety and depression .
Hartgrove Behavioral Health System. The relationship between anxiety and depression .
Kalin NH. The critical relationship between anxiety and depression . AJP . 2020;177(5):365-367. doi:10.1176/appi.ajp.2020.20030305
Hopwood M. Anxiety symptoms in patients with major depressive disorder: commentary on prevalence and clinical implications . Neurol Ther . 2023;12(1):5-12. doi:10.1007/s40120-023-00469-6
Möller HJ, Bandelow B, Volz HP, Barnikol UB, Seifritz E, Kasper S. The relevance of ‘mixed anxiety and depression’ as a diagnostic category in clinical practice . Eur Arch Psychiatry Clin Neurosci . 2016;266(8):725-736. doi:10.1007/s00406-016-0684-7
Cleveland Clinic Health Essentials. Anxiety vs. depression: which do I have (or is it both)?
Mental Health Foundation. Generalized anxiety disorder .
American Psychiatric Association. What is depression?
Pennisi E. Gut microbe linked to depression in large health study . Science . Published online February 4, 2022. doi:10.1126/science.ada0998
Harvard Health Publishing Harvard Medical School. Medication or therapy for depression? Or both?
National Institute of Mental Health. Caring for your mental health .
David D, Cristea I, Hofmann SG. Why cognitive behavioral therapy is the current gold standard of psychotherapy . Front Psychiatry . 2018;9. doi:10.3389/fpsyt.2018.00004
Coffey SF, Banducci AN, Vinci C. Common questions about cognitive behavior therapy for psychiatric disorders . Am Fam Physician . 2015;92(9):807-812. PMID: 26554473.
International Society of Interpersonal Psychotherapy. Overview of IPT .
The Linehan Institute Behavioral Tech. What is dialectical behavior therapy (DBT)? .
Dindo L, Van Liew JR, Arch JJ. Acceptance and commitment therapy: a transdiagnostic behavioral intervention for mental health and medical conditions . Neurotherapeutics . 2017;14(3):546-553. doi:10.1007/s13311-017-0521-3
Centre for Addiction and Mental Health (CAMH). Antidepressant medications .
Coplan JD, Aaronson CJ, Panthangi V, Kim Y. Treating comorbid anxiety and depression: Psychosocial and pharmacological approaches . World Journal of Psychiatry . 2015;5(4):366. doi:10.5498/wjp.v5.i4.366
UpToDate. Patient education: medicines for depression (the basics) .
Columbia University Department of Psychiatry. Finding solutions when depression resists treatment .
UCSanDiego Health. Transcranial magnetic stimulation .
American Psychiatric Association. What is electroconvulsive therapy?
Nebraska Medicine. What is esketamine, and is it effective in treating depression?
Yale Medicine. How ketamine drug helps with depression .
By Anna Giorgi Giorgi is a freelance writer with more than 25 years of experience writing health and wellness-related content.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Anxiety, Depression and Quality of Life—A Systematic Review of Evidence from Longitudinal Observational Studies
Associated data.
Not applicable.
This review aimed to systematically review observational studies investigating the longitudinal association between anxiety, depression and quality of life (QoL). A systematic search of five electronic databases (PubMed, PsycINFO, PSYNDEX, NHS EED and EconLit) as well as forward/backward reference searches were conducted to identify observational studies on the longitudinal association between anxiety, depression and QoL. Studies were synthesized narratively. Additionally, a random-effects meta-analysis was performed using studies applying the mental and physical summary scores (MCS, PCS) of the Short Form Health Survey. The review was prospectively registered with PROSPERO and a study protocol was published. n = 47 studies on heterogeneous research questions were included, with sample sizes ranging from n = 28 to 43,093. Narrative synthesis indicated that QoL was reduced before disorder onset, dropped further during the disorder and improved with remission. Before onset and after remission, QoL was lower in comparison to healthy comparisons. n = 8 studies were included in random-effects meta-analyses. The pooled estimates of QoL at follow-up (FU) were of small to large effect sizes and showed that QoL at FU differed by disorder status at baseline as well as by disorder course over time. Disorder course groups differed in their MCS scores at baseline. Effect sizes were generally larger for MCS relative to PCS. The results highlight the relevance of preventive measures and treatment. Future research should consider individual QoL domains, individual anxiety/depressive disorders as well as the course of both over time to allow more differentiated statements in a meta-analysis.

1. Introduction
The World Health Organization [ 1 ] estimates that 264 million people worldwide were suffering from an anxiety disorder and 322 million from a depressive disorder in 2015, corresponding to prevalence rates of 3.6% and 4.4%. While their prevalence varies slightly by age and gender [ 1 ], they are among the most common mental disorders in the general population [ 2 , 3 , 4 , 5 , 6 ]. During the COVID-19 pandemic, multiple challenges have arisen for many, such as loneliness [ 7 ] or financial hardship. A meta-analysis showed a prevalence of anxiety of about 32% (95% CI: 28–37) and a prevalence of depression ( n = 14 studies) of about 34% (95% CI: 28–41) in general populations during the COVID-19 pandemic [ 8 ].
Anxiety and depression have been associated with adverse societal and individual correlates, including higher health care costs [ 9 , 10 , 11 ] and an increased risk for physical comorbidities, such as cardiovascular illnesses [ 12 , 13 ]. Moreover, they have been linked to a reduced quality of life (QoL) in numerous cross-sectional as well as longitudinal studies in which they significantly predicted QoL outcomes [ 14 , 15 , 16 , 17 , 18 ]. Other studies have reported a reverse association, whereby QoL was predictive of mental health outcomes [ 19 ] or a bi-directional association [ 20 , 21 ]. Some very recent studies also examined these associations among quite different samples (e.g., [ 22 , 23 , 24 , 25 ]).
Looking at longitudinal rather than cross-sectional data from observational studies has several advantages. It allows for the identification of trajectories over time within the same individuals rather than focusing on group differences at one point in time only [ 26 ]. Moreover, when appropriate methods are applied to longitudinal data, intraindividual heterogeneity can be taken into account, resulting in more consistent estimates [ 27 ]. This has previously been demonstrated in QoL research [ 28 ]. A need to analyze longitudinal changes in QoL domains in QoL research in people with mental disorders has also been previously identified [ 29 ]. Beyond individual longitudinal studies suggesting a link between anxiety or depression and QoL, several systematic reviews have synthesized longitudinal evidence on these associations and mostly reported negative associations between the variables. These reviews have tended to focus on specific age groups, such as older adults [ 30 ], samples with specific diseases [ 31 , 32 ], or have investigated the effect of specific treatments on QoL in patients with anxiety [ 33 ]. Investigating these associations in samples without these limitations could reduce the effect of specific conditions and treatments on the association and strengthen the conclusions that can be drawn.
In light of the previous findings, this study aims to add to the present literature by systematically synthesizing evidence from observational studies on the longitudinal association between anxiety, depression and QoL across all age groups in samples who do not have other specific illnesses and do not receive specific treatments.
2. Materials and Methods
This review was registered with PROSPERO (CRD42018108008) and a study protocol was published [ 34 ].
2.1. Search Strategy
Five electronic databases from several fields of research (PubMed, PsycINFO, PSYNDEX, NHS EED and EconLit) were examined until December 2020. Where possible, search terms were entered as Medical Subject Headings (MeSH) or as keywords in the title/abstract. The PubMed search strategy was: (anxi*[Title/Abstract] or depress*[Title/Abstract] or anxiety disorder[MeSH] or depressive disorder[MeSH]) and quality of life[MeSH] and longitudinal study[MeSH]. Please note that “*” is a truncation symbol. Time or location were not restricted. In addition, we applied backward and forward reference searches of included studies to identify additional references. The forward reference search was conducted until January 2021 using Web of Science to identify cited papers.
2.2. Study Selection Process
The study selection process is displayed in Figure 1 . Most identified studies were screened in a two-step process (title/abstract; full-text screening) independently by two reviewers (J.K.H., E.Q.) against defined criteria (see Table 1 ). The last updated literature screening before submission was conducted by one reviewer (J.K.H.) and encompassed 9% of the studies included for title/abstract screening. Before the final criteria were applied, they were pretested and refined. Disagreements during the selection process were resolved through discussion or by the inclusion of a third party (A.H.) if a consensus could not be reached.

Study flow (PRISMA flow chart).
Study selection criteria.
Abbreviations: QoL = quality of life; ICD = International Classification of Diseases; DSM = Diagnostic and Statistical Manual of Mental Disorders; BL = study baseline; KIDSCREEN = Health Related Quality of Life Questionnaire for Children and Young People and their Parents; KINDL = German generic quality of life instrument for children
2.3. Data Extraction and Synthesis
We extracted information regarding the study design, operationalization of the variables, sample characteristics, statistical methods and results regarding the research question of interest. If several analyses were presented for the same research question, we extracted the final covariate-adjusted model for narrative synthesis. Data were extracted by one reviewer (J.K.H.) and cross-checked by a second reviewer (E.Q.). If needed, extracted data were standardized (e.g., by calculating the weighted average means when combining groups) to present comparable information. If clarification was needed, the corresponding authors were contacted.
For the narrative synthesis, all studies were first grouped by research question, e.g., whether disorders or the degree of symptoms were analyzed, which comparison groups were used, which QoL domains were considered, and at which waves the variables of interest were considered in the analyses. Because research questions and analyses were heterogeneous, a concise narrative synthesis of the main results of all studies was not feasible. Therefore, we provide an overview of all identified studies in the tables and a detailed narrative synthesis of those studies, analyzing trajectories of disorders or changes in symptoms in association with changes in QoL over time.
Additionally, we examined whether data were appropriate for meta-analysis. The specific research questions, the operationalization of main variables and statistical methods were heterogeneous across studies and not all the statistical estimates needed could be obtained from covariate-adjusted analyses. Therefore, to enhance the comparability of the underlying data and the interpretation of the pooled estimates, we used descriptive information. Because most papers applied variations of the Short Form Health Survey and analyzed mental and physical component scores (MCS, PCS), we considered these studies as eligible for meta-analysis. The necessary information could be obtained for 8 publications. Random-effects meta-analysis was used for pooling. Heterogeneity was assessed by means of I 2 , with higher values representing a larger degree of heterogeneity in terms of variability in effect size estimates between studies [ 41 ]. Pooled estimates are reported as Hedge’s g standardized mean difference (SMD), representing the difference in mean outcomes between groups relative to outcome measure variability [ 42 ]. According to Cohen (as cited in [ 43 ]), SMDs can be grouped into small ≤0.20, medium = 0.50 and large effects ≥0.80. Stata 16 was used for meta-analyses.
2.4. Quality/Risk of Bias Assessment
Two reviewers (J.K.H., E.Q.) independently assessed the quality and risk of bias of the included studies using the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies, which was developed by the National Heart, Lung, and Blood Institute [ 44 ].
3.1. Selection Process
The literature search yielded 4027 unique references. After title/abstract screening, 215 studies were included for full-text screening. Finally, 47 publications were included in the final synthesis. During full-text screening, most studies were excluded because they exclusively analyzed data on a cross-sectional level (56.5%). For further details, see the PRISMA flow chart ( Figure 1 ).
3.2. Overview of Included Studies
Descriptive characteristics and quality/risk of bias assessment of the included studies are provided in Table S1 (Supplementary Material) . In short, sample size ranged from 28 to 43,093. Most studies focused on adults; only four analyzed children/adolescents. Regarding the settings, 17 of the analyzed samples were exclusively recruited in a health care setting, 12 of the studies analyzed general population samples, 14 recruited in another or in several settings, and all studies on children/adolescents recruited in schools ( n = 4). Twenty studies (42.6%) applied data from the same seven underlying datasets. Most studies reported on depression ( n = 36), less reported on anxiety ( n = 20) and some reported on the comorbidity between depression and anxiety ( n = 7). To assess mental disorders, half (48.9%) used structured interviews. Regarding QoL, most studies applied variations of the Short Form Health Survey (SF, n = 27) or the WHOQOL ( n = 12). A total of 38.3% of the studies were rated as “good”, 55.3% as “fair” and 6.4% as “poor” in the quality assessment.
3.3. Overview of Studies on the Association between Anxiety/Depression as Independent Variables and QoL Outcomes
Detailed results on all studies investigating the association between anxiety/depression as independent variables and QoL outcomes are reported in Table 2 . As described in the methods section, the following paragraphs give an overview of those studies focusing on disorder trajectories/changes in symptoms over time and changes in QoL outcomes over time, because they allow for more differentiated interpretations.
Studies on depression/anxiety as independent variables and QoL outcomes.
Abbreviations: QoL = quality of life; MD = major depression; FU = follow-up; DSM = Diagnostic and Statistical Manual of Mental Disorders; HDRS = Hamilton Depression Rating Scale; PCS = Physical Component Score; MDS = Mental Component Score; MDD = major depressive disorder; ANOVA = analysis of variance; BL = baseline; MDE = major depressive episode; CIDI = Composite International Diagnostic Interview; SF-36 = Short Form 36; AUDADIS = Alcohol Use Disorders and Associated Disabilities Interview Schedule; SF-12 = Short Form 12; PHQ = Patient Health Questionnaire; SF-12v2: Short Form 12, Version 2; HRSD = Hamilton Rating Scale for Depression; HADS = Hospital Anxiety and Depression Scale; QLDS = Quality of Life in Depression Scale; EQ-VAS = EQ Visual Analogue Scale; DIS = Diagnostic Interview Schedule; BDI = Beck Depression Inventory; SCID = Short Children’s Depression Inventory; MINI = Mini-International Neuropsychiatric Interview; PTSD = post-traumatic stress disorder; hrqol = health-related quality of life, IES-15 = Impact of Event Scale 15; Q-DIS = Quick Version of the Mental Health’s Diagnostic Interview Schedule; MADRS = Montgomery–Åsberg Depression Rating Scale; FDD-DSM-IV = Fragebogen zur Depressionsdiagnostik nach Diagnostic and Statistical Manual of Mental Disorders IV; SCAN = Schedule for Clinical Assessment in Neuropsychiatry; DASS = Depression Anxiety Stress Scales; MOS SF = Medical Outcomes Study Short Form; CES-D = Center for Epidemiological Studies Depression Scale; WHOQOL-Bref-TW = WHOQOL-Bref Taiwan Version; MHI-5 = Mental Health Inventory 5; OCD = obsessive compulsive disorder; Y-BOCS = Yale–Brown Obsessive Compulsive Scale; BAI = Beck Angst Inventar; DD = depressive disorder; PD = psychiatric disorder; SAD = social anxiety disorder; Q-LES-Q = Quality of Life Enjoyment and Satisfaction Questionnaire; GHQ-28 = General Health Questionnaire 28; PCL-S = Post-traumatic Stress Disorder Checklist Scale; VETR-PTSD = Vietnam Era Twin Registry Posttraumatic Stress Disorder; DRPST = Disaster-Related Psychological Screening Test; SCL-90 = Symptomcheckliste bei psychischen Störungen 90; SASC = SpLD Assessment Standards Committee; QOLS = Quality of Life Scale; CDI = Children’s Depression Inventory.
Depression as independent variable and QoL as outcome. One study investigated QoL at several time points during the entire course of an episode of MD .
Buist-Bouwman, Ormel, de Graaf and Vollebergh [ 46 ] analyzed an MD group from a general population setting (NEMESIS) with data on SF-36 domains in the onset, acute and recovery phase of the depressive episode. The onset of MD was associated with a significant drop in several QoL domains and recovery with a significant increase. Pre- and post-morbid QoL levels were not significantly different for most domains, and post-morbid QoL was even higher for the psychological role functioning and psychological health domains. In comparison to a group without MD, pre- and post-morbid QoL levels in the MD group were significantly lower, except for the psychological role functioning domain, where no significant differences were found. Additionally, it should be noted that 40% of the sample had lower post-morbid QoL compared to pre-morbid levels.
Two studies investigated changes in QoL for people experiencing an onset of depression relative to different comparison groups over two points in time.
One study investigated incident MD in a general population sample (NESARC; Rubio, Olfson, Perez-Fuentes, Garcia-Toro, Wang and Blanco [ 14 ]). Here, incident MD (compared to those without a history of MD as well as to a group without any mental disorder) was associated with a significant drop in QoL (SF-12 MCS). Additionally, analyzing two waves, Pyne, Patterson, Kaplan, Ho, Gillin, Golshan and Grant [ 67 ] compared the QoL (Quality of Well-Being scale) between MD patients and community controls. The patient group was further divided into those continuously not receiving an MD diagnosis, those who continuously received the diagnosis and those who only received the diagnosis at FU (onset). The authors found that changes in QoL did not differ between the groups. At both points in time, QoL scores differed significantly between the groups, except for the incident and the continuous depression group [ 67 ].
Six studies investigated different courses of depression over time in people with depression at BL with or without a healthy comparison group as reference.
Two primary care studies analyzed groups with clinical depression at BL with different FU depression statuses (remission, no remission). One study [ 51 ] analyzed changes in generic QoL measures (SF-12, WHOQOL-Bref) and the disease-specific Quality of Life in Depression Scale. In this study, remission was associated with an improvement in all QoL domains, whereas QoL did not change significantly over time for the non-remitted group. Another study [ 60 ] investigated SF-12 MCS and PCS scores and reported a significant increase in MCS over time in the remitting group. MCS scores in the continuously depressed group and PCS scores in both groups improved, albeit not significantly.
Another study [ 47 ] investigated whether chronic MD in a general population sample (NESARC) was associated with domain-specific reduced QoL (SF-12). They found that chronic MD was a significant risk factor for persistently reduced QoL in all domains and for the onset of reduced QoL at FU in all domains except for physical role.
Two population-based studies further differentiated between the depressive disorders. Analyzing MCS scores (NESARC), Rubio, Olfson, Villegas, Perez-Fuentes, Wang and Blanco [ 15 ] reported a significant increase in QoL for those who remitted from MD and from dysthymia relative to those who had a persistent disorder. Rhebergen, Beekman, de Graaf, Nolen, Spijker, Hoogendijk and Penninx [ 69 ] differentiated between people with MD, double depression or dysthymia at BL who remitted until FU relative to a group without a mental health diagnosis (NEMESIS). Physical health (SF-36) was lowest at BL for double depression, dysthymia and then the MD group. Over time, the MD and double depression groups improved significantly in their physical health, while the dysthymia group did not improve significantly. QoL was significantly lower relative to healthy comparisons for all depression groups at all waves. There were no significant differences regarding physical health trajectories over time among the depressive disorder groups.
Stegenga, Kamphuis, King, Nazareth and Geerlings [ 75 ] investigated more than two MD course groups over time (remitted, intermittent and chronic MD) in association with SF-12 MCS and PCS over time in a primary care-recruited sample with BL MD (Predict study). MCS increased over time in all groups, while changes in PCS were small. Compared to those who remitted, MCS at BL was significantly lower for the chronic course group. While the intermittent group also displayed a lower mean MCS at BL, the coefficient was not significant.
Three studies investigated changes in depressive symptom levels as the independent variable and changes in QoL as outcomes in adults.
One study found no significant association between an initial change in depressive symptoms and subsequent change in QoL (EQ-VAS) in older adults recruited in primary care [ 21 ]. The two other studies analyzed changes in depressive symptoms in samples with MD at BL [ 50 , 51 ]. Chung, Tso, Yeung and Li [ 50 ] found that changes in depressive symptom levels was associated with changes in several QoL domains (SF-36: general health, vitality, social functioning, mental health and MCS). Diehr, Derleth, McKenna, Martin, Bushnell, Simon and Patrick [ 51 ] investigated whether quartiles of change in depressive symptoms were associated with changes in QoL (SF-12, QLDS and WHOQOL-Bref). Those without any change in depressive symptoms generally showed no change in QoL. For all QoL domains and scores except for SF-12 PCS, improvement in depressive symptoms over time was associated with a significant increase in QoL, while a reduction in depressive symptoms was associated with a significant reduction in QoL. Those who had the largest reduction in depressive symptoms also had the largest improvement in QoL measures.
Anxiety as an independent variable and QoL as an outcome. Two publications used a general population sample (NESARC) to investigate incident anxiety disorders [ 14 ] and the remission of anxiety disorders [ 15 ] in association with SF-12 MCS. Both studies separated generalized anxiety disorder (GAD), social anxiety disorder (SAD), panic disorder (PD) and social phobia (SP). All incident disorders were associated with a significant reduction in QoL compared to people without a history of the specific disorders. When the analysis was restricted to incident cases without comorbidities, QoL levels were not significantly different compared to people without a history of any psychiatric disorder [ 14 ]. Those who remitted from SAD showed a significant increase in QoL compared to persistent cases. While QoL improved for all remitting anxiety disorders, change scores for PD and SP were not significant [ 15 ].
Another study investigated different courses (intermittent, chronic or remitting) of obsessive compulsive disorder (OCD) and course in QoL (EQ-5D) as well as a comparison group from the general population [ 68 ]. They found that the OCD groups mostly reported a lower QoL compared to the general population. Moreover, the course groups differed regarding their QoL over time, with remitters reporting small to moderate improvements compared to the chronic group.
One study investigated changes in anxiety symptoms in association with changes in all SF-36 domains and both summary scores over time in a sample with MD at BL [ 50 ]. Changes in anxiety symptoms were significantly associated with changes in bodily pain, general health and the mental health domain.
3.4. Overview of Studies on the Association between QoL as Independent Variable and Anxiety/Depression as Outcomes
Additionally, we identified publications operationalizing QoL as the independent variable and anxiety/depression as outcomes with details on all studies reported in Table 3 . Only one study reported on change in QoL over time and change/trajectories in mental health outcomes over time. This study operationalized change in QoL as a predictor of future change in depressive symptoms over time and reported that an initial improvement in EQ-VAS was associated with a future reduction in depressive symptoms in older adults [ 21 ].
Studies on QoL as the independent variable and depression/anxiety as outcome.
Abbreviations: CES-D-20 = Center for Epidemiological Studies Depression Scale 20; BL = baseline; FU = follow-up; QoL = quality of life; CIDI = Composite International Diagnostic Interview; QLDS = Quality of Life in Depression Scale; SF-12 = Short Form 12; PCS = Physical Component Score; MCS = Mental Component Score; GDS = Geriatric Depression Scale; EQ-VAS = EQ Visual Analogue Scale; MD = mental disorder; AUDADIS-IV = Alcohol Use Disorders and Associated Disabilities Interview Schedule; SF-12v2 = Short Form 12 Version 2; PTSD = post-traumatic stress disorder; IES-15 = Impact of Event Scale 15; MADRS = Montgomery–Åsberg Depression Rating Scale; MDD = major depressive disorder; PHQ = Patient Health Questionnaire; SASC = SpLD Assessment Standards Committee; QOLS = Quality of Life Scale; CDI = Children’s Depression Inventory.
3.5. Meta-Analyses on Anxiety, Depression and SF Summary Scores
In total, eight studies on adults were included in a supplementary meta-analyses of several research questions on SF PCS and MCS in association with anxiety and depressive disorders. Forest plots for the analyses are provided in the supplementary materials (Figures S1–S10) .
Differences in SF summary scores at FU among adults with and without depressive disorders at BL. Based on a pooling of four studies [ 45 , 49 , 52 , 54 ], those with depression at BL showed lower MCS scores at FU compared to a group without depression at BL with a large effect size (SMD = −0.96, 95% CI: −1.04 to −0.88, p < 0.001, I 2 = 0.0%). PCS scores at FU were lower for the depression group compared to the non-depression group with a medium effect size (SMD = −0.68, 95% CI: −1.06 to −0.30, p < 0.001, I 2 = 94.6%). Excluding the study rated “poor” in the quality/risk of bias assessment from the pooling did not substantially affect the results (MCS: SMD = −0.96, 95% CI: −1.03 to −0.88, p < 0.001, I 2 = 0.01%; PCS: SMD = −0.63, 95% CI: −1.08 to −0.19, p < 0.01, I 2 = 96.8%).
BL differences in SF summary scores among adults with MD at BL with and without remitting courses over time. Based on a pooling of two studies [ 19 , 84 ] of samples with MD at BL, those with persistent MD at FU had significantly lower MCS at BL (SMD = −0.25, 95% CI: −0.41 to −0.10, p = 0.001, I 2 = 74.95) and PCS scores at BL (SMD = −0.24, 95% CI: −0.39 to −0.09, p = 0.002, I 2 = 73.14) compared to those who achieved remission until FU. Effect sizes were small for both summary scores.
FU differences in SF summary scores among adults with depressive and anxiety disorders at BL with and without remitting courses . Based on the pooling of two studies [ 71 , 81 ] of samples with MD and/or dysthymia, the group where the disorder had persisted/a co-morbid condition was present/had a suicide attempt until FU had significantly lower MCS scores at FU compared to the group where the disorder had remitted without treatment until FU, with a medium effect size for depressive disorders (SMD = −0.59, 95% CI: −0.75 to −0.42, p < 0.001, I 2 = 37.72) and a small effect size for anxiety disorders (SMD = −0.44, 95% CI: −0.58 to −0.30, p < 0.001, I 2 = 58.87). The SMD for PCS scores at FU was negligible in terms of effect size for both disorder groups (depressive disorders: SMD = 0.02, 95% CI: −0.24 to 0.27, p = 0.90, I 2 = 73.65; anxiety disorders: SMD = −0.09, 95% CI: −0.17 to −0.01, p = 0.03, I 2 = 0.01).
4. Discussion
4.1. main results.
This review adds to the present literature by providing an overview of longitudinal observational studies investigating the association between depression, anxiety and QoL in samples without other specific illnesses or specific treatments. Additional meta-analyses investigated group differences according to SF MCS and PCS.
While a concise synthesis of all the identified studies is challenging due to heterogeneity, the following picture emerges from studies investigating change–change associations: before the onset of disorders, QoL is already lower in disorder groups in comparison to healthy comparisons. The onset of the disorders further reduces the QoL. Remission is associated with an increase in QoL, mostly to pre-morbid levels. Additionally, some studies show that remission patterns are relevant for QoL outcomes as well. Moreover, a bi-directional effect was reported, whereby QoL is also predictive of mental health outcomes.
Evidence for a bi-directional association as well as studies showing lower QoL across the entire course of the disorders (before onset, during disorder, after disorder) relative to a healthy comparison group seem to suggest that impairments in QoL may result from a certain pre-disorder vulnerability in these groups. Longitudinal studies using general population data have investigated different hypotheses on (QoL) impairments after remission of anxiety disorders and MD [ 87 , 88 ]. One hypothesis suggests that impairments after the illness episode reflect a pre-disorder vulnerability (vulnerability or trait hypothesis), while the another states that impairments develop during the mental health episode and remain as a residual after recovery (scar hypothesis). Generally, both studies favored the vulnerability hypothesis [ 87 , 88 ]. For subgroups with recurrent anxiety disorders, scarring effects were also found for mental functioning [ 88 ]. Yet, it has to be noted that it was not the aim of our review to gather evidence for these hypotheses using QoL as an indicator, which represents an opportunity for future research.
To be able to investigate possible domain-specific differences across studies, we aimed to conduct a meta-analysis on all studies on the same research question which reported on QoL subdomains (e.g., using WHOQOL and SF). However, as described in the Methods section above, only eight studies reported comparable information on different research questions and could be included in meta-analyses. Due to the limited number of studies included in each meta-analysis, the focus on SF MCS and PCS scores, and most studies reporting on depression, the results of the meta-analyses should be viewed with caution. Keeping this in mind, our results indicate that both mental and physical QoL are significantly impacted by anxiety and depressive disorders and that the course of the disorder is also relevant for QoL outcomes. Not surprisingly, effect sizes for MCS were larger compared to PCS for most research questions. A pooling of two studies on different courses of anxiety and depressive disorders found that effect sizes for MCS at FU were of moderate size for depressive (SMD = −0.59) and of small size for anxiety disorders (SMD = −0.44), while SMDs for PCS at FU were negligible in size.
Overall, effect sizes from meta-analyses ranged from negligible to large, and heterogeneity varied considerably (I 2 between 0% and 95%). Because of the small number of studies, possible influential study-level factors (e.g., setting, operationalization of the variables, length of FU) could not be investigated in further detail by means of a meta-regression, which remains a question for future research.
4.2. Implications for Future Research
Based on the results described and study heterogeneity discussed above, we provide recommendations for future research.
First recommendation: future research should differentiate between individual disorders and focus on anxiety disorders. The majority of the studies investigated depressive disorders or symptoms. On the level of individual disorders, most focused on MD, while two studies additionally reported on dysthymia [ 15 , 69 ]. One of these investigated double depression [ 69 ]. On the level of anxiety disorders, three publications differentiated between individual anxiety disorders within the same study [ 14 , 15 , 63 ]. While it was not possible to conduct a meta-analysis comparing different anxiety disorders in our case, individual studies suggest possible disorder-specific differences when analyzing changes in QoL over time: Rubio, Olfson, Villegas, Perez-Fuentes, Wang and Blanco [ 15 ] suggest that QoL significantly improved for those remitting from GAD and SAD (compared to non-remission). QoL improved for PD and SP as well, but differences in change scores were smaller and did not reach statistical significance. The incidences of all of these disorders were associated with a significant drop in QoL [ 14 ]. In summary, future longitudinal studies should focus on anxiety disorders and generally differentiate between individual disorders to investigate possible disorder-specific differences.
Second recommendation: future research should consider trajectories of disorders/change in symptoms and changes in QoL over time. We would have liked to include a meta-analysis of disorder trajectories and change scores in QoL over time. Because of the small, diverse number of studies on this association in general and the number of assumptions that would have had to have been made for a meta-analysis, we refrained from pooling effects for this research question. In total, 17 studies investigated changes in independent variables associated with changes in outcomes. This approach has several advantages. On the one hand, different disorder or symptom trajectories can be identified. Several studies reported that QoL outcomes differ according to disorder course and the degree of change in symptoms. The focus on the change in characteristics over time in future research could additionally reduce the problem of unobserved time-constant heterogeneity in observational studies when appropriate methods are applied [ 26 ].
Third recommendation: future research should investigate individual QoL domains. Several systematic reviews on cross-sectional studies found that effect sizes differed by QoL domains [ 32 , 89 ]. For example, Olatunji, Cisler and Tolin [ 89 ] reported that health and social functioning were most impaired for anxiety disorders (compared to non-clinical controls). Comparing individuals with diabetes and depressive symptoms to those with diabetes only, Schram, Baan and Pouwer [ 32 ] reported that while SF pain scores were mild to moderately impaired, role and social functioning displayed moderate to severe impairments in those with comorbid depressive symptoms. The other scores were moderately impaired. As described above in detail, a meta-analysis using all subdomains was not feasible in this review. Further research differentiating between QoL domains would thus allow future meta-analyses to investigate whether the observed domain-specific differences reported in previous reviews of cross-sectional data can be observed in longitudinal studies as well.
Fourth recommendation: future research should consider bi-directional effects. While investigating QoL as the outcome measure and anxiety/depression as independent variables seems relatively straightforward, ten studies investigated QoL as the independent variable and anxiety/depression as outcomes. In light of possible bi-directional effects and pre-existing vulnerability suggested by individual studies, future research considering QoL as an independent variable could inform a deeper understanding of this complex association.
4.3. Strengths and Limitations
A strength of this work is the transparent methodological process: the review was prospectively registered with PROSPERO and a study protocol was published [ 34 ]. Two reviewers were included in screening, data extraction and quality assessment processes. There were no limitations regarding the time or location of the publications. Moreover, all versions of the ICD/DSM and validated questionnaires were considered eligible to identify anxiety or depression. Another strength is the thorough literature search that enabled us to identify all relevant studies. Additionally, we did not limit the age range and were therefore able to shed light on studies investigating children/adolescents. Moreover, some studies could be pooled using random-effects meta-analyses, which allows for stronger conclusions regarding effect sizes compared to individual studies. Besides the content analysis, this review emphasizes difficulties in meta-analysis from observational, longitudinal studies. We hope that our work can facilitate discussion on this topic.
The study has some limitations. We did not limit our search to specific research questions, which led to the inclusion of heterogeneous studies. Heterogeneity particularly stemmed from the operationalization of the variables of interest. Due to this, a concise narrative synthesis of all results was not feasible. The positive aspect of this broad focus is that it allowed us to provide an overview of studies and research questions analyzed and to formulate more nuanced recommendations for future research. We have to acknowledge that there is an abundance of QoL assessments used in medicine and health sciences [ 37 ]. The list applied in this work was derived with respect to previous relevant reviews on QoL research. It was not designed to be fully comprehensive or exhaustive. Rather, it provided us with a working definition for this review and helped to enhance the transparency of our selection processes. Additionally, because we included validated QoL measures frequently used in research, we assume that exclusion would particularly have been the case for novel or study-specific measures. Finally, the focus on peer-reviewed literature means that studies in other languages and gray literature were not considered. Nonetheless, this focus on literature published in peer-reviewed journals should ensure a certain scientific quality.
5. Conclusions and Relevance for Clinical Practice
Overall, the results indicate that QoL is lower before the onset of anxiety and depressive disorders, further reduces upon onset of the disorders and generally improves with remission to pre-morbid levels. Moreover, disorder course (e.g., remitted, intermittent, chronic) seems to play an important role; however, only a few studies analyzed this. Changes in anxiety and depressive symptoms were also associated with changes in QoL over time. Meta-analyses found that effect sizes were larger for MCS relative to PCS, highlighting the relevance of differentiation between QoL domains. While our review identified some gaps in the current literature and made recommendations for future research, the following should be noted for clinical practice. On the one hand, an improvement in mental health is associated with better QoL, which emphasizes the relevance of support during the disorders. This is also shown by meta-analyses, which show that cognitive behavioral therapy additionally improves QoL [ 90 , 91 ]. Moreover, the results indicate reduced QoL even before disorder onset, highlighting the relevance of early preventive measures in vulnerable groups. In line with this, studies on school-based prevention programs show a significant reduction in anxiety and depressive symptoms [ 92 , 93 ], and psychosocial prevention programs may additionally improve QoL [ 94 ].
During the COVID-19 pandemic, it is of high relevance to tackle the arising challenges associated with this pandemic. For example, it is important to face the high prevalence rates of both depression and anxiety with appropriate measures.
Acknowledgments
The authors would like to thank Elzbieta Kuzma for her consultation (Albertinen-Haus Centre for Geriatrics and Gerontology, University of Hamburg, Hamburg, Germany; University of Exeter Medical School, Exeter, UK).
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph182212022/s1 , Table S1: detailed descriptive information for included studies ( n = 47); Figure S1: forest plot for differences in SF MCS at FU among adults with and without depressive disorders at BL; Figure S2: forest plot for differences in SF PCS at FU among adults with and without depressive disorders at BL; Figure S3: forest plot for differences in SF MCS at FU among adults with and without depressive disorders at BL (sensitivity analysis); Figure S4: forest plot for differences in SF PCS at FU among adults with and without depressive disorders at BL (sensitivity analysis); Figure S5: forest plot for BL differences in SF MCS among adults with MD at BL with and without remitting courses over time; Figure S6: forest plot for BL differences in SF PCS among adults with MD at BL with and without remitting courses over time; Figure S7: forest plot for FU differences in SF MCS among adults with depressive disorders at BL with and without remitting courses; Figure S8: forest plot for FU differences in SF PCS among adults with depressive disorders at BL with and without remitting courses; Figure S9: forest plot for FU differences in SF MCS among adults with anxiety disorders at BL with and without remitting courses; Figure S10: forest plot for FU differences in SF PCS among adults with anxiety disorders at BL with and without remitting courses.
Author Contributions
J.K.H.: conceptualization of research question; development of search strategy; study screening and selection; risk of bias/quality assessment; study synthesis; writing—original draft, review and editing; H.-H.K.: conceptualization of research question; writing—review and editing; E.Q.: study screening and selection; risk of bias/quality assessment; writing—review and editing; A.H.: conceptualization of research question; development of search strategy; study screening and selection (third party); study synthesis; writing—review and editing. All authors have read and agreed to the published version of the manuscript.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
Data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Home — Essay Samples — Nursing & Health — Psychiatry & Mental Health — Depression
Essays About Depression
Depression essay topic examples.
Explore topics like the impact of stigma on depression, compare it across age groups or in literature and media, describe the emotional journey of depression, discuss how education can help, and share personal stories related to it. These essay ideas offer a broad perspective on depression, making it easier to understand and engage with this important subject.
Argumentative Essays
Argumentative essays require you to analyze and present arguments related to depression. Here are some topic examples:
- 1. Argue whether mental health stigma contributes to the prevalence of depression in society.
- 2. Analyze the effectiveness of different treatment approaches for depression, such as therapy versus medication.
Example Introduction Paragraph for an Argumentative Essay: Depression is a pervasive mental health issue that affects millions of individuals worldwide. This essay delves into the complex relationship between mental health stigma and the prevalence of depression in society, examining the barriers to seeking help and the consequences of this stigma.
Example Conclusion Paragraph for an Argumentative Essay: In conclusion, the analysis of mental health stigma's impact on depression underscores the urgent need to challenge and dismantle the stereotypes surrounding mental health. As we reflect on the far-reaching consequences of stigma, we are called to create a society that fosters empathy, understanding, and open dialogue about mental health.
Compare and Contrast Essays
Compare and contrast essays enable you to examine similarities and differences within the context of depression. Consider these topics:
- 1. Compare and contrast the symptoms and risk factors of depression in adolescents and adults.
- 2. Analyze the similarities and differences between the portrayal of depression in literature and its depiction in modern media.
Example Introduction Paragraph for a Compare and Contrast Essay: Depression manifests differently in various age groups and mediums of expression. This essay embarks on a journey to compare and contrast the symptoms and risk factors of depression in adolescents and adults, shedding light on the unique challenges faced by each demographic.
Example Conclusion Paragraph for a Compare and Contrast Essay: In conclusion, the comparison and contrast of depression in adolescents and adults highlight the importance of tailored interventions and support systems. As we contemplate the distinct challenges faced by these age groups, we are reminded of the need for age-appropriate mental health resources and strategies.
Descriptive Essays
Descriptive essays allow you to vividly depict aspects of depression, whether it's the experience of the individual or the societal impact. Here are some topic ideas:
- 1. Describe the emotional rollercoaster of living with depression, highlighting the highs and lows of the experience.
- 2. Paint a detailed portrait of the consequences of untreated depression on an individual's personal and professional life.
Example Introduction Paragraph for a Descriptive Essay: Depression is a complex emotional journey that defies easy characterization. This essay embarks on a descriptive exploration of the emotional rollercoaster that individuals with depression experience, delving into the profound impact it has on their daily lives.
Example Conclusion Paragraph for a Descriptive Essay: In conclusion, the descriptive portrayal of the emotional rollercoaster of depression underscores the need for empathy and support for those grappling with this condition. Through this exploration, we are reminded of the resilience of the human spirit and the importance of compassionate understanding.
Persuasive Essays
Persuasive essays involve arguing a point of view related to depression. Consider these persuasive topics:
- 1. Persuade your readers that incorporating mental health education into the school curriculum can reduce the prevalence of depression among students.
- 2. Argue for or against the idea that employers should prioritize the mental well-being of their employees to combat workplace depression.
Example Introduction Paragraph for a Persuasive Essay: The prevalence of depression underscores the urgent need for proactive measures to address mental health. This persuasive essay asserts that integrating mental health education into the school curriculum can significantly reduce the prevalence of depression among students, offering them the tools to navigate emotional challenges.
Example Conclusion Paragraph for a Persuasive Essay: In conclusion, the persuasive argument for mental health education in schools highlights the potential for early intervention and prevention. As we consider the well-being of future generations, we are called to prioritize mental health education as an essential component of a holistic education system.
Narrative Essays
Narrative essays offer you the opportunity to tell a story or share personal experiences related to depression. Explore these narrative essay topics:
- 1. Narrate a personal experience of overcoming depression or supporting a loved one through their journey.
- 2. Imagine yourself in a fictional scenario where you advocate for mental health awareness and destigmatization on a global scale.
Example Introduction Paragraph for a Narrative Essay: Personal experiences with depression can be transformative and enlightening. This narrative essay delves into a personal journey of overcoming depression, highlighting the challenges faced, the support received, and the lessons learned along the way.
Example Conclusion Paragraph for a Narrative Essay: In conclusion, the narrative of my personal journey through depression reminds us of the resilience of the human spirit and the power of compassion and understanding. As we reflect on our own experiences, we are encouraged to share our stories and contribute to the ongoing conversation about mental health.
Critical Appraisal of Cognitive Behavioral Therapy in Treating Depression
Depression is depression an actual illness, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Holden Caulfield Symptoms
The epidemic of depression among students and teenagers, the effects of depression in your body and its treatment, the issue of depression and its reality nowadays, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Overview of Biological Predispositions and Risk Factors Associated with Depression
How to overcome depression and anxiety, depression: definition, risks, symptoms and treatment, the best way to help someone who is depressed, get a personalized essay in under 3 hours.
Expert-written essays crafted with your exact needs in mind
The Issue of Depression: Mental Battle
What is a depression, living in depression: a firsthand account, teen depression - symptoms and causes, adolescent depression and its contribution to teenage suicides, the issue of depression and its affect in an emerging adulthood, depression: definition and ways of resolving caused problems, depression in teenagers: causes and ways to overcome, depression and its main causes, genetic disorder report: clinical depression, the way teachers can help their students to overcome anxiety and depression, depression and its effects of mind and body, the effectiveness of cognitive behavioural therapy (cbt) for treating individuals with depression and anxiety, how to overcome teenage depression, depression as the reason of serious health problems and suicide, a depressing world with different obstacles, the link between self-esteem and adolescent depression, darwinian psychology and depression: the gender differential hypothesis, prevention of depression, anxiety and burnout in resident doctors – a systematic review, dysregulated processing of negative and positive responses in depression.
Depression, known as major depressive disorder or clinical depression, is a psychological condition characterized by enduring feelings of sadness and a significant loss of interest in activities. It is a mood disorder that affects a person's emotional state, thoughts, behaviors, and overall well-being.
Its origin can be traced back to ancient civilizations, where melancholia was described as a state of sadness and melancholy. In the 19th century, depression began to be studied more systematically, and terms such as "melancholic depression" and "nervous breakdown" emerged. The understanding and classification of depression have evolved over time. In the early 20th century, Sigmund Freud and other psychoanalysts explored the role of unconscious conflicts in the development of depression. In the mid-20th century, the Diagnostic and Statistical Manual of Mental Disorders (DSM) was established, providing a standardized criteria for diagnosing depressive disorders.
Biological Factors: Genetic predisposition plays a role in depression, as individuals with a family history of the disorder are at a higher risk. Psychological Factors: These may include a history of trauma or abuse, low self-esteem, pessimistic thinking patterns, and a tendency to ruminate on negative thoughts. Environmental Factors: Adverse life events, such as the loss of a loved one, financial difficulties, relationship problems, or chronic stress, can increase the risk of depression. Additionally, living in a socioeconomically disadvantaged area or lacking access to social support can be contributing factors. Health-related Factors: Chronic illnesses, such as cardiovascular disease, diabetes, and chronic pain, are associated with a higher risk of depression. Substance abuse and certain medications can also increase vulnerability to depression. Developmental Factors: Certain life stages, including adolescence and the postpartum period, bring about unique challenges and changes that can contribute to the development of depression.
Depression is characterized by a range of symptoms that affect an individual's emotional, cognitive, and physical well-being. These characteristics can vary in intensity and duration but generally include persistent feelings of sadness, hopelessness, and a loss of interest or pleasure in activities once enjoyed. One prominent characteristic of depression is a noticeable change in mood, which can manifest as a constant feeling of sadness or emptiness. Individuals may also experience a significant decrease or increase in appetite, leading to weight loss or gain. Sleep disturbances, such as insomnia or excessive sleepiness, are common as well. Depression can impact cognitive functioning, causing difficulties in concentration, decision-making, and memory recall. Negative thoughts, self-criticism, and feelings of guilt or worthlessness are also common cognitive symptoms. Furthermore, physical symptoms may arise, including fatigue, low energy levels, and a general lack of motivation. Physical aches and pains, without an apparent medical cause, may also be present.
The treatment of depression typically involves a comprehensive approach that addresses both the physical and psychological aspects of the condition. It is important to note that the most effective treatment may vary for each individual, and a personalized approach is often necessary. One common form of treatment is psychotherapy, which involves talking to a mental health professional to explore and address the underlying causes and triggers of depression. Cognitive-behavioral therapy (CBT) is a widely used approach that helps individuals identify and change negative thought patterns and behaviors associated with depression. In some cases, medication may be prescribed to help manage depressive symptoms. Antidepressant medications work by balancing neurotransmitters in the brain that are associated with mood regulation. It is crucial to work closely with a healthcare provider to find the right medication and dosage that suits an individual's needs. Additionally, lifestyle changes can play a significant role in managing depression. Regular exercise, a balanced diet, sufficient sleep, and stress reduction techniques can all contribute to improving mood and overall well-being. In severe cases of depression, when other treatments have not been effective, electroconvulsive therapy (ECT) may be considered. ECT involves administering controlled electric currents to the brain to induce a brief seizure, which can have a positive impact on depressive symptoms.
1. According to the World Health Organization (WHO), over 264 million people worldwide suffer from depression, making it one of the leading causes of disability globally. 2. Depression can affect people of all ages, including children and adolescents. In fact, the prevalence of depression in young people is increasing, with an estimated 3.3 million adolescents in the United States experiencing at least one major depressive episode in a year. 3. Research has shown that there is a strong link between depression and other physical health conditions. People with depression are more likely to experience chronic pain, cardiovascular diseases, and autoimmune disorders, among other medical conditions.
The topic of depression holds immense significance and should be explored through essays due to its widespread impact on individuals and society as a whole. Understanding and raising awareness about depression is crucial for several reasons. Firstly, depression affects a significant portion of the global population, making it a pressing public health issue. Exploring its causes, symptoms, and treatment options can contribute to better mental health outcomes and improved quality of life for individuals affected by this condition. Additionally, writing an essay about depression can help combat the stigma surrounding mental health. By promoting open discussions and providing accurate information, essays can challenge misconceptions and foster empathy and support for those experiencing depression. Furthermore, studying depression allows for a deeper examination of its complex nature, including its psychological, biological, and sociocultural factors. Lastly, essays on depression can highlight the importance of early detection and intervention, promoting timely help-seeking behaviors and reducing the burden of the condition on individuals and healthcare systems. By shedding light on this critical topic, essays have the potential to educate, inspire action, and contribute to the overall well-being of individuals and society.
1. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. 2. World Health Organization. (2017). Depression and other common mental disorders: Global health estimates. World Health Organization. 3. Kessler, R. C., Bromet, E. J., & Quinlan, J. (2013). The burden of mental disorders: Global perspectives from the WHO World Mental Health Surveys. Cambridge University Press. 4. Beck, A. T., Rush, A. J., Shaw, B. F., & Emery, G. (1979). Cognitive therapy of depression. Guilford Press. 5. Nierenberg, A. A., & DeCecco, L. M. (2001). Definitions and diagnosis of depression. The Journal of Clinical Psychiatry, 62(Suppl 22), 5-9. 6. Greenberg, P. E., Fournier, A. A., Sisitsky, T., Pike, C. T., & Kessler, R. C. (2015). The economic burden of adults with major depressive disorder in the United States (2005 and 2010). Journal of Clinical Psychiatry, 76(2), 155-162. 7. Cuijpers, P., Berking, M., Andersson, G., Quigley, L., Kleiboer, A., & Dobson, K. S. (2013). A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Canadian Journal of Psychiatry, 58(7), 376-385. 8. Hirschfeld, R. M. A. (2014). The comorbidity of major depression and anxiety disorders: Recognition and management in primary care. Primary Care Companion for CNS Disorders, 16(2), PCC.13r01611. 9. Rush, A. J., Trivedi, M. H., Wisniewski, S. R., Nierenberg, A. A., Stewart, J. W., Warden, D., ... & Fava, M. (2006). Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR*D report. American Journal of Psychiatry, 163(11), 1905-1917. 10. Kendler, K. S., Kessler, R. C., Walters, E. E., MacLean, C., Neale, M. C., Heath, A. C., & Eaves, L. J. (1995). Stressful life events, genetic liability, and onset of an episode of major depression in women. American Journal of Psychiatry, 152(6), 833-842.
Relevant topics
- Mental Health
- Eating Disorders
- Drug Addiction
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- The Open University
- Guest user / Sign out
- Study with The Open University
My OpenLearn Profile
Personalise your OpenLearn profile, save your favourite content and get recognition for your learning
About this free course
Become an ou student, download this course, share this free course.

Start this free course now. Just create an account and sign in. Enrol and complete the course for a free statement of participation or digital badge if available.
A major aim of this course was to shed some light on the aetiology of depression and anxiety. At the end of it you should have some idea of the complexity of this enterprise. We have focused on one of the best-studied and hence best-understood contributors to psychopathology – stress. This has biological, social and psychological significance, and its operation can be studied and understood at all these levels.
The clear message you should take away is that interaction between these levels is enormously important in aetiology. Biological factors, such as dysregulation of the HPA axis and its consequences, possible abnormalities in brain neurotransmitter systems, the effects of stress on the developing brain at different ages, and the kinds of genes that an individual carries, appear to play an important part in the development and maintenance of emotional disorders such as depression and anxiety. However, these biological factors cannot be divorced from factors that are thought of as psychosocial, such as abuse in childhood, or stressful events and how we perceive them. This is very evident from the most recent developments in genetics, which show how, via epigenetic processes, experiences are translated into the activity (or expression) of genes, which then modify the workings of the brain in ways that affect mood.
Research into epigenetic influences on mental health and ill-health is burgeoning and is likely to make a very significant contribution to our understanding of aetiology in the years to come. If so, it should also help clarify how existing treatments, both pharmacological and psychotherapeutic, for emotional disorders work, or suggest new approaches that would work more effectively.
The HPA axis is overactive in those with depression and anxiety, suggesting a role for chronic stress. Elevated levels of glucocorticoids such as cortisol and corticosterone, resulting from chronic stress, have toxic effects in some areas of the brain and promote neurogenesis in others.
The monoamine hypothesis of mood disorders has been influential in trying to explain the causes of depression. However the picture is now more complex and the view of a simple chemical imbalance as a cause of depression is outdated.
Hypotheses such as the neurotrophic hypothesis and the network hypothesis have been developed to try to account for the complex effects of antidepressant treatments on the brain.
The life-cycle model of stress links brain development with stress effects over the lifetime.
The cognitive approach concentrates on particular ways of thinking and how these cause and sustain depression.
Genetic and other vulnerabilities (also called predispositions or diatheses) can interact with environmental factors, which include psychosocial stressors such as stressful life events and early life stress (including child abuse) to cause emotional disorders such as depression.
Epigenetic processes add another layer of complexity to the interaction between genes and environment. There is increasingly evidence of the importance of epigenetic processes in the aetiology of mood disorders.

Zooming Out Can Ease Anxiety and Depression
A personal perspective: seeing the big picture reduces my anxiety..
Posted March 31, 2024 | Reviewed by Devon Frye
- What Is Anxiety?
- Find counselling to overcome anxiety

For the past four weeks, I was in a low-grade depression , up until this past Tuesday. I’m out on the other side now. Hallelujah. During that time, I did all the things that normally help shift my mood:
- Seeing friends
- Exercising (even if it’s 15 minutes)
- Eating healthy foods
- Treating myself to unhealthy foods
- Taking my medication
- Watching saccharine cute baby bunny videos
- Using my light box
- Using positive self-talk
- Regulating my sleep
- Listening to music
I even journaled! Which, for the record (the record I don’t have), I rarely do. I’m not a fan. I know others swear by it; I usually just swear.
Yet I still couldn’t shake this awful lethargy, the familiar disinterest in life, this shame and mean-heartedness towards myself. Even a session with my therapist Hard-Ass Andie , though helpful, didn’t budge it all that much. Until I had a second session with her.
As Andie and I talked, I mentioned there were two things that had been weighing a bit on my mind: My career is moving in a very different direction (very enjoyable, but very different), and my wuz-band and I (if you haven’t guessed we’re on good terms) have begun amicable formal divorce proceedings.
Over a FaceTime appointment, Andie said: “You’re in transition in two major areas of your life. That’s a lot.”
Pricks of tears bubbled. “Those are two pretty significant changes, aren’t they?” But before that conversation, I hadn’t given them any thought, because they were, well… just my life. Not sizeable transitions.
“It’s natural to grieve,” Andie said.
I’m grieving? No, it’s not that big a deal, I thought. But of course, it is. Slowly as we talked, under that malaise of depression, I felt sadness, and that sadness opening to relief.
I couldn’t see I was going through transitions. Andie reminded me that sometimes I have a tendency to forget about the big picture. When I’m in a vice grip of depression and anxiety , figuratively and literally, I get tunnel vision. I see only the blades of grass, not the whole yard.
One of the body’s physiological responses to stress can be tunnel vision so we focus solely on things related to our survival such as paths of escape. Our nervous system jumps to our aid to protect us even if we’re actually safe and it’s "only" a perceived threat.
I wasn’t broken or to blame or stupid because I couldn’t see what was going on. I wasn’t in any true danger, but my body didn’t know that. My flight and freeze response was my nervous system’s innate wisdom to keep me from harm.
What’s the Solution?
Zooming out . See the bigger picture to gain perspective. It may sound obvious, but it’s not easy. I now know to check in and take a tally of what’s happening in my life; identify changes and acknowledge their magnitude instead of minimizing them. I can do this alone, but not always.
Sometimes, talking things through is the way I need to zoom out. Chatting with a friend works, as does talking with Andie when I need more.
Andie offers me acknowledgment and validation. She knows me. I trust her. With this connection and trust, it’s safe enough to see the big picture and feel what’s underneath. As a result, I can soften and offer the kindness to myself that she’s offering me.
© Victoria Maxwell

Victoria Maxwell is a playwright, actor, and lecturer on her 'lived' experiences of bipolar disorder, anxiety, psychosis and recovery.
- Find a Therapist
- Find a Treatment Center
- Find a Support Group
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience

22 Subtle Ways Anxiety and Depression Affect Your Daily Life
S ometimes when you live with anxiety and depression, it’s not just one big thing, but the accumulation of “little” things, that can make everyday life challenging. While these things may seem “subtle” to the outside world, they’re often huge for the person dealing with them. Just because others can’t see the effects doesn’t make them any less real.
To find out how these little things add up, we asked people in our mental health community to share how anxiety and depression affect their daily life.
Here’s what they had to say:
1. “My body hurts, and the aches can’t be cured with exercise or a healthy diet. It’s a pain in the soul that affects the body. It’s hard for people to understand if they haven’t felt it themselves.” — Starr P.
2. “Depression makes me want to lay in bed all day, but anxiety makes me think that if I do that, I’ll miss something, something bad will happen or I’ll fall behind in work or class.” — Cailey C.
3. “Absolutely everything I do is a fight. Even the most simple daily tasks. It’s like two opposites fist fighting in my brain. But I’m the one who gets hurt and depression and anxiety keep going strong.” — Merica M.
4 . “Depression makes me want to leave work early. Anxiety tells me if I do I’ll be fired. So I end up spending my days at work being super unproductive. Then depression starts to wonder if getting fired even matters and anxiety is convinced I’ll be fired anyway since I haven’t gotten a lot done.” — Megan R.
5. “Anxiety is the stream of thoughts that can’t stop, even if you tell yourself to calm down. Anxiety is being nervous for something and you have no idea why. Depression, though… depression is the drowning in those streams of thoughts. It’s the darkness that pulls you in and makes you believe you’re nothing. Unworthy. Depression is the monster that wants to win.” — David S.
6. “Depression makes me so tired 24/7, but the anxiety keeps my brain awake which keeps me awake 24/7. I almost never sleep more than two to three hours a night.” — Suewanda B.
7. “Depression makes me have no motivation to do anything. Anxiety convinces me I’m a terrible person for not doing anything and that I have a million things I should be doing instead of laying in bed all day — and the fact I’m not doing them means I’m going to fall behind and fail at life.” — Zoe S.
8. “Instead of looking people in the face I watch the ground because I am afraid they will speak to me if we have eye contact. I am afraid I won’t know what to say back.” — Vicki V.
9. “Anxiety makes me question everything: is my boyfriend going to get sick of me? Am I smart enough for grad school? Am doing enough at work? Am I good enough? The depression makes me feel like all the negative thoughts my anxiety brings up must be true: I’m am a complete failure. I’m stupid, worthless, a burden and deserve the bad things that have happened to me. It makes me feel hopeless.” — Martine E.
10. “Some days I just don’t’ know which way is up. I don’t know where to focus because my depression pulls me one way and my anxiety another.” — Mandy L.
11. “Depression makes me not want to go to school, but my anxiety makes me freak out if I miss school. Anxiety keeps me up at night , but my depression makes me so tired. I am constantly fighting myself. It is completely exhausting.” — Jordan R.
12. “I feel like I have to create a carefully curated version of myself to cover both my anxiety and depression. When they are both in full swing, I can feel the mask slip because I can no longer perfectly portray the happy, centered version of myself people have come to expect. It’s challenging because although people routinely come to me to seek that steady, level-headed person I portray from 8-6 each day, no one sees me, and when they do see the mask slip even a little, they rebuff me. It’s incredibly lonely to feel like I can’t breath, but I have to portray calm assurance to feel like I can barely drag myself through work I typically love and know no one really sees me.” — Charity L.
13. “When my anxiety gets going and my brain jumps into overdrive thinking about the million things that need my attention, that’s when the depression shows up and says, ‘Let’s not do any of that.’” — Julia A.
14. “Often my depression is a symptom of my anxiety. I do things that are fueled by my anxiety and then afterward will beat myself up over my decision and end up in a very low spot for the rest of the day. It’s like I’m either in a state of anxiety or a state of depression. When I’m in both it’s like a hurricane.” — Kira M.
15. “They contradict each other and affect me as a student especially. Sometimes I will have no motivation to do an assignment, but yet it makes me anxious turning it in late or not doing it and receiving a bad grade.” — Joanna M.
16. “Anxiety stops me from having good relationships with people caused by repeating thoughts that they hate me, they’ll leave me, etc. Depression is not caring about anything, and both are hell. I care, but I don’t care at all. This all stops me from moving forward with anything because it feels useless.” — Amber W.
17. “The anxiety makes me worry that the reason a person isn’t replying is because they’re ignoring me on purpose or that they have better things to do. The depression tells me I’m not worth their time, and I should just leave them alone instead of bothering them.” — Randi B.
18. “When the doorbell rings and the tainted mix of anxiety and depression takes you to ‘it’s the police, something dreadful has happened,’ but you can’t bring yourself to stand up and find out.” — Heather B.
19. “I have constant arguments with myself. I know that it is good for me to speak to people and have company, but my depression means I have no motivation to go out, and my anxiety tells me that even if I did speak to anyone, I’d only bore them and keep them from something more enjoyable.: — Jenny B.
20. “Going to grocery store seems like the hardest most terrifying experience. You question your hair, your clothes, your walk, the drive, the walking down the aisles. It’s scarier than climbing Everest. I just resign myself to order in.” — Ana E.
21. “Anxiety means I always have to have an ‘escape route.’ I sit close to the door, or at the end of the row in theaters.” — Gordon M.
22. “It may look subtle to be people on the outside, but on the inside to us these subtle effects can be distressing. Not wanting to get up out of bed, not having the energy to shower, some of us either don’t feel like eating or eating becomes a big comfort. Socializing is a huge effort, it can drain every last bit out of you, and when you finally sit down the thoughts then start. I would not say there is any subtle way to explain it — there’s just silent to those around, and that is the short of it.” — Shona-Lee G.

Read our research on: Gun Policy | International Conflict | Election 2024
Regions & Countries
3. problems students are facing at public k-12 schools.
We asked teachers about how students are doing at their school. Overall, many teachers hold negative views about students’ academic performance and behavior.
- 48% say the academic performance of most students at their school is fair or poor; a third say it’s good and only 17% say it’s excellent or very good.
- 49% say students’ behavior at their school is fair or poor; 35% say it’s good and 13% rate it as excellent or very good.
Teachers in elementary, middle and high schools give similar answers when asked about students’ academic performance. But when it comes to students’ behavior, elementary and middle school teachers are more likely than high school teachers to say it’s fair or poor (51% and 54%, respectively, vs. 43%).
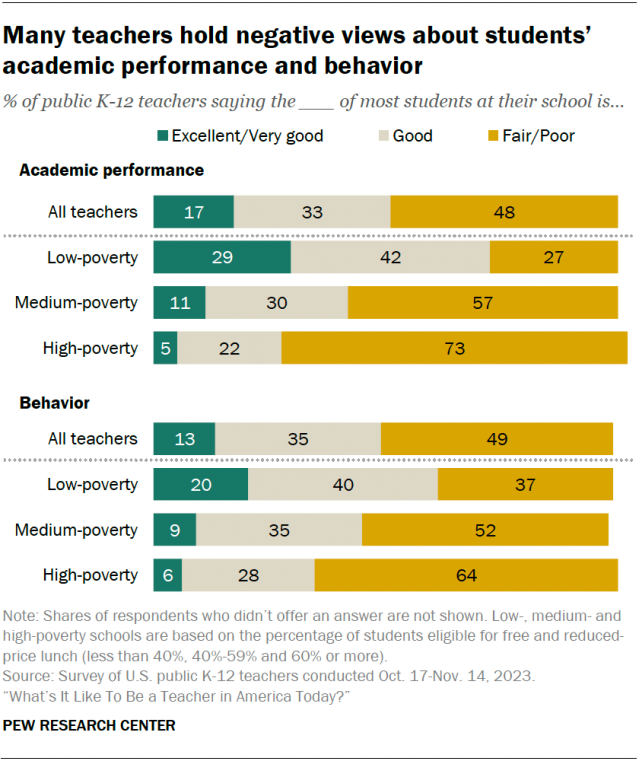
Teachers from high-poverty schools are more likely than those in medium- and low-poverty schools to say the academic performance and behavior of most students at their school are fair or poor.
The differences between high- and low-poverty schools are particularly striking. Most teachers from high-poverty schools say the academic performance (73%) and behavior (64%) of most students at their school are fair or poor. Much smaller shares of teachers from low-poverty schools say the same (27% for academic performance and 37% for behavior).
In turn, teachers from low-poverty schools are far more likely than those from high-poverty schools to say the academic performance and behavior of most students at their school are excellent or very good.
Lasting impact of the COVID-19 pandemic
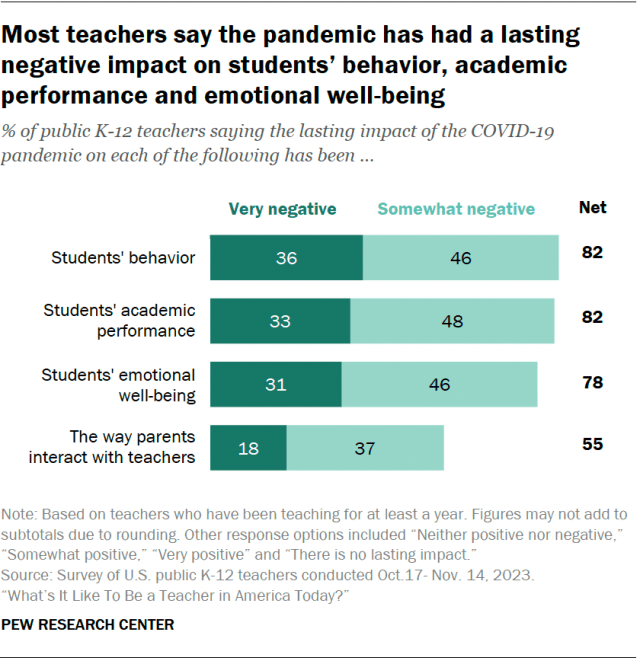
Among those who have been teaching for at least a year, about eight-in-ten teachers say the lasting impact of the pandemic on students’ behavior, academic performance and emotional well-being has been very or somewhat negative. This includes about a third or more saying that the lasting impact has been very negative in each area.
Shares ranging from 11% to 15% of teachers say the pandemic has had no lasting impact on these aspects of students’ lives, or that the impact has been neither positive nor negative. Only about 5% say that the pandemic has had a positive lasting impact on these things.
A smaller majority of teachers (55%) say the pandemic has had a negative impact on the way parents interact with teachers, with 18% saying its lasting impact has been very negative.
These results are mostly consistent across teachers of different grade levels and school poverty levels.
Major problems at school
When we asked teachers about a range of problems that may affect students who attend their school, the following issues top the list:
- Poverty (53% say this is a major problem at their school)
- Chronic absenteeism – that is, students missing a substantial number of school days (49%)
- Anxiety and depression (48%)
One-in-five say bullying is a major problem among students at their school. Smaller shares of teachers point to drug use (14%), school fights (12%), alcohol use (4%) and gangs (3%).
Differences by school level
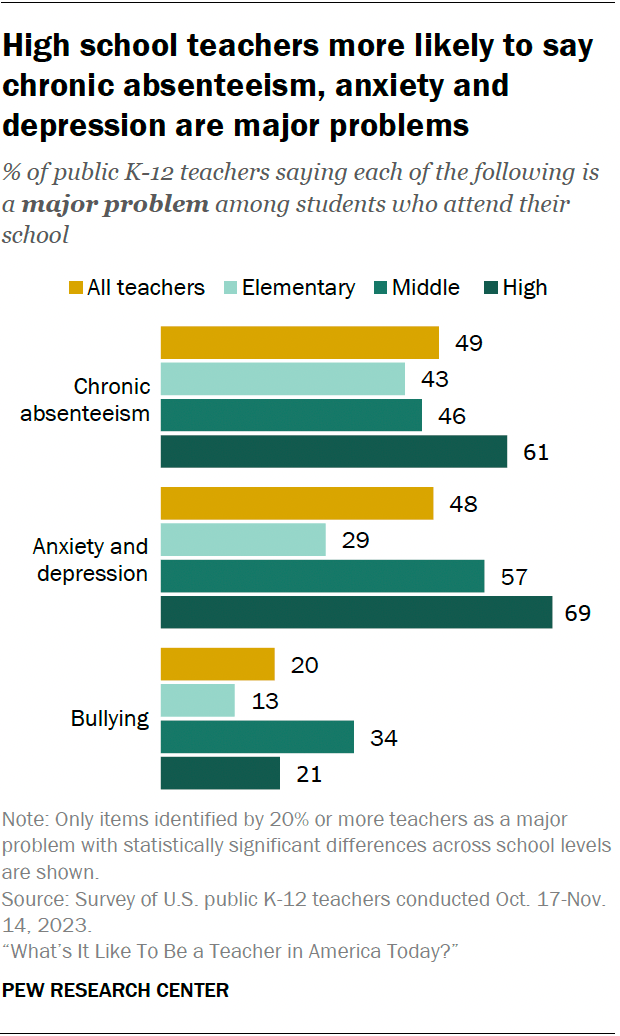
Similar shares of teachers across grade levels say poverty is a major problem at their school, but other problems are more common in middle or high schools:
- 61% of high school teachers say chronic absenteeism is a major problem at their school, compared with 43% of elementary school teachers and 46% of middle school teachers.
- 69% of high school teachers and 57% of middle school teachers say anxiety and depression are a major problem, compared with 29% of elementary school teachers.
- 34% of middle school teachers say bullying is a major problem, compared with 13% of elementary school teachers and 21% of high school teachers.
Not surprisingly, drug use, school fights, alcohol use and gangs are more likely to be viewed as major problems by secondary school teachers than by those teaching in elementary schools.
Differences by poverty level
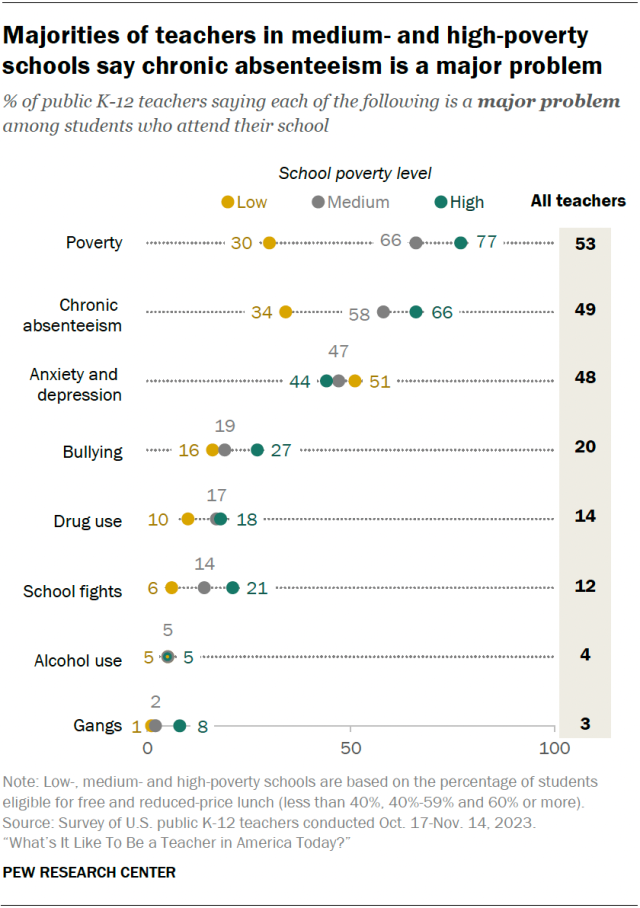
Teachers’ views on problems students face at their school also vary by school poverty level.
Majorities of teachers in high- and medium-poverty schools say chronic absenteeism is a major problem where they teach (66% and 58%, respectively). A much smaller share of teachers in low-poverty schools say this (34%).
Bullying, school fights and gangs are viewed as major problems by larger shares of teachers in high-poverty schools than in medium- and low-poverty schools.
When it comes to anxiety and depression, a slightly larger share of teachers in low-poverty schools (51%) than in high-poverty schools (44%) say these are a major problem among students where they teach.
Discipline practices
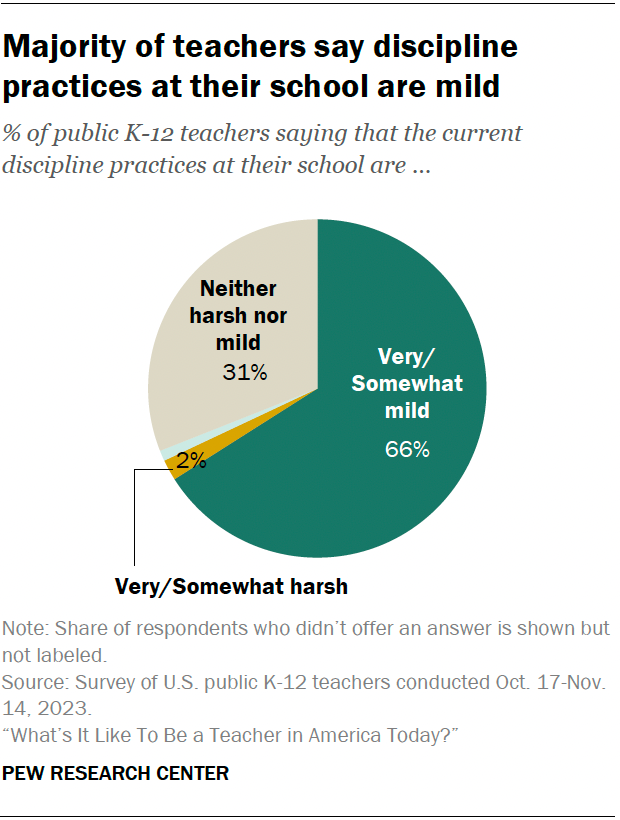
About two-thirds of teachers (66%) say that the current discipline practices at their school are very or somewhat mild – including 27% who say they’re very mild. Only 2% say the discipline practices at their school are very or somewhat harsh, while 31% say they are neither harsh nor mild.
We also asked teachers about the amount of influence different groups have when it comes to determining discipline practices at their school.
- 67% say teachers themselves don’t have enough influence. Very few (2%) say teachers have too much influence, and 29% say their influence is about right.
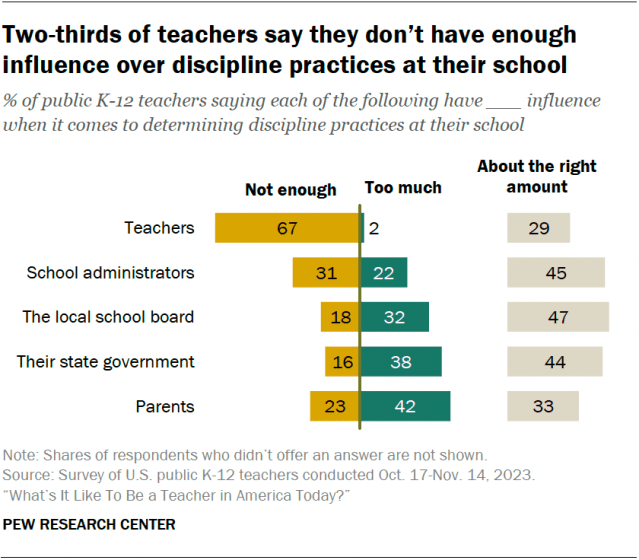
- 31% of teachers say school administrators don’t have enough influence, 22% say they have too much, and 45% say their influence is about right.
- On balance, teachers are more likely to say parents, their state government and the local school board have too much influence rather than not enough influence in determining discipline practices at their school. Still, substantial shares say these groups have about the right amount of influence.
Teachers from low- and medium-poverty schools (46% each) are more likely than those in high-poverty schools (36%) to say parents have too much influence over discipline practices.
In turn, teachers from high-poverty schools (34%) are more likely than those from low- and medium-poverty schools (17% and 18%, respectively) to say that parents don’t have enough influence.
Social Trends Monthly Newsletter
Sign up to to receive a monthly digest of the Center's latest research on the attitudes and behaviors of Americans in key realms of daily life
Report Materials
Table of contents, ‘back to school’ means anytime from late july to after labor day, depending on where in the u.s. you live, among many u.s. children, reading for fun has become less common, federal data shows, most european students learn english in school, for u.s. teens today, summer means more schooling and less leisure time than in the past, about one-in-six u.s. teachers work second jobs – and not just in the summer, most popular.
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .

IMAGES
VIDEO
COMMENTS
Anxiety disorders are normally brained reactions to stress as they alert a person of impending danger. Most people feel sad and low due to disappointments. Feelings normally overwhelm a person leading to depression, especially during sad moments such as losing a loved one or divorce. When people are depressed, they engage in reckless behaviors ...
In addition, initial presentation with social phobia was associated with a 5.7-fold increased risk of developing major depressive disorder. These associations between anxiety and depression can be traced back even earlier in life. For example, childhood behavioral inhibition in response to novelty or strangers, or an extreme anxious temperament ...
Depression is a mood-affective disorder that causes a persistent feeling of sadness, loneliness, and starting loss of interest in things. A major depressive disorder or clinical depression is that which affects feeling, thinking, and behavior and can lead to a variety of emotional and physical problems. Depression causes feelings of sadness and ...
A: Generalized anxiety disorder (GAD) is defined by the American Psychiatric Association as exhibiting symptoms such as excessive worry and anxiety on most days about upcoming events or activities. An individual with GAD may experience restlessness, fatigue, difficulty concentrating, irritability, muscle tension, and sleep disturbance. 7 In the United States, individuals who experience ...
Connect by phone 800-950-6264 or text "Helpline". to 62640, or chat. In a crisis call or text 988.*. Over the past several decades, NAMI has helped change the conversation around mental health, but there's more to do to ensure everyone can access the mental health care and support they need. one-time.
Persistent depression can also exacerbate a person's perception of pain and increase their chances of developing chronic pain. "Depression diminishes a person's capacity to analyze and respond rationally to stress," Dr. Spiegel said. "They end up on a vicious cycle with limited capacity to get out of a negative mental state.".
Anxiety disorders affect nearly 20 percent of American adults. That means millions are beset by an overabundance of the fight-or-flight response that primes the body for action. When you're ...
Both are normal emotions to experience, routinely occurring in response to high-stakes or potentially dangerous situations (in the case of anxiety) or disappointing, upsetting circumstances (in the case of depression). The relationship between these emotions—and their associated clinical conditions, anxiety disorders and mood disorders—is ...
The following strategies are ways to prioritize self-care: Establish and maintain a regular exercise routine with a target of 30 minutes daily. Exercising for smaller amounts of time can also make a difference. Follow a diet of nutritious meals and adequate hydration. Limit caffeinated beverages, alcohol, and added sugar.
This article is a systematic review of the literature on the impact of anxiety and depression on health-related quality of life (HRQoL) in patients with various medical conditions. It summarizes the evidence from 42 studies and discusses the possible mechanisms, implications and limitations of the findings. The article aims to provide a comprehensive overview of the topic and suggest ...
A clinical diagnosis of depression requires several of the following symptoms. These symptoms must occur persistently for nearly every day in a 2-week period . The criteria include feelings of: sadness, anxiety, or "emptiness". hopelessness or pessimism. irritability, frustration, or restlessness.
Anxiety disorders are the most common mental health issue in the United States, affecting about 40 million adults. Major depressive disorder (MDD), or depression, is less common but still affects ...
Essay grade: Good. 2 pages / 978 words. Depression is a disease that afflicts the human psyche in such a way that the afflicted tends to act and react abnormally toward others and themselves. Therefore it comes to no surprise to discover that adolescent depression is strongly linked to teen suicide.
Bipolar Disorder used to be known as "manic depression", because the person experiences depression, normal mood and mania, which is basically the opposite of depression. Symptoms for Bipolar Disorder include feeling great, having a lot of energy, having racing thoughts, little need for sleep, taking fast, having difficulty focusing on tasks ...
Depression and Anxiety will remain a Wiley title but will be published and hosted by Hindawi and will benefit from Hindawi's experience and expertise in publishing open access titles. Depression and Anxiety will continue to undergo a rigorous peer review process ensuring that quality remains high. Manuscripts published after January 1, 2023 ...
Webinar Notice. My name is Kellene Diana and I used to struggle with anxiety and depression. Nobody understood or wanted to understand; in fact they called me names and passed judgment before they even knew what I was going through. It made me so afraid to speak up and speak out about it that it completely silenced me for years.
Conclusion. A major aim of this course was to shed some light on the aetiology of depression and anxiety. At the end of it you should have some idea of the complexity of this enterprise. We have focused on one of the best-studied and hence best-understood contributors to psychopathology - stress. This has biological, social and psychological ...
population aged 16-85 years, 14.4% have an anxiety. disorder. The pre valence of depression is 6.2%, with the. prevalence of unipolar depressive episodes being 4.1%, dysthymia, 1.3%, and bipolar ...
Depression And Anxiety - Free Essay Examples and Topic Ideas. Depression is a serious mental illness that is characterized by a persistent feeling of sadness or hopelessness, loss of interest in activities, changes in appetite and sleeping patterns, fatigue, difficulty concentrating, and sometimes thoughts of self-harm or suicide.
When I'm in a vice grip of depression and anxiety, figuratively and literally, I get tunnel vision. I see only the blades of grass, not the whole yard. One of the body's physiological ...
17. "The anxiety makes me worry that the reason a person isn't replying is because they're ignoring me on purpose or that they have better things to do. The depression tells me I'm not ...
Including over 1,500 participants, the study found that individuals who received medication and psychotherapy for anxiety or depression were 75% less likely to have to stay in the hospital again ...
Major problems at school. When we asked teachers about a range of problems that may affect students who attend their school, the following issues top the list: Poverty (53% say this is a major problem at their school) Chronic absenteeism - that is, students missing a substantial number of school days (49%) Anxiety and depression (48%) One-in ...
41%. Percentage of teens with the highest social media use who rate their overall mental health as poor or very poor, compared with 23% of those with the lowest use. For example, 10% of the highest use group expressed suicidal intent or self-harm in the past 12 months compared with 5% of the lowest use group, and 17% of the highest users expressed poor body image compared with 6% of the lowest ...
DOI: 10.1016/j.ejca.2024.113663 Corpus ID: 268658476; Prevalence of depression, anxiety and stress and its associated factors among women with breast cancer in Sri Lanka @article{Jayarajah2024PrevalenceOD, title={Prevalence of depression, anxiety and stress and its associated factors among women with breast cancer in Sri Lanka}, author={U. Jayarajah and J. Mithushan and W.P.H. Priyan and K ...