- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support

The Importance of Mental Health
Elizabeth is a freelance health and wellness writer. She helps brands craft factual, yet relatable content that resonates with diverse audiences.
:max_bytes(150000):strip_icc():format(webp)/Beth-Plumptre-1000-6a0f2d14202a47fc8c1ec0d21a3e4e4f.jpg)
Akeem Marsh, MD, is a board-certified child, adolescent, and adult psychiatrist who has dedicated his career to working with medically underserved communities.
:max_bytes(150000):strip_icc():format(webp)/akeemmarsh_1000-d247c981705a46aba45acff9939ff8b0.jpg)
Westend61 / Getty Images
Risk Factors for Poor Mental Health
Signs of mental health problems, benefits of good mental health, how to maintain mental health and well-being.
Your mental health is an important part of your well-being. This aspect of your welfare determines how you’re able to operate psychologically, emotionally, and socially among others.
Considering how much of a role your mental health plays in each aspect of your life, it's important to guard and improve psychological wellness using appropriate measures.
Because different circumstances can affect your mental health, we’ll be highlighting risk factors and signs that may indicate mental distress. But most importantly, we’ll dive into all of the benefits of having your mental health in its best shape.
Mental health is described as a state of well-being where a person is able to cope with the normal stresses of life. This state permits productive work output and allows for meaningful contributions to society.
However, different circumstances exist that may affect the ability to handle life’s curveballs. These factors may also disrupt daily activities, and the capacity to manage these changes.
The following factors, listed below, may affect mental well-being and could increase the risk of developing psychological disorders .
Childhood Abuse
When a child is subjected to physical assault, sexual violence, emotional abuse, or neglect while growing up, it can lead to severe mental and emotional distress.
Abuse increases the risk of developing mental disorders like depression, anxiety, post-traumatic stress disorder, or personality disorders.
Children who have been abused may eventually deal with alcohol and substance use issues. But beyond mental health challenges, child abuse may also lead to medical complications such as diabetes, stroke, and other forms of heart disease.
The Environment
A strong contributor to mental well-being is the state of a person’s usual environment . Adverse environmental circumstances can cause negative effects on psychological wellness.
For instance, weather conditions may influence an increase in suicide cases. Likewise, experiencing natural disasters firsthand can increase the chances of developing PTSD. In certain cases, air pollution may produce negative effects on depression symptoms.
In contrast, living in a positive social environment can provide protection against mental challenges.
Your biological makeup could determine the state of your well-being. A number of mental health disorders have been found to run in families and may be passed down to members.
These include conditions such as autism , attention deficit hyperactivity disorder , bipolar disorder , depression , and schizophrenia .
Your lifestyle can also impact your mental health. Smoking, a poor diet , alcohol consumption , substance use , and risky sexual behavior may cause psychological harm. These behaviors have been linked to depression.
When mental health is compromised, it isn’t always apparent to the individual or those around them. However, there are certain warning signs to look out for, that may signify negative changes for the well-being. These include:
- A switch in eating habits, whether over or undereating
- A noticeable reduction in energy levels
- Being more reclusive and shying away from others
- Feeling persistent despair
- Indulging in alcohol, tobacco, or other substances more than usual
- Experiencing unexplained confusion, anger, guilt, or worry
- Severe mood swings
- Picking fights with family and friends
- Hearing voices with no identifiable source
- Thinking of self-harm or causing harm to others
- Being unable to perform daily tasks with ease
Whether young or old, the importance of mental health for total well-being cannot be overstated. When psychological wellness is affected, it can cause negative behaviors that may not only affect personal health but can also compromise relationships with others.
Below are some of the benefits of good mental health.
A Stronger Ability to Cope With Life’s Stressors
When mental and emotional states are at peak levels, the challenges of life can be easier to overcome.
Where alcohol/drugs, isolation, tantrums, or fighting may have been adopted to manage relationship disputes, financial woes, work challenges, and other life issues—a stable mental state can encourage healthier coping mechanisms.
A Positive Self-Image
Mental health greatly correlates with personal feelings about oneself. Overall mental wellness plays a part in your self-esteem . Confidence can often be a good indicator of a healthy mental state.
A person whose mental health is flourishing is more likely to focus on the good in themselves. They will hone in on these qualities, and will generally have ambitions that strive for a healthy, happy life.
Healthier Relationships
If your mental health is in good standing, you might be more capable of providing your friends and family with quality time , affection , and support. When you're not in emotional distress, it can be easier to show up and support the people you care about.
Better Productivity
Dealing with depression or other mental health disorders can impact your productivity levels. If you feel mentally strong , it's more likely that you will be able to work more efficiently and provide higher quality work.
Higher Quality of Life
When mental well-being thrives, your quality of life may improve. This can give room for greater participation in community building. For example, you may begin volunteering in soup kitchens, at food drives, shelters, etc.
You might also pick up new hobbies , and make new acquaintances , and travel to new cities.
Because mental health is so important to general wellness, it’s important that you take care of your mental health.
To keep mental health in shape, a few introductions to and changes to lifestyle practices may be required. These include:
- Taking up regular exercise
- Prioritizing rest and sleep on a daily basis
- Trying meditation
- Learning coping skills for life challenges
- Keeping in touch with loved ones
- Maintaining a positive outlook on life
Another proven way to improve and maintain mental well-being is through the guidance of a professional. Talk therapy can teach you healthier ways to interact with others and coping mechanisms to try during difficult times.
Therapy can also help you address some of your own negative behaviors and provide you with the tools to make some changes in your own life.
A Word From Verywell
Your mental health state can have a profound impact on all areas of your life. If you're finding it difficult to address mental health concerns on your own, don't hesitate to seek help from a licensed therapist .
World Health Organization. Mental Health: Strengthening our Response .
Lippard ETC, Nemeroff CB. The Devastating Clinical Consequences of Child Abuse and Neglect: Increased Disease Vulnerability and Poor Treatment Response in Mood Disorders . Am J Psychiatry . 2020;177(1):20-36. doi:10.1176/appi.ajp.2019.19010020
Helbich M. Mental Health and Environmental Exposures: An Editorial. Int J Environ Res Public Health . 2018;15(10):2207. Published 2018 Oct 10. doi:10.3390/ijerph15102207
Helbich M. Mental Health and Environmental Exposures: An Editorial. Int J Environ Res Public Health . 2018;15(10):2207. Published 2018 Oct 10. doi:10.3390/ijerph15102207
National Institutes of Health. Common Genetic Factors Found in 5 Mental Disorders .
Zaman R, Hankir A, Jemni M. Lifestyle Factors and Mental Health . Psychiatr Danub . 2019;31(Suppl 3):217-220.
Medline Plus. What Is mental health? .
National Alliance on Mental Health. Why Self-Esteem Is Important for Mental Health .
By Elizabeth Plumptre Elizabeth is a freelance health and wellness writer. She helps brands craft factual, yet relatable content that resonates with diverse audiences.
Talk to our experts
1800-120-456-456
- Mental Health Essay

Essay on Mental Health
According to WHO, there is no single 'official' definition of mental health. Mental health refers to a person's psychological, emotional, and social well-being; it influences what they feel and how they think, and behave. The state of cognitive and behavioural well-being is referred to as mental health. The term 'mental health' is also used to refer to the absence of mental disease.
Mental health means keeping our minds healthy. Mankind generally is more focused on keeping their physical body healthy. People tend to ignore the state of their minds. Human superiority over other animals lies in his superior mind. Man has been able to control life due to his highly developed brain. So, it becomes very important for a man to keep both his body and mind fit and healthy. Both physical and mental health are equally important for better performance and results.
Importance of Mental Health
An emotionally fit and stable person always feels vibrant and truly alive and can easily manage emotionally difficult situations. To be emotionally strong, one has to be physically fit too. Although mental health is a personal issue, what affects one person may or may not affect another; yet, several key elements lead to mental health issues.
Many emotional factors have a significant effect on our fitness level like depression, aggression, negative thinking, frustration, and fear, etc. A physically fit person is always in a good mood and can easily cope up with situations of distress and depression resulting in regular training contributing to a good physical fitness standard.
Mental fitness implies a state of psychological well-being. It denotes having a positive sense of how we feel, think, and act, which improves one’s ability to enjoy life. It contributes to one’s inner ability to be self-determined. It is a proactive, positive term and forsakes negative thoughts that may come to mind. The term mental fitness is increasingly being used by psychologists, mental health practitioners, schools, organisations, and the general population to denote logical thinking, clear comprehension, and reasoning ability.
Negative Impact of Mental Health
The way we physically fall sick, we can also fall sick mentally. Mental illness is the instability of one’s health, which includes changes in emotion, thinking, and behaviour. Mental illness can be caused due to stress or reaction to a certain incident. It could also arise due to genetic factors, biochemical imbalances, child abuse or trauma, social disadvantage, poor physical health condition, etc. Mental illness is curable. One can seek help from the experts in this particular area or can overcome this illness by positive thinking and changing their lifestyle.
Regular fitness exercises like morning walks, yoga, and meditation have proved to be great medicine for curing mental health. Besides this, it is imperative to have a good diet and enough sleep. A person needs 7 to 9 hours of sleep every night on average. When someone is tired yet still can't sleep, it's a symptom that their mental health is unstable. Overworking oneself can sometimes result in not just physical tiredness but also significant mental exhaustion. As a result, people get insomnia (the inability to fall asleep). Anxiety is another indicator.
There are many symptoms of mental health issues that differ from person to person and among the different kinds of issues as well. For instance, panic attacks and racing thoughts are common side effects. As a result of this mental strain, a person may experience chest aches and breathing difficulties. Another sign of poor mental health is a lack of focus. It occurs when you have too much going on in your life at once, and you begin to make thoughtless mistakes, resulting in a loss of capacity to focus effectively. Another element is being on edge all of the time.
It's noticeable when you're quickly irritated by minor events or statements, become offended, and argue with your family, friends, or co-workers. It occurs as a result of a build-up of internal irritation. A sense of alienation from your loved ones might have a negative influence on your mental health. It makes you feel lonely and might even put you in a state of despair. You can prevent mental illness by taking care of yourself like calming your mind by listening to soft music, being more social, setting realistic goals for yourself, and taking care of your body.
Surround yourself with individuals who understand your circumstances and respect you as the unique individual that you are. This practice will assist you in dealing with the sickness successfully. Improve your mental health knowledge to receive the help you need to deal with the problem. To gain emotional support, connect with other people, family, and friends. Always remember to be grateful in life. Pursue a hobby or any other creative activity that you enjoy.
What does Experts say
Many health experts have stated that mental, social, and emotional health is an important part of overall fitness. Physical fitness is a combination of physical, emotional, and mental fitness. Emotional fitness has been recognized as the state in which the mind is capable of staying away from negative thoughts and can focus on creative and constructive tasks.
He should not overreact to situations. He should not get upset or disturbed by setbacks, which are parts of life. Those who do so are not emotionally fit though they may be physically strong and healthy. There are no gyms to set this right but yoga, meditation, and reading books, which tell us how to be emotionally strong, help to acquire emotional fitness.
Stress and depression can lead to a variety of serious health problems, including suicide in extreme situations. Being mentally healthy extends your life by allowing you to experience more joy and happiness. Mental health also improves our ability to think clearly and boosts our self-esteem. We may also connect spiritually with ourselves and serve as role models for others. We'd also be able to serve people without being a mental drain on them.
Mental sickness is becoming a growing issue in the 21st century. Not everyone receives the help that they need. Even though mental illness is common these days and can affect anyone, there is still a stigma attached to it. People are still reluctant to accept the illness of mind because of this stigma. They feel shame to acknowledge it and seek help from the doctors. It's important to remember that "mental health" and "mental sickness" are not interchangeable.
Mental health and mental illness are inextricably linked. Individuals with good mental health can develop mental illness, while those with no mental disease can have poor mental health. Mental illness does not imply that someone is insane, and it is not anything to be embarrassed by. Our society's perception of mental disease or disorder must shift. Mental health cannot be separated from physical health. They both are equally important for a person.
Our society needs to change its perception of mental illness or disorder. People have to remove the stigma attached to this illness and educate themselves about it. Only about 20% of adolescents and children with diagnosable mental health issues receive the therapy they need.
According to research conducted on adults, mental illness affects 19% of the adult population. Nearly one in every five children and adolescents on the globe has a mental illness. Depression, which affects 246 million people worldwide, is one of the leading causes of disability. If mental illness is not treated at the correct time then the consequences can be grave.
One of the essential roles of school and education is to protect boys’ and girls' mental health as teenagers are at a high risk of mental health issues. It can also impair the proper growth and development of various emotional and social skills in teenagers. Many factors can cause such problems in children. Feelings of inferiority and insecurity are the two key factors that have the greatest impact. As a result, they lose their independence and confidence, which can be avoided by encouraging the children to believe in themselves at all times.
To make people more aware of mental health, 10th October is observed as World Mental Health. The object of this day is to spread awareness about mental health issues around the world and make all efforts in the support of mental health.
The mind is one of the most powerful organs in the body, regulating the functioning of all other organs. When our minds are unstable, they affect the whole functioning of our bodies. Being both physically and emotionally fit is the key to success in all aspects of life. People should be aware of the consequences of mental illness and must give utmost importance to keeping the mind healthy like the way the physical body is kept healthy. Mental and physical health cannot be separated from each other. And only when both are balanced can we call a person perfectly healthy and well. So, it is crucial for everyone to work towards achieving a balance between mental and physical wellbeing and get the necessary help when either of them falters.

Mental Health Essay for Students and Children
500+ words essay on mental health.
Every year world mental health day is observed on October 10. It was started as an annual activity by the world federation for mental health by deputy secretary-general of UNO at that time. Mental health resources differ significantly from one country to another. While the developed countries in the western world provide mental health programs for all age groups. Also, there are third world countries they struggle to find the basic needs of the families. Thus, it becomes prudent that we are asked to focus on mental health importance for one day. The mental health essay is an insight into the importance of mental health in everyone’s life.

Mental Health
In the formidable years, this had no specific theme planned. The main aim was to promote and advocate the public on important issues. Also, in the first three years, one of the central activities done to help the day become special was the 2-hour telecast by the US information agency satellite system.
Mental health is not just a concept that refers to an individual’s psychological and emotional well being. Rather it’s a state of psychological and emotional well being where an individual is able to use their cognitive and emotional capabilities, meet the ordinary demand and functions in the society. According to WHO, there is no single ‘official’ definition of mental health.
Thus, there are many factors like cultural differences, competing professional theories, and subjective assessments that affect how mental health is defined. Also, there are many experts that agree that mental illness and mental health are not antonyms. So, in other words, when the recognized mental disorder is absent, it is not necessarily a sign of mental health.
Get the huge list of more than 500 Essay Topics and Ideas
One way to think about mental health is to look at how effectively and successfully does a person acts. So, there are factors such as feeling competent, capable, able to handle the normal stress levels, maintaining satisfying relationships and also leading an independent life. Also, this includes recovering from difficult situations and being able to bounce back.
Important Benefits of Good Mental Health
Mental health is related to the personality as a whole of that person. Thus, the most important function of school and education is to safeguard the mental health of boys and girls. Physical fitness is not the only measure of good health alone. Rather it’s just a means of promoting mental as well as moral health of the child. The two main factors that affect the most are feeling of inferiority and insecurity. Thus, it affects the child the most. So, they lose self-initiative and confidence. This should be avoided and children should be constantly encouraged to believe in themselves.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

Home — Essay Samples — Nursing & Health — Mental Health — The Importance of Mental Health Awareness
The Importance of Mental Health Awareness
- Categories: Mental Health Social Isolation Stress Management
About this sample

Words: 1622 |
Updated: 4 November, 2023
Words: 1622 | Pages: 4 | 9 min read
Table of contents
Introduction, mental health awareness, video version, emotional well-being, psychological well‐being, social well-being.
- Health Effects of Social Isolation and Loneliness. (n.d.). Retrieved from https://www.aginglifecarejournal.org/health-effects-of-social-isolation-and-loneliness/.
- Top of Form Mental Health Myths and Facts https://www.mentalhealth.gov/basics/mental-health-myths-facts
- Mental Health Care Services by Family Physicians Position Paper. American Academy of Family Physicians Web site. http://www.aafp.org/online/en/home/policy/policies/m/mentalhealthcareservices.htm. Accessed February 11, 2013. [Google Scholar]
- Newman, T. (2017, August 24). Mental health: Definition , common disorders, and early signs. Retrieved from https://www.medicalnewstoday.com/articles/154543.php.
- Bottom of Form Rodriguez, B. D., Hurley, K., Upham, B., Kilroy, D. S., Dark, N., & Abreu, E (n.d.).Happiness and Emotional Well-Being. Retrieved from https://www.everydayhealth.com/emotional-health/understanding/index.aspx.
- World Health Organization. The Global Burden of Disease, 2004 Update. Part 4, Burden of Disease, DALYs. http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf . Accessed January 10, 2013. [Google Scholar]

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
7 pages / 3006 words
5 pages / 2449 words
5 pages / 2111 words
2 pages / 834 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Mental Health
However, psychology also uses behavior along with the mapping to the DSM from the checklist survey to separate genuine from faked mental illness and this epistemological problem can be solved using the proven to be successful [...]
Mental health stigma is a pervasive issue that hinders individuals from seeking help, perpetuates myths, and marginalizes those who experience mental health challenges. This essay explores the nature of mental health stigma in [...]
Mental health stigma is a pervasive issue that has long hindered individuals from seeking the help they need and perpetuated damaging stereotypes and misconceptions. In this comprehensive essay, we will delve deeply into the [...]
Mental illness within the criminal justice system is a complex and pressing issue that intersects legal, medical, and ethical considerations. This essay examines the challenges posed by mental illness among individuals in the [...]
“Eat your vegetables! Exercise! Get a good night's sleep!” We’ve all known to take care of our bodies since grade school P. E. class. But what about our mental health, isn’t mental health just as important as physical health? [...]
Arnekrans et al. (2018) state that childhood trauma is also known as developmental trauma and this refers to numerous amounts of stressful experiences in child development. Many of these stressful experiences consist of divorce, [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Expository Essay
Expository Essay About Mental Health
Learn to Write Expository Essay About Mental Health - Examples & Tips
People also read
Complete Guide to Expository Essays: Writing Help and Topics
Interesting Expository Essay Topics For Your Next Paper
How to Write an Expository Essay Outline Like a Pro
Types of Expository Writing - Definition and Examples
Free Expository Essay Examples For Students
Ultimate Guide to Writing an Expository Essay About a Person
Learn to Write an Expository Essay About Yourself
Learn the Basics of Crafting an Expository Essay about a Book
How to Write an Expository Essay about Bullying: A Guide
Expository Essay About Dogs: Steps, Examples & Topics
A Guide to Writing an Expository Essay about Education
Expository Essay About Friendship: A Writing Guide
Discover How to Write Expository Essays About Music – A Step-by-Step Guide
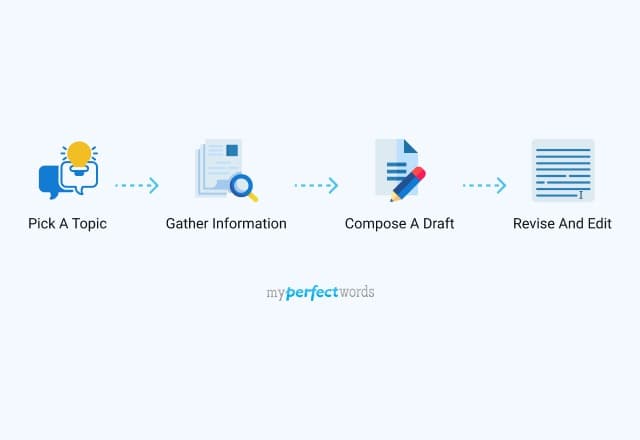
Do you need to write an expository essay about mental health but don't know how to begin?
Essays about mental health are common for students of psychology, sociology, and health care. However, other students also get to write such essays to raise awareness about this important issue.
Writing about mental health can help raise awareness and educate others about the importance of mental health. It can also provide a platform for you to express your thoughts, feelings, and experiences on the subject.
In this blog post, we will discuss what is an expository essay, provide examples, and outline the steps for writing one. So read on to learn more about how to write an expository essay on mental health.
Tough Essay Due? Hire Tough Writers!
- 1. What is an Expository Essay About Mental Health?
- 2. Essay About Mental Health Examples
- 3. Expository Essay Topics About Mental Illness
- 4. How To Write an Essay About Mental Health
- 5. Tips for Writing a Mental Health Essay
What is an Expository Essay About Mental Health?
An expository essay is a type of academic writing that provides an explanation, description, or argument about a certain topic. It seeks to explain and clarify the subject matter for the readers.
The goal of this type of essay is not to share your opinion or persuade the readers, but rather to inform them.
An expository essay on mental health aims to discuss and inform about different aspects of mental health.
The term mental health can refer to various aspects, such as mental health issues, psychological resilience, emotional health, etc. So, the scope of an expository essay on mental health is quite broad depending on your topic.
Here is a video that explains what mental health means in simple words:
Essay About Mental Health Examples
If you are wondering what a good essay about mental health issues looks like, here are a few example essays to help you get started:
Expository Essay About Social Media And Mental Health
Expository Essay Example About Depression
Expository Essay About Mental Health Awareness
Importance of Mental Health Essay Example
Expository Essay About Mental Health Of Students
Need more expository writing samples? Check out our expository essay examples blog!
Expository Essay Topics About Mental Illness
Here is a list of topics about mental health to help you start.
- How does mental health affect physical health in children and adolescents?
- The role of stigma in mental health problems.
- What are the basic principles of positive psychology?
- How are physical & emotional health related?
- How can mindfulness improve mental health condition?
- What is the importance of world mental health day?
- Technology's impact on modern mental health issues.
- Understanding trauma-informed care and its importance.
- The role of the media in creating stereotypes about mental health issues.
- How do different cultures view mental health disorders?
- Common misconceptions about mental health in the United States.
You can choose one of these topics, to begin with. Moreover, these topics will help you brainstorm your own topic as well.
You can check out our expository essay topics blog for a list of creative topic ideas.
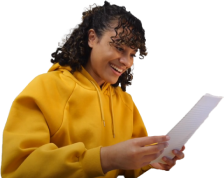
How To Write an Essay About Mental Health
Now that you know what an expository essay on mental health is and have some topics to choose from, it’s time to start writing.
Here are the steps you need to follow:
1. Choose Your Topic:
Brainstorm some ideas related to mental health. Try to pick a topic that interests you so that researching and writing about it will be easier for you.
Choosing a topic that is narrow enough to be covered within the word limit is also important. Moreover, make sure that the topic is not too complex for you to explain.
2. Conduct Research:
Once you have chosen your topic, it’s time to conduct extensive research.
A good expository essay should include facts, evidence, and other supporting information from reliable sources like journals, books, and articles. Make sure that you cite your sources properly.
3. Outline the Essay:
An outline will help you organize your ideas and create a clear structure for your essay. It is also an important step to ensure that all the necessary information is included in the essay.
In an expository essay outline , you should include the main points you want to discuss. Additionally, it should include the supporting evidence and arguments you gathered during the research.
4. Write the Introduction:
The introduction is the first part of your essay. It should include a hook to grab the reader’s attention and introduce the topic. Additionally, you should provide a brief overview of what will be discussed in the essay.
Finally, you should end your mental illness essay introduction with a thesis statement. A thesis statement is a sentence that states the main idea of your essay.
5. Write the Body Paragraphs:
The body paragraphs are where you explain and expand on your main points. Each paragraph should include evidence to support your claims and a brief explanation of how the evidence is related to the topic.
Remember that each body paragraph should focus on one main point and be organized in a logical manner.
6. Write the Conclusion:
The conclusion is where you restate the thesis statement and summarize the main points of the essay. Additionally, you should provide a brief explanation of how these points support your thesis statement.
Finally, end your conclusion with a call to action or an insightful thought that encourages readers to learn more about mental health.
7. Edit and Proofread:
Once you are done writing the essay, it’s important to go through each sentence and look for mistakes.
Make sure that all grammar, spelling, and punctuation errors are corrected. Additionally, make sure that the essay is well-structured and flows logically from one point to another.
Editing and proofreading can help you improve the quality of your work and ensure that all necessary information is included.
Following these steps will help you write a clear and well-researched expository essay on mental health.
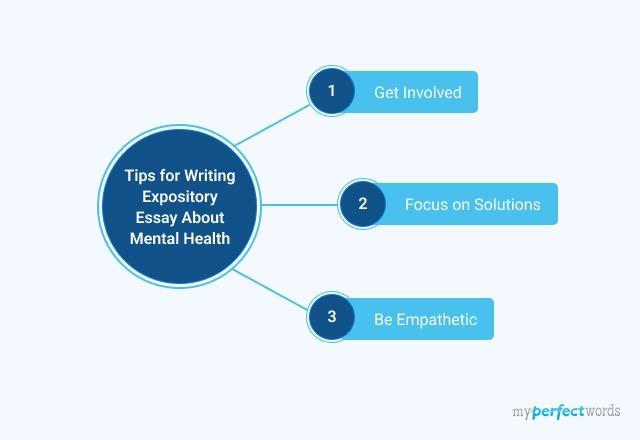
Tips for Writing a Mental Health Essay
Writing about mental health requires more than a basic understanding of the subject. It is a sensitive and emerging topic, and new research is being produced every day. So, you need to be careful while proceeding with your essay.
Here are a few tips that can help you write a worthwhile essay on mental health:
- Get Involved
Mental health essays often benefit greatly when written with personal insight or experience.
If you have any personal life experiences related to mental health, incorporate them into your essay to add more depth. Make your essay relatable to people’s daily life.
- Focus on Solutions
When discussing a sensitive topic like mental health it’s important to focus on the solutions.
Consider suggesting ways people can manage their own mental wellness or outlining how families can support each other during difficult times.
- Be Empathetic
While writing your essay try to put yourself in the reader’s shoes so that you present the information in a kind and sympathetic manner.
For many people, mental problems are a part of life. So avoid any language that could potentially be offensive or insensitive towards those who struggle with mental illness.
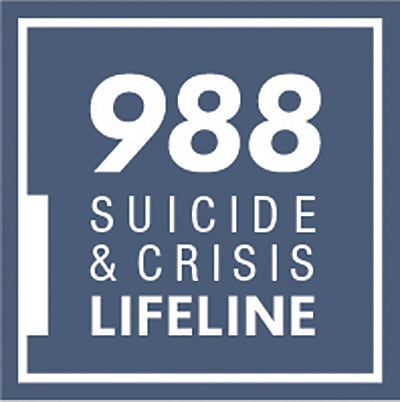
If you or someone you know is going through a rough time, feeling depressed, or thinking about self-harm, you can call the National Suicide Prevention Lifeline at 1-800-273-8255 or visit its website here. Other international suicide helplines can be found at befrienders.org.
Wrapping it up,
Mental health is a complex and important issue, and writing an essay on it requires proper research, understanding, empathy, and focus. By following these steps and tips, you can write an effective essay on mental health that will be well-received by your readers.
Do you want a professional to write it for you instead? Don't worry, we've got your back.
MyPerfectWords.com provides pro essay writing service and can help you write the perfect mental health essay. Our team of expository essay writers has in-depth knowledge of the subject.
Our expository essay writing service will provide you with a well-written, high-quality essay that is sure to get you top grades.
So, why wait? Hire the top essay writer now!

Write Essay Within 60 Seconds!

Caleb S. has been providing writing services for over five years and has a Masters degree from Oxford University. He is an expert in his craft and takes great pride in helping students achieve their academic goals. Caleb is a dedicated professional who always puts his clients first.

Paper Due? Why Suffer? That’s our Job!
Keep reading
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley - PMC COVID-19 Collection

Debate: Student mental health matters – the heightened need for school‐based mental health in the era of COVID‐19
Deborah m. weisbrot.
1 Department of Psychiatry, Renaissance School of Medicine, Stony Brook University, Stony Brook NY, USA
2 Nevada Center for Excellence in Disabilities, College of Education and Human Development, University of Nevada, Reno NV, USA
The COVID‐19 pandemic has highlighted existing gaps in school‐based mental health services and created new and urgent needs to address student mental health. Evidence from early in the pandemic already suggests that preexisting educational and mental health disparities have increased under the stress of the current health crisis. School mental health professionals are essential to help address anxiety, to promote social adjustment in the 'new normal', and to address trauma, grief, and loss. Schools will also need to creatively support teachers during this unprecedented time. Such efforts will require adequate funding and advocacy for the inclusion of school‐based mental health supports within governmental COVID‐19 aid packages.
Child and adolescent psychiatrists are taught from day 1 of training to always place the child’s best interest first. However, children can only do well when their caregivers and communities are similarly well supported. In considering the complex challenges of the COVID‐19 crisis, the best interests of children can only be met by simultaneously considering the best interests of parents, families, teachers, and school staff.
As schools open, in whatever shape or form, mental health practitioners who work in schools will be busier than ever. Even before this COVID‐19 apocalypse began, schools were already ill equipped to meet students’ mental health needs. It has been estimated that more than seven million children in the United States have a mental health disorder; less than half of those diagnosed actually receive treatment, and of those who do receive treatment, over 75% receive this treatment at schools (McKay, Lynn, & Bannon, 2005 ; Merikangas et al., 2011 ). Whether schools open, stay closed, or work semivirtually, the existing challenges will multiply and vary according to the specific solutions developed. Just as hospitals faced a crisis when the pandemic began, now school administrators, families, students, and school staff face similar distress, uncertainty, and confusion about how to return to school given the new realities of COVID‐19. The solutions will necessarily vary by community, level of COVID infection, school size, and resources. Surprisingly, in all that has been written about returning to school, very little has been targeted toward meeting the mental health needs of students, teachers, and other school staff.
Mental health contributes to overall health, and students must be healthy enough to learn. We know our children should return to school, but to do that they need a safe, secure, and supportive learning environment with professionals who also feel safe and cared about. If the stress and illness burden is not too great, we hope that the resilience of youth will prevail. However, those children already burdened by mental health challenges may suffer more. Mental health and educational disparities will widen the pandemic’s negative impact in marginalized and under‐resourced communities. Evidence from two U.S. national surveys conducted by the Edweek Research Center in Spring of 2020 already confirm vast disparities, with schools located in lower socioeconomic communities less able to provide access to technology, to reach all students, or to provide 'live' distance learning instruction (Herold B, April 2020 ). Fairness and equity require that those bearing a disproportionate impact of the pandemic be provided sufficient access to equipment, services, and technology, and mental health support to address systemic cultural disadvantages in education and mental health worsened by COVID‐19.
Decisions related to school reopening must be data‐driven, relying on the best available medical understanding and public health guidance. In addition, different populations, such as children receiving special education, children in foster care, or non‐English‐language learners, may require approaches that differ from the general approach. Children at different developmental stages will have specific needs. What is good for some students and their families will not necessarily be good for others.
Multiple potential mental health consequences arise from school closures related to COVID‐19. Lost learning opportunities during school closures result in possible regression of educational and emotional coping skills, particularly in children with special education needs. For some children, the pandemic may produce heightened fear, anxiety, and depression, leading to further difficulty in emotion regulation and behavior, learning, and interpersonal relationships. The fears of school staff will also need to be recognized and discussed, as these will impact the students in their care.
School mental health professionals will be essential in helping to shape messages to students and families about school re‐entry, to address anxiety, to promote social adjustment to the 'new normal', and to address other unanticipated mental health concerns that are sure to arise during this national trauma experience. Teachers and school personnel should receive training on how to talk with and support children during a pandemic. Intentional strategies to help students adapt to new school environments should be developed. Schools will also need to creatively support teachers in their efforts during this unprecedented time. Addressing the grief of those who have suffered loss will also be critical. Fortunately, many great resources to assist in this effort have already been developed. For example, the National Center for School Mental Health ( http://www.schoolmentalhealth.org/COVID‐19/ ) and the Mental Health Technology Transfer Center Network ( https://mhttcnetwork.org/centers/global‐mhttc/responding‐covid‐19‐school‐mental‐health‐resources ) have both developed school mental health resource pages for dealing with COVID‐19.
It is hard to imagine how children can return to school safely without providing additional (and substantial) financial support. Added to the costs of the physical needs created by the pandemic will be the increased costs necessary to bolster a full continuum of educational AND mental health supports. Funding of school‐based mental health supports will be necessary for prevention of staff burnout and trauma effects, as well as early identification and intervention of mental health problems in the increased numbers of students at high risk for adverse outcomes.
Child mental health organizations should be advocating to ensure that mental health programs, specifically children’s mental health, are included in governmental aid packages. Solidarity with other mental health organizations is essential to ensure that such provisions are included in any governmental COVID‐19 relief packages. Provisions should include increasing funding for existing and new mental health programs. The American Academy of Child and Adolescent Psychiatry (AACAP) Schools Committee, which cowrote this editorial, is especially concerned with ensuring that the best information on school mental health is available as it is developed. Toward that end, a recently published 'Children and Schools Resource Center' is available on the AACAP website: https://www.aacap.org/AACAP/Families_and_Youth/Resource_Centers/Schools_Resource_Center/Home.aspx .
As child and adolescent psychiatrists, mental health is definitely 'our lane'. Every student, every family, and every school staff member will have a COVID‐19 story. We need to do our best to hear them all and respond when help is needed.
Ethical approval
No ethical approval was required for this article.
Acknowledgements
D.M.W. receives royalties from Cambridge University Press for co‐editing two textbooks. E.R. receives grant funding from the Maternal and Child Health Bureau/Health Resources and Services Administration and from the Nevada Division of Public and Behavioral Health; she also receives funding from the Washoe County School District for school consultation. The authors have declared that they have no competing or potential conflicts of interest.
- Herold, B. (2020). “ The Disparities in Remote Learning Under Coronavirus (in Charts) ”, April 10, 2020, Education Week.
- McKay, M.M. , Lynn, C.J. , & Bannon, W.M. (2005). Understanding inner city child mental health need and trauma exposure: implications for preparing urban service providers . American Journal of Orthopsychiatry , 75 , 201–210. [ PubMed ] [ Google Scholar ]
- Merikangas, K.R. , He, J.P. , Burstein, M. , Swendsen, J. , Avenevoli, S. , Case, B. , … & Olfson, M. (2011). Service utilization for lifetime mental disorders in US adolescents: Results of the National Comorbidity Survey‐Adolescent Supplement (NCS‐A) . Journal of the American Academy of Child and Adolescent Psychiatry , 50 , 32–45. [ PMC free article ] [ PubMed ] [ Google Scholar ]
About Mental Health
- Mental Health Basics
- Types of Mental Illness
What is mental health?
Mental health includes our emotional, psychological, and social well-being. It affects how we think, feel, and act. It also helps determine how we handle stress, relate to others, and make healthy choices. 1 Mental health is important at every stage of life, from childhood and adolescence through adulthood.
Why is mental health important for overall health?
Mental and physical health are equally important components of overall health. For example, depression increases the risk for many types of physical health problems, particularly long-lasting conditions like diabetes , heart disease , and stroke. Similarly, the presence of chronic conditions can increase the risk for mental illness. 2
Can your mental health change over time?
Yes, it’s important to remember that a person’s mental health can change over time, depending on many factors. When the demands placed on a person exceed their resources and coping abilities, their mental health could be impacted. For example, if someone is working long hours, caring for a relative, or experiencing economic hardship, they may experience poor mental health.
How common are mental illnesses?
Mental illnesses are among the most common health conditions in the United States.
- More than 1 in 5 US adults live with a mental illness.
- Over 1 in 5 youth (ages 13-18) either currently or at some point during their life, have had a seriously debilitating mental illness. 5
- About 1 in 25 U.S. adults lives with a serious mental illness, such as schizophrenia, bipolar disorder, or major depression. 6
What causes mental illness?
There is no single cause for mental illness. A number of factors can contribute to risk for mental illness, such as
- Adverse Childhood Experiences , such as trauma or a history of abuse (for example, child abuse, sexual assault, witnessing violence, etc.)
- Experiences related to other ongoing (chronic) medical conditions, such as cancer or diabetes
- Biological factors or chemical imbalances in the brain
- Use of alcohol or drugs
- Having feelings of loneliness or isolation
People can experience different types of mental illnesses or disorders, and they can often occur at the same time. Mental illnesses can occur over a short period of time or be episodic. This means that the mental illness comes and goes with discrete beginnings and ends. Mental illness can also be ongoing or long-lasting.
There are more than 200 types of mental illness. Some of the main types of mental illness and disorders are listed here .
- Strengthening Mental Health Promotion . Fact sheet no. 220. Geneva, Switzerland: World Health Organization.
- Chronic Illness & Mental Health . Bethesda, MD: National Institutes of Health, National Institute of Mental Health. 2015.
- Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6(3):168-176.
- Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. Rockville, MD: Center for Behavioral Health Statistics and Quality. Substance Abuse and Mental Health Services Administration. 2016.
- Merikangas KR, He J, Burstein M, et al. Lifetime Prevalence of Mental Disorders in US Adolescents: Results from the National Comorbidity Study-Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(10):980-989. doi:10.1016/j.jaac.2010.05.017.
- Health & Education Statistics . Bethesda, MD: National Institute of Mental Health. National Institutes of Health. 2016.
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, Severity, and Comorbidity of Twelve-month DSM-IV Disorders in the National Comorbidity Survey Replication (NCS-R). Archives of general psychiatry. 2005;62(6):617-627. doi:10.1001/archpsyc.62.6.617.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. (2016). Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. Rockville, MD.
- Rui P, Hing E, Okeyode T. National Ambulatory Medical Care Survey: 2014 State and National Summary Tables. Atlanta, GA: National Center for Health Statistics. Centers for Disease Control and Prevention. 2014.
- Web-based Injury Statistics Query and Reporting System (WISQARS) . Atlanta, GA: National Center for Injury Prevention and Control. Centers for Disease Control and Prevention. 2015.
- Insel, T.R. Assessing the Economic Costs of Serious Mental Illness. Am J Psychiatry. 2008 Jun;165(6):663-5. doi: 10.1176/appi.ajp.2008.08030366.
- HCUP Facts and Figures: Statistics on Hospital-based Care in the United States, 2009. Rockville, MD: Agency for Healthcare Research and Quality. 2009.
- Reeves, WC et al. CDC Report: Mental Illness Surveillance Among Adults in the United States. MMWR Morb Mortal Wkly Rep 2011;60(03);1-32.
- Parks, J., et al. Morbidity and Mortality in People with Serious Mental Illness. Alexandria, VA: National Association of State Mental Health Program Directors Council. 2006.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

Online Students
For All Online Programs
International Students
On Campus, need or have Visa
Campus Students
For All Campus Programs
Why is Mental Health Important?

(Note: This article discusses suicide and other serious issues pertaining to mental health.)
Whether through a minor bump in your journey or a full-blown crisis, you may have struggled with your mental health in some capacity in the last few years. Faced with a seemingly endless onslaught of bad news on top of life’s usual challenges, it can be difficult to prioritize yourself while pursuing educational and professional goals. Focusing on your mental health is perhaps the most powerful step you can take to improve your overall quality of life.
According to the National Institute of Mental Health (NIMH), 1 in 5 adults now lives with a moderate to severe mental health condition. The Centers for Disease Control and Prevention (CDC) further notes that over 50% of Americans will be diagnosed with mental illness in their lifetime. But what exactly is mental health, and why is it so important?
What is Mental Health?

“When in a state of good mental health, a person has a general positive outlook, can accomplish daily tasks, maintain relationships and engage in meaningful recreation,” said Dr. Darleen Dempster , a Southern New Hampshire University (SNHU) clinical faculty member in the clinical mental health counseling program . “This includes a sense of balance and empowerment to set boundaries and address life and work goals, step by step.”
In addition to the impact that mental health has on your day-to-day life, serious mental health issues can affect your relationships, career, education and long-term goals. As rates of mental illness increase worldwide, addressing your mental health challenges as they arise can change —or even save — your life.
Why is Mental Health Important for Students?
The World Heath Organization (WHO) reports a sharp rise in the number of people experiencing mental illness in recent years, with the COVID-19 pandemic exacerbating mental health problems throughout the world. For students, it is more important than ever to address your mental health issues to stay mentally healthy and keep up with your educational and personal goals.
Even before the pandemic, mental health was a prominent concern for students. In 2019, the National College Health Assessment (NCHA) noted that many students reported feeling exhausted, lonely and overwhelmed, among other symptoms and difficulties ( NCHA PDF Source ). Of the surveyed students, 20.2% reported experiencing depression and 27.8% reported experiencing anxiety that affected their studies in the preceding year.
“College can be a stressful time as you manage academic demands on top of other life demands,” Dempster said. “However, just as many students can learn to be successful academically, you can also learn to manage and improve mental health outcomes, including managing stress.”
Ways to Cope with Stress
Stress management can be a vital aspect of student success, especially for busy students who may also be working or caring for others. Dempster and the CDC recommend several methods to help manage stress:
- Adequate sleep
- Avoidance of alcohol and substance abuse
- Breaking down large tasks into smaller, more manageable tasks
- Cultivating healthy relationships
- Eating well
- Meditation, breathing exercises and other self-care activities
“At times, it is necessary also to set boundaries, to communicate needs, to be flexible to changing circumstances and to let go of perfectionistic standards,” Dempster said. “There should be no shame in seeking out mental health care as needed, just as one would not feel shame in seeking medical care for a persistent medical issue.”
Some colleges have free, real-time mental health services for students—for example, students at SNHU can access the school’s HelpU program. If you are a student struggling with mental health, look into what resources are available through your school.
How is Mental Health Connected to Physical Health?
The NIMH reports that some mental illnesses like depression and anxiety can cause physical symptoms that are otherwise unexplained. The CDC also reports that mental illness can increase the risk of diabetes, stroke and heart disease and has recognized that severe mental illness can increase the likelihood of a person becoming seriously ill after contracting COVID-19. At the same time, chronic physical health issues can also contribute to mental health issues.
“Factors like proper diet, sleep and exercise can positively impact our mental health. Conversely, lack of sleep, poor diet and lack of exercise can impede our ability to manage stress and life’s demands,” Dempster said. “Sometimes mental health symptoms can lead to somatic symptoms due to tension, worrisome thoughts or other reactions. Therefore, there is a circular loop between mental and physical symptoms.”
What Are Examples of Mental Health Problems?
Mental health problems can affect your life in various ways, depending upon the issue or disorder. The following are examples of different mental health problems and their corresponding challenges and symptoms.
Anxiety and Depression
Anxiety disorders are a leading mental health issue globally, and the NIMH approximates that almost 1 in 3 people will experience an anxiety disorder in their lifetime. Symptoms of anxiety can range from tenseness or nervousness to panic attacks and physical illness. Anxiety can refer to generalized anxiety disorder, social anxiety, separation anxiety, specific phobias and other anxiety-based disorders.
Depression is another common disorder with the capacity to severely impact a person’s life, according to NIMH. Symptoms typically include persistent sadness, emptiness, irritability, impaired motivation, guilt or feelings of low self-worth. People with depression also may have difficulties focusing, aches, pains, digestive issues or changes in their sleep and eating habits.
Some of the most serious symptoms of depression are suicidal thoughts and actions. Suicide is the 12th leading cause of death in the United States overall—yet it is the 2nd leading cause of death among individuals between the ages of 10-14 and 24-34 and the 3rd leading cause of death for Americans 15-24 years old, per the NIMH. The CDC reports that suicide rates rose 30% between 2000 and 2020.
Trauma and Addiction
The psychological impact of a traumatic event or experience can lead to post-traumatic stress disorder (PTSD). Symptoms of PTSD include flashbacks, unwanted memories, nightmares and panic attacks. Although the disorder is often associated with war veterans, a wide variety of traumatic experiences can lead to PTSD, like assault, abuse, serious accidents and loss.
Addiction is another mental health concern that has been on the rise in recent years, with drug overdose deaths having rapidly increased since the 1990s according to the CDC. Alcohol is the most abused substance, with 5.3% of deaths worldwide attributed to alcohol consumption, according to the National Institute on Alcohol Abuse and Alcoholism. Addiction is a complex disease that many are only able to overcome with professional help.

Other Disorders
Psychotic disorders are among the most stigmatized in our society, which only serves to further alienate people living with psychosis and seeking treatment, according to the National Alliance on Mental Illness (NAMI). Psychosis is defined as a disconnect from reality by way of auditory/visual hallucinations, disorganized thinking or delusions. Some psychotic disorders include schizophrenia and schizoaffective disorder . Despite misconceptions regarding psychosis and violence, the World Psychiatry Journal notes that experiencers of psychosis are far more likely to be victims of violence than perpetrators.
Other common psychiatric disorders include Obsessive Compulsive Disorder (OCD), eating disorders like anorexia and bulimia, personality disorders like borderline personality disorder, and mood disorders like bipolar disorder . Each mental health disorder has its own set of challenges—and its own set of treatments.
What Are Warning Signs and Risk Factors of Mental Illness?
Some mental illnesses may be hereditary, while others are developed. Dempster notes a variety of warning signs that signal mental health issues as well as additional risk factors that can lead to mental health problems.
Some warning signs of mental illness are:
- Appetite changes
- Disruption of sleep
- Engaging in risky behaviors (self-harm, sexual acting out, disordered eating or other compulsive behaviors)
- Mental distress (worrisome thoughts, tension, insecurity)
- Negative impacts on relationships (isolating, arguing, etc.)
- Substance abuse
- Suicidal thoughts
Other risk factors of mental illness include:
- Adverse childhood experiences
- Past or present trauma
- Present or past experiences of being abused or assaulted
- Sudden loss
If you are experiencing warning signs of mental illness, consider reaching out to a professional for help. If someone you know is struggling with any of these symptoms, Dempster recommends the “QPR” approach.
“A great way to help a loved one into care is to remember the acronym QPR, which stands for Question, Persuade, Refer,” Dempster said. “ Question : Directly ask the individual you are concerned about how they are doing, sharing your care and concern. Persuade: Talk to the person about the benefits of seeking out care with a mental health professional who can provide support and resources to address overwhelming thoughts and feelings. Refer: Support the individual in seeking out care by helping them to find available care, helping them to make an appointment or even taking them to the appointment.”
What Mental Health Treatments and Resources Are Available?
A variety of treatment options exist for different mental health issues. “There are times that some mental health problems can be treated by increasing self-care, accessing one’s support system and by careful problem-solving and communication,” Dempster said. “However, there are other times that professional mental health care, including therapy, medication or some other form of treatment offered by a professional can help to address mental health problems much more expediently through evidence-based methods.”
Many patients visit multiple mental health providers–for example, seeing a psychiatrist regarding medications and a therapist for more frequent counseling sessions. Consult the Mayo Clinic’s guide to finding a mental health provider , and reach out to your health insurance provider to find mental health services near you. You can also use Psychology Today’s expansive directory to help locate a provider in your area, and Findtreatment.gov offers a substance abuse treatment locator tool. For serious mental health concerns, The National Substance Abuse and Mental Health Services Administration (SAMHSA) has an early serious mental health treatment locator tool to find treatment centers in the United States.
“Historically, there has been a stigma with seeking mental health care that is not evident in seeking care for physical problems, and this stigma prolonged the suffering of many needlessly and has even cost lives,” Dempster said. “Seeking out care for mental health concerns is a sign of strength and there is robust evidence that demonstrates that mental health care is effective.”
If you or someone you know needs help now, consult these resources or contact a professional mental health provider. In the event of an emergency, please call 911.
- 988 Suicide and Crisis Lifeline : 988
- Substance Abuse and Mental Health Services Administration : 1-800-662-HELP (4357)
- National Action Alliance for Suicide Prevention
- Veterans Crisis Line
- National Strategy for Suicide Prevention
Mars Girolimon '21 is a writer and student at Southern New Hampshire University, pursuing a master's in English and creative writing. Connect with them on LinkedIn .
Explore more content like this article

Is a Bachelor's Degree Worth It?

Is a Master’s Degree Worth It?

Is an Associate Degree Worth It?
About southern new hampshire university.

SNHU is a nonprofit, accredited university with a mission to make high-quality education more accessible and affordable for everyone.
Founded in 1932, and online since 1995, we’ve helped countless students reach their goals with flexible, career-focused programs . Our 300-acre campus in Manchester, NH is home to over 3,000 students, and we serve over 135,000 students online. Visit our about SNHU page to learn more about our mission, accreditations, leadership team, national recognitions and awards.

- Mission and Vision
- Scientific Advancement Plan
- Science Visioning
- Research Framework
- Minority Health and Health Disparities Definitions
- Organizational Structure
- Staff Directory
- About the Director
- Director’s Messages
- News Mentions
- Presentations
- Selected Publications
- Director's Laboratory
- Congressional Justification
- Congressional Testimony
- Legislative History
- NIH Minority Health and Health Disparities Strategic Plan 2021-2025
- Minority Health and Health Disparities: Definitions and Parameters
- NIH and HHS Commitment
- Foundation for Planning
- Structure of This Plan
- Strategic Plan Categories
- Summary of Categories and Goals
- Scientific Goals, Research Strategies, and Priority Areas
- Research-Sustaining Activities: Goals, Strategies, and Priority Areas
- Outreach, Collaboration, and Dissemination: Goals and Strategies
- Leap Forward Research Challenge
- Future Plans
- Research Interest Areas
- Research Centers
- Research Endowment
- Community Based Participatory Research Program (CBPR)
- SBIR/STTR: Small Business Innovation/Tech Transfer
- Solicited and Investigator-Initiated Research Project Grants
- Scientific Conferences
- Training and Career Development
- Loan Repayment Program (LRP)
- Data Management and Sharing
- Social and Behavioral Sciences
- Population and Community Health Sciences
- Epidemiology and Genetics
- Medical Research Scholars Program (MRSP)
- Coleman Research Innovation Award
- Health Disparities Interest Group
- Art Challenge
- Breathe Better Network
- Healthy Hearts Network
- DEBUT Challenge
- Healthy Mind Initiative
- Mental Health Essay Contest
- Science Day for Students at NIH
- Fuel Up to Play 60 en Español
- Brother, You're on My Mind
- Celebrating National Minority Health Month
- Reaching People in Multiple Languages
- Funding Strategy
- Active Funding Opportunities
- Expired Funding Opportunities
- Technical Assistance Webinars

- Community Health and Population Sciences
- Clinical and Health Services Research
- Integrative Biological and Behavioral Sciences
- Intramural Research Program
- Training and Diverse Workforce Development
- Inside NIMHD
- ScHARe HDPulse PhenX SDOH Toolkit Understanding Health Disparities For Research Applicants For Research Grantees Research and Training Programs Reports and Data Resources Health Information for the Public Science Education

- NIMHD Programs
- NIMHD Education and Outreach
- NIH Teen Mental Health Essay Contest
- Extramural Research
- Intramural Research
- NIMHD Collaborations
- Fuel Up to Play 60 en Espanol
- COVID-19 Information and Resources
Speaking Up About Mental Health
National essay contest.
SUBMIT YOUR ESSAY The contest is open to high school students ages 16-18
PROMOTION TOOLKIT Help spread the word with social media and email tools
December 1, 2023
Dec. 1, 2023
January 16, 2024
Jan. 16, 2024
May 31, 2024
Mental health is an important part of overall health across all life stages. However, far too often, symptoms are not addressed or recognized among teens.
Speaking Up About Mental Health is an essay contest that challenges high school students ages 16-18 to raise awareness of mental health. The contest gives students a platform to share ways to eliminate and/or reduce mental health stigma faced by young people, especially in diverse communities.
This contest is soliciting essays that:
- Discuss ways to eliminate and/or reduce mental health stigma faced by young people, especially in diverse communities
- Share resilience and coping strategies to overcome mental health issues such as social isolation and loneliness, depression, and anxiety
- Address mental health stigma
- Encourage conversations about mental health, social media, and/or technology
- Suggest school policies or practices that could help reduce stigma
- Describe barriers to mental health treatment
- Cover other areas of concern to individuals and their communities with respect to mental health
Get details on contest rules and submit your entry on Challenge.gov
Promotion toolkit : Help promote the Speaking Up About Mental Health essay contest
The contest is led by:
National Institute of Mental Health
National Institute on Minority Health and Health Disparities
Eunice Kennedy Shriver National Institute of Child Health and Human Development
Page updated Jan. 23, 2024
September 2022: NIH Announces Winners of High School Mental Health Essay Contest
2022 Essay Awardees
2019 Essay Awardees

Staying Connected
- Funding Opportunities
- News & Events
- HHS Vulnerability Disclosure
- Privacy/Disclaimer/Accessibility Policy
- Viewers & Players
Safeguarding the Mental Health of Teachers
- Posted December 3, 2019
- By Emily Boudreau

Teachers tell their students that mindset matters. Yet teachers do not always allow themselves space to receive those same messages of reflection and self-care.
Henry Seton , a longtime high school teacher and department head, learned that firsthand. In a courageous and insightful essay in Educational Leadership , Seton explored the hurdles that teachers face — especially those who work in schools in high-poverty settings — in safeguarding their mental health. He also revealed the challenges he’d faced in his own life.
“Teachers are attuned to the social-emotional wellbeing of our students and trained to monitor for signs such as trauma, anxiety, bullying, or microaggressions,” he wrote. “Yet we are still just learning how to discuss a huge, lurking threat to our work: our own mental health.”
Usable Knowledge sat down with Seton, who earned his master's degree at the Harvard Graduate School of Education last May, to talk about the ways in which school communities can both hinder and support the wellbeing of their members.
Where do you think the silence around teacher mental health originates from?
I think so many educators, especially in high-poverty settings, are barely holding on as is. To acknowledge, head on, where we are in terms of our mental health might not be something we feel like we can bear. High-poverty schools also often attract a certain type of intensity junkie who loves the intensity of that work — a person who, previously, has always been able to get through it. Talking about issues of mental health can be seen as a weakness and there’s this mentality of “I just need to be tougher. I just need to work harder and work smarter.”
How have you seen that mindset translate into a school culture? Did you feel equipped, at an early stage in your career, to handle it?
I worked for a decade at a young charter school that, like many young start-up organizations, had a blurring of work-life boundaries. It was predominately young people in their twenties, and we were all super mission-oriented, very energetic, very committed. I think we came into the work with a lot of unprocessed insecurities, whether it was our desire to be a savior or issues of our own guilt, that we were never doing enough. Just like open offices today, you see who gets there earliest, you see who stays there latest.
And there’s always this feeling that you could be doing more. Instead of the neighbor’s grass being greener, it’s the classroom next door that’s always operating at a higher level than yours. We all loved each other and worked hard to support each other but intimidated each other to death. It drove us to wonderful growth and phenomenal outcomes for students. Also, at times, it burnt through our emotional resilience and destabilized our emotional constancy with one another and with students. It affected our mental health. As the school transitioned, it did learn how to support teachers over time, but that transition is difficult for all sorts of schools and organizations.
"It’s not uncommon to have school leaders who sometimes sleep in their offices because they’re so busy, who don’t take a single break during the day. ... They often model, I think unintentionally, that we can’t take breaks, we can’t ease up, we need to always be going full throttle."
How do schools perpetuate the silence around teacher wellbeing — and how might schools break that silence?
It’s not uncommon to have school leaders who sometimes sleep in their offices because they’re so busy, who don’t take a single break during the day. I want to name school leaders, in particular, as people who can steer the conversation. They often model, I think unintentionally, that we can’t take breaks, we can’t ease up, we need to always be going full throttle. That trickles down in organizations to the point where we feel we can’t attend to ourselves.
What do you see as the first step toward making teaching more sustainable?
Technology makes it so easy to stay connected with the work, but this can also make it hard to find balance. If we could double the amount of time teachers stay in high-poverty settings, we would change the education sector so much. In order to stay in this game — which is something I want to do for my whole life — teachers need to have boundaries. Veteran teachers, in order to survive, inevitably learn how to erect boundaries. But young teachers in younger schools don’t always have the model of boundary setting. There are not as many older teacher colleagues with children who, by necessity, set stricter boundaries.
You mentioned school leaders as being a group that had a lot of influence over how issues around teacher mental health and wellbeing are talked about in a school community. What else might leaders do?
I believe the number one step is leaders talking about these issues more vulnerably. I was really impressed by Eva Moskowitz of Success Academy Charter Schools. She has a reputation for being very hard-driving in terms of how she leads her organization, but she spoke in her memoir about the importance of therapists for teachers to be able to process this work, which I thought was phenomenal. It’s just so rare in the high-performing charter space and high-poverty settings that school leaders talk about seeing therapists or the importance of mindfulness practices, let alone practice vulnerability in front of their staff. And I think that’s so critical because it gives everybody else that permission to discuss this…. Leaders need to regularly gather input around the stress points for teachers and respond to it. Healthcare plans for teachers should allow access to free or minimal copay mental health services. And there needs to be a space for teachers to process the intensity of their work.
"The most important thing we can do for each other is just to listen. If we have the bandwidth and time to just stop and listen to a colleague, that’s just such an important first step towards healing and wholeness."
How could that space be created?
The most important thing we can do for each other is just to listen. If we have the bandwidth and time to just stop and listen to a colleague, that’s just such an important first step towards healing and wholeness. Listening dyads are connected to the Buddhist tradition. You just listen and you don’t need to say anything or even respond. Then, if colleagues are open to it, you can talk towards some action steps.
Where might people begin to find resources, supports, and answers to questions?
I see more colleagues starting to talk about issues related to mental health. I feel like terms like mindfulness, vulnerability, and self-compassion are coming up more in teacher spaces. The number one place I’d start is Elena Aguilar’s work on cultivating resilience in educators. It is the best introduction to a myriad of practices that support teacher mental health — everything from mindfulness, to compassion, gratitude. Authors like Brene Brown have appeared in TED Talks that have helped bring attention to it. But I think there’s still more we can do — we’re still not discussing it enough.
Additional Resources:
- A recent Harvard EdCast explores why teachers leave the profession and how leaders can better provide support
- Harvard Ed. Magazine offers tips for early childhood educators to practice mindfulness and destress
- A guide to helping first-year teachers cultivate resilience

Usable Knowledge
Connecting education research to practice — with timely insights for educators, families, and communities
Related Articles

Hanging by a Thread?

Why Rest is Best
And why it’s an act of justice

A Space for Joy
Educators talk about the impact COVID has had on school happiness
Mental Health Matters: Strategies for Managing Anxiety and Feeling Happier
Published may 24, 2023, courses mentioned in this post: building personal resilience: managing anxiety and mental health and the path to happiness: what chinese philosophy teaches us about the good life.
Has the COVID-19 pandemic affected rising rates of anxiety globally? Can we actually help ourselves feel happier? Is it possible to support others who are experiencing symptoms of anxiety and other mental health challenges?

Harvard leaders Dr. Luana Marques and Professor Michael Puett gathered with moderator Anna Bartuska to answer these questions and more in our latest webinar, Mental Health Matters: Strategies for Managing Anxiety and Feeling Happier.
In this 60-minute webinar, Dr. Marques and Professor Puett shared their personal experience with anxiety, discussed trending topics in mental health, answered participant questions, and gave advice on how to manage anxiety and feel happier by implementing science- and philosophy-driven solutions into your daily life.
Puett says, “We’ve gone through a pandemic, we have been living in the world of social media for the last 15 years, and we are facing a difficult structural future with issues like climate change, rising inequality, and lack of social mobility. All of this is playing into the rise of anxiety. But of course, while most of these challenges are new, people have been wrestling with issues of anxiety for thousands of years.”
Marques notes, “Anxiety itself is not the problem, it’s what we do when we are anxious that is the problem.”
Dr. Marques is the author of Bold Move , course faculty for Building Personal Resilience , Associate Professor of Psychiatry at Harvard Medical School, Founder and Director of Community Psychiatry PRIDE at Massachusetts General Hospital , and former President of the Anxiety and Depression Association of America .
Professor Puett is the Walter C. Klein Professor of Chinese History and Anthropology at Harvard University. His interests are focused on the inter-relations between history, anthropology, religion, and philosophy, with the hope of bringing the study of China into larger historical and comparative frameworks. He is the author of The Path: A New Way to Think About Everything , The Ambivalence of Creation: Debates Concerning Innovation and Artifice in Early China, and To Become a God: Cosmology, Sacrifice, and Self-Divinization in Early China, as well as the course faculty for Harvard Online’s course The Path to Happiness .
Moderator Anna Bartuska is a doctoral student at the University of Oregon and former coordinator at PRIDE at Massachusetts General Hospital .
“Imagine a world where people would spend as much time training their brain as they do their physical body,” notes Marques.
“You can start training your brain to break patterns by going back to the mundane level of your life. When you’re walking down the street on a daily basis, start training your brain to notice everything that is going on around you,” shares Puett.
“There is magic in the mundane,” agrees Marques.
For more discussion and strategies on managing anxiety and feeling happier, view the full webinar:
To continue learning about managing anxiety and building resilience from Dr. Luana Marques, register for her course Building Personal Resilience: Managing Anxiety and Mental Health .
To continue learning about how to experience more happiness, register for Professor Michael Puett’s online course The Path to Happiness: What Chinese Philosophy Teaches us about the Good Life .
Disclaimer: The content provided in this webinar is intended for informational purposes only, and should not be considered as medical advice. The content is not, and should not, be relied upon as medical advice, and should not be used to make a clinical diagnosis, to provide treatment, or to replace or overrule a licensed health care provider's judgment.
Related Blog Posts
Is remote work the key to increasing open innovation.
Creating collaborative global teams has never been more essential. Harvard Business School Professors discuss how to bring the outside world into your organization.
New Course Announcement: Building Personal Resilience: Managing Anxiety and Mental Health
Join Harvard Medical School faculty Dr. Luana Marques to use five science-driven skills to build resilience.
Explore Your Interests, Find Your Courses
From health care and digital transformation to climate change and racial justice, our current course offerings, and those in development, are centered around the key questions of today.

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Science News
- Meetings and Events
- Social Media
- Press Resources
- Email Updates
- Innovation Speaker Series
High School Students Invited to Reflect on Mental Health Stigma in National Essay Contest
December 4, 2023 • Institute Update
Mental health is an essential aspect of overall well-being, and it is important for people of all ages, including teenagers. Unfortunately, there's still significant stigma surrounding mental health care, and many teens hesitate to seek help due to fear, shame, or misconceptions.
To encourage teens to be a part of the solution, the National Institutes of Health invites students ages 16 to 18 years old to participate in the “ Speaking Up About Mental Health ” essay contest. This contest gives teens the opportunity to make their voices heard and explore ways to reduce mental health stigma that young people may face when seeking mental health treatment.
The topic is meant to be broad, but ideas for essay topics could include:
- The impact of mental health stigma on teens
- The media's role in perpetuating or addressing mental health stigma
- The role of family and friends in reducing mental health stigma
- Cultural barriers to mental health care
- School policies or practices that could help reduce stigma
The contest, supported by the National Institute of Mental Health (NIMH), the National Institute on Minority Health and Health Disparities (NIMHD), and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), will award a total of $15,000 in cash prizes to multiple winners.
Through these short essays, teens can shed light on the mental health challenges they or their peers face. They can also share innovative ideas and insights for reducing stigma and helping teens seek mental health support without judgment or fear.
Important dates
Contest opens : December 1, 2023
Submission deadline : January 16, 2024
Winners announced : May 31, 2024
Additional information
There is no application fee to participate. Entries must be submitted on Challenge.gov .
For more information on the rules of the contest and registration requirements, see the contest webpage at www.challenge.gov or contact [email protected] .
- CalMatters annual reader survey
- Help us better serve our readers for a chance to win a $100 Amazon gift card.
- California, explained
- We’re a big state with big challenges. Each morning we explain the top issues and how Californians are trying to solve them.
- We’re a big state with big challenges. Each morning we explain the top issues.
By signing up, you agree to the terms .
- Newsletters
- Environment
- 2024 Voter Guide
- Legislator Tracker
- Daily Newsletter
- Data & Trackers
- California Divide
- CalMatters for Learning
- College Journalism Network
- What’s Working
- Youth Journalism
- Manage donation
- News and Awards
- Sponsorship
- Inside the Newsroom
- CalMatters en Español
Newsom’s ‘new strategy’ would force some homeless, mentally ill Californians into treatment

Share this:
- Click to share on X (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on WhatsApp (Opens in new window)

The governor’s new proposal would require all 58 counties to participate in the program to assist people with serious mental illnesses and substance use disorders.
Lea este artículo en español .
Gov. Gavin Newsom today unveiled a much anticipated proposal to address a mental health crisis increasingly visible on trash-strewn sidewalks and in cramped jail cells around California.
The proposal, known as the Community Assistance, Recovery and Empowerment (or CARE) Court , would provide a framework for courts to compel people with serious mental illnesses and substance use disorders into treatment, while also providing participants with supportive housing and wrap-around services.
“This is a completely new strategy,” Newsom said at a press conference today to introduce the new plan. “And I hope that creates a space for a different conversation than we’ve had in the past.”
All 58 counties would be required to participate in the program, which is currently just a policy framework and still needs to be approved by the Legislature. Counties could face penalties for failing to provide requisite services, administration officials said.
“This is a completely new strategy. And I hope that creates a space for a different conversation than we’ve had in the past.” Gov. Gavin Newsom
That’s one of several details that differentiates this proposal from Laura’s Law, which also entails court-ordered treatment but allows counties to decide whether they want to participate. Newsom noted that, in one year, only 218 people were served by Laura’s Law. The Newsom administration estimates that the CARE Court program could serve between 7,000 and 12,000 Californians.
Administration officials say the new proposal is different, in part, because of the resources it comes with. It builds on a $12 billion allocation to address homelessness last year, as well as another $2 billion proposed this year, they said.
People could come into the program through short-term involuntary hospital stays (also known as “5150s”), through the criminal justice system or at the recommendation of family members, mental health providers or first responders, among others. They would not need to be homeless to participate.
The court would order a tailored plan involving some combination of housing, medication and services, and would offer the support of a full clinical team, as well as a public defender and a “supporter” who could help a participant make care decisions and prepare advanced mental health directives.
Unlike with conservatorships, which can be indefinite, participation would be time limited – one year, with the possibility of an additional one-year extension.
A stream of state and local leaders spoke to the urgency of the need at the news conference, held on the San Jose campus of Momentum for Health, a behavioral health treatment organization.
Santa Clara County Superior Court Judge Stephen Manley, a widely regarded trailblazer who has presided over that county’s mental health court for decades, told those gathered: “We need to stop trying to fix a failed system that is rapidly, in my view, from what I see every day, moving us back to where we were 100 years ago when the answer for the mentally ill was simply to incarcerate them, put them in the hospital and keep them there until they die.”
Oakland Mayor Libby Schaaf, whose city has seen a dramatic burgeoning of encampments in its parks, vacant lots and underpasses, described joining the city’s homeless count on a recent freezing morning. She lost her composure as she shooed a rat off of a sleeping woman, she said. She later learned that the woman had spent three years living in that same spot, feeding rats because they were her “chosen company” and refusing services.
“She had been offered care, shelter, housing countless times but had been left to freeze on the pavement of our city,” Schaaf said.
“It’s time that our Golden State stops walking by our greatest moral shame and faces it head-on with clarity and compassion,” she said.
“It’s time that our Golden State stops walking by our greatest moral shame and faces it head-on with clarity and compassion.” Oakland Mayor Libby Schaaf
With the new proposal, state leaders are trying to forge a new path beyond the decades-long stalemate surrounding involuntary treatment of the most seriously mentaly ill.
Dr. Mark Ghaly, the secretary of Health and Human Services, described the need to move beyond “old and broken models.” The Lanterman-Petris-Short Act, which established the standards for involuntary treatment for people with disabilities, passed in 1967, more than half a century ago. In recent years, much of the debate about how to serve people with serious mental illness has centered on whether or not to change that law. Bills moving through the Legislature are still grappling with that question.
Newsom took care to emphasize his interest in working with disability rights groups on the new proposal.
Kevin Baker, director of governmental relations for ACLU California Action, said in an email to CalMatters that his organization is “keeping an open mind” while waiting to see more details, though noting that “there are a million questions and a million things that could go wrong.”
“The problem of homelessness is caused by the cost of housing, and we won’t solve homelessness, mental health or substance abuse problems in our communities by locking people up and drugging them against their will,” he said. “New funding for housing and services would be good, if we also keep in mind that people don’t lose their civil liberties just because the government wants to help them, no matter how sincerely.”
He added that he thought the proposal is a significant and complex change in the law that should be heard by legislative committees and “not quietly slipped into a budget trailer bill as I hear may be the plan.”
County behavioral health departments would shoulder significant responsibility for implementing the new plan. Michelle Doty Cabrera, executive director of the California Behavioral Health Directors Association, told CalMatters that her members are all too aware of the “runaway train of need” for mental health services. While celebrating Newsom’s commitment to bring in more funding for housing, she said she worried that the administration was not planning to allocate enough resources for increased services.
“There’s no way you can squeeze blood from a turnip,” she said. “We’re at our limit in terms of what we can do. We need more resources to do more.”
The California State Association of Public Administrators, Public Guardians, and Public Conservators echoed this sentiment in a similar statement, saying they needed more resources to meet the “significant impacts” the program would undoubtedly have on demand for their services.
“The governor has thrown down the gauntlet and said we’re going to change things in a big way.” Randall Hagar, legislative advocate and policy consultant for the Psychiatric Physicians Alliance of California
Randall Hagar, legislative advocate and policy consultant for the Psychiatric Physicians Alliance of California, called the new proposal “really welcome.
“The governor has thrown down the gauntlet and said we’re going to change things in a big way,” he said. “It’s one of the first new ideas I’ve heard in a long time.”
We want to hear from you
Help us better serve our readers by taking the 2024 Annual Reader Survey. Take the survey
Jocelyn Wiener Health Reporter
Jocelyn Wiener writes about health and mental health for CalMatters, exploring the intersection between government policies and people’s lives. She has worked as a reporter in her native California for... More by Jocelyn Wiener
We've recently sent you an authentication link. Please, check your inbox!
Sign in with a password below, or sign in using your email .
Get a code sent to your email to sign in, or sign in using a password .
Enter the code you received via email to sign in, or sign in using a password .
Subscribe to our newsletters:
- WeeklyMatters Catch up on the top stories in California with a summary of our reporting and commentary from the past week.
- Weekly Walters Get a digest of new insights from veteran journalist Dan Walters, who holds powerful people in California accountable.
- WhatMatters Start your day with a comprehensive rundown of the most important stories in California politics and policy.
- Inequality Insights Your weekly must-read to stay on top of inequality, one of California’s most pressing issues.
Sign in with your email
Lost your password?
Try a different email
Send another code
Sign in with a password

"Mental Health Matters" Isn't Enough
It's not just what's in your head that shapes your wellbeing..
Posted October 11, 2022 | Reviewed by Ekua Hagan
- Individual health is not solely determined by biological or behavioral factors within one’s control but also by a layer of interacting systems.
- Certain social, societal, and natural environments can be either more or less conducive to mental health.
- Mental health is physical health and vice versa. It is not simply a cluster of unwanted feelings or self-deprecating thoughts.
Yesterday was World Mental Health Day. Businesses globally touted the importance of how much “mental health matters.” While awareness of mental health as an influential factor in health more broadly is a necessary step toward eliminating the stigma which accompanies help-seeking behaviors, there seems to be little acknowledgment of how contextually embedded mental health actually is.
The social-ecological model of health
The social-ecological model of health is one model proposed over three decades ago by public health scientists. It has increasingly received more attention , particularly in the context of the COVID-19 pandemic and societal injustices which continue to be perpetuated around the globe, such as the recent death of Mahsa Amini in Iran or police brutality against Black Americans like George Floyd in the United States.
According to this model, individual health is not solely determined by biological or behavioral factors within one’s control but is also influenced by a delicate collection of interacting systems at various levels including interpersonal, institutional, community, and public policy which can be a source of stress or resilience .
What this means, in effect, is that individual lifestyle factors such as health behaviors, exercise, cognitive load, mindset, and spirituality which are ripe for intervention are but one layer of a complex web resulting in a person’s mental health status. Older or younger age, lack of education , and genetics are individual determinants of health that can also be acted upon to improve one’s mental health, such as through providing health education tools to communities at higher risk of developing mental or physical health problems. Beyond individual lifestyle and intrapersonal factors are the social, societal, and natural environments that are either more or less conducive to mental health.
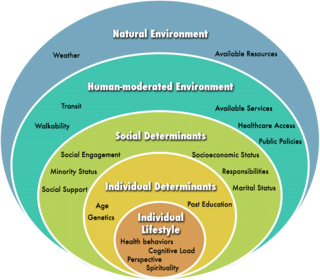
For instance, people who identify as part of minority status in the U.S. (e.g. usually those who do not fit the mold of a heterosexual, White, cisgender, middle-class, or above male) may struggle more with their mental health due to lack of social support, social engagement, socioeconomic status, increased responsibilities, marital status, and more. Those who live in food deserts, who are unemployed, have limited healthcare access, lack transit options, and have limited public spaces with safe walkability are also at risk for mental health challenges simply due to the nature of their human-moderated environment. Lastly, the natural environment is a factor in mental health too, which includes pieces of the puzzle like natural disasters which befall a specific geographic region, epidemics, pandemics, and naturally-available resources like fresh water access.
All of that is to say, mental health is more than just what’s in your head. It’s shaped by your personal history, your finances, your chosen behaviors, the people you surround yourself with, your community, your geographic region, and global events. Many of these layers go beyond what's in one's control and in fact, are out of the person's control and require systemic changes and overhauls to ameliorate. Mental health is physical health and vice versa. It is not simply a cluster of unwanted feelings or self-deprecating thoughts.
Though all of these additional layers contributing to mental health may appear bleak, by acknowledging the real challenges which exist, communities may be uplifted and empowered. Accurate awareness, though uncomfortable at times, is one step closer to problem-solving and creating generalizable interventions that can not only withstand socio-ecological challenges but reshape the landscape of these environments to create a more proactive and equitable health environment for all.
McLeroy, K.R., Bibeau, D., Steckler, A., & Glanz, K. (1988) An ecological perspective on health promotion programs. Health Education. 15:351–77.

Sarah-Nicole Bostan, Ph.D., B.C.B., is a clinical health psychologist, researcher, and digital health technology advisor.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
- Health Care
The Menstrual Mood Disorder You’ve Never Heard About

E ver since she was a teenager, Tanya knew her mood swings were a problem. She had periodic bouts of anger and depression that left her wanting to die. Her life was a roller coaster of highs and lows but doctors couldn’t figure out what was wrong. Five years ago, she decided she’d had enough. She wanted to end her life.
Tanya managed to talk herself out of it and instead did some googling. She stumbled across a website about premenstrual dysphoric disorder (PMDD), a menstrual mood disorder, that impacts roughly 3 to 8% of menstruators. PMDD means having severe and debilitating mood swings right around one’s period. Around a third of people with PMDD have attempted suicide, and over 70% have regular suicidal ideation .
“It just hit me,” Tanya told me. “I went through my life and so many moments made sense.” She called her doctor the next day. He sent her to get tested for diabetes.
Tanya finally managed to get a PMDD diagnosis in 2019 at the age of 26, but she was haunted by the question: Why had she never heard of PMDD before and why was it so hard to get a diagnosis?
Although research shows suicidal ideation is linked to specific times during the menstrual cycle, today most people still haven’t heard of PMDD, including doctors. According to a 2022 survey of PMDD patients, over a third said their general practitioners had no knowledge of premenstrual disorders, and about 40% said their mental-health-care providers had no knowledge of premenstrual disorders. But PMDD has been around since periods have been around and we’ve known about it for nearly a century.
So why aren’t we getting people the help they need? The answer, as history shows, is more complicated than we think.
While the menstrual cycle has been notoriously understudied, the first papers on PMDD appeared in 1930s. In the 1950s British physician Dr. Katrina Dalton began studying PMDD —or “premenstrual syndrome” as she called it, and opened a clinic in London . Still, PMDD mostly flew under the radar until 1980, when Dalton served as a medical expert for three women accused of crime. During the trials Dalton showed that the women committed the crimes right before their period, and that their symptoms disappeared with treatment. She was able to get them a reduced sentence.
Overnight there was a media boom around PMS. The magazine Glamour even polled readers about the validity of using PMS as a legal defense: (24% were for, 71% against, and 5% unsure). As a result, the growing awareness around PMS bled over to the medical community. In 1984 psychiatrist Robert Spitzer proposed PMS should be added to the Diagnostic and Statistical Manual of Mental Disorders (DSM), the handbook used by doctors to diagnosis mental health problems. Spitzer was the chair of the committee revising the third version of the DSM, and he’d been getting several invites to conferences about PMS. Adding PMS to the DSM meant that the medical community was recognizing it as a formal disorder that could be diagnosed and treated.
Read More: 5 Foods That Ease PMS Symptoms
However, experts were divided on where to draw the line between PMDD (the severe, debilitating mood swings) and PMS (garden variety grumpiness and irritability). When the Washington Post asked experts about the prevalence of PMS in 1984, estimates ranged from 3% to 90% of women . In a sense, both of these estimates were true: only a few people have severe symptoms, but up to 90% of people do have mild symptoms before their period. It became clear that experts were conflating PMDD and PMS and this was reflected in popular culture. Suddenly, anyone who had a period was seen as unstable. Products with sexist jokes abounded, such as greeting cards that read “What’s the difference between a woman with PMS and a terrorist? Answer: You can negotiate with a terrorist.”
Controversy erupted. A group of feminists spearheaded a campaign to stop PMDD’s inclusion in the DSM. They argued that including PMDD would be tantamount to calling menstruation a mental illness. Much of their reaction was rooted in the atmosphere of the ‘70s and ‘80s as women were fighting for gender equality on several fronts from work to reproductive rights. In the 1970s, for the first time, over half of women were working outside the home. The Supreme Court ruled to protect the right to abortion in Roe v. Wade. However, this equality was also precarious and under threat—conservatives defeated the Equal Rights Amendment which would have prohibited gender discrimination. For feminists, PMDD and the sexist jokes it generated seemed to be another attempt to discredit women and chip away at the progress feminists had made for women’s rights.
One of PMDD’s major critics, Dr. Joan Chrisler, attended a lecture in the 1970s, early on in her career on why there were no great women artists or novelists. The conclusion: women’s creativity declines when they are menstruating. This inspired Chrisler to devote her career to fighting menstrual stigma. In an era rife with sexism, adding PMDD to the DSM set off alarm bells.
Read More: A History of How Employers Have Addressed Women’s Periods
To further complicate matters, in the early 2000s, drug manufacturer Eli Lilly stuck its finger in the pie. Eli Lilly’s patent on its blockbuster drug Prozac, which treated depression, was set to expire and it’s share prices had tanked. The company desperately needed a new market that would buy Prozac.
Eli Lilly landed on PMDD as their next likely market. Early studies already suggested that Prozac could treat PMDD, but the problem was that experts were still debating whether PMDD belonged in the DSM as an official diagnosis at all. Undaunted, Eli Lilly embarked on a massive campaign to market Prozac to people with PMDD. It sponsored a round table discussion on Prozac’s effectiveness for PMDD, which found that at least 60% of patients with PMDD respond to antidepressants. It repackaged Prozac as “Serafem” a play on the word “seraphim”, the angels who guard the throne of God. If that wasn’t enough to drive home the point, they changed Prozac’s green and yellow pills to pink and purple. Finally, they rolled out a series of ads that suggested any woman who was feeling grumpy should consider medication. The ads didn’t distinguish between PMDD and PMS. Rather, they imply any sign of irritability in women should be treated.
This unleashed another wave of furor. Feminists were insulted—and rightfully so. The last thing the women’s movement needed was a drug companies suggesting a woman’s anger is a mental health condition. The media had a field day writing about drug companies “inventing” new diseases and marketing drugs without diagnoses. (Tragically, Prozac actually works on PMDD. Studies have found SSRIs like Prozac can relieve PMDD symptoms in up to twelve hours, even though it takes weeks to work for anxiety and depression.)
In some ways the feminists lost their battle. PMDD eventually did become a diagnosis in the DSM in 2013, nearly three decades after it’d been first debated in the ‘80s. In other ways, they won the war. Dr. Tory Eisenlohr-Moul, a premenstrual mood disorder researcher at the University of Illinois Chicago, estimates that the backlash around PMDD set care back by 10 to 15 years. She pointed out there’s been a chilling effect on the conversation around the link between menstruation and mood. Doctors are afraid to bring it up, because they don’t want patients to think they are sexist.
Yet, in reality, the biggest victims of the fight over PMDD’s existence are people who have PMDD and the people who love them. Today, thousands of people still suffer because they don’t know they have PMDD.
Tanya’s PMDD diagnosis changed her life. While she elected not to try medication, the diagnosis alone helped her understand her breakdowns, and helped her explain what was going on to family and friends. She decided to train in psychotherapy so she can help other people understand PMDD. “My tutor has been a counselor for 10 years and still hasn’t heard of PMDD,” she said. “I want to help people work through this pain.”
More Must-Reads From TIME
- Jane Fonda Champions Climate Action for Every Generation
- Passengers Are Flying up to 30 Hours to See Four Minutes of the Eclipse
- Biden’s Campaign Is In Trouble. Will the Turnaround Plan Work?
- Essay: The Complicated Dread of Early Spring
- Why Walking Isn’t Enough When It Comes to Exercise
- The Financial Influencers Women Actually Want to Listen To
- The Best TV Shows to Watch on Peacock
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
You May Also Like
I deleted my email app. My mental health, free time, and productivity skyrocketed.
- I've deleted social media apps from my phone, but was still hooked to my email app.
- Deleting it freed up time in my day for more meaningful things.
- Checking my email less actually helped me to stay on top of my emails.

Deleting apps for the sake of my mental health and productivity is nothing new for me. Instagram and TikTok don't live on my phone; they're merely temporary tenants I let stop by on weekends. But as a self-employed writer, there's one app that's haunted me far more than social media: my email app.
Unlike social media, my email is inherently tied to my work. Where TikTok shows me trending dances, my inbox shows me all the people I've yet to respond to. Not to mention, email itself is work. I can dip into social media as I dip my hands into a rushing stream — delighting in the cool waters of a distracting video, then dip back out. With email, I am Sisyphus, desperately trying to scoop the whole stream into little buckets all day while the gods laugh at their sick joke — the stream never stops rushing.
It wasn't until I attended a small business workshop a few months ago that I latched onto a radical idea for curbing my email addiction . Toward the end of the workshop, the host offhandedly mentioned she hadn't had email on her phone since 2020. It had never occurred to me: you could just... delete your email app?
Staying on top of my email had become synonymous with staying on top of my work . But I had to know: what would happen if I ditched my email app and only checked my inbox on my computer a few times a day?
It immediately freed up my time for more meaningful work
From the first day, it became clear just how much time I wasted trying to stay on top of my inbox . Instead of focusing on my to-do list for the day, all too often I'd get sucked into requests from others.
Related stories
Over the coming weeks, it became easier to dive into my creative flow and focus on my own priorities when the temptation to check my email app was gone. I was no longer stuck on the hamster wheel of reacting to others' needs and subsequently sacrificing my own.
It transformed my work-life balance
When I first deleted my email app , I decided I would only check my desktop inbox three times a day: in the morning, at lunch, and at the end of my workday. The habit became a powerful signal of stepping in and out of my professional identity. I'd put on my metaphorical Writer Hat by checking my email in the morning, and I'd hang it up again when I checked my inbox in the afternoon.
My work stopped bleeding into evenings and weekends. While it was scary at first, I realized anyone who genuinely needed me in an emergency had my phone number and knew how to use it.
It actually helped me stay on top of my email
Paradoxically, I consistently live closer to Inbox Zero than I ever have. Before, checking my email multiple times an hour was an easy way to get a hit of feel-good chemicals to my brain.
Now that I check less frequently, I'm not browsing for a dopamine hit — I'm really there to check my email. I've been shocked to realize how much easier it is to handle my inbox in a few fell swoops throughout the day rather than sitting and hitting refresh all daylong.
I have more time for what matters
For me, keeping on top of my emails simply isn't as important as other work tasks. So why was I treating my inbox as one of my highest priorities by checking it all the time? My email app had become a facade of busyness and efficiency. By stepping away, I've found greater clarity and peace.
Anyone interested in the same is welcome to message me — just remember, it may take me a little while to get back your email.
Watch: Threads vs. Twitter: What we know about the apps
- Main content

Governor Newsom Puts Historic Mental Health Transformation on March 2024 Ballot
Published: Oct 12, 2023
WHAT YOU NEED TO KNOW: For the first time in decades, Californians will have the ability to transform the state’s mental health system – modernizing to meet the needs of all Californians. Governor Newsom signed Senate Bill 326 (Eggman), modernizing the Mental Health Services Act, and Assembly Bill 531 (Irwin), a $6.38 Billion bond to build new behavioral health housing and treatment settings across the state. Californians will vote on this package, collectively known as Proposition 1, on the March 2024 ballot.
LOS ANGELES – Today, Governor Gavin Newsom, accompanied by Legislative and local leaders, families, advocates, veterans, and health care professionals, signed Senate Bill 326 (Eggman, D – Stockton) and Assembly Bill 531 (Irwin, D – Thousand Oaks) which collectively will transform California’s mental health and substance use disorder treatment systems for the first time in decades

WHY THIS MATTERS: These reforms re-focus billions of dollars in existing funds to prioritize Californians with the deepest mental health needs, living in encampments, or suffering the worst substance use issues. The $6.38 billion bond will provide funding to build more than 11,150 new behavioral health beds and housing and 26,700 outpatient treatment slots – capacity that will touch many tens of thousands of people’s lives every year – filling critical needs across the state for homeless Californians with severe behavioral health issues, to kids suffering from depression, and everyone in between. Recent polling from the Public Policy Institute of California (PPIC) found an overwhelming majority (87%) of Californians say there is a mental health crisis in the United States.

- SB 326 Author & Senate Health Committee Chair Senator Susan Talamantes Eggman: “The Mental Health Services Act has been a great success – but after nearly 20 years it’s time to update it in a manner that is consistent with reforms in health care coverage and our increased understanding of behavioral health. The new Behavioral Health Services Act will drive resources to those with the greatest needs, including those with substance use disorders, and provide for real accountability with a focus on outcomes. Paired with Assemblymember Irwin’s essential bond, these new and restructured investments deliver on exactly what Californians deserve to address this crisis of behavioral health and homelessness. I’m grateful to this Governor for his commitment to those suffering and for his laser focus on critical reform.”
- AB 531 Author Assemblymember Jacqui Irwin : “Getting veterans experiencing homelessness off the streets has long been a priority for California, but getting some of our most vulnerable veterans into needed treatment for behavioral health challenges will be transformative. One of the only groups that has seen a recent significant decline in percent of homelessness are veterans, thanks primarily to the very successful Veterans Housing and Homeless Prevention (VHHP) program. By placing a renewed focus on existing programs like Homekey and the Behavioral Health Continuum Infrastructure program, AB 531 and SB 326 will provide housing and treatment services to veterans that focus on serious mental illness and substance use disorders. Funding and expanding this program is the right thing to do, and I look forward to working with the Governor and veterans organizations to put these important advances before the voters.”
- AB 531 Co-Author Senator Richard Roth: “This is a terrific day for California as the Governor’s signature sets in motion the transformation of our state’s behavioral health system to fully reflect the many challenges we face today. The bond provides, among other things, $1.5 billion dollars to expand the continuum of behavioral health treatment resources, specifically including, for the first time, new acute care inpatient psychiatric beds which are critically needed for emergency situations where a short-term stay is essential for mental health stabilization and treatment.”
- SB 326 Co-Author & Assembly Health Committee Chair Assemblymember Jim Wood : “Modernizing the 20-year-old MHSA as the Behavioral Health Services Act responds to the critical need to address the tragic reality of unhoused people we see on our streets and the mental health and substance use issues that many experience, but also pays heed to the housing and critical wraparound support services that people struggling with homelessness need. The services and funding provided in both SB 326 and AB 531 help the very young to the elderly, those in desperate need of affordable housing as well as those with the most serious need for treatment and support services to help people suffering from serious mental illness and substance use disorder.”
- Original Author of the Mental Health Services Act Sacramento Mayor Darrell Steinberg : “When we proposed and passed the Mental Health Services Act in 2004, our goal was ambitious. We sought to uphold that failed promise made by prior generations of state leaders: to fully fund whatever it takes to ensure that people living with serious mental illness live with dignity, independence, and safety in our communities. MHSA’s twenty-year history and $31 billion of community based services has saved many lives and moved us farther towards keeping our word. But the work is incomplete. Today’s historic signing of SB 326 and AB 531 moves us dramatically closer to making good on our sixty-year promise and will ensure that the original intent of the MHSA is met. Governor Newsom is the first Governor in history to make mental health and substance abuse care a signature state priority. Thanks to his leadership and the leadership of Senator Eggman, and Assemblymember Irwin, these billions will now be focused much more effectively on people who are the most vulnerable and help ensure that fewer people with serious illnesses live in conditions that no one should have to endure.”
- San Diego Mayor and Chair of the CA Big City Mayors Coalition Todd Gloria: “Thanks to Governor Newsom and the Legislature, Californians will have an opportunity to vote to create more than 10,000 new beds to provide residential settings for people struggling with mental illness and addiction to get the care they need. We can no longer leave people to languish on our streets, often ending up in emergency rooms or jails. California is reforming our behavioral health system by taking action that addresses the lack of services and includes desperately needed accountability.”
- Los Angeles Mayor Karen Bass: “We cannot address the homelessness crisis if we do not also address the mental health and substance abuse crisis on our streets. Thank you to Governor Newsom for locking arms with us by signing these two critical bills, and thank you to Senator Eggman and Assemblymember Irwin for their leadership. This is an emergency and that’s exactly how we’re treating it.”
- Los Angeles County Board of Supervisors Chair Janice Hahn : “We all know that those with the most serious mental illness have been the most difficult to help, but this Governor did not give up on them. This problem demands bold change, and with voters’ support we can build tens of thousands of places where we can treat mental illness and where people with severe mental illness can live and get well. Californians want a pathway forward to help people who are suffering, and this is it.”
- San Diego County Board of Supervisors Chair Nora Vargas: “I’m honored to stand with Governor Newsom as he delivers major mental health care for all Californians,” said Chairwoman Nora Vargas. “The monumental reform of the Mental Health Services Act represents a step forward in our commitment to providing comprehensive, compassionate, and effective mental health services for all Californians. As Chairwoman of the Board of Supervisors for San Diego County, I have seen firsthand the profound impact that untreated mental illness can have on individuals, families, and communities. We stand united in our commitment to ensuring that every Californian can access the mental health care they need and that they are treated with dignity and respect.”
- NAMI California CEO Jessica Cruz: “NAMI California is proud to support the modernization of the Behavioral Health Services Act through SB 326 and AB 531. We thank Governor Newsom for signing this critical legislation and Senator Eggman and Assemblymember Irwin for their instrumental leadership. We are proud of the collaboration with the Administration and partner agencies listening to families and individuals impacted by severe mental illness and substance use. This partnership ensured that the MHSA’s original intent was upheld as our state reforms its behavioral health system to better serve Californians in need.”
- California Association of Alcohol and Drug Program Executives Executive Director Robb Layne: “For far too long Californians have been battling substance abuse disorder without fully funded community treatment. We applaud the Governor for recognizing an opportunity to take a full circle approach and provide solutions that includes an “every tool in the toolbox” strategy to save lives and combat this epidemic. Our state is on the cusp of revolutionizing care through systemwide reform that paves the way for more accessible, human-centered treatment. This will provide a lifeline for those grappling with homelessness, substance abuse disorder, and mental illness.”
- U.S. Vets President and CEO Stephen Peck : “California continues to reduce the number of veterans living on our streets—a feat to be celebrated—but there are still thousands more who won’t have a place to sleep tonight. Governor Newsom’s successful legislative push to reform the Mental Health Services Act will allow providers to attack this problem head on. Refocusing funding that prioritizes care for those with the most serious mental illnesses combined with the promise of thousands of new, dedicated veteran housing units offers one of the state’s most sweeping and welcome reforms in favor of vulnerable veterans who need the stability and services to live a life of dignity.”
- California Medical Association President Donaldo Hernandez, MD, FACP: “For decades we have chronically under-resourced our community-based safety nets, which has now led us to a humanitarian crisis for which we don’t have the adequate tools to address. A sustainable model of care delivery for our residents struggling with serious mental health and substance use disorders must include, not only expanded access to services, but also stable and reliable access to housing. I applaud the Governor for continuing to remove barriers while working to assure that we can overcome the gaps that exist in serving those suffering from mental health and substance use disorders.”
- California Alliance of Child and Family Services CEO Chris Stoner-Mertz: “The Behavioral Health Services Act is strengthened by the Governor’s commitment to children and youth. California’s non profit providers of community based services to children and families are particularly proud that SB326 prioritizes Prevention and Early Intervention services that are culturally responsive, help keep families together, and improve long-term behavioral health outcomes.”
- SEIU California Executive Board Member and President of SEIU Local 721 David Green: “California’s approach to mental health services, though well-intentioned, has suffered from a lack of coordination, transparency, and accountability – in addition to limits on housing that no longer serve the urgent mental health crises playing out on our cities’ streets. Governor Newsom’s leadership on this complex issue has moved California toward a more coordinated and effective system of behavioral health services. SEIU members do the essential and emotionally difficult work of reaching out to Californians living in encampments, under freeways, and in our city parks, so we know better than anyone that a safe place to sleep and receive services is almost always the best medicine for people who are in crisis. Increasing program accountability and expanding access to housing and substance use disorder treatment options are the right things to do for our communities. This plan provides the opportunity to remove silos and ensure resources are aligned with the greatest needs. SEIU members are confident this reform effort will put California on a path toward more accountable and responsive behavioral health services. Meanwhile, we know the crises of housing affordability, inequality, and racism driving our state’s surge in homelessness won’t be solved overnight. SEIU members pledge our continued partnership in the critical work ahead.”
- California Professional Firefighters President Brian Rice: “We applaud Governor Newsom, Senator Eggman and Assemblymember Irwin for their leadership on SB 326 and AB 531. Every day, our firefighters and paramedics see the impact of severe mental illness and substance use disorder in our communities. We have to do more than just take people through a revolving door in the emergency room. By focusing on housing and treating those most in need, the Behavioral Health Modernization package can transform our approach to homelessness, mental illness and substance use disorder.”
- California Conference of Carpenters Director Danny Curtin: “We applaud Governor Newsom and the state legislature for not only recognizing the critical link between stable housing and mental health but actually doing something about it. We especially thank Senator Eggman and Assemblywoman Irwin for taking the reins on this issue.”
- California Chamber of Commerce CEO Jennifer Berrera: “We applaud Governor Newsom and the legislature for taking these bold steps to address the social crises manifesting on our streets. California employers, especially retailers, public-facing leisure and hospitality businesses, and health care, are at the front lines, and many struggle daily to stay open and provide a safe and welcoming business environment for their workers and customers. This ambitious response provides the necessary resources to enable a more effective response by service providers and get help to those most in need.”
Read our research on: Gun Policy | International Conflict | Election 2024
Regions & Countries
What public k-12 teachers want americans to know about teaching.
Illustrations by Hokyoung Kim

At a time when most teachers are feeling stressed and overwhelmed in their jobs, we asked 2,531 public K-12 teachers this open-ended question:
If there’s one thing you’d want the public to know about teachers, what would it be?
We also asked Americans what they think about teachers to compare with teachers’ perceptions of how the public views them.
Related: What’s It Like To Be a Teacher in America Today?
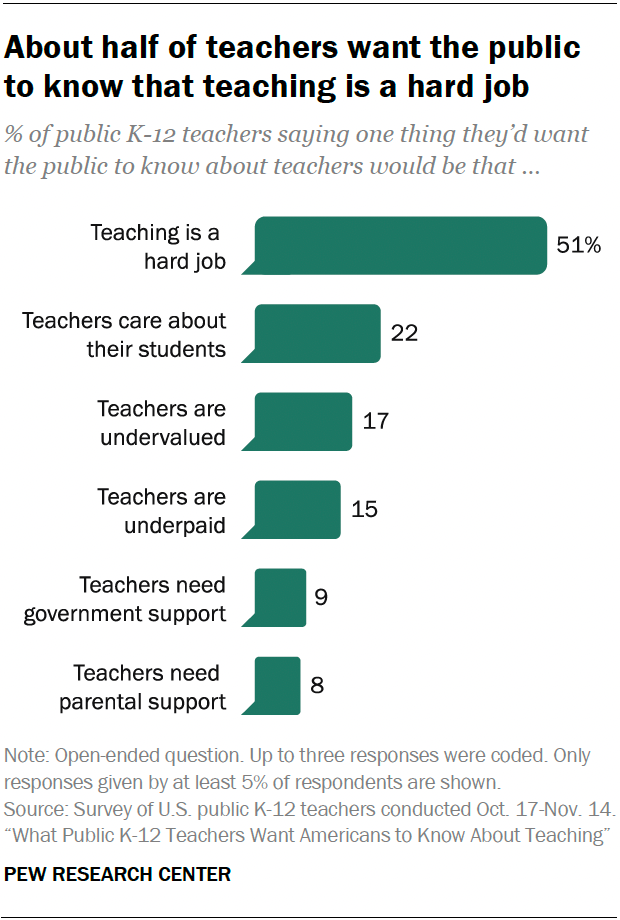
Pew Research Center conducted this analysis to better understand what public K-12 teachers would like Americans to know about their profession. We also wanted to learn how the public thinks about teachers.
For the open-end question, we surveyed 2,531 U.S. public K-12 teachers from Oct. 17 to Nov. 14, 2023. The teachers surveyed are members of RAND’s American Teacher Panel, a nationally representative panel of public K-12 school teachers recruited through MDR Education. Survey data is weighted to state and national teacher characteristics to account for differences in sampling and response to ensure they are representative of the target population.
Overall, 96% of surveyed teachers provided an answer to the open-ended question. Center researchers developed a coding scheme categorizing the responses, coded all responses, and then grouped them into the six themes explored in the data essay.
For the questions for the general public, we surveyed 5,029 U.S. adults from Nov. 9 to Nov. 16, 2023. The adults surveyed are members of the Ipsos KnowledgePanel, a nationally representative online survey panel. Panel members are randomly recruited through probability-based sampling, and households are provided with access to the Internet and hardware if needed. To ensure that the results of this survey reflect a balanced cross section of the nation, the data is weighted to match the U.S. adult population by gender, age, education, race and ethnicity and other categories.
Here are the questions used for this analysis , along with responses, the teacher survey methodology and the general public survey methodology .
Most of the responses to the open-ended question fell into one of these six themes:
Teaching is a hard job
About half of teachers (51%) said they want the public to know that teaching is a difficult job and that teachers are hardworking. Within this share, many mentioned that they have roles and responsibilities in the classroom besides teaching, which makes the job stressful. Many also talked about working long hours, beyond those they’re contracted for.
“Teachers serve multiple roles other than being responsible for teaching curriculum. We are counselors, behavioral specialists and parents for students who need us to fill those roles. We sacrifice a lot to give all of ourselves to the role as teacher.”
– Elementary school teacher
“The amount of extra hours that teachers have to put in beyond the contractual time is ridiculous. Arriving 30 minutes before and leaving an hour after is just the tip of the iceberg. … And as far as ‘having summers off,’ most of August is taken up with preparing materials for the upcoming school year or attending three, four, seven days’ worth of unpaid development training.”
– High school teacher
Teachers care about their students
The next most common theme: 22% of teachers brought up how fulfilling teaching is and how much teachers care about their students. Many gave examples of the hardships of teaching but reaffirmed that they do their job because they love the kids and helping them succeed.

“We are passionate about what we do. Every child we teach is important to us and we look out for them like they are our own.”
– Middle school teacher
“We are in it for the kids, and the most incredible moments are when children make connections with learning.”
Teachers are undervalued and disrespected
Some 17% of teachers want the public to know that they feel undervalued and disrespected, and that they need more public support. Some mentioned that they are well-educated professionals but are not treated as such. And many teachers in this category responded with a general plea for support from the public, which they don’t feel they’re getting now.
“We feel undervalued. The public and many parents of my students treat me and my peers as if we do not know as much as they do, as if we are uneducated.”
“The public attitudes toward teachers have been degrading, and it is making it impossible for well-qualified teachers to be found. People are simply not wanting to go into the profession because of public sentiments.”
Teachers are underpaid
A similar share of teachers (15%) want the public to know that teachers are underpaid. Many teachers said their salary doesn’t account for the effort and care they put into their students’ education and believe that their pay should reflect this.
“We are sorely underpaid for the amount of hours we work and the education level we have attained.”
Teachers need support and resources from government and administrators
About one-in-ten teachers (9%) said they need more support from the government, their administrators and other key stakeholders. Many mentioned working in understaffed schools, not having enough funding and paying for supplies out of pocket. Some teachers also expressed that they have little control over the curriculum that they teach.
“The world-class education we used to be proud of does not exist because of all the red tape we are constantly navigating. If you want to see real change in the classroom, advocate for smaller class sizes for your child, push your district to cap class sizes at a reasonable level and have real, authentic conversations with your child’s teacher about what is going on in the classroom if you’re curious.”
Teachers need more support from parents
Roughly the same share of teachers (8%) want the public to know that teachers need more support from parents, emphasizing that the parent-teacher relationship is strained. Many view parents as partners in their child’s education and believe that a strong relationship improves kids’ overall social and emotional development.

“Teachers help students to reach their potential. However, that job is near impossible if parents/guardians do not take an active part in their student’s education.”
How the U.S. public views teachers
While the top response from teachers in the open-ended question is that they want the public to know that teaching is a hard job, most Americans already see it that way. Two-thirds of U.S. adults say being a public K-12 teacher is harder than most other jobs, with 33% saying it’s a lot harder.
And about three-quarters of Americans (74%) say teachers should be paid more than they are now, including 39% who say teachers should be paid a lot more.
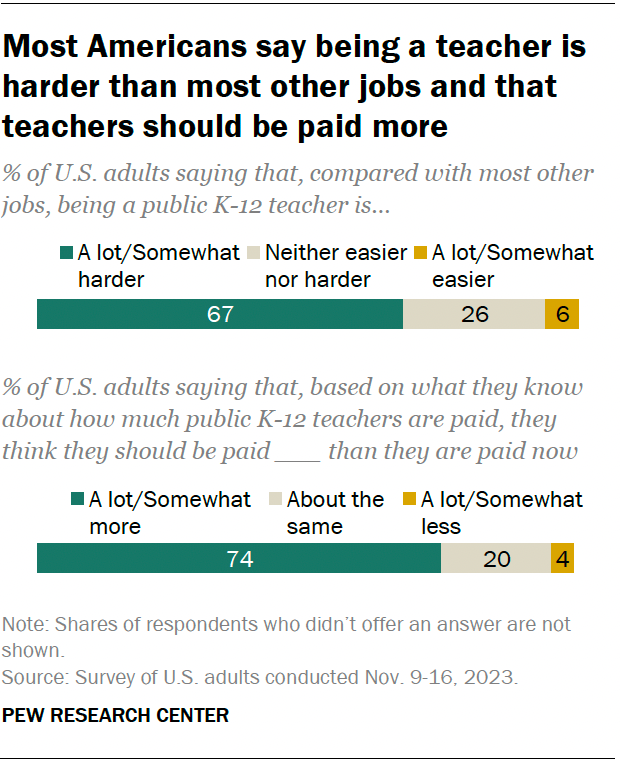
Americans are about evenly divided on whether the public generally looks up to (32%) or down on (30%) public K-12 teachers. Some 37% say Americans neither look up to or down on public K-12 teachers.
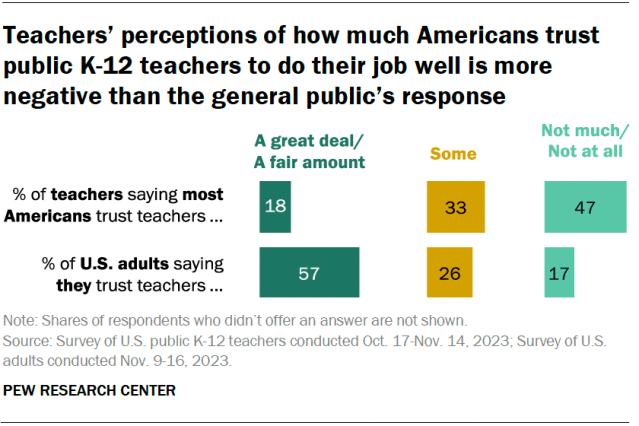
In addition to the open-ended question about what they want the public to know about them, we asked teachers how much they think most Americans trust public K-12 teachers to do their job well. We also asked the public how much they trust teachers. Answers differ considerably.
Nearly half of public K-12 teachers (47%) say most Americans don’t trust teachers much or at all. A third say most Americans trust teachers some, and 18% say the public trusts teachers a great deal or a fair amount.
In contrast, a majority of Americans (57%) say they do trust public K-12 teachers to do their job well a great deal or a fair amount. About a quarter (26%) say they trust teachers some, and 17% say they don’t trust teachers much or at all.
Related: About half of Americans say public K-12 education is going in the wrong direction
How the public’s views differ by party
There are sizable party differences in Americans’ views of teachers. In particular, Democrats and Democratic-leaning independents are more likely than Republicans and Republican leaners to say:
- They trust teachers to do their job well a great deal or a fair amount (70% vs. 44%)
- Teaching is a lot or somewhat harder when compared with most other jobs (77% vs. 59%)
- Teachers should be paid a lot or somewhat more than they are now (86% vs. 63%)
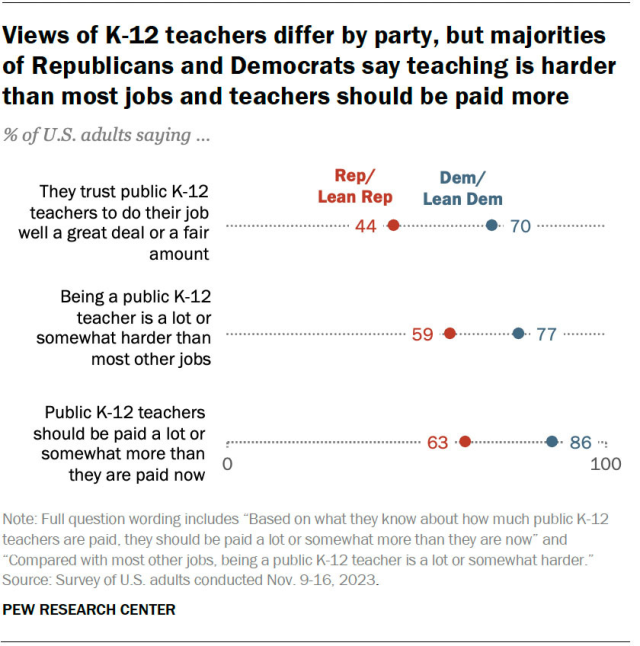
In their own words
Below, we have a selection of quotes that describe what teachers want the public to know about them and their profession.
Social Trends Monthly Newsletter
Sign up to to receive a monthly digest of the Center's latest research on the attitudes and behaviors of Americans in key realms of daily life
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .

IMAGES
COMMENTS
Because mental health is so important to general wellness, it's important that you take care of your mental health. To keep mental health in shape, a few introductions to and changes to lifestyle practices may be required. These include: Taking up regular exercise. Prioritizing rest and sleep on a daily basis.
Our mental health can affect factors like: Your self-esteem and self-worth. The way you socialize with others. The way you find meaning and value in your life. Your psychological functioning as it ...
The state of cognitive and behavioural well-being is referred to as mental health. The term 'mental health' is also used to refer to the absence of mental disease. Mental health means keeping our minds healthy. Mankind generally is more focused on keeping their physical body healthy. People tend to ignore the state of their minds.
The mental health essay is an insight into the importance of mental health in everyone's life. Mental Health. In the formidable years, this had no specific theme planned. The main aim was to promote and advocate the public on important issues. Also, in the first three years, one of the central activities done to help the day become special ...
Mental health is very important at every stage of our life, from childhood and adolescence through adulthood and even until we get old. Mental health is the state of an individual who is functioning at a satisfactory level of emotional and behavioral adjustment. It affects how we think, act and feel. Also, it helps to determine how we handle ...
Good mental health is not possible without policies and an environment that respects and protects basic civil, cultural, political, and socio-economic rights. People must have the security and ...
Make your essay relatable to people's daily life. Focus on Solutions. When discussing a sensitive topic like mental health it's important to focus on the solutions. Consider suggesting ways people can manage their own mental wellness or outlining how families can support each other during difficult times. Be Empathetic.
It is an integral component of health and well-being that underpins our individual and collective abilities to make decisions, build relationships and shape the world we live in. Mental health is a basic human right. And it is crucial to personal, community and socio-economic development. Mental health is more than the absence of mental disorders.
Here are some self-care tips: Get regular exercise. Just 30 minutes of walking every day can boost your mood and improve your health. Small amounts of exercise add up, so don't be discouraged if you can't do 30 minutes at one time. Eat healthy, regular meals and stay hydrated.
For this reason, mental health is one of the greatest assets. It not only helps you focus, overcome obstacles in life, gets along with the people around you, but also stay well. One doesn't need to have a mental illness to pay attention to their mental well-being. Everyone knows how to look after their physical health.
Debate: Student mental health matters - the heightened need for school‐based mental health in the era of COVID‐19. Deborah M. Weisbrot 1 and Erika Ryst 2 ... School mental health professionals will be essential in helping to shape messages to students and families about school re‐entry, to address anxiety, to promote social adjustment ...
Mental health includes our emotional, psychological, and social well-being. It affects how we think, feel, and act. It also helps determine how we handle stress, relate to others, and make healthy choices. 1 Mental health is important at every stage of life, from childhood and adolescence through adulthood.
Mental Health Matters Coping with stress in a connected world Mary McNaughton-Cassill, Ph.D. , is a Professor of Clinical Psychology and an award-winning teacher at the University of Texas at San ...
Anxiety disorders are a leading mental health issue globally, and the NIMH approximates that almost 1 in 3 people will experience an anxiety disorder in their lifetime. Symptoms of anxiety can range from tenseness or nervousness to panic attacks and physical illness. Anxiety can refer to generalized anxiety disorder, social anxiety, separation ...
Speaking Up About Mental Health is an essay contest that challenges high school students ages 16-18 to raise awareness of mental health. The contest gives students a platform to share ways to eliminate and/or reduce mental health stigma faced by young people, especially in diverse communities. This contest is soliciting essays that: Get details ...
Breakdown: California's mental health system, explained. Mental health advocates have long described California's fragmented mental health system with words like "struggling" and "broken.". Evidence of its consequences can be found in our jails and prisons, our hospitals and clinics, our schools and colleges. The problem touches ...
Safeguarding the Mental Health of Teachers. Teachers tell their students that mindset matters. Yet teachers do not always allow themselves space to receive those same messages of reflection and self-care. Henry Seton, a longtime high school teacher and department head, learned that firsthand. In a courageous and insightful essay in Educational ...
Harvard leaders Dr. Luana Marques and Professor Michael Puett gathered with moderator Anna Bartuska to answer these questions and more in our latest webinar, Mental Health Matters: Strategies for Managing Anxiety and Feeling Happier.. In this 60-minute webinar, Dr. Marques and Professor Puett shared their personal experience with anxiety, discussed trending topics in mental health, answered ...
Through these short essays, teens can shed light on the mental health challenges they or their peers face. They can also share innovative ideas and insights for reducing stigma and helping teens seek mental health support without judgment or fear. Important dates. Contest opens: December 1, 2023. Submission deadline: January 16, 2024
Gov. Gavin Newsom today unveiled a much anticipated proposal to address a mental health crisis increasingly visible on trash-strewn sidewalks and in cramped jail cells around California. The proposal, known as the Community Assistance, Recovery and Empowerment (or CARE) Court, would provide a framework for courts to compel people with serious ...
Mental health is physical health and vice versa. It is not simply a cluster of unwanted feelings or self-deprecating thoughts. Yesterday was World Mental Health Day. Businesses globally touted the ...
Each Mind Matters Celebrated Across the State. 248. 10. Number of times on May 13th that @EachMindMatters was favorited, retweeted and mentioned on Twitter. Number of new "likes" on the Each Mind Matters Face-book page ahead of Mental Health Matters Day. The culmination of Mental Health Matters Day was the Directing Change Student Video ...
To further complicate matters, in the early 2000s, drug manufacturer Eli Lilly stuck its finger in the pie. Eli Lilly's patent on its blockbuster drug Prozac, which treated depression, was set ...
MHA in New York State, Inc. Albany, NY (518) 434-0439 mhanys.org. Allegany Co. MHA Wellsville, NY (585) 593-1991 Association for Mental Health and Wellness Ronkonkoma, NY (631) 471-7242 mentalhealthandwellness.org. Community Connections of Franklin Co.
My mental health, free time, and productivity skyrocketed. ... Essay by Katie Lemon. 2024-03-27T10:04:01Z An curved arrow pointing right. ... I have more time for what matters. For me, keeping on ...
WHY THIS MATTERS: These reforms re-focus billions of dollars in existing funds to prioritize Californians with the deepest mental health needs, living in encampments, or suffering the worst substance use issues. The $6.38 billion bond will provide funding to build more than 11,150 new behavioral health beds and housing and 26,700 outpatient ...
How the U.S. public views teachers. While the top response from teachers in the open-ended question is that they want the public to know that teaching is a hard job, most Americans already see it that way. Two-thirds of U.S. adults say being a public K-12 teacher is harder than most other jobs, with 33% saying it's a lot harder.