- Research article
- Open access
- Published: 12 January 2021

Social justice in health system; a neglected component of academic nursing education: a qualitative study
- Hosein Habibzadeh 1 ,
- Madineh Jasemi 1 &
- Fariba Hosseinzadegan ORCID: orcid.org/0000-0002-3464-7385 1
BMC Nursing volume 20 , Article number: 16 ( 2021 ) Cite this article
36k Accesses
11 Citations
Metrics details
In recent decades, increasing social and health inequalities all over the world has highlighted the importance of social justice as a core nursing value. Therefore, proper education of nursing students is necessary for preparing them to comply with social justice in health systems. This study is aimed to identify the main factors for teaching the concept of social justice in the nursing curriculum.
This is a qualitative study, in which the conventional content analysis approach was employed to analyze a sample of 13 participants selected using purposive sampling method. Semi-structured interviews were conducted to collect and analyze the data.
Analysis of the interviews indicated that insufficient education content, incompetency of educators, and inappropriate education approaches made social justice a neglected component in the academic nursing education. These factors were the main sub-categories of the study and showed the negligence of social justice in academic nursing education.
Research findings revealed the weaknesses in teaching the concept of social justice in the nursing education. Accordingly, it is necessary to modify the content of nursing curriculum and education approaches in order to convey this core value. Since nursing educators act as role models for students, especially in practical and ethical areas, more attention should be paid to competency of nursing educators, specially training in the area of ethical ideology and social justice.
Peer Review reports
Professional values include action standards that are accepted by group members and provide a framework for evaluating beliefs and notions affecting behavior [ 1 ]. Acquisition of professional nursing values is a prerequisite for resolving conflicts; it improves service quality and increases job satisfaction of nurses [ 2 ]. The core values accepted and presented by American Association of Colleges of Nursing (AACN) (1998) include human dignity, integrity, autonomy, altruism, and social justice [ 3 ], out of which social justice has attracted more attention in recent years. Disproportionate burden of diseases and deaths in parts of the society associated with environmental and socioeconomic factors has been recognized for decades; however, the number of documents on these issues has increased dramatically over the past 15 years [ 4 ]. The WHO Commission on Social Determinants of Health attributes these differences to social inequalities in the distribution of power, income, shelter, education, and healthcare as well as climate change, vulnerability, and other life conditions. It also prioritizes social justice as a mechanism for correcting and eliminating inequalities [ 5 ]. Social justice in the health system refers to providing equal healthcare services for all individuals, regardless of their personal characteristics [ 6 ]. The AACN defines social justice as fair treatment, regardless of one’s economic status, race, ethnicity, age, citizenship, disability, or sexual orientation [ 7 ].
Although social justice has been identified as a professional value in documents issued by reputable nursing associations such as International Council of Nurses (ICN), Canadian Nurses Association (CNA), American Nurses Association (ANA), and AACN [ 8 ], the discussion of social justice in nursing profession has always been accompanied by serious doubts and concerns [ 9 ]. In addition, nurses’ responses to social injustice have not always been admirable, and nursing profession’s poor performance originates from various factors such as unawareness [ 10 ].
Development of a professional value such as social justice is a continuous and long-term process that begins with professional nursing education and continues throughout years of nursing practice. Education plays a key role in acquiring professional values [ 11 ]. Students, educators, faculties, clinical and educational experiences, and individual values are among the most important components of learning and development of professional values [ 12 ]. It is very important to train highly skilled and qualified nurses to provide necessary care for heterogeneous populations in today’s ever-changing demographic prospect. Nursing students must understand their responsibility for poplulation health issues and social factors affecting health (eg, world hunger, environmental pollution, lack of access to health care, violation of human rights, and inequitable distribution of health care resources, including nursing services) and in this regard acquire the necessary knowledge and skills [ 13 ].
To institutionalize the concept of social justice in nursing students, especially in developed countries, measures have been taken in the area of education, which include modifications made to nursing curriculum and education approaches [ 14 ]. For instance, simulation is a one of new methods utilized for teaching this concept [ 15 ]. Since the mid-2000s, there has been an increase in tendency towards online learning [ 16 ], co-curricular experiences [ 17 ], and digital storytelling [ 18 ] in order to promote students’ understanding of social justice issues. Nevertheless, some studies have addressed the weaknesses of nursing curriculum in teaching social justice [ 19 , 20 ] and have attributed nurses’ inability in pursuing social justice to their poor scientific and practical competencies [ 21 ]. Although several quantitative and qualitative studies have been conducted in recent decades to institutionalize the concept of social justice among nursing graduates [ 22 , 23 , 24 , 25 ], academic nursing education has unfortunately failed to train competent nurses who seek information and training on social justice. Considering the importance of this subject, a qualitative approach [ 26 ] was adopted to provide an in-depth understanding of social justice based on the realistic results derived from the participants’ real experiences. Therefore, in this study, the experiences of nursing educators and students in identifying the main factors for teaching the concept of social justice in nursing education program were analyzed.
Study design and setting
This qualitative study was conducted using a conventional content analysis method. The participants were recruited from three nursing faculties (Urmia, Tabriz, and Tehran) and two teaching hospitals of Tehran (Motahari Hospital) and Urmia (Talegani Hospital) in Iran. These cities were selected due to their large size and forerun in educational, clinical, and social nursing activities.
Study participants
In view of the objective of the study - identify the main factors for teaching the concept of social justice in the nursing curriculum - we initially selected nursing educators by purposive sampling method. Nursing educators who had more than 5 years of service experience and among the prominent educators with activity in nursing institutions that involved in developing social justice were selected. The data from the study then led us to students and clinical nurses. Among the students, the final year undergraduate students, exemplary and active in social fields, and among the nurses, those with more than 2 years of service experience, accepted by the system professionally and actively in the field of social justice, such as voluntary activities in public health promotion, were selected for the interview.
The participants included 6 men and 9 women with the mean age of 39.07 ± 12.92 years old and mean work experience of 20.00 ± 7.22 years. Out of all the participants, 5 individuals had PhD, whereas 2 had Master’s degrees; the rest had Bachelor’s degrees in nursing. In total, 7 individuals were nursing educators, 2 individuals were clinical nurses, and 4 individuals were nursing students (Table 1 ).
Data collection
The data were collected using in-depth, semi-structured individual interviews conducted at the times and in the places selected by the participants (mainly at nursing faculties). Each interview lasted for 30–90 min; they were audio recorded upon the participants’ permission and transcribed verbatim. All the 13 interviews were conducted by the research team (FH, MJ, and HH) between February and November 2019. The participants were asked questions about their experiences of (learning/teaching) social justice issues. Considering the abstract nature of the research subject, the researchers raised more objective questions. For instance, the educators were asked to “describe their experiences of modification to the curriculum to cover social justice issues”, whereas the students were asked to “describe their experiences of social justice-based practices during internships”. In addition, to better identify factors affecting social justice education in nursing, the educators and students were asked questions such as “Considering your experiences, what factors have affected your engagement in social justice in education?” and “How do you describe education approaches adopted by educators for teaching social justice?”, respectively. (See Additional file 1 for details). The researchers continued the interviews until the data were completely saturated, i.e. when no new idea, concept, or category was derived from the final interviews.
To better relate to the environments of the study and the participants and analyze the data realistically, the researchers also used field notes. Field notes are a brief summary of the observations made while collecting data. This is not limited to a particular type of activity or behavior and assesses the non-verbal behaviors of the participants and their interactions with others. It also depicts a picture of a social position. In this study, field notes also made a detailed presentation of the situation in the right place immediately after the interview and provided the opportunity to confirm the psychological and emotional reactions of the participants. For example, attending the emergency ward of one of the teaching hospitals in Urmia city and observing nursing education in the clinical environment led to a field note focusing the training on the clinical procedures that confirm the insufficient educational content and lack of attention to social justice in nursing education.
Data analysis
After the data were collected, they were analyzed using the conventional content analysis approach. For this purpose, Grundheim and Lundman’s (2004) method was adopted [ 27 ]. In this method, an entire interview is regarded as an analysis unit involving notes that must be analyzed and coded. The researchers listened to the interviews for several times and transcribed the recorded interviews verbatim. The paragraphs, sentences, and words were considered meaning units. A meaning unit is a set of words and sentences that are related to each other in content and are categorized based on their content and context. The texts were reviewed several times to highlight words containing key concepts or meaning units and extract the initial codes. The codes were then reviewed several times in a continuous process from code extraction to labeling. Similar codes were merged, categorized, and labeled and the subcategories were determined. The extracted subcategories were finally compared and merged (if possible) to form the main categories.
Assessing data accuracy and stability
Guba and Lincoln’s (1986) criteria were used to ensure the accuracy and stability of the research data. The credibility of the data was assessed using member-checking and prolonged engagement techniques. For member-checking technique, the participants reviewed the content of the interview and the resulting codes to ensure the accurate meaning and for really reflecting their experiences. The data were also assessed by an external researcher (peer debriefing). To ensure the dependability, data collection methods, interview, taking notes, coding, and data analysis were expressed in detail in order to make judging by the external auditor (external auditing). In order to achieve confirmability, the audit trail method was used, so that all stages of the research, especially the stages of data analysis and the results, were provided to checking of two expert colleagues in the field of qualitative research. The transferability of the findings was also established by providing a rich description of the research report and the content of the interviews was represented by the selected quotations from the participants [ 28 ].
Ethical considerations
The participants were selected after the approval of Ethics Committee of Urmia University of Medical Sciences and the necessary permissions (Code: IR.UMSU.REC.1397.223) were granted. Prior to the interviews, the participants were informed about their anonymity, confidentiality of their information, the research method and objectives, and their right to leave the study at will. The participants also signed informed consent forms.
Classification of the interviews showed that three sub-categories of “insufficient educational content”, “limited competency of nursing educators”, and “inappropriate education approaches” led to the emergence of the main category called “social justice; a neglected component of academic education” (Table 2 ).
Social justice; a neglected component of academic education
Proper education plays a major role in training justice-seeking nurses. Social justice and its importance in healthcare are constituents of the nursing syllabus. Paying more attention to this issue in practical and objective areas of education by educators can influence students’ thoughts, attitudes, and behaviors to pursue justice in health systems. However, Iran’s education system has unfortunately failed to promote justice because of insufficient educational content, limited competency of nursing educators, and inappropriate education approaches.
Insufficient educational content
Development of a comprehensive nursing curriculum, especially on ethical issues such as social justice, could substantially contribute to the preparation of socially and morally conscious nurses who are able to make significant changes in the public health at local, national, and international levels. In this study, the participants highlighted some weaknesses in the content of the existing nursing curriculum such as lack of attention to social justice, discontinuity in presenting courses on ethical values, and allocating most of the nursing courses to medical issues and clinical care.
Lack of attention to social justice in nursing curriculum
Social justice is a core nursing value which plays a significant role in promoting justice by nursing students and nurses. However, according to the participants, it has unfortunately been neglected in the existing nursing curriculum. In this regard, one participant stated,
“In the fourth semester, we studied a course on nursing ethics. I think there was no discussion on social justice because I don’t remember anything about this topic” (Participant No. 7/Nursing Student).
Regarding the importance of teaching social determinants of health, another participant stated,
“I was not aware of the importance of social issues in health until I participated in a workshop called ‘Social Justice in Health’. It really changed my beliefs and broadened my perspective” (Participant No. 10/Clinical Nurse).
Discontinuity in presenting courses on ethical values
Values are major components of the nursing profession. The institutionalization and development of professional values such as social justice contribute significantly to the future of this profession. The few number of courses presented on ethical values and discontinuity in the presented courses (for instance, no course on ethical values is provided for post-graduate students) were major items mentioned by the participants. In this regard, one of the participants stated,
“When students are repeatedly reminded of the importance of a value, they will realize its importance and the value will be institutionalized in them. We partially studied professional values and social justice issues in the fourth semester of our undergraduate courses; however, no similar course was provided for us afterwards during the Master’s program” (Participant No. 5/ Faculty Member).
Or another participant stated:
“We cannot deny that the ethical issues have been institutionalized in our professional graduates to some extent. But, these issues are not worked on in a principled and scientific manner and that there is no constant focus on them. After all, the effect of the hidden curriculum has been more prominent.”(Participant No.1/Faculty Member).
Allocating most of nursing courses to medical issues and clinical care
Diseases and clinical care are among the most fundamental parts of theoretical and practical training provided for nursing students; however, due to the multi-dimensional nature of the nursing profession, special attention should be paid to other dimensions as well. According to the research results, the existing nursing curriculum focuses mainly on transferring knowledge and skills associated with physical and routine care. One participant expressed,
“Most of our courses were related to various diseases and nursing care, and educators rarely talked about ethical and legal issues during their lectures” (Participant No. 6/ Nursing Student).
Another participant stated the reasons for the focus of nursing education on the physical and caring dimensions:
“Well, when we see that our graduates have problems in providing quality clinical care, we also have to do more in the field of clinical care.”(Participant No.3/ Faculty Member).
Limited competency of nursing educators
Educators play an undeniable role in training competent nurses through institutionalizing beliefs and behaviors. Using proper teaching and behavioral approaches, educators can improve students’ critical thinking skills and prepare them to promote justice in health systems. According to the participants, insufficient competency of nursing educators in teaching social justice issues and inappropriate value perspectives of educators in developing social justice were the main properties of this category.
Insufficient capabilities of educators in teaching social justice issues
Educators must be equipped with sufficient scientific, practical, and ethical capacities in order to effectively institutionalize the concept of social justice in students. According to the participants, nursing educators’ insufficient knowledge and experience about social justice issues make it difficult for them to transfer such knowledge to their students. One participant said,
“When I was a student, I once informed my educator about the unjust patient admission procedure in the surgical department. Yet, my educator recommended me to do what the head nurses would say. I did not see the necessary authority in my educator to establish justice” (Participant No. 11/ Clinical Nurse).
Low presence of nursing educators in clinical and community settings is also one of the factors that, according to the participants, has contributed to this problem.
“Unfortunately, our professors are so involved in education and research, especially to promote themselves, that they do not have the opportunity to address social issues.” (Participant No.9/ Faculty Member).
Inappropriate value perspectives of educators in developing social justice
The participants highlighted the important role of nursing educators’ ethical perspectives in promoting the quality of education and training qualified nurses who would provide services tailored to the needs of the society. They also argued that ethical values could help educators establish and expand social justice in health systems. According to the results, most of the educators had undesirable value perspectives on establishing social justice in the area of health. In this respect, participant no. 5 stated,
“When a nurse has no right to make any decisions in a healthcare system, what can I say to the student about social justice?” (Participant No. 5/ Faculty Member).
“My main responsibility is to transfer knowledge in the field of nursing and I think ethics should be taught by educators in medical ethics.” (Participant No.2/ Faculty Member).
Inappropriate education approaches
Education approaches are considered an essential part of the educational structure and play a key role in transferring ethical values such as social justice to students. Given the abstract nature of social justice, choosing the best education approach could help educators resolve complicated problems during teaching in order to institutionalize professional values and beliefs. According to the findings, educators adopt poor education approaches to transfer ethical values such as social justice and self-awareness to students. In this regard, focusing on traditional education approaches and using insufficient affective learning approaches were cited by the participants.
Focusing on traditional education approaches
Undoubtedly, lecturing is one of the most widely used education approaches; however, this traditional method is very ineffective in teaching abstract concepts such as social justice. According to the participants, educators mostly use lecturing approach to teach social justice issues and students are rarely involved in the teaching process. One participant argued that educators mainly use teacher-centered approaches in ethical discussions, stating,
“We (the students) had no active role in the professional ethics class. The educator spoke on relevant topics based on the availed syllabus and provided some examples of clinical ethical issues. However, I think that educators must discuss social justice issues with students to help them visualize and understand cases of injustice and discuss appropriate reactions in such situations” (Participant No. 13/ Nursing Student).
Another participant stated this:
“The predominant teaching method in professional ethics classes has been lecturing. Every now and then, there was some discussions in between, but it was very rare. Other nursing educators were also using the lecture method when talking about ethics” (Participant No. 7/ Nursing Student).
Using insufficient affective learning approaches
The use of affective learning strategies such as reflective activities and simulations leading to emotional responses plays an important role in creating self-reflection and transferring professional knowledge and skills to nursing students. However, based on the participants’ experience, affective learning approaches are not used effectively and systematically in teaching ethical issues such as social justice. In this regard, one participant stated,
“Since there are too many topics on professional ethics, we (educators) can only convey basic issues to students and it is difficult for us to adopt other learning strategies such as the affective approach” (Participant No. 4/ Faculty Member).
The same participant further stated:
“Now, in the professional ethics class, I do my best to teach the content with a combination of methods. For example, we have formed a group for medical students in the cyberspace (WhatsApp) and asked students to express the issues and questions of clinical ethics. They should raise it there because there is no time in the classroom for these issues. However, we have not performed the same for nursing students yet” (Participant No. 4/ Faculty Member).
According to the research findings, social justice in a health system is a neglected component of academic nursing education due to factors including insufficient educational content, limited competency of nursing educators, and inappropriate education approaches. These factors were introduced as the main research subcategories in this study.
Some weaknesses were observed in the content of nursing curriculum, which is an main factor in promoting professional nursing values such as social justice in nursing students. Lack of attention to the issue of social justice in nursing curriculum has also been mentioned in other studies [ 13 , 20 ]. Based on the participants’ experience, most of the nursing courses are allocated to medical issues and clinical care. According to Thurman, clinical specialties have received the main focus of nursing curriculum, whereas little attention has been paid to social justice issues [ 21 ] . This problem can be attributed to the poor performance of nurses in clinical care. The participants also believed that there was discontinuity in presenting courses on ethical values because the professional ethics course was presented only to undergraduate students. This issue disrupts the proper institutionalization of ethical values such as social justice in nursing students. Frenk et al. believe that the preparation of healthcare professionals to address current healthcare inequalities and challenges has been slowed down by obsolete, fragmented, and static curriculum [ 29 ]. In addition, Rozendo et al. highlighted inconsistencies in terms of presenting social justice-related issues in nursing curricula and argued that there was little material on social justice in post-graduate nursing programs [ 14 ].
Nursing educators’ competencies also affect teaching social justice issues. In today’s rapidly-changing world facing numerous crises, experienced educators play a significant role in training qualified nurses equipped with various skills enabling them to create social development. Accordingly, Read et al. highlighted the critical role of nursing educators in institutionalizing fundamental principles of social justice and health equity in students [ 30 ]. According to Ellis, educators should shift nursing students’ learning and thinking attitudes from individualism to community-centered frameworks and from tertiary (reactionary) to primary (preventive) care approaches [ 31 ]. However, unfortunately, the research findings indicated that nursing educators are not sufficiently qualified to teach and institutionalize social justice in students. In this regard, educators’ insufficient knowledge and experience in teaching social justice issues were highlighted by the participants. Borhani et al. found that ethical knowledge of nursing educators determined their students’ professional ethics competencies [ 32 ]. Akbas et al also argued that nursing educators’ knowledge and skills were the first and most important factors affecting their success in teaching issues of professional ethics [ 33 ]. As mentioned by the participants, inappropriate value perspectives of educators in developing social justice was another weakness of nursing educators. The significant impact of educators’ perspectives on teaching ethical values such as social justice has also been emphasized by Parandeh et al. [ 12 ].
Education approaches adopted to present and convey ethical values to students are of high importance. In this regard, Einhellig discussed the ineffectiveness of traditional approaches such as lecturing in institutionalizing social justice in nursing graduates and outlined the benefits of affective learning approaches [ 19 ]. According to the findings, lecturing is the dominant approach used to teach social justice in Iran’s nursing faculties, which is an inefficient teaching approach, as suggested by the research literature. This is probably due to the large number of students and limited time allocated to each academic course. While cognitive learning approaches rely on principles and concepts, affective learning approaches support the integration of knowledge with emotions, attitudes, and personal beliefs [ 34 ]. Neumann found that affective education approaches could enhance students’ understanding and use of ethical values [ 35 ]. Einhellig highlighted that nursing faculties need to use various strategies with a focus on behavior changes in order to successfully institutionalize the concept of social justice in nursing graduates [ 24 ].
Limitations
The findings of the present study were limited to factors affecting education of social justice in the nursing curriculum in the health system in the culture of Iran. Other limitations of this study was the consideration of the three nursing faculties and two teaching hospitals in Iran. As such, it may not be a representative of the experiences of all the nursing profession members in Iran. Limitations of our study proposed the need for conducting further studies with larger and mixed groups and in different cultures.
The research findings provided researchers with an insight into the weaknesses of nursing curricula, educators, and education approaches in social justice development in Iran. It seems that more attention must be paid to professional values and social determinant of health in nursing curricula in order to train justice-seeking nurses with a sense of responsibility. Educators play a prominent role in training competent individuals who are aware of and sensitive to social issues and inequalities. It is necessary to change the education approaches adopted by nursing educators in order to institutionalize the concept of social justice in students. After changing the content of nursing curriculum and applying different education approaches, future studies can focus on the impact of such changes on social development and social justice promotion.
Availability of data and materials
The interview dataset generated and analysed during the current study are not publicly available due to promises of participant anonymity and confidentiality. However, on reasonable request the data could be available from the corresponding author. All applications should be sent to [email protected] . All requests will be answered within a maximum of 1 month by email.
Abbreviations
World Health Organization
American Association of Colleges of Nursing
International Council of Nurses
American Nurses Association
Canadian Nurses Association
Kaya H, et al. Personal and professional values held by baccalaureate nursing students. Nurs Ethics. 2017;24(6):716–31.
Article PubMed Google Scholar
Tehranineshat, B., C. Torabizadeh, and M. Bijani, A study of the relationship between professional values and ethical climate and nurses' professional quality of life. Int J Nurs Sciences. 2020;7(3):313-19.
American Association of Colleges of Nursing, The essentials of baccalaureate education for professional nursing practice. Washington, DC: American Association of Colleges of Nursing; 1998.
Perry DJ, et al. Exercising nursing essential and effective freedom in behalf of social justice: a humanizing model. ANS Adv Nurs Sci. 2017;40(3):242–60.
Plamondon KM, et al. The integration of evidence from the commission on social determinants of health in the field of health equity: a scoping review. Crit Pub Health. 2020;30(4):415–28.
Institute of Medicine, The future of nursing: Leading change, advancing health. Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing. Washington, D.C.: National Academies Press; 2011.
Davis RK, et al. Social justice as an expression of caring through holistic admissions in a nursing program: a proposed conceptual model. Nurs Forum. 2020;55(4):723–9.
Matwick AL, Woodgate RL. Social justice: a concept analysis. Public Health Nurs. 2017;34(2):176–84.
Browne AJ, Reimer-Kirkham S. Problematizing social justice discourses in nursing. In: Philosophies and practices of emancipatory nursing: Social justice as praxis; 2014. p. 21–38.
Chapter Google Scholar
Walter RR. Emancipatory nursing praxis: a theory of social justice in nursing. Adv Nurs Sci. 2017;40(3):225–43.
Article Google Scholar
Parvan K, Hosseini F, Zamanzadeh V. Professional Values from Nursing Students' Perspective in Tabriz University of Medical Sciences: a pilot study. Iran J Nurs (2008-5923). 2012;25(76):69–82.
Parandeh A, et al. Factors influencing development of professional values among nursing students and instructors: a systematic review. Global J Health Sci. 2015;7(2):284.
Google Scholar
Waite R, Brooks S. Cultivating social justice learning & leadership skills: a timely endeavor for undergraduate student nurses. Nurse Educ Today. 2014;34(6):890–3.
Rozendo CA, Santos Salas A, Cameron B. A critical review of social and health inequalities in the nursing curriculum. Nurse Educ Today. 2017;50:62–71.
Menzel N, Willson LH, Doolen J. Effectiveness of a poverty simulation in second life®: changing nursing student attitudes toward poor people. Int J Nurs Educ Scholarsh. 2014;11(1):39–45.
Breen H, Jones M. Experiential learning: using virtual simulation in an online RN-to-BSN program. J Contin Educ Nurs. 2015;46(1):27–33.
Davis JN, Sullivan K, Guzman A. Catalyst for growth: the implications of co-curricular experiences for nursing education. J Nurs Educ. 2018;57(2):110–4.
LeBlanc RG. Digital story telling in social justice nursing education. Public Health Nurs. 2017;34(4):395–400.
Einhellig K, Hummel F, Gryskiewicz C. The power of affective learning strategies on social justice development in nursing education. J Nurs Educ Pract. 2015;5(1):121.
Canales MK, Drevdahl DJ. Social justice: from educational mandate to transformative core value, in Philosophies and practices of emancipatory nursing: Social Justice as Praxis. New York, NY: Routledge; 2014. p. 155–74.
Thurman W, Pfitzinger-Lippe M. Returning to the profession's roots: social justice in nursing education for the 21st century response. Adv Nurs Sci. 2017;40(4):318.
Torres-Harding SR, Meyers SA. Teaching for social justice and social action. J Prev Interv Community. 2013;41(4):213–9.
Groh CJ, Stallwood LG, Daniels JJ. Service-learning in nursing education: its impact on leadership and social justice. Nurs Educ Perspect. 2011;32(6):400–5.
Einhellig K, Gryskiewicz C, Hummel F. Social justice in nursing education: leap into action. J Nurs Care. 2016;5(374):2167–1168.1000374.
Hellman AN, et al. Understanding poverty: teaching social justice in undergraduate nursing education. J Forensic Nurs. 2018;14(1):11–7.
Speziale HS, Streubert HJ, Carpenter DR. Qualitative research in nursing: advancing the humanistic imperative. 5 th edition. 2011: Wolters Kluer: Lippincott Williams & Wilkins; 2011.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12.
Article CAS Google Scholar
Lincoln YS, Guba EG. But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Dir Prog Eval. 1986;1986(30):73–84.
Frenk J, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376(9756):1923–58.
Read CY, Betancourt DMP, Morrison C. Social change: a framework for inclusive leadership development in nursing education. J Nurs Educ. 2016;55(3):164–7.
Ellis S. The existing intersection of social justice and nursing; 2013.
Borhani F, et al. Professional Ethical Competence in nursing: the role of nursing instructors. J Med Ethics Hist Med. 2010;3(3):1-8.
Akbas M, Kadioglu S, Tuncer I. Ethics in nursing education from the viewpoints of Turkish nursing educators. Int J Educ Sci. 2017;19(2–3):104–12.
Holt KM. Affective domain learning in high-fidelity simulation: students’ perspectives; 2017.
Neumann JA, Forsyth D. Teaching in the affective domain for institutional values. J Contin Educ Nurs. 2008;39(6):248–52.
Download references
Acknowledgments
This study is a part of a PhD dissertation approved and funded by Vice Chancellor for Research, Urmia University of Medical Sciences. The researchers would like to thank the authorities of School of Nursing and Midwifery, Urmia University of Medical Sciences, as well as the participants for their kind cooperation.
This study was funded by Department of Research, Urmia University of Medical Sciences, which had no role in the design of the study, data collection, analysis, interpretation of data, or writing the manuscript.
Author information
Authors and affiliations.
Faculty of Nursing and Midwifery, Urmia University of Medical Sciences, Urmia, Iran
Hosein Habibzadeh, Madineh Jasemi & Fariba Hosseinzadegan
You can also search for this author in PubMed Google Scholar
Contributions
The study was designed by HH,MJ and FH. FH participated as the main interviewer. The initial deductive data analysis was done by FH and used as validation of the analysis carried out by HH and MJ. The final data analysis of the interviews was discussed and consented to by all authors. A first draft of the article was developed by FH and MJ. All authors then contributed to this, and finalized it together. FH was responsible for the final draft of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Fariba Hosseinzadegan .
Ethics declarations
Ethics approval and consent to participate.
The participants were selected after the approval of Ethics Committee of Urmia University of Medical Sciences and necessary permissions (Code: IR.UMSU.REC.1397.223) were granted. Prior to the interviews, the participants were informed about their anonymity, confidentiality of their information, the research method and objectives, and their right to leave the study at will. The participants also signed informed consent forms.

Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Habibzadeh, H., Jasemi, M. & Hosseinzadegan, F. Social justice in health system; a neglected component of academic nursing education: a qualitative study. BMC Nurs 20 , 16 (2021). https://doi.org/10.1186/s12912-021-00534-1
Download citation
Received : 04 July 2020
Accepted : 02 January 2021
Published : 12 January 2021
DOI : https://doi.org/10.1186/s12912-021-00534-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Social justice
- Health equity
- Qualitative study
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity (2021)
Chapter: 5 the role of nurses in improving health equity, 5 the role of nurses in improving health equity.
Being a nurse … in 2020 must mean being aware of social injustices and the systemic racism that exist in much of nursing … and having a personal and professional responsibility to challenge and help end them.
—Calvin Moorley, RN, and colleagues, “Dismantling Structural Racism: Nursing Must Not Be Caught on the Wrong Side of History”
When this study was envisioned in 2019, it was clear that the future of nursing would look different by 2030; however, no one could predict how rapidly and dramatically circumstances would shift before the end of 2020. Over the coming decade, the nursing profession will continue to be shaped by the pressing health, social, and ethical challenges facing the nation today. Having illuminated many
of the health and social inequities affecting communities across the nation, the COVID-19 pandemic, along with other health crises, such as the opioid epidemic ( Abellanoza et al., 2018 ), presents an opportunity to take a critical look at the nursing profession, and society at large, and work collaboratively to enable all individuals to have a fair and just opportunity for health and well-being, reflecting the concept of “social mission” described by Mullan (2017, p. 122) as “making health not only better but fairer.” This chapter examines health equity and the role of nursing in its advancement in the United States.
As stated previously, health equity is defined as “the state in which everyone has the opportunity to attain full health potential and no one is disadvantaged from achieving this potential because of social position or any other socially defined circumstance” ( NASEM, 2017a , p. 32). While access to equitable health care, discussed in Chapter 4 , is an important part of achieving health equity, it is not sufficient. Health is affected by a wide range of other factors, including housing, transportation, nutrition, physical activity, education, income, laws and policies, and discrimination. Chapter 2 presents the Social Determinants of Health and Social Needs Model of Castrucci and Auerbach (2019) , in which upstream factors represent the social determinants of health (SDOH) that affect individuals and communities in a broad and, today, inequitable way. Low educational status and opportunity, income disparities, discrimination, and social marginalization are examples of upstream factors that impede good health outcomes. Midstream factors comprise social needs, or the individual factors that may affect a person’s health, such as homelessness, food insecurity, and trauma. Finally, downstream factors include disease treatment and chronic disease management.
Much of the focus on the education and training of nurses and the public perception of their role is on the treatment and management of disease. This chapter shifts that focus to nurses’ role in addressing SDOH and social needs, including their potential future roles and responsibilities in this regard, and describes existing exemplars. First, the chapter provides a brief overview of nurses’ role in addressing health equity. Next, it describes opportunities for nurses to improve health equity through four approaches: addressing social needs in clinical settings, addressing social needs and SDOH in the community, working across disciplines and sectors to meet multiple needs, and advocating for policy change. The chapter then details the opportunities and barriers associated with each of these approaches.
NURSES’ ROLE IN ADDRESSING HEALTH EQUITY
As described in Chapter 1 , the history of nursing is grounded in social justice and community health advocacy ( Donley and Flaherty, 2002 ; Pittman, 2019 ; Rafferty, 2015 ; Tyson et al., 2018 ), and as noted in Chapter 2 , the Code of Ethics for Nurses with Interpretive Statements, reiterated by American Nurses Association (ANA) President Ernest J. Grant in a public statement, “obligates nurses to be allies and to advocate and speak up against racism, discrimination, and injustice” ( ANA, 2020 ).
Addressing social needs across the health system can improve health equity from the individual to the system level. The report Integrating Social Care into the Delivery of Health Care identifies activities in five complementary areas that can facilitate the integration of social care into health care: adjustment, assistance, alignment, advocacy, and awareness ( NASEM, 2019 ) (see Figure 5-1 and Table 5-1 ). In
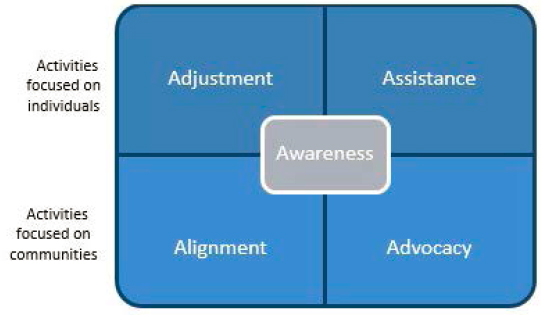
TABLE 5-1 Definitions of Areas of Activities That Strengthen Integration of Social Care into Health Care
SOURCE: NASEM, 2019 .
the area of awareness, for example, clinical nurses in a hospital setting can identify the fall risks their patients might face upon discharge and the assets they can incorporate into their lives to improve their health. In the area of adjustment, telehealth and/or home health and home visiting nurses can alter clinical care to reduce the risk of falls by, for example, helping patients to adjust risks in their homes and learn to navigate their environment. And these activities can continue to the high level of system change through advocacy for health policies aimed at altering community infrastructure to help prevent falls.
In short, improving population health entails challenging and changing the factors and institutions that give rise to health inequity through interventions and reforms that influence the institutions, social systems, and public policies that drive health ( Lantz, 2019 ). It is important to note, however, that there are shortcomings in how evaluations of health equity interventions are carried out (see Box 5-1 ).
ADDRESSING SOCIAL NEEDS IN CLINICAL SETTINGS
Although the provision of clinical care is a downstream determinant of health, the clinical setting presents an opportunity for nurses to address midstream determinants, or social needs, as well. Screening for social needs and making referrals to social services is becoming more commonplace in clinical settings as part of efforts to provide holistic care ( Gottlieb et al., 2016 ; Makelarski et al., 2017 ; Thomas-Henkel and Schulman, 2017 ). Nurses may conduct screenings; review their results; create care plans based on social needs as indicated by those results; refer patients to appropriate professionals and social services; and coordinate care by interfacing with social workers, community health workers, and social services providers. Although the importance of screening people for social needs has led more providers to take on this role, it has yet to become a universal practice ( CMS, 2020 ; NASEM, 2016 ), as most physician practices and hospitals do not perform screenings for the five key domains of social need 1 : food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence ( CMS, 2020 ; Fraze et al., 2019 ). As trusted professionals that spend significant time with patients and families, nurses are well equipped to conduct these screenings ( AHA, 2019 ). Federally qualified health centers (FQHCs)—community-based health centers that receive funds from the Health Resources and Services Administration’s (HRSA’s) Health Center Program—often screen for social needs.
In many clinical settings, however, challenges arise with screening for social needs. Individuals may be hesitant to provide information about such issues as housing or food insecurity, and technology is required to collect social needs data and once obtained, to share these data across settings and incorporate them into
___________________
1 These five domains of social needs are part of the Centers for Medicare & Medicaid Services’ Accountable Health Communities Model ( Fraze et al., 2019 ).
nursing practice in a meaningful way. While nurses have an educational foundation for building the skills needed to expand their role from assessing health issues to conducting assessments and incorporating findings related to social needs into care plans, this focus needs to be supported by policies where nurses are employed. As the incorporation of social needs into clinical consideration expands, nurses’ education and training will need to ensure knowledge of the impact of social needs and SDOH on individual and population health (see Chapter 7 ). Communicating appropriately with people about social needs can be difficult, and training is required to ensure that people feel comfortable responding to personal questions related to such issues as housing instability, domestic violence, and financial insecurity ( Thomas-Henkel and Schulman, 2017 ). Finally, the utility of social needs screening depends on networks of agencies that offer services and resources in the community. Without the ability to connect with relevant services, screenings and care plans can have little impact. Consequently, it is important for health care organizations to dedicate resources to ensuring that people are connected to appropriate resources, and to follow up by tracking those connections and offering other options as needed ( Thomas-Henkel and Schulman, 2017 ).
ADDRESSING SOCIAL NEEDS AND SOCIAL DETERMINANTS OF HEALTH IN THE COMMUNITY
While interest in and action to address social needs in the clinical setting is rapidly expanding, nurse engagement in these issues in community settings has been long-standing. Nurses serving in the community often work directly to address social needs at the individual and family levels, and often work as well to address SDOH at the community and population levels. Public health nurses in particular have broad knowledge of health issues and the associated SDOH, as well as needs and resources, at the community level. Embedded within the community, they also are well positioned to build trust and are respected among community leaders. Also playing important roles in addressing social needs within the community are home visiting nurses. At the individual and family levels, home visiting nurses often represent the first line of health care providers with sustained engagement in addressing social needs for many individuals. They recognize and act on the limitations associated with social needs, such as the inability to afford transportation, or may work with an interdisciplinary team at the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) clinic to address food issues and other social needs. By connecting with individuals in their neighborhoods and homes, public health and other community-based nurses promote health and well-being for families within communities and engage in this work with partners from across social, health, and other services.
At the population health level, public health nurses work to achieve health equity within communities through both health promotion and disease prevention and control. They often work in municipal and state health departments and apply
nursing, social, epidemiology, and other public health sciences in their contributions to population health ( Bigbee and Issel, 2012 ; IOM, 2011 [see AARP, 2010 ]; Larsen et al., 2018 ). They offer a wide range of services to individuals and community members and are engaged in activities ranging from policy development and coalition building to health teaching and case management ( Minnesota Department of Health, n.d. ). Public health nurses serve populations that include those with complex health and social needs, frail elderly, homeless individuals, teenage mothers, and those at risk for a specific disease ( Kulbok et al., 2012 ). Their interventions may target specific health risks, such as substance use disorder, HIV, and tobacco use, or populations at risk for health problems, such as individuals with complex health and social needs. Specific knowledge and skills they bring to communities include the ability to perform assessments of individual, family, and community health needs; use data and knowledge of environmental factors to plan for and respond to public health issues in their community; provide community and health department input in the development of policies and programs designed to improve the health of the community; implement evidence-based public health programs; and develop and manage program budgets ( Minnesota Department of Health, n.d. ).
Public health nursing roles are characterized by collaboration and partnerships with communities to address SDOH ( Kulbok et al., 2012 ). Core to public health nursing is working across disciplines and sectors to advance the health of populations through community organizing, coalition building, policy analysis, involvement in local city and county meetings, collaboration with state health departments, and social marketing ( Canales et al., 2018 ; Keller et al., 2004 ). Yet, while the work of public health nurses is foundational to the health of communities, their work is rarely visible. Additionally, regarding measurable reductions in health disparities, little research is available that connects directly and explicitly to public health nursing roles ( Davies and Donovan, 2016 ; Schaffer et al., 2015 ; Swider et al., 2017 ).
Recent experiences with H1N1, Ebola, Zika, and COVID-19 underscore the importance of having strong, well-connected, well-resourced social services, public health, and health care systems, matched by an adequate supply of well-educated nurses. A 2017 report from the National Academies of Sciences, Engineering, and Medicine focused on global health notes that when infectious disease outbreaks occur, significant costs are often associated with fear and the worried-well seeking care ( NASEM, 2017b ). In their role as trusted professionals, and given their widespread presence in communities, incorporating public health nurses into community, state, and federal government strategies for health education and dissemination of information can help extend the reach and impact of messaging during infectious disease outbreaks and other public health emergencies. Nurses can serve as expert sources of information (e.g., on preventing infectious disease transmission within their communities) ( Audain and Maher, 2017 ). In the United States, for example, as Zika infections were
identified and spreading, one of the strategies used by the U.S. Department of Health and Human Services (HHS) was to work through nursing associations to reach nurses and through them, help reach the public with factual information and minimize unnecessary resource use ( Minnesota Department of Health, 2019 ). Given their expertise in community engagement and knowledge of local and state government health and social services assets, public health nurses are well positioned to link to and share health-related information with community partners to help reach underresourced populations, including homeless individuals, non-English-speaking families, and others.
WORKING ACROSS DISCIPLINES AND SECTORS TO MEET MULTIPLE NEEDS
As nurses work in concert with other sectors and disciplines, interventions that address multiple and complex needs of individuals and communities can have far-reaching impacts on health outcomes and health care utilization. Through partnerships, community-based nurses work to address an array of health-related needs ranging from population-level diabetes management to community-based transportation to enable low-income families to access health care services.
Because multiple factors influence individual and population health, a multidisciplinary, multisectoral approach is necessary to improve health and reduce health inequity. While an approach focusing on only one SDOH may improve one dimension of health, such as food insecurity, intersectional approaches that simultaneously address complex, holistic needs of individuals, families, and communities are often required. Commonly found across underresourced communities are layers of intersecting challenges impacting health, ranging from adverse environmental exposures to food deserts. Health care systems, community-based organizations, government entitities, nurses, and others are increasingly working together to design interventions that reflect this complexity ( NASEM, 2017a , 2019 ). Creative alliances are being built with for-profit and not-for-profit organizations, community groups, federal programs, hospitals, lending institutions, technology companies, and others ( NASEM, 2019 ).
Work to prioritize and address health disparities and achieve health equity is predicated on meaningful, often multidimensional, assessments of community characteristics. One key opportunity to inform multisectoral efforts lies in community health needs assessments. The Patient Protection and Affordable Care Act requires nonprofit hospitals to conduct these assessments every 3 years, with input from local public health agencies. These assessments are then used to identify and prioritize significant health needs of the community served by the hospital while also identifying resources and plans for addressing these needs. Conducting a community health needs assessment is itself a multisectoral collaboration as it requires engaging community-based stakeholders ( Heath, 2018 ). The results of the assessment present opportunities for multiple sectors to work
together. For example, a hospital may partner with public health and area food banks to address food insecurity. Or it may partner with a health technology company and a local school board to address digital literacy for underserved youth and their families, and also extend the reach of broadband to support health care access through telehealth technology and strengthen digital literacy. In assessing the community’s health needs, these hospitals are required to obtain and consider community-based input, including input from individuals or organizations with knowledge of or expertise in public health. The reports produced as part of this process are required to be publicly available ( IRS, 2020 ).
These and other community engagement efforts can involve nurses from a variety of clinical and community-based settings in any and all steps of the process, from design to implementation and evaluation of the assessments themselves or the processes and programs established to address identified priorities. For example, the Magnet recognition program of the American Nurses Credentialing Center requires participating hospitals to involve nurses in their community health needs assessments ( ANCC, 2017 ).
A variety of models feature nurses directly addressing health and social needs through multidisciplinary, multisectoral collaboration. Two illustrative programs are described below: the Camden Core Model and Edge Runner.
Camden Core Model
The Camden Coalition, based in Camden, New Jersey, is a multidisciplinary, nonprofit organization that works across sectors to address health and social needs. The Coalition’s formation was based on the recognition that the U.S. health care system far too often fails people with complex health and social needs. These individuals cycle repeatedly through multiple health care, social services, and other systems without realizing lasting improvements in their health or well-being. The Coalition employs multiple approaches that include using faith-based partnerships to deliver health services and encourage healthy choices; sharing data among the criminal justice, health care, and housing sectors to identify points of intervention; and building local and national coalitions to support and educate others interested in implementing this model ( Camden Coalition, n.d. ). One of the Coalition’s best-known programs is the Camden Core Model. This nationally recognized care management intervention is an example of a nurse-led care management program for people with complex medical and social needs. It applies the principles of trauma-informed care and harm reduction with the aim of empowering people with the skills and support they need to avoid preventable hospital use and improve their well-being ( Finkelstein et al., 2020 ; Gawande, 2011 ). The model uses real-time data on hospital admissions to identify “superutilizers,” people with complex health issues who frequently use emergency care. An interprofessional team of registered nurses (RNs) and licensed practical nurses (LPNs), social workers, and community health workers engage in person
with these individuals to help them navigate their care by connecting them with medical care, government benefits, and social services ( Camden Coalition, n.d. ; Finkelstein et al., 2020 ). With federal funding, similar versions of the model have been extended to cities outside of Camden ( AF4Q, 2012 ; Crippen and Isasi, 2013 ; Mann, 2013 ).
Camden Coalition partnerships optimize the use of nurses in the community in several ways. An interprofessional team of nurses, social workers, and community health workers visits program participants, helps reconcile their medications, accompanies them to medical visits, and links them to social and legal services. Critical to the model’s success is recruiting nurses who are from the local community, capitalizing on their cultural and systems-level knowledge to facilitate and improve access to and utilization of local health and social services. The culture of the Camden Coalition model has been key to its success. The uniform commitment of nurses, staff, and leadership to addressing people’s complex needs has created a supportive work environment in which each team member’s role is optimized. Care Team members have accompanied people to their meetings and appointments for primary care, helped with applications for such public benefits as food stamps, provided referrals to social services and housing agencies, arranged for medication delivery in partnership with local pharmacies, and coordinated care among providers.
The Camden Coalition focuses on “authentic healing relationships,” defined as secure, genuine, and continuous partnerships between Care Team members and patients. This emphasis has evolved into a framework for patient engagement known as COACH, which stands for C onnect tasks with vision and priorities, O bserve the normal routine, A ssume a coaching style, C reate a backward plan, and H ighlight progress with data. An interprofessional team of nurses, social workers, and community health workers visits participants in the community. Team members are trained to problem solve with patients to achieve the program goals of helping them manage their chronic health conditions and reducing preventable hospital admissions.
Early evidence of the program’s effect in a small sample showed a 56 percent reduction in monthly hospital charges, a roughly 40 percent reduction in monthly visits to hospitals and emergency departments, and an approximately 52 percent increase in rates of reimbursement to care providers ( Green et al., 2010 ), although later evidence from a randomized controlled trial (RCT) indicated that the Camden Core Model did not reduce hospital readmissions ( Finkelstein et al., 2020 ). Other RCTs, conducted in Philadelphia and Chicago, showed that similar social care programs using case management and community health workers can reduce hospital admissions and save money in addition to improving health and quality of health care. Kangovi and colleagues (2018) conducted an RCT in Philadelphia to assess Individualized Management for Patient-Centered Targets (IMPaCT), a standardized community health worker intervention addressing unmet social needs across three health systems ( Kangovi et al., 2018 ). After 6 months, patients
in the intervention group compared with controls were more likely to report the highest quality of care and spent fewer total days in the hospital (reduced by about two-thirds), saving $2.47 for each dollar invested by Medicaid annually ( Kangovi et al., 2020 ). The RCT in Chicago assessed the effectiveness of a case management and housing program in reducing use of urgent medical services among homeless adults with chronic medical conditions and found a 29 percent reduction in hospitalizations and a 24 percent reduction in emergency department visits ( Sadowski et al., 2009 ).
Edge Runner
The American Academy of Nurses’ Edge Runner initiative identifies and promotes nurse-designed models of care and interventions that can improve health, increase health care access and quality, and/or reduce costs ( AAN, n.d.a ). As of February 2020, 59 such programs had been evaluated against a set of criteria and designated as part of this initiative. Many Edge Runner programs are built around the needs of underserved communities and seek to improve health through holistic care that addresses social needs and SDOH, including a range of upstream, midstream, and downstream determinants. Mason and colleagues (2015) assessed 30 Edge Runner models identified as of 2012, finding four main commonalities that illustrate these programs’ broad and encompassing approach to health.
A holistic definition of health. Across the programs, health was defined broadly to include physical, psychological, social, spiritual, functional, quality-of-life, personal happiness, and well-being aspects. Additionally, the definition of health was based on the values of clients and shaped around their preferences. Typically, programs were grounded in SDOH to inform their design of individual- and community-level interventions.
Individual-, family-, and community-centric design. Most programs prioritized individual, family, and community goals over provider-defined goals through a “participant-led care environment” and “meeting people where they are.” Thus, interventions were tailored to the values and culture present at each of these three levels.
Relationship-based care. The programs reflected the importance of building trusting relationships with individuals, families, and communities to help them engage in ways to create and sustain their own health.
Ongoing group and public health approaches to improving the health of underserved populations. The nurses who designed the programs viewed serving underserved populations as a moral imperative. Through peer-to-peer education, support groups, and public health approaches, they sought to empower clients, give them a sense of control, build self-care agency, and increase resilience.
An in-depth study of three Edge Runner programs (the Centering Pregnancy model, INSIGHTS, and the Family Practice and Counseling Network) revealed particular lessons: the essential role of collaboration and leaders who can col-
laborate with a wide range of stakeholders, the need for plans for scalability and financial sustainability, and the importance of social support and empowerment to help people ( Martsolf et al., 2017 ). In these and other models, the capacity and knowledge associated with building meaningful, sustained partnerships across sectors is a key dimension of nursing practice that impacts health equity. The Edge Runner programs emphasize how, in the pursuit of improving care, lowering costs, and increasing satisfaction for people and families, nurses are actively working to achieve person-centered care that addresses social needs and SDOH and focusing on the needs of underserved populations to promote health equity ( Martsolf et al., 2016 , 2017 ; Mason et al., 2015 ). However, evidence directly linking the programs to decreases in disparities is generally not available. Two examples of Edge Runner programs are described in Box 5-2 .
As models continue to evolve and be disseminated, it is critical to establish an evidence base that can help understand their impact on health and well-being and their contribution to achieving the broader aim of health equity. For care management programs incorporating social care, it is important to consider a broad array of both quantitative and qualitative measures beyond health care utilization ( Noonan, 2020 ). Although RCTs generate the most reliable evidence, this evidence can be limited in scope. For example, the RCTs cited above assessed neither the multidimensional nature of care management/social care models that might be reflected in such outcomes as client self-efficacy, satisfaction, or long-term health outcomes nor their potential social impacts. Also important to note is that care management models incorporating social care are limited by the availability of resources in the community, such as behavioral health services, addiction treatment, housing, and transportation. Programs that connect clients to health and social
services are unlikely to work if relevant services are unavailable ( Noonan, 2020 ). Important to underscore in the context of this report is that multisector engagement, as well as health care teams that may involve social workers, community health workers, physicians, and others engaging alongside nurses, all are oriented to a shared agenda focused on improving health and advancing health equity.
ADVOCATING FOR POLICY CHANGE
Public policies have a major influence on health care providers, systems, and the populations they serve. Accordingly, nurses can help promote health equity by bringing a health lens to bear on public policies and decision making at the community, state, and federal levels. Informing health-related public policy can involve communicating about health disparities and SDOH with the public, policy makers, and organizational leaders, focusing on both challenges and solutions for addressing health through actions targeted to achieving health equity.
When nurses engage with policy change as an upstream determinant of health, they can have a powerful and far-reaching impact on the health of populations. In the National Academy of Medicine’s Vital Directions series, Nancy Adler and colleagues (2016) note that “powerful drivers of health lie outside the conventional medical care delivery system…. Health policies need to expand to address factors outside the medical system that promote or damage health.” Because health inequities and SDOH are based in social structures and policies, efforts to address them upstream as the root of poor health among certain populations and communities need to focus on policy change ( NASEM, 2017a ). Nurses alone cannot solve the problems associated with upstream SDOH that exist outside of health care systems. However, by engaging in efforts aimed at changing local, state, or federal policy with a Health in All Policies approach, 2 they can address SDOH that underlie poor health ( IOM, 2011 ; NASEM, 2017a ; Williams et al., 2018 ). Whether nurses engage in policy making full time or work to inform policy part time as a professional responsibility, their attention to policies that either create or eliminate health inequities can improve the underlying conditions that frame people’s health. Nurses can bring a health and social justice lens to public policies and decision making at the community, state, and federal levels most effectively by serving in public- and private-sector leadership positions. Much of this work is discussed in Chapter 9 on nursing leadership, but it is noted in this chapter given the substantial
2 Health in All Policies (HiAP) is a collaborative approach that integrates health considerations into policy making across sectors. It recognizes that health is created by a multitude of factors beyond health care and in many cases, beyond the scope of traditional public health activities. In accordance with HiAP, for example, decision makers in the health care sector should consider transportation, education, housing, commerce, and other sectors impacting communities. HiAP stresses the need to work across government agencies and with private partners from these different sectors to achieve healthy and safe communities. It also encourages partnerships between the health care sector and community developers, for example ( CDC, 2016 ).
influence that policy decisions have on health equity. Nurses can and should use their expertise to promote policies that support health equity.
For example, a nurse in Delaware was influential in getting the state’s legislature to pass legislation to implement a colorectal cancer screening program that has increased access to care and reduced disparities in morbidity and mortality from colorectal cancer (see Box 5-3 ). While individual nurses, often through their workplace and professional associations, engage in upstream efforts to impact health equity, there have been repeated calls from within the nursing community for more nurses to engage in informing public policy to improve health outcomes for individuals and populations.
CONCLUSIONS
In the coming decade, the United States will make substantial progress in achieving health equity only if it devotes resources and attention to addressing the adverse effects of SDOH on the health of underresourced populations. As 2030 approaches, numerous initiatives to address health equity are likely to be launched at the local, state, and national levels. Many of these initiatives will focus on health care equity. Yet, while expanding access to quality care is critical to reducing disparities and improving health outcomes, such efforts need to be accompanied by additional efforts to identify and change the social institutions, dynamics, and systems underlying health inequities from the local to the national level. Nurses can contribute to reshaping the landscape of health equity over the coming decade by serving in expanded roles, working in new settings and new ways, and partnering with communities and other sectors beyond health care. Some nurses are already working in roles and settings that support health equity and are engaged in educating about and advocating for health equity through their professional associations. Nonetheless, broader engagement as a core activity of every nurse will help advance health equity nationwide. To achieve this aim will require
- support for and the willingness of the nursing workforce to take on new roles in new settings in the community;
- consistency in nurses’ preparation for engaging in downstream, midstream, and upstream strategies aimed at improving health equity by addressing issues that compromise health, such as geographic disparities, poverty, racism, homelessness, trauma, drug abuse, and behavioral health conditions;
- more experiential learning and opportunities to work in community settings throughout nursing education to ensure that nurses have skills and competencies to address individuals’ complex needs and promote efforts to improve the well-being of communities;
- nursing education that goes beyond teaching the principles of diversity, equity, and inclusion to provide sustained student engagement in hands-on community and clinical experiences with these issues;
- funding to support new models of care and functions that address SDOH, health equity, and population health; and
- evaluation of models to build the evidence needed to scale programs and the policies and resources necessary to sustain them.
These issues are discussed in the chapters that follow. Programs described in this chapter, such as the Camden Coalition and the Edge Runner initiatives, are exemplars of the kind of multidisciplinary, multisector efforts that will be necessary to address the complex needs of individuals and communities and make a lasting impact by eliminating health disparities, with the goal of achieving health equity. Central to these future efforts, however, are parallel efforts that evaluate
and provide the evidence base on which to determine the effectiveness of models. One of the greatest challenges this committee faced was finding evidence directly linking the efforts of nurses to address social needs and SDOH to reductions in health disparities that would signal improved population health outcomes and health equity. Such evidence is essential to informing payment policy decisions that can ensure the sustainability of and nurse engagement in these models (discussed further in Chapter 6 ). Through evidence, the nursing profession can leverage its own potential, and the public, other professionals, and other sectors can understand the impact and value of such nursing engagement.
Conclusion 5-1: Nurses are in a position to improve outcomes for the underserved and can work to address the structural and institutional factors that produce health disparities in the first place.
Conclusion 5-2: Nurses can use their unique expertise and perspective to help develop and advocate for policies and programs that promote health equity.
AAN (American Academy of Nursing). n.d.a. Transforming America’s health system through nursing solutions . https://www.aannet.org/initiatives/edge-runners (accessed November 3, 2020).
AAN. n.d.b. ¡Cuídate!: A culturally-based program to reduce sexual risk behavior among Latino youth . https://www.aannet.org/initiatives/edge-runners/profiles/edge-runners--cuidate (accessed November 3, 2020).
AAN. n.d.c. Insights into children’s temperament: Supporting the development of low-income children . https://www.aannet.org/initiatives/edge-runners/profiles/edge-runners--insights-into-childrens-temperament (accessed November 3, 2020).
AARP. 2010. Preparation and roles of nursing care providers in America. http://championnursing.org/resources/preparation-and-roles-nursing-care-providers-america (accessed June 3, 2021).
Abellanoza, A., N. Provenzano-Hass, and R. J. Gatchel. 2018. Burnout in ER nurses: Review of the literature and interview themes. Journal of Applied Biobehavioral Research 23(1):e12117.
Adler, N. E., M. M. Glymour, and J. Fielding. 2016. Addressing social determinants of health and health inequalities. Journal of the American Medical Association 316(16):1641–1642.
AF4Q (Aligning Forces for Quality). 2012. Expanding “hot spotting” to new communities . http://forces4quality.org/node/5182.html (accessed November 3, 2020).
Agurs-Collins, T., S. Persky, E. D. Paskett, S. L. Barkin, H. I. Meissner, T. R. Nansel, S. S. Arteaga, X. Zhang, R. Das, and T. Farhat. 2019. Designing and assessing multilevel interventions to improve minority health and reduce health disparities. American Journal of Public Health 109(S1):S86–S93.
AHA (American Hospital Association). 2019. Screening for social needs: Guiding care teams to engage patients. Chicago, IL: American Hospital Association.
ANA (American Nurses Association). 2020. ANA president condemns racism, brutality and senseless violence against black communities . https://www.nursingworld.org/news/news-releases/2020/ana-president-condemns-racism-brutality-and-senseless-violence-against-black-communities (accessed September 17, 2020).
ANCC (American Nurses Credentialing Center). 2017. 2019 Magnet ® application manual. Silver Spring, MD: American Nurses Credentialing Center.
Audain, G., and C. Maher. 2017. Prevention and control of worldwide mosquito-borne illnesses: Nurses as teachers. Online Journal of Issues in Nursing 22(1):5.
Bigbee, J. L., and L. M. Issel. 2012. Conceptual models for population-focused public health nursing interventions and outcomes: The state of the art. Public Health Nursing 29(4):370–379.
Braveman, P., E. Arkin, T. Orleans, D. Proctor, and A. Plough. 2017. What is health equity? And what difference does a definition make? Princeton, NJ: Robert Wood Johnson Foundation.
Bridge, J. A., L. Asti, L. M. Horowitz, J. B. Greenhouse, C. A. Fontanella, A. H. Sheftall, K. J. Kelleher, and J. V. Campo. 2015. Suicide trends among elementary school–aged children in the United States from 1993 to 2012. JAMA Pediatrics 169(7):673–677.
Brown, A. F., G. X. Ma, J. Miranda, E. Eng, D. Castille, T. Brockie, P. Jones, C. O. Airhihenbuwa, T. Farhat, L. Zhu, and C. Trinh-Shevrin. 2019. Structural interventions to reduce and eliminate health disparities. American Journal of Public Health 109(S1):S72–S78.
Camden Coalition. n.d. Camden core model . https://camdenhealth.org/care-interventions/camden-core-model (accessed November 4, 2020).
Canales, M. K., D. J. Drevdahl, and S. M. Kneipp. 2018. Letter to the editor: Public health nursing. Nursing Outlook 66(2):110–111.
Castrucci, B., and J. Auerbach. 2019. Meeting individual social needs falls short of addressing social determinants of health. Health Affairs Blog . doi: 10.1377/hblog20190115.234942.
CDC (Centers for Disease Control and Prevention). 2016. Health in all policies . https://www.cdc.gov/policy/hiap/index.html (accessed June 2, 2021).
CMS (Centers for Medicare & Medicaid Services). 2020. Z codes utilization among Medicare fee-for-service (FFS) beneficiaries in 2017. Baltimore, MD: Centers for Medicare & Medicaid Services Office of Minority Health.
Crippen, D., and F. Isasi. 2013. The untold story of 2013: Governors lead in health care transformation. Health Affairs Blog . https://www.healthaffairs.org/do/10.1377/hblog20131217.035878/full (accessed June 2, 2021).
Davies, N., and H. Donovan. 2016. National survey of commissioners’ and service planners’ views of public health nursing in the UK. Public Health 141:218–221.
Donley, R., and M. J. Flaherty. 2002. Revisiting the American Nurses Association’s first position on education for nurses. Online Journal of Issues in Nursing 7(2):2.
Duran, D., Y. Asada, J. Millum, and M. Gezmu. 2019. Harmonizing health disparities measurement. American Journal of Public Health 109(S1):S25–S27.
Dye, B. A., D. G. Duran, D. M. Murray, J. W. Creswell, P. Richard, T. Farhat, N. Breen, and M. M. Engelgau. 2019. The importance of evaluating health disparities research. American Journal of Public Health 109(S1):S34–S40.
Finkelstein, A., A. Zhou, S. Taubman, and J. Doyle. 2020. Health care hotspotting—A randomized, controlled trial. New England Journal of Medicine 382(2):152–162.
Fraze, T. K., A. L. Brewster, V. A. Lewis, L. B. Beidler, G. F. Murray, and C. H. Colla. 2019. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by us physician practices and hospitals. JAMA Network Open 2(9):e1911514.
Gawande, A. 2011 (January 24). The hot spotters . https://www.newyorker.com/magazine/2011/01/24/the-hot-spotters (accessed October 14, 2020).
Gottlieb, L. M., D. Hessler, D. Long, E. Laves, A. R. Burns, A. Amaya, P. Sweeney, C. Schudel, and N. E. Adler. 2016. Effects of social needs screening and in-person service navigation on child health: A randomized clinical trial. JAMA Pediatrics 170(11):e162521.
Green, S. R., V. Singh, and W. O’Byrne. 2010. Hope for New Jersey’s city hospitals: The Camden initiative. Perspectives in Health Information Management 7(Spring):1d.
Grubbs, S. S., B. N. Polite, J. Carney, Jr., W. Bowser, J. Rogers, N. Katurakes, P. Hess, and E. D. Paskett. 2013. Eliminating racial disparities in colorectal cancer in the real world: It took a village. Journal of Clinical Oncology 31(16):1928–1930.
Healthy Delaware. 2020. Welcome Consortium Members and Partners . https://www.healthydelaware.org/Consortium (accessed November 3, 2020).
Heath, S. 2018. 3 things to know to conduct a community health needs assessment . https://patientengagementhit.com/news/3-things-to-know-to-conduct-a-community-health-needs-assessment (accessed October 6, 2020).
IOM (Institute of Medicine). 2011. The future of nursing: Leading change, advancing health . Washington, DC: The National Academies Press.
IRS (Internal Revenue Service). 2020. Community health needs assessment for charitable hospital organizations-Section 501(r)(3) . https://www.irs.gov/charities-non-profits/community-health-needs-assessment-for-charitable-hospital-organizations-section-501r3 (accessed June 2, 2021).
Jones, N. L., N. Breen, R. Das, T. Farhat, and R. Palmer. 2019. Cross-cutting themes to advance the science of minority health and health disparities. American Journal of Public Health 109(S1):S21–S24.
Kangovi, S., N. Mitra, L. Norton, R. Harte, X. Zhao, T. Carter, D. Grande, and J. A. Long. 2018. Effect of community health worker support on clinical outcomes of low-income patients across primary care facilities: A randomized clinical trial. JAMA Internal Medicine 178(12):1635–1643.
Kangovi, S., N. Mitra, D. Grande, J. Long, and D. Asch. 2020. Evidence-based community health worker program addresses unmet social needs and generates positive return on investment. Health Affairs 39(2). doi: 10.1377/hlthaff.2019.00981.
Keller, L. O., S. Strohschein, M. A. Schaffer, and B. Lia-Hoagberg. 2004. Population-based public health interventions: Innovations in practice, teaching, and management. Part II. Public Health Nursing 21(5):469–487.
Krist, A. H., T. A. Wolff, D. E. Jonas, R. P. Harris, M. L. LeFevre, A. R. Kemper, C. M. Mangione, C.-W. Tseng, and D. C. Grossman. 2018. Update on the methods of the U.S. Preventive Services task force: Methods for understanding certainty and net benefit when making recommendations. American Journal of Preventive Medicine 54(1 Suppl 1):S11–S18.
Kulbok, P. A., E. Thatcher, E. Park, and P. S. Meszaros. 2012. Evolving public health nursing roles: Focus on community participatory health promotion and prevention. Online Journal of Issues in Nursing 17(2):1.
Lantz, P. M. 2019. The medicalization of population health: Who will stay upstream? Milbank Quarterly 97(1):36–39.
Larsen, R., J. Ashley, T. Ellens, R. Frauendienst, K. Jorgensen-Royce, and M. Zelenak. 2018. Development of a new graduate public health nurse residency program using the core competencies of public health nursing. Public Health Nursing 35(6):606–612.
Makelarski, J. A., E. Abramsohn, J. H. Benjamin, S. Du, and S. T. Lindau. 2017. Diagnostic accuracy of two food insecurity screeners recommended for use in health care settings. American Journal of Public Health 107(11):1812–1817.
Mann, C. 2013. CMCS informational bulletin: Targeting Medicaid super-utilizers to decrease costs and improve quality. Baltimore, MD: Centers for Medicare & Medicaid Services.
Martsolf, G. R., T. Gordon, L. Warren May, D. Mason, C. Sullivan, and A. Villarruel. 2016. Innovative nursing care models and culture of health: Early evidence. Nursing Outlook 64(4):367–376.
Martsolf, G. R., D. J. Mason, J. Sloan, C. G. Sullivan, and A. M. Villarruel. 2017. Nurse-designed care models: What can they tell us about advancing a culture of health? Santa Monica, CA: RAND Corporation.
Mason, D. J., D. A. Jones, C. Roy, C. G. Sullivan, and L. J. Wood. 2015. Commonalities of nurse-designed models of health care. Nursing Outlook 63(5):540–553.
Minnesota Department of Health. 2019. Public health interventions: Applications for public health nursing practice , 2nd ed. St. Paul, MN: Minnesota Department of Health.
Minnesota Department of Health. n.d. Public health nurse orientation and resource guide . https://www.health.state.mn.us/communities/practice/ta/phnconsultants/guide-phn.html (accessed October 5, 2020).
Mullan, F. 2017. Social mission in health professions education: Beyond flexner. Journal of the American Medical Association 318(2):122–123.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2016. Accounting for social risk factors in Medicare payment: Identifying social risk factors . Washington, DC: The National Academies Press.
NASEM. 2017a. Communities in action: Pathways to health equity . Washington, DC: The National Academies Press.
NASEM. 2017b. Global health and the future role of the United States . Washington, DC: The National Academies Press.
NASEM. 2019. Integrating social care into the delivery of health care: Moving upstream to improve the nation’s health . Washington, DC: The National Academies Press.
Noonan, K. 2020. Disappointing randomized controlled trial results show a way forward on complex care in Camden and beyond. Health Affairs Blog . doi: 10.1377/hblog20200102.864819.
Pittman, P. 2019. Rising to the challenge: Re-embracing the Wald model of nursing. American Journal of Nursing 119(7):46–52.
Rafferty, A. M. 2015 (January 27). Reinventing nursing’s social mission . Video. https://www.youtube.com/watch?v=8PjoiO8v-dE (accessed September 6, 2020).
Sadowski, L. S., R. A. Kee, T. J. VanderWeele, and D. Buchanan. 2009. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: A randomized trial. Journal of the American Medical Association 301(17):1771–1778.
Schaffer, M. A., L. O. Keller, and D. Reckinger. 2015. Public health nursing activities: Visible or invisible? Public Health Nursing 32(6):711–720.
Swider, S. M., P. F. Levin, and V. Reising. 2017. Evidence of public health nursing effectiveness: A realist review. Public Health Nursing 34(4):324–334.
Thomas-Henkel, C., and M. Schulman. 2017. Screening for social determinants of health in populations with complex needs: Implementation considerations. Trenton, NJ: Center for Health Care Strategies.
Tyson, T., C. J. Kenon, Jr., and K. Nance. 2018. Nursing at historically black colleges and universities. Journal of Professional Nursing 34(3):167–170.
Williams, D. R., and V. Purdie-Vaughns. 2016. Needed interventions to reduce racial/ethnic disparities in health. Journal of Health Politics, Policy and Law 41(4):627–651.
Williams, S. D., J. M. Phillips, and K. Koyama. 2018. Nurse advocacy: Adopting a health in all policies approach. Online Journal of Issues in Nursing 23(3).
Woolf, S. H., J. Q. Purnell, S. M. Simon, E. B. Zimmerman, G. J. Camberos, A. Haley, and R. P. Fields. 2015. Translating evidence into population health improvement: Strategies and barriers. Annual Review of Public Health 36(1):463–482.
This page intentionally left blank.
The decade ahead will test the nation's nearly 4 million nurses in new and complex ways. Nurses live and work at the intersection of health, education, and communities. Nurses work in a wide array of settings and practice at a range of professional levels. They are often the first and most frequent line of contact with people of all backgrounds and experiences seeking care and they represent the largest of the health care professions.
A nation cannot fully thrive until everyone - no matter who they are, where they live, or how much money they make - can live their healthiest possible life, and helping people live their healthiest life is and has always been the essential role of nurses. Nurses have a critical role to play in achieving the goal of health equity, but they need robust education, supportive work environments, and autonomy. Accordingly, at the request of the Robert Wood Johnson Foundation, on behalf of the National Academy of Medicine, an ad hoc committee under the auspices of the National Academies of Sciences, Engineering, and Medicine conducted a study aimed at envisioning and charting a path forward for the nursing profession to help reduce inequities in people's ability to achieve their full health potential. The ultimate goal is the achievement of health equity in the United States built on strengthened nursing capacity and expertise. By leveraging these attributes, nursing will help to create and contribute comprehensively to equitable public health and health care systems that are designed to work for everyone.
The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity explores how nurses can work to reduce health disparities and promote equity, while keeping costs at bay, utilizing technology, and maintaining patient and family-focused care into 2030. This work builds on the foundation set out by The Future of Nursing: Leading Change, Advancing Health (2011) report.
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on the Future of Nursing 2020–2030; Flaubert JL, Le Menestrel S, Williams DR, et al., editors. The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. Washington (DC): National Academies Press (US); 2021 May 11.

The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity.
- Hardcopy Version at National Academies Press
5 The Role of Nurses in Improving Health Equity
Being a nurse … in 2020 must mean being aware of social injustices and the systemic racism that exist in much of nursing … and having a personal and professional responsibility to challenge and help end them. —Calvin Moorley, RN, and colleagues, “Dismantling Structural Racism: Nursing Must Not Be Caught on the Wrong Side of History”
Health equity is achieved when everyone has a fair and just opportunity to be as healthy as possible. Nurses are well positioned to play a major role in addressing the underlying causes of poor health by understanding and recognizing the wide range of factors that influence how well and long people live, helping to create individual- and community-targeted solutions, and facilitating and working with interdisciplinary and multisector teams and partners to implement those solutions. Nurses have the potential to reshape the landscape of health equity over the next decade by expanding their roles, working in new settings and in new ways, and markedly expanding efforts to partner with communities and other sectors. But for the United States to make substantial progress in achieving health equity, it will need to devote resources and attention to the conditions that affect people’s health and make expanded investments in building nurse capacity. And nursing schools will need to shift education, training, and mindsets to support nurses’ new and expanded roles.
When this study was envisioned in 2019, it was clear that the future of nursing would look different by 2030; however, no one could predict how rapidly and dramatically circumstances would shift before the end of 2020. Over the coming decade, the nursing profession will continue to be shaped by the pressing health, social, and ethical challenges facing the nation today. Having illuminated many of the health and social inequities affecting communities across the nation, the COVID-19 pandemic, along with other health crises, such as the opioid epidemic ( Abellanoza et al., 2018 ), presents an opportunity to take a critical look at the nursing profession, and society at large, and work collaboratively to enable all individuals to have a fair and just opportunity for health and well-being, reflecting the concept of “social mission” described by Mullan (2017 , p. 122) as “making health not only better but fairer.” This chapter examines health equity and the role of nursing in its advancement in the United States.
As stated previously, health equity is defined as “the state in which everyone has the opportunity to attain full health potential and no one is disadvantaged from achieving this potential because of social position or any other socially defined circumstance” ( NASEM, 2017a , p. 32). While access to equitable health care, discussed in Chapter 4 , is an important part of achieving health equity, it is not sufficient. Health is affected by a wide range of other factors, including housing, transportation, nutrition, physical activity, education, income, laws and policies, and discrimination. Chapter 2 presents the Social Determinants of Health and Social Needs Model of Castrucci and Auerbach (2019) , in which upstream factors represent the social determinants of health (SDOH) that affect individuals and communities in a broad and, today, inequitable way. Low educational status and opportunity, income disparities, discrimination, and social marginalization are examples of upstream factors that impede good health outcomes. Midstream factors comprise social needs, or the individual factors that may affect a person’s health, such as homelessness, food insecurity, and trauma. Finally, downstream factors include disease treatment and chronic disease management.
Much of the focus on the education and training of nurses and the public perception of their role is on the treatment and management of disease. This chapter shifts that focus to nurses’ role in addressing SDOH and social needs, including their potential future roles and responsibilities in this regard, and describes existing exemplars. First, the chapter provides a brief overview of nurses’ role in addressing health equity. Next, it describes opportunities for nurses to improve health equity through four approaches: addressing social needs in clinical settings, addressing social needs and SDOH in the community, working across disciplines and sectors to meet multiple needs, and advocating for policy change. The chapter then details the opportunities and barriers associated with each of these approaches.
NURSES’ ROLE IN ADDRESSING HEALTH EQUITY
As described in Chapter 1 , the history of nursing is grounded in social justice and community health advocacy ( Donley and Flaherty, 2002 ; Pittman, 2019 ; Rafferty, 2015 ; Tyson et al., 2018 ), and as noted in Chapter 2 , the Code of Ethics for Nurses with Interpretive Statements, reiterated by American Nurses Association (ANA) President Ernest J. Grant in a public statement, “obligates nurses to be allies and to advocate and speak up against racism, discrimination, and injustice” ( ANA, 2020 ).
Addressing social needs across the health system can improve health equity from the individual to the system level. The report Integrating Social Care into the Delivery of Health Care identifies activities in five complementary areas that can facilitate the integration of social care into health care: adjustment, assistance, alignment, advocacy, and awareness ( NASEM, 2019 ) (see Figure 5-1 and Table 5-1 ). In the area of awareness, for example, clinical nurses in a hospital setting can identify the fall risks their patients might face upon discharge and the assets they can incorporate into their lives to improve their health. In the area of adjustment, telehealth and/or home health and home visiting nurses can alter clinical care to reduce the risk of falls by, for example, helping patients to adjust risks in their homes and learn to navigate their environment. And these activities can continue to the high level of system change through advocacy for health policies aimed at altering community infrastructure to help prevent falls.
Areas of activity that strengthen integration of social care into health care. SOURCE: NASEM, 2019.
Definitions of Areas of Activities That Strengthen Integration of Social Care into Health Care.
In short, improving population health entails challenging and changing the factors and institutions that give rise to health inequity through interventions and reforms that influence the institutions, social systems, and public policies that drive health ( Lantz, 2019 ). It is important to note, however, that there are shortcomings in how evaluations of health equity interventions are carried out (see Box 5-1 ).
Shortcomings of Evaluations of Health Equity Interventions.
- ADDRESSING SOCIAL NEEDS IN CLINICAL SETTINGS
Although the provision of clinical care is a downstream determinant of health, the clinical setting presents an opportunity for nurses to address midstream determinants, or social needs, as well. Screening for social needs and making referrals to social services is becoming more commonplace in clinical settings as part of efforts to provide holistic care ( Gottlieb et al., 2016 ; Makelarski et al., 2017 ; Thomas-Henkel and Schulman, 2017 ). Nurses may conduct screenings; review their results; create care plans based on social needs as indicated by those results; refer patients to appropriate professionals and social services; and coordinate care by interfacing with social workers, community health workers, and social services providers. Although the importance of screening people for social needs has led more providers to take on this role, it has yet to become a universal practice ( CMS, 2020 ; NASEM, 2016 ), as most physician practices and hospitals do not perform screenings for the five key domains of social need 1 : food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence ( CMS, 2020 ; Fraze et al., 2019 ). As trusted professionals that spend significant time with patients and families, nurses are well equipped to conduct these screenings ( AHA, 2019 ). Federally qualified health centers (FQHCs)—community-based health centers that receive funds from the Health Resources and Services Administration’s (HRSA’s) Health Center Program—often screen for social needs.
In many clinical settings, however, challenges arise with screening for social needs. Individuals may be hesitant to provide information about such issues as housing or food insecurity, and technology is required to collect social needs data and once obtained, to share these data across settings and incorporate them into nursing practice in a meaningful way. While nurses have an educational foundation for building the skills needed to expand their role from assessing health issues to conducting assessments and incorporating findings related to social needs into care plans, this focus needs to be supported by policies where nurses are employed. As the incorporation of social needs into clinical consideration expands, nurses’ education and training will need to ensure knowledge of the impact of social needs and SDOH on individual and population health (see Chapter 7 ). Communicating appropriately with people about social needs can be difficult, and training is required to ensure that people feel comfortable responding to personal questions related to such issues as housing instability, domestic violence, and financial insecurity ( Thomas-Henkel and Schulman, 2017 ). Finally, the utility of social needs screening depends on networks of agencies that offer services and resources in the community. Without the ability to connect with relevant services, screenings and care plans can have little impact. Consequently, it is important for health care organizations to dedicate resources to ensuring that people are connected to appropriate resources, and to follow up by tracking those connections and offering other options as needed ( Thomas-Henkel and Schulman, 2017 ).
- ADDRESSING SOCIAL NEEDS AND SOCIAL DETERMINANTS OF HEALTH IN THE COMMUNITY
While interest in and action to address social needs in the clinical setting is rapidly expanding, nurse engagement in these issues in community settings has been long-standing. Nurses serving in the community often work directly to address social needs at the individual and family levels, and often work as well to address SDOH at the community and population levels. Public health nurses in particular have broad knowledge of health issues and the associated SDOH, as well as needs and resources, at the community level. Embedded within the community, they also are well positioned to build trust and are respected among community leaders. Also playing important roles in addressing social needs within the community are home visiting nurses. At the individual and family levels, home visiting nurses often represent the first line of health care providers with sustained engagement in addressing social needs for many individuals. They recognize and act on the limitations associated with social needs, such as the inability to afford transportation, or may work with an interdisciplinary team at the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) clinic to address food issues and other social needs. By connecting with individuals in their neighborhoods and homes, public health and other community-based nurses promote health and well-being for families within communities and engage in this work with partners from across social, health, and other services.
At the population health level, public health nurses work to achieve health equity within communities through both health promotion and disease prevention and control. They often work in municipal and state health departments and apply nursing, social, epidemiology, and other public health sciences in their contributions to population health ( Bigbee and Issel, 2012 ; IOM, 2011 [see AARP, 2010 ]; Larsen et al., 2018 ). They offer a wide range of services to individuals and community members and are engaged in activities ranging from policy development and coalition building to health teaching and case management ( Minnesota Department of Health, n.d. ). Public health nurses serve populations that include those with complex health and social needs, frail elderly, homeless individuals, teenage mothers, and those at risk for a specific disease ( Kulbok et al., 2012 ). Their interventions may target specific health risks, such as substance use disorder, HIV, and tobacco use, or populations at risk for health problems, such as individuals with complex health and social needs. Specific knowledge and skills they bring to communities include the ability to perform assessments of individual, family, and community health needs; use data and knowledge of environmental factors to plan for and respond to public health issues in their community; provide community and health department input in the development of policies and programs designed to improve the health of the community; implement evidence-based public health programs; and develop and manage program budgets ( Minnesota Department of Health, n.d. ).
Public health nursing roles are characterized by collaboration and partnerships with communities to address SDOH ( Kulbok et al., 2012 ). Core to public health nursing is working across disciplines and sectors to advance the health of populations through community organizing, coalition building, policy analysis, involvement in local city and county meetings, collaboration with state health departments, and social marketing ( Canales et al., 2018 ; Keller et al., 2004 ). Yet, while the work of public health nurses is foundational to the health of communities, their work is rarely visible. Additionally, regarding measurable reductions in health disparities, little research is available that connects directly and explicitly to public health nursing roles ( Davies and Donovan, 2016 ; Schaffer et al., 2015 ; Swider et al., 2017 ).
Recent experiences with H1N1, Ebola, Zika, and COVID-19 underscore the importance of having strong, well-connected, well-resourced social services, public health, and health care systems, matched by an adequate supply of well-educated nurses. A 2017 report from the National Academies of Sciences, Engineering, and Medicine focused on global health notes that when infectious disease outbreaks occur, significant costs are often associated with fear and the worried-well seeking care ( NASEM, 2017b ). In their role as trusted professionals, and given their widespread presence in communities, incorporating public health nurses into community, state, and federal government strategies for health education and dissemination of information can help extend the reach and impact of messaging during infectious disease outbreaks and other public health emergencies. Nurses can serve as expert sources of information (e.g., on preventing infectious disease transmission within their communities) ( Audain and Maher, 2017 ). In the United States, for example, as Zika infections were identified and spreading, one of the strategies used by the U.S. Department of Health and Human Services (HHS) was to work through nursing associations to reach nurses and through them, help reach the public with factual information and minimize unnecessary resource use (Minnesota Department of Health, 2019 ). Given their expertise in community engagement and knowledge of local and state government health and social services assets, public health nurses are well positioned to link to and share health-related information with community partners to help reach underresourced populations, including homeless individuals, non-English-speaking families, and others.
- WORKING ACROSS DISCIPLINES AND SECTORS TO MEET MULTIPLE NEEDS
As nurses work in concert with other sectors and disciplines, interventions that address multiple and complex needs of individuals and communities can have far-reaching impacts on health outcomes and health care utilization. Through partnerships, community-based nurses work to address an array of health-related needs ranging from population-level diabetes management to community-based transportation to enable low-income families to access health care services.
Because multiple factors influence individual and population health, a multidisciplinary, multisectoral approach is necessary to improve health and reduce health inequity. While an approach focusing on only one SDOH may improve one dimension of health, such as food insecurity, intersectional approaches that simultaneously address complex, holistic needs of individuals, families, and communities are often required. Commonly found across underresourced communities are layers of intersecting challenges impacting health, ranging from adverse environmental exposures to food deserts. Health care systems, community-based organizations, government entitities, nurses, and others are increasingly working together to design interventions that reflect this complexity ( NASEM, 2017a , 2019 ). Creative alliances are being built with for-profit and not-for-profit organizations, community groups, federal programs, hospitals, lending institutions, technology companies, and others ( NASEM, 2019 ).
Work to prioritize and address health disparities and achieve health equity is predicated on meaningful, often multidimensional, assessments of community characteristics. One key opportunity to inform multisectoral efforts lies in community health needs assessments. The Patient Protection and Affordable Care Act requires nonprofit hospitals to conduct these assessments every 3 years, with input from local public health agencies. These assessments are then used to identify and prioritize significant health needs of the community served by the hospital while also identifying resources and plans for addressing these needs. Conducting a community health needs assessment is itself a multisectoral collaboration as it requires engaging community-based stakeholders ( Heath, 2018 ). The results of the assessment present opportunities for multiple sectors to work together. For example, a hospital may partner with public health and area food banks to address food insecurity. Or it may partner with a health technology company and a local school board to address digital literacy for underserved youth and their families, and also extend the reach of broadband to support health care access through telehealth technology and strengthen digital literacy. In assessing the community’s health needs, these hospitals are required to obtain and consider community-based input, including input from individuals or organizations with knowledge of or expertise in public health. The reports produced as part of this process are required to be publicly available ( IRS, 2020 ).
These and other community engagement efforts can involve nurses from a variety of clinical and community-based settings in any and all steps of the process, from design to implementation and evaluation of the assessments themselves or the processes and programs established to address identified priorities. For example, the Magnet recognition program of the American Nurses Credentialing Center requires participating hospitals to involve nurses in their community health needs assessments ( ANCC, 2017 ).
A variety of models feature nurses directly addressing health and social needs through multidisciplinary, multisectoral collaboration. Two illustrative programs are described below: the Camden Core Model and Edge Runner.
Camden Core Model
The Camden Coalition, based in Camden, New Jersey, is a multidisciplinary, nonprofit organization that works across sectors to address health and social needs. The Coalition’s formation was based on the recognition that the U.S. health care system far too often fails people with complex health and social needs. These individuals cycle repeatedly through multiple health care, social services, and other systems without realizing lasting improvements in their health or well-being. The Coalition employs multiple approaches that include using faith-based partnerships to deliver health services and encourage healthy choices; sharing data among the criminal justice, health care, and housing sectors to identify points of intervention; and building local and national coalitions to support and educate others interested in implementing this model ( Camden Coalition, n.d. ). One of the Coalition’s best-known programs is the Camden Core Model. This nationally recognized care management intervention is an example of a nurse-led care management program for people with complex medical and social needs. It applies the principles of trauma-informed care and harm reduction with the aim of empowering people with the skills and support they need to avoid preventable hospital use and improve their well-being ( Finkelstein et al., 2020 ; Gawande, 2011 ). The model uses real-time data on hospital admissions to identify “superutilizers,” people with complex health issues who frequently use emergency care. An interprofessional team of registered nurses (RNs) and licensed practical nurses (LPNs), social workers, and community health workers engage in person with these individuals to help them navigate their care by connecting them with medical care, government benefits, and social services ( Camden Coalition, n.d. ; Finkelstein et al., 2020 ). With federal funding, similar versions of the model have been extended to cities outside of Camden (AF4 Q, 2012 ; Crippen and Isasi, 2013 ; Mann, 2013 ).
Camden Coalition partnerships optimize the use of nurses in the community in several ways. An interprofessional team of nurses, social workers, and community health workers visits program participants, helps reconcile their medications, accompanies them to medical visits, and links them to social and legal services. Critical to the model’s success is recruiting nurses who are from the local community, capitalizing on their cultural and systems-level knowledge to facilitate and improve access to and utilization of local health and social services. The culture of the Camden Coalition model has been key to its success. The uniform commitment of nurses, staff, and leadership to addressing people’s complex needs has created a supportive work environment in which each team member’s role is optimized. Care Team members have accompanied people to their meetings and appointments for primary care, helped with applications for such public benefits as food stamps, provided referrals to social services and housing agencies, arranged for medication delivery in partnership with local pharmacies, and coordinated care among providers.
The Camden Coalition focuses on “authentic healing relationships,” defined as secure, genuine, and continuous partnerships between Care Team members and patients. This emphasis has evolved into a framework for patient engagement known as COACH, which stands for C onnect tasks with vision and priorities, O bserve the normal routine, A ssume a coaching style, C reate a backward plan, and H ighlight progress with data. An interprofessional team of nurses, social workers, and community health workers visits participants in the community. Team members are trained to problem solve with patients to achieve the program goals of helping them manage their chronic health conditions and reducing preventable hospital admissions.
Early evidence of the program’s effect in a small sample showed a 56 percent reduction in monthly hospital charges, a roughly 40 percent reduction in monthly visits to hospitals and emergency departments, and an approximately 52 percent increase in rates of reimbursement to care providers ( Green et al., 2010 ), although later evidence from a randomized controlled trial (RCT) indicated that the Camden Core Model did not reduce hospital readmissions ( Finkelstein et al., 2020 ). Other RCTs, conducted in Philadelphia and Chicago, showed that similar social care programs using case management and community health workers can reduce hospital admissions and save money in addition to improving health and quality of health care. Kangovi and colleagues (2018) conducted an RCT in Philadelphia to assess Individualized Management for Patient-Centered Targets (IMPaCT), a standardized community health worker intervention addressing unmet social needs across three health systems ( Kangovi et al., 2018 ). After 6 months, patients in the intervention group compared with controls were more likely to report the highest quality of care and spent fewer total days in the hospital (reduced by about two-thirds), saving $2.47 for each dollar invested by Medicaid annually ( Kangovi et al., 2020 ). The RCT in Chicago assessed the effectiveness of a case management and housing program in reducing use of urgent medical services among homeless adults with chronic medical conditions and found a 29 percent reduction in hospitalizations and a 24 percent reduction in emergency department visits ( Sadowski et al., 2009 ).
Edge Runner
The American Academy of Nurses’ Edge Runner initiative identifies and promotes nurse-designed models of care and interventions that can improve health, increase health care access and quality, and/or reduce costs ( AAN, n.d.a ). As of February 2020, 59 such programs had been evaluated against a set of criteria and designated as part of this initiative. Many Edge Runner programs are built around the needs of underserved communities and seek to improve health through holistic care that addresses social needs and SDOH, including a range of upstream, midstream, and downstream determinants. Mason and colleagues (2015) assessed 30 Edge Runner models identified as of 2012, finding four main commonalities that illustrate these programs’ broad and encompassing approach to health.
A holistic definition of health. Across the programs, health was defined broadly to include physical, psychological, social, spiritual, functional, quality-of-life, personal happiness, and well-being aspects. Additionally, the definition of health was based on the values of clients and shaped around their preferences. Typically, programs were grounded in SDOH to inform their design of individual- and community-level interventions.
Individual-, family-, and community-centric design. Most programs prioritized individual, family, and community goals over provider-defined goals through a “participant-led care environment” and “meeting people where they are.” Thus, interventions were tailored to the values and culture present at each of these three levels.
Relationship-based care. The programs reflected the importance of building trusting relationships with individuals, families, and communities to help them engage in ways to create and sustain their own health.
Ongoing group and public health approaches to improving the health of underserved populations. The nurses who designed the programs viewed serving underserved populations as a moral imperative. Through peer-to-peer education, support groups, and public health approaches, they sought to empower clients, give them a sense of control, build self-care agency, and increase resilience.
An in-depth study of three Edge Runner programs (the Centering Pregnancy model, INSIGHTS, and the Family Practice and Counseling Network) revealed particular lessons: the essential role of collaboration and leaders who can collaborate with a wide range of stakeholders, the need for plans for scalability and financial sustainability, and the importance of social support and empowerment to help people ( Martsolf et al., 2017 ). In these and other models, the capacity and knowledge associated with building meaningful, sustained partnerships across sectors is a key dimension of nursing practice that impacts health equity. The Edge Runner programs emphasize how, in the pursuit of improving care, lowering costs, and increasing satisfaction for people and families, nurses are actively working to achieve person-centered care that addresses social needs and SDOH and focusing on the needs of underserved populations to promote health equity ( Martsolf et al., 2016 , 2017 ; Mason et al., 2015 ). However, evidence directly linking the programs to decreases in disparities is generally not available. Two examples of Edge Runner programs are described in Box 5-2 .
Examples of Edge Runner Programs.
As models continue to evolve and be disseminated, it is critical to establish an evidence base that can help understand their impact on health and well-being and their contribution to achieving the broader aim of health equity. For care management programs incorporating social care, it is important to consider a broad array of both quantitative and qualitative measures beyond health care utilization ( Noonan, 2020 ). Although RCTs generate the most reliable evidence, this evidence can be limited in scope. For example, the RCTs cited above assessed neither the multidimensional nature of care management/social care models that might be reflected in such outcomes as client self-efficacy, satisfaction, or long-term health outcomes nor their potential social impacts. Also important to note is that care management models incorporating social care are limited by the availability of resources in the community, such as behavioral health services, addiction treatment, housing, and transportation. Programs that connect clients to health and social services are unlikely to work if relevant services are unavailable ( Noonan, 2020 ). Important to underscore in the context of this report is that multisector engagement, as well as health care teams that may involve social workers, community health workers, physicians, and others engaging alongside nurses, all are oriented to a shared agenda focused on improving health and advancing health equity.
- ADVOCATING FOR POLICY CHANGE
Public policies have a major influence on health care providers, systems, and the populations they serve. Accordingly, nurses can help promote health equity by bringing a health lens to bear on public policies and decision making at the community, state, and federal levels. Informing health-related public policy can involve communicating about health disparities and SDOH with the public, policy makers, and organizational leaders, focusing on both challenges and solutions for addressing health through actions targeted to achieving health equity.
When nurses engage with policy change as an upstream determinant of health, they can have a powerful and far-reaching impact on the health of populations. In the National Academy of Medicine’s Vital Directions series, Nancy Adler and colleagues (2016) note that “powerful drivers of health lie outside the conventional medical care delivery system…. Health policies need to expand to address factors outside the medical system that promote or damage health.” Because health inequities and SDOH are based in social structures and policies, efforts to address them upstream as the root of poor health among certain populations and communities need to focus on policy change ( NASEM, 2017a ). Nurses alone cannot solve the problems associated with upstream SDOH that exist outside of health care systems. However, by engaging in efforts aimed at changing local, state, or federal policy with a Health in All Policies approach, 2 they can address SDOH that underlie poor health ( IOM, 2011 ; NASEM, 2017a ; Williams et al., 2018 ). Whether nurses engage in policy making full time or work to inform policy part time as a professional responsibility, their attention to policies that either create or eliminate health inequities can improve the underlying conditions that frame people’s health. Nurses can bring a health and social justice lens to public policies and decision making at the community, state, and federal levels most effectively by serving in public- and private-sector leadership positions. Much of this work is discussed in Chapter 9 on nursing leadership, but it is noted in this chapter given the substantial influence that policy decisions have on health equity. Nurses can and should use their expertise to promote policies that support health equity.
For example, a nurse in Delaware was influential in getting the state’s legislature to pass legislation to implement a colorectal cancer screening program that has increased access to care and reduced disparities in morbidity and mortality from colorectal cancer (see Box 5-3 ). While individual nurses, often through their workplace and professional associations, engage in upstream efforts to impact health equity, there have been repeated calls from within the nursing community for more nurses to engage in informing public policy to improve health outcomes for individuals and populations.
Delaware Cancer Consortium.
- CONCLUSIONS
In the coming decade, the United States will make substantial progress in achieving health equity only if it devotes resources and attention to addressing the adverse effects of SDOH on the health of underresourced populations. As 2030 approaches, numerous initiatives to address health equity are likely to be launched at the local, state, and national levels. Many of these initiatives will focus on health care equity. Yet, while expanding access to quality care is critical to reducing disparities and improving health outcomes, such efforts need to be accompanied by additional efforts to identify and change the social institutions, dynamics, and systems underlying health inequities from the local to the national level. Nurses can contribute to reshaping the landscape of health equity over the coming decade by serving in expanded roles, working in new settings and new ways, and partnering with communities and other sectors beyond health care. Some nurses are already working in roles and settings that support health equity and are engaged in educating about and advocating for health equity through their professional associations. Nonetheless, broader engagement as a core activity of every nurse will help advance health equity nationwide. To achieve this aim will require
- support for and the willingness of the nursing workforce to take on new roles in new settings in the community;
- consistency in nurses’ preparation for engaging in downstream, midstream, and upstream strategies aimed at improving health equity by addressing issues that compromise health, such as geographic disparities, poverty, racism, homelessness, trauma, drug abuse, and behavioral health conditions;
- more experiential learning and opportunities to work in community settings throughout nursing education to ensure that nurses have skills and competencies to address individuals’ complex needs and promote efforts to improve the well-being of communities;
- nursing education that goes beyond teaching the principles of diversity, equity, and inclusion to provide sustained student engagement in hands-on community and clinical experiences with these issues;
- funding to support new models of care and functions that address SDOH, health equity, and population health; and
- evaluation of models to build the evidence needed to scale programs and the policies and resources necessary to sustain them.
These issues are discussed in the chapters that follow. Programs described in this chapter, such as the Camden Coalition and the Edge Runner initiatives, are exemplars of the kind of multidisciplinary, multisector efforts that will be necessary to address the complex needs of individuals and communities and make a lasting impact by eliminating health disparities, with the goal of achieving health equity. Central to these future efforts, however, are parallel efforts that evaluate and provide the evidence base on which to determine the effectiveness of models. One of the greatest challenges this committee faced was finding evidence directly linking the efforts of nurses to address social needs and SDOH to reductions in health disparities that would signal improved population health outcomes and health equity. Such evidence is essential to informing payment policy decisions that can ensure the sustainability of and nurse engagement in these models (discussed further in Chapter 6 ). Through evidence, the nursing profession can leverage its own potential, and the public, other professionals, and other sectors can understand the impact and value of such nursing engagement.
Conclusion 5-1: Nurses are in a position to improve outcomes for the underserved and can work to address the structural and institutional factors that produce health disparities in the first place. Conclusion 5-2: Nurses can use their unique expertise and perspective to help develop and advocate for policies and programs that promote health equity.
- AAN (American Academy of Nursing). Transforming America’s health system through nursing solutions. [November 3, 2020]. n.d.a. https://www .aannet.org /initiatives/edge-runners .
- AAN. [November 3, 2020]. ¡Cuídate!: A culturally-based program to reduce sexual risk behavior among Latino youth. n.d.b. https://www .aannet.org /initiatives/edge-runners /profiles/edge-runners--cuidate .
- AAN. [November 3, 2020]. Insights into children’s temperament: Supporting the development of low-income children. n.d.c. https://www .aannet.org /initiatives/edge-runners /profiles/edge-runners--insights-into-childrens-temperament .
- AARP. Preparation and roles of nursing care providers in America. 2010. [June 3, 2021]. http: //championnursing .org/resources/preparation-and-roles-nursing-care-providers-america .
- Abellanoza A, Provenzano-Hass N, Gatchel RJ. Burnout in ER nurses: Review of the literature and interview themes. Journal of Applied Biobehavioral Research. 2018; 23 (1):e12117.
- Adler NE, Glymour MM, Fielding J. Addressing social determinants of health and health inequalities. Journal of the American Medical Association. 2016; 316 (16):1641–1642. [ PubMed : 27669456 ]
- AF4Q (Aligning Forces for Quality). Expanding “hot spotting” to new communities. 2012. [November 3, 2020]. http: //forces4quality.org/node/5182.html .
- Agurs-Collins T, Persky S, Paskett ED, Barkin SL, Meissner HI, Nansel TR, Arteaga SS, Zhang X, Das R, Farhat T. Designing and assessing multilevel interventions to improve minority health and reduce health disparities. American Journal of Public Health. 2019; 109 (S1):S86–S93. [ PMC free article : PMC6356127 ] [ PubMed : 30699029 ]
- AHA (American Hospital Association). Screening for social needs: Guiding care teams to engage patients. Chicago, IL: American Hospital Association; 2019.
- ANA (American Nurses Association). ANA president condemns racism, brutality and senseless violence against black communities. 2020. [September 17, 2020]. https://www .nursingworld .org/news/news-releases /2020/ana-president-condemns-racism-brutality-and-senseless-violence-against-black-communities .
- ANCC (American Nurses Credentialing Center). Magnet® application manual. Silver Spring, MD: American Nurses Credentialing Center; 2017. 2019.
- Audain G, Maher C. Prevention and control of worldwide mosquito-borne illnesses: Nurses as teachers. Online Journal of Issues in Nursing. 2017; 22 (1):5. [ PubMed : 28488821 ]
- Bigbee JL, Issel LM. Conceptual models for population-focused public health nursing interventions and outcomes: The state of the art. Public Health Nursing. 2012; 29 (4):370–379. [ PubMed : 22765249 ]
- Braveman P, Arkin E, Orleans T, Proctor D, Plough A. What is health equity? And what difference does a definition make? Princeton, NJ: Robert Wood Johnson Foundation; 2017.
- Bridge JA, Asti L, Horowitz LM, Greenhouse JB, Fontanella CA, Sheftall AH, Kelleher KJ, Campo JV. Suicide trends among elementary school–aged children in the United States from 1993 to 2012. JAMA Pediatrics. 2015; 169 (7):673–677. [ PubMed : 25984947 ]
- Brown AF, Ma GX, Miranda J, Eng E, Castille D, Brockie T, Jones P, Airhihenbuwa CO, Farhat T, Zhu L, Trinh-Shevrin C. Structural interventions to reduce and eliminate health disparities. American Journal of Public Health. 2019; 109 (S1):S72–S78. [ PMC free article : PMC6356131 ] [ PubMed : 30699019 ]
- Camden Coalition. Camden core model. [November 4, 2020]. n.d. https: //camdenhealth .org/care-interventions /camden-core-model .
- Canales MK, Drevdahl DJ, Kneipp SM. Letter to the editor: Public health nursing. Nursing Outlook. 2018; 66 (2):110–111. [ PubMed : 29580625 ]
- Castrucci B, Auerbach J. Health Affairs Blog. 2019. Meeting individual social needs falls short of addressing social determinants of health. doi: 10.1377/hblog20190115.234942.
- CDC (Centers for Disease Control and Prevention). Health in all policies. 2016. [June 2, 2021]. https://www .cdc.gov/policy/hiap/index .html .
- CMS (Centers for Medicare & Medicaid Services). Z codes utilization among Medicare fee-for-service (FFS) beneficiaries in 2017. Baltimore, MD: Centers for Medicare & Medicaid Services Office of Minority Health; 2020.
- Crippen D, Isasi F. Health Affairs Blog. 2013. [June 2, 2021]. The untold story of 2013: Governors lead in health care transformation. https://www .healthaffairs .org/do/10.1377/hblog20131217 .035878/full .
- Davies N, Donovan H. National survey of commissioners’ and service planners’ views of public health nursing in the UK. Public Health. 2016; 141 :218–221. [ PubMed : 27932004 ]
- Donley R, Flaherty MJ. Revisiting the American Nurses Association’s first position on education for nurses. Online Journal of Issues in Nursing. 2002; 7 (2):2. [ PubMed : 12059278 ]
- Duran D, Asada Y, Millum J, Gezmu M. Harmonizing health disparities measurement. American Journal of Public Health. 2019; 109 (S1):S25–S27. [ PMC free article : PMC6356133 ] [ PubMed : 30699026 ]
- Dye BA, Duran DG, Murray DM, Creswell JW, Richard P, Farhat T, Breen N, Engelgau MM. The importance of evaluating health disparities research. American Journal of Public Health. 2019; 109 (S1):S34–S40. [ PMC free article : PMC6356135 ] [ PubMed : 30699014 ]
- Finkelstein A, Zhou A, Taubman S, Doyle J. Health care hotspotting—A randomized, controlled trial. New England Journal of Medicine. 2020; 382 (2):152–162. [ PMC free article : PMC7046127 ] [ PubMed : 31914242 ]
- Fraze TK, Brewster AL, Lewis VA, Beidler LB, Murray GF, Colla CH. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by us physician practices and hospitals. JAMA Network Open. 2019; 2 (9):e1911514. [ PMC free article : PMC6752088 ] [ PubMed : 31532515 ]
- Gawande A. The hot spotters. Jan 24, 2011. [October 14, 2020]. https://www .newyorker .com/magazine/2011/01 /24/the-hot-spotters .
- Gottlieb LM, Hessler D, Long D, Laves E, Burns AR, Amaya A, Sweeney P, Schudel C, Adler NE. Effects of social needs screening and in-person service navigation on child health: A randomized clinical trial. JAMA Pediatrics. 2016; 170 (11):e162521. [ PubMed : 27599265 ]
- Green SR, Singh V, O’Byrne W. Hope for New Jersey’s city hospitals: The Camden initiative. Perspectives in Health Information Management. 2010; 7 (Spring):1d. [ PMC free article : PMC2889370 ] [ PubMed : 20697470 ]
- Grubbs SS, Polite BN, Carney J Jr, Bowser W, Rogers J, Katurakes N, Hess P, Paskett ED. Eliminating racial disparities in colorectal cancer in the real world: It took a village. Journal of Clinical Oncology. 2013; 31 (16):1928–1930. [ PMC free article : PMC3661932 ] [ PubMed : 23589553 ]
- Healthy Delaware. Welcome Consortium Members and Partners. 2020. [November 3, 2020]. https://www .healthydelaware .org/Consortium .
- Heath S. 3 things to know to conduct a community health needs assessment. 2018. [October 6, 2020]. https: //patientengagementhit .com/news/3-things-to-know-to-conduct-a-community-health-needs-assessment .
- IOM (Institute of Medicine). The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press; 2011. [ PubMed : 24983041 ]
- IRS (Internal Revenue Service). Community health needs assessment for charitable hospital organizations-Section 501(r)(3). 2020. [June 2, 2021]. https://www .irs.gov/charities-non-profits /community-health-needs-assessment-for-charitable-hospital-organizations-section-501r3 .
- Jones NL, Breen N, Das R, Farhat T, Palmer R. Cross-cutting themes to advance the science of minority health and health disparities. American Journal of Public Health. 2019; 109 (S1):S21–S24. [ PMC free article : PMC6356138 ] [ PubMed : 30699031 ]
- Kangovi S, Mitra N, Norton L, Harte R, Zhao X, Carter T, Grande D, Long JA. Effect of community health worker support on clinical outcomes of low-income patients across primary care facilities: A randomized clinical trial. JAMA Internal Medicine. 2018; 178 (12):1635–1643. [ PMC free article : PMC6469661 ] [ PubMed : 30422224 ]
- Kangovi S, Mitra N, Grande D, Long J, Asch D. Evidence-based community health worker program addresses unmet social needs and generates positive return on investment. Health Affairs. 2020; 39 (2 doi) 10.1377/hlthaff.2019.00981. [ PMC free article : PMC8564553 ] [ PubMed : 32011942 ]
- Keller LO, Strohschein S, Schaffer MA, Lia-Hoagberg B. Population-based public health interventions: Innovations in practice, teaching, and management. Part II. Public Health Nursing. 2004; 21 (5):469–487. [ PubMed : 15363027 ]
- Krist AH, Wolff TA, Jonas DE, Harris RP, LeFevre ML, Kemper AR, Mangione CM, Tseng C-W, Grossman DC. Update on the methods of the U.S. Preventive Services task force: Methods for understanding certainty and net benefit when making recommendations. American Journal of Preventive Medicine. 2018; 54 (1)(Suppl 1):S11–S18. [ PubMed : 29254521 ]
- Kulbok PA, Thatcher E, Park E, Meszaros PS. Evolving public health nursing roles: Focus on community participatory health promotion and prevention. Online Journal of Issues in Nursing. 2012; 17 (2):1. [ PubMed : 22686109 ]
- Lantz PM. The medicalization of population health: Who will stay upstream? Milbank Quarterly. 2019; 97 (1):36–39. [ PMC free article : PMC6422602 ] [ PubMed : 30549108 ]
- Larsen R, Ashley J, Ellens T, Frauendienst R, Jorgensen-Royce K, Zelenak M. Development of a new graduate public health nurse residency program using the core competencies of public health nursing. Public Health Nursing. 2018; 35 (6):606–612. [ PubMed : 29947429 ]
- Makelarski JA, Abramsohn E, Benjamin JH, Du S, Lindau ST. Diagnostic accuracy of two food insecurity screeners recommended for use in health care settings. American Journal of Public Health. 2017; 107 (11):1812–1817. [ PMC free article : PMC5636681 ] [ PubMed : 28933929 ]
- Mann C. CMCS informational bulletin: Targeting Medicaid super-utilizers to decrease costs and improve quality. Baltimore, MD: Centers for Medicare & Medicaid Services; 2013.
- Martsolf GR, Gordon T, Warren May L, Mason D, Sullivan C, Villarruel A. Innovative nursing care models and culture of health: Early evidence. Nursing Outlook. 2016; 64 (4):367–376. [ PubMed : 27063477 ]
- Martsolf GR, Mason DJ, Sloan J, Sullivan CG, Villarruel AM. Nurse-designed care models: What can they tell us about advancing a culture of health? Santa Monica, CA: RAND Corporation; 2017.
- Mason DJ, Jones DA, Roy C, Sullivan CG, Wood LJ. Commonalities of nurse-designed models of health care. Nursing Outlook. 2015; 63 (5):540–553. [ PubMed : 26211847 ]
- Minnesota Department of Health. Public health interventions: Applications for public health nursing practice. 2nd ed. St. Paul, MN: Minnesota Department of Health; 2019.
- Minnesota Department of Health. Public health nurse orientation and resource guide. [October 5, 2020]. n.d. https://www .health.state .mn.us/communities /practice/ta/phnconsultants/guide-phn .html .
- Mullan F. Social mission in health professions education: Beyond flexner. Journal of the American Medical Association. 2017; 318 (2):122–123. [ PubMed : 28654979 ]
- NASEM (National Academies of Sciences, Engineering, and Medicine). Accounting for social risk factors in Medicare payment: Identifying social risk factors. Washington, DC: The National Academies Press; 2016. [ PubMed : 26844313 ]
- NASEM. Communities in action: Pathways to health equity. Washington, DC: The National Academies Press; 2017a. [ PubMed : 28418632 ]
- NASEM. Global health and the future role of the United States. Washington, DC: The National Academies Press; 2017b. [ PubMed : 29001490 ]
- NASEM. Integrating social care into the delivery of health care: Moving upstream to improve the nation’s health. Washington, DC: The National Academies Press; 2019. [ PubMed : 31940159 ]
- Noonan K. Health Affairs Blog. 2020. Disappointing randomized controlled trial results show a way forward on complex care in Camden and beyond. doi: 10.1377/hblog20200102.864819.
- Pittman P. Rising to the challenge: Re-embracing the Wald model of nursing. American Journal of Nursing. 2019; 119 (7):46–52. [ PubMed : 31232775 ]
- Rafferty AM. Video. Jan 27, 2015. [September 6, 2020]. Reinventing nursing’s social mission. https://www .youtube.com /watch?v=8PjoiO8v-dE .
- Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: A randomized trial. Journal of the American Medical Association. 2009; 301 (17):1771–1778. [ PubMed : 19417194 ]
- Schaffer MA, Keller LO, Reckinger D. Public health nursing activities: Visible or invisible? Public Health Nursing. 2015; 32 (6):711–720. [ PubMed : 25808923 ]
- Swider SM, Levin PF, Reising V. Evidence of public health nursing effectiveness: A realist review. Public Health Nursing. 2017; 34 (4):324–334. [ PubMed : 28295536 ]
- Thomas-Henkel C, Schulman M. Screening for social determinants of health in populations with complex needs: Implementation considerations. Trenton, NJ: Center for Health Care Strategies; 2017.
- Tyson T, Kenon CJ Jr, Nance K. Nursing at historically black colleges and universities. Journal of Professional Nursing. 2018; 34 (3):167–170. [ PubMed : 29929795 ]
- Williams DR, Purdie-Vaughns V. Needed interventions to reduce racial/ethnic disparities in health. Journal of Health Politics, Policy and Law. 2016; 41 (4):627–651. [ PubMed : 27127267 ]
- Williams SD, Phillips JM, Koyama K. Nurse advocacy: Adopting a health in all policies approach. Online Journal of Issues in Nursing. 2018; 23 (3)
- Woolf SH, Purnell JQ, Simon SM, Zimmerman EB, Camberos GJ, Haley A, Fields RP. Translating evidence into population health improvement: Strategies and barriers. Annual Review of Public Health. 2015; 36 (1):463–482. [ PMC free article : PMC8489033 ] [ PubMed : 25581146 ]
These five domains of social needs are part of the Centers for Medicare & Medicaid Services’ Accountable Health Communities Model ( Fraze et al., 2019 ).
Health in All Policies (HiAP) is a collaborative approach that integrates health considerations into policy making across sectors. It recognizes that health is created by a multitude of factors beyond health care and in many cases, beyond the scope of traditional public health activities. In accordance with HiAP, for example, decision makers in the health care sector should consider transportation, education, housing, commerce, and other sectors impacting communities. HiAP stresses the need to work across government agencies and with private partners from these different sectors to achieve healthy and safe communities. It also encourages partnerships between the health care sector and community developers, for example ( CDC, 2016 ).
- Cite this Page National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on the Future of Nursing 2020–2030; Flaubert JL, Le Menestrel S, Williams DR, et al., editors. The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. Washington (DC): National Academies Press (US); 2021 May 11. 5, The Role of Nurses in Improving Health Equity.
- PDF version of this title (5.6M)
In this Page
- NURSES’ ROLE IN ADDRESSING HEALTH EQUITY
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- The Role of Nurses in Improving Health Equity - The Future of Nursing 2020-2030 The Role of Nurses in Improving Health Equity - The Future of Nursing 2020-2030
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
Professional nursing is rooted in social justice responsibilities. •. Student nurses should be aware of and take actions for social justice issues that affect people's health. •. Awareness of and actions for social justice are not explicit in nursing documents in the United Kingdom. •. The Nursing and Midwifery Council (NMC) and schools ...
Background In recent decades, increasing social and health inequalities all over the world has highlighted the importance of social justice as a core nursing value. Therefore, proper education of nursing students is necessary for preparing them to comply with social justice in health systems. This study is aimed to identify the main factors for teaching the concept of social justice in the ...
As described in Chapter 1, the history of nursing is grounded in social justice and community health advocacy (Donley and Flaherty, 2002; Pittman, 2019; Rafferty, 2015; Tyson et al., 2018), and as noted in Chapter 2, the Code of Ethics for Nurses with Interpretive Statements, reiterated by American Nurses Association (ANA) President Ernest J ...
NURSES’ ROLE IN ADDRESSING HEALTH EQUITY. As described in Chapter 1, the history of nursing is grounded in social justice and community health advocacy (Donley and Flaherty, 2002; Pittman, 2019; Rafferty, 2015; Tyson et al., 2018), and as noted in Chapter 2, the Code of Ethics for Nurses with Interpretive Statements, reiterated by American Nurses Association (ANA) President Ernest J. Grant ...
The term “social justice” was first coined by Jesuit Luigi Taparelli in 1840, who defined it as a virtue that included actions toward common good and rectifying unfair treatment. 5 Social justice in the health system refers to the provision of equal health services to all people, regardless of their personal characteristics (e.g. gender, ethnicity, geographical location, and socioeconomic ...
This study discusses two key nursing movements for health and social justice, the public health nursing movement and the nurse practitioner movement. This study also describes how the re-emerging focus on population health nursing and the increasing nurse activism are building on our history of addressing the social and environmental root ...
Escalating health care costs, COVID-19, and racial conflict have spotlighted the impact of our social and health inequities and the interconnectedness of everyone's health. This study discusses two key nursing movements for health and social justice, the public health nursing movement and the nurse practitioner movement.
Social justice, ethics, and the nursing profession. By: Tahitia Timmons, MSN, PMGT-BC, OCN, CDP. A celebration of nurses’ month seems an odd time to discuss the importance of social justice however nurses have long been change agents from their inception to today. When we discuss social justice, we are referring to the fair and equal ...
Efforts to integrate tenets of social justice into PhD nursing programs are long-standing but have intensified in the past few years in response to civil unrest, threats to human rights, and health inequities exacerbated during the COVID-19 pandemic. In this paper, we present an overview of our School of Nursing’s efforts and processes to evaluate and ensure that social justice principles ...