- Behavioral Health
- Anorexia nervosa

Anorexia nervosa-Quiz
Machen Sie einen Quiz, um herauszufinden, ob Sie an Anorexia nervosa leiden.
Nehmen Sie am Anorexia nervosa-Quiz teil
Was ist Magersucht?
Magersucht, auch Anorexia nervosa genannt, ist eine Essstörung.
Jemand mit Magersucht hat drei Hauptsymptome: Er hat große Angst vor einer Gewichtszunahme, er schränket die Nahrungsaufnahme ein (was zu einem erheblichen Gewichtsverlust führt) und er hat möglicherweise eine verzerrte Sicht auf seinen Körper (und denkt, er sei übergewichtig, obwohl dies nicht der Fall ist).
Es gibt zwei Arten von Magersucht: den einschränkenden und den Essattacken-/Purging-Typ. Der restriktive Typ liegt vor, wenn jemand seine Nahrungs- und Kalorienaufnahme einschränkt, was zu einem extremen Gewichtsverlust führt.
Beim Binge-Eating/Purging-Typ isst jemand regelmäßig zu viel (Essattacken) und muss sich dann übergeben oder Abführmittel verwenden, um die Nahrung aus dem Körper zu spülen. Auch wenn das nach Bulimie (einer anderen Essstörung) klingt, gibt es doch feine Unterschiede. Menschen mit Essattacken/Magersucht vom Purging-Typ schränken ihre Kalorienzufuhr ein, Menschen mit Bulimie hingegen nicht. Typischerweise verlieren Menschen mit Magersucht viel Gewicht, während Menschen mit Bulimie dies möglicherweise nicht tun.
Magersucht entsteht durch eine Kombination genetischer, sozialer und emotionaler Probleme wie schlechtes Körperbild, geringes Selbstwertgefühl, Stress, Missbrauch in der Vorgeschichte oder Kontrollprobleme.
Es handelt sich um eine sehr ernste Erkrankung, wenn sie nicht behandelt wird. Es kann zu Herzproblemen, Unfruchtbarkeit, Anämie und hormonellen Komplikationen führen.
Die Behandlung umfasst Gesprächstherapie, Ernährungsberatung, Familientherapie oder eine Selbsthilfegruppe und möglicherweise Medikamente.
Die häufigsten Symptome
Die Menschen in Ihrem Leben werden Ihnen sagen, Sie sollen „einfach essen“. Eine häufige Fehleinschätzung ist, dass dies bei jemandem möglich ist, der an Magersucht leidet. Auch wenn es für Ihre Freunde und Familie schwer zu verstehen ist, wissen wir, dass Sie nicht „einfach essen“ können. — Bobbi Wegner
Magersucht ist eine schwere Essstörung, bei der Sie große Angst vor einer Gewichtszunahme haben. Möglicherweise halten Sie sich selbst für übergewichtig (obwohl dies nicht der Fall ist) und schränken Ihre Nahrungsaufnahme ein, um Gewicht zu verlieren.
Hauptsymptome
Die Hauptsymptome der Magersucht lassen sich in vier Kategorien einteilen: verhaltensbedingt, emotional, körperlich und kognitiv.
- Essen Sie nur sehr kleine Mengen und beschränken Sie die Nahrungsaufnahme
- Entleerung durch induziertes Erbrechen, Einnahme von Abführmitteln und Diuretika, Fasten oder übermäßige sportliche Betätigung
- Geheimnisvolles Verhalten (z. B. vorgeben, etwas zu essen oder alleine zu essen)
- Sozialer Rückzug
- Depression /Traurigkeit
- Ich fühle mich gereizt
- Angst vor Gewichtszunahme
- Überwältigt fühlen
- Das Gefühl, die Kontrolle verloren zu haben
- Schlaflosigkeit
- Schwindel, Ohnmacht
- Verlust Ihrer Periode
- Haarwuchs (am Körper und im Gesicht)
- Haarausfall am Kopf
- Bläuliche Fingernägel
- Verlust des Interesses an Sex
- Selbstkritisch
- Irrationales Denken
- Negative Gedankenmuster
- Zwangsgedanken rund ums Essen
- Sich zu sehr auf das Essen konzentrieren
Nächste Schritte
Magersucht ist eine komplexe Krankheit. Wer an Magersucht leidet, muss einen Psychologen aufsuchen. Bitten Sie Ihren Arzt um eine Überweisung. Oder erkundigen Sie sich bei Ihrer Versicherungsgesellschaft nach einer Liste der abgedeckten Anbieter. Auch, psychologytoday.com verfügt über eine Liste von Therapeuten, die Sie durchsuchen können.
Wenn Anorexie nicht behandelt wird, kann sie zu anderen Arten von Problemen wie Angstzuständen, Depressionen und Drogenmissbrauch führen. Es kann auch zu schwerwiegenden Erkrankungen wie Herz- und Unfruchtbarkeitsproblemen führen.
Wenn Sie daran denken, sich selbst zu verletzen, gehen Sie zur Notaufnahme oder rufen Sie 911 an. Die National Suicide Prevention Lifeline ist unter 800-273-8255 erreichbar und bietet rund um die Uhr kostenlose, vertrauliche Unterstützung.
Behandlung von Anorexia nervosa
Magersucht ist ein ernstes psychisches und medizinisches Problem. Es geht weit über den bloßen Wunsch hinaus, dünn zu sein. Magersucht ist eine Form des Selbsthungerns und hat schwerwiegende medizinische Folgen, darunter Herzprobleme und sogar den Tod. Ich teile dies nicht, um Ihnen Angst zu machen, sondern um früher als später Hilfe zu suchen. — Dr. Wegner
Die Behandlung von Magersucht erfordert oft mehr als eine Therapie. Sie können mit einem Psychiater, einem Psychologen, einem Sozialarbeiter und einem Ernährungsberater zusammenarbeiten. Der Die National Eating Disorders Association verfügt über weitere Informations- und Unterstützungsressourcen .
Zu den Therapiearten gehören:
- Gesprächstherapie. In Sitzungen mit einem Therapeuten erforschen Sie Ihre Beziehung zwischen Gedanken, Emotionen und Ihrem Verhalten. Ziel der Behandlung ist es, zu lernen, ungesunde Denkmuster und Verhaltensweisen wahrzunehmen und gleichzeitig positive Bewältigungsstrategien zu entwickeln.
- Familientherapie kann Familienmitgliedern mehr über Magersucht beibringen und ihnen zeigen, wie sie ihre Liebsten am besten unterstützen können.
- Selbsthilfegruppen sind eine Möglichkeit, Informationen auszutauschen und emotionale Unterstützung von anderen zu erhalten, denen es genauso geht.
- Ernährungsberatung kann dabei hilfreich sein, eine gesündere Beziehung zu Lebensmitteln und gesunden Essgewohnheiten zu entwickeln. Sie erfahren auch, wie es geht Folgen Sie Ihrem natürlichen Hungergefühl .
- Medikament. Antidepressiva wie Fluoxetin (Prozac) werden häufig zur Behandlung von Anorexie eingesetzt. Andere Antidepressiva werden manchmal zur Behandlung zugrunde liegender psychischer Erkrankungen wie Angstzuständen oder Depressionen verabreicht.
Ready to treat your anorexia nervosa?
Wer wird es wahrscheinlich haben.
- Frauen sind häufiger von Anorexie betroffen als Männer, obwohl beide Geschlechter davon betroffen sind.
- Mädchen im Teenageralter und junge Frauen sind einem höheren Risiko ausgesetzt.
- Es betrifft Menschen aller Rassen und Ethnien.
- Menschen, die fleißig, perfektionistisch, kontrollierend, introvertiert und selbstkritisch sind, haben ein erhöhtes Risiko, an Magersucht zu erkranken.
- Menschen aus Familien mit hohem Einkommen haben ein erhöhtes Risiko, an Magersucht zu erkranken.
Magersucht verursacht
Kontrolle ist meist ein großer Teil der Magersucht. Wenn Menschen das Gefühl haben, in anderen Bereichen ihres Lebens die Kontrolle verloren zu haben, besteht ein Bewältigungsmechanismus darin, ihre Nahrungsaufnahme und ihren Körper zu kontrollieren. — Dr. Wegner
Niemand weiß genau, was dazu führt, dass Menschen eine Essstörung entwickeln. Experten sind sich einig, dass bestimmte Faktoren das Risiko erhöhen, an Magersucht zu erkranken. Mögliche Ursachen sind:
- Familiengeschichte von Magersucht
- Familien mit hohem Einkommen und hohen Leistungen
- Schlechtes Körperbild
- Geringe Selbstachtung
- Sich an einer Sportart oder einer anderen Aktivität beteiligen, bei der Aussehen und Leistung im Vordergrund stehen, wie etwa Ballett
- Vorgeschichte von Missbrauch oder Trauma
- Allgemeiner Stress
Vorbeugung gegen Magersucht
Es gibt keinen klaren Weg, Magersucht vorzubeugen. Viele Faktoren, darunter auch die Genetik, spielen eine Rolle. Das Befolgen gesunder Lebensgewohnheiten kann einen Unterschied machen. Eltern können ihren Kindern helfen, indem sie einen gesunden Umgang mit Lebensmitteln fördern.
- Entwickeln Sie eine gesunde Herangehensweise an Essen und Trinken. Probieren Sie viel Essen, essen Sie, wenn Sie hungrig sind, und hören Sie auf, wenn Sie satt sind.
- Üben Sie achtsames Essen, bei dem Sie dem Essen beim Verzehr große Aufmerksamkeit schenken, ohne zu urteilen.
- Entwickeln Sie ein gesundes Körperbild und konzentrieren Sie sich dabei auf die Funktion Ihres Körpers, nicht auf die Form.
- Versuchen Sie, mit Stress und Ängsten umzugehen.
- Achten Sie auf Menschen in Ihrem Umfeld (Familie und Freunde), die ein ungesundes Verhältnis zum Essen haben.
- Holen Sie sich beim ersten Anzeichen von Veränderungen in der ungesunden Ernährung oder den Gedanken rund ums Essen Hilfe von einem Spezialisten für psychische Gesundheit.
Required field
Was this article helpful?
SYSTEMATIC REVIEW article
Descriptions of disordered eating in german psychiatric textbooks, 1803–2017.
A commentary has been posted on this article:
Commentary: Descriptions of Disordered Eating in German Psychiatric Textbooks, 1803 – 2017
- Read general commentary

- 1 Archiv für Leipziger Psychiatriegeschichte, Klinik und Poliklinik für Psychiatrie und Psychotherapie, Medizinische Fakultät der Universität Leipzig, Leipzig, Germany
- 2 Department of Psychological Medicine, King's College London, London, United Kingdom
- 3 Department of Psychiatry, University of Tasmania, Hobart, TAS, Australia
The most common eating disorders (EDs) according to DSM-5 are anorexia nervosa (AN), bulimia nervosa (BN) and binge eating disorder (BED). These disorders have received increasing attention in psychiatry due to rising prevalence and high morbidity and mortality. The diagnostic category “anorexia nervosa,” introduced by Ernest-Charles Lasègue and William Gull in 1873, first appears a century later in a German textbook of psychiatry, authored by Gerd Huber in 1974. However, disordered eating behavior has been described and discussed in German psychiatric textbooks throughout the past 200 years. We reviewed content regarding eating disorder diagnoses but also descriptions of disordered eating behavior in general. As material, we carefully selected eighteen German-language textbooks of psychiatry across the period 1803–2017. Previously, in German psychiatry, disordered eating behaviors were seen as symptoms of depressive disorders, bipolar disorder or schizophrenia, or as manifestations of historical diagnoses no longer used by the majority of psychiatrists such as neurasthenia, hypochondria and hysteria. Interestingly, 19th and early 20th century psychiatrists like Kraepelin, Bumke, Hoff, Bleuler, and Jaspers reported symptom clusters such as food refusal and vomiting under these outdated diagnostic categories, whereas nowadays they are listed as core criteria for specific eating disorder subtypes. A wide range of medical conditions such as endocrinopathies, intestinal or brain lesions were also cited as causes of abnormal food intake and body weight. An additional consideration in the delayed adoption of eating disorder diagnoses in German psychiatry is that people with EDs are commonly treated in the specialty discipline of psychosomatic medicine, introduced in Germany after World War II, rather than in psychiatry. Viewed from today's perspective, the classification of disorders associated with disordered eating is continuously evolving. Major depressive disorder, schizophrenia and physical diseases have been enduringly associated with abnormal eating behavior and are listed as important differential diagnoses of EDs in DSM-5. Moreover, there are overlaps regarding the neurobiological basis and psychological and psychopharmacological therapies applied to all of these disorders.
Introduction
The diagnosis and treatment of eating disorders (EDs) is an important domain of psychiatry. DSM-5 dedicates a separate chapter to eating disorder diagnoses. Anorexia nervosa (AN), bulimia nervosa (BN) and binge eating disorder (BED) are noted as the clinically most serious and prevalent conditions ( 1 ). Additional distinct EDs in DSM-5 include pica, rumination and avoidant-restrictive food intake disorder (ARFID). Prevalence rates of AN and BN are 10 and BED 2 times higher in women than men ( 1 ). One in six young women experience an ED ( 2 ). Life-time incidence is estimated up to 4% for AN and 2% each for BN and BED ( 3 ). Twelve-month prevalence is 0.4% for AN and 1–1.5% for BN. Twelve-month-prevalence of BED in adults is estimated at 0.8–1.6%. Mortality rates for AN at 5 to 20% are the highest of any psychiatric disorder ( 4 ) exceeding schizophrenia and depression [( 5 ), p. 426]. Typical causes of death are somatic complications due to food refusal and starvation, but suicide is also common accounting for one in five deaths ( 4 ). Although mortality rates in BN are significantly lower than in AN, bulimia is associated with serious complications, such as electrolyte and pH disturbances, and tooth erosion [( 5 ), p. 425]. Recovery rates of 52% in AN and BN in a 6-year follow up ( 6 ) indicate the need for more effective treatment.
As well as serious implications for the individual, EDs have significant economic consequences. It is estimated that ~€ 1 trillion per year is spent on the ~20 million patients with eating disorders in the European Union. The direct costs of health care are the same quantum as for anxiety and depression, indirect costs due to burden of disease are even higher ( 7 ).
In the English-language literature, the conceptualization of eating disorders as discrete diagnostic entities has developed over the past 150 years. Anorexia nervosa (AN) was first described in 1873 by the French physician Ernest-Charles Lasègue and by the English physician and neurologist William Gull ( 8 ). The first description of bulimia nervosa (BN), by Otto Dörr-Zegers, a Chilean of German descent, in the Revista Chilena de Neuro-Psiquiatria (1972), was exceeded in recognition and influence by the description by the British psychiatrist Gerald Russell in Psychological Medicine in 1979 ( 9 , 10 ). Binge eating disorder (BED) as a separate diagnostic entity debuted as recently as 2013, the time of its inception in DSM-5 ( 1 ). The classification of eating disorders is subject to ongoing change. Diagnostic criteria for AN and BN have been subject to frequent alteration. The chapter on eating disorders was extensively revised for DSM-5 and further changes are under consideration for the upcoming edition, including possible new diagnostic entities such as Night Eating Syndrome and Purging Disorder ( 11 , 12 ).
In the German-language literature, the historical development has been strikingly different. Systematic reviews have already shown that eating disorders received little attention in German-speaking psychiatry until the 20th century. This resulted in a small number of published articles, while in France and England numerous articles on this particular field were published at the same time [( 13 ), p. 204–13, ( 14 )].
Our aim was to investigate whether this low reception also applies to the most common textbooks of that time.
Textbook accounts of disordered eating behavior and related diagnostic entities are of particular value in discerning historical developments. Textbooks generally present a systematic account of the field of psychiatry, incorporate received views of the profession at a given time, detail perspectives promoted by the authors, and indicate formative influences and trends in education and training of psychiatrists and other medical practitioners. This article examines the representation of disordered eating behavior and EDs in German-language textbooks over the past two centuries, in particular addressing the following questions:
• When were eating disorders first mentioned as discrete diagnoses?
• Which other psychiatric diseases were associated with disturbed eating habits?
• What explanations were given for disordered eating behavior?
• In how much detail and to what extent did influential psychiatrists address these issues?
• What continuities and changes can be observed in the conceptualization of disordered eating behavior and diagnostic categories of eating disorders across these more than 200 years?
• Finally, from the perspective of today's clinical practice and available research findings:
• Are there any concepts that are still valid today?
• To what extent do current research findings support or refute the ideas of the past?
Materials and Methods
In order to gain a comprehensive picture of changing perspectives on disordered eating behavior and eating disorders in the past 200 years of German academic psychiatry, we compiled a list of 18 representative textbooks, taking into account the influence of the authors and distribution of year of publication across the period. This method has been previously applied in a longitudinal historical study ( 15 ).
For the selection of literature, we decided on the following strategy: We intentionally chose to focus on psychiatric textbooks because we wanted to present the knowledge that was considered valid at the time, representing the most common and generally accepted views within the clinical and scientific community on disordered eating in the past 200 years. Articles in journals were not taken into consideration, as they did not necessarily represent valid and widespread knowledge.
All the authors considered were professors and therefore their publications had a formative influence on psychiatry and contributed significantly to the teaching of future psychiatrists. Some of the chairs held by the authors of these historic textbooks were even considered to be the most important psychiatric chairs in the world at the time: Heinroth held the world's first psychiatric chair in Leipzig ( 16 ). Kraepelin taught in Munich and Heidelberg. He shaped German-speaking psychiatry far beyond his time, introducing clinical-empirical psychiatry and nosology. Other chairs of central importance for psychiatry have been in Vienna (Hoff), Zurich (M. Bleuler) and Breslau (Neumann).
In addition, all considered authors made significant contributions to psychiatry: Griesinger is considered the founder of the scientific and biological phase of psychiatry ( 17 ). Eugen Bleuler is considered the founder of the concept of schizophrenia ( 18 ). With Kurt Kolle and Helmut Rennert, two of the most important psychiatrists from Eastern and Western Germany are represented as well. Their textbooks have been published in numerous editions, showing their wide and long-term distribution in the field of psychiatry ( 19 , 20 ). These are exemplary contributions of the cited authors to the field of psychiatry. Further important scientific contributions by the other cited authors can be found in Table 1 , listing the cited textbooks and relevant publication data.
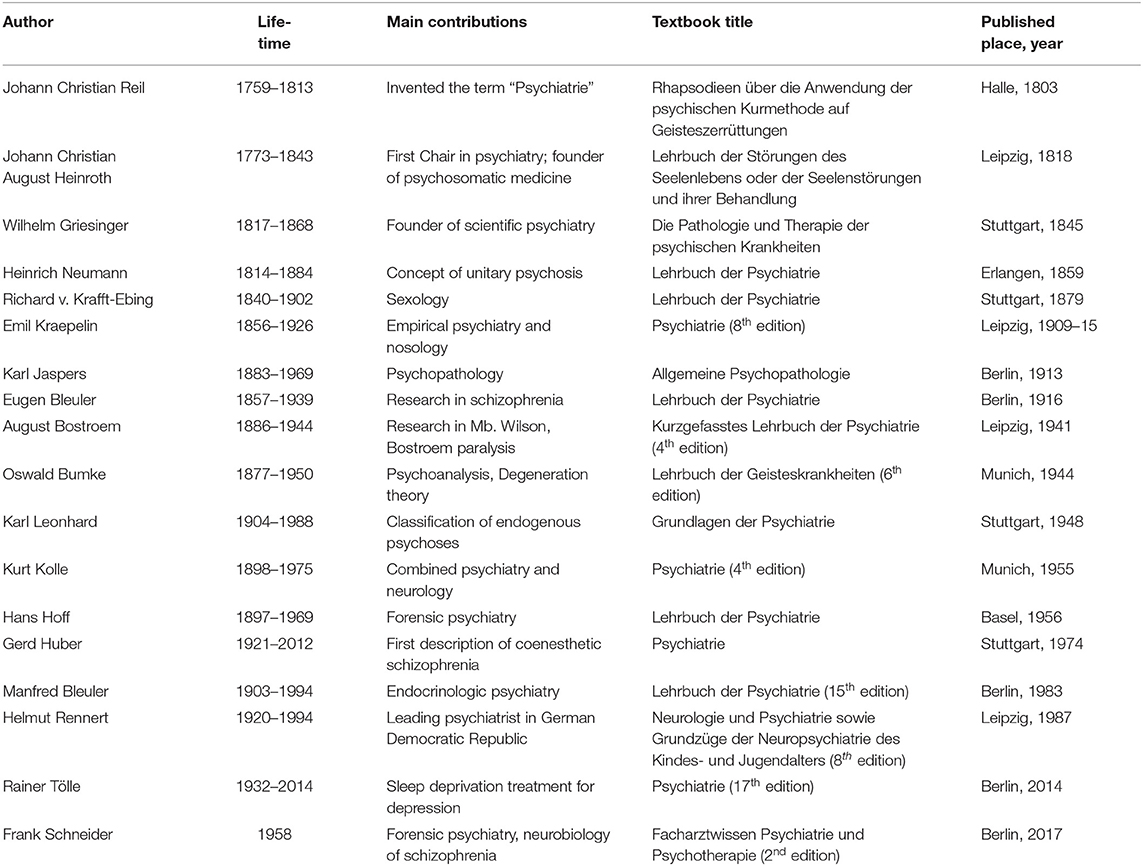
Table 1 . List of authors, lifetime, main contributions to psychiatric science, textbook details.
Inclusion criteria comprised: textbook of psychiatry in German language; authored by a professor of psychiatry at a German-speaking university; author a recognized authority in psychiatry; published between 1800 and 2017.
Eighteen textbooks were identified, spanning publication years 1803–2017. The timeline is presented in Figure 1 .
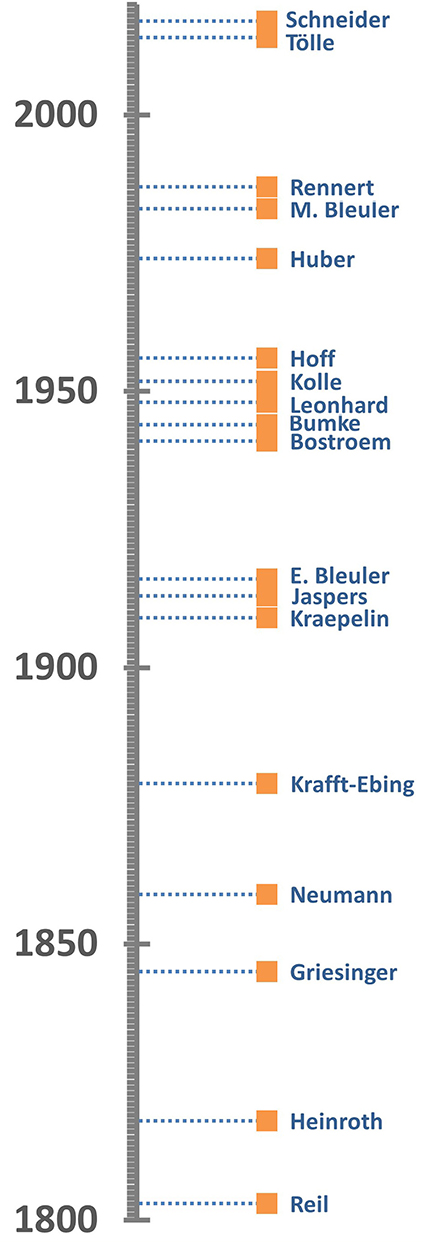
Figure 1 . Timeline showing the distribution of the years of publication of the textbooks in this study.
In each textbook, relevant passages on eating disorders or their symptoms, such as food denial, emaciation or cravings, were identified, excerpted, and sorted thematically. Historical perspectives and individual views of the authors that shaped their eating disorder narrative were identified. Points of similarity and difference between these historical perspectives and present-day conceptualization of and research findings on eating disorders are summarized and discussed.
Eating Disorders as Distinct Diagnostic Entities
The first author to mention eating disorders as a separate disease entity in a German textbook is Gerd Huber in 1974. Huber describes “anorexia mentalis,” characterized by refusal to eat, substantial weight loss, amenorrhea, use of appetite inhibitors and laxatives. This is noted to be most common in pubertal women, Huber discusses delayed “psychosexual maturation” as well as rejection of female roles as possible triggers [( 21 ), p. 270]. This explanation is repeated in later textbooks by Manfred Bleuler and Helmut Rennert ( 20 , 22 ). Only Rennert mentions fear of obesity as a possible causal factor ( 20 ). Tölle and Windgassen emphasize the pathophysiologic role of body image distortion in their current textbook ( 23 ).
In our sample, eating disorders as distinct diseases are found in all textbooks published after 1974. However, initially, only AN was listed as an eating disorder. Another 40 years elapsed before BED and BN appeared as independent diagnoses, in the current textbook by Tölle and Windgassen ( 23 ). Prior to 1974, disturbed eating behaviors were not categorized as a separate diagnostic condition, even though such behaviors were mentioned as symptoms accompanying a variety of psychiatric disorders.
Disordered Eating in Depressive Disorders
Abnormal eating habits are described extensively as symptoms of depressive disorders. All considered authors mention changes in appetite, food intake or body weight as symptoms of depression. As early as 1803, Johann Christian Reil described loss of weight and emaciation as symptoms of “melancholy” ( 24 ). Johann Christian August Heinroth from Leipzig added reduced appetite a few years later ( 25 ). Over the next 200 years, loss of weight and appetite are consistently mentioned as common features of depression ( 5 , 21 – 35 ). A number of explanations of loss of appetite in depression are discussed. Several authors mention delusions of poverty, leading to patients fearing they will die of starvation ( 20 , 24 , 28 , 29 ). Reil describes a patient who believed that voluntarily starving oneself to death was preferable to succumbing to the starvation that inevitably and inexorably accompanied (imagined) dire poverty. As a potential therapeutic approach, Reil suggested reassuring the patient the food provided was free of charge ( 24 ). Loss of appetite and weight were linked to feelings of guilt. Wilhelm Griesinger and Krafft-Ebing, the former acknowledged as a pioneer of scientific psychiatry, described fasting as a strategy of sinners to atone for their sins ( 26 , 28 ). Religious motives are also mentioned by Emil Kraepelin ( Figure 2 ) and persist in Rennert's 1987 textbook where the conviction of having sinned is seen as a reason for loss of appetite, along the lines of a penitential fast [( 20 ), p. 278, ( 29 )]. Finally, several psychiatrists mention delusions of worthlessness ( Mikromanie ) as a reason for reduced food intake. Affected patients believe they don't deserve food ( 27 , 29 , 31 , 35 ). Krafft-Ebing describes this, in extreme form, as based on nihilistic delusions. Affected patients deny their very existence, negating the need for food [( 28 ), vol. 2, p. 28]. Thus, delusions are presented as one definitive explanation for food refusal in depressive patients.
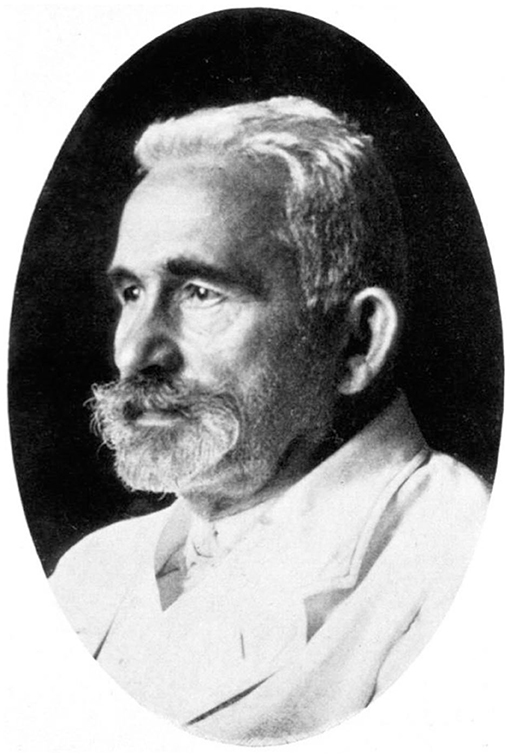
Figure 2 . Emil Kraepelin measured body weight attentively in order to comprehend the course and prognosis of mental disorders, at the beginning of 20th century. Source: In public domai, URL: https://wellcomecollection.org/works/mw4ah4kq .
Krafft-Ebing formulated a remarkable approach to monitoring the course of depressive illness, regularly measuring body weight for early detection of depressive episodes. In 1879 he states that a masked depression ( larvierte Depression ) may initially present somatic symptoms, even before characteristic symptoms of depressed mood occur. Thus, “those swallowed tears, those inner wounds that have been covered by smiles, pride and lies for an extremely long time” can lead to emaciation, digestive problems, amenorrhea or irregular menstruation before mood alteration occurs [( 28 ), vol. 1, p. 129]. Such physical findings are also referred to in Frank Schneider's current textbook as typical somatic complications of AN [( 5 ), p. 424]. However, food intake does not play a key role in Krafft-Ebing's account of masked depression, so it does not appear to constitute an early depiction of AN.
Food Refusal as a Suicidal Act
Beginning with Heinroth, food refusal as a suicidal act was a focus of attention in the 19th and early 20th century ( 25 – 30 ). Heinrich Neumann from Breslau, founder of the concept of unitary psychosis, held that the danger of suicide persisted even after beginning force feeding, since the patient could fall back on suicide methods other than food refusal [( 27 ), p. 207]. Krafft-Ebing considered food refusal a rare form of suicidal act [( 28 ), vol. 2, p. 28]. Kraepelin names suicide as one of the most frequent motives for the refusal to eat [( 29 ), vol. 1, p. 618]. Kraepelin is the only author to mention suicide by eating inedible objects such as “nails, stones, fragments of glass, animals,” providing the patient could consciously overcome feelings of disgust [( 29 ), vol. 1, p. 364]. Suicide by starvation associated with depression is not mentioned in the later textbooks. It was not until 1987, that Rennert claimed that food refusal may be an accompaniment of suicidal intent in patients with anorexia [( 20 ), p. 457]. Finally, Tölle and Windgassen explicitly mention eating disorders in their chapter on suicidality where they refer to anorexia nervosa as a form of “chronic suicide.” Obesity is also noted as a possible variant of this suicide type [( 23 ), p. 100, 126].
Disordered Eating Behavior in Schizophrenia
Altered eating behavior is also found in descriptions of schizophrenia, mostly in relation to reduced food intake. Delusions and hallucinations are implicated as valid explanations. In 1818, Heinroth states the preoccupation with intense delusions in “madness (paranoia)” may lead to neglect of sleep and eating. Furthermore, abeyance of appetite can occur as a result of incessant preoccupation with supernatural phenomena and religious writings [( 25 ), vol. 1, p. 296–304].
A number of authors link the content of delusions to possible effects on eating ( 15 , 17 , 18 , 21 – 24 , 28 ). Griesinger describes delusions of poisoning and that human flesh had been offered to eat, as leading to food refusal [( 26 ), p. 77–83]. Neumann considered delusions to be the most common reason for food refusal. In addition, he describes strategies to persuade affected patients to eat. The treating physician might partake of the food on offer to convince the patient it is safe. One patient had even devised his own strategy to circumvent starvation, solely eating eggs, since these could not contain human flesh [( 27 ), p. 206]. Krafft-Ebing describes delusions that one's own body does not exist or has already died, and delusions of poisoning associated with paranoia as leading to food refusal. He also notes that certain delusions could lead to increased appetite. Affected patients were convinced of “having several children in their womb, or of being double bodied” [( 28 ), vol. 1, p. 65f., 103]. Reil had previously described a patient with a delusional belief of double existence, who ate double the normal serves of food [( 24 ), p. 80]. Overall, however, delusions causing reduction in food intake dominate in the literature considered. Describing “dementia praecox” (DP), Kraepelin mentions the example of a delusion of state-organized poisoning. Under the “paranoid form” of DP he mentions that a delusion of poisoning may result in only certain foods being eaten or food intake ceased, worsening the overall disease prognosis [( 29 ), vol. 3, p. 696, 842, 896]. In 1941, August Bostroem emphasized food refusal not only as a complication, but also an indication for in-patient treatment in patients with schizophrenia [( 32 ), p. 194]. Gerd Huber describes various vegetative symptoms that may occur in the course of schizophrenia: “Loss of appetite, nausea and vomiting, constipation and diarrhea.” Food intake may be increased or decreased and sudden changes in eating habits may occur [( 21 ), p. 165f.]. In the second half of the 20th century, Huber and Rennert describe delusions of poisoning as a symptom of schizophrenia [( 20 ), p. 278, ( 21 ), p. 177]. Tölle and Windgassen also discuss a link between these conditions [( 23 ), p. 198]. Thus, delusions of poisoning have been consistently regarded and taught as a symptom of schizophrenia in the past 200 years of German academic psychiatry and often linked to eating behavior.
Gustatory and auditory hallucinations in schizophrenia are also cited as potential triggers of disordered eating ( 20 , 21 , 26 – 28 ). This primarily involves the perception of unpleasant tastes. For example, Griesinger notes tastes that are “disgusting, metallic, pungent, rotten, earthy.” Gustatory hallucinations involving a pleasant taste were much rarer [( 26 ), p. 83f.]. In the mid-19th century, Griesinger, Neumann and Krafft-Ebing discussed gustatory hallucinations as leading to delusions of poisoning [( 26 ), p. 83, ( 27 ), p. 115, ( 28 ), vol. 1, p. 66, 104], only for mention of this link to fall into abeyance for the next 100 years until Huber and Rennert discussed gustatory hallucinations triggering refusal to eat [( 20 ), p. 278, ( 21 ), p. 177].
Neumann also described auditory hallucinations as the basis of a case of food denial. Voices stated there was human flesh in the food and commanded a food ban [( 27 ), p. 116]. A few years later, Krafft-Ebing described voices prohibiting food on religious grounds [( 28 ), vol. 2, p. 28].
Abnormal eating habits are also found in the descriptions of catatonic and hebephrenic forms of schizophrenia by the great nosologist Kraepelin. In hebephrenic schizophrenia ( läppische Verblödung ), food intake may fluctuate considerably, corresponding to phases of increased and decreased appetite. In megalomania, patients may deny needing food, insisting they are fueled by “supernatural power.” In catatonia, delusions of poisoning are occasionally found [( 29 ), vol. 3, p. 768–76, 810]. Some patients would consume inedible substances, even their own excretions. Patients may rigorously enforce refusal to eat by clenching their teeth, protesting they are neither hungry nor require food [( 29 ), vol. 3, p. 816–29]. Three other leading German psychiatrists, Eugen Bleuler, Karl Leonhard and Manfred Bleuler, describe food denial in patients with catatonia [( 22 ), p. 198, ( 31 ), p. 106, ( 34 ), p. 121]. Kurt Kolle mentions “pubertal anorexia” (“ Pubertätsmagersucht ”) as a special form of schizophrenia in his textbook from 1955. Describing emaciation and food deprivation as its core symptoms, he discusses parallels to hebephrenic schizophrenia and a possible common pathophysiology. Eating disorders as a distinct category of mental disorders are not described by Kolle ( 19 ).
Increased Appetite in Mania
Descriptions of bipolar disorder, formerly referred to as “mixed states” or “circular insanity” report less consistent connections to eating behaviors. Many authors describe an increase in appetite during a manic phase ( 25 , 26 , 28 , 29 , 34 , 35 ). Griesinger regarded increased appetite as a symptom of mania, attributing it as a lack of satiety [( 26 ), p. 64, 224]. However, he noted that some manic patients cited their great appetite as justification for their claim not to suffer from any disease. Several authors in the first half of the 20th century described reduction of appetite during a manic phase. According to Eugen Bleuler, patients with mania ate not to appease their hunger, but rather in order to occupy themselves. “Submanic” patients with moderate activity, on the other hand, showed a diminished eating behavior [( 31 ), p. 359]. In 1941, Oswald Bumke described a lack of appetite during mania, leading to weight loss [( 33 ), p. 279–88]. The authors of recent textbooks again see mania linked with increased appetite. According to Leonhard, internationally known for his differentiated classification of endogenous psychoses, this could lead to a more vital appearance of the patient [( 34 ), p. 90]. In 1987, Rennert even describes “greed” as a symptom in manic patients [( 20 ), p. 278], however, weight gain is not described as a typical consequence of the increased appetite. Most psychiatrists rather considered weight loss a sign of mania ( 26 , 28 , 31 , 33 – 35 ). A possible explanation for this apparent contradiction can be found in Hans Hoff's textbook, describing increased metabolism in manic patients [( 35 ), p. 403]. Kraepelin alone offers the more nuanced description of increased weight in milder cases of mania, while more severe cases are associated with weight loss [( 29 ), vol. 3, p. 1228].
Disordered Eating Behavior in Descriptions of Historical Disease Categories
In addition to these psychiatric diagnoses that are well-known today, abnormal eating habits have also been described in diseases that are no longer diagnosed in the present day, have been dissolved into other concepts or bear another name.
Kraepelin describes “neurasthenia” as a disease state, caused by overload of the human body and mind, resulting in exhaustion and loss of performance. Another symptom is lack of appetite; prolonged refusal to eat may also cause stomach discomfort, which can be counteracted by eating small amounts of food frequently [( 29 ), vol. 4, p. 1401, 1465]. According to Oswald Bumke, malnutrition is not only a symptom but may cause neurasthenia. He also mentions stomach discomfort as a possible symptom in addition to other vegetative disorders in the cardiovascular system and gastrointestinal tract, with decreased appetite being the generic consequence [( 33 ), p. 297]. Hans Hoff departs from this description of neurasthenia. He too describes manifold symptoms of the digestive tract, such as stomach pain or gastroesophageal reflux. However, with respect to eating behaviors, Hoff describes as typical a “ravenous appetite” at night resulting in overweight. Rumination of already eaten food may also occur [( 35 ), p. 589]. The last textbook in our series with an entry for “neurasthenia” was published in 1974 by Gerd Huber. Therein he states that both reduced and increased appetite can be observed in this disease, manifesting as “loss of appetite” or “bulimia and polyphagia.” He brackets neurasthenia and anorexia mentalis as typical representatives of psychiatric disorders showing both physical and psychiatric symptoms [( 21 ), p. 258–64].
In the 19th and early 20th century, occasional descriptions of abnormal food intake are found in “hypochondria.” Griesinger described heart problems, headaches and sleep disturbances as well as indigestion and lack of appetite as possible symptoms of this condition. Weight loss only occurred in cases of concurrent physical illness [( 26 ), p.159 f.]. According to Neumann, on the other hand, patients with hypochondria focus on meticulously choosing the foods eaten [( 27 ), p. 95, 160]. Krafft-Ebing describes a preference for inedible food. Patients consumed “spiders, toads, worms, human blood,” as they hoped for a healing effect [( 28 ), vol. 1, p. 66]. Furthermore, hypochondriacal symptoms could also occur in other psychiatric disorders. Krafft-Ebing describes “hypochondriacal melancholy” as an example: Affected patients claimed that their intestines were blocked and therefore they could not eat anything [( 28 ), vol. 2, p. 28]. Eugen Bleuler describes a case of “schizophrenic hypochondria”: one patient was convinced that she was suffering from an ileus and that the food in the intestine was going to rot. Subsequent intake of laxatives led to weight loss [( 31 ), p. 320]. More generally, Karl Jaspers, well-known today for his seminal work on descriptive psychopathology, mentions hypochondriacal symptoms as a complication of psychiatric illnesses that could cause severe weight loss [( 30 ), p. 129].
Descriptions of abnormal eating habits are also found in accounts of “hysteria.” Although Kraepelin viewed hysteria as an inconsistently described disease, he regarded instability of affect as its cardinal symptom, which could cause both mental and somatic sequelae. Affects could perturb body functions: Thus, “nausea, choking movements, and vomiting” would be an expression of disgust, loss of appetite a sign of sadness [( 29 ), vol. 4, p. 1548–56]. Ingestion of food may be blocked by spasm of the esophagus, and vomiting was a frequently observed symptom. Nutritional status might only be slightly impaired, but in some cases could be greatly reduced. Further, the amount of food eaten by patients could be reduced over months or years so extensively that it was barely sufficient for survival. Young women most commonly suffered from this disease, with amenorrhea a typical complication. To treat the above symptoms, Kraepelin recommended a “mast cure” (a fattening diet regime) [( 29 ), vol. 4, p. 1598–603, 1697]. Eugen Bleuler also saw vomiting, refusal of food and difficulty swallowing as symptoms of “hysteria.” However, metabolism would be down-regulated in affected patients so that the weight remained constant [( 31 ), p. 380–7]. Jaspers was concerned with the causes of vomiting, which he too regarded as a symptom of “hysteria.” A stressful feeling that occurs during ingestion would be suppressed and could manifest later through months of vomiting [( 30 ), p. 176]. Bumke's explanation for food refusal was that whilst a self-injurious behavior it served primarily to attract attention. On the other hand, when alone, the patient would eat secretly and deliberately, intentionally deceiving those around them [( 33 ), p. 212f.]. Hans Hoff describes “hysterical anorexia” as a special form of “hysteria” with some parallels to AN. It typically occurred following puberty in young women, who were averse to maturing to womanhood, denying food in order to delay the development of their body. This process would happen unconsciously and might lead to an “endogenous anorexia” [( 35 ), p. 618].
Somatic Conditions and Altered Brain Function
In addition to psychiatric disorders, somatic conditions are discussed as possible triggers of altered eating behavior, especially diseases of the gastrointestinal tract, endocrinological disorders, and lesions of the brain and pituitary gland.
Pathologies of the gastrointestinal tract were particularly seen as responsible for changes in eating behavior in the 19th century. According to Reil, increased appetite may occur due to increased activity of the nervous system in the gastrointestinal tract [( 24 ), p. 258]. By contrast, Krafft-Ebing considered hypersensitivity of the gastric nerves to cause decreased appetite, leading to a premature feeling of satiety [( 28 ), vol. 1, p. 66]. He also cited inflammatory changes in the gastrointestinal tract, which were also discussed by Kraepelin and Griesinger as a plausible cause of loss of appetite [( 26 ), p. 327, ( 28 ), vol. 1, p. 204, ( 29 ), vol. 1, p. 618]. In addition, pain could trigger refusal to eat. According to Griesinger, pain sensations could impair food intake and lead to weight loss [( 26 ), p. 29]. Neumann emphasized that abdominal pain in particular could have a significant impact on a person's nutritional status, although gastrointestinal diseases could also lead to increased appetite [( 27 ), p. 59, 79].
In the 20th century, more attention was devoted to the brain than to the gastrointestinal tract. In particular, brain lesions were cited as a somatic cause of altered eating habits. Both increase and decrease in appetite were considered possible. According to Bumke, emaciation may occur as a result of degeneration of brain areas associated with vegetative functions [( 33 ), p. 387]. More generally, Huber stated that a disturbed appetite may result from local brain damage [( 21 ), p. 49]. According to Bostroem, an increased appetite could occur in the course of a frontal-brain lesion and may cause a craving for food [( 32 ), p. 23]. Hoff described a lesion of the diencephalon as a possible trigger for periodic food cravings [( 35 ), p. 195]. According to Leonhard, increased intracranial pressure could increase or decrease appetite [( 34 ), p. 228].
In addition, panhypopituitarism (“Morbus Simmonds”), a hypofunction of the hypophysis, was previously considered responsible for emaciation. In the 1940's however, Bostroem and Leonhard described personality changes, altered affectivity and cognition as symptoms of the disease, but did not mention possible effects on body weight [( 32 ), p. 60, ( 34 ), p. 140]. Not until 1974 did Huber cite pituitary disease in the differential diagnosis of “anorexia mentalis” [( 21 ), p. 271]. Even Manfred Bleuler did not equate these two clinical pictures. Rather, he emphasized that AN is psychogenic in origin and not an endocrinopathy. Pituitary hypofunction may be considered as a differential diagnosis [( 22 ), p. 357]. Rennert also considered “Simmond's cachexia” in 1987 as a differential diagnosis of anorexia [( 20 ), p. 278]. In the current textbook by Frank Schneider, panhypopituitarism only receives historical attention along the lines that at the beginning of the 20th century, anorexia was attributed to malfunction of the pituitary gland according to a publication by the Hamburg pathologist Morris Simmonds. Diseased patients were treated with hormonal therapies or even pituitary transplants, whereas psychotherapy was not used [( 5 ), p. 422].
Appetite and Body Weight as a Prognostic Factor
In the first half of the 19th century, Heinroth and Neumann regarded body weight and appetite as prognostic markers: they describe increasing appetite and weight as a sign of convalescence in patients with “melancholy” [( 25 ), vol. 1, p. 335]. According to Neumann, the body weight may even exceed the original weight before the disease [( 27 ), p. 189]. Krafft-Ebing, Kraepelin and Jaspers extended the prognostic significance of body weight to all psychiatric illnesses. In the presence of improved psychopathological state, weight gain would be a sign of healing. In the views of Krafft-Ebing and Kraepelin, weight has such prominence that they doubt that successful cure of a mental illness without increase in bodyweight is possible [( 28 ), vol. 1, p. 214f, ( 29 ), vol. 1, p. 445, ( 30 ), p. 327]. The most unfavorable constellation is considered to be increasing body weight with unimproved psychopathological state, indicating the persistence of the mental disorder [( 28 ), vol. 1, p. 215, ( 29 ), vol. 2, p. 892, ( 30 ), p. 130].
Kraepelin reported from his clinical research that body weight could reflect the course and severity of psychiatric disorders. In his four-volume textbook there are illustrations of weight curves with descriptions of the associated course of the disease. Figure 3 illustrates this with regard to a case of “periodic insanity,” an historic diagnosis that resembles today's concept of bipolar disorder. The graph illustrates fluctuations in weight during the course of the disease. The first weight loss represents a manic phase followed by increase in weight indicating a remission. The second drop, on the other hand, represents a depressive phase. The severity of a disease can be measured by the amount of weight fluctuation. Figure 4 describes similar observations in a recurrent depressive disorder with minor and major episodes of symptoms.
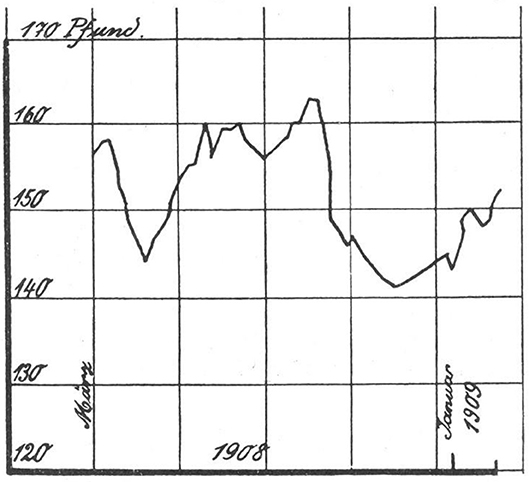
Figure 3 . Weight fluctuations in periodic insanity, as reported by Kraepelin. Abscissa: time [~ 1 year]; Ordinate: bodyweight [pounds]. The first drop in weight occurred during a manic phase, with weight regained in convalescence, followed by significant weight loss during a more prolonged major depressive episode. Source: Obtained from [( 29 ), vol. 3, p. 1231].
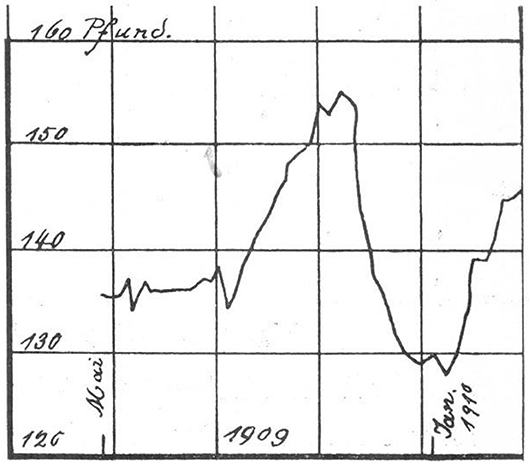
Figure 4 . Abscissa: time [~ 1 year]; Ordinate: bodyweight [pounds]. According to Kraepelin, changes in weight indicate the severity of psychiatric symptoms: Whilst the first two slight weight drops occur in mild depressive phases, the following rapid and substantial weight loss represents a severe depressive episode. Source: Obtained from [( 29 ), vol. 3, p. 1231].
In the time following Kraepelin's interest in body weight, the tenet that weight can be a marker for severity and prognosis largely disappears from view. Bumke strongly states the contrary case, that in patients with schizophrenia, weight fluctuations are completely independent of psychiatric symptoms [( 33 ), p. 572]. In later textbooks, weight is no longer mentioned as a prognostic factor in mental disorders.
The review of textbook entries confirms that diet and especially altered eating habits have been addressed in German psychiatric textbooks throughout the past 200 years. The main findings are summarized in Table 2 .
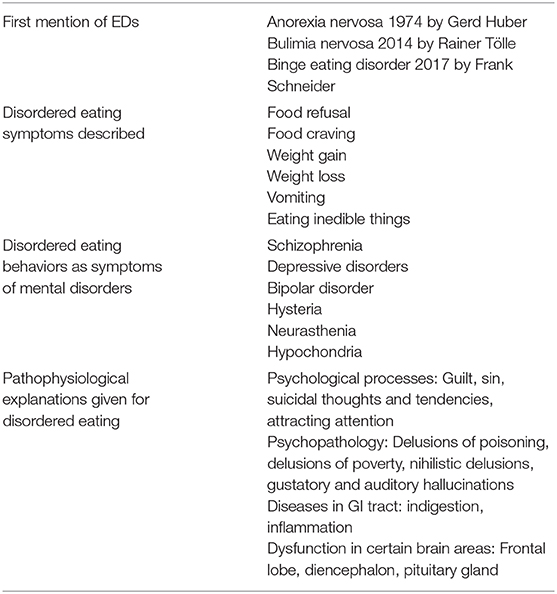
Table 2 . Summary of main findings of review of eating disturbance and disorder content in textbooks.
As early as 1879 Krafft-Ebing dedicated a separate chapter in his textbook to disordered eating ( Figure 5 ). In particular, he regarded the nutritional status and appetite as markers for mental health and the prognosis of psychiatric disorders. Changed eating habits, however, were not regarded as an independent disease entity, but rather as symptoms of other mental or somatic diseases. This view has been maintained for almost a century. Only in 1974 Gerd Huber mentions “Anorexia mentalis” as a specific disorder in his textbook [( 21 ), p. 270f.].

Figure 5 . Richard von Krafft-Ebing addressed disordered eating extensively, dedicating a distinct chapter to this topic in his textbook of 1879. Source: In public domain, URL: http://resource.nlm.nih.gov/101420138 .
In German-speaking psychiatry, eating disorders were mentioned occasionally, as an article by Anton Stichl from 1892 shows: His article on the “Anorexia mentale,” describes the fear of being fat as a causal factor and named self-induced vomiting and lack of insight as characteristics of the disease. This description of the AN is still valid today and let Stichl's publication appear very modern ( 1 , 36 ). Overall, however, only a few German-language articles featured eating disorders well into the 20th century ( 14 ). Our review shows clearly that this also applies to the published textbooks of that time.
This is in contrast to the developments in other European countries, especially France and England: There, Gull and Lasègue described “anorexia hysterica” and “anorexia nervosa” almost simultaneously in 1873 and 1874. Their descriptions resemble today's concepts of AN in many respects, emphasizing the psychogenesis of this disease and rejecting somatic explanations like a disease of the gastrointestinal tract. They also described the therapy as difficult due to a lack of insight and mentioned typical complications such as constipation and amenorrhea ( 37 , 38 ). The publications aroused great interest in France and England, and numerous articles on this “new disease” were published in specialist journals [( 13 ), p. 204–13].
The late reception in German speaking psychiatry however is particularly noteworthy due to its leading contributions in fields like descriptive psychopathology, diagnosis and neurosciences.
In the following we want to explain reasons for this particular development in the German-speaking world.
The Role of Somatic and Psychosomatic Medicine in German-Speaking Countries
There is no single universal explanation for the sparse and late reception of eating disorders in the German-language literature. Rather, multiple factors and historical circumstances must be taken in account. An important factor is that eating disorders were not considered the preserve of psychiatrists in German-speaking countries, a review of AN treatment at the end of the 19th century indicated that pediatricians, gynecologists and in particular internists dedicated themselves to those diseases ( 14 ). It is likely the multiple physical complications of AN aroused the interest of somatic doctors, thus DSM-5 lists anemia, amenorrhea, constipation, abdominal pain, cold intolerance, hypotension and hypothermia [( 1 ), p. 343]. Also, until the early 1900's, diseases presenting with cachexia were commonplace and sometimes occult, most notable tuberculosis. Therefore, it was a challenge for the attending physicians to determine whether emaciation was caused by reduced food intake or by a physical disorder, reducing diagnostic clarity.
Another special feature of the German health system is that psychosomatic medicine is established as a medical specialty separate from psychiatry. Psychosomatic medicine deals with psychological, social and biological influences on body functions and the development and therapy of somatic diseases ( 39 ). The term “psychosomatic” was introduced by Heinroth, whose 1818 textbook was included in our study. Heinroth urged that diseases should be grasped holistically in their somatic and psychological dimensions and special attention should be paid to the patient's biography. Thus, he saw many mental illnesses conditioned by the individual life stories of the affected patients [( 40 ), p. 60]. Psychosomatic medicine has thrived to become an important independent medical specialty in the German-speaking world ( 41 , 42 ) and has played a dominant role in the treatment of eating disorders. In the past as well as in present day, patients with eating disorders have been treated not only in psychiatric hospitals but also in psychosomatic clinics. This has resulted in a net reduction of involvement of psychiatrists in the diagnosis and treatment of ED, which may explain their reluctance to address this issue.
Coverage of Disordered Eating and Eating Disorders in Textbooks
The extent to which the authors of textbooks include disordered eating behaviors in their narratives varies widely. Analysis of the texts reveals continuities, discontinuities and differences over the two centuries. At the beginning of the 19th century, authors mentioned disordered eating behavior only sporadically. Reil, the originator of the term “psychiatry,” made important contributions to neuroanatomical research and was anxious to assign the corresponding correlate in the nervous system to certain body functions and symptoms [( 43 ), p. 19–23]. It is therefore traceable that Reil hypothesized increased appetite signified an overactive nervous system in the gastrointestinal tract in his textbook from 1803 [( 24 ), p. 258]. In the period following Reil, German psychiatry was influenced above all by the psychicists ( Psychiker ), who regarded psychiatric illness in primarily moral terms, as a result of disobedient and godless behavior [( 43 ), p. 35f.]. Heinroth is a leading representative of this movement, for example describing the “starvation cure” as a therapeutic procedure to make disobedient patients docile. Patients on a severely restrictive diet would perceive hunger as a punishment for their behavior, notice their need for help and dependence, and consequently end their disobedient behavior [( 25 ), vol. 2, p. 111–24]. On the other hand, the starvation cure had not only an educational function: According to Neumann, it can be seen as a form of asceticism, which would allow the patient to concentrate on the essential. Therefore, the starvation cure was not a pure punishment, but should also encourage the patient's mindfulness. Besides promoting therapies based on strict moral elements and drawing on religious precepts, Heinroth was one of the first psychiatrists to adopt an individual, patient-oriented approach. He interpreted mental disorders as a result of past pathogenic experiences and consequences of behaviors in the patient's life. This led him to advocate consideration of the patient's biography, social circumstances and lifestyle in tailoring therapy ( 41 ). He states in his textbook: “Very much depends on detailed knowledge of the individual situation of the ill person. Often this exclusively explains the whole illness (or at least the most relevant factors) and clearly indicates what will benefit or harm them.” [( 25 ), vol. 1, p. 44]. The therapy should be arranged in a manner that “The entire treatment of the ill person is tailored to the specifics of the illness (.). The factors considered include sex, age, constitution, temperament, most importantly the personality, that is the character, cultivation of the mind, inclinations and habits, finally the individual circumstances of the ill person.” [( 25 ), vol. 1, p. 3] Additionally, he made use of activation, fostered the mental powers of his patients and applied other strategies still used in modern cognitive, behavioral and conversational therapy ( 44 ). However, despite Heinroth's promulgation of these therapeutic tools in general, there is no evidence as to whether he applied them specifically to address disordered eating behavior.
A more comprehensive study of abnormal eating behavior begins in the mid-19th century, starting with Griesinger and continuing with Neumann, Krafft-Ebing and Kraepelin with the topic increasing in importance. It is noteworthy that all four authors considered reduced food intake as a trigger for psychiatric illness. This pathophysiological approach is not represented in the earlier or later literature, with the exception of Schneider's current textbook [( 5 ), p. 526]. For Griesinger, this approach exemplifies his psychiatric work, he was one of the leading somaticists ( Somatiker ) who aimed for a scientific basis of psychiatry and interpreted psychiatric disorders as arising from somatic conditions [( 45 ), p. 43–9]. Therefore, it is not surprising that Griesinger considered inadequate nutrition as a possible cause of “melancholy” [( 26 ), p. 153]. However, Griesinger was by no means a pure materialist. He also considered psychological aspects in the pathogenesis of mental disorders: “We consider psychological causes to be the most frequent and productive sources of insanity, both as predisposing factors and most importantly as immediate precipitants of the disease.” [( 46 ), p. 169]. Furthermore, Griesinger emphasized that pathogenesis is strongly subjective and that the observed triggers of mental disorders “are most diverse: sometimes it is a suddenly aroused anger, fright or sorrow in response to an insult, financial loss, shame, a sudden death” [( 46 ), p. 169].
Another achievement of Griesinger was the establishment of asylums attached to small towns (“Stadtasyle”): He did not support the prevailing model of custody of psychiatric patients in remotely located madhouses, instead promoting asylums “preferably in the immediate neighborhood of a small town (.), in order to stay in touch with its habitants” [( 46 ), p. 532]. This reflects Griesinger's early appreciation and enforcement of patients' personal autonomy. Kraepelin gives the most extensive account of disordered eating behavior, albeit his four-volume work is also by far the largest of the textbooks included here. Kraepelin is well-known as the founder of empirical, experimental and scientifically founded psychiatry. In particular, he was interested in the detailed study of the course of diseases [( 43 ), p. 106ff.]. Body weight served Kraepelin as an objective parameter to understand the course of a mental disorder and to frame a prognosis, emphasizing his systematic and scientific approach to psychiatry.
By contrast, in the first half of the 20th century a markedly reduced interest in disordered eating is evident in the psychiatric textbooks selected for in this study. This may be explained by a peculiarity of German-speaking psychiatry history. From 1914 to the mid-20th century, reduced food intake in the sense of AN was not seen as a psychiatric illness, but rather as a symptom of hypopituitarism. The Hamburg pathologist Morris Simmonds had published an article in 1914 in which he reported lethal food refusal due to a malfunction of the pituitary gland, known as “Morbus Simmonds” in the German speaking world and panhypopituitarism in English ( 47 ). This publication was particularly well-received in Germany, leading to neglect of psychogenic factors in anorexia ( 48 ). Most patients with AN were treated by medical disciplines other than psychiatry. At the Charité in Berlin, the famous surgeon Ferdinand Sauerbruch performed transplantation of pituitary glands. In this case, a calf or cattle pituitary gland was transplanted into the greater omentum. A therapeutic effect, ranging from short-lasting weight gain to complete healing was described. Previously, conservative methods such as oral ingestion of pituitary extract and sugar solutions had already been attempted ( 49 ). Even during the post-war period, changes in eating behavior made only marginal appearances in psychiatry textbooks and EDs haven't been described as distinct mental disorders in German textbooks at all ( 19 , 34 , 35 ). Not until the mention of “Anorexia mentalis” by Gerd Huber, did eating disorders receive increasing attention in the German literature and recognition as distinct disorders. Some perspectives still seem current from today's perspective, while others can be considered obsolete: The rejection of physical development to womanhood, as emphasized by Huber as a core symptom, is not mentioned in the DSM-5. Instead, disturbed body image as well as the fear of getting fat are included in diagnostic criteria for AN ( 1 ). On the other hand, Huber's description that “anorexia mentalis” can turn into an addiction in the course of the disease appears highly topical. It is subject of current research, which investigates possible connections between these two clinical pictures. Godier and Park identified parallels between addictions and AN in a clinical study, including loss of control, functional impairment, self-harming behavior, and occupational and social limitations as intersections of both disease entities ( 50 ).
Rennert also emphasizes an “addictive process” in 1987 in patients with AN. It is also striking that he does not list any physical illnesses, such as a disturbed pituitary function, as a possible cause of the disease. Rather, he sees “contact-weak, even defiant, idiosyncratic, ambitious, egoistic or anankastic, hypochondriacal and sensitive characters” as forming the predisposition to AN [( 20 ), p. 457]. Describing a purely psychogenic pathophysiology, Rennert is the first of our authors to suggest psychotherapy as a therapeutic tool. The importance of circumscribed areas of the brain in appetite regulation is discussed again in Schneider's current textbook. It highlights the importance of the hypothalamus as well as orexigenic and anorexigenic hormones. However, cognitive behavior therapy is acknowledged as the most effective treatment [( 5 ), p. 422].
The Presentation of Food Denial as a Dominant Concern
Food supply has varied markedly over the time period of this study. Between 1800 and the 1950's food was often in short supply. For example, during 1816, the “year without a summer” there was a serious famine in Central Europe ( 51 ). Later, at the time of the two world wars, food supply in many parts of Europe was catastrophic and hunger omnipresent. The economic upswing starting in the 1960's has introduced an era of unprecedented abundance of food. Over the same period diseases causing inanition such as tuberculosis and chronic anaemias have reduced markedly in prevalence. The net result has been for psychogenic refusal of food to be more conspicuous and more negatively connoted as pathological, favoring the acceptance of AN into the nosology and AN becomes a distinct diagnosis in German-language psychiatric textbooks [( 21 ), p. 270f, ( 22 ), p. 543f.]. This change in emphasis has also resulted in reduced food intake being less commonly attributed as a symptom of other psychiatric disorders.
The more recent rise in obesity has also focused attention on disorders of excessive eating. Historically, it appears that increased food intake was not considered as deviant behavior for a long time. This is supported by the interpretation of increased food intake as a sign of convalescence in psychiatric disorders as described above, but also by the beauty ideals of past times. In the 19th century, for example, excessive body mass was still considered a sign of prosperity, even wealth, and not regarded as a sign of abnormal eating habits or even a mental disorder [( 52 ), p. 34f.]. In our sample, mention of BN as a condition with increased food intake is found only in the current textbooks by Schneider and Tölle/Windgassen ( 5 , 23 ). Although in 1879, Krafft-Ebing used the term “bulimia” in relation to increased appetite, he did not mention measures to avoid weight gain that are regarded as typical for this disease today ( 28 ). In 1974, Huber still equated “bulimia” with hyperphagia. As early as 1972, Otto Doerr-Zegers had aptly described “Bulimia nervosa” as a distinct mental disorder. He and Gerald Russell are considered to be the first to describe this disease ( 9 , 10 ). As an eating disorder with increased food intake without compensatory behaviors as countermeasures, BED was first listed in DSM-5 ( 1 ). Schneider's latest textbook of 2017 is the only textbook in our sample that mentions this disorder. BED was first described by Albert J. Stunkard who published an apt description of this disease in 1959 ( 53 ). However, it took a long time for BED to be included in the DSM and considered as a discrete entity. In the selected textbooks of the past 200 years of German-speaking psychiatry, this mental disorder played practically no role at all.
Disordered Eating in Mental Disorders
In the textbooks in our sample, decreased food intake and weight loss have been regarded as symptoms of depressive disorders, schizophrenia and somatic diseases. DSM-5 mentions all of those conditions as possible differential diagnoses of AN, underlining that alterations in food intake are still today considered as crucial symptoms of these disorders ( 1 ). Additionally, further overlaps between depressive disorders, schizophrenia, medical conditions and AN have been found, regarding their symptoms, pathophysiology, genetics and possible treatment strategies.
In depressive disorders, severe weight loss can occur. Changes in weight are mentioned as a diagnostic criterion in DSM-5 ( 1 ). Furthermore, depression is the most common comorbidity of patients with AN, prevalence of mood disorders ranging from 31 to 89% ( 54 , 55 ). Comorbid depressive disorder worsens the outcome and prognosis in patients with AN ( 56 ).
Besides the frequent coexistence of these disorders, they share some symptoms, notably menstruation, libido and sleep disturbances occur commonly in both disorders. Shared genetic predispositions ( 57 ) and fluoxetine as a treatment in common for both disorders have been reported ( 58 ).
The feeling of guilt is a typical symptom and a strong indicator of depression ( 1 ). Whether reduced food intake is associated with an increased perception of guilt, as described by Griesinger, Krafft-Ebing, Kraepelin and Rennert ( 20 , 26 , 28 , 29 ) in depressed patients, is of current scientific interest in ED research. In people with AN, guilt, anguish, sadness, fear and anger have been found to be associated with eating ( 59 ). A recent systematic review found that guilt is not consistently linked to AN and BN presentations, but the relationship is unclear due to a lack of data ( 60 ).
Suicidality
Restrictive eating or self-starvation in patients with AN are currently not interpreted as suicidal behavior, as was perceived by the 19th century psychiatrists Heinroth, Neumann, Krafft-Ebing and Kraepelin ( 25 , 27 – 29 ). However, AN has the highest mortality rate amongst all psychiatric illnesses. This is explained by the physical consequences of the disorder, but also the high suicide rate ( 61 ). Suicide attempts are a major issue in EDs ( 62 ), with suicide the second leading cause of death among individuals with AN ( 63 ). Therefore, studies have examined possible risk factors for suicidality in patients with EDs in order to prevent suicides in these patient groups. Known risk factors include frequent purge behavior, poor emotional regulation, childhood abuse and psychiatric comorbidities ( 64 ).
Schizophrenia
Reduced food intake has been listed as a symptom of schizophrenia by numerous authors ( 20 , 21 , 23 , 26 – 29 , 33 ). As explanations, the authors mainly described delusions of poisoning, gustatory hallucinations and command auditory hallucinations ( 21 , 26 – 29 ). From today's perspective, these are still valid reasons for reduced food intake in patients with schizophrenia ( 65 ). Furthermore, overlaps between AN and schizophrenia regarding their symptoms, pathophysiology, genetics, and even their therapy have been discussed recently.
In schizophrenia, eating disorders are much more common than in the general population. Disordered eating is up to 5 times more common in patients with schizophrenia ( 66 ). On the other hand, diagnosable psychotic episodes are reported in 10–15% of AN patients ( 67 ). Additionally, some symptoms of AN resemble those of schizophrenia. These include odd thinking processes, fixed illogical beliefs or deficits in work and social life that can occur in both disorders ( 68 ). Due to these reciprocal findings in AN and schizophrenia, several hypotheses have been discussed as possible explanations: psychoses could be a result of starvation, disturbed body image a result of delusions, extreme fasting a counteraction against weight gain from antipsychotics. AN could even be a prodrome of schizophrenia ( 69 ). One study took up the last thought: In the study group considered, an ED preceded 10%, in 5% this was AN. The ED occurred 4–8 years before schizophrenia in these cases; women were more frequently affected than men. As a distinguishing feature, gustatory hallucinations were found only in the group with premorbid EDs. The authors discussed the possibility that patients could represent a distinct subtype of schizophrenia ( 68 ).
There are also similarities in pathophysiology: Genome-wide association studies (GWAS) in EDs have been used to calculate genetic correlations between different disorders. It is worth mentioning that significant positive genetic correlations were observed between AN and schizophrenia which suggests an overlap in the biological pathophysiology of both disorders ( 70 , 71 ).
Furthermore, there are overlaps of AN and schizophrenia concerning both psychotherapies and medication. Aripiprazole and especially olanzapine, two atypical antipsychotics, have been trialed successfully as psychopharmacological treatments of AN and might become the first approved psychotropic drugs for AN treatment ( 72 , 73 ).
Historical Disorders
Although hysteria, hypochondria and neurasthenia are considered historical disorders, and their concepts have emerged in other mental disorders, we have found overlaps with eating disorders. A specific question is whether these historical disorders could represent an early appearance of eating disorders in the literature.
Hysteria was covered extensively in the textbooks published in the first half of the 20th century. Comparing the historic descriptions of hysteria with the modern view on AN, we found overlaps, especially for the binge-eating/purging type of AN. As noted above, the authors described refusal to eat as a common symptom of hysteria, resulting in amenorrhea and severe weight loss. Vomiting was considered a common symptom of hysteria, and is described as a possible purge strategy in patients with AN in DSM-5 ( 1 , 29 , 31 , 33 , 35 ).
On the other hand, we did not find the other main DSM-5 diagnostic criteria, fear of weight gain and disturbed perception of body shape in any of the textbooks. It is possible that in the past patients with AN were diagnosed with hysteria. However, due to the absence of some of the main diagnostic criteria for AN in the descriptions of hysteria, we do not regard this disorder as an early description of AN. Our findings support previous research in the history of psychiatry by Vandereycken and van Deth who discussed possible overlaps between hysteria and eating disorders ( 74 ). They also found food refusal and vomiting listed as typical symptoms of hysteria. However, they found no literature describing a disturbed body shape or a fear of gaining weight in this context. Further, vomiting in hysteria was not primarily directed at weight loss, rather it was demonstrative, aiming to attract attention. This is in direct contrast to the behavior of patients with eating disorders, who vomit and purge covertly. On these grounds, Vandereycken and van Deth considered hysteria to be a historical precursor of conversion disorder and not EDs. In conversion disorder, a shift of psychic conflicts to somatic symptoms is seen as the critical trigger for its manifestation ( 74 ). This pathophysiological explanation was already in use for hysteria: Karl Jaspers wrote that the hysterical vomiting would be a result of “a painful affect that arises during the meal, but is suppressed, then provokes nausea and vomiting, which persists for months as hysterical vomiting” [( 30 ), p. 176]. Hysteria is not viewed as a distinct disorder in the present day, its precepts having been scattered across dissociative or conversion disorder, neurotic disorders or psycho-reactive syndromes, and histrionic personality disorder.
Gastrointestinal Symptoms and Eating Disorders
The textbook authors described numerous gastrointestinal medical conditions as possible triggers for food refusal, especially in the 19th century. Most common explanations for reduced food intake were hypersensitivity of the gastrointestinal nervous system, abdominal pain and gastrointestinal inflammation ( 26 , 28 , 29 ). To the present day, somatic diseases are listed as important differential diagnoses of AN in DSM 5, requiring careful evaluation ( 1 ).
The combination of restricted eating and gastrointestinal symptoms is commonly observed in patients with EDs and often leads to additional pharmacological treatment with antacids, proton-pump inhibitors, antispasmodics, gastroprokinetics, non-absorbable sugar laxative or hyperosmotic laxatives in patients with EDs ( 75 ).
As described by the cited authors in their historic textbooks, the enteric nervous system has a significant impact on appetite. Being part of the “gut-brain-axis,” it registers the amount of consumed food to the CNS. The vagus nerve plays a key role, taking part in the regulation of the digestive system, satiety and food intake ( 76 ). Abnormal function of the enteric nervous system has been described in patients with AN, including increased sensitivity to gastric expansion and nutrients in the small intestine ( 77 ). This may contribute to the manifestations of eating disorders, though etiological implications are unclear and further research is needed.
Krafft-Ebing, Kraepelin and Griesinger discussed inflammatory changes in the gastrointestinal tract as pathophysiological factors resulting from changes in food intake and eating behavior ( 26 , 28 , 29 ). This could be seen as an early scientific hypothesis that inflammation is involved in the pathophysiology of eating disorders. This idea is currently followed by researchers focusing on cytokine changes in EDs ( 78 ), discovering immunologically important genes as relevant in AN ( 79 ) and exploring the role of the gastrointestinal microbiome in the development of EDs ( 80 ).
EDs and Brain Areas
In the German textbooks of the 19 and 20th century, brain areas with vegetative functions, frontal areas, the diencephalon, and the pituitary gland were seen as decisive for altered food intake and eating behavior by Bumke, Bostroem, Hoff and Huber ( 21 , 32 , 33 , 35 ).
Currently, three main neurocircuits are held to be principally involved in food intake, appetite, body weight regulation and the pathophysiology of EDs: These are the self-regulation, hedonic and homeostatic systems.
The self-regulation system embeds eating in the social context, creates individual values and performs self-regulatory control. Its main center lies in the prefrontal cortex ( 58 ). It has been debated whether the enhanced control of food intake in patients with AN might be an effect of augmented control in general ( 81 ). An fMRI study showed that patients with AN have deviant folding in the prefrontal cortex, persistent even after weight gain and possibly of pathophysiological significance ( 82 ). On the other hand, reduced self-regulatory control has been put forward as a neurocognitive feature of BN and BED. In particular, the uncontrolld binge eating that occurs in these disorders suggests reduced control over behavior. Recent findings of an fMRI study underline the possible impact of the self-regulatory system in BN: Reduced thickness in parts of the prefrontal cortex (orbitofrontal cortex, inferior frontal cortex) was associated with more frequent manifestation of BN symptoms in patients ( 83 ).
The function of the hedonic system is to elicit the desire to eat and to evoke pleasure during food consumption. Its neurons and synapses are found mainly in the prefrontal cortex, basal ganglia and thalamus ( 58 ). In AN, an altered response to reward stimuli is proposed, affecting eating behavior. For patients with AN, food seems to be less rewarding than for the general population. Patients with AN might be able to ignore food-related rewards ( 84 ). Alterations in the reward system do not seem to be confined to eating behavior and persist even after convalescence: A fMRI study showed deviant activity in the reward system when patients were confronted with monetary stimuli ( 85 ). In BED, on the other hand, patients show an increased reward from food intake and hedonic eating behavior, which could explain the increased food intake ( 86 ). For BN, there have been no consistent findings, and studies have found both increased and decreased reward responses to food stimuli ( 87 ).
The homeostatic system integrates peripheral signals of food consumption and energy storages and regulates appetite. The hypothalamus and the pituitary gland play a prominent role in this system ( 58 ).
The historical assumption that AN could be a consequence of hypofunction of the hypophysis is considered obsolete today. Although there have been observed alterations in hypothalamic-hypophysis-axis in patients with AN, this phenomenon is not considered to have a pathophysiological impact. It is rather considered as an non-specific consequence of starvation in patients with AN ( 88 ), a bodily adaptation to decreased food intake and energy deficit, explaining some of the typical somatic complications of AN. Elevated CRH and ACTH levels lead to hypercortisolism, resulting in lowered bone density. Alterations in the pulsatility of LH-secretion contribute to amenorrhea ( 89 ).
From today's point of view, the pathophysiological contributions made by Bostroem and Hoff stand out. In the middle of the 20th century, both authors elucidated brain areas that are still considered to play an important role in food regulation. Bostroem identified frontal brain damage as a possible cause of food cravings [( 32 ), p. 23]. As noted above the prefrontal cortex, as a part of frontal cortex, influences food behavior substantially and is considered to play a role in the pathophysiology of EDs. Hoff, on the other hand, considered lesions of the diencephalon as a possible cause of food cravings [( 35 ), p. 199]. Distinct areas of the diencephalon, namely the hypothalamus and the pituitary gland, are still considered to regulate food intake. This emphasizes the early adoption by Hoff and Bumke of the study of circumscribed brain areas as possible causes or loci of disordered eating. This contrasts with the dominant approach in the 20th century to frame the causality of EDs in terms of social, environmental or cultural issues. Today's research seeks to understand both aspects of this equation in relation to EDs, whereby it is postulated that such social factors, together with increased vulnerability due to altered brain functions, could lead to the manifestation of eating disorders ( 90 ).
Limitations
A systematic literature review according to modern standards is currently not possible for a longitudinal study with historical literature: Historical sources are not included in today's literature databases, the quality standards for scientific work common today did not exist in the past. As a result, the selection of literature using PRISMA guidelines or similar criteria was not possible.
Nonetheless, we have made use of the structured and predefined PRISMA methodical approach as outlined in the PRISMA checklist ( 91 ) by describing the rationale for the review, providing an explicit statement of questions being addressed, defining eligibility criteria of the psychiatric textbooks as information sources and describing the selection and data extraction process. We also summarized the evidence in a structured way, addressed the limitations and drew comprehensible conclusions that are justified by the applied methods and the obtained results. Overall, we applied the PRISMA approach and its philosophy as far as possible to adhere to contemporary scientific quality standards and to provide evidence-based scientific work. But due to the nature of the historic material, a methodological compromise had to be attained. Whilst his may be seen as a limitation it could also be perceived as the result of successful interdisciplinary cooperation.
Historical textbooks are difficult to compare with each other, especially due to the substantially changed terminology over the course of time. For the selection of literature, we decided on the following strategy: We intentionally chose psychiatric textbooks because we wanted to present the knowledge that was considered valid at the time, representing the most common and generally accepted views of medical doctors and psychiatrists on disordered eating in the past 200 years. The resulting inclusion criteria are noted in the methods section. Articles in journals were not taken into consideration, as they did not necessarily represent valid and widespread knowledge. The main intention was not to compare the sources with each other, but rather to chart how disturbed eating behavior has been viewed over the course of the study period, 1803–2017. This allows a representation of progressions, continuities and breaks over time that would not be possible with a cross-sectional study. A further limitation is the small number of publications considered. This makes it impossible to obtain an all-encompassing overview of all the concepts discussed regarding disordered eating behavior. However, by limiting the literature selection to relevant textbooks from acknowledged authors, it is possible to obtain an overview of the predominant and widespread concepts on disordered eating behavior and eating disorders, gaining an impression how patients suffering from those disorders have been diagnosed and treated in psychiatric clinics.
In this article, we have contrasted the content of important German textbooks with the DSM classification even though we are aware that this comparison may be misleading. It would have been more adequate to compare English language textbooks of psychiatry over the same period with their German counterparts, covering the same breadth of perspectives. Similarly, with the French literature, which also has some historical alignment. Such an approach would be highly informative, but it was well-beyond the scope of the current study. The emphasis on the DSM classification was chosen largely to emphasize two points, firstly the convergence of illness concepts in German with those in the English-speaking world and, secondly, to illustrate how much the illness concepts and disease categories of disordered eating are in flux. This may be seen as supporting the need for a detailed historical analysis to illustrate areas of firm agreement over two centuries vs. areas which have only consolidated in the past decades.
Although AN was first described in the late 19th century and received broad attention in France and the United Kingdom, it took a long time until AN was recognized as a distinct mental disorder in German-speaking psychiatry. We found the first mention in Huber's textbook of 1974, a full century after its first description in France and England. BN and BED appeared only recently in German textbooks. However, throughout the past two centuries, disordered eating has been recognized as a symptom of various mental disorders, including those classified today as depressive disorders, schizophrenia and bipolar disorder. Interestingly, there are numerous overlaps between those mental disorders and EDs, and DSM-5 features some of them as possible differential diagnoses. Similarities can be found in their genetics, pathophysiology, symptoms and therapy, possibly leading to promising new therapeutic approaches for EDs in the future.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Author Contributions
HS and LB conceptualized the study. HS provided methodological advice for literature review, provided information regarding the history of psychiatry, and the selected psychiatrists. HH provided professional support and made additional remarks regarding the current state of scientific knowledge of eating disorders. KK revised language style of the article and provided professional remarks. LB examined the selected textbooks, undertook a literature search, and wrote the first manuscript draft. All authors contributed and have approved the final manuscript.
This work was supported by the German Research Foundation (DFG) and Leipzig University within the program of Open Access Publishing.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank all subjects participating in this study.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5 . Washington, DC: American Psychiatric Publishing (2013). p. 947.
Google Scholar
2. Hay P, Girosi F, Mond J. Prevalence and sociodemographic correlates of DSM-5 eating disorders in the Australian population. J Eat Disord. (2015) 3:19. doi: 10.1186/s40337-015-0056-0
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Smink FR, van Hoeken D, Hoek HW. Epidemiology, course, and outcome of eating disorders. Curr Opin Psychiatr. (2013) 26:543–8. doi: 10.1097/YCO.0b013e328365a24f
4. Smink FR, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatr Rep. (2012) 14:406–14. doi: 10.1007/s11920-012-0282-y
5. Schneider F. Facharztwissen Psychiatrie, Psychosomatik und Psychotherapie . Berlin: Springer (2017). p. 725.
6. Castellini G, Lo Sauro C, Mannucci E, Ravaldi C, Rotella CM, Faravelli C, et al. Diagnostic crossover and outcome predictors in eating disorders according to DSM-IV and DSM-V proposed criteria: a 6-year follow-up study. Psychosomatic Med. (2011) 73:270–9. doi: 10.1097/PSY.0b013e31820a1838
7. Schmidt U, Adan R, Böhm I, Campbell IC, Dingemans A, Ehrlich S, et al. Eating disorders: the big issue. Lancet Psychiatr. (2016) 3:313–5. doi: 10.1016/S2215-0366(16)00081-X
8. van Deth R, Vandereycken W. Eating disorders: clinical section. In: Berrios G, editor. A History of Psychiatry . London: Routledge (2008). p. 593–601.
9. Russell G. Bulimia nervosa: an ominous variant of anorexia nervosa. Psychol Med. (1979) 9:429–48. doi: 10.1017/S0033291700031974
10. Doerr-Zegers O. About a particular type of oral perversion in the female: hyperphagia followed by vomitting. Int J Eating Disord . (1994) 16:117–32. doi: 10.1002/1098-108X(199409)16:2<;117::AID-EAT2260160203>;3.0.CO;2-6
11. Allison KC, Tarves EP. Treatment of night eating syndrome. Psychiatr Clin North Am. (2011) 34:785–96. doi: 10.1016/j.psc.2011.08.002
12. Keel PK. Purging disorder: recent advances and future challenges. Curr Opin Psychiatr . (2019) 32:518–24. doi: 10.1097/YCO.0000000000000541
13. Vandereycken W, van Deth R, Meermann R. Hungerkünstler, Fastenwunder, Magersucht: Eine Kulturgeschichte der Essstörungen . München: Taschenbuch-Verl (1992). p. 350.
14. Habermas T, Vandereycken W, van Deth R, Meermann R. Die Anorexia nervosa in der deutschsprachigen medizinischen Literatur des 19. Jahrhunderts. Psychother Psychosom Med Psychol . (1990) 40:466–73.
PubMed Abstract | Google Scholar
15. Gnoth M, Glaesmer H, Steinberg H. Suizidalität in der deutschsprachigen Schulpsychiatrie. Thematisierung in Lehrbüchern von 1803 bis heute. Nervenarzt . (2018) 89:828–36. doi: 10.1007/s00115-017-0425-9
16. Steinberg H. Die Errichtung des ersten psychiatrischen Lehrstuhls: Johann Christian August Heinroth in Leipzig. Nervenarzt . (2004) 75:303–7. doi: 10.1007/s00115-003-1605-3
17. Arens K. Wilhelm Griesinger: psychiatry between philosophy and praxis. Philosophy Psychiatr Psychol . (1996) 3:147–63. doi: 10.1353/ppp.1996.0025
CrossRef Full Text | Google Scholar
18. Ashok AH, Baugh J, Yeragani VK. Paul Eugen Bleuler and the origin of the term schizophrenia (SCHIZOPRENIEGRUPPE). Indian J Psychiatr. (2012) 54:95–6. doi: 10.4103/0019-5545.94660
19. Kolle K. Psychiatrie: Ein Lehrbuch für Studierende und Ärzte . München: Verlag von Urban und Schwarzenberg (1955). p. 349.
20. Lemke R, Rennert H. Neurologie und Psychiatrie sowie Grundzüge der Neuropsychiatrie des Kindes- und Jugendalters: Ein Lehrbuch für Praxis und Studium . Leipzig: Johann Ambrosius Barth. (1987). p. 534.
21. Huber G. Psychiatrie - systematischer Lehrtext für Studenten und Ärzte . Stuttgart: Schattauer (1974). p. 369.
22. Bleuler M. Lehrbuch der Psychiatrie . Berlin: Springer (1983). p. 719.
23. Tölle R, Windgassen K, Lempp R. Psychiatrie: Einschließlich Psychotherapie; mit 12 Tabellen . Berlin: Springer Medizin (2014). p. 434.
24. Reil JC. Rhapsodieen über die Anwendung der psychischen Curmethode auf Geisteszerrüttungen . Halle: Curtsche Buchhandlung. (1803). p. 504.
25. Heinroth JC. Lehrbuch der Störungen des Seelenlebens oder der Seelenstörungen und ihrer Behandlung . Leipzig: Bey Fr Chr Wilh Vogel. (1818). p. 781.
26. Griesinger W. Die Pathologie und Therapie der psychischen Krankheiten . Stuttgart: Verlag von Adolph Krabbe (1845). p. 396.
27. Neumann H. Lehrbuch der Psychiatrie . Erlangen: Verlag von Ferdinand Enke (1859). p. 242.
28. Krafft-Ebing R. Lehrbuch der Psychiatrie . Stuttgart: Verlag von Ferdinand Enke. (1879). p. 490.
29. Kraepelin E. Psychiatrie, ein Lehrbuch für Studierende und Ärzte . Leipzig: Verlag von Johann Ambrosius Barth. (1909–1915). p. 3018.
30. Jaspers K. Allgemeine Psychopathologie . Berlin: Springer (1913). p. 333.
31. Bleuler E. Lehrbuch der Psychiatrie . Berlin: Springer (1916). p. 507.
32. Bostroem A. Kurzgefasstes Lehrbuch der Psychiatrie, von Johannes Lange und August Bostroem . Leipzig: Thieme (1941). p. 274.
33. Bumke O. Lehrbuch der Geisteskrankheiten . München: J. F. Bergmann Verlag (1944). p. 625.
34. Leonhard K. Grundlagen der Psychiatrie . Stuttgart: Verlag von Ferdinand Enke (1948). p. 231.
35. Hoff H. Lehrbuch der Psychiatrie . Basel: Benno Schwabe & Co. Verlag (1956). p. 899.
36. Gugl H, Stichl A. Neuropathologische Studien . Stuttgart: Enke (1892).
37. Gull WW. Anorexia nervosa (apepsia hysterica, anorexia hysterica). Trans Clin Soc London. (1874) 7:22–8.
38. Lasègue E-C. De l'anorexie hystérique. Archi Générales Méd. (1873) 21:385–403.
39. Kapfhammer H-P. Psychosomatische medizin – geschichte, definition, extension, organisation. Psychiatrie Psychother . (2010) 6:216–29. doi: 10.1007/s11326-010-0133-6
40. Ackerknecht EH. Kurze Geschichte der Psychiatrie . Stuttgart: Enke (1985). p. 108.
41. Steinberg H, Herrmann-Lingen C, Himmerich H. Johann Christian August Heinroth: psychosomatic medicine eighty years before Freud. Psychiatr Danub . (2013) 25:11–6.
42. Steinberg H. Die Geburt des Wortes ‘psychosomatisch' in der medizinischen Weltliteratur durch Johann Christian August Heinroth. Fortschr Neurol Psychiatr . (2007) 75:413–7. doi: 10.1055/s-2006-955010
43. Steger F. Prägende Persönlichkeiten in Psychiatrie und Psychotherapie . Berlin: Medizinisch Wissenschaftliche Verlagsgesellschaft (2015). p. 283.
44. Steinberg H, Himmerich H. Johann Christian August Heinroth (1773–1843): the first professor of psychiatry as a psychotherapist. J Religion Health. (2012) 51:256–8. doi: 10.1007/s10943-011-9562-9
45. Payk TR. Psychiater: Forscher im Labyrinth der Seele . Stuttgart: Kohlhammer (2000). p. 376.
46. Griesinger W. Die Pathologie und Therapie der Psychischen Krankheiten . Stuttgart: Verlag von Adolph Krabbe (1861).
47. Simmonds M. Über embolische Prozesse in der Hypophysis. Virchows Arch Path Anat. (1914) 217:226–39. doi: 10.1007/BF01989185
48. Habermas T. Die Anorexia nervosa (Magersucht) in der deutschsprachigen medizinischen Literatur von 1900 bis 1945: Die Rolle der Magersucht in der Entstehung der Psychosomatik. Sudhoffs Archiv . (1992) 76:38–62.
49. Von Bergmann G. Magerkeit und Magersucht. Deutsche Medizinische Wochenschrift . (1934) 60:159–63. doi: 10.1055/s-0028-1129777
50. Godier LR, Park RJ. Does compulsive behavior in Anorexia Nervosa resemble an addiction? a qualitative investigation. Front Psychol. (2015) 6:1608. doi: 10.3389/fpsyg.2015.01608
51. Frommelt F, Hitz F, Kasper M, Thöny C editors. Das Jahr ohne Sommer: Die Hungerkrise 1816/17 im mittleren Alpenraum . Innsbruck: Universitätsverlag Wagner (2017). p. 165.
52. Bruch H. Eßstörungen: Zur Psychologie und Therapie von Übergewicht und Magersucht . Frankfurt am Main: Fischer (2004). p. 389.
53. Stunkard AJ. Eating patterns and obesity. Psychiatr Q. (1959) 33:284–95. doi: 10.1007/BF01575455
54. Kaye W. Neurobiology of anorexia and bulimia nervosa. Physiol Behav. (2008) 94:121–35. doi: 10.1016/j.physbeh.2007.11.037
55. O'Brien KM, Vincent NK. Psychiatric comorbidity in anorexia and bulimia nervosa: nature, prevalence, and causal relationships. Clin Psychol Rev. (2003) 23:57–74. doi: 10.1016/S0272-7358(02)00201-5
56. Brand-Gothelf A, Leor S, Apter A, Fennig S. The impact of comorbid depressive and anxiety disorders on severity of anorexia nervosa in adolescent girls. J Nerv Ment Dis . (2014) 202:759–62. doi: 10.1097/NMD.0000000000000194
57. Watson HJ, Yilmaz Z, Thornton LM, Hübel C, Coleman JR, Gaspar HA, et al. Genome-wide association study identifies eight risk loci and implicates metabo-psychiatric origins for anorexia nervosa. Nat Genet. (2019) 51:1207–14. doi: 10.1038/s41588-019-0439-2
58. Himmerich H, Treasure J. Psychopharmacological advances in eating disorders. Expert Rev Clin Pharmacol. (2018) 11:95–108. doi: 10.1080/17512433.2018.1383895
59. Petry N, Vasconcelos de FA, Costa LD. Feelings and perceptions of women recovering from anorexia nervosa regarding their eating behavior. Cad Saude Publica . (2017) 33:e00048716. doi: 10.1590/0102-311x00048716
60. Blythin SP, Nicholson HL, Macintyre VG, Dickson JM, Fox JR, Taylor PJ. Experiences of shame and guilt in anorexia and bulimia nervosa: a systematic review. Psychol Psychother . (2018) 93:134–59. doi: 10.1111/papt.12198
61. Moskowitz L, Weiselberg E. Anorexia nervosa/atypical anorexia nervosa. Curr Probl Pediatr Adolesc Health Care. (2017) 47:70–84. doi: 10.1016/j.cppeds.2017.02.003
62. Mandelli L, Arminio A, Atti A-R, de Ronchi D. Suicide attempts in eating disorder subtypes: a meta-analysis of the literature employing DSM-IV, DSM-5, or ICD-10 diagnostic criteria. Psychol Med. (2019) 49:1237–49. doi: 10.1017/S0033291718003549
63. Smith AR, Zuromski KL, Dodd DR. Eating disorders and suicidality: what we know, what we don't know, and suggestions for future research. Curr Opin Psychol. (2018) 22:63–7. doi: 10.1016/j.copsyc.2017.08.023
64. Goldstein A, Gvion Y. Socio-demographic and psychological risk factors for suicidal behavior among individuals with anorexia and bulimia nervosa: a systematic review. J Affect Disord. (2019) 245:1149–67. doi: 10.1016/j.jad.2018.12.015
65. Morylowska-Topolska J, Ziemiński R, Molas A, Gajewski J, Flis M, Stelmach E, et al. Schizophrenia and anorexia nervosa – reciprocal relationships. A literature review. Psychiatr Pol. (2017) 51:261–70. doi: 10.12740/PP/OnlineFirst/63514
66. Kouidrat Y, Amad A, Lalau J-D, Loas G. Eating disorders in schizophrenia: implications for research and management. Schizophr Res Treat. (2014) 2014:791573. doi: 10.1155/2014/791573
67. Sarró S. Transient psychosis in anorexia nervosa: review and case report. Eat Weight Disord. (2009) 14:e139–43. doi: 10.1007/BF03327812
68. Malaspina D, Walsh-Messinger J, Brunner A, Rahman N, Corcoran C, Kimhy D, et al. Features of schizophrenia following premorbid eating disorders. Psychiatr Res. (2019) 278:275–80. doi: 10.1016/j.psychres.2019.06.035
69. Seeman MV. Eating disorders and psychosis: seven hypotheses. World J Psychiatr. (2014) 4:112–9. doi: 10.5498/wjp.v4.i4.112
70. Bulik-Sullivan B, Finucane HK, Anttila V, Gusev A, Day FR, Loh P-R, et al. An atlas of genetic correlations across human diseases and traits. Nat Genet. (2015) 47:1236–41. doi: 10.1038/ng.3406
71. Nordsletten AE, Larsson H, Crowley JJ, Almqvist C, Lichtenstein P, Mataix-Cols D. Patterns of nonrandom mating within and across 11 major psychiatric disorders. JAMA Psychiatry. (2016) 73:354–61. doi: 10.1001/jamapsychiatry.2015.3192
72. Stip E, Lungu OV. Salience network and olanzapine in schizophrenia: implications for treatment in anorexia nervosa. Can J Psychiatr. (2015) 60:35–9.
73. Marzola E, Desedime N, Giovannone C, Amianto F, Fassino S, Abbate-Daga G. Atypical antipsychotics as augmentation therapy in anorexia nervosa. PLoS ONE. (2015) 10:e0125569. doi: 10.1371/journal.pone.0125569
74. van Deth R, Vandereycken W. Was late-nineteenth-century nervous vomiting an early variant of bulimia nervosa? Hist Psychiatry. (1995) 6:333–47. doi: 10.1177/0957154X9500602304
75. Himmerich H, Bentley J, Lichtblau N, Brennan C, Au K. Facets of shared decision-making on drug treatment for adults with an eating disorder. Int Rev Psychiatr. (2019) 31:332–46. doi: 10.1080/09540261.2019.1571995
76. Camilleri M. Peripheral mechanisms in appetite regulation. Gastroenterology. (2015) 148:1219–33. doi: 10.1053/j.gastro.2014.09.016
77. Hajishafiee M, Bitarafan V, Feinle-Bisset C. Gastrointestinal sensing of meal-related signals in humans, and dysregulations in eating-related disorders. Nutrients. (2019) 11:1298. doi: 10.3390/nu11061298
78. Dalton B, Bartholdy S, Robinson L, Solmi M, Ibrahim MA, Breen G, et al. A meta-analysis of cytokine concentrations in eating disorders. J Psychiatr Res. (2018) 103:252–64. doi: 10.1016/j.jpsychires.2018.06.002
79. Himmerich H, Bentley J, Kan C, Treasure J. Genetic risk factors for eating disorders: an update and insights into pathophysiology. Ther Adv Psychopharmacol. (2019) 9:2045125318814734. doi: 10.1177/2045125318814734
80. Roubalová R, Procházková P, PapeŽová H, Smitka K, Bilej M, Tlaskalová-Hogenová H. Anorexia nervosa: Gut microbiota-immune-brain interactions. Clin Nutr . (2019) 39:676–84. doi: 10.1016/j.clnu.2019.03.023
81. Wierenga CE, Ely A, Bischoff-Grethe A, Bailer UF, Simmons AN, Kaye WH. Are extremes of consumption in eating disorders related to an altered balance between reward and inhibition? Front Behav Neurosci. (2014) 8:410. doi: 10.3389/fnbeh.2014.00410
82. Schultz CC, Wagner G, La Cruz de F, Berger S, Reichenbach JR, Sauer H, et al. Evidence for alterations of cortical folding in anorexia nervosa. Eur Arch Psychiatr Clin Neurosci. (2017) 267:41–9. doi: 10.1007/s00406-015-0666-1
83. Cyr M, Kopala-Sibley DC, Lee S, Chen C, Stefan M, Fontaine M, et al. Reduced inferior and orbital frontal thickness in adolescent bulimia nervosa persists over two-year follow-up. J Am Acad Child Adolesc Psychiatr. (2017) 56:866–74.e7. doi: 10.1016/j.jaac.2017.08.008
84. Wierenga CE, Bischoff-Grethe A, Melrose AJ, Irvine Z, Torres L, Bailer UF, et al. Hunger does not motivate reward in women remitted from anorexia nervosa. Biol Psychiatr. (2015) 77:642–52. doi: 10.1016/j.biopsych.2014.09.024
85. Wagner A, Aizenstein H, Venkatraman VK, Fudge J, May JC, Mazurkewicz L, et al. Altered reward processing in women recovered from anorexia nervosa. Am J Psychiatr. (2007) 164:1842–9. doi: 10.1176/appi.ajp.2007.07040575
86. Davis CA, Levitan RD, Reid C, Carter JC, Kaplan AS, Patte KA, et al. Dopamine for “wanting” and opioids for “liking”: a comparison of obese adults with and without binge eating. Obesity. (2009) 17:1220–5. doi: 10.1038/oby.2009.52
87. Steinglass JE, Berner LA, Attia E. Cognitive neuroscience of eating disorders. Psychiatr Clin North Am. (2019) 42:75–91. doi: 10.1016/j.psc.2018.10.008
88. Bou Khalil R, Souaiby L, Farès N. The importance of the hypothalamo-pituitary-adrenal axis as a therapeutic target in anorexia nervosa. Physiol Behav. (2017) 171:13–20. doi: 10.1016/j.physbeh.2016.12.035
89. Schorr M, Miller KK. The endocrine manifestations of anorexia nervosa: mechanisms and management. Nat Rev Endocrinol. (2017) 13:174–86. doi: 10.1038/nrendo.2016.175
90. Weir K. New insights on eating disorders: scientists are uncovering the faulty neurobiology behind anorexia and bulimia, debunking the myth that such eating disorders are solely driven by culture and environment. Monitor Psychol. (2016) 47:36.
91. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
Keywords: eating disorders, anorexia nervosa, bulimia nervosa, history of psychiatry, German psychiatry
Citation: Bergner L, Himmerich H, Kirkby KC and Steinberg H (2021) Descriptions of Disordered Eating in German Psychiatric Textbooks, 1803–2017. Front. Psychiatry 11:504157. doi: 10.3389/fpsyt.2020.504157
Received: 08 November 2019; Accepted: 25 November 2020; Published: 14 January 2021.
Reviewed by:
Copyright © 2021 Bergner, Himmerich, Kirkby and Steinberg. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Holger Steinberg, holger.steinberg@medizin.uni-leipzig.de
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

Handbuch Essstörungen und Adipositas pp 17–28 Cite as
Essstörungen im ICD-11 und DSM-5
- Gertraud Gradl-Dietsch 4 ,
- Manuel Föcker 5 &
- Johannes Hebebrand 4
- First Online: 26 August 2022
10k Accesses
1 Citations
Zusammenfassung
Die Umstellung auf die elfte Revision der Internationalen statistischen Klassifikation der Krankheiten und verwandter Gesundheitsprobleme (ICD-11) bedingt wesentliche Neuerungen für das Kapitel Essstörungen. Durch die Zusammenführung der Fütter- und Essstörungen zu einer übergeordneten Kategorie werden Störungsbilder nach ihrer Psychopathologie gruppiert im Sinne eines Kontinuums psychopathologischer Auffälligkeiten zwischen Kindheit, Adoleszenz und Erwachsenenalter. Des Weiteren finden kulturelle Unterschiede in der klinischen Manifestation von Fütter- und Essstörungen Berücksichtigung. Neu in die Klassifikation aufgenommene Diagnosen sind die Störung mit Vermeidung oder Einschränkung der Nahrungsaufnahme (ARFID) und die Binge-Eating-Störung. Für die Diagnose Anorexia nervosa wurde das Gewichtskriterium neu definiert und die Diagnose „Anorexia Nervosa in Remission mit normalem Körpergewicht“ neu aufgenommen. Das Kriterium der Amenorrhö wurde entfernt, und die Angst vor einer Gewichtszunahme (fat phobia) wird nicht mehr als Sine-qua-non-Kriterium aufgeführt.
Bei der Bulimia nervosa wurde das Kriterium Essanfälle erweitert und das Zeitkriterium verändert, um atypische und entwicklungsabhängige Variationen des klinischen Bildes mit einzuschließen. Die ICD-10-Diagnosen „Atypische Bulimie“ (F50.3), „Essattacken bei anderen psychischen Störungen“ (F50.4) und „Erbrechen bei anderen psychischen Störungen“ (F50.5) fehlen in der ICD-11.
Die Diagnosen Sonstige Essstörungen (F50.8) und Nicht näher bezeichnete Essstörung (F50.9) werden entsprechend überführt in Andere näher bezeichnete Fütter- oder Essstörungen und Nicht näher bezeichnete Fütter- oder Essstörung.
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Al-Adawi S, Bax B, Bryant-Waugh R, Claudino AM, Hay P, Monteleone P, Norring C, Pike KM, Pilon DJ, Rausch-Herscovici C, Reed GM, Rydelius PA, Sharan P, Thiels C, Treasure J, Uher R (2013) Revision of ICD – status update on feeding and eating disorders. Adv Eating Disord 1(1):10–20
Article Google Scholar
Andersen SB, Lindgreen P, Rokkedal K, Clausen L (2018) Grasping the weight cut-off for anorexia nervosa in children and adolescents. Int J Eat Disord 51(12):1346–1351
PubMed Google Scholar
APA (2013) Diagnostic and statistical manual of mental disorders (DSM-5). American Psychiatric Publishing, Washington, DC
Google Scholar
APA (2015) Diagnostisches und statistisches Manual Psychischer Störungen DSM-5, deutsche Ausgabe. Hogrefe, Göttingen
Attia E, Becker AE, Bryant-Waugh R, Hoek HW, Kreipe RE, Marcus MD, Mitchell JE, Striegel RH, Walsh BT, Wilson GT, Wolfe BE, Wonderlich S (2013) Feeding and eating disorders in DSM-5. Am J Psychiatry 170(11):1237–1239
Avnon A, Orkaby N, Hadas A, Berger U, Brunstein Klomek A, Fennig S (2018) Inpatient weight curve trajectory as a prognostic factor among adolescents with anorexia nervosa: a preliminary report. Eat Weight Disord 23(5):645–651
Claudino AM, Pike KM, Hay P, Keeley JW, Evans SC, Rebello TJ, Bryant-Waugh R, Dai Y, Zhao M, Matsumoto C, Herscovici CR, Mellor-Marsa B, Stona AC, Kogan CS, Andrews HF, Monteleone P, Pilon DJ, Thiels C, Sharan P, Al-Adawi S, Reed GM (2019) The classification of feeding and eating disorders in the ICD-11: results of a field study comparing proposed ICD-11 guidelines with existing ICD-10 guidelines. BMC Med 17(1):93
Engelhardt C, Föcker M, Bühren K, Dahmen B, Becker K, Weber L, Correll CU, Egberts KM, Ehrlich S, Roessner V, Fleischhaker C, von Gontard A, Hahn F, Jenetzky E, Kaess M, Legenbauer T, Renner TJ, Schulze UME, Sinzig J, Wessing I, Antony G, Herpertz-Dahlmann B, Peters T, Hebebrand J (2021) Age dependency of body mass index distribution in childhood and adolescent inpatients with anorexia nervosa with a focus on DSM-5 and ICD-11 weight criteria and severity specifiers. Eur Child Adolesc Psychiatry. 30(7):1081–1094
Exner C, Hebebrand J, Remschmidt H, Wewetzer C, Ziegler A, Herpertz S, Schweiger U, Blum WF, Preibisch G, Heldmaier G, Klingenspor M (2000) Leptin suppresses semi-starvation induced hyperactivity in rats: implications for anorexia nervosa. Mol Psychiatry 5(5):476–481
Article CAS Google Scholar
Föcker M, Timmesfeld N, Scherag S, Bühren K, Langkamp M, Dempfle A, Sheridan EM, de Zwaan M, Fleischhaker C, Herzog W, Egberts K, Zipfel S, Herpertz-Dahlmann B, Hebebrand J (2011) Screening for anorexia nervosa via measurement of serum leptin levels. J Neural Transm (Vienna) 118(4):571–578
Hartmann AS, Poulain T, Vogel M, Hiemisch A, Kiess W, Hilbert A (2018) Prevalence of pica and rumination behaviors in German children aged 7–14 and their associations with feeding, eating, and general psychopathology: a population-based study. Eur Child Adolesc Psychiatry 27(11):1499–1508
Hebebrand J, Bulik CM (2011) Critical appraisal of the provisional DSM-5 criteria for anorexia nervosa and an alternative proposal. Int J Eat Disord 44(8):665–678
Hebebrand J, Milos G, Wabitsch M, Teufel M, Fuhrer D, Buhlmeier J, Libuda L, Ludwig C, Antel J (2019) Clinical trials required to assess potential benefits and side effects of treatment of patients with anorexia nervosa with recombinant human leptin. Front Psychol 10:769
Herpertz-Dahlmann B, Hagenah U (2015) Essstörungen in Kindheit und Adoleszenz. Monatsschrift Kinderheilkunde 163:688–695
Holtkamp K, Herpertz-Dahlmann B, Hebebrand K, Mika C, Kratzsch J, Hebebrand J (2006) Physical activity and restlessness correlate with leptin levels in patients with adolescent anorexia nervosa. Biol Psychiatry 60(3):311–313
Knoll S, Föcker M, Hebebrand J (2014) DSM-5 Kommentar Essstörungen – Veränderungen im DSM-5. Z Kinder Jugendpsychiatr Psychother 42(5):361–366
Micali N, Hebebrand J (2015) Anorexia nervosa through the looking glass of the draft ICD-11 diagnostic criteria: a disorder in transition. Eur Child Adolesc Psychiatry 24(10):1149–1152
Milos G, Antel J, Kaufmann LK, Barth N, Koller A, Tan S, Wiesing U, Hinney A, Libuda L, Wabitsch M, von Kanel R, Hebebrand J (2020) Short-term metreleptin treatment of patients with anorexia nervosa: rapid on-set of beneficial cognitive, emotional, and behavioral effects. Transl Psychiatry 10(1):303
Reas DL, Ro O (2017) Investigating the DSM-5 severity specifiers based on thinness for adults with anorexia nervosa. Int J Eat Disord 50(8):990–994
Reed GM, First MB, Kogan CS, Hyman SE, Gureje O, Gaebel W, Maj M, Stein DJ, Maercker A, Tyrer P, Claudino A, Garralda E, Salvador-Carulla L, Ray R, Saunders JB, Dua T, Poznyak V, Medina-Mora ME, Pike KM, Ayuso-Mateos JL, Kanba S, Keeley JW, Khoury B, Krasnov VN, Kulygina M, Lovell AM, de Jesus Mari J, Maruta T, Matsumoto C, Rebello TJ, Roberts MC, Robles R, Sharan P, Zhao M, Jablensky A, Udomratn P, Rahimi-Movaghar A, Rydelius PA, Bahrer-Kohler S, Watts AD, Saxena S (2019) Innovations and changes in the ICD-11 classification of mental, behavioural and neurodevelopmental disorders. World Psychiatry 18(1):3–19
Smith KE, Ellison JM, Crosby RD, Engel SG, Mitchell JE, Crow SJ, Peterson CB, Le Grange D, Wonderlich SA (2017) The validity of DSM-5 severity specifiers for anorexia nervosa, bulimia nervosa, and binge-eating disorder. Int J Eat Disord 50(9):1109–1113
Sonneville KR, Horton NJ, Micali N, Crosby RD, Swanson SA, Solmi F, Field AE (2013) Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: does loss of control matter? JAMA Pediatr 167(2):149–155
Swenne I (2016) Influence of premorbid BMI on clinical characteristics at presentation of adolescent girls with eating disorders. BMC Psychiatry 16:81
Tanofsky-Kraff M, Marcus MD, Yanovski SZ, Yanovski JA (2008) Loss of control eating disorder in children age 12 years and younger: proposed research criteria. Eat Behav 9(3):360–365
Uher R, Rutter M (2012) Classification of feeding and eating disorders: review of evidence and proposals for ICD-11. World Psychiatry 11(2):80–92
WHO (2019). https://icd.who.int/browse11/l-m/en . Zugegriffen am 07.08.2020
Wonderlich SA, Gordon KH, Mitchell JE, Crosby RD, Engel SG (2009) The validity and clinical utility of binge eating disorder. Int J Eat Disord 42(8):687–705
Download references
Author information
Authors and affiliations.
Klinik für Psychiatrie, Psychosomatik und Psychotherapie des Kindes- und Jugendalters, Kliniken/Institut der Universität Duisburg-Essen, LVR-Klinikum Essen, Essen, Deutschland
Gertraud Gradl-Dietsch & Johannes Hebebrand
Klinik für Kinder- und Jugendpsychiatrie, -psychosomatik und –psychotherapie, Universitätsklinikum Münster, Münster, Deutschland
Manuel Föcker
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Gertraud Gradl-Dietsch .
Editor information
Editors and affiliations.
Klinik für Psychosomatische Medizin und Psychotherapie, Ruhr-Universität Bochum, LWL-Universitätsklinikum, Bochum, Deutschland
Stephan Herpertz
Klinik für Psychosomatik und Psychotherapie, Medizinische Hochschule Hannover, Hannover, Deutschland
Martina de Zwaan
Klinik für Psychosomatische Medizin und Psychotherapie, Medizinische Universitätsklinik Tübingen, Tübingen, Deutschland
Stephan Zipfel
Rights and permissions
Reprints and permissions
Copyright information
© 2022 Der/die Autor(en), exklusiv lizenziert durch Springer-Verlag GmbH, DE, ein Teil von Springer Nature
About this chapter
Cite this chapter.
Gradl-Dietsch, G., Föcker, M., Hebebrand, J. (2022). Essstörungen im ICD-11 und DSM-5. In: Herpertz, S., de Zwaan, M., Zipfel, S. (eds) Handbuch Essstörungen und Adipositas. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-63544-5_3
Download citation
DOI : https://doi.org/10.1007/978-3-662-63544-5_3
Published : 26 August 2022
Publisher Name : Springer, Berlin, Heidelberg
Print ISBN : 978-3-662-63543-8
Online ISBN : 978-3-662-63544-5
eBook Packages : Medicine (German Language)

Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Enter search terms to find related medical topics, multimedia and more.
Advanced Search:
- Use “ “ for exact phrases.
- For example: “pediatric abdominal pain”
- Use – to remove results with certain keywords.
- For example: abdominal pain -pediatric
- Use OR to account for alternate keywords.
- For example: teenager OR adolescent
Anorexia Nervosa
, MD, Columbia University Medical Center;
, MD, College of Physicians and Surgeons, Columbia University
- Pathophysiology
- Symptoms and Signs
- 3D Models (0)
Anorexia nervosa is characterized by a relentless pursuit of thinness, a morbid fear of obesity, a distorted body image, and restriction of intake relative to requirements, leading to a significantly low body weight. Diagnosis is clinical. Most treatment is with some form of psychologic and behavioral therapy. Involvement of the family is crucial to the care of younger patients. Olanzapine may help with weight gain.
(See also Introduction to Eating Disorders Introduction to Eating Disorders Eating disorders involve a persistent disturbance of eating or of behavior related to eating that Alters consumption or absorption of food Significantly impairs physical health and/or psychosocial... read more .)
Anorexia nervosa occurs predominantly in girls and young women. Onset is usually during adolescence and rarely after age 40.
Two types of anorexia nervosa are recognized:
Restricting type: Patients restrict food intake but do not regularly engage in binge eating or purging behavior; some patients exercise excessively.
Binge eating/purging type: Patients regularly binge eat and/or induce vomiting and/or misuse laxatives, diuretics, or enemas.
Binges are defined as consumption of a much larger amount of food than most people would eat in a similar time period under similar circumstances with loss of control, ie, perceived inability to resist or stop eating.
Etiology of Anorexia Nervosa
The etiology of anorexia nervosa is unknown.
Other than being female, few risk factors have been identified. In some cultures, obesity is considered unattractive and unhealthy, and the desire to be thin is pervasive, even among children. More than 50% of prepubertal girls in the US diet or take other measures to control their weight. Excessive concern about weight or a history of dieting appears to indicate increased risk, and there is a genetic predisposition, and genome-wide studies have begun to identify specific loci that are associated with increased risk.
Family and social factors probably play a role. Many patients belong to middle or upper socioeconomic classes, are meticulous and compulsive, have average intelligence, and have very high standards for achievement and success.

Pathophysiology of Anorexia Nervosa
Endocrine abnormalities are common in anorexia nervosa; they include
Low levels of gonadal hormones
Mildly reduced levels of thyroxine (T4) and triiodothyronine (T3)
Increased cortisol secretion
Menses usually cease, but cessation of menses is no longer a criterion for diagnosis. Bone density declines. In severely undernourished patients, virtually every major organ system may be affected. However, susceptibility to infections is typically not increased.
Dehydration and metabolic alkalosis may occur, and serum potassium and/or sodium may be low; all are aggravated by induced vomiting and laxative or diuretic use.
Cardiac muscle mass, chamber size, and output decrease; mitral valve prolapse is commonly detected. Some patients have prolonged QT intervals (even when corrected for heart rate), which, with the risks imposed by electrolyte disturbances, may predispose to tachyarrhythmias. Sudden death, most likely due to ventricular tachyarrhythmias, may occur.
Symptoms and Signs of Anorexia Nervosa
Anorexia nervosa may be mild and transient or severe and persistent.
Even though underweight, most patients are concerned that they weigh too much or that specific body areas (eg, thighs, buttocks) are too fat. They persist in efforts to lose weight despite reassurances and warnings from friends and family members that they are thin or even significantly underweight, and they view any weight gain as an unacceptable failure of self-control. Preoccupation with and anxiety about weight increase even as emaciation develops.
Anorexia is a misnomer because appetite often remains until patients become significantly cachectic. Patients are preoccupied with food:
They may study diets and calories.
They may hoard, conceal, and waste food.
They may collect recipes.
They may prepare elaborate meals for other people.
Patients often exaggerate their food intake and conceal behavior, such as induced vomiting. Binge eating/purging occurs in 30 to 50% of patients. The others simply restrict their food intake.
Many patients with anorexia nervosa also exercise excessively to control weight. Even patients who are cachectic tend to remain very active (including pursuing vigorous exercise programs).
Reports of bloating, abdominal distress, and constipation are common. Most women with anorexia nervosa stop having menstrual periods. Patients usually lose interest in sex. Depression Depressive Disorders Depressive disorders are characterized by sadness severe enough or persistent enough to interfere with function and often by decreased interest or pleasure in activities. Exact cause is unknown... read more occurs frequently.
Common physical findings include bradycardia, low blood pressure, hypothermia, lanugo hair (soft, fine hair usually found only on neonates) or slight hirsutism, and edema. Body fat is greatly reduced. Patients who vomit frequently may have eroded dental enamel, painless salivary gland enlargement, and/or an inflamed esophagus.
Diagnosis of Anorexia Nervosa
Clinical criteria
Not recognizing the seriousness of the low body weight and restrictive eating are prominent features of anorexia nervosa. Patients resist evaluation and treatment; they are usually brought to the physician’s attention by family members or by intercurrent illness.
Clinical criteria for diagnosis of anorexia nervosa ( 1 Diagnosis reference Anorexia nervosa is characterized by a relentless pursuit of thinness, a morbid fear of obesity, a distorted body image, and restriction of intake relative to requirements, leading to a significantly... read more ) include the following:
Restriction of food intake resulting in a significantly low body weight
Fear of excessive weight gain or obesity (stated specifically by the patient or manifested as behavior that interferes with weight gain)
Body image disturbance (misperception of body weight and/or appearance) or denial of the seriousness of illness
In adults, low body weight is defined using the body mass index (BMI). BMI of < 17 kg/m 2 is considered significantly low; BMI 17 to < 18.5 kg/m 2 may be significantly low depending on the patient's starting point.
For children and adolescents, the BMI percentile for age is used; the 5th percentile is usually given as the cutoff. However, children above the 5th percentile who have not maintained their projected growth trajectory may also be considered to meet the criterion for low body weight; BMI percentile for age tables and standard growth charts are available from the Centers for Disease Control and Prevention (see CDC Growth Charts ). Separate BMI calculators are available for children and adolescents.
Patients may otherwise appear well and have few, if any, abnormalities in blood tests. The key to diagnosis is identifying persistent active efforts to avoid weight gain and an intense fear of fatness that is not diminished by weight loss.
Differential diagnosis
Another psychiatric disorder, such as schizophrenia Schizophrenia Schizophrenia is characterized by psychosis (loss of contact with reality), hallucinations (false perceptions), delusions (false beliefs), disorganized speech and behavior, flattened affect... read more or primary depression Depressive Disorders Depressive disorders are characterized by sadness severe enough or persistent enough to interfere with function and often by decreased interest or pleasure in activities. Exact cause is unknown... read more , may cause weight loss and reluctance to eat, but patients with these disorders do not have a distorted body image.
Rarely, an unrecognized severe physical disorder may cause substantial weight loss. Disorders to consider include malabsorption syndromes Overview of Malabsorption Malabsorption is inadequate assimilation of dietary substances due to defects in digestion, absorption, or transport. Malabsorption can affect macronutrients (eg, proteins, carbohydrates, fats)... read more (eg, due to inflammatory bowel disease or celiac disease), new-onset type 1 diabetes Diabetes Mellitus (DM) Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia. Early symptoms are related to hyperglycemia and include polydipsia... read more , adrenal insufficiency Clinical syndromes , and cancer. Amphetamine abuse Amphetamines Amphetamines are sympathomimetic drugs with central nervous system stimulant and euphoriant properties whose toxic adverse effects include delirium, hypertension, seizures, and hyperthermia... read more may cause similar symptoms.
Diagnosis reference
1. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition Text Revision , DSM-5-TR TM , Feeding and eating disorders.
Prognosis for Anorexia Nervosa
Mortality rates are high, approaching 10% per decade among affected people who come to clinical attention; unrecognized mild disease probably rarely leads to death. With treatment, prognosis is as follows:
Half of patients regain most or all of lost weight, and any endocrine and other complications are reversed.
About one fourth have intermediate outcomes and may relapse.
The remaining one fourth have a poor outcome, including relapses and persistent physical and mental complications
Children and adolescents treated for anorexia nervosa have better outcomes than adults.
Treatment of Anorexia Nervosa
Nutrition supplementation
Psychotherapy (eg, cognitive behavioral therapy)
For children and adolescents, family-based treatment
Sometimes 2nd-generation antipsychotics
Treatment of anorexia nervosa may require life-saving short-term intervention to restore body weight. When weight loss has been severe or rapid or when weight has fallen below about 75% of recommended weight, prompt restoration of weight becomes critical, and hospitalization should be considered. If any doubt exists, patients should be hospitalized.
Outpatient treatments may include varying degrees of support and supervision and commonly involve a team of practitioners.
Nutritional supplementation is often used with behavioral therapy that has clear weight-restoration goals. Nutritional supplementation begins by providing about 30 to 40 kcal/kg/day; it can produce weight gains of up to 1.5 kg/week during inpatient care and 0.5 kg/week during outpatient care. Oral feedings using solid foods are best; many weight restoration plans also use liquid supplements. Very resistant, undernourished patients occasionally require nasogastric tube feedings.
Elemental calcium 1200 to 1500 mg/day and vitamin D 600 to 800 IU/day are commonly prescribed for bone loss.
Once nutritional, fluid, and electrolyte status has been stabilized, long-term treatment begins. Outpatient psychotherapy is the cornerstone of treatment. Treatments should emphasize behavioral outcomes such as normalized eating and weight. Treatment should continue for a full year after weight is restored. Results are best in adolescents who have had the disorder < 6 months.
Family therapy, particularly using the Maudsley model (also called family-based treatment), is useful for adolescents. This model has 3 phases:
Family members are taught how to refeed the adolescent (eg, through a supervised family meal) and thus restore the adolescent’s weight (in contrast to earlier approaches, this model does not assign blame for the development of the disorder to the family or the adolescent).
Control over eating is gradually returned to the adolescent.
After the adolescent is able to maintain the restored weight, therapy focuses on engendering a healthy adolescent identity.
Treatment of anorexia nervosa is complicated by patients' abhorrence of weight gain and denial of illness. The physician should attempt to provide a calm, concerned, stable relationship while firmly encouraging a reasonable caloric intake.
Treatment also involves regular follow-up monitoring and often a team of health care practitioners, including a nutritionist, who may provide specific meal plans or information about the calories needed to restore weight to a normal level.
Although psychotherapy is primary, drugs are sometimes helpful. Olanzapine up to 10 mg orally once daily may aid weight gain.
Patients with anorexia nervosa have an intense fear of gaining weight or becoming fat that persists despite all evidence to the contrary.
In the restricting type of anorexia nervosa, patients restrict food intake and sometimes exercise excessively but do not regularly engage in binge eating or purging.
In the binge eating/purging type, patients regularly binge eat and/or induce vomiting and/or misuse laxatives, diuretics, or enemas in an attempt to purge themselves of food.
In adults, BMI is significantly low (usually BMI of < 17 kg/m 2 ), and in adolescents, BMI percentile is low (usually < 5th percentile) or does not increase as expected for normal growth.
Endocrine or electrolyte abnormalities or cardiac arrhythmias may develop, and death can occur.
Treat with nutritional supplementation, psychotherapy (eg, cognitive behavioral therapy), and, for adolescents, family-based therapy; olanzapine may be helpful.

Was This Page Helpful?

Test your knowledge
Brought to you by Merck & Co, Inc., Rahway, NJ, USA (known as MSD outside the US and Canada) — dedicated to using leading-edge science to save and improve lives around the world. Learn more about the MSD Manuals and our commitment to Global Medical Knowledge.
- Permissions
- Cookie Settings
- Terms of use
- Veterinary Manual

- IN THIS TOPIC
What is the translation of "anorexia" in German?
"anorexia" in german, anorexia {noun}.
- volume_up Appetitlosigkeit
- anorexia nervosa
- volume_up Magersucht
"Anorexia" in English
- volume_up anorexia
Translations
- open_in_new Link to source
- warning Request revision
Context sentences
English german contextual examples of "anorexia" in german.
These sentences come from external sources and may not be accurate. bab.la is not responsible for their content.
Monolingual examples
English how to use "anorexia" in a sentence, english how to use "anorexia nervosa" in a sentence, collocations, "anorexia nervosa" in german.
- volume_up Anorexia nervosa
- volume_up Magersucht nervosa
"battling anorexia" in German
- volume_up Kampf gegen Anorexie
- volume_up Kampf gegen Magersucht
"case of anorexia" in German
- volume_up Fall von Anorexie
- anonymous user
- anonymous writer
- anonymously
- anonymousness
- anopheles mosquito
- anopisthographic
- anorexic patients
- anorthosite
- another layer of bureaucracy
- another layer of complexity
Have a look at the French-English dictionary by bab.la.
Social Login
- Patient Care & Health Information
- Diseases & Conditions
- Anorexia nervosa
If your doctor suspects that you have anorexia nervosa, he or she will typically do several tests and exams to help pinpoint a diagnosis, rule out medical causes for the weight loss, and check for any related complications.
These exams and tests generally include:
- Physical exam. This may include measuring your height and weight; checking your vital signs, such as heart rate, blood pressure and temperature; checking your skin and nails for problems; listening to your heart and lungs; and examining your abdomen.
- Lab tests. These may include a complete blood count (CBC) and more-specialized blood tests to check electrolytes and protein as well as functioning of your liver, kidney and thyroid. A urinalysis also may be done.
- Psychological evaluation. A doctor or mental health professional will likely ask about your thoughts, feelings and eating habits. You may also be asked to complete psychological self-assessment questionnaires.
- Other studies. X-rays may be taken to check your bone density, check for stress fractures or broken bones, or check for pneumonia or heart problems. Electrocardiograms may be done to look for heart irregularities.
Your mental health professional also may use the diagnostic criteria for anorexia in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
More Information
- Bone density test
- Complete blood count (CBC)
- Electrocardiogram (ECG or EKG)
- Liver function tests
Treatment for anorexia is generally done using a team approach, which includes doctors, mental health professionals and dietitians, all with experience in eating disorders. Ongoing therapy and nutrition education are highly important to continued recovery.
Here's a look at what's commonly involved in treating people with anorexia.
Hospitalization and other programs
If your life is in immediate danger, you may need treatment in a hospital emergency room for such issues as a heart rhythm disturbance, dehydration, electrolyte imbalances or a psychiatric emergency. Hospitalization may be required for medical complications, severe psychiatric problems, severe malnutrition or continued refusal to eat.
Some clinics specialize in treating people with eating disorders. They may offer day programs or residential programs rather than full hospitalization. Specialized eating disorder programs may offer more-intensive treatment over longer periods of time.
Medical care
Because of the host of complications anorexia causes, you may need frequent monitoring of vital signs, hydration level and electrolytes, as well as related physical conditions. In severe cases, people with anorexia may initially require feeding through a tube that's placed in their nose and goes to the stomach (nasogastric tube).
Care is usually coordinated by a primary care doctor or a mental health professional, with other professionals involved.
Restoring a healthy weight
The first goal of treatment is getting back to a healthy weight. You can't recover from anorexia without returning to a healthy weight and learning proper nutrition. Those involved in this process may include:
- Your primary care doctor, who can provide medical care and supervise your calorie needs and weight gain
- A psychologist or other mental health professional, who can work with you to develop behavioral strategies to help you return to a healthy weight
- A dietitian, who can offer guidance getting back to regular patterns of eating, including providing specific meal plans and calorie requirements that help you meet your weight goals
- Your family, who will likely be involved in helping you maintain normal eating habits
- Psychotherapy
These types of therapy may be beneficial for anorexia:
- Family-based therapy. This is the only evidence-based treatment for teenagers with anorexia. Because the teenager with anorexia is unable to make good choices about eating and health while in the grips of this serious condition, this therapy mobilizes parents to help their child with re-feeding and weight restoration until the child can make good choices about health.
- Individual therapy. For adults, cognitive behavioral therapy — specifically enhanced cognitive behavioral therapy — has been shown to help. The main goal is to normalize eating patterns and behaviors to support weight gain. The second goal is to help change distorted beliefs and thoughts that maintain restrictive eating.
Medications
No medications are approved to treat anorexia because none has been found to work very well. However, antidepressants or other psychiatric medications can help treat other mental health disorders you may also have, such as depression or anxiety.
Treatment challenges in anorexia
One of the biggest challenges in treating anorexia is that people may not want treatment. Barriers to treatment may include:
- Thinking you don't need treatment
- Fearing weight gain
- Not seeing anorexia as an illness but rather a lifestyle choice
People with anorexia can recover. However, they're at increased risk of relapse during periods of high stress or during triggering situations. Ongoing therapy or periodic appointments during times of stress may help you stay healthy.
- Acupuncture
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
When you have anorexia, it can be difficult to take care of yourself properly. In addition to professional treatment, follow these steps:
- Stick to your treatment plan. Don't skip therapy sessions and try not to stray from meal plans, even if they make you uncomfortable.
- Talk to your doctor about appropriate vitamin and mineral supplements. If you're not eating well, chances are your body isn't getting all of the nutrients it needs, such as Vitamin D or iron. However, getting most of your vitamins and minerals from food is typically recommended.
- Don't isolate yourself from caring family members and friends who want to see you get healthy. Understand that they have your best interests at heart.
- Resist urges to weigh yourself or check yourself in the mirror frequently. These may do nothing but fuel your drive to maintain unhealthy habits.
Alternative medicine
Dietary supplements and herbal products designed to suppress the appetite or aid in weight loss may be abused by people with anorexia. Weight-loss supplements or herbs can have serious side effects and dangerously interact with other medications. These products do not go through a rigorous review process and may have ingredients that are not posted on the bottle.
Keep in mind that natural doesn't always mean safe. If you use dietary supplements or herbs, discuss the potential risks with your doctor.
Anxiety-reducing approaches that complement anorexia treatment may increase the sense of well-being and promote relaxation. Examples of these approaches include massage, yoga and meditation.
Coping and support
You may find it difficult to cope with anorexia when you're hit with mixed messages by the media, culture, and perhaps your own family or friends. You may even have heard people joke that they wish they could have anorexia for a while so that they could lose weight.
Whether you have anorexia or your loved one has anorexia, ask your doctor or mental health professional for advice on coping strategies and emotional support. Learning effective coping strategies and getting the support you need from family and friends are vital to successful treatment.
Preparing for your appointment
Here's some information to help you get ready for your appointment and know what to expect from your doctor or mental health professional.
You may want to ask a family member or friend to go with you. Someone who accompanies you may remember something that you missed or forgot. A family member may also be able to give your doctor a fuller picture of your home life.
What you can do
Before your appointment, make a list of:
- Any symptoms you're experiencing, including any that may seem unrelated to the reason for the appointment. Try to recall when your symptoms began.
- Key personal information, including any major stresses or recent life changes.
- All medications, vitamins, herbal products, over-the-counter medications and other supplements that you're taking, and their dosages.
- Questions to ask your doctor so that you'll remember to cover everything you wanted to.
Some questions you might want to ask your doctor or mental health professional include:
- What kinds of tests do I need? Do these tests require any special preparation?
- Is this condition temporary or long lasting?
- What treatments are available, and which do you recommend?
- Is there a generic alternative to the medicine you're prescribing?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your doctor or mental health professional is likely to ask you a number of questions, including:
- How long have you been worried about your weight?
- Do you exercise? How often?
- What ways have you used to lose weight?
- Are you having any physical symptoms?
- Have you ever vomited because you were uncomfortably full?
- Have others expressed concern that you're too thin?
- Do you think about food often?
- Do you ever eat in secret?
- Have any of your family members ever had symptoms of an eating disorder or been diagnosed with an eating disorder?
Be ready to answer these questions to reserve time to go over any points you want to focus on.
- Sim LA (expert opinion). Mayo Clinic, Rochester, Minn. Jan. 31, 2018.
- Anorexia nervosa. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. Arlington, Va.: American Psychiatric Association; 2013. http://dsm.psychiatryonline.org. Accessed Nov. 13, 2017.
- Hales RE, et al. Anorexia nervosa. In: The American Psychiatric Publishing Textbook of Psychiatry. 6th ed. Washington, D.C.: American Psychiatric Publishing; 2014. http://psychiatryonline.org. Accessed Nov. 13, 2017.
- Klein D, et al. Anorexia nervosa in adults: Clinical features, course of illness, assessment, and diagnosis. https://www.uptodate.com/contents/search. Accessed Nov. 13, 2017.
- Mehler P. Anorexia nervosa in adults and adolescents: Medical complications and their management. https://www.uptodate.com/contents/search. Accessed Nov. 13, 2017.
- Mehler P. Anorexia nervosa in adults: Evaluation for medical complications and criteria for hospitalization to manage these complications. https://www.uptodate.com/contents/search. Accessed Nov. 13, 2017.
- Pike K. Anorexia nervosa in adults: Cognitive behavioral therapy (CBT). https://www.uptodate.com/contents/search. Accessed Nov. 13, 2017.
- Walsh BT. Anorexia nervosa in adults: Pharmacotherapy. https://www.uptodate.com/contents/search. Accessed Nov. 13, 2017.
- Anorexia nervosa. Merck Manual Professional Version. http://www.merckmanuals.com/professional/psychiatric-disorders/eating-disorders/anorexia-nervosa. Accessed Nov. 13, 2017.
- Harrington BC, et al. Initial evaluation, diagnosis, and treatment of anorexia nervosa and bulimia nervosa. American Family Physician. 2015;91:46.
- Brockmeyer T, et al. Advances in the treatment of anorexia nervosa: A review of established and emerging interventions. Psychological Medicine. In press. Accessed Nov. 13, 2017.
- Davis H, et al. Pharmacotherapy of eating disorders. Current Opinion in Psychiatry. 2017;30:452.
- Herpertz-Dahlmann B. Treatment of eating disorders in child and adolescent psychiatry. Current Opinion in Psychiatry. 2017;30:438.
- Fogarty S, et al. The role of complementary and alternative medicine in the treatment of eating disorders: A systematic review. Eating Behaviors. 2016;21:179.
- Eating disorders. National Alliance on Mental Illness. https://www.nami.org/Learn-More/Mental-Health-Conditions/Eating-Disorders/Overview. Accessed Nov. 13, 2017.
- Lebow J, et al. Is there clinical consensus in defining weight restoration for adolescents with anorexia nervosa? Eating Disorders. In press. Accessed Dec. 4, 2017.
- Lebow J, et al. The effect of atypical antipsychotic medications in individuals with anorexia nervosa: A systematic review and meta-analysis. International Journal of Eating Disorders. 2013;46:332.
- Five things to know about safety of dietary supplements for children and teens. National Center for Complementary and Integrative Health. https://nccih.nih.gov/health/tips/child-supplements. Accessed Feb. 9, 2018.
Associated Procedures
Products & services.
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Psychiatry hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Anorexia nervosa.
Christine A. Moore ; Brooke R. Bokor .
Affiliations
Last Update: August 28, 2023 .
- Continuing Education Activity
Anorexia nervosa is defined by the restriction of nutrient intake relative to requirements, which leads to significantly low body weight. Patients with this eating disorder will have a fear of gaining weight along and a distorted body image with the inability to comprehend the seriousness of their condition. This activity reviews the evaluation and management of anorexia nervosa and highlights the role of the interprofessional team in improving care for patients with this condition.
- Outline the epidemiology of anorexia nervosa.
- Explain the pathophysiology of anorexia nervosa.
- Describe the management of anorexia nervosa.
- Summarize the importance of improving care coordination among the interprofessional team members to enhance the delivery of care for those with anorexia nervosa.
- Introduction
Anorexia nervosa is an eating disorder defined by restriction of energy intake relative to requirements, leading to a significantly low body weight. Patients will have an intense fear of gaining weight and distorted body image with the inability to recognize the seriousness of their significantly low body weight. [1] [2] [3]
The success of many professions depends on a person's weight. Models and actors portray a level of thinness that is difficult to attain, and it is enhanced by make-up and photographic alterations. Athletes in sports such as ballet, long-distance running, and martial arts are pressured to maintain lean body weights to outperform the competition. Media outlets promote diet secrets and weight loss tips in excess. Populations such as maturing females identify thin body types with increased self-esteem and link weight loss with self-control. [4] [5]
- Epidemiology
Anorexia nervosa is more common in females than males. Onset is late adolescence and early adulthood. Lifetime prevalence is 0.3% to 1% (European studies have demonstrated a prevalence of 2% to 4%), irrespective of culture, ethnicity, and race. Risk factors for eating disorders include childhood obesity, female sex, mood disorders, personality traits (impulsivity and perfectionism), sexual abuse, or weight-related concerns from family or peer environments. [6] [7] [8]
- Pathophysiology
Studies demonstrate biological factors play a role in the development of anorexia nervosa in addition to environmental factors. Genetic correlations exist between educational attainment, neuroticism, and schizophrenia. Patients with anorexia nervosa have altered brain function and structure there are deficits in neurotransmitters dopamine (eating behavior and reward) and serotonin (impulse control and neuroticism), differential activation of the corticolimbic system (appetite and fear), and diminished activity among the frontostriatal circuits (habitual behaviors). Patients have co-morbid psychiatric disorders such as major depressive disorder and generalized anxiety disorder.
- History and Physical
Patients will report symptoms such as amenorrhea, cold intolerance, constipation, extremity edema, fatigue, and irritability. They may describe restrictive behaviors related to food like calorie counting or portion control, and purging methods, for example, self-induced vomiting or use of diuretics or laxatives. Many exercise compulsively for extended periods of time. Patients with anorexia nervosa develop multiple complications related to prolonged starvation and purging behaviors.
Workup includes a thorough medical history (comprehensive review of systems, family and social history, medications including nonprescribed, past medical and psychiatric history, prior abuse) and physical exam (looking for complications above). Basic labs include coagulation panel, complete blood count, complete metabolic profile, 25-hydroxyvitamin D, testosterone (males), thyroid-stimulating hormone, and urine testing (beta-hCG [females] and drugs, either illicit or prescription). An electrocardiogram is recommended to assess for life-threatening arrhythmias. Additional studies may be necessary if BMI is less than 14 kg/m, for example, echocardiogram in patients with hemodynamic compromise (dyspnea, murmurs, syncope) or computed tomography of the abdomen to rule out superior mesenteric artery syndrome or amenorrhea more than 9 months (dual-energy x-ray absorptiometry). [9] [8]
Complications of anorexia nervosa are listed:
- Cardiovascular: bradycardia, dilated cardiomyopathy, electrolyte-induced arrhythmias, hypotension, mitral valve prolapse, pericardial effusion
- Constitutional: arrested growth, hypothermia, low body mass index (BMI), muscle wasting
- Dermatologic: carotenoderma, lanugo, xerosis
- Endocrine: hypothalamic hypogonadism, osteoporosis
- Gastrointestinal: constipation (laxative abuse), gastroparesis
- Hematologic: cytopenias (inc. normocytic anemia), bone marrow hypoplasia/aplasia
- Neurologic: brain atrophy, peripheral neuropathy (mineral and vitamin deficiencies)
- Obstetric: antenatal and postnatal complications
- Psychiatric: depression, impaired concentration, insomnia, irritability
- Renal and electrolytes: hypokalemic metabolic acidosis or alkalosis (laxative or diuretic abuse, resp.), prerenal renal failure, refeeding syndrome.
The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) provides the diagnostic criteria for anorexia nervosa (A-C). It classifies the disease by type, status, and severity.
Of note, amenorrhea has been removed from the DSM-5 criteria. Patients who meet the new criteria and continue to menstruate have similar outcomes as those who do not.
Other eating disorders have similar features to anorexia nervosa. Avoidant or restrictive food intake disorder involves food restriction with failure to meet the nutritional need. While patients are often underweight, this disturbance does not meet diagnostic criteria for anorexia nervosa. Individuals with binge eating disorder eat excessive amounts of calories in a short period with a lack of self-control but do not display compensatory behaviors such as purging or restriction. Patients with bulimia nervosa will binge and purge without a corresponding low BMI. Pica refers to chronic ingestion of nonfood substances and may be a manifestation of underlying medical or psychiatric condition. For example, patients with anorexia nervosa may eat toilet paper when they are hungry. Rumination disorder occurs when patients repeatedly regurgitate food for one month when no other medical condition can be identified and does not occur solely during the course of another eating disorder. Other specified feeding or eating disorder refers to conditions with symptoms that impair functioning but do not meet criteria for a specific eating disorder, for example, patients who meet criteria for anorexia nervosa but have BMI more than 18.5 kg/m are classified as “atypical anorexia nervosa.”
Major depressive disorder can cause anorexia and weight loss. However, patients are not obsessed with body habitus. Patients with obsessive-compulsive disorder may have food rituals but maintain a normal weight. Patients who abuse stimulants such as cocaine and methamphetamine experience weight loss through increased metabolism and concentrated efforts to obtain illicit substances rather than consume calories.
Medical conditions can cause weight loss. Examples are celiac disease, hyperthyroidism, inflammatory bowel disease, malignancy, poorly controlled diabetes mellitus, primary adrenal insufficiency, and tuberculosis. The diagnosis will come from the history and physical examination. Order labs as dictated by the clinical picture.
- Treatment / Management
Treatment for anorexia nervosa is centered on nutrition rehabilitation and psychotherapy. Patients who need inpatient treatment have the following characteristics:
- Existing psychiatric disorders requiring hospitalization
- High risk for suicide (intent with highly lethal plan or failed attempt)
- Lack of support system (severe family conflict or homelessness)
- Limited access (lives too far away to participate in a daily treatment program)
- Medically unstable (bradycardia, dehydration, hypoglycemia or poorly controlled diabetes, hypokalemia or other electrolyte imbalances indicative of refeeding syndrome, hypothermia, hypotension, organ compromise requiring acute treatment)
- Poorly motivated to recover (uncooperative, preoccupied with intrusive thoughts)
- Purging behaviors that are persistent, severe, and occur multiple times a day
- Severe anorexia nervosa (less than 70% of ideal body weight or acute weight loss with food refusal)
- Supervised feeding and/or specialized feeding (nasogastric tube) required
- Unable to stop compulsively exercising (not a sole indication for hospitalization).
Outpatient treatment includes intensive therapy (2 to 3 hours per weekday) and partial hospitalization (6 hours per day). Pediatric patients benefit from family-based psychotherapy to explore underlying dynamics and restructure the home environment.
Refeeding syndrome can occur following prolonged starvation. As the body utilizes glucose to produce molecules of adenosine triphosphate (ATP), it depletes the remaining stores of phosphorus. Also, glucose entry into cells is mediated by insulin and occurs rapidly following long periods without food. Both cause electrolyte abnormalities such as hypophosphatemia and hypokalemia, triggering cardiac and respiratory compromise. Patients should be followed carefully for signs of refeeding syndrome and electrolytes closely monitored.
Pharmacotherapy is not used initially. For acutely ill patients who do not respond to initial treatment, olanzapine is a first-line medication. Other antipsychotics have not demonstrated similar effects on weight gain. For patients who are not acutely ill but have co-morbid psychiatric conditions such as generalized anxiety disorder or major depressive disorder, combination therapy with selective serotonin reuptake inhibitors (SSRIs) and therapy is best. Patients who do not respond to SSRIs may need a second-generation antipsychotic. Tricyclic antidepressants (TCAs) are less preferred due to concerns about cardiotoxicity, especially in malnourished patients. Bupropion is contraindicated in patients with eating disorders due to the increased risk of seizures. [10] [11] [12]
- Differential Diagnosis
- Chronic mesenteric ischemia
- Malabsorption
- Hyperthyroidism
- Irritable bowel syndrome
- Celiac disease
Remission in AN varies. Three-fourths of patients treated in out-patient settings remit within 5 years and the same percentage experience intermediate-good outcomes (including weight gain). Relapse is more common in patients who are older with a longer duration of disease or lower body fat/weight at the end of treatment, have co-morbid psychiatric disorders, or receive therapy outside of a specialized clinic. Patients who achieve partial remission often develop another form of eating disorder (ex. bulimia nervosa or unspecified eating disorder).
All-cause mortality is greater in AN compared to the rest of the population. It has one of the highest mortality rates of all eating disorders due to medical complications, substance abuse, and suicide. Patients with AN have increased rates of suicide and this accounts for 25% of deaths associated.
- Complications
- Delayed puberty
- Hypercarotenemia
- Hypothermia
- Hypoglycemia
- Osteoporosis
- Failure to thrive
- Cardiomyopathy
- Bradycardia
- Arrhythmias
- Renal failure
- Constipation
- Peripheral neuropathy
- Pancytopenia
- Infertility
- Deterrence and Patient Education
Anorexia nervosa is a psychiatric disease in which patients restrict their food intake relative to their energy requirements through eating less, exercising more, and/or purging food through laxatives and vomiting. Despite being severely underweight, they do not recognize it and have distorted body images. They can develop complications from being underweight and purging food. Diagnose by history, physical, and lab work that rules out other conditions that can make people lose weight. Treatment includes gain weight (sometimes in a hospital if severe), therapy to address body image, and management of complications from malnourishment.
- Enhancing Healthcare Team Outcomes
Anorexia nervosa is a serious eating disorder that has very high morbidity. The disorder is usually managed with an interprofessional team that consists of a psychiatrist, dietitian, social worker, internist, endocrinologist, gastroenterologist, and nurses. The disorder cannot be prevented and there is no cure. Hence patient and family education is key to preventing high morbidity. The dietitian should educate the family on the importance of nutrition and limiting exercise. The mental health nurse should educate the patient on changes in behavior, easing stress, and overcoming any emotional issues. The pharmacist should educate the patient and family on the use of drugs like laxatives and weight loss pills. Only through close follow-up and monitoring can patient outcomes be improved. [13] [14] [Level 5]
Evidence-based Outcomes
Remission in anorexia nervosa varies. Three-fourths of patients treated in out-patient settings remit within five years and the same percentage experience intermediate-good outcomes, including weight gain. Relapse is more common in patients who are older with a longer duration of disease or lower body fat/weight at the end of treatment, have co-morbid psychiatric disorders, or receive therapy outside of a specialized clinic. Often, patients who achieve partial remission develop another form of eating disorders like bulimia nervosa or unspecified eating disorder.
All-cause mortality is greater in anorexia nervosa compared to the rest of the population. It has one of the highest mortality rates of all eating disorders due to medical complications, substance abuse, and suicide. Patients with anorexia nervosa have increased rates of suicide, and this accounts for 25% of deaths associated with the disorder. [15] [16] [9] [Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) Criteria for Anorexia Nervosa Contributed by Christine Moore, D.O.
Disclosure: Christine Moore declares no relevant financial relationships with ineligible companies.
Disclosure: Brooke Bokor declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Moore CA, Bokor BR. Anorexia Nervosa. [Updated 2023 Aug 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Developmental Consequences of Restrictive Eating Disorders after Childhood Obesity: Two Case Reports. [Spartan Med Res J. 2017] Developmental Consequences of Restrictive Eating Disorders after Childhood Obesity: Two Case Reports. Kennedy SF, Krive K. Spartan Med Res J. 2017 Feb 2; 1(2):5782. Epub 2017 Feb 2.
- Animal Models for Anorexia Nervosa-A Systematic Review. [Front Hum Neurosci. 2020] Animal Models for Anorexia Nervosa-A Systematic Review. Scharner S, Stengel A. Front Hum Neurosci. 2020; 14:596381. Epub 2021 Jan 20.
- Review [Anorexia nervosa as differential diagnosis in underweight patients]. [Dtsch Med Wochenschr. 2016] Review [Anorexia nervosa as differential diagnosis in underweight patients]. Rapps N, Skoda E, Zipfel S. Dtsch Med Wochenschr. 2016 Feb; 141(4):261-4. Epub 2016 Feb 17.
- [Early onset anorexia nervosa]. [Rev Prat. 2020] [Early onset anorexia nervosa]. Lefebvre A, Stordeur C. Rev Prat. 2020 Oct; 70(8):875-880.
- Review [Anorexia nervosa and involuntary treatment]. [Duodecim. 2011] Review [Anorexia nervosa and involuntary treatment]. Lindberg N, Sailas E. Duodecim. 2011; 127(11):1090-6.
Recent Activity
- Anorexia Nervosa - StatPearls Anorexia Nervosa - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
Anorexia nervosa (griechisch-lateinisch; übersetzt etwa „nervlich bedingte Appetitlosigkeit", abgekürzt AN) oder Magersucht ist eine Form der Essstörung.Davon betroffene Menschen besitzen eine gestörte Wahrnehmung des eigenen Körpers (Körperschemastörung) und verweigern aus Furcht vor Gewichtszunahme oder dem Wunsch nach Gewichtsverlust die Aufnahme von Nahrung.
Anorexia nervosa (Magersucht) ist eine Essstörung , die durch einen unablässigen Schlankheitswahn, ein verzerrtes Körperbild, eine extreme Angst vor Fettleibigkeit sowie die Einschränkung der Nahrungsaufnahme gekennzeichnet ist, was zu einem erheblichen Gewichtsverlust führt. Anorexia nervosa beginnt normalerweise in der Jugend und tritt ...
Unter einer Anorexia nervosa versteht man eine Verhaltensstörung bzw. Essstörung, bei der es zum beabsichtigten Gewichtsverlust durch verminderte Nahrungsaufnahme, induziertes Erbrechen, Laxantien -Abusus und Hyperaktivität kommt. Abzugrenzen von der Anorexie ist die Bulimie, welche als Ess-Brechsucht mit anfallsartigen Ess-Brech-Anfällen ...
Was ist Magersucht? Magersucht, auch Anorexia nervosa genannt, ist eine Essstörung. Jemand mit Magersucht hat drei Hauptsymptome: Er hat große Angst vor einer Gewichtszunahme, er schränket die Nahrungsaufnahme ein (was zu einem erheblichen Gewichtsverlust führt) und er hat möglicherweise eine verzerrte Sicht auf seinen Körper (und denkt, er sei übergewichtig, obwohl dies nicht der Fall ...
Von Anorexia nervosa und Bulimia nervosa sind überwiegend Frauen betroffen, bei Binge-Eating-Störung ist das Geschlechterverhältnis eher ausgeglichen. Soziokulturelle, biologische und psychologische Faktoren werden hinsichtlich der Krankheitsentstehung diskutiert. ... Nach den deutschen Leitlinien von 2019 ist bei Anorexia nervosa auch die ...
Frauen bzw. Mädchen sind bei der Anorexia nervosa und der Bulimie nervosa deutlich häufiger von Essstörungen betroffen als Männer bzw. Jungen. Der Verlauf von Essstörungen ist meist mit erheblichen somatischen Komplikationen und bei der Anorexia nervosa mit einem erheblichen Mortalitätsrisiko verbunden.
Anorexia nervosa, also known as just anorexia, is an eating disorder. This disorder makes you obsess about your weight and food. If you have this problem, you may have a warped body image. You may see yourself as fat even though you have a very low body weight. With anorexia, you may use unusual eating habits to cope with stress, anxiety, and ...
Anorexia nervosa (AN) gehört zu den psychiatrischen Erkrankungen und hat in dieser Erkrankungsentität die höchste Mortalitäts- und geringste Remissionsrate. ... Im aktuellen Krankenhausreport der Deutschen Angestellten Krankenkasse DAK (veröffentlicht am 09.09.2021) ist bei insgesamt sinkenden stationären Behandlungszahlen in den ...
The diagnostic category "anorexia nervosa," introduced by Ernest-Charles Lasègue and William Gull in 1873, first appears a century later in a German textbook of psychiatry, authored by Gerd Huber in 1974. However, disordered eating behavior has been described and discussed in German psychiatric textbooks throughout the past 200 years.
Anorexia nervosa is a condition where one becomes obsessed with losing weight and practices self-starvation in an attempt to achieve significant weight loss or to maintain extremely unhealthy level of body weight.
Eine Essstörung, die nicht alle ICD-11-Kriterien der Anorexia nervosa erfüllt, wäre als Andere spezifische Anorexia nervosa oder Sonstige Anorexia nervosa zu verschlüsseln. Nach DSM-5 ist bei einer Atypischen Anorexia nervosa das Gewichtskriterium nicht erfüllt. In Tab. 3.1 sind die ICD-11- und DSM-5-Kriterien im Vergleich dargestellt.
Anorexia nervosa (AN), often referred to simply as anorexia, is an eating disorder characterized by food restriction, body image disturbance, fear of gaining weight, and an overpowering desire to be thin.. Individuals with anorexia nervosa have a fear of being overweight or being seen as such, despite the fact that they are typically underweight. The DSM-5 describes this perceptual symptom as ...
Anorexia (an-o-REK-see-uh) nervosa — often simply called anorexia — is an eating disorder characterized by an abnormally low body weight, an intense fear of gaining weight and a distorted perception of weight. People with anorexia place a high value on controlling their weight and shape, using extreme efforts that tend to significantly ...
Possible BE variation of 'binge'? (anorexia, bulimia) Last post 29 Sep 10, 21:37: I have a quote from a British text about an anorexic/bulimic girl who writes "I can feel the… 3 Replies: Anorexia nervosa Patientenr reagieren tatsächlich positiv auf body cues, wenn man sie mit Bildern dünner Models konfrontiert. Last post 24 Mar 11, 10:35
Anorexia nervosa occurs predominantly in girls and young women. Onset is usually during adolescence and rarely after age 40. Two types of anorexia nervosa are recognized: Restricting type: Patients restrict food intake but do not regularly engage in binge eating or purging behavior; some patients exercise excessively.
Anorexia nervosa is an eating disorder characterized by weight loss (or lack of appropriate weight gain in growing children); difficulties maintaining an appropriate body weight for height, age, and stature; and, in many individuals, distorted body image. People with anorexia nervosa generally restrict the number of calories and the types of ...
&NA; An abiding mystery of the mind‐body connection is that it should seem mysterious at all—an indication, perhaps, of how deeply conditioned we have been by "dualism." That doctrine, laid down more than three centuries ago by French philosopher Rene Descartes, sees mind and body as distinct entities, to be treated separately. It became the paradigm for medicine, and still dominates ...
Zusammenfassung. Die Umstellung auf die 11. Revision der Internationalen Klassifikation der Krankheiten und verwandter Gesundheitsprobleme (ICD-11) bedingt wesentliche Neuerungen bezüglich i) Zusammenführung der Fütter- und Essstörungen zu einer übergeordneten Kategorie, ii) Gruppierung der Störungsbilder nach ihrer Psychopathologie im Sinne eines Kontinuums psychopathologischer ...
Anorexia (lat.) = Appetitverlust/ Appetitverminderung; nervosa (lat.) = psychische Auslöser. Magersucht. krankhafte Essstörung. tritt häufiger bei Frauen und Mädchen auf. Erkrankungsgipfel zwischen 15 und 25. BMI unter 17,5. Sterbensrate bei 10.15 %. tritt häufig in Verbindung mit Bulimie auf.
de Deutsch ; en English ... Eating disorders include abnormal mental and behavioural conduct related to food and body weight, such as anorexia nervosa and bulimia nervosa. more_vert. open_in_new Link to source; warning Request revision; I think anorexia nervosa is a combination of genetics and environmental factors. ...
Diagnosis. If your doctor suspects that you have anorexia nervosa, he or she will typically do several tests and exams to help pinpoint a diagnosis, rule out medical causes for the weight loss, and check for any related complications. These exams and tests generally include: Physical exam. This may include measuring your height and weight ...
Anorexia nervosa is the most severe eating disorder; it has a protracted course of illness and the highest mortality rate among all psychiatric illnesses. It is characterised by a restriction of energy intake followed by substantial weight loss, which can culminate in cachexia and related medical consequences. ... Psycho. 3rd ed. Deutscher ...
Anorexia nervosa is an eating disorder defined by restriction of energy intake relative to requirements, leading to a significantly low body weight. Patients will have an intense fear of gaining weight and distorted body image with the inability to recognize the seriousness of their significantly low body weight.[1][2][3]