- Alzheimer's & Dementia
- Asthma & Allergies
- Atopic Dermatitis
- Breast Cancer
- Cardiovascular Health
- Environment & Sustainability
- Exercise & Fitness
- Headache & Migraine
- Health Equity
- HIV & AIDS
- Human Biology
- Men's Health
- Mental Health
- Multiple Sclerosis (MS)
- Parkinson's Disease
- Psoriatic Arthritis
- Sexual Health
- Ulcerative Colitis
- Women's Health
- Nutrition & Fitness
- Vitamins & Supplements
- At-Home Testing
- Men’s Health
- Women’s Health
- Latest News
- Medical Myths
- Honest Nutrition
- Through My Eyes
- New Normal Health
- 2023 in medicine
- Why exercise is key to living a long and healthy life
- What do we know about the gut microbiome in IBD?
- My podcast changed me
- Can 'biological race' explain disparities in health?
- Why Parkinson's research is zooming in on the gut
- Health Hubs
- Find a Doctor
- BMI Calculators and Charts
- Blood Pressure Chart: Ranges and Guide
- Breast Cancer: Self-Examination Guide
- Sleep Calculator
- RA Myths vs Facts
- Type 2 Diabetes: Managing Blood Sugar
- Ankylosing Spondylitis Pain: Fact or Fiction
- Our Editorial Process
- Content Integrity
- Conscious Language
- Health Conditions
- Health Products

The reasons why smoking is bad for you

Smoking damages nearly every organ in the body and is bad for a person’s overall health. People can significantly reduce their chance of smoking-related disease by giving it up.
Smoking is the leading preventable cause of early disease and death in the United States. Giving up smoking is difficult for many people, but the number of former smokers is increasing all the time.
According to the Centers for Disease Control and Prevention (CDC) , current smoking in the U.S. has declined from 20.9% in 2005 to 13.7% in 2018. The number of smokers who have quit is also rising.
In this article, we look at the health impact of smoking, including its effects on the brain, heart, lungs, and immune system. We also discuss the benefits of quitting.
How does smoking affect health?

Every year, more than 480,000 people die in the U.S. due to tobacco-related diseases — around 1 in 5 of all deaths — according to the American Cancer Society.
They also state that around half of people in the U.S. who keep smoking will die from smoking-related causes.
Life expectancy is at least 10 years less for smokers compared with nonsmokers. The American Cancer Society state that smoking shortens lifespan by about 12 years in males and 11 years in females.
The CDC comment that smoking causes more deaths in the U.S. each year than the following combined:
- motor vehicle injuries
- alcohol or illicit drug use
- firearm-related incidents
Tobacco contains poisonous substances that affect people’s health. Two of these poisons are:
- Carbon monoxide . Car exhaust fumes also produce this substance, and it is fatal in large doses. It replaces oxygen in the blood and starves the organs of oxygen, stopping them from functioning correctly.
- Tar . This is a sticky, brown substance that coats the lungs and affects breathing.
While the statistics are alarming, it is important to bear in mind that giving up smoking reduces the risk of disease dramatically.
Below, we discuss the impact smoking can have on different parts of the body.
Smoking can increase the likelihood of having a stroke by 2–4 times . Strokes can cause brain damage and death.
One way that stroke can cause brain injury is through a brain aneurysm , which occurs when the wall of a blood vessel weakens and creates a bulge. This bulge can burst and cause a subarachnoid hemorrhage , which can lead to a stroke.
Chemicals in tobacco smoke increase the chance of heart problems and cardiovascular diseases.
Smoking causes atherosclerosis , which is when plaque builds up in the blood and sticks to the artery walls. This makes them narrower, reducing blood flow and increasing the risk of blood clots.
Smoking also damages the blood vessels, making them thicker and narrower. This makes it harder for blood to flow, and also increases blood pressure and heart rate.
Smoking has links with the following cardiovascular conditions:
- coronary heart disease , one of the leading causes of death in the U.S
- a heart attack , as smoking doubles the risk of heart attack
- blockages that reduce blood flow to the skin and legs
- stroke due to blood clots or burst blood vessels in the brain
Even smokers who smoke 5 or fewer cigarettes a day may develop early signs of cardiovascular disease.
Carbon monoxide and nicotine make the heart work harder and faster. This means that smoking makes it more challenging to exercise. A lack of exercise further increases the risk of health problems.
According to the National Institutes of Health (NIH) , smoking reduces bone density, making the bones weaker and more brittle. Smoking can also impair bone healing after a fracture.
Researchers find it difficult to say whether this is a direct effect of smoking, or due to other risk factors prevalent in people who smoke. These include lower body weight and doing less physical exercise.
This may affect females more than males. Females are more prone to osteoporosis and broken bones.
Quitting smoking, even later in life, can help limit bone loss linked with smoking.
Immune system
The immune system protects the body against infection and disease.
According to one 2017 study , smoking reduces immune function and causes inflammation in the body. This can lead to autoimmune conditions, including:
- Crohn’s disease
- rheumatoid arthritis
- ulcerative colitis
- systemic lupus erythematosus
Smoking also has links with type 2 diabetes .
The lungs are perhaps the most obvious organ that smoking affects.
It often takes many years before a person notices any symptoms of smoking-related lung disease. This means that people may not receive a diagnosis until the disease is quite advanced.
Smoking can impact the lungs in several ways. The primary reason is that smoking damages the airways and air sacs — known as alveoli — in the lungs.
Three of the most common smoking-related lung conditions in the U.S. are:
- Chronic obstructive pulmonary disease (COPD) . COPD is a long-term disease. It causes wheezing, shortness of breath, and chest tightness. COPD is the third leading cause of death in the U.S.
- Chronic bronchitis . Chronic bronchitis occurs when the airways produce too much mucus. This leads to a long-lasting cough and inflamed airways. Over time, scar tissue and mucus can completely block the airways and cause infection.
- Emphysema: Emphysema is a type of COPD that reduces the number of alveoli and breaks down the walls between them. This makes it difficult to breathe, even at rest, and over time, a person may need an oxygen mask.
Other lung diseases caused by smoking include pneumonia , asthma , and tuberculosis .
Smoking can have several effects on oral health and may cause:
- halitosis , or bad breath
- stained teeth
- reduced sense of taste
Smoking irritates the gum tissues. The American Dental Association (ADA) state that smoking increases the risk of gum disease , which can add to halitosis.
Reproduction
Smoking can also affect the reproductive system and fertility.
Females who smoke can have more difficulty becoming pregnant. In males, smoking can cause impotence by damaging blood vessels in the penis. It can also damage sperm and affect sperm count.
According to some studies, males who smoke have a lower sperm count than those who do not.
Smoking while pregnant increases a number of risks for the baby, including:
- premature birth
- pregnancy loss
- low birth weight
- sudden infant death syndrome
- infant illnesses
Smoking reduces the amount of oxygen that can reach the skin. This speeds up the aging process and can make skin appear dull or gray.
Smoking can cause:
- facial wrinkles, especially around the lips
- baggy eyelids
- uneven skin coloring, such as a yellow or gray tone
- dry, coarse skin
- temporary yellowing of the fingers and fingernails
Smoking reduces how quickly skin wounds heal, increases the risk of skin infections, and increases the severity of skin conditions, including psoriasis .
Smoking and cancer risk
Smoking increases the risk of many types of cancer . According to the National Cancer Institute , tobacco smoke contains around 7,000 chemicals, of which at least 69 can cause cancer.
Figures from the American Cancer Society state that smoking causes around 30% of all cancer deaths in the U.S., and 80% of all lung cancer deaths.
Lung cancer is the leading cause of cancer death in both men and women. It is one of the most difficult to treat.
Smoking is a risk factor for the following cancers:
- larynx , or voice box
- pharynx , or throat
- esophagus , the tube connecting the mouth and stomach
- myeloid leukemia
Cigars, pipe-smoking, menthol cigarettes, chewing tobacco, and other forms of tobacco all cause cancer and other health problems. There is no safe way to use tobacco.
Read more about how smoking affects the body here.
The benefits of quitting
While the statistics are alarming, the good news is that quitting smoking reduces the risk of disease and death significantly. The risks drop further, the longer a person refrains from smoking.
In fact, some research says that quitting before the age of 40 reduces the risk of dying from smoking-related disease by about 90% .
These statistics illustrate the health benefits of quitting smoking:
- Cardiovascular risks : After 1 year of quitting, the risk of having a heart attack drops sharply.
- Stroke : Within 2–5 years, the risk of a stroke reduces to half that of a non-smoker.
- Cancers : The risks for mouth, throat, esophagus, and bladder cancer drop by half within 5 years of quitting, and 10 years for lung cancer.
Soon after quitting, people experience the following health benefits that can significantly improve their quality of life and serve as reminders of the health benefits that quitting can have:
- breathing becomes easier
- daily coughing and wheezing reduces then disappears
- sense of taste and smell get better
- exercise and activities become easier
- circulation to the hands and feet improves
Read more about what happens when you quit smoking here.
Though quitting can be stressful, people often start to notice their daily stress levels are much lower than when they were smoking within 6 months or so.
Quitting smoking is a different journey for everyone, and what works for one person will not always work for the next. Try out a few different ways to see which ones work best.
When trying to quit smoking, these tips may help:
- Make lists of reasons why it is a good idea to quit. Read over these when the temptation to smoke strikes.
- Use an app to track your progress. Reaching milestones, such as a day without smoking, can help motivate a person to continue. There are many free and paid apps on the market.
- Try nicotine replacement products. Nicotine patches, gums, and lozenges can help reduce cravings, making it easier to resist at any particular moment.
Many people find that reaching out to a healthcare provider for support can help them quit for good. A doctor can prescribe medication, such as varenicline (Chantix). Experts currently recommend this as a first-line therapy for people who want to quit smoking.
Last medically reviewed on April 24, 2020
- Lung Cancer
- Respiratory
- Alcohol / Addiction / Illegal Drugs
- Smoking / Quit Smoking
How we reviewed this article:
- Bad breath: 6 causes (and 6 solutions). (n.d.). https://www.mouthhealthy.org/en/az-topics/b/bad-breath
- Current cigarette smoking among adults in the United States. (2019). https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm
- Halitosis. (n.d.). https://www.mouthhealthy.org/en/az-topics/h/halitosis
- Harms of cigarette smoking and health benefits of quitting. (2017). https://www.cancer.gov/about-cancer/causes-prevention/risk/tobacco/cessation-fact-sheet
- Health effects of cigarette smoking. (n.d). https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm
- Health risks of smoking tobacco. (2018). https://www.cancer.org/cancer/cancer-causes/tobacco-and-cancer/health-risks-of-smoking-tobacco.html
- How smoking affects your body. (n.d.). https://www.nhs.uk/smokefree/why-quit/smoking-health-problems
- Jha, P., et al. (2013). 21st-century hazards of smoking and benefits of cessation in the United States. https://www.nejm.org/doi/pdf/10.1056/NEJMsa1211128
- Kovac, J. R. (2015). The effects of cigarette smoking on male fertility. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4639396/
- Leone, F. T., et al. (2020). Initiating pharmacologic treatment in tobacco-dependent adults. An official American Thoracic Society Clinical Practice guideline. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7365361/
- Qiu, F., et al. (2017). Impacts of cigarette smoking on immune responsiveness: Up and down or upside down? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5352117/
- Simpkin, S. (2016). Smoking and its effects on the skin. https://dermnetnz.org/topics/smoking-and-its-effects-on-the-skin/
- Smoking and bone health. (2018). https://www.bones.nih.gov/health-info/bone/osteoporosis/conditions-behaviors/bone-smoking
- The health benefits of quitting smoking. (n.d.). https://www.quit.org.au/articles/the-health-benefits-of-quitting-smoking/
- Smoking and your heart. (n.d.). https://www.nhlbi.nih.gov/health-topics/smoking-and-your-heart
- The health consequences of smoking — 50 years of progress: A report of the Surgeon General executive summary. (2014). https://www.hhs.gov/sites/default/files/consequences-smoking-exec-summary.pdf
- Tobacco-related mortality. (n.d). https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/tobacco_related_mortality/index.htm
Share this article
Latest news
Related coverage.
Many people use vapes because they believe them to be safer than smoking and are an effective tool to quit smoking. But is it safe? Learn more about…
Hypnosis is a popular method for smoking cessation. Learn more about its effectiveness, how it works, possible benefits, and more here.
Although vaping water may seem like a "safe" alternative to nicotine e-liquids, it carries many of the same risks. Researchers are still investigating…
Tobacco and other ingredients in tobacco products can potentially cause allergies or allergy-like symptoms, such as wheezing and sneezing. Read more…
EnglishGrammarSoft

500 Words Essay on Smoking is bad for health
Essay on smoking is bad for health.
One of the most common problems that is killing people all over the world today is smoking.
This horrible habit cause stress, personal problems and lung problems to many people all over the world.
Some people start it as an exhibition while some people use it to enjoy it.
One smoker can cause another person to smoke, which can lead to addiction. When a person smokes or smokes, he hurts not only himself but also others around him.
Smoking causes many terrible diseases to the human body. Almost everyone knows that smoking causes cancer and heart disease.
Studies have shown that the habit of smoking can shorten a person’s life by about 10 years and this bad habit causes thousands of cigarettes to be smoked every year.
Read also: Essay on Education for All
Obviously, smoking is a very bad habit because tobacco contains nicotine which is highly addictive, and because of which one cannot give up this addiction easily.
Most teenagers use this drink because they want to stay fit. When teenagers see their friends smoking, it becomes clear to them that they look happy or free because of smoking, although this is not the case at all.
The first cause of smoking, which is nicotine, is an addictive and harmful substance in cigarettes. It reduces stress and is thought to calm people who are restless and anxious.
The second most common cause of smoking is “psychological”, which is a very important factor in getting people into the habit. Some children get addicted to it at an early age due to which they have to face serious health issues.
Many people who start smoking are family members or close friends of the person whom they also become addicted to and start smoking.
Smoking is like a slow death. There are various examples of the harms of smoking. Such as smoking causes lung cancer, heart disease, stroke, asthma, and a wide variety of other diseases.
You might be interested: Essay on Why Trees are Important in our Life
Smokers have more coughs and colds than non-smokers. In addition to affecting themselves, smokers also have a negative effect on other people around them, which is also called second hand smoking.
Also, pregnant women who are exposed to cigarette smoke have an increased risk of having abnormal babies.
Have you ever thought, what is in cigarettes that is pushing millions of people to smoke every day?
Cigarettes contain more than 4,000 toxins, some of which are: arsenic (found in rat poison), acetic acid (found in hair dye manufacturers), ammonia (found in household cleaners), benzene (found in rubber cement), butane (found in light liquids), carbon monoxide (found in car smoke), hydrazine and methanol (both found in rocket fuels).
Smoking is a habit that people find it difficult to quit. Many people prepare in various ways in an effort to get rid of the habit of months.
Many teenagers smoke due to stress and tension but they do not know how smoking kills them slowly and puts their health at risk. But teenagers don’t think.
Always try to avoid smoking. Keep in mind the consequences before starting it. Smoking is bad for everyone !!!!!!
Similar Posts
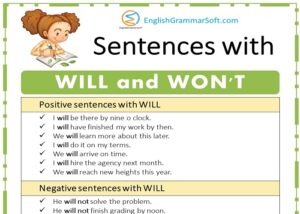
Sentences with WILL and WON’T
Will expresses intention and is usually followed by an infinitive (“I will see him”). Won’t expresses unwillingness or denial (“I won’t see him”) and is…
Essay about Can Money Buy Happiness?
Can money buy happiness? Many people would answer ‘yes’, that if you have enough money, you will be happy. But not everyone has the same…
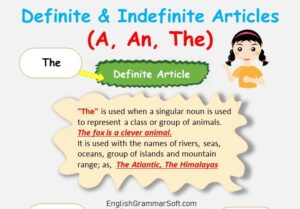
Definite and Indefinite Articles (A, An, The) Rules, Examples & Definition
‘A’, ‘An’, and ‘The’ are called articles. They are really demonstrative. It means they are adjectives used to point to something. Definite and Indefinite Articles…
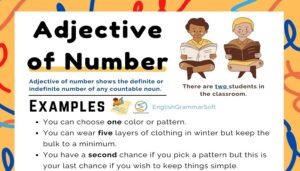
Adjective of Number (Examples, List & Worksheet)
Adjective of number shows the definite or indefinite number of a person, thing or place. For example, I have two bikes. It is used with…
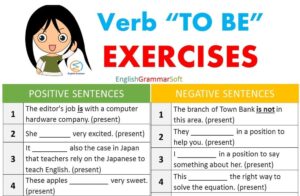
Verb TO BE Positive Negative and Questions Exercises (for beginners)
Verb TO BE Positive Negative and Questions Exercises Verb ‘TO BE’ Positive The editor’s job is with a computer hardware company. (be) She __________ very…
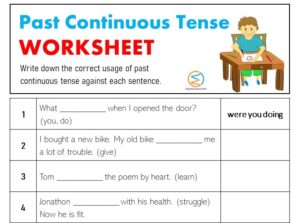
Past Continuous Tense Worksheet with Answers
Past Continuous Tense Worksheet with Answers What __________ when I opened the door? (you, do) I bought a new bike. My old bike __________ me…
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Essay on Smoking
500 words essay on smoking.
One of the most common problems we are facing in today’s world which is killing people is smoking. A lot of people pick up this habit because of stress , personal issues and more. In fact, some even begin showing it off. When someone smokes a cigarette, they not only hurt themselves but everyone around them. It has many ill-effects on the human body which we will go through in the essay on smoking.

Ill-Effects of Smoking
Tobacco can have a disastrous impact on our health. Nonetheless, people consume it daily for a long period of time till it’s too late. Nearly one billion people in the whole world smoke. It is a shocking figure as that 1 billion puts millions of people at risk along with themselves.
Cigarettes have a major impact on the lungs. Around a third of all cancer cases happen due to smoking. For instance, it can affect breathing and causes shortness of breath and coughing. Further, it also increases the risk of respiratory tract infection which ultimately reduces the quality of life.
In addition to these serious health consequences, smoking impacts the well-being of a person as well. It alters the sense of smell and taste. Further, it also reduces the ability to perform physical exercises.
It also hampers your physical appearances like giving yellow teeth and aged skin. You also get a greater risk of depression or anxiety . Smoking also affects our relationship with our family, friends and colleagues.
Most importantly, it is also an expensive habit. In other words, it entails heavy financial costs. Even though some people don’t have money to get by, they waste it on cigarettes because of their addiction.
How to Quit Smoking?
There are many ways through which one can quit smoking. The first one is preparing for the day when you will quit. It is not easy to quit a habit abruptly, so set a date to give yourself time to prepare mentally.
Further, you can also use NRTs for your nicotine dependence. They can reduce your craving and withdrawal symptoms. NRTs like skin patches, chewing gums, lozenges, nasal spray and inhalers can help greatly.
Moreover, you can also consider non-nicotine medications. They require a prescription so it is essential to talk to your doctor to get access to it. Most importantly, seek behavioural support. To tackle your dependence on nicotine, it is essential to get counselling services, self-materials or more to get through this phase.
One can also try alternative therapies if they want to try them. There is no harm in trying as long as you are determined to quit smoking. For instance, filters, smoking deterrents, e-cigarettes, acupuncture, cold laser therapy, yoga and more can work for some people.
Always remember that you cannot quit smoking instantly as it will be bad for you as well. Try cutting down on it and then slowly and steadily give it up altogether.
Get the huge list of more than 500 Essay Topics and Ideas
Conclusion of the Essay on Smoking
Thus, if anyone is a slave to cigarettes, it is essential for them to understand that it is never too late to stop smoking. With the help and a good action plan, anyone can quit it for good. Moreover, the benefits will be evident within a few days of quitting.
FAQ of Essay on Smoking
Question 1: What are the effects of smoking?
Answer 1: Smoking has major effects like cancer, heart disease, stroke, lung diseases, diabetes, and more. It also increases the risk for tuberculosis, certain eye diseases, and problems with the immune system .
Question 2: Why should we avoid smoking?
Answer 2: We must avoid smoking as it can lengthen your life expectancy. Moreover, by not smoking, you decrease your risk of disease which includes lung cancer, throat cancer, heart disease, high blood pressure, and more.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

- Help & Support
- Quit Smoking
- Tobacco Facts
- Health Effects of Smoking and Tobacco Products
Health Effects of Smoking
Smoking is the number one cause of preventable disease and death worldwide. Smoking-related diseases claim more than 480,000 lives in the U.S. each year. Smoking costs the U.S. at least $289 billion each year, including at least $151 billion in lost productivity and $130 billion in direct healthcare expenditures. 1
Key Facts about Smoking
- Cigarette smoke contains more than 7,000 chemicals, at least 69 of which are known to cause cancer. 2 Smoking is directly responsible for approximately 90 percent of lung cancer deaths and approximately 80 percent of deaths caused by chronic obstructive pulmonary disease (COPD), including emphysema and chronic bronchitis. 1
- Among adults who have ever smoked daily, 78% had smoked their first cigarette by the time they were 18 years of age, and 94% had by age 21. 3
- Among current smokers, 73% of their diagnosed smoking-related conditions are chronic lung diseases. Even among smokers who have quit, chronic lung disease still accounts for 50% of smoking-related conditions. 4
- Smoking harms nearly every organ in the body, and is a main cause of lung cancer and COPD. It also is a cause of coronary heart disease, stroke and a host of other cancers and diseases. 1 See more of the health effects caused by smoking.
Smoking Rates among Adults & Youth
- In 2017, an estimated 34.3 million, or 14.0% of adults 18 years of age and older were current cigarette smokers. 5
- Men tend to smoke more than women. In 2017, 15.8% of men currently smoked cigarettes daily compared to 12.2% of women. 5
- Prevalence of current cigarette smoking in 2017 was highest among American Indians/Alaska Natives (24.6%), non-Hispanic whites (15.3%) and non-Hispanic blacks (15.1%), and was lowest among Hispanics (9.9%) and Asian-Americans (7.0%). 5
- In 2017, 7.6 % of high school students and 2.1% of middle school students were current cigarette users. 6
Facts about Quitting Smoking
- Nicotine is the chemical in cigarettes that causes addiction. Smokers not only become physically addicted to nicotine; they also link smoking with many social activities, making smoking an extremely difficult addiction to break. 7
- In 2017, an estimated 55.2 million adults were former smokers. Of the 34.3 million current adult smokers, 48.4% stopped smoking for a day or more in the preceding year because they were trying to quit smoking completely. 5
- Quitting smoking for good often requires multiple attempts. Using counseling or medication alone increases the chance of a quit attempt being successful; the combination of both is even more effective. 8
- There are seven medications approved by the U.S. Food and Drug Administration to aid in quitting smoking. Nicotine patches, nicotine gum and nicotine lozenges are available over the counter, and a nicotine nasal spray and inhaler are currently available by prescription. Bupropion SR (Zyban®) and varenicline (Chantix®) are non-nicotine pills. 8
- Individual, group and telephone counseling are effective. Telephone quitline counseling is available in all 50 states and is effective for many different groups of smokers. 8
Learn about the American Lung Association’s programs to help you or a loved one quit smoking , and join our advocacy efforts to reduce tobacco use and exposure to secondhand smoke. Visit Lung.org or call the Lung HelpLine at 1-800-LUNGUSA (1-800-586-4872).
The Health Effects of Smoking
U.S. Department of Health and Human Services. The Health Consequences of Smoking - 50 Years of Progress: A Report of the Surgeon General. 2014.
U.S. Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease A Report of the Surgeon General. 2010.
Substance Abuse and Mental Health Services Administration. National Survey on Drug Use and Health, 2017. Analysis by the American Lung Association Epidemiology and Statistics Unit using SPSS software.
U.S. Department of Health and Human Services. The Health Consequences of Smoking: A Report of the Surgeon General, 2004.
Centers for Disease Control and Prevention. National Center for Health Statistics. National Health Interview Survey, 2015. Analysis performed by the American Lung Association Epidemiology and Statistics Unit using SPSS software.
Centers for Disease Control and Prevention. National Youth Tobacco Survey, 2017. Analysis by the American Lung Association Epidemiology and Statistics Unit using SPSS software.
National Institute on Drug Abuse. Tobacco/Nicotine Research Report: Is Nicotine Addictive? January 2018.
Fiore M, Jaen C, Baker T, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Vol 35. Rockville, MD; 2008.
Page last updated: May 31, 2023
A Breath of Fresh Air in Your Inbox
Join over 700,000 people who receive the latest news about lung health, including research, lung disease, air quality, quitting tobacco, inspiring stories and more!
You will now receive email updates from the American Lung Association.
Make a Donation
Your tax-deductible donation funds lung disease and lung cancer research, new treatments, lung health education, and more.
Become a Lung Health Insider
Thank you! You will now receive email updates from the American Lung Association.
Select Your Location
Select your location to view local American Lung Association events and news near you.
Change Language
Lung helpline.
Talk to our lung health experts at the American Lung Association. Our service is free and we are here to help you.
1-800-LUNG-USA
(1-800-586-4872)

Essay on Negative Effects Of Smoking
Students are often asked to write an essay on Negative Effects Of Smoking in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Negative Effects Of Smoking
Introduction to smoking.
Smoking is a bad habit that harms our body. Many people smoke cigarettes, cigars, or pipes. Some people also chew tobacco. These things contain nicotine, a harmful chemical. It’s highly addictive, meaning once you start smoking, it’s very hard to stop.
Health Problems Caused by Smoking
Smoking can cause many health problems. It can lead to lung cancer, heart disease, and stroke. It can also cause other types of cancer, like mouth and throat cancer. Smoking can make it hard to breathe and can cause chronic coughing.
Smoking and Secondhand Smoke
Not only does smoking hurt the smoker, but it also harms others around them. This is called secondhand smoke. It can cause the same health problems in non-smokers. Children exposed to secondhand smoke can get sick more often.
Smoking and Appearance
Smoking can also affect how you look. It can cause yellow teeth and bad breath. It can also cause your skin to age faster, leading to wrinkles. Smoking can even cause hair loss and turn your fingers yellow.
In conclusion, smoking is very harmful. It can cause many health problems and can even harm others around you. It’s best to avoid this bad habit. If you or someone you know smokes, try to quit. Your body will thank you.
250 Words Essay on Negative Effects Of Smoking
Introduction.
Smoking is a harmful habit that many people around the world have. It is bad for our health and the environment. This essay will talk about the negative effects of smoking.
Damages to Health
Smoking hurts our bodies in many ways. It is the main cause of lung cancer. This is a very serious disease that can lead to death. Other than lung cancer, smoking can also cause heart disease. This is because the smoke makes it harder for the heart to pump blood.
Problems for the Environment
Smoking is not just bad for our health, but also for our environment. Cigarette butts are often thrown on the ground, causing pollution. Also, the smoke from cigarettes adds to air pollution. This is bad for all living things, not just humans.
Effects on Others
Smoking is not only harmful to the person who smokes, but also to the people around them. This is called second-hand smoke. It can cause the same health problems as smoking does. This means that even if you do not smoke, you can still get sick from being around someone who does.
In conclusion, smoking is a harmful habit with many negative effects. It causes health problems, harms the environment, and can even make others sick. It is important to avoid smoking for a healthier and safer world.
500 Words Essay on Negative Effects Of Smoking
Smoking is a habit that many people pick up due to various reasons, such as stress, peer pressure, or even out of curiosity. Despite its popularity, smoking has many negative effects on our health and the environment. This essay will discuss these harmful effects in simple terms.
Effects on Personal Health
Firstly, let’s talk about how smoking harms our own health. When you smoke, you inhale many dangerous chemicals. These chemicals can harm nearly every organ in your body. The most commonly known health problem caused by smoking is lung cancer. But that’s not all. Smoking can also lead to other types of cancer, such as mouth cancer and throat cancer.
Apart from cancer, smoking can cause heart disease. The chemicals in smoke make it harder for your heart to work properly. This can lead to heart attacks. Smoking also harms your lungs, making it difficult to breathe. This can lead to diseases like bronchitis and emphysema.
Effects on Others’ Health
Smoking is not only harmful to the smoker but also to those around them. This is called secondhand smoke. When you smoke, the people around you also breathe in the harmful chemicals. This can lead to the same health problems that smokers face. Children are particularly at risk. They can suffer from problems like asthma, ear infections, and even sudden infant death syndrome.
Effects on the Environment
Smoking also hurts our environment. Cigarette butts, which are often thrown away carelessly, are a form of litter. They can take many years to break down and are harmful to wildlife. The smoke from cigarettes also adds to air pollution. This can harm the air we all breathe and contribute to climate change.
Effects on Personal Life
Lastly, smoking can affect your personal life. It can make your clothes and breath smell bad, which can affect your relationships with others. It can also be a costly habit. The money spent on cigarettes could be used for other things like education, hobbies, or saving for the future.
In conclusion, smoking has many negative effects. It harms our health, the health of those around us, our environment, and our personal lives. It’s important to understand these effects and to make healthy choices for ourselves and our communities. Remember, it’s never too late to quit smoking and start living a healthier life.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Negative Effects Of Religion
- Essay on Negative Effects Of Music
- Essay on Negative Effects Of Mobile Phones
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Health Effects
Smoking leads to disease and disability and harms nearly every organ of the body.
More than 16 million Americans are living with a disease caused by smoking. For every person who dies because of smoking, at least 30 people live with a serious smoking-related illness. Smoking causes cancer, heart disease, stroke, lung diseases, diabetes, and chronic obstructive pulmonary disease (COPD), which includes emphysema and chronic bronchitis. Smoking also increases risk for tuberculosis, certain eye diseases, and problems of the immune system, including rheumatoid arthritis.
Secondhand smoke exposure contributes to approximately 41,000 deaths among nonsmoking adults and 400 deaths in infants each year. Secondhand smoke causes stroke, lung cancer, and coronary heart disease in adults. Children who are exposed to secondhand smoke are at increased risk for sudden infant death syndrome, acute respiratory infections, middle ear disease, more severe asthma, respiratory symptoms, and slowed lung growth.

Tobacco use increases the risk for many types of cancer, such as Lung cancer.

Heart Disease
Studies show a direct link between cigarette smoking and coronary heart disease.

Smoking, including during the teenage years, increases the risk of dying from COPD.

Smoking during pregnancy increases the risk for pregnancy complications.
Related Materials
- Health Effects of Cigarette Smoking
- Health Effects of Secondhand Smoke
- Tobacco-Related Mortality
- 50 Years of Progress: A Report of the Surgeon General [PDF–35.9 MB]
- U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General . Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014 [accessed 2016 Dec 20].
To receive email updates about Smoking & Tobacco Use, enter your email address:
- Tips From Former Smokers ®
- Division of Cancer Prevention and Control
- Lung Cancer
- National Comprehensive Cancer Control Program
- Division of Reproductive Health

Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Persuasive Essay Guide
Persuasive Essay About Smoking
Persuasive Essay About Smoking - Making a Powerful Argument with Examples

People also read
A Comprehensive Guide to Writing an Effective Persuasive Essay
200+ Persuasive Essay Topics to Help You Out
Learn How to Create a Persuasive Essay Outline
30+ Free Persuasive Essay Examples To Get You Started
Read Excellent Examples of Persuasive Essay About Gun Control
How to Write a Persuasive Essay About Covid19 | Examples & Tips
Crafting a Convincing Persuasive Essay About Abortion
Learn to Write Persuasive Essay About Business With Examples and Tips
Check Out 12 Persuasive Essay About Online Education Examples
Are you wondering how to write your next persuasive essay about smoking?
Smoking has been one of the most controversial topics in our society for years. It is associated with many health risks and can be seen as a danger to both individuals and communities.
Writing an effective persuasive essay about smoking can help sway public opinion. It can also encourage people to make healthier choices and stop smoking.
But where do you begin?
In this blog, we’ll provide some examples to get you started. So read on to get inspired!
- 1. What You Need To Know About Persuasive Essay
- 2. Persuasive Essay Examples About Smoking
- 3. Argumentative Essay About Smoking Examples
- 4. Tips for Writing a Persuasive Essay About Smoking
What You Need To Know About Persuasive Essay
A persuasive essay is a type of writing that aims to convince its readers to take a certain stance or action. It often uses logical arguments and evidence to back up its argument in order to persuade readers.
It also utilizes rhetorical techniques such as ethos, pathos, and logos to make the argument more convincing. In other words, persuasive essays use facts and evidence as well as emotion to make their points.
A persuasive essay about smoking would use these techniques to convince its readers about any point about smoking. Check out an example below:
Simple persuasive essay about smoking
Tough Essay Due? Hire Tough Writers!
Persuasive Essay Examples About Smoking
Smoking is one of the leading causes of preventable death in the world. It leads to adverse health effects, including lung cancer, heart disease, and damage to the respiratory tract. However, the number of people who smoke cigarettes has been on the rise globally.
A lot has been written on topics related to the effects of smoking. Reading essays about it can help you get an idea of what makes a good persuasive essay.
Here are some sample persuasive essays about smoking that you can use as inspiration for your own writing:
Persuasive speech on smoking outline
Persuasive essay about smoking should be banned
Persuasive essay about smoking pdf
Persuasive essay about smoking cannot relieve stress
Persuasive essay about smoking in public places
Speech about smoking is dangerous
Persuasive Essay About Smoking Introduction
Persuasive Essay About Stop Smoking
Short Persuasive Essay About Smoking
Stop Smoking Persuasive Speech
Check out some more persuasive essay examples on various other topics.
Argumentative Essay About Smoking Examples
An argumentative essay is a type of essay that uses facts and logical arguments to back up a point. It is similar to a persuasive essay but differs in that it utilizes more evidence than emotion.
If you’re looking to write an argumentative essay about smoking, here are some examples to get you started on the arguments of why you should not smoke.
Argumentative essay about smoking pdf
Argumentative essay about smoking in public places
Argumentative essay about smoking introduction
Check out the video below to find useful arguments against smoking:
Tips for Writing a Persuasive Essay About Smoking
You have read some examples of persuasive and argumentative essays about smoking. Now here are some tips that will help you craft a powerful essay on this topic.
Choose a Specific Angle
Select a particular perspective on the issue that you can use to form your argument. When talking about smoking, you can focus on any aspect such as the health risks, economic costs, or environmental impact.
Think about how you want to approach the topic. For instance, you could write about why smoking should be banned.
Check out the list of persuasive essay topics to help you while you are thinking of an angle to choose!
Research the Facts
Before writing your essay, make sure to research the facts about smoking. This will give you reliable information to use in your arguments and evidence for why people should avoid smoking.
You can find and use credible data and information from reputable sources such as government websites, health organizations, and scientific studies.
For instance, you should gather facts about health issues and negative effects of tobacco if arguing against smoking. Moreover, you should use and cite sources carefully.
Paper Due? Why Suffer? That's our Job!
Make an Outline
The next step is to create an outline for your essay. This will help you organize your thoughts and make sure that all the points in your essay flow together logically.
Your outline should include the introduction, body paragraphs, and conclusion. This will help ensure that your essay has a clear structure and argument.
Use Persuasive Language
When writing your essay, make sure to use persuasive language such as “it is necessary” or “people must be aware”. This will help you convey your message more effectively and emphasize the importance of your point.
Also, don’t forget to use rhetorical devices such as ethos, pathos, and logos to make your arguments more convincing. That is, you should incorporate emotion, personal experience, and logic into your arguments.
Introduce Opposing Arguments
Another important tip when writing a persuasive essay on smoking is to introduce opposing arguments. It will show that you are aware of the counterarguments and can provide evidence to refute them. This will help you strengthen your argument.
By doing this, your essay will come off as more balanced and objective, making it more convincing.
Finish Strong
Finally, make sure to finish your essay with a powerful conclusion. This will help you leave a lasting impression on your readers and reinforce the main points of your argument. You can end by summarizing the key points or giving some advice to the reader.
A powerful conclusion could either include food for thought or a call to action. So be sure to use persuasive language and make your conclusion strong.
To conclude,
By following these tips, you can write an effective and persuasive essay on smoking. Remember to research the facts, make an outline, and use persuasive language.
However, don't stress if you need expert help to write your essay! We're the best essay writing service for you!
Our persuasive essay writing service is fast, affordable, and trustworthy.
Try it out today!

Write Essay Within 60 Seconds!

Caleb S. has been providing writing services for over five years and has a Masters degree from Oxford University. He is an expert in his craft and takes great pride in helping students achieve their academic goals. Caleb is a dedicated professional who always puts his clients first.

Paper Due? Why Suffer? That’s our Job!
Keep reading


Smoking Cigarettes: Bad for One's Health Essay examples
Smoking Cigarettes: Bad for One’s Health Smoking cigarettes is very bad for one’s health. Yet people all over the world do it every day. No matter how many warnings that the Surgeon General puts on cigarette packs people still smoke. . I feel that as years go by people are understanding the risks that go along with smoking cigarettes more and more. Hopefully in the future everyone will understand the risks and cigarettes will be banned. Smoking cigarettes can cause many different types of diseases and illnesses, such as cancer, chronic obstructive pulmonary disease , and coronary artery disease, throughout the human body. First of all, cigarette smoking can cause a person to have cancer. It doesn’t have a specific place in the body …show more content…
Chronic pulmonary disease is a very serious disease caused by cigarette smoking. Last of all, cigarettes can make a person to have coronary artery disease, which is a very serious disease. The toxins in tobacco smoke, particularly tar and carbon monoxide, harden the arteries and increase the risk of blood clots (healthy.yahoo.net/channel/coronary- heart -disease.html). This can lead to a heart attack or a stroke (healthy.yahoo.net/channel/coronary-heart-disease.html). One way a person can tell if they have this disease is if they have chest pain or discomfort. The pain may feel like someone is squeezing ones heart. The pain usually occurs with activity or emotion, and goes away with rest or a medication. Other symptoms include shortness of breath and fatigue. If a person has a lot of chest pains, they need to get checked immediately. Coronary artery disease can be treated and controlled, but can accelerate quickly with smoking cigarettes. Cigarette smoking is dangerous and very bad for one’s health. Smoking can cause many kinds of diseases. Cancer, chronic pulmonary disease, and coronary artery disease are all very serious diseases but can be prevented and cured with the right care. If someone smokes the need to find a way to quit smoking, that works for them. I am a person that is trying to quit smoking. It is a very hard thing to accomplish, but I know with hard work and determination I will be able to kick this
Should Smoking In Public Areas Be Allowed
Cigarettes don’t only cause lung cancers but can also cause other problems to the heart and blood vessels. Some other cancers associated with smoking include larynx, esophagus, bladder, kidney, pancreas, stomach, and some other organs.
Should The NHS Treat Smoking-Related Diseases?
Smoking can bring about lung infection by harming your airways routes and the little air sacs (alveoli) found in your lungs. Smoking can bring about lethal infections, for example, pneumonia, lung growth and emphysema. Additionally smoking causes 83% of deaths from chronic obstructive pulmonary disease (COPD) and smoking causes 84% of deaths from lung cancer (NHS , 2017) . However, there is a considerable measure of terrible illnesses connected to smoking cigarettes. Illnesses like throat malignancy, mouth tumour, bladder growth, lung growth, constant bronchitis, emphysema, and coronary illness are altogether brought about by smoking. Also smoking is addictive. Nicotine is the addictive substance
Persuasive Essay: Why People Shouldn T Smoke
You shouldn’t smoke because it is bad for your lungs, it can cause heart attacks, and it is harsh for people who work in tobacco fields. Smoking is bad for your lungs because it can cause lung cancer. More than 80% of cases of lung cancer are caused by smoking. Smoking can cause heart attacks because smoking increases the risk of developing Cardiovascular, which includes Coronary Heart disease and stroke. It is also bad to smoke because you could die at a young age.
Should The Us Banning Cigarettes
This year alone cigarettes will end up killing over 500,000 Americans, and many more will suffer from different types of cancer, circulatory, and respiratory system diseases, due to smoking cigarettes. Cigarettes have been known to cause these illnesses for a long time. The FDA has proven that nicotine, one of the main chemicals in cigarettes, is addictive. This explains why smokers continue to use cigarettes even though they are aware of the health dangers that come from smoking cigarettes. Researchers have also found out that when people smoke by pregnant women it causes the deaths of over 4,000 babies and 110,000 miscarriages. The only way to prevent death by cigarettes would be to ban them.
Vaping Research Papers
While it’s true that smoking cigarette is not good for the health, many people are still smoking cigarettes. Though some of them have tried to stop this habit, however, most of them have failed and have continued to smoke at the expense of their health.
Nutrition and Life Style
Tobacco smoking is responsible for nearly all cases of a chronic breathing obstruction known as Chronic Obstructive Pulmonary Disease (COPD). COPD includes diseases like emphysema and chronic bronchitis, and leaves sufferers breathless and unable to do many activities. Lung cancer is the disease of the smoker, with 90% of primary lung cancers caused by smoking. Nearly one in four smokers who die prematurely will die of lung cancer. Lung cancer is the biggest cancer killer in the UK. Your lungs are damaged not only by the number of cigarettes you smoke a day, but more importantly by the number of years you have been a smoker. So,
COPD Paragraph
Cigarette smoking can lead to several different types of cancer that can cause death. People who smoke cigarettes put their self at greater risk for types of cancer. If you smoke you can get COPD. COPD stands for Chronic Obstruction Pulmonary Disease. COPD is a disease that a lot of smokers get that causes them great difficulty breathing. People with COPD have other symptoms as well like wheezing, large amounts of mucus, and
Smoking Builds In The Artery
Smoking produces plaque which builds in the arteries. Over time, once enough plaque builds up, it will cause a heart attack or stroke. Whereas, if the plaque builds in the heart arteries it causes coronary heart disease which immensely increases one chance of having a heart attack, heart failure, arrhythmias, or death. The building of plaque in the arteries is harmful to the body.
Rheumatoid Smoking
Smoking is a leading cause of cancer throughout the body including: the lungs, esophagus, larynx, mouth, throat, kidney, bladder, liver, pancreas, stomach, cervix, colon, and rectum, as well as acute myeloid leukemia. Smoking causes a number of diseases within your body including heart disease, stroke, aortic aneurysm, COPD, chronic bronchitis, emphysema, diabetes, osteoporosis, rheumatoid arthritis, age-related macular degeneration, cataracts, and also worsens asthma symptoms in adults. Smoking not only
Smoking In The United States
Smoking can lead to health problems that can destroy the consumers future. Smoking is one of the leading causes of death in the U.S. each year. For example, "Smoking has killed more people in the U.S. alone than the number of Americans killed in battle or who died of war related diseases in all wars ever fought by this nation. The total number of U.S. deaths in the Vietnam War was 58,151,¨(¨Other Health Dangers¨). Smoking has many different chemicals that are harmful to the body. Some of the problems that are caused by smoking are lung cancer, cancers of the mouth, larynx (throat), esophagus, bladder, kidney, cervix, and blood (leukemia). These can all be caused by smoking and then there will be a greater risk of getting these
Nicotine Addiction To Smoking Essay
Smoking is the number one cause of preventable death in the United States. Nicotine addiction is a serious and expensive problem. Smokers have decreased productivity and on average make less than non-smokers. Smoking is lethal to the human body through heart disease, respiratory illness, and increased likelihood and mortality of cancer.
Persuasive Essay On Tobacco
Furthermore, the use of tobacco products can have a negative impact on almost every major organ in the human body. The impact of smoking greatly reduces the function of the heart and blood vessels as well as, how smoking can affect an individual lungs and breathing. Smoking can create negative health conditions such as atherosclerosis that can be developed due to impact of smoking. Other medical conditions that can be developed due to the use of smoking is the development of aneurysms and/or cardiovascular disease, high blood pressure, chest pains, and the potential for having a heart attack. Additionally, the U.S Department of Health and Human Services (2012), states,
Don T Smoke Persuasive Research Paper
Studies done by the CDC show that cigarette smoke takes 480,000 lives a year? They cause more death than HIV, alcohol use, motor vehicle related deaths, firearm related deaths and illegal drug use death combined. The effects of smoking can cause cancer to appear in any part of the human body including your lungs, bladder and liver. Cigarette smoke affects heart by forming clots due to your blood vessels thickening and growing narrow. This effect causes individuals to have high blood pressure and faster heartbeats. Also, did you know that cigarettes affect pregnancy in women and compromise baby health. Preterm delivery, stillbirth and orofacial cleft are some of the problems that are presented with smoking. So, the next time you want to pick up a cigarette, you should think about your health and the severe effects
Cigarette Smoking Essay
- 2 Works Cited
The effects of cigarette smoking can be horrifying. Smoking is dangerous not only to those who smoke, but to non-smokers and unborn children as well. Cigarette smoking is also physically and socially harming.
Essay On Cigarette Smoking
Cigarette smoking is something people all over the world have been doing for about 2000 years. Back in 2003, the first electronic cigarette was successfully created by a gentleman named Hon Lik. Lik was a 52 year old pharmacist at the time, whom of which was also a smoker. The inspiration behind making the electronic cigarette came after Lik’s father passed away from lung cancer due to him also being a heavy smoker. “A Historical Timeline of Electronic Cigarettes.” cassia.org. Consumer Advocates for Smoke Free Alternatives Association, 15 June 2017. The idea behind creating this device was to give smokers a way to still ingest nicotine, the most addictive chemical in tobacco cigarettes, without the countless negative health effects that
Related Topics
- Chronic obstructive pulmonary disease
- Lung cancer
- Tobacco smoking

- Environment
- Information Science
- Social Issues
- Argumentative
- Cause and Effect
- Classification
- Compare and Contrast
- Descriptive
- Exemplification
- Informative
- Controversial
- Exploratory
- What Is an Essay
- Length of an Essay
- Generate Ideas
- Types of Essays
- Structuring an Essay
- Outline For Essay
- Essay Introduction
- Thesis Statement
- Body of an Essay
- Writing a Conclusion
- Essay Writing Tips
- Drafting an Essay
- Revision Process
- Fix a Broken Essay
- Format of an Essay
- Essay Examples
- Essay Checklist
- Essay Writing Service
- Pay for Research Paper
- Write My Research Paper
- Write My Essay
- Custom Essay Writing Service
- Admission Essay Writing Service
- Pay for Essay
- Academic Ghostwriting
- Write My Book Report
- Case Study Writing Service
- Dissertation Writing Service
- Coursework Writing Service
- Lab Report Writing Service
- Do My Assignment
- Buy College Papers
- Capstone Project Writing Service
- Buy Research Paper
- Custom Essays for Sale
Can’t find a perfect paper?
- Free Essay Samples
Essays on Smoking
Essay-writers in each smoking essay emphasize the dangers of smoking, and fairly so. After all, smoking is one of the most widespread bad habits in the world – there are about 2 billion smokers worldwide. It is a detrimental habit, as cigarette smoke contains more than 30 toxic components – you can go into them one by one in your essays on smoking. It's no secret how dangerous smoking is, however, around 18 billion cigarettes are sold globally every day. Smoking essays often include a lot of statistics, as facts speak louder than opinions. An estimated $50 billion a year is spent on treating smoking-related diseases in the United States alone. This means that for every pack of cigarettes, about $2 are spent on treating smoking-related diseases. Crazy, right? If you need more info on smoking for your essays, review our smoking essay samples.
Smoking and its Impact on Health Smoking predisposes one to various health problems including cancer of the lung, addiction, and adoption of harmful behaviors. Amongst adult smokers, smoking patterns have shown no significant reduction and a possible rise in smoking in the young individuals and the preteens has been reported (Lando,...
Words: 1022
1. Do you agree with the no smoking law in all public buildings in the state of Illinois? Should other states pass this law? What are the physical effects of second hand smoke on a child's airway? Should smoking in the presence of young children be...
Smoking in Public Places: A Health Hazard Smoking in public places is a health hazard for the smokers as well as the non-smoking public. The main dangers of smoking in public are often health-related as well as accident fires. More fatalities arise from public smoking are connected to the adverse effects...
Words: 1538
The World Health Organization suggests that approximately 5 million people die every year in the world because of tobacco use. Further, the report argues that, “the use of tobacco may cause about one billion deaths in the 21st century if current trends continue” (World Health Organization, " Research for International...
The Health Risks of Public Smoking The ban on smoking in public spaces has been an ongoing topic of discussion in different health platforms all over the world. Every year, several people are reported to die from lung cancer and other smoking-related health conditions. Nonetheless, despite the several reported deaths, tobacco...
Words: 1695
The number of the individuals who smoke has risen over the years. Even though they are aware of how harmful smoking can be, the public still decides to use a cigarette. It is an individual decision, and it is a habit which is extremely addictive. It is not the responsibility...
Words: 1413
Found a perfect essay sample but want a unique one?
Request writing help from expert writer in you feed!
The opening sentence The opening sentence used by the author does not induce vigor of reading the article. Words arrangement in the sentence is not right, it should have read, ‘Herbert A. Gilbert filed the first electronic cigarette for a patent in 1963.’ The writer assumes that the reader knows what...
The Importance of Tobacco Control Policies Over the years, tobacco smoking has become a worldwide concern for health. Thus, the US government alongside other countries has been on the move in passing policies and ordinances which control the use of tobacco. The health implications associated with tobacco smoking have been more...
Smoking is an endemic problem that not only affects smokers, but also goes as far as affecting innocent non-smoking public. At the core of this problem is the issue of smoking in public places. Being a risk to public health a ban on public smoking can be a life saver,...
Introduction Even though almost every smoker realizes the harm caused by smoking, the number of smokers in the world remains enormous. Due to a low price, availability, legality, and the promotion of cigarettes in the media, almost every second there is a new person that starts smoking. The main reason for...
Words: 1220
The cigarette is one of the deadliest drugs known to human beings. In the developed countries, there are attempts to minimize the smoking rates. There are different measures which have been suggested to help reduce the risks posed by consumption of the drug which includes increased taxes, bans on cigarette...
Words: 1017
The Question of Outlawing Cigarettes and Tobacco Products The question of whether cigarettes and other tobacco products should be outlawed is still an argument as many agree as well as disagree from the same. Tobacco is a plant which is grown and contains nicotine which affects one to be dependent on...
Words: 1040
Related topic to Smoking
Smoking: Causes and Effects Essay
Among numerous bad habits of modern society smoking seems to be of the greatest importance. Not only does it affect the person who smokes, but also those who are around him. Many people argue about the appropriate definition of smoking, whether it is a disease or just a bad habit. Considering the peculiarities of a habit and of a disease, smoking can be considered as a habit rather than a disease. Among signifiers of a bad habit, it should be pointed out that a bad habit can be controlled by willpower, it can be prevented, and it can be cured (Gilman and Zun 33). Smoking can be fought against with the help of all the points mentioned above. Thus, it is a bad habit which can be easily refused if an individual possessing it has a strong decision to quit. Moreover, it can be cured in many different ways, and it can be prevented by education and other social norms.
Considering the first element, which one of the most important out of the three, willpower is a key to get rid of such a bad habit as smoking, which is very difficult to give up. If a person has a strong determination to quit smoking, he will have to endure considerably a short period of time of physical discomfort. One of the most important part of quitting, is that that is doesn’t require medical help, that is to say, a person is not likely to suffer a procedure that is risky to health and life. In comparison to alcoholism or drug addiction, where medical help is essential to save life of a person who needs a certain amount of an alcohol or drug substance in has blood to survive, the lack of nicotine in blood produces just a physical discomfort that is not dangerous for health and can be handled with the help of willpower. Regarding the second aspect of a bad habit, prevention, smoking can be prevented in early childhood with the help of proper education and social norms (Brinkman et al 689). Many people start smoking when they are teenagers just to prove they are adults in companies. If the society was able to produce a negative impression of this bad habit, so that it doesn’t seem to be sign of being an adult, it would be easier to prevent many children from smoking (Albaum et al 11).
The last aspect of a bad habit is a cure for it. Smoking can be cured in many different ways. There are many different techniques, starting from a nicotine plaster and ending with special clinics and communities helping people to get rid of this problem. If a person wants to quit, he or she has various options to help him or her to solve this problem. To conclude, smoking is a bad habit that can be easily quitted. Although there is an addiction to smoking, the lack of nicotine is not dangerous to the life of a smoker and can be handled without medical intervention. The most important aspect of this bad habit, which actually makes a habit, is that it can be quitted with the help of willpower. Moreover, it can be prevented with alteration of attitude towards smoking and it can be cured in many different ways (Albaum et al 23).
Despite widespread public awareness of the multiple health risks associated with smoking, one out of every four girls under age 18 is a smoker and more than 25 million American women smoke. Whereas the last two decades have seen an overall decrease in smoking prevalence, the rate of smoking has declined much more slowly among women than among men. If current trends continue, smoking rates of women will overtake those of men by the year 2000. Smoking rates are highest, approaching 30%, among women of reproductive age (18–44 years). Rates of smoking are particularly high among young White women with a high school education or less and low income. Cessation rates are lower among African American women (30% have quit) compared to White women (43% have quit). Minority and young women who have low rates of self-initiated cessation are also underrepresented in formal smoking cessation programs (Gilman and Zun 87). A greater proportion of women than men are pre-contemplators, that is, not considering quitting smoking within 6 months and have lower self-confidence that they could quit if they were to try. The debate continues regarding whether or not women are less likely to be successful at quitting when they try than men, with some evidence suggesting that women are more likely than men to relapse and others indicating no gender differences). Regardless, rates of relapse are very high, both among self-quitters and those who participate in formal cessation programs (Albaum et al 24).
Interventions specifically designed for smokers have attempted to address the role of weight concerns as an inhibitor to cessation and long-term maintenance. A randomized trial tested nicotine gum or a behavioral weight control program each alone, or in combination as adjuncts to an intensive group cessation intervention for weight concerned women smokers. The intervention integrated accepted cognitive and behavioral coping strategies for quitting smoking, changing eating behaviors, and developing a walking program.
Works Cited
Albaum, G., Baker, K.G., Hozier, G.C., Rogers, R.D. Smoking Behavior, Information Sources, and Consumption Values of Teenagers: Implications for Public Policy and Other Intervention Failures. Journal of Consumer Affairs , 36 (1), 2002: 5-55.
Brinkman, M.C., Callahan, P.J., Gordon, S.M., Kenny, D.V., Wallace, L.A. Volatile Organic Compounds as Breath Biomarkers for Active and Passive Smoking. Environmental Health Perspectives, 110 (7), 2002, p. 689.
Gilman Sander L. and Xhou Zun. Smoke: A GlobalHistory of Smoking. Reaktion Books; illustrated edition edition, 2004.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, November 29). Smoking: Causes and Effects. https://ivypanda.com/essays/smoking-causes-and-effects/
"Smoking: Causes and Effects." IvyPanda , 29 Nov. 2021, ivypanda.com/essays/smoking-causes-and-effects/.
IvyPanda . (2021) 'Smoking: Causes and Effects'. 29 November.
IvyPanda . 2021. "Smoking: Causes and Effects." November 29, 2021. https://ivypanda.com/essays/smoking-causes-and-effects/.
1. IvyPanda . "Smoking: Causes and Effects." November 29, 2021. https://ivypanda.com/essays/smoking-causes-and-effects/.
Bibliography
IvyPanda . "Smoking: Causes and Effects." November 29, 2021. https://ivypanda.com/essays/smoking-causes-and-effects/.
- Free Will and Willpower: Is Consciousness Necessary?
- Francois Marie Arouet (Voltaire)
- Smoking Cessation for Ages 15-30
- Quitting Smoking: Strategies and Consequences
- Importance of Quitting Smoking
- Phineas Taylor Barnum - Biography Study
- Smoking Cessation Project Implementation
- Lifestyle Management While Quitting Smoking
- Is Alex in Burgess' "A Clockwork Orange" Cured?
- Advocating for Smoking Cessation: Health Professional Role
- The Relationship Between the High Rate of Urbanization in Africa and AIDS Spread
- California’s Growing Healthcare Crisis: An Existing Reality
- Environmental Health Problems and Health Inequity
- Public Health: Pertussis Cases in Wisconsin
- The Need for Health Care Reform in the USA
Premium Content

- MIND, BODY, WONDER
Do you smoke weed recreationally? Here's what experts want you to know.
Today’s cannabis strains are not your grandma’s weed—and they may be impacting your mental health, heart health, and more.
Some 23 states and the District of Columbia have legalized recreational cannabis in recent years, and others, including Florida, will vote to do so in November. This changing landscape has led to a dramatic rise in consumption, with some 62 million Americans using cannabis in 2023. But legalization of cannabis doesn’t mean that regular consumption is completely safe.
A growing body of evidence has documented an array of health concerns beyond just dry mouth and fatigue and includes both mental and physical illnesses. One recent study even links cannabis consumption to heart disease .
“People think about Bob Marley when they think about cannabis. They think it’s natural, it’s Mother Nature, that it’s not going to do any harm,” says Marco Solmi, a psychiatrist at the University of Ottawa. Yet his review of the substance published in the BMJ found numerous potential problems .
Cannabis isn’t dangerous in the same way opioids are, says Deborah Hasin, an epidemiologist at Columbia University who has researched cannabis use and abuse. “People don’t die from cannabis overdose,” she says. “But it can have a lot of other consequences to both physical and psychological health.”
Stronger strains abound

Some of the problems can be attributed to the stronger strains now available . As Maria Rahmandar, medical director of the substance use and prevention program at Chicago’s Lurie Children’s Hospital, put it at a recent discussion of cannabis at the National Academies of Sciences, Engineering, and Medicine, today’s products are “not your grandmother’s weed.”
“These products are much more potent and come in so many different formulations, that it’s very different from those in the sixties and even the nineties,” Rahmandar says.
The way people consume cannabis today increases the amount of the active ingredient, tetrahydrocannabinol (THC), they ingest. Vaping and edibles generally deliver higher quantities than rolling and smoking joints does, Rahmandar says.

Psychological distress a significant problem
One of the lesser-known but troublesome risks of regular cannabis use is substance-abuse psychosis, where a person has delusions or paranoia, hears voices, and otherwise temporarily loses touch with reality. The psychosis generally resolves within a few days, but in some cases requires hospitalization.
This condition can occur with any psychologically altering substances, but the risk from cannabis is higher even than from cocaine, Solmi says.
“You’re more likely to develop substance-abuse psychosis if you use cannabis daily, but I cannot tell you there’s a safe amount that would prevent this,” he says. Young adults and males are the most prone.
Especially worrisome, up to a third of people who experience substance-abuse psychosis go on to develop the more permanent condition of schizophrenia, Solmi says.
( Schizophrenia in women is widely misunderstood—and misdiagnosed )
Observational studies also connect other mental-health conditions to frequent cannabis use. Solmi’s review found that depression increases, as does violence among dating couples. And since cannabis causes cognitive impairment—as well as visual impairment—car accidents have risen among users who drive while under the influence.
Experts especially worry about the mental health impacts for teenagers. Some 17 percent of tenth graders report using cannabis, even though no state has legalized the drug for anyone under 21.
Adolescents are 37 percent more likely to develop depression by young adulthood if they regularly use cannabis compared to non-users. Rates of suicide are also higher.
You May Also Like

Do you really need 10,000 steps a day? Here’s what the science says.

There’s a better way to wake up. Here’s what experts advise.

Melanoma is overdiagnosed at ‘alarming’ rates. Here’s what to know.
“Teenage brains are going through a time of maturity and pruning, so when substances are put in there, they have more of an influence than they do on adult brains,” Rahmandar says.
Cannabis harms the heart
Regular use of cannabis can also lead to significant physical problems.
People who use the drug regularly have a higher risk for heart attack, stroke, and other heart disease , according to a large population-based study published in the Journal of the American Heart Association in February. Heart attack rates rose 25 percent while stroke increased 42 percent in this group, the researchers found.
This likely occurs because THC affects blood flow in the arteries and because receptors for cannabinoids exist throughout the cardiovascular system, the authors state. People who smoke their weed also boost their heart disease risk from the particulate matter they inhale alongside the THC.
Other studies have linked cannabis with improving nausea and vomiting after chemotherapy, but the BMJ review found regular users can actually suffer from an extended vomiting condition known as hyperemesis. “This is rare, but it’s increasing as more people use the drug,” Hasin says.
Pregnant women who use cannabis regularly are more likely to have preterm births and dangerously small babies. More research is needed to determine whether this results from the drug itself or from other lifestyle factors among those who choose to use cannabis while they are pregnant, Solmi says.
Cannabis addiction is a concern
Many people perceive cannabis to be safer than alcohol, but one in five cannabis users develop an addiction to the drug. Symptoms of cannabis use disorder are like those for other substances.
“If people experience cravings, feel they need more and more to get the same effects, they’ve had unsuccessful attempts to quit or cut down,” or have any of several other symptoms “that’s a warning,” Hasin says.
As with alcohol, cannabis addiction can lead to personal, financial, legal, and health problems .
Certain groups are at particularly heightened risk for this addiction. Rates in veterans have increased substantially since 2005, Hasin found in her research. She attributes this to a combination of increased potency and greater acceptance of the drug from its legal status, as well as the likely use of cannabis to self-medicate chronic pain and psychiatric disorders. “The VA has done a good job of reducing unnecessary prescribing of opioids in veterans, so some of them might be turning to cannabis,” she says.
( Is pain relief from cannabis all in your head? )
Young people are also at risk for developing this disorder. Youth who begin using the drug at earlier ages or who have a family history of addiction especially heighten their odds for trouble .
“People younger than 25 should avoid cannabis altogether,” Solmi says. “They have no idea how they will react to cannabis. You’re gambling with your brain and your health.”
For everyone else, moderation is key.
“This isn’t a benign substance that has no risk,” Rahmandar says. “Most users will be fine, but we can’t predict who will develop problems.”
Related Topics
- MENTAL HEALTH

Multiple COVID infections can lead to chronic health issues. Here’s what to know.

No food or medicine can do what olive oil can do. Here's why.

What is white lung syndrome? Here's what to know about pneumonia

Ozempic is a serious drug with serious risks. Here’s what to know.

Ozempic was tested on monkeys IUCN listed as endangered. Here’s what we know
- History & Culture
- Photography
- Environment
- Paid Content
History & Culture
- Mind, Body, Wonder
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
- Search the site GO Please fill out this field.
- Newsletters
- Health Conditions A-Z
- Skin, Hair & Nail Conditions
6 Reasons Your Skin Is Dry
:max_bytes(150000):strip_icc():format(webp)/LauraSchober-LauraSchober-966c4fa3c0004a67b4fa525878316f7d.jpg)
Catherine McQueen / Getty Images
Xeroderma, also known as dry skin, is a common condition resulting from a lack of moisture in the skin that causes flaky, scaly, or itchy patches on the face or body. When external or internal factors weaken the protective function of the outermost layer of the skin, called the skin barrier, excessive water loss occurs. This moisture loss causes dry skin.
Dry skin is something many people experience at some point in their lives. It also becomes more common as people age, as the skin gradually starts to lose sweat and oil glands.
You can care for dry skin by using moisturizers and other self-care measures to restore hydration and moisture to the skin barrier.
Dry Skin Symptoms
Dry skin can feel rough, tight, or itchy, with the appearance of visible flaky or scaly patches on the areas of dry skin. Skin may also appear cracked in some areas.
Dry skin can present anywhere on the body or face, but it tends to occur more frequently in areas with fewer oil glands, such as the elbows, lower legs, hands, feet, and lower arms.
When left untreated, dry skin may lead to pruritus , which is severe itching of the skin. Pruritus increases the likelihood of scratching, which can damage the skin and lead to a greater risk of getting skin infections.
Causes of Dry Skin
There are many causes of dry skin. External factors like exposure to harsh weather or irritating cleansers are common triggers for dryness. However, internal factors like aging and some medical conditions can also contribute to dry skin.
Environmental Factors
Exposure to certain outdoor or indoor elements can impact the skin's moisture. For example, the sun, cold weather, dry indoor heating, and low humidity can all dry out the skin and cause it to lose moisture.
Reducing your exposure to these environmental stressors, such as applying a broad-spectrum sunscreen to your skin while outside, will help prevent dry skin.
Over-Cleansing Your Skin
Washing your face and body with harsh cleansers or body washes , or cleansing your skin for too long, can make the skin become dry. Taking hot showers for long periods can also lead to skin dryness. To combat this, limit the amount of time you spend in the shower to under 10 minutes and use gentle, fragrance-free cleansers. After bathing or showering, apply a moisturizer to damp skin, which will help seal in moisture.
As you age, your pores produce less sebum , an oily substance that moisturizes and protects your skin. This decline typically begins around age 40. From your 40s onwards, your sebum levels will continue to drop, leading to drier skin as you get older.
Multiple studies have found that smoking is associated with premature aging of skin. The chemicals in cigarettes have been found to accelerate skin aging, which causes your skin to become drier. Smoking may also lower estrogen levels in females, which could contribute to dry skin.
Inflammatory Skin Conditions
Inflammatory skin conditions are long-lasting dysfunctions of the skin barrier that are triggered by pruritogens, substances that act on sensory nerves in the skin. When the skin is scratched, the body releases pruritogens, which cause dry, itchy skin and other inflammatory symptoms.
One common inflammatory skin condition is atopic dermatitis, also known as eczema. This condition causes dry, itchy, and inflamed skin.
Another common condition is psoriasis . About 80-90% of people with psoriasis have plaque psoriasis. This type is characterized by patches of dry, thick, raised skin (called plaques), which are sometimes covered by a dry, itchy, silvery-white coating called scales .
Medical Conditions and Treatments
Some medical conditions and treatments can cause dry or extremely dry skin. These include:
- Human immunodeficiency virus (HIV)
- Thyroid disease
- Kidney disease
- Statins, medications that help lower cholesterol levels in the blood
- Diuretics, medications that help move fluids out of the body by increasing the production of urine
- Dialysis, a treatment for kidney failure
- Cancer treatments, such as chemotherapy (a treatment that uses drugs to kill cancer cells), targeted therapy (a treatment that targets the proteins that cancer cells need to grow and survive), and radiation treatments (a treatment that applies high doses of radiation that reduce the size of tumors and kill cancer cells)
Treatments for Dry Skin
There are many ways to relieve dry skin . Applying moisturizing products directly to the skin and making changes in your environment can help treat dryness and address the cause of your dry skin.
You can manage symptoms of dry skin at home by following a gentle skincare routine . Use moisturizers for the face and body that contain hydrating ingredients such as ceramides, urea, or lactic acids. In cases of very dry or itchy skin, you might need a prescription moisturizer from a healthcare provider.
Older adults who are more susceptible to dry skin should aim to moisturize their skin twice per day. One Japanese study found that a moisturizer containing sericin (a silk protein) and ceramide NP (an ingredient that improves skin barrier function) was the most effective in improving the appearance of dry skin on the lower leg, among 39 healthy adults over the age of 65.
Making certain changes to your home or work environment can help improve symptoms, too. Regularly using a humidifier in your home will help add moisture to the air and improve your symptoms of dry skin.
If high exposure to sun, cold weather, or water is causing your dry skin, take measures to protect your skin in these conditions. For example, keep your skin covered when outdoors or wear rubber gloves while washing dishes.
If your dry skin is from a medical condition or medication, visit a healthcare provider or board-certified dermatologist (a medical doctor who specializes in treating conditions of the skin, hair, and nails) to discuss treatment options.
How To Prevent Dry Skin
Keeping your skin barrier protected and hydrated can help prevent dry skin. Here are a few ways to maintain your skin health and avoid dryness:
- Apply moisturizer immediately after washing your hands or within five minutes of showering or bathing, and apply to your body and face as needed throughout the day.
- Use gentle, fragrance-free cleansers.
- Use moisturizing lotions, ointments, or creams containing hydrating ingredients such as hyaluronic acid , jojoba oil, glycerin, lactic acid, or shea butter.
- Choose laundry detergents labeled as hypoallergenic. It may also be helpful to avoid wearing wool or scratchy clothing, which can irritate dry, itchy skin, and opt for clothes made out of cotton or silk.
- Wear gloves while outside in the winter, while cleaning or gardening, or to protect hands during jobs where they might get wet or cold.
- Avoid smoking.
When To See a Healthcare Provider for Dry Skin
If your dry skin is not improving with self-care practices or changes to your environment, or if your skin becomes very itchy, see a board-certified dermatologist or healthcare provider to discuss other treatment options. At your appointment, the provider may ask you about your family history of medical conditions and allergies, any known triggers for dry skin, and any treatments you have previously tried.
The provider may prescribe a medical-grade moisturizer or take further steps to diagnose and treat any underlying medical conditions. If one of your medications is causing dry skin, a healthcare provider may also be able to recommend alternative options.
A Quick Review
Moisture loss in the skin barrier can result in dry skin, a common condition that can occur anywhere on the face or body. Symptoms of dry skin include rough, tight, or itchy skin. Visible flakes, cracked skin, or scaly patches may also appear on dry skin.
Factors like hygiene habits, age, environmental exposures, and certain medical conditions can all lead to dry skin. You can typically treat and prevent dry skin by moisturizing your face and body regularly. Making lifestyle changes like using a humidifier at home, quitting smoking, and covering your skin in sunny or cold weather can also help.
If self-care efforts to restore moisture to the skin are not effective or if your skin becomes very itchy, visit a dermatologist or healthcare provider to discuss further treatment options.
Gade A, Matin T, Rubenstein R. Xeroderma . In: StatPearls . StatPearls Publishing; 2024.
Moniaga CS, Tominaga M, Takamori K. Mechanisms and management of itch in dry skin . Acta Derm Venereol . 2020;100(2):adv00024. doi:10.2340/00015555-3344
National Institute on Aging. Skin care and aging .
Rodan K, Fields K, Majewski G, Falla T. Skincare bootcamp: The evolving role of skincare . Plast Reconstr Surg Glob Open . 2016;4(12Suppl):e1152. doi:10.1097/GOX.0000000000001152
American Academy of Dermatology Association. Dry skin: Who gets and causes .
American Academy of Dermatology Association. Dermatologists' top tips for relieving dry skin .
Yazdanparast T, Hassanzadeh H, Nasrollahi SA, et al. Cigarettes smoking and skin: A comparison study of the biophysical properties of skin in smokers and non-smokers . Tanaffos . 2019;18(2):163-168.
Smokefree. Health effects .
American Academy of Dermatology Association. What is atopic dermatitis? .
American Academy of Dermatology Association. Psoriasis: Signs and symptoms .
National Cancer Institute. Chemotherapy to treat cancer .
National Cancer Institute. Radiation therapy for cancer .
National Cancer Institute. Targeted therapy .
American Academy of Dermatology Association. Dry skin: Diagnosis and treatment .
Aoki M, Hata N, Yotsuya J. Effectiveness of three types of moisturizers on senile dry skin: A randomized controlled pilot trial . Dermatol Res Pract . 2023;2023:1809109. doi:10.1155/2023/1809109
American Academy of Dermatology Association. What is a dermatologist? .
American Academy of Dermatology Association. Dry skin: Tips for managing .
Related Articles

Is Smoking Weed Bad for Your Heart?
I t’s 2024 and you’re just out here trying to give a damn. Perhaps you’ve considered making the “healthy” swaps that talking-head docs on TV have promised will fix everything: fish instead of red meat , dark chocolate for milk, water for soda. Maybe you’ve even subbed out wine for weed, especially since research shows that drinking alcohol can be really hard on your heart. But, as ever, taking care of yourself isn’t quite as all-or-nothing as “one thing is definitively good for you, and the other is definitively bad for you.” In the case of cannabis, a growing pool of research indicates that weed might spell trouble for your cardiovascular health too. [ Heavy sigh while exhaling a huge cloud of smoke. ]
The move to use cannabis in place of alcohol is a wide-reaching wellness trend, as you probably know from all the hype that surrounded Dry January . Celebrities like John Mayer have reportedly made a permanent switch from alcohol to cannabis too. As Mayer told Rolling Stone , “I put [weed] where drinking used to go, and the quality of life has gone up considerably.” Country music legend Willie Nelson, too, is reportedly “ California sober ,” a term that means a person isn’t using hard drugs or drinking alcohol, but still doin’ the weed. Meanwhile, cannabis-infused beverages have shown up to rival canned cocktails on store shelves, and edibles have expanded beyond gummies and into popcorn, hot sauces, and coffee—meaning there’s a huge array of fun new ways to get stony bologna.
It makes sense that weed is having a moment : Since the mid-2010s, when some states began legalizing cannabis, more people in the US are using it. A 2022 report from the Substance Abuse and Mental Health Services Administration indicates that 22% of people 12 and older have smoked weed in the past year, compared with 8.9% of people in 2016 . Other data showed a dip in booze consumption—2023 saw the lowest number of beer sales in the US since 1999, according to an industry report , and wine consumption fell by about 2% in 2022.
Weed is appealing to many folks for more than just the high right now. If you’re one of them, we’re not here to take that away from you. We just want you to know that using cannabis, even if you’re doing that to cut back on drinking, isn’t without its own set of risks for your heart—which is especially important to be aware of when it is increasingly portrayed as a health-enhancer. Lets light this conversation up.
Cannabis is associated with serious heart complications—including heart attack and stroke.
“Unlike the potential heart risks associated with smoking cigarettes , which are more broadly understood, I think few people are aware of the potential risks of smoking marijuana,” Ersilia M. DeFilippis, MD , a cardiologist at New York-Presbyterian/Columbia University Irving Medical Center, tells SELF. “Many assume that the drug is harmless, given the increasing legalization of marijuana in states across the country. We should also remember that smoking cigarettes is legal, but we all know that’s bad for us.”
The cannabis flower is filled with between 80 and 100 cannabinoids that affect your body in different ways. Two of the best-known cannabinoids are cannabidiol (CBD), which is a non-psychoactive (and commonly name-checked) cannabinoid that’s often touted for therapeutic benefits, and tetrahydrocannabinol (THC), which is the psychoactive compound of the cannabis plant, meaning it’ll get you high.
These different compounds can have different effects on your system. For example, some limited research indicates that CBD can have positive impacts, decreasing anxiety , helping to mitigate pain , and assisting with sleep . When it comes to your heart, the news is less rosy—and that’s because of THC. A large-scale study of 2,000 folks below 50 who had a heart attack found marijuana users to be two times more likely to suffer from cardiac arrest. Building on this research, a separate large-scale Stanford study tried to answer why. “We found that there is really good evidence that marijuana, and specifically THC, is associated with cardiovascular heart attacks and strokes,” Mark Chandy, MD, PhD , a cardiologist and coauthor of the Stanford study, tells SELF.
The authors showed that THC causes inflammation and oxidative stress in the cells lining the blood vessels (endothelial cells), particularly for those who used cannabis more than one time per month. When these kinds of cells are impaired or inflamed, particularly over time, it can result in heart disease, high blood pressure, and hardening of the vessel walls (a.k.a. atherosclerosis). If you think of your system as an intricate set of pipes, atherosclerosis causes clogs, which can result in heart attack and stroke. Following the human results of the trial, the team observed in mice that THC caused atherosclerosis. (It’s worth noting here that the mice study was meant to supplement the trend they observed in humans and it showed similar outcomes.)
“I wish we had better news about THC,” Matthew Springer, PhD, a molecular biologist and senior author of a notable UCSF School of Medicine paper about heart health and cannabis, said when he presented the results at the American Heart Association annual meeting last year. That research, which is referred to as CANDIDE (CANnabis: Does It Damage Endothelium), looked at people who smoke marijuana, people who smoke cigarettes, people who don’t smoke but take edibles, and people who abstain from all those things, and they found that across all forms of THC and tobacco use, the vascular system was impaired, which is believed to be a factor in the occurrence of cardiovascular disease . (Big caveat: Weed is still almost certainly less of a cause of heart-related events than cigarettes, which the Surgeon General has attributed to be the cause of 25% of cardiovascular deaths .)
If you’re wondering whether edibles are a better bet than smoking weed…yes, but they still pose a risk to your heart.
They pay me to tell you the bad news, so, straightforwardly: Maybe a little, but they’re still not great for your heart. Whether you’re smoking, vaping , or eating a gummy (or whatever edible you prefer), you’re still going to experience the harmful effects of cannabis on the heart. When I connected with Dr. Springer, he told me that, while we already knew smoke of any kind, including from marijuana and tobacco, caused vascular impairment, the research he did confirmed in human studies that THC itself seems to cause impaired vascular function too. “The way we interpret all this is that smoke of any sort impairs blood vessel function, and THC also impairs blood vessel function for different reasons” and through a different pathway, he says.
Given this, you could posit that smoking weed is a double whammy of impairment, but that edibles only provide a single avenue to potential heart effects, making them a better but not completely risk-averse option. The jury’s still out, but in Dr. Chandy’s view, “It doesn’t matter what form you’re taking with respect to smoking, vaping, or taking [THC] in orally, there’s data not just from our paper but from other clinical studies showing that it can cause adverse effects [to the heart].”
Here’s how this all stacks up to booze, heart-health-wise.
It’s a bit of a game of apple (martinis) versus orange (kush) here. Alcohol and weed work very differently in your body. The former works to depress the central nervous system , temporarily putting your brain in chill mode while the liver metabolizes it; the latter conversely activates the endocannabinoid receptors in your brain.
However, we can say with certainty that the more of either thing you use, the more potential for cardiological trouble it comes with. Correlations between increased amounts of either substance are associated with higher risks for your heart. “There is definitely a dose-dependent response,” Dr. Chandy says. In the past few years, leading health organizations have come out against any alcohol use. The World Heart Federation says that for each 100 grams of alcohol per week that you drink ( around 12.5 units or six-ish glasses of wine), you raise your risk of stroke by 14%, heart failure by 9%, and coronary disease by 6%.
At the end of the day (perhaps the kind where you really need a drink?), we’re talking about correlation, not causality. That means that the more you drink or consume THC, the higher the chance either of those things might affect your heart; however, just because you occasionally drink or pop an edible does not definitively mean you’ll absolutely have heart-related issues. Cheers to that?
What about if you only use weed occasionally—that’s probably better, right?
Yeah, it seems like it. According to Dr. Chandy, “[The harm] does seem to be correlated with the amount that’s used.” His team looked at folks who smoked three to five times a week and saw more inflammatory markers or signals that people were likely to have a heart attack when they took THC, and because of this they believe the potential damage will depend on how often you use it and how potent it is.
That last bit is significant because, as Dr. Chandy says, “In the ’60s and ’70s, the concentration was no more than 3% , and now you can vape 85% pure THC .”
Dr. DeFilippis says that because recreational marijuana products aren’t regulated, they “vary considerably in dose, concentration, and labeling.” Theoretically, lower concentrations of THC in edibles should result in a lower risk of cardiac or vascular issues (though you won’t dodge them altogether). If you’re buying edibles in a state that legally sells them, take note of what the percentage or gram dosage of THC is—it should be on the packaging . On edibles, you’ll see the percentage of THC per serving (in grams) and in the entire container, which allows you to monitor your consumption. In pens or other inhalable options, you’ll find just the percentage of THC that you’ll consume. Again, for your heart, the lower the percentage of THC here, the better.
Here’s the bottom line about what we know about cannabis and heart health so far.
It’s honestly kind of TBD on CBD—but that’s where things look most promising in terms of getting stoned for wellness reasons. CBD seems to have some support for lowering blood pressure through a process called vasorelaxation , which has been shown to help relax the arteries of rats , but the jury’s still out since rodents are not, you know, people. Another smaller study seemed to indicate that medical cannabis lowered systolic and diastolic blood pressure in older adults.
In all, we just need more isolated studies for this stuff to be able to say with any authority or assurance—and those are hard to make happen in reality. That’s because marijuana is classified as a Schedule I drug , meaning that there’s a ton of red tape in place in terms of clinically studying it. “When it comes to research, it’s actually very difficult to study, because you have to have special licenses from the DEA , but it definitely merits a lot of investigation,” Dr. Chandy says.
For now, though, it seems like it’s probably best not to use marijuana if you’re hoping to protect your heart health. “As results have accumulated in the last several years, more and more studies are indicating that using cannabis, including smoking it, increases cardiovascular risk, such as the increased occurrence of heart attacks ,” Dr. Springer says.
Unfortunately, while it would be amazing if we could just get high as hell all the time without worry, cannabis isn’t the wellness miracle drug some companies make it out to be, as far as your cardiological health is concerned. Even if you don’t see yourself totally cutting out weed, it’s good to know the facts and potentially adjust your intake accordingly. And, while we know it’s not quite the same, there are plenty of other ways to de-stress that won’t also mess with your heart.
- A Black Cardiologist Shares the #1 Thing She Does to Prevent Heart Disease
- How Cutting Corners on Dental Hygiene Can Mess With Your Heart
- What Are Antioxidants and How Much of Them Should You Be Eating?


Lawsuit seeks to force ban on menthol…
Share this:.
- Click to share on Facebook (Opens in new window)
- Click to share on X (Opens in new window)
Daily e-Edition
Evening e-Edition
- Entertainment
- Restaurants, Food & Drink
Lawsuit seeks to force ban on menthol cigarettes after months of delays by Biden administration

By MATTHEW PERRONE (AP Health Writer)
WASHINGTON (AP) — Anti-smoking groups sued the U.S. government Tuesday over a long-awaited ban on menthol cigarettes, which has been idling at the White House for months.
The lawsuit is the latest effort to force the government to ban menthols, which are disproportionately used by Black smokers and young people. It comes amid growing concerns from advocates that the federal plan could be derailed by election-year politics.
Health officials under President Joe Biden initially targeted last August to publish the rule eliminating the minty flavor. Late last year, White House officials said they would take until March to review the rule. Three nonprofit groups, including Action on Smoking and Health, filed their lawsuit in a federal court in California after the March deadline passed.
“Because of defendants’ inaction, tobacco companies have continued to use menthol cigarettes to target youth, women, and the Black community — all to the detriment of public health,” the groups state in their complaint.
A spokesperson for the White House declined to comment on the lawsuit Tuesday.
The Food and Drug Administration has spent years developing the plan to eliminate menthol, estimating it could prevent 300,000 to 650,000 smoking deaths over several decades. Most of those preventable deaths would be among Black Americans.
Like all major federal regulations, the plan must get final approval from the White House.
Previous FDA efforts on menthol have been scuttled by tobacco industry pushback or competing political priorities across several administrations. The latest delay comes as Democrats voice worries about Biden’s prospects in a rematch against former President Donald Trump.
White House officials have held dozens of meetings with groups opposing the menthol ban, including civil rights advocates, business owners and law enforcement officials. Some suggested a rule targeting menthols could suppress Biden’s turnout among Black voters. In almost all cases, groups opposing the ban receive financial support from tobacco companies.
In recent months, supporters of the plan have tried to assure the White House that banning menthol will not hurt Biden’s re-election chances.
“If Black lives truly matter, then we must end the sale of menthol cigarettes and do it now,” said Dr. Carol McGruder, of the African American Tobacco Control Leadership, in a statement. McGruder’s group is among those suing the FDA and its parent agency, the Department of Health and Human Services.
A lawyer who helped file the lawsuit said the government will have about two months to respond.
A 2020 lawsuit by the same groups jump-started FDA’s work on menthol, alleging that the agency had “unreasonably delayed” action against the flavor.
Menthol is the only cigarette flavor that was not banned under the 2009 law that gave the FDA authority over tobacco products, an exemption negotiated by industry lobbyists. The act did, though, instruct the agency to continue to weigh whether to ban menthol.
The flavor’s persistence has infuriated anti-smoking advocates, who point to research that menthol’s numbing effect masks the harshness of smoking, making it easier to start and harder to quit.
More than 11% of U.S. adults smoke, with rates roughly even between white and Black populations. About 80% of Black smokers — and most teenagers who smoke — use menthol.
Associated Press writer Zeke Miller contributed to this story
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.
More in News

National Politics | Judge rejects Donald Trump’s request to delay hush-money trial until Supreme Court rules on immunity

SUBSCRIBER ONLY
Transportation | govenor, dot tout coming $2.5 billion overhaul of congested i-4 west of orlando.

Education | Eatonville, OCPS seek deal on slice of Hungerford property to help museum pitch

World News | US braces for retaliation after attack on Iran consulate — even as it says it wasn’t involved
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Office on Smoking and Health (US). The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2006.

The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General.
1 introduction, summary, and conclusions.
- Introduction
The topic of passive or involuntary smoking was first addressed in the 1972 U.S. Surgeon General’s report ( The Health Consequences of Smoking , U.S. Department of Health, Education, and Welfare [USDHEW] 1972 ), only eight years after the first Surgeon General’s report on the health consequences of active smoking ( USDHEW 1964 ). Surgeon General Dr. Jesse Steinfeld had raised concerns about this topic, leading to its inclusion in that report. According to the 1972 report, nonsmokers inhale the mixture of sidestream smoke given off by a smoldering cigarette and mainstream smoke exhaled by a smoker, a mixture now referred to as “secondhand smoke” or “environmental tobacco smoke.” Cited experimental studies showed that smoking in enclosed spaces could lead to high levels of cigarette smoke components in the air. For carbon monoxide ( CO ) specifically, levels in enclosed spaces could exceed levels then permitted in outdoor air. The studies supported a conclusion that “an atmosphere contaminated with tobacco smoke can contribute to the discomfort of many individuals” ( USDHEW 1972 , p. 7). The possibility that CO emitted from cigarettes could harm persons with chronic heart or lung disease was also mentioned.
Secondhand tobacco smoke was then addressed in greater depth in Chapter 4 (Involuntary Smoking) of the 1975 Surgeon General’s report, The Health Consequences of Smoking ( USDHEW 1975 ). The chapter noted that involuntary smoking takes place when nonsmokers inhale both sidestream and exhaled mainstream smoke and that this “smoking” is “involuntary” when “the exposure occurs as an unavoidable consequence of breathing in a smoke-filled environment” (p. 87). The report covered exposures and potential health consequences of involuntary smoking, and the researchers concluded that smoking on buses and airplanes was annoying to nonsmokers and that involuntary smoking had potentially adverse consequences for persons with heart and lung diseases. Two studies on nicotine concentrations in nonsmokers raised concerns about nicotine as a contributing factor to atherosclerotic cardiovascular disease in nonsmokers.
The 1979 Surgeon General’s report, Smoking and Health: A Report of the Surgeon General ( USDHEW 1979 ), also contained a chapter entitled “Involuntary Smoking.” The chapter stressed that “attention to involuntary smoking is of recent vintage, and only limited information regarding the health effects of such exposure upon the nonsmoker is available” (p. 11–35). The chapter concluded with recommendations for research including epidemiologic and clinical studies. The 1982 Surgeon General’s report specifically addressed smoking and cancer ( U.S. Department of Health and Human Services [USDHHS] 1982 ). By 1982, there were three published epidemiologic studies on involuntary smoking and lung cancer, and the 1982 Surgeon General’s report included a brief chapter on this topic. That chapter commented on the methodologic difficulties inherent in such studies, including exposure assessment, the lengthy interval during which exposures are likely to be relevant, and accounting for exposures to other carcinogens. Nonetheless, the report concluded that “Although the currently available evidence is not sufficient to conclude that passive or involuntary smoking causes lung cancer in nonsmokers, the evidence does raise concern about a possible serious public health problem” (p. 251).
Involuntary smoking was also reviewed in the 1984 report, which focused on chronic obstructive pulmonary disease and smoking ( USDHHS 1984 ). Chapter 7 (Passive Smoking) of that report included a comprehensive review of the mounting information on smoking by parents and the effects on respiratory health of their children, data on irritation of the eye, and the more limited evidence on pulmonary effects of involuntary smoking on adults. The chapter began with a compilation of measurements of tobacco smoke components in various indoor environments. The extent of the data had increased substantially since 1972. By 1984, the data included measurements of more specific indicators such as acrolein and nicotine, and less specific indicators such as particulate matter ( PM ), nitrogen oxides, and CO . The report reviewed new evidence on exposures of nonsmokers using bio-markers, with substantial information on levels of cotinine, a major nicotine metabolite. The report anticipated future conclusions with regard to respiratory effects of parental smoking on child respiratory health ( Table 1.1 ).
Conclusions from previous Surgeon General’s reports on the health effects of secondhand smoke exposure
Involuntary smoking was the topic for the entire 1986 Surgeon General’s report, The Health Consequences of Involuntary Smoking ( USDHHS 1986 ). In its 359 pages, the report covered the full breadth of the topic, addressing toxicology and dosimetry of tobacco smoke; the relevant evidence on active smoking; patterns of exposure of nonsmokers to tobacco smoke; the epidemiologic evidence on involuntary smoking and disease risks for infants, children, and adults; and policies to control involuntary exposure to tobacco smoke. That report concluded that involuntary smoking caused lung cancer in lifetime nonsmoking adults and was associated with adverse effects on respiratory health in children. The report also stated that simply separating smokers and nonsmokers within the same airspace reduced but did not eliminate exposure to secondhand smoke. All of these findings are relevant to public health and public policy ( Table 1.1 ). The lung cancer conclusion was based on extensive information already available on the carcinogenicity of active smoking, the qualitative similarities between secondhand and mainstream smoke, the uptake of tobacco smoke components by nonsmokers, and the epidemiologic data on involuntary smoking. The three major conclusions of the report ( Table 1.2 ), led Dr. C. Everett Koop, Surgeon General at the time, to comment in his preface that “the right of smokers to smoke ends where their behavior affects the health and well-being of others; furthermore, it is the smokers’ responsibility to ensure that they do not expose nonsmokers to the potential [ sic ] harmful effects of tobacco smoke” ( USDHHS 1986 , p. xii).
Major conclusions of the 1986 Surgeon General’s report, The Health Consequences of Involuntary Smoking
Two other reports published in 1986 also reached the conclusion that involuntary smoking increased the risk for lung cancer. The International Agency for Research on Cancer ( IARC ) of the World Health Organization concluded that “passive smoking gives rise to some risk of cancer” ( IARC 1986 , p. 314). In its monograph on tobacco smoking, the agency supported this conclusion on the basis of the characteristics of sidestream and mainstream smoke, the absorption of tobacco smoke materials during an involuntary exposure, and the nature of dose-response relationships for carcinogenesis. In the same year, the National Research Council ( NRC ) also concluded that involuntary smoking increases the incidence of lung cancer in nonsmokers ( NRC 1986 ). In reaching this conclusion, the NRC report cited the biologic plausibility of the association between exposure to secondhand smoke and lung cancer and the supporting epidemiologic evidence. On the basis of a pooled analysis of the epidemiologic data adjusted for bias, the report concluded that the best estimate for the excess risk of lung cancer in nonsmokers married to smokers was 25 percent, compared with nonsmokers married to nonsmokers. With regard to the effects of involuntary smoking on children, the NRC report commented on the literature linking secondhand smoke exposures from parental smoking to increased risks for respiratory symptoms and infections and to a slightly diminished rate of lung growth.
Since 1986, the conclusions with regard to both the carcinogenicity of secondhand smoke and the adverse effects of parental smoking on the health of children have been echoed and expanded ( Table 1.3 ). In 1992, the U.S. Environmental Protection Agency ( EPA ) published its risk assessment of secondhand smoke as a carcinogen ( USEPA 1992 ). The agency’s evaluation drew on toxicologic information on secondhand smoke and the extensive literature on active smoking. A comprehensive meta-analysis of the 31 epidemiologic studies of secondhand smoke and lung cancer published up to that time was central to the decision to classify secondhand smoke as a group A carcinogen—namely, a known human carcinogen. Estimates of approximately 3,000 U.S. lung cancer deaths per year in non-smokers were attributed to secondhand smoke. The report also covered other respiratory health effects in children and adults and concluded that involuntary smoking is causally associated with several adverse respiratory effects in children. There was also a quantitative risk assessment for the impact of involuntary smoking on childhood asthma and lower respiratory tract infections in young children.
Selected major reports, other than those of the U.S. Surgeon General, addressing adverse effects from exposure to tobacco smoke
In the decade since the 1992 EPA report, scientific panels continued to evaluate the mounting evidence linking involuntary smoking to adverse health effects ( Table 1.3 ). The most recent was the 2005 report of the California EPA ( Cal/EPA 2005 ). Over time, research has repeatedly affirmed the conclusions of the 1986 Surgeon General’s reports and studies have further identified causal associations of involuntary smoking with diseases and other health disorders. The epidemiologic evidence on involuntary smoking has markedly expanded since 1986, as have the data on exposure to tobacco smoke in the many environments where people spend time. An understanding of the mechanisms by which involuntary smoking causes disease has also deepened.
As part of the environmental health hazard assessment, Cal/EPA identified specific health effects causally associated with exposure to secondhand smoke. The agency estimated the annual excess deaths in the United States that are attributable to secondhand smoke exposure for specific disorders: sudden infant death syndrome ( SIDS ), cardiac-related illnesses (ischemic heart disease), and lung cancer ( Cal/EPA 2005 ). For the excess incidence of other health outcomes, either new estimates were provided or estimates from the 1997 health hazard assessment were used without any revisions ( Cal/EPA 1997 ). Overall, Cal/EPA estimated that about 50,000 excess deaths result annually from exposure to secondhand smoke ( Cal/EPA 2005 ). Estimated annual excess deaths for the total U.S. population are about 3,400 (a range of 3,423 to 8,866) from lung cancer, 46,000 (a range of 22,700 to 69,600) from cardiac-related illnesses, and 430 from SIDS. The agency also estimated that between 24,300 and 71,900 low birth weight or pre-term deliveries, about 202,300 episodes of childhood asthma (new cases and exacerbations), between 150,000 and 300,000 cases of lower respiratory illness in children, and about 789,700 cases of middle ear infections in children occur each year in the United States as a result of exposure to secondhand smoke.
This new 2006 Surgeon General’s report returns to the topic of involuntary smoking. The health effects of involuntary smoking have not received comprehensive coverage in this series of reports since 1986. Reports since then have touched on selected aspects of the topic: the 1994 report on tobacco use among young people ( USDHHS 1994 ), the 1998 report on tobacco use among U.S. racial and ethnic minorities ( USDHHS 1998 ), and the 2001 report on women and smoking ( USDHHS 2001 ). As involuntary smoking remains widespread in the United States and elsewhere, the preparation of this report was motivated by the persistence of involuntary smoking as a public health problem and the need to evaluate the substantial new evidence reported since 1986. This report substantially expands the list of topics that were included in the 1986 report. Additional topics include SIDS , developmental effects, and other reproductive effects; heart disease in adults; and cancer sites beyond the lung. For some associations of involuntary smoking with adverse health effects, only a few studies were reviewed in 1986 (e. g ., ear disease in children); now, the relevant literature is substantial. Consequently, this report uses meta-analysis to quantitatively summarize evidence as appropriate. Following the approach used in the 2004 report ( The Health Consequences of Smoking , USDHHS 2004 ), this 2006 report also systematically evaluates the evidence for causality, judging the extent of the evidence available and then making an inference as to the nature of the association.
Organization of the Report
This twenty-ninth report of the Surgeon General examines the topics of toxicology of secondhand smoke, assessment and prevalence of exposure to secondhand smoke, reproductive and developmental health effects, respiratory effects of exposure to secondhand smoke in children and adults, cancer among adults, cardiovascular diseases, and the control of secondhand smoke exposure.
This introductory chapter (Chapter 1) includes a discussion of the concept of causation and introduces concepts of causality that are used throughout this report; this chapter also summarizes the major conclusions of the report. Chapter 2 (Toxicology of Secondhand Smoke) sets out a foundation for interpreting the observational evidence that is the focus of most of the following chapters. The discussion details the mechanisms that enable tobacco smoke components to injure the respiratory tract and cause nonmalignant and malignant diseases and other adverse effects. Chapter 3 (Assessment of Exposure to Secondhand Smoke) provides a perspective on key factors that determine exposures of people to secondhand smoke in indoor environments, including building designs and operations, atmospheric markers of secondhand smoke, exposure models, and biomarkers of exposure to secondhand smoke. Chapter 4 (Prevalence of Exposure to Secondhand Smoke) summarizes findings that focus on nicotine measurements in the air and cotinine measurements in biologic materials. The chapter includes exposures in the home, workplace, public places, and special populations. Chapter 5 (Reproductive and Developmental Effects from Exposure to Secondhand Smoke) reviews the health effects on reproduction, on infants, and on child development. Chapter 6 (Respiratory Effects in Children from Exposure to Secondhand Smoke) examines the effects of parental smoking on the respiratory health of children. Chapter 7 (Cancer Among Adults from Exposure to Secondhand Smoke) summarizes the evidence on cancer of the lung, breast, nasal sinuses, and the cervix. Chapter 8 (Cardiovascular Diseases from Exposure to Secondhand Smoke) discusses coronary heart disease ( CHD ), stroke, and subclinical vascular disease. Chapter 9 (Respiratory Effects in Adults from Exposure to Secondhand Smoke) examines odor and irritation, respiratory symptoms, lung function, and respiratory diseases such as asthma and chronic obstructive pulmonary disease. Chapter 10 (Control of Secondhand Smoke Exposure) considers measures used to control exposure to secondhand smoke in public places, including legislation, education, and approaches based on building designs and operations. The report concludes with “A Vision for the Future.” Major conclusions of the report were distilled from the chapter conclusions and appear later in this chapter.
Preparation of the Report
This report of the Surgeon General was prepared by the Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, Coordinating Center for Health Promotion, Centers for Disease Control and Prevention ( CDC ), and U.S. DHHS. Initial chapters were written by 22 experts who were selected because of their knowledge of a particular topic. The contributions of the initial experts were consolidated into 10 major chapters that were then reviewed by more than 40 peer reviewers. The entire manuscript was then sent to more than 30 scientists and experts who reviewed it for its scientific integrity. After each review cycle, the drafts were revised by the scientific editors on the basis of the experts’ comments. Subsequently, the report was reviewed by various institutes and agencies within U.S. DHHS. Publication lags, even short ones, prevent an up-to-the-minute inclusion of all recently published articles and data. Therefore, by the time the public reads this report, there may be additional published studies or data. To provide published information as current as possible, this report includes an Appendix of more recent studies that represent major additions to the literature.
This report is also accompanied by a companion database of key evidence that is accessible through the Internet ( http://www.cdc.gov/tobacco ). The database includes a uniform description of the studies and results on the health effects of exposure to secondhand smoke that were presented in a format compatible with abstraction into standardized tables. Readers of the report may access these data for additional analyses, tables, or figures.
- Definitions and Terminology
The inhalation of tobacco smoke by nonsmokers has been variably referred to as “passive smoking” or “involuntary smoking.” Smokers, of course, also inhale secondhand smoke. Cigarette smoke contains both particles and gases generated by the combustion at high temperatures of tobacco, paper, and additives. The smoke inhaled by nonsmokers that contaminates indoor spaces and outdoor environments has often been referred to as “secondhand smoke” or “environmental tobacco smoke.” This inhaled smoke is the mixture of sidestream smoke released by the smoldering cigarette and the mainstream smoke that is exhaled by a smoker. Sidestream smoke, generated at lower temperatures and under somewhat different combustion conditions than mainstream smoke, tends to have higher concentrations of many of the toxins found in cigarette smoke ( USDHHS 1986 ). However, it is rapidly diluted as it travels away from the burning cigarette.
Secondhand smoke is an inherently dynamic mixture that changes in characteristics and concentration with the time since it was formed and the distance it has traveled. The smoke particles change in size and composition as gaseous components are volatilized and moisture content changes; gaseous elements of secondhand smoke may be adsorbed onto materials, and particle concentrations drop with both dilution in the air or environment and impaction on surfaces, including the lungs or on the body. Because of its dynamic nature, a specific quantitative definition of secondhand smoke cannot be offered.
This report uses the term secondhand smoke in preference to environmental tobacco smoke, even though the latter may have been used more frequently in previous reports. The descriptor “secondhand” captures the involuntary nature of the exposure, while “environmental” does not. This report also refers to the inhalation of secondhand smoke as involuntary smoking, acknowledging that most nonsmokers do not want to inhale tobacco smoke. The exposure of the fetus to tobacco smoke, whether from active smoking by the mother or from her exposure to secondhand smoke, also constitutes involuntary smoking.
- Evidence Evaluation
Following the model of the 1964 report, the Surgeon General’s reports on smoking have included comprehensive compilations of the evidence on the health effects of smoking. The evidence is analyzed to identify causal associations between smoking and disease according to enunciated principles, sometimes referred to as the “Surgeon General’s criteria” or the “Hill” criteria (after Sir Austin Bradford Hill) for causality ( USDHEW 1964 ; USDHHS 2004 ). Application of these criteria involves covering all relevant observational and experimental evidence. The criteria, offered in a brief chapter of the 1964 report entitled “Criteria for Judgment,” included (1) the consistency of the association, (2) the strength of the association, (3) the specificity of the association, (4) the temporal relationship of the association, and (5) the coherence of the association. Although these criteria have been criticized (e. g ., Rothman and Greenland 1998 ), they have proved useful as a framework for interpreting evidence on smoking and other postulated causes of disease, and for judging whether causality can be inferred.
In the 2004 report of the Surgeon General, The Health Consequences of Smoking , the framework for interpreting evidence on smoking and health was revisited in depth for the first time since the 1964 report ( USDHHS 2004 ). The 2004 report provided a four-level hierarchy for interpreting evidence ( Table 1.4 ). The categories acknowledge that evidence can be “suggestive” but not adequate to infer a causal relationship, and also allows for evidence that is “suggestive of no causal relationship.” Since the 2004 report, the individual chapter conclusions have consistently used this four-level hierarchy ( Table 1.4 ), but evidence syntheses and other summary statements may use either the term “increased risk” or “cause” to describe instances in which there is sufficient evidence to conclude that active or involuntary smoking causes a disease or condition. This four-level framework also sharply and completely separates conclusions regarding causality from the implications of such conclusions.
Four-level hierarchy for classifying the strength of causal inferences based on available evidence
That same framework was used in this report on involuntary smoking and health. The criteria dating back to the 1964 Surgeon General’s report remain useful as guidelines for evaluating evidence ( USDHEW 1964 ), but they were not intended to be applied strictly or as a “checklist” that needed to be met before the designation of “causal” could be applied to an association. In fact, for involuntary smoking and health, several of the criteria will not be met for some associations. Specificity, referring to a unique exposure-disease relationship (e. g ., the association between thalidomide use during pregnancy and unusual birth defects), can be set aside as not relevant, as all of the health effects considered in this report have causes other than involuntary smoking. Associations are considered more likely to be causal as the strength of an association increases because competing explanations become less plausible alternatives. However, based on knowledge of dosimetry and mechanisms of injury and disease causation, the risk is anticipated to be only slightly or modestly increased for some associations of involuntary smoking with disease, such as lung cancer, particularly when the very strong relative risks found for active smokers are compared with those for lifetime nonsmokers. The finding of only a small elevation in risk, as in the example of spousal smoking and lung cancer risk in lifetime nonsmokers, does not weigh against a causal association; however, alternative explanations for a risk of a small magnitude need full exploration and cannot be so easily set aside as alternative explanations for a stronger association. Consistency, coherence, and the temporal relationship of involuntary smoking with disease are central to the interpretations in this report. To address coherence, the report draws not only on the evidence for involuntary smoking, but on the even more extensive literature on active smoking and disease.
Although the evidence reviewed in this report comes largely from investigations of secondhand smoke specifically, the larger body of evidence on active smoking is also relevant to many of the associations that were evaluated. The 1986 report found secondhand smoke to be qualitatively similar to mainstream smoke inhaled by the smoker and concluded that secondhand smoke would be expected to have “a toxic and carcinogenic potential that would not be expected to be qualitatively different from that of MS [mainstream smoke]” ( USDHHS 1986 , p. 23). The 2004 report of the Surgeon General revisited the health consequences of active smoking ( USDHHS 2004 ), and the conclusions substantially expanded the list of diseases and conditions caused by smoking. Chapters in the present report consider the evidence on active smoking that is relevant to biologic plausibility for causal associations between involuntary smoking and disease. The reviews included in this report cover evidence identified through search strategies set out in each chapter. Of necessity, the evidence on mechanisms was selectively reviewed. However, an attempt was made to cover all health studies through specified target dates. Because of the substantial amount of time involved in preparing this report, lists of new key references published after these cut-off dates are included in an Appendix . Literature reviews were extended when new evidence was sufficient to possibly change the level of a causal conclusion.
- Major Conclusions
This report returns to involuntary smoking, the topic of the 1986 Surgeon General’s report. Since then, there have been many advances in the research on secondhand smoke, and substantial evidence has been reported over the ensuing 20 years. This report uses the revised language for causal conclusions that was implemented in the 2004 Surgeon General’s report ( USDHHS 2004 ). Each chapter provides a comprehensive review of the evidence, a quantitative synthesis of the evidence if appropriate, and a rigorous assessment of sources of bias that may affect interpretations of the findings. The reviews in this report reaffirm and strengthen the findings of the 1986 report. With regard to the involuntary exposure of nonsmokers to tobacco smoke, the scientific evidence now supports the following major conclusions:
- Secondhand smoke causes premature death and disease in children and in adults who do not smoke.
- Children exposed to secondhand smoke are at an increased risk for sudden infant death syndrome ( SIDS ), acute respiratory infections, ear problems, and more severe asthma. Smoking by parents causes respiratory symptoms and slows lung growth in their children.
- Exposure of adults to secondhand smoke has immediate adverse effects on the cardiovascular system and causes coronary heart disease and lung cancer.
- The scientific evidence indicates that there is no risk-free level of exposure to secondhand smoke.
- Many millions of Americans, both children and adults, are still exposed to secondhand smoke in their homes and workplaces despite substantial progress in tobacco control.
- Eliminating smoking in indoor spaces fully protects nonsmokers from exposure to secondhand smoke. Separating smokers from nonsmokers, cleaning the air, and ventilating buildings cannot eliminate exposures of nonsmokers to secondhand smoke.
- Chapter Conclusions
Chapter 2 Toxicology of Secondhand Smoke
Evidence of carcinogenic effects from secondhand smoke exposure.
- 1. More than 50 carcinogens have been identified in sidestream and secondhand smoke.
- 2. The evidence is sufficient to infer a causal relationship between exposure to secondhand smoke and its condensates and tumors in laboratory animals.
- 3. The evidence is sufficient to infer that exposure of nonsmokers to secondhand smoke causes a significant increase in urinary levels of metabolites of the tobacco-specific lung carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone ( NNK ). The presence of these metabolites links exposure to secondhand smoke with an increased risk for lung cancer.
- 4. The mechanisms by which secondhand smoke causes lung cancer are probably similar to those observed in smokers. The overall risk of secondhand smoke exposure, compared with active smoking, is diminished by a substantially lower carcinogenic dose.
Mechanisms of Respiratory Tract Injury and Disease Caused by Secondhand Smoke Exposure
- 5. The evidence indicates multiple mechanisms by which secondhand smoke exposure causes injury to the respiratory tract.
- 6. The evidence indicates mechanisms by which secondhand smoke exposure could increase the risk for sudden infant death syndrome.
Mechanisms of Secondhand Smoke Exposure and Heart Disease
- 7. The evidence is sufficient to infer that exposure to secondhand smoke has a prothrombotic effect.
- 8. The evidence is sufficient to infer that exposure to secondhand smoke causes endothelial cell dysfunctions.
- 9. The evidence is sufficient to infer that exposure to secondhand smoke causes atherosclerosis in animal models.
Chapter 3. Assessment of Exposure to Secondhand Smoke
Building designs and operations.
- 1. Current heating, ventilating, and air conditioning systems alone cannot control exposure to secondhand smoke.
- 2. The operation of a heating, ventilating, and air conditioning system can distribute secondhand smoke throughout a building.
Exposure Models
- 3. Atmospheric concentration of nicotine is a sensitive and specific indicator for secondhand smoke.
- 4. Smoking increases indoor particle concentrations.
- 5. Models can be used to estimate concentrations of secondhand smoke.
Biomarkers of Exposure to Secondhand Smoke
- 6. Biomarkers suitable for assessing recent exposures to secondhand smoke are available.
- 7. At this time, cotinine, the primary proximate metabolite of nicotine, remains the biomarker of choice for assessing secondhand smoke exposure.
- 8. Individual biomarkers of exposure to secondhand smoke represent only one component of a complex mixture, and measurements of one marker may not wholly reflect an exposure to other components of concern as a result of involuntary smoking.
Chapter 4. Prevalence of Exposure to Secondhand Smoke
- The evidence is sufficient to infer that large numbers of nonsmokers are still exposed to secondhand smoke.
- Exposure of nonsmokers to secondhand smoke has declined in the United States since the 1986 Surgeon General’s report, The Health Consequences of Involuntary Smoking .
- The evidence indicates that the extent of secondhand smoke exposure varies across the country.
- Homes and workplaces are the predominant locations for exposure to secondhand smoke.
- Exposure to secondhand smoke tends to be greater for persons with lower incomes.
- Exposure to secondhand smoke continues in restaurants, bars, casinos, gaming halls, and vehicles.
Chapter 5. Reproductive and Developmental Effects from Exposure to Secondhand Smoke
- 1. The evidence is inadequate to infer the presence or absence of a causal relationship between maternal exposure to secondhand smoke and female fertility or fecundability. No data were found on paternal exposure to secondhand smoke and male fertility or fecundability.
Pregnancy (Spontaneous Abortion and Perinatal Death)
- 2. The evidence is inadequate to infer the presence or absence of a causal relationship between maternal exposure to secondhand smoke during pregnancy and spontaneous abortion.
Infant Deaths
- 3. The evidence is inadequate to infer the presence or absence of a causal relationship between exposure to secondhand smoke and neonatal mortality.
Sudden Infant Death Syndrome
- 4. The evidence is sufficient to infer a causal relationship between exposure to secondhand smoke and sudden infant death syndrome.
Preterm Delivery
- 5. The evidence is suggestive but not sufficient to infer a causal relationship between maternal exposure to secondhand smoke during pregnancy and preterm delivery.
Low Birth Weight
- 6. The evidence is sufficient to infer a causal relationship between maternal exposure to secondhand smoke during pregnancy and a small reduction in birth weight.
Congenital Malformations
- 7. The evidence is inadequate to infer the presence or absence of a causal relationship between exposure to secondhand smoke and congenital malformations.
Cognitive Development
- 8. The evidence is inadequate to infer the presence or absence of a causal relationship between exposure to secondhand smoke and cognitive functioning among children.
Behavioral Development
- 9. The evidence is inadequate to infer the presence or absence of a causal relationship between exposure to secondhand smoke and behavioral problems among children.
Height/Growth
- 10. The evidence is inadequate to infer the presence or absence of a causal relationship between exposure to secondhand smoke and children’s height/growth.
Childhood Cancer
- 11. The evidence is suggestive but not sufficient to infer a causal relationship between prenatal and postnatal exposure to secondhand smoke and childhood cancer.
- 12. The evidence is inadequate to infer the presence or absence of a causal relationship between maternal exposure to secondhand smoke during pregnancy and childhood cancer.
- 13. The evidence is inadequate to infer the presence or absence of a causal relationship between exposure to secondhand smoke during infancy and childhood cancer.
- 14. The evidence is suggestive but not sufficient to infer a causal relationship between prenatal and postnatal exposure to secondhand smoke and childhood leukemias.
- 15. The evidence is suggestive but not sufficient to infer a causal relationship between prenatal and postnatal exposure to secondhand smoke and childhood lymphomas.
- 16. The evidence is suggestive but not sufficient to infer a causal relationship between prenatal and postnatal exposure to secondhand smoke and childhood brain tumors.
- 17. The evidence is inadequate to infer the presence or absence of a causal relationship between prenatal and postnatal exposure to secondhand smoke and other childhood cancer types.
Chapter 6. Respiratory Effects in Children from Exposure to Secondhand Smoke
Lower respiratory illnesses in infancy and early childhood.
- 1. The evidence is sufficient to infer a causal relationship between secondhand smoke exposure from parental smoking and lower respiratory illnesses in infants and children.
- 2. The increased risk for lower respiratory illnesses is greatest from smoking by the mother.
Middle Ear Disease and Adenotonsillectomy
- 3. The evidence is sufficient to infer a causal relationship between parental smoking and middle ear disease in children, including acute and recurrent otitis media and chronic middle ear effusion.
- 4. The evidence is suggestive but not sufficient to infer a causal relationship between parental smoking and the natural history of middle ear effusion.
- 5. The evidence is inadequate to infer the presence or absence of a causal relationship between parental smoking and an increase in the risk of adenoidectomy or tonsillectomy among children.
Respiratory Symptoms and Prevalent Asthma in School-Age Children
- 6. The evidence is sufficient to infer a causal relationship between parental smoking and cough, phlegm, wheeze, and breathlessness among children of school age.
- 7. The evidence is sufficient to infer a causal relationship between parental smoking and ever having asthma among children of school age.
Childhood Asthma Onset
- 8. The evidence is sufficient to infer a causal relationship between secondhand smoke exposure from parental smoking and the onset of wheeze illnesses in early childhood.
- 9. The evidence is suggestive but not sufficient to infer a causal relationship between secondhand smoke exposure from parental smoking and the onset of childhood asthma.
- 10. The evidence is inadequate to infer the presence or absence of a causal relationship between parental smoking and the risk of immunoglobulin E-mediated allergy in their children.
Lung Growth and Pulmonary Function
- 11. The evidence is sufficient to infer a causal relationship between maternal smoking during pregnancy and persistent adverse effects on lung function across childhood.
- 12. The evidence is sufficient to infer a causal relationship between exposure to secondhand smoke after birth and a lower level of lung function during childhood.
Chapter 7. Cancer Among Adults from Exposure to Secondhand Smoke
Lung cancer.
- 1. The evidence is sufficient to infer a causal relationship between secondhand smoke exposure and lung cancer among lifetime nonsmokers. This conclusion extends to all secondhand smoke exposure, regardless of location.
- 2. The pooled evidence indicates a 20 to 30 percent increase in the risk of lung cancer from secondhand smoke exposure associated with living with a smoker.
Breast Cancer
- 3. The evidence is suggestive but not sufficient to infer a causal relationship between secondhand smoke and breast cancer.
Nasal Sinus Cavity and Nasopharyngeal Carcinoma
- 4. The evidence is suggestive but not sufficient to infer a causal relationship between secondhand smoke exposure and a risk of nasal sinus cancer among nonsmokers.
- 5. The evidence is inadequate to infer the presence or absence of a causal relationship between secondhand smoke exposure and a risk of nasopharyngeal carcinoma among nonsmokers.
Cervical Cancer
- 6. The evidence is inadequate to infer the presence or absence of a causal relationship between secondhand smoke exposure and the risk of cervical cancer among lifetime nonsmokers.
Chapter 8. Cardiovascular Diseases from Exposure to Secondhand Smoke
- The evidence is sufficient to infer a causal relationship between exposure to secondhand smoke and increased risks of coronary heart disease morbidity and mortality among both men and women.
- Pooled relative risks from meta-analyses indicate a 25 to 30 percent increase in the risk of coronary heart disease from exposure to secondhand smoke.
- The evidence is suggestive but not sufficient to infer a causal relationship between exposure to secondhand smoke and an increased risk of stroke.
- Studies of secondhand smoke and subclinical vascular disease, particularly carotid arterial wall thickening, are suggestive but not sufficient to infer a causal relationship between exposure to secondhand smoke and atherosclerosis.
Chapter 9. Respiratory Effects in Adults from Exposure to Secondhand Smoke
Odor and irritation.
- 1. The evidence is sufficient to infer a causal relationship between secondhand smoke exposure and odor annoyance.
- 2. The evidence is sufficient to infer a causal relationship between secondhand smoke exposure and nasal irritation.
- 3. The evidence is suggestive but not sufficient to conclude that persons with nasal allergies or a history of respiratory illnesses are more susceptible to developing nasal irritation from secondhand smoke exposure.
Respiratory Symptoms
- 4. The evidence is suggestive but not sufficient to infer a causal relationship between secondhand smoke exposure and acute respiratory symptoms including cough, wheeze, chest tightness, and difficulty breathing among persons with asthma.
- 5. The evidence is suggestive but not sufficient to infer a causal relationship between secondhand smoke exposure and acute respiratory symptoms including cough, wheeze, chest tightness, and difficulty breathing among healthy persons.
- 6. The evidence is suggestive but not sufficient to infer a causal relationship between secondhand smoke exposure and chronic respiratory symptoms.
Lung Function
- 7. The evidence is suggestive but not sufficient to infer a causal relationship between short-term secondhand smoke exposure and an acute decline in lung function in persons with asthma.
- 8. The evidence is inadequate to infer the presence or absence of a causal relationship between short-term secondhand smoke exposure and an acute decline in lung function in healthy persons.
- 9. The evidence is suggestive but not sufficient to infer a causal relationship between chronic secondhand smoke exposure and a small decrement in lung function in the general population.
- 10. The evidence is inadequate to infer the presence or absence of a causal relationship between chronic secondhand smoke exposure and an accelerated decline in lung function.
- 11. The evidence is suggestive but not sufficient to infer a causal relationship between secondhand smoke exposure and adult-onset asthma.
- 12. The evidence is suggestive but not sufficient to infer a causal relationship between secondhand smoke exposure and a worsening of asthma control.
Chronic Obstructive Pulmonary Disease
- 13. The evidence is suggestive but not sufficient to infer a causal relationship between secondhand smoke exposure and risk for chronic obstructive pulmonary disease.
- 14. The evidence is inadequate to infer the presence or absence of a causal relationship between secondhand smoke exposure and morbidity in persons with chronic obstructive pulmonary disease.
Chapter 10. Control of Secondhand Smoke Exposure
- Workplace smoking restrictions are effective in reducing secondhand smoke exposure.
- Workplace smoking restrictions lead to less smoking among covered workers.
- Establishing smoke-free workplaces is the only effective way to ensure that secondhand smoke exposure does not occur in the workplace.
- The majority of workers in the United States are now covered by smoke-free policies.
- The extent to which workplaces are covered by smoke-free policies varies among worker groups, across states, and by sociodemographic factors. Workplaces related to the entertainment and hospitality industries have notably high potential for secondhand smoke exposure.
- Evidence from peer-reviewed studies shows that smoke-free policies and regulations do not have an adverse economic impact on the hospitality industry.
- Evidence suggests that exposure to secondhand smoke varies by ethnicity and gender.
- In the United States, the home is now becoming the predominant location for exposure of children and adults to secondhand smoke.
- Total bans on indoor smoking in hospitals, restaurants, bars, and offices substantially reduce secondhand smoke exposure, up to several orders of magnitude with incomplete compliance, and with full compliance, exposures are eliminated.
- Exposures of nonsmokers to secondhand smoke cannot be controlled by air cleaning or mechanical air exchange.
- Methodologic Issues
Much of the evidence on the health effects of involuntary smoking comes from observational epidemiologic studies that were carried out to test hypotheses related to secondhand smoke and risk for diseases and other adverse health effects. The challenges faced in carrying out these studies reflect those of observational research generally: assessment of the relevant exposures and outcomes with sufficient validity and precision, selection of an appropriate study design, identification of an appropriate and sufficiently large study population, and collection of information on other relevant factors that may confound or modify the association being studied. The challenge of accurately classifying secondhand smoke exposures confronts all studies of such exposures, and consequently the literature on approaches to and limitations of exposure classification is substantial. Sources of bias that can affect the findings of epidemiologic studies have been widely discussed ( Rothman and Greenland 1998 ), both in general and in relation to studies of involuntary smoking. Concerns about bias apply to any study of an environmental agent and disease risk: misclassification of exposures or outcomes, confounding effect modification, and proper selection of study participants. In addition, the generalizability of findings from one population to another (external validity) further determines the value of evidence from a study. Another methodologic concern affecting secondhand smoke literature comes from the use of meta-analysis to combine the findings of epidemiologic studies; general concerns related to the use of meta-analysis for observational data and more specific concerns related to involuntary smoking have also been raised. This chapter considers these methodologic issues in anticipation of more specific treatment in the following chapters.
Classification of Secondhand Smoke Exposure
For secondhand smoke, as for any environmental factor that may be a cause of disease, the exposure assessment might encompass the time and place of the exposure, cumulative exposures, exposure during a particular time, or a recent exposure ( Jaakkola and Jaakkola 1997 ; Jaakkola and Samet 1999 ). For example, exposures to secondhand smoke across the full life span may be of interest for lung cancer, while only more recent exposures may be relevant to the exacerbation of asthma. For CHD , both temporally remote and current exposures may affect risk. Assessments of exposures are further complicated by the multiplicity of environments where exposures take place and the difficulty of characterizing the exposure in some locations, such as public places or workplaces. Additionally, exposures probably vary qualitatively and quantitatively over time and across locations because of temporal changes and geographic differences in smoking patterns.
Nonetheless, researchers have used a variety of approaches for exposure assessments in epidemiologic studies of adverse health effects from involuntary smoking. Several core concepts that are fundamental to these approaches are illustrated in Figure 1.1 ( Samet and Jaakkola 1999 ). Cigarette smoking is, of course, the source of most secondhand smoke in the United States, followed by pipes, cigars, and other products. Epidemiologic studies generally focus on assessing the exposure, which is the contact with secondhand smoke. The concentrations of secondhand smoke components in a space depend on the number of smokers and the rate at which they are smoking, the volume into which the smoke is distributed, the rate at which the air in the space exchanges with uncontaminated air, and the rate at which the secondhand smoke is removed from the air. Concentration, exposure, and dose differ in their definitions, although the terms are sometimes used without sharp distinctions. However, surrogate indicators that generally describe a source of exposure may also be used to assess the exposure, such as marriage to a smoker or the number of cigarettes smoked in the home. Biomarkers can provide an indication of an exposure or possibly the dose, but for secondhand smoke they are used for recent exposure only.
The determinants of exposure, dose, and biologically effective dose that underlie the development of health effects from smoking. Source: Samet and Jaakkola (more...)
People are exposed to secondhand smoke in a number of different places, often referred to as “microenvironments” ( NRC 1991 ). A microenvironment is a definable location that has a constant concentration of the contaminant of interest, such as secondhand smoke, during the time that a person is there. Some key microenvironments for secondhand smoke include the home, the workplace, public places, and transportation environments ( Klepeis 1999 ). Based on the microenvironmental model, total exposure can be estimated as the weighted average of the concentrations of secondhand smoke or indicator compounds, such as nicotine, in the microenvironments where time is spent; the weights are the time spent in each microenvironment. Klepeis (1999) illustrates the application of the microenvironmental model with national data from the National Human Activity Pattern Survey conducted by the EPA . His calculations yield an overall estimate of exposure to airborne particles from smoking and of the contributions to this exposure from various microenvironments.
Much of the epidemiologic evidence addresses the consequences of an exposure in a particular microenvironment, such as the home (spousal smoking and lung cancer risk or maternal smoking and risk for asthma exacerbation), or the workplace (exacerbation of asthma by the presence of smokers). Some studies have attempted to cover multiple microenvironments and to characterize exposures over time. For example, in the multicenter study of secondhand smoke exposure and lung cancer carried out in the United States, Fontham and colleagues (1994) assessed exposures during childhood, in workplaces, and at home during adulthood. Questionnaires that assess exposures have been the primary tool used in epidemiologic studies of secondhand smoke and disease. Measurement of biomarkers has been added in some studies, either as an additional and complementary exposure assessment approach or for validating questionnaire responses. Some studies have also measured components of secondhand smoke in the air.
Questionnaires generally address sources of exposure in microenvironments and can be tailored to address the time period of interest. Questionnaires represent the only approach that can be used to assess exposures retrospectively over a life span, because available biomarkers only reflect exposures over recent days or, at most, weeks. Questionnaires on secondhand smoke exposure have been assessed for their reliability and validity, generally based on comparisons with either biomarker or air monitoring data as the “gold” standard ( Jaakkola and Jaakkola 1997 ). Two studies evaluated the reliability of questionnaires on lifetime exposures ( Pron et al. 1988 ; Coultas et al. 1989 ). Both showed a high degree of repeatability for questions concerning whether a spouse had smoked, but a lower reliability for responses concerning the quantitative aspects of an exposure. Emerson and colleagues (1995) evaluated the repeatability of information from parents of children with asthma. They found a high reliability for parent-reported tobacco use and for the number of cigarettes to which the child was exposed in the home during the past week.
To assess validity, questionnaire reports of current or recent exposures have been compared with levels of cotinine and other biomarkers. These studies tend to show a moderate correlation between levels of cotinine and questionnaire indicators of exposures ( Kawachi and Colditz 1996 ; Cal/EPA 1997 ; Jaakkola and Jaakkola 1997 ). However, cotinine levels reflect not only exposure but metabolism and excretion ( Benowitz 1999 ). Consequently, exposure is only one determinant of variation in cotinine levels among persons; there also are individual variations in metabolism and excretion rates. In spite of these sources of variability, mean levels of cotinine vary as anticipated across categories of self-reported exposures ( Cal/EPA 1997 ; Jaakkola and Jaakkola 1997 ), and self-reported exposures are moderately associated with measured levels of markers ( Cal/EPA 1997 ; Jaakkola and Jaakkola 1997 ).
Biomarkers are also used for assessing exposures to secondhand smoke. A number of biomarkers are available, but they vary in their specificity and in the dynamics of the temporal relationship between the exposure and the marker level ( Cal/EPA 1997 ; Benowitz 1999 ). These markers include specific tobacco smoke components (nicotine) or metabolites (cotinine and tobacco-specific nitrosamines), nonspecific biomarkers (thiocyanate and CO ), adducts with tobacco smoke components or metabolites (4-amino-biphenyl hemoglobin adducts, benzo[ a ]pyrene DNA adducts, and polycyclic aromatic hydrocarbon albumin adducts), and nonspecific assays (urinary mutagenicity). Cotinine has been the most widely used biomarker, primarily because of its specificity, half-life, and ease of measurement in body fluids (e. g ., urine, blood, and saliva). Biomarkers are discussed in detail in Chapter 3 (Assessment of Exposure to Secondhand Smoke).
Some epidemiologic studies have also incorporated air monitoring, either direct personal sampling or the indirect approach based on the microenvironmental model. Nicotine, present in the gas phase of secondhand smoke, can be monitored passively with a special filter or actively using a pump and a sorbent. Hammond and Leaderer (1987) first described a diffusion monitor for the passive sampling of nicotine in 1987; this device has now been widely used to assess concentrations in different environments and to study health effects. Airborne particles have also been measured using active monitoring devices.
Each of these approaches for assessing exposures has strengths and limitations, and preference for one over another will depend on the research question and its context ( Jaakkola and Jaakkola 1997 ; Jaakkola and Samet 1999 ). Questionnaires can be used to characterize sources of exposures, such as smoking by parents. With air concentrations of markers and time-activity information, estimates of secondhand smoke exposures can be made with the microenvironmental model. Biomarkers provide exposure measures that reflect the patterns of exposure and the kinetics of the marker; the cotinine level in body fluids, for example, reflects an exposure during several days. Air monitoring may be useful for validating measurements of exposure. Exposure assessment strategies are matched to the research question and often employ a mixture of approaches determined by feasibility and cost constraints.
Misclassification of Secondhand Smoke Exposure
Misclassification may occur when classifying exposures, outcomes, confounding factors, or modifying factors. Misclassification may be differential on either exposure or outcome, or it may be random ( Armstrong et al. 1992 ). Differential or nonrandom misclassification may either increase or decrease estimates of effect, while random misclassification tends to reduce the apparent effect and weaken the relationship of exposure with disease risk. In studies of secondhand smoke and disease risk, exposure misclassification has been a major consideration in the interpretation of the evidence, although misclassification of health outcome measures has not been a substantial issue in this research. The consequences for epidemiologic studies of misclassification in general are well established ( Rothman and Greenland 1998 ).
An extensive body of literature on the classification of exposures to secondhand smoke is reviewed in this and other chapters, as well as in some publications on the consequences of misclassification ( Wu 1999 ). Two general patterns of exposure misclassification are of concern to secondhand smoke: (1) random misclassification that is not differential by the presence or absence of the health outcome and (2) systematic misclassification that is differential by the health outcome. In studying the health effects of secondhand smoke in adults, there is a further concern as to the classification of the active smoking status (never, current, or former smoking); in studies of children, the accuracy of secondhand smoke exposure classification is the primary methodologic issue around exposure assessment, but unreported active smoking by adolescents is also a concern.
With regard to random misclassification of secondhand smoke exposures, there is an inherent degree of unavoidable measurement error in the exposure measures used in epidemiologic studies. Questionnaires generally assess contact with sources of an exposure (e. g ., smoking in the home or work-place) and cannot capture all exposures nor the intensity of exposures; biomarkers provide an exposure index for a particular time window and have intrinsic variability. Some building-related factors that determine an exposure cannot be assessed accurately by a questionnaire, such as the rate of air exchange and the size of the microenvironment where time is spent, nor can concentrations be assessed accurately by subjective reports of the perceived level of tobacco smoke. In general, random misclassification of exposures tends to reduce the likelihood that studies of secondhand smoke exposure will find an effect. This type of misclassification lessens the contrast between exposure groups, because some truly exposed persons are placed in the unexposed group and some truly unexposed persons are placed in the exposed group. Differential misclassification, also a concern, may increase or decrease associations, depending on the pattern of misreporting.
One particular form of misclassification has been raised with regard to secondhand smoke exposure and lung cancer: the classification of some current or former smokers as lifetime nonsmokers ( USEPA 1992 ; Lee and Forey 1995 ; Hackshaw et al. 1997 ; Wu 1999 ). The resulting bias would tend to increase the apparent association of secondhand smoke with lung cancer, if the misclassified active smokers are also more likely to be classified as involuntary smokers. Most studies of lung cancer and secondhand smoke have used spousal smoking as a main exposure variable. As smoking tends to aggregate between spouses (smokers are more likely to marry smokers), misclassification of active smoking would tend to be differential on the basis of spousal smoking (the exposure under investigation). Because active smoking is strongly associated with increased disease risk, greater misclassification of an actively smoking spouse as a non-smoker among spouses of smokers compared with spouses of nonsmokers would lead to risk estimates for spousal smoking that are biased upward by the effect of active smoking. This type of misclassification is also relevant to studies of spousal exposure and CHD risk or other diseases also caused by active smoking, although the potential for bias is less because the association of active smoking with CHD is not as strong as with lung cancer.
There have been a number of publications on this form of misclassification. Wu (1999) provides a review, and Lee and colleagues (2001) offer an assessment of potential consequences. A number of models have been developed to assess the extent of bias resulting from the misclassification of active smokers as lifetime nonsmokers ( USEPA 1992 ; Hackshaw et al. 1997 ). These models incorporate estimates of the rate of misclassification, the degree of aggregation of smokers by marriage, the prevalence of smoking in the population, and the risk of lung cancer in misclassified smokers ( Wu 1999 ). Although debate about this issue continues, analyses show that estimates of upward bias from misclassifying active smokers as lifetime nonsmokers cannot fully explain the observed increase in risk for lung cancer among lifetime non-smokers married to smokers ( Hackshaw et al. 1997 ; Wu 1999 ).
There is one additional issue related to exposure misclassification. During the time the epidemiologic studies of secondhand smoke have been carried out, exposure has been widespread and almost unavoidable. Therefore, the risk estimates may be biased downward because there are no truly unexposed persons. The 1986 Surgeon General’s report recognized this methodologic issue and noted the need for further data on population exposures to secondhand smoke ( USDHHS 1986 ). This bias was also recognized in the 1986 report of the NRC , and an adjustment for this misclassification was made to the lung cancer estimate ( NRC 1986 ). Similarly, the 1992 report of the EPA commented on background exposure and made an adjustment ( USEPA 1992 ). Some later studies have attempted to address this issue; for example, in a case-control study of active and involuntary smoking and breast cancer in Switzerland, Morabia and colleagues (2000) used a questionnaire to assess exposure and identified a small group of lifetime nonsmokers who also reported no exposure to secondhand smoke. With this subgroup of controls as the reference population, the risks of secondhand smoke exposure were substantially greater for active smoking than when the full control population was used.
This Surgeon General’s report further addresses specific issues of exposure misclassification when they are relevant to the health outcome under consideration.
Use of Meta-Analysis
Meta-analysis refers to the process of evaluating and combining a body of research literature that addresses a common question. Meta-analysis is composed of qualitative and quantitative components. The qualitative component involves the systematic identification of all relevant investigations, a systematic assessment of their characteristics and quality, and the decision to include or exclude studies based on predetermined criteria. Consideration can be directed toward sources of bias that might affect the findings. The quantitative component involves the calculation and display of study results on common scales and, if appropriate, the statistical combination of these results across studies and an exploration of the reasons for any heterogeneity of findings. Viewing the findings of all studies as a single plot provides insights into the consistency of results and the precision of the studies considered. Most meta-analyses are based on published summary results, although they are most powerful when applied to data at the level of individual participants. Meta-analysis is most widely used to synthesize evidence from randomized clinical trials, sometimes yielding findings that were not evident from the results of individual studies. Meta-analysis also has been used extensively to examine bodies of observational evidence.
Beginning with the 1986 NRC report, meta-analysis has been used to summarize the evidence on involuntary smoking and health. Meta-analysis was central to the 1992 EPA risk assessment of secondhand smoke, and a series of meta-analyses supported the conclusions of the 1998 report of the Scientific Committee on Tobacco and Health in the United Kingdom. The central role of meta-analysis in interpreting and applying the evidence related to involuntary smoking and disease has led to focused criticisms of the use of meta-analysis in this context. Several papers that acknowledged support from the tobacco industry have addressed the epidemiologic findings for lung cancer, including the selection and quality of the studies, the methods for meta-analysis, and dose-response associations ( Fleiss and Gross 1991 ; Tweedie and Mengersen 1995 ; Lee 1998 , 1999 ). In a lawsuit brought by the tobacco industry against the EPA, the 1998 decision handed down by Judge William L . Osteen, Sr., in the North Carolina Federal District Court criticized the approach EPA had used to select studies for its meta-analysis and criticized the use of 90 percent rather than 95 percent confidence intervals for the summary estimates ( Flue-Cured Tobacco Cooperative Stabilization Corp. v. United States Environmental Protection Agency , 857 F. Supp. 1137 [M.D.N.C. 1993]). In December 2002, the 4th U.S. Circuit Court of Appeals threw out the lawsuit on the basis that tobacco companies cannot sue the EPA over its secondhand smoke report because the report was not a final agency action and therefore not subject to court review ( Flue-Cured Tobacco Cooperative Stabilization Corp. v. The United States Environmental Protection Agency , No. 98–2407 [4th Cir., December 11, 2002], cited in 17.7 TPLR 2.472 [2003]).
Recognizing that there is still an active discussion around the use of meta-analysis to pool data from observational studies (versus clinical trials), the authors of this Surgeon General’s report used this methodology to summarize the available data when deemed appropriate and useful, even while recognizing that the uncertainty around the meta-analytic estimates may exceed the uncertainty indicated by conventional statistical indices, because of biases either within the observational studies or produced by the manner of their selection. However, a decision to not combine estimates might have produced conclusions that are far more uncertain than the data warrant because the review would have focused on individual study results without considering their overall pattern, and without allowing for a full accounting of different sample sizes and effect estimates.
The possibility of publication bias has been raised as a potential limitation to the interpretation of evidence on involuntary smoking and disease in general, and on lung cancer and secondhand smoke exposure specifically. A 1988 paper by Vandenbroucke used a descriptive approach, called a “funnel plot,” to assess the possibility that publication bias affected the 13 studies considered in a review by Wald and colleagues (1986) . This type of plot characterizes the relationship between the magnitude of estimates and their precision. Vandenbroucke suggested the possibility of publication bias only in reference to the studies of men. Bero and colleagues (1994) concluded that there had not been a publication bias against studies with statistically significant findings, nor against the publication of studies with nonsignificant or mixed findings in the research literature. The researchers were able to identify only five unpublished “negative” studies, of which two were dissertations that tend to be delayed in publication. A subsequent study by Misakian and Bero (1998) did find a delay in the publication of studies with nonsignificant results in comparison with studies having significant results; whether this pattern has varied over the several decades of research on secondhand smoke was not addressed. More recently, Copas and Shi (2000) assessed the 37 studies considered in the meta-analysis by Hackshaw and colleagues (1997) for publication bias. Copas and Shi (2000) found a significant correlation between the estimated risk of exposure and sample size, such that smaller studies tended to have higher values. This pattern suggests the possibility of publication bias. However, using a funnel plot of the same studies, Lubin (1999) found little evidence for publication bias.
On this issue of publication bias, it is critical to distinguish between indirect statistical arguments and arguments based on actual identification of previously unidentified research. The strongest case against substantive publication bias has been made by researchers who mounted intensive efforts to find the possibly missing studies; these efforts have yielded little nothing that would alter published conclusions ( Bero et al. 1994 ; Glantz 2000 ). Presumably because this exposure is a great public health concern, the findings of studies that do not have statistically significant outcomes continue to be published ( Kawachi and Colditz 1996 ).
The quantitative results of the meta-analyses, however, were not determinate in making causal inferences in this Surgeon General’s report. In particular, the level of statistical significance of estimates from the meta-analyses was not a predominant factor in making a causal conclusion. For that purpose, this report relied on the approach and criteria set out in the 1964 and 2004 reports of the Surgeon General, which involved judgments based on an array of quantitative and qualitative considerations that included the degree of heterogeneity in the designs of the studies that were examined. Sometimes this heterogeneity limits the inference from meta-analysis by weakening the rationale for pooling the study results. However, the availability of consistent evidence from heterogenous designs can strengthen the meta-analytic findings by making it unlikely that a common bias could persist across different study designs and populations.
Confounding
Confounding, which refers in this context to the mixing of the effect of another factor with that of secondhand smoke, has been proposed as an explanation for associations of secondhand smoke with adverse health consequences. Confounding occurs when the factor of interest (secondhand smoke) is associated in the data under consideration with another factor (the confounder) that, by itself, increases the risk for the disease ( Rothman and Greenland 1998 ). Correlates of secondhand smoke exposures are not confounding factors unless an exposure to them increases the risk of disease. A factor proposed as a potential confounder is not necessarily an actual confounder unless it fulfills the two elements of the definition. Although lengthy lists of potential confounding factors have been offered as alternatives to direct associations of secondhand smoke exposures with the risk for disease, the factors on these lists generally have not been shown to be confounding in the particular data of interest.
The term confounding also conveys an implicit conceptualization as to the causal pathways that link secondhand smoke and the confounding factor to disease risk. Confounding implies that the confounding factor has an effect on risk that is independent of secondhand smoke exposure. Some factors considered as potential confounders may, however, be in the same causal pathway as a secondhand smoke exposure. Although socioeconomic status ( SES ) is often cited as a potential confounding factor, it may not have an independent effect but can affect disease risk through its association with secondhand smoke exposure ( Figure 1.2 ). This figure shows general alternative relationships among SES, secondhand smoke exposure, and risk for an adverse effect. SES may have a direct effect, or it may indirectly exert its effect through an association with secondhand smoke exposure, or it may confound the relationship between secondhand smoke exposure and disease risk. To control for SES as a potential confounding factor without considering underlying relationships may lead to incorrect risk estimates. For example, controlling for SES would not be appropriate if it is a determinant of secondhand smoke exposure but has no direct effect.
Model for socioeconomic status (SES) and secondhand smoke (SHS) exposure. Arrows indicate directionality of association.
Nonetheless, because the health effects of involuntary smoking have other causes, the possibility of confounding needs careful exploration when assessing associations of secondhand smoke exposure with adverse health effects. In addition, survey data from the last several decades show that secondhand smoke exposure is associated with correlates of lifestyle that may influence the risk for some health effects, thus increasing concerns for the possibility of confounding ( Kawachi and Colditz 1996 ). Survey data from the United States ( Matanoski et al. 1995 ) and the United Kingdom ( Thornton et al. 1994 ) show that adults with secondhand smoke exposures generally tend to have less healthful lifestyles. However, the extent to which these patterns of association can be generalized, either to other countries or to the past, is uncertain.
The potential bias from confounding varies with the association of the confounder to secondhand smoke exposures in a particular study and to the strength of the confounder as a risk factor. The importance of confounding to the interpretation of evidence depends further on the magnitude of the effect of secondhand smoke on disease. As the strength of an association lessens, confounding as an alternative explanation for an association becomes an increasing concern. In prior reviews, confounding has been addressed either quantitatively ( Hackshaw et al. 1997 ) or qualitatively ( Cal/EPA 1997 ; Thun et al. 1999 ). In the chapters in this report that focus on specific diseases, confounding is specifically addressed in the context of potential confounding factors for the particular diseases.
- Tobacco Industry Activities
The evidence on secondhand smoke and disease risk, given the public health and public policy implications, has been reviewed extensively in the published peer-reviewed literature and in evaluations by a number of expert panels. In addition, the evidence has been criticized repeatedly by the tobacco industry and its consultants in venues that have included the peer-reviewed literature, public meetings and hearings, and scientific symposia that included symposia sponsored by the industry. Open criticism in the peer-reviewed literature can strengthen the credibility of scientific evidence by challenging researchers to consider the arguments proposed by critics and to rebut them.
Industry documents indicate that the tobacco industry has engaged in widespread activities, however, that have gone beyond the bounds of accepted scientific practice ( Glantz 1996 ; Ong and Glantz 2000 , 2001 ; Rampton and Stauber 2000 ; Yach and Bialous 2001 ; Hong and Bero 2002 ; Diethelm et al. 2004 ). Through a variety of organized tactics, the industry has attempted to undermine the credibility of the scientific evidence on secondhand smoke. The industry has funded or carried out research that has been judged to be biased, supported scientists to generate letters to editors that criticized research publications, attempted to undermine the findings of key studies, assisted in establishing a scientific society with a journal, and attempted to sustain controversy even as the scientific community reached consensus ( Garne et al. 2005 ). These tactics are not a topic of this report, but to the extent that the scientific literature has been distorted, they are addressed as the evidence is reviewed. This report does not specifically identify tobacco industry sponsorship of publications unless that information is relevant to the interpretation of the findings and conclusions.
- Armstrong BK, White E, Saracci R, editors. Monographs in Epidemiology and Biostatistics. Vol. 21. New York: Oxford University Press; 1992. Principles of Exposure Measurement in Epidemiology.
- Benowitz NL. Biomarkers of environmental tobacco smoke. Environmental Health Perspectives. 1999; 107 (Suppl 2):349–55. [ PMC free article : PMC1566286 ] [ PubMed : 10350520 ]
- Bero LA, Glantz SA, Rennie D. Publication bias and public health policy on environmental tobacco smoke. Journal of the American Medical Association. 1994; 272 (2):133–6. [ PubMed : 8015124 ]
- California Environmental Protection Agency. Health Effects of Exposure to Environmental Tobacco Smoke. Sacramento (CA): California Environmental Protection Agency, Office of Environmental Health Hazard Assessment, Reproductive and Cancer Hazard Assessment Section and Air Toxicology and Epidemiology Section; 1997.
- California Environmental Protection Agency. Part B: Health Effects. Sacramento (CA): California Environmental Protection Agency, Office of Environmental Health Hazard Assessment; 2005. Proposed Identification of Environmental Tobacco Smoke as a Toxic Air Contaminant.
- Copas JB, Shi JQ. Reanalysis of epidemiological evidence on lung cancer and passive smoking. British Medical Journal. 2000; 320 (7232):417–8. [ PMC free article : PMC27286 ] [ PubMed : 10669446 ]
- Coultas DB, Peake GT, Samet JM. Questionnaire assessment of lifetime and recent exposure to environmental tobacco smoke. American Journal of Epidemiology. 1989; 130 (2):338–47. [ PubMed : 2750729 ]
- Diethelm PA, Rielle JC, McKee M.The whole truth and nothing but the truth? The research that Phillip Morris did not want you to see. Nov 11, 2004. [accessed: January 6, 2005]. http://image .thelancet .com/extras/03art7306web.pdf [ PubMed : 15993237 ]
- Emerson JA, Hovell MF, Meltzer SB, Zakarian JM, Hofstetter CR, Wahlgren DR, Leaderer BP, Meltzer EO. The accuracy of environmental tobacco smoke exposure measures among asthmatic children. Journal of Clinical Epidemiology. 1995; 48 (10):1251–9. [ PubMed : 7561987 ]
- Fleiss JL, Gross AJ. Meta-analysis in epidemiology, with special reference to studies of the association between exposure to environmental tobacco smoke and lung cancer: a critique. Journal of Clinical Epidemiology. 1991; 44 (2):127–39. [ PubMed : 1995774 ]
- Flue-Cured Tobacco Cooperative Stabilization Corp. v. United States Environmental Protection Agency (M.D.N.C. June 22, 1993), cited in 8.2 TPLR 3.97 (1993).
- Flue-Cured Tobacco Cooperative Stabilization Corp. v. The United States Environmental Protection Agency, No. 98–2407 (4th Cir., December 11, 2002), cited in 17.7 TPLR 2.472 (2003) (Overturning lower court’s decision invalidating EPA’s findings that secondhand smoke is a “known human carcinogen”).
- Fontham ET, Correa P, Reynolds P, Wu-Williams A, Buffler PA, Greenberg RS, Chen VW, Alterman T, Boyd P, Austin DF, Liff J. Environmental tobacco smoke and lung cancer in nonsmoking women: a multicenter study. Journal of the American Medical Association. 1994; 271 (22):1752–9. [ PubMed : 8196118 ]
- Garne D, Watson M, Chapman S, Byrne F. Environmental tobacco smoke research published in the journal Indoor and Built Environment and associations with the tobacco industry. Lancet. 2005; 365 (9461):804–9. [ PubMed : 15733724 ]
- Glantz SA. The ledger of tobacco control. Journal of the American Medical Association. 1996; 276 (11):871–2. [ PubMed : 8782631 ]
- Glantz SA. Lung cancer and passive smoking: nothing new was said. British Medical Journal. 2000; 321 (7270):1222–3. [ PubMed : 11073523 ]
- Hackshaw AK, Law MR, Wald NJ. The accumulated evidence on lung cancer and environmental tobacco smoke. British Medical Journal. 1997; 315 (7114):980–8. [ PMC free article : PMC2127653 ] [ PubMed : 9365295 ]
- Hammond SK, Leaderer BP. A diffusion monitor to measure exposure to passive smoking. Environmental Science & Technology. 1987; 21 (5):494–7. [ PubMed : 22296139 ]
- Hong MK, Bero LA. How the tobacco industry responded to an influential study of the health effects of secondhand smoke. British Medical Journal. 2002; 325 (7377):1413–6. [ PMC free article : PMC1124865 ] [ PubMed : 12480862 ]
- International Agency for Research on Cancer. IARC Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans: Tobacco Smoking. Vol. 38. Lyon (France): International Agency for Research on Cancer; 1986.
- International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Tobacco Smoke and Involuntary Smoking. Vol. 83. Lyon (France): International Agency for Research on Cancer; 2004. [ PMC free article : PMC4781536 ] [ PubMed : 15285078 ]
- Jaakkola MS, Jaakkola JJ. Assessment of exposure to environmental tobacco smoke. European Respiratory Journal. 1997; 10 (10):2384–97. [ PubMed : 9387970 ]
- Jaakkola MS, Samet JM. Environmental tobacco smoke: risk assessment. Environmental Health Perspectives. 1999; 107 (Suppl 6):823–904. [ PMC free article : PMC1566195 ] [ PubMed : 10592138 ]
- Kawachi I, Colditz GA. Invited commentary: confounding, measurement error, and publication bias in studies of passive smoking. American Journal of Epidemiology. 1996; 144 (10):909–15. [ PubMed : 8916501 ]
- Klepeis NE. An introduction to the indirect exposure assessment approach: modeling human exposure using microenvironmental measurements and the recent National Human Activity Pattern Survey. Environmental Health Perspectives. 1999; 107 (Suppl 2):365–74. [ PMC free article : PMC1566279 ] [ PubMed : 10350522 ]
- Lee PN. Difficulties in assessing the relationship between passive smoking and lung cancer. Statistical Methods in Medical Research. 1998; 7 (2):137–63. [ PubMed : 9654639 ]
- Lee PN. Simple methods for checking for possible errors in reported odds ratios, relative risks and confidence intervals. Statistics in Medicine. 1999; 18 (15):1973–81. [ PubMed : 10440880 ]
- Lee PN, Forey BA. Misclassification of smoking habits as determined by cotinine or by repeated self-report—summary of evidence from 42 studies. Journal of Smoking-Related Diseases. 1995; 6 :109–29.
- Lee PN, Forey B, Fry JS. Revisiting the association between environmental tobacco smoke exposure and lung cancer risk. III: Adjusting for the biasing effect of misclassification of smoking habits. Indoor and Built Environment. 2001; 10 (6):384–98.
- Lubin JH. Estimating lung cancer risk with exposure to environmental tobacco smoke. Environmental Health Perspectives. 1999; 107 (Suppl 6):879–83. [ PMC free article : PMC1566203 ] [ PubMed : 10592146 ]
- Matanoski G, Kanchanaraksa S, Lantry D, Chang Y. Characteristics of nonsmoking women in NHANES I and NHANES I Epidemiologic Follow-up Study with exposure to spouses who smoke. American Journal of Epidemiology. 1995; 142 (2):149–57. [ PubMed : 7598114 ]
- Misakian AL, Bero LA. Publication bias and research on passive smoking: comparison of published and unpublished studies. Journal of the American Medical Association. 1998; 280 (3):250–3. [ PubMed : 9676672 ]
- Morabia A, Bernstein MS, Bouchardy I, Kurtz J, Morris MA. Breast cancer and active and passive smoking: the role of the N -acetyltransferase 2 genotype. American Journal of Epidemiology. 2000; 152 (3):226–32. [ PubMed : 10933269 ]
- National Health and Medical Research Council. A scientific information paper. Canberra (Commonwealth of Australia): Canberra ACT; 1997. The Health Effects of Passive Smoking.
- National Research Council. Environmental Tobacco Smoke: Measuring Exposures and Assessing Health Effects. Washington: National Academy Press; 1986. [ PubMed : 25032469 ]
- National Research Council. Human Exposure Assessment for Airborne Pollutants: Advances and Opportunities. Washington: National Academy Press; 1991.
- Ong EK, Glantz SA. Tobacco industry efforts subverting International Agency for Research on Cancer’s second-hand smoke study. Lancet. 2000; 355 (9211):1253–9. [ PubMed : 10770318 ]
- Ong EK, Glantz SA. Constructing “sound science” and “good epidemiology”: tobacco, lawyers, and public relations rms. American Journal of Public Health. 2001; 91 (11):1749–57. [ PMC free article : PMC1446868 ] [ PubMed : 11684593 ]
- Pron GE, Burch JD, Howe GR, Miller AB. The reliability of passive smoking histories reported in a case-control study of lung cancer. American Journal of Epidemiology. 1988; 127 (2):267–73. [ PubMed : 3337082 ]
- Rampton S, Stauber J. Trust Us, We’re Experts: How Industry Manipulates Science and Gambles with Your Future. Los Angeles: J.P. Tarcher; 2000.
- Rothman KJ, Greenland S. Modern Epidemiology. 2nd ed. Philadelphia: Lippincott-Raven; 1998.
- Samet JM, Jaakkola JJK. The epidemiologic approach to investigating outdoor air pollution. In: Holgate ST, Samet JM, Koren HS, Maynard RL, editors. Air Pollution and Health. San Diego: Academic Press; 1999. pp. 431–60.
- Scientific Committee on Tobacco and Health . Report of the Scientific Committee on Tobacco and Health. London: The Stationery Office; 1998.
- Thornton A, Lee P, Fry J. Differences between smokers, ex-smokers, passive smokers and non-smokers. Journal of Clinical Epidemiology. 1994; 47 (10):1143–62. [ PubMed : 7722548 ]
- Thun M, Henley J, Apicella L. Epidemiologic studies of fatal and nonfatal cardiovascular disease and ETS exposure from spousal smoking. Environmental Health Perspectives. 1999; 107 (Suppl 6):841–6. [ PMC free article : PMC1566204 ] [ PubMed : 10592140 ]
- Tweedie RL, Mengersen KL. Meta-analytic approaches to dose-response relationships, with application in studies of lung cancer and exposure to environmental tobacco smoke. Statistics in Medicine. 1995; 14 (5–7):545–69. [ PubMed : 7792447 ]
- US Department of Health and Human Services . The Health Consequences of Smoking: Cancer A Report of the Surgeon General. Rockville (MD): U.S. Department of Health and Human Services, Public Health Service, Office on Smoking and Health; 1982. DHHS Publication No. (PHS) 82–50179.
- US Department of Health and Human Services. A Report of the Surgeon General. Rockville (MD): U.S. Department of Health and Human Services, Public Health Service, Office on Smoking and Health; 1984. The Health Consequences of Smoking: Chronic Obstructive Lung Disease. DHHS Publication No. (PHS) 84–50205.
- US Department of Health and Human Services. A Report of the Surgeon General. Rockville (MD): U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Health Promotion and Education, Office on Smoking and Health; 1986. The Health Consequences of Involuntary Smoking. DHHS Publication No. (CDC) 87–8398.
- US Department of Health and Human Services. A Report of the Surgeon General. Atlanta: US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1994. Preventing Tobacco Use Among Young People.
- US Department of Health and Human Services. A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1998. Tobacco Use Among US Racial/Ethnic Minority Groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics.
- US Department of Health and Human Services. A Report of the Surgeon General. Rockville (MD): U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2001. Women and Smoking.
- US Department of Health and Human Services. The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004.
- US Department of Health, Education, and Welfare. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington: U.S. Department of Health, Education, and Welfare, Public Health Service, Center for Disease Control; 1964. PHS Publication No. 1103.
- US Department of Health, Education, and Welfare. A Report of the Surgeon General: 1972. Washington: U.S. Department of Health, Education, and Welfare, Public Health Service, Health Services and Mental Health Administration; 1972. The Health Consequences of Smoking. DHEW Publication No. (HSM) 72–7516.
- US Department of Health, Education, and Welfare. A Report of the Surgeon General, 1975. Washington: U.S. Department of Health, Education, and Welfare, Public Health Service, Center for Disease Control; 1975. The Health Consequences of Smoking. DHEW Publication No. (CDC) 77–8704.
- US Department of Health, Education, and Welfare. A Report of the Surgeon General. Washington: U.S. Department of Health, Education, and Welfare, Public Health Service, Office of the Assistant Secretary for Health, Office of Smoking and Health; 1979. Smoking and Health. DHEW Publication No. (PHS) 79–50066.
- U.S. Environmental Protection Agency. Respiratory Health Effects of Passive Smoking: Lung Cancer and Other Disorders. Washington: U.S. Environmental Protection Agency, Office of Research and Development, Office of Air Radiation; 1992. Report No. EPA/600/6-90/0006F.
- Vandenbroucke JP. Passive smoking and lung cancer: a publication bias? British Medical Journal (Clinical Research Edition). 1988; 296 (6619):391–2. [ PMC free article : PMC2544973 ] [ PubMed : 3125912 ]
- Wald NJ, Nanchahal K, Thompson SG, Cuckle HS. Does breathing other people’s tobacco smoke cause lung cancer? British Medical Journal (Clinical Research Edition). 1986; 293 (6556):1217–22. [ PMC free article : PMC1341990 ] [ PubMed : 3096439 ]
- World Health Organization. International Consultation on Environmental Tobacco Smoke (ETS) and Child Health: Consultation Report. Geneva: World Health Organization; 1999.
- Wu AH. Exposure misclassification bias in studies of environmental tobacco smoke and lung cancer. Environmental Health Perspectives. 1999; 107 (Suppl 6):873–7. [ PMC free article : PMC1566193 ] [ PubMed : 10592145 ]
- Yach D, Bialous SA. Junking science to promote tobacco. American Journal of Public Health. 2001; 91 (11):1745–8. [ PMC free article : PMC1446867 ] [ PubMed : 11684592 ]
- Cite this Page Office on Smoking and Health (US). The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2006. 1, Introduction, Summary, and Conclusions.
- PDF version of this title (20M)
- Disable Glossary Links
In this Page
Other titles in these collections.
- Publications and Reports of the Surgeon General
- Health Services/Technology Assessment Text (HSTAT)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Introduction, Summary, and Conclusions - The Health Consequences of Involuntary ... Introduction, Summary, and Conclusions - The Health Consequences of Involuntary Exposure to Tobacco Smoke
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Hepatitis C cases dropped in the US. Health officials aren’t sure if it’s a blip or a trend
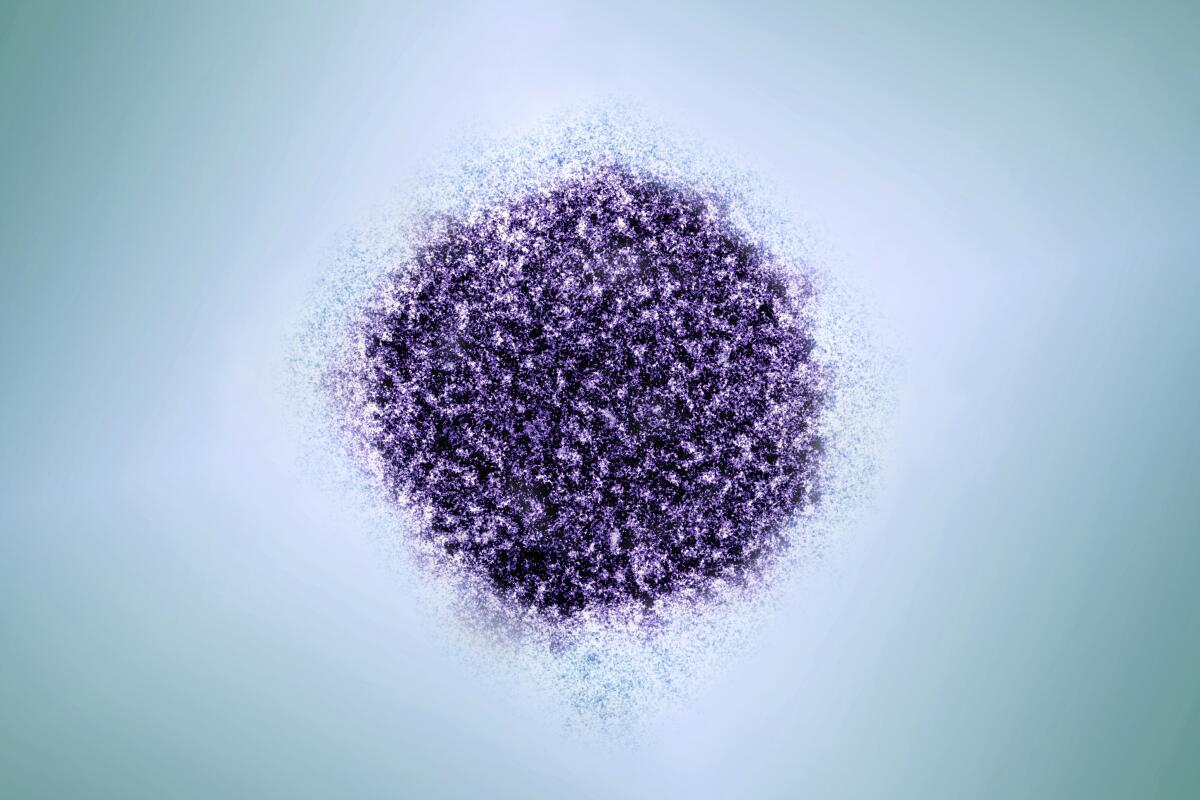
- Show more sharing options
- Copy Link URL Copied!
New U.S. hepatitis C infections dropped slightly in 2022, a surprising improvement after more than a decade of steady increases , federal health officials said Wednesday.
Experts are not sure whether the 6% decline is a statistical blip or the start of a downward trend. Seeing 2023 and 2024 data, when it’s available, will help public health officials understand what’s going on, said Daniel Raymond, director of policy at the National Viral Hepatitis Roundtable, an advocacy organization.
“We’ve had a decade of bad news ... I am cautiously encouraged,” he said. “You always want to hope like something like this is real, and a potential sign that the tide has turned.”
Infection rates did not occur across the board. They declined for white Americans, but continued to rise in Black, Latino and Native American communities, according to Dr. Neil Gupta, who oversees the branch of the Centers for Disease Control and Prevention that tracks viral hepatitis.
The hepatitis C virus is spread through contact with blood from an infected person. The virus does most of its damage by infecting the liver, and, if left untreated , can lead to cirrhosis or liver cancer. Infections are driven mainly by people injecting illicit drugs.
Data released by the CDC for 2022 shows 4,848 new infections, down from 5,023 reported the year before. The CDC estimates about 67,000 new hepatitis C infections actually occurred in 2022, because many people who become infected don’t realize it, meaning most new infections are not diagnosed and reported. But that too is down, from 70,000 estimated for 2021.
The new infection rate — used to better compare data from one year to another — dropped 6%. Though the decline is encouraging, Gupta said, the 2022 statistics are still twice as high was what the nation saw in 2015.
Cases had consistently gone up since 2013 during the longstanding opioid epidemic due to drug users shooting heroin and fentanyl. Experts say a couple of factors could have contributed to a decline in 2022, including successful prevention efforts and needle exchanges.
The North America Syringe Exchange Network keeps a directory of U.S. programs, and listings have grown from about 300 to nearly 500 in the last several years, said Paul LaKosky, NASEN’s executive director. Many programs also have boosted hepatitis C testing and found ways to get infected people to treatment, he noted.
But LaKosky and others think something else may be at play, too: Drug users are shifting from injecting to smoking. A recent CDC report found that between early 2020 and late 2022, the percentage of overdose deaths with evidence of smoking rose 74% while the percentage of deaths with evidence of injection fell 29%.
Fewer people injecting drugs like fentanyl means fewer opportunities for the spread of hepatitis C, experts noted.
“There has been a tremendous shift in the way people are consuming their drugs. There’s been a decrease in demand for syringes. We’ve seen this nationwide,” said LaKosky, who added there is more demand for supplies to snort or smoke drugs.
More than 2 million Americans are infected with hepatitis C, some of them having lived with infections for many years, the CDC estimates. About 12,700 Americans died in 2022 of hepatitis C-related causes, the CDC said.
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.
Top headlines by email, weekday mornings
Get top headlines from the Union-Tribune in your inbox weekday mornings, including top news, local, sports, business, entertainment and opinion.
You may occasionally receive promotional content from the San Diego Union-Tribune.
More in this section

Nation-World
Idaho lawmakers pass bills targeting LGBTQ+ citizens. Protesters toss paper hearts in protest
Idaho lawmakers have passed a series of bills targeting LGBTQ+ residents this year, including two this week that redefine gender as being synonymous with sex and prevent public employees from being required to use someone’s preferred pronouns
Mexican cartel not only forced vendors to buy chicken at inflated prices, they sold them bad birds
A Mexican drug cartel not only forced vendors to buy chicken at wildly inflated prices — they sold them chicken “not fit for human consumption.”
Man sentenced to 37 years on hate crime charges in deadly shooting at Muslim-owned tire shop
Authorities say a man who shot someone to death at a Muslim-owned tire shop in Dallas has been sentenced to 37 years in prison on federal hate crime charges

At least 241 people have died in El Salvador’s prisons during the ‘war on gangs,’ rights group says
The rights group Humanitarian Legal Relief says at least 241 people have died in El Salvador prisons since the start of President Nayib Bukele’s “war on gangs” two years ago
Chinese signatures on graduation certificates upset northern Virginia police chief
A northern Virginia town has been excluded from a countywide police training academy after the town’s chief complained about Chinese signatures on trainees’ graduation certificates

In rare call, Russian defense minister warns French counterpart against sending troops to Ukraine
Russia’s defense minister has warned his French counterpart against deploying troops to Ukraine in a rare phone call and noted that Moscow stands ready to take part in talks to end the fighting
- Skip to main content
- Keyboard shortcuts for audio player
'Our kids are not OK,' child psychiatrist Harold Koplewicz says

Terry Gross
The founder of the Child Mind Institute explains why young people are experiencing unprecedented levels of anxiety and depression — and what parents can do about it. His book is Scaffold Parenting.
TERRY GROSS, HOST:
This is FRESH AIR. I'm Terry Gross. There are so many reasons for children to be anxious today beyond all the standard childhood problems. There's the setbacks from the COVID lockdown, mass shootings in schools, feelings they're not measuring up to the great lives they see represented on social media, fears about the whole planet being in jeopardy. It's hardly unusual for parents to be unsure how to handle their child's anxiety, depression, learning problems, anger, tantrums. And it can be difficult for parents to evaluate whether their child should see a therapist or take medication.
My guest, child psychiatrist Harold Koplewicz, has dealt with these issues with many children and their parents. And there have been times he's been confounded about issues his own children faced. He's the founding president of the Child Mind Institute. Its stated mission is transforming the lives of children and families struggling with mental health and learning disorders by giving them the help they need to thrive. The institute also conducts related research.
From 1997 to 2009, he was the first director of the NYU Child Study Center. Koplewicz recently stepped down from his 25-year tenure as editor-in-chief of the Journal of Child and Adolescent Psychopharmacology. His latest book is titled "Scaffold Parenting: Raising Resilient, Self-Reliant And Secure Kids In An Age Of Anxiety." Dr. Harold Koplewicz, welcome to FRESH AIR. What are some of the problems and anxieties you're seeing now that you can connect to outside problems, like the COVID lockdown and its lingering aftereffects? How are you seeing that manifest in the children's anxieties that you're seeing?
HAROLD KOPLEWICZ: Well, I think our kids are not OK. And unfortunately, they weren't doing very well before COVID. But COVID has had a negative effect on all children. Children with mental health disorders and kids who are typically developing children being locked up for two years and living with fear that somebody close to you - someone near and dear - will die is very problematic. And we also know that 1 million Americans did die, which means that about 170,000 American children lost a caregiver or a parent.
And if we go back to 2001, after 9/11, we lost 3,000 Americans. And I can tell you that in New York, in certain pockets - Staten Island, where there were a lot of firemen, and Manhasset, where there were a lot of finance people who were in the building, and certainly people around ground zero - it was very hard to get kids to go back to school. Attendance rates didn't return to 9/10 - to September 10 levels for over a year and sometimes even longer.
So we do know that this kind of traumatic event is going to have lingering effects. And we have seen increases in anxiety disorders and in depression, particularly in girls but certainly even in boys. There are higher rates of kids trying to hurt themselves. And there is even an increase in the number of young people who have committed suicide. So there is no doubt that we had a problem before. And we have a greater problem now.
GROSS: The average child isn't necessarily, like, watching cable news or reading the newspaper. But you pick up a lot of this on social media. And it's also just in the air. Like, everybody's talking about these issues, like, environmental catastrophe, you know, political divisions. Is this the end of democracy? Is the planet burning? I mean, you're just - it's just in the air now.
KOPLEWICZ: Well, you know, there's something dramatically changed between 2010 and 2018. So the numbers start to jump when we started looking at children's mental health. There were higher rates of visits to emergency rooms by kids for suicidal thought and suicidal behavior. And the increase in the number of kids who died from suicide went from around 5,000 to 6,000. Now, just think about that. If it was diabetes, if it was cancer, that would have made the front page of every newspaper every single day. It would be on cable news 24/7. And somehow, we don't take mental health disorders as seriously as we take physical disorders.
And so, you know, what happened between 2010 and 2018 is that all of us started carrying a device with us that connected us to everybody on the planet 24/7. And that definitely had a negative effect on a certain percentage of the population. So I want to be clear that social media is not like smoking. It doesn't - it's not terrible for everyone. But it is particularly bad for kids who have mental health disorders. And we've really looked at this very carefully at the Child Mind Institute, where we had done a study before COVID that was looking for an objective test - a biological test. Psychiatry is the only discipline in medicine that doesn't have an objective test - doesn't have a chest X-ray or a blood test or a strep test. And therefore, that's the holy grail, right? We make the diagnosis with clinical information, which is how you start all diagnosis in every part of medicine. But you can confirm it with an EKG or with a brain scan. So psychiatry is missing that.
And so we started something called the Healthy Brain Network, where we offered any parent who was worried about their child - who was between the ages of 5 and 21 - a free psychiatric evaluation, free neuropsych testing, which looks for learning disabilities, a functional MRI and EEG, physical fitness, cardiovascular status, nutritional status. And this became the - and is still the largest collection of the developing brain of kids 5 to 21 that's ever been collected. And we share it with scientists around the world, who make an agreement with us that they won't try to find out who the subjects are.
GROSS: Wait. So is the point of this to figure out, is there a - like, a biological diagnosis you can make? Does the cohort of people who have, like, depression or anxiety or whatever share certain biological markers? Is that the point?
KOPLEWICZ: That would be the point. The real trick is, can you tell the difference between one atypical child and another? Not the difference between a typical developing child and someone who may have a mental health disorder or a learning disorder but the difference between Terry, who has anxiety, and Harold, who has depression. And is there something on the EEG or on the functional MRI? Can we find a definitive objective test? But the good news here is that when you collect all this data - and it turns out that 9% of the 7,000 kids that participated did not have a disorder. They had symptoms, but they didn't meet psychiatric criteria for a diagnosis. You now have described, very accurately and very specifically, phenotypically what these kids look like. And then you get COVID. And you find that their use of social media jumps. They are using the internet six to eight hours a day. And a...
GROSS: All the kids in the study?
KOPLEWICZ: No, no, no. Just a large percentage of them. And we start defining that as problematic internet usage. Not only are you using it a lot, but when you force them to stop, they get distressed. It almost feels like an addiction, right? And we do know that - it turns out for the 9%, who are typically developing kids, that when you use the internet more than six to eight hours a day, you will sleep less. You will exercise less. And you'll have less interactions in real life. All three of them are important for healthy brain development, but you don't become mentally ill. However, if you have a mental health disorder and you start behaving that way, your symptoms get worse. It's almost like a toxic agent. It turns out that the internet usage of over six to eight hours a day can make your symptoms of depression, your symptoms of ADHD significantly worse, which is a really important phenomena.
GROSS: Why do you think that is?
KOPLEWICZ: Well, it's a very good question. Why? Our guess is that for these kids, someone who has depression, they're already socially more isolated than the average person, and they start losing their skill set and their ambition to interact with the rest of the world. Kids with ADHD can get very hyper-focused with certain activities and at times feel very lost, very impulsive, feel very often like a failure when they can't pay attention in school or are missing things that everyone else is picking up. So what's important about this is that if you're a parent and you know your child has one of these disorders, you have to be very aware that their usage of social media, it could potentially be toxic and it has to be controlled. It can't be unlimited. Not that it's good for anyone to have unlimited, but it's particularly bad for those kids.
So we know that social media was out there between 2010 and 2018. And unfortunately, there's no regulation on it. And it means that parents have to be more aware. I mean, I think of it as, you know, a jungle, right? The jungle is an exciting place, very nutritious fruit and vegetables and lots of terrific stuff. Maybe medicines even can get discovered in the jungle. But it also has snakes, it also has dangerous plants that can kill you, it also has animals. And therefore, if you're going to let your child participate, you should be a very active participant in that permission.
GROSS: So if you think that social media can be very harmful to certain children, how would you suggest parents try to limit their time on social media? That's something that is really hard to do.
KOPLEWICZ: I think it is challenging, but I think it's very doable. We also have some good data. We know that parents who are using the internet in a, you know, problematic way are more likely to have kids that are doing it. Parents have to model this. They have to have periods where, we're putting the phone away at nighttime, and you're not allowed to look at it because we want you to sleep. We do want to look and see how much time you're spending on it, and we want you to be aware of how much time you're spending on it. So it's not, you know, punitive. It's a collaboration, especially if they're a teenager or a pre-teen. But I also think that, you know, it's time for us to get much more sophisticated about this.
GROSS: I want to talk with you a little bit about suicide since you brought it up. And I want to ask you first - just in terms of our show, we always give warnings when we're going to be talking about suicide. And we always give the suicide prevention hotline number, the idea being that hearing talk about suicide can almost be encouraging to someone who has had suicidal ideation. So do you think that's helpful?
KOPLEWICZ: Well, I think it's important to recognize that even if it's a small percentage, to give people that information - that lifeline is very important - and also to let them know that they're not alone. So I think the way to think about this is, why are teenagers so much more at risk than you or me? And the way to think about a teenager is, they feel everything. They're boiling. They're freezing. I hate you. I love you. You know, what happened to I'm warm or it's a little cool in here? That doesn't happen. And in some ways, it's really kind of terrific because they are so creative and they see opportunity everywhere. And they don't recognize risk very well.
I mean, there's some really interesting studies of a teenage boy who goes and picks up a friend to come into his car. And the teenager driver is wearing a seatbelt, and the teenage male who sits down next to him doesn't put a seatbelt on, and the teenage driver takes his seatbelt off. He goes and picks up a girl, and the girl gets into the car and she puts her seatbelt on, and the teenage driver now puts his seatbelt on.
So they're very easily moved by their peer group in a way that they hadn't been before. And parents should note this, that even though the peer group becomes significantly more influential when you're a teenager, parents are still the most influential factor in a kid's life. But it's important that parents keep talking, keep sharing their viewpoint, keep listening to their kid's viewpoint and not back off because their kids say, well, everyone's doing it.
GROSS: A child comes into your office, let's say a teenager comes into your office. You think that the possibility of this teenager attempting suicide is real. What do you do to try to prevent that from happening?
KOPLEWICZ: Well, it really depends on how serious they are about the attempt. Do they have a plan? Have they been thinking about it a long time? Have they stopped doing their usual pleasurable experiences? They no longer are hanging out with friends or not eating the food that they love. And you have to really recognize that if they are very serious about it, you have to intervene. You have to save their lives. You have to either say to them, I don't feel you're safe, or ask them if they feel safe, and then sometimes make the decision that they have to be in an environment where they'll be watched, in a hospital. Or you'll talk to their parents and see can they watch them until this mood and this ideation actually passes.
GROSS: So I just want to pause here and give the national Suicide and Crisis hotline number. And this is the number to call or to text. It's 988, so it's a simple number. Just three numbers, 988, to either call or text the national Suicide and Crisis hotline. So if you are having thoughts of suicide, please get some help. Well, let me reintroduce you. If you're just joining us, my guest is Harold Koplewicz and he is a child psychiatrist, the founding president of the Child Mind Institute. His books include "Scaffold Parenting: Raising Resilient, Self-Reliant, And Secure Kids In An Age Of Anxiety." We have to take a short break here, and we'll be right back. This is FRESH AIR.
(SOUNDBITE OF MUSIC)
GROSS: This is FRESH AIR. Let's get back to my interview with Dr. Harold Koplewicz. He is a child psychiatrist, he's the founding president of the Child Mind Institute, and his books include "Scaffold Parenting: Raising Resilient, Self-Reliant, And Secure Kids In An Age Of Anxiety."
You specialize in ADHD - attention-deficit/hyperactivity disorder. Why don't you define what the symptoms are and how to recognize it?
KOPLEWICZ: So it's a challenge for lots of people to think about it because they think, oh, aren't we all hyperactive at some time? But the difference here is a deficit in attention toward what's normal developmentally. So the attention span of a 5-year-old is very different than the attention span of a 10-year-old. But any individual who has ADHD is chronically less attentive, tends to be more impulsive, and if they have hyperactivity, they're moving around more. They can get themselves into physical problems because they basically have ants in their pants. They're constantly in motion. The diagnosis when you have hyperactivity is much easier to make than when you just have ADD without H. But it's a chronic illness, and therefore, it may change over time. Your symptoms might lessen. Hyperactivity might go away when you become a teenager. But you are always going to have a shorter attention span and going to be more impulsive than the average person your age.
GROSS: I think this is one of the problems in which brain imaging is starting to be used - fMRIs, where you can see, like, which parts of the brain light up in different situations and different thoughts. How are fMRIs being used in ADHD?
KOPLEWICZ: Right. It's the holy grail for us to find that objective test. One of the things we've discovered at the Child Mind Institute is that the way your brain connects to itself while a child's at rest turns out to be diagnostic. It's called connectomes. So does the front of the brain connect to the side of the brain or to the back of the brain?
And what's been very interesting is that we took a few hundred scans and sent them to a group of people who were statisticians, who were electrical engineers, and asked them if they could group those different scans in different buckets. And we found the group that actually won this competition were statisticians from Hopkins. And they said, well, these 150 scans go together, and these 50 scans go together, and these hundred scans go together. And these are individuals who have never seen a patient with psychiatric disorder. But what's really interesting - in bucket one, the overwhelming majority of those patients had ADHD. In the group of 50, they had autism. And the group of a hundred, they had both ADHD and autism. So we're really excited by the fact that we have found something that might lead us to a definitive, objective test.
Now, the important part for everyone to remember - it's not just one child. It's not a strep test - yes, you're positive or someone else is negative. It's a group difference. But that's the way we're going to get closer and closer to making a definitive diagnosis.
GROSS: So in a study like the fMRI study that you were referring to, how do you know whether the brain is reflecting the behavior or whether the behavior is predetermined by the brain? Do you know what I mean?
KOPLEWICZ: Sure. Well, it's...
GROSS: It's, like, if I move my left arm - if I say, I'm going to move my left arm right now, and I'm doing it with intent, it's going to register on an fMRI, probably. But it's not like I have a disorder that's moving my left arm. It's, like, I've decided to behave this way, and it's registering in my brain.
KOPLEWICZ: So, you know, let's think about this for a second. This is exactly where the field of research in functional MRI has gone to. You know, they used to give a trigger to a kid. You know, pay attention to this while you're in the machine, or we're going to show you scary faces and see what happened to the brain. It turns out that the most powerful way of doing this is just letting kids rest or sleep in the functional MRI. And your brain is incredibly active while you're at rest or sleeping. And that's when you're going to see most of these connections. So in the case of the study, we weren't triggering them. We weren't saying, you know, this clearly should be what makes the - you know, we'll catch them being inattentive, and then we'll look at the MRI. We're just looking at their brains at rest.
GROSS: Oh, that's really interesting. So has this affected your treatment at all?
KOPLEWICZ: So we're not there yet. You know, it's not ready for prime time. I wish it - you know, I could say, oh, we're going to give everyone EEGs, because they're only 60 bucks, and an MRI is 500, and we found some correlation. That's what I'm hoping for. But, you know, science has to wait for real data. So at this moment, we still have to rely on clinical diagnosis. You're asking parents what they think. You're asking teachers and report cards, because this is not something that just pops up when you're about to apply to college or because you didn't make partner at the law firm. This is a lifelong illness. And you can document that by looking at things from a longitudinal basis.
And then you have to examine the child. The child basically confirms the diagnosis or doesn't. I think it's fascinating when you do give a kid meds, and they do significantly better, that a young child will tell you the medicine's not working. And you say, really? What's changed? He said, my teacher is much nicer. I said, that's really interesting.
GROSS: (Laughter).
KOPLEWICZ: You take a pill and your kid - your teacher's much nicer. That really is absolutely amazing. And they said, yeah. You know, you're 8 years old. OK.
GROSS: Well, we need to take another break here, so let me reintroduce you. If you're just joining us, my guest is Dr. Harold Koplewicz. He's a child psychiatrist. He's the founding president of the Child Mind Institute. And his books include "Scaffold Parenting: Raising Resilient, Self-Reliant And Secure Kids In An Age Of Anxiety." We'll be right back after a short break. I'm Terry Gross, and this is FRESH AIR.
GROSS: This is FRESH AIR. I'm Terry Gross. Let's get back to my interview with Dr. Harold Koplewicz. He's a child psychiatrist and the founding president of the Child Mind Institute. His books include "Scaffold Parenting: Raising Resilient, Self-Reliant, And Secure Kids In An Age Of Anxiety." Your middle son has dyslexia. No one realized it at first. How did you discover what it was? Because this is, I assume, one of the issues that you treat as a child psychiatrist.
KOPLEWICZ: Right. Well, I think dyslexia has very often been put into another category until about the last 25 years, so that it was something educational experts did and not necessarily child psychiatrists. And brain scans and functional MRIs have changed that, but in the case of our family, he was 4 years old. We were visiting his grandmother for a day, and she was a pretty neutral individual, very careful not to say anything critical or even say anything overly praising, and she mentioned that she had trouble understanding him. And we said, Well, you know, his articulation isn't great. And she said, no, his stories are out of sequence, and I don't think he knows my name. I love listening to him, but everything seems a little mixed up. And I was the one who said, you know, we should listen to grandma here.
And we went on this journey to figure out what was wrong. We had him tested, and the tester said, oh, he's very bright. Well, at 4 years old, you don't read on these kinds of neuropsych testing, but she did mention that he had some word retrieval problems and that he couldn't name certain things, and she was concerned that maybe he didn't recognize the alphabet. And I remember at the time saying, What do we do about it? And she said, well, it's going to cost a lot of money, and it's going to take a lot of time. And I thought, well, he's 4 years old. He has a lot of time. And for this, we'll find a lot of money. We'll mortgage our house. He's got to learn how to read.
So we went on this journey, and it turned out that we wasted a lot of time. There were a lot of dead ends where we thought we were doing well, but it turns out he was memorizing words, that he couldn't decode the language. He couldn't tell the difference between Sally, Susan, and Sarah. And it was only by third grade, when math turned into word problems, that we saw how frustrated he was and how he recognized that he was ahead of kids in math but way behind them in reading, and he knew this was happening. And that gave us the moment to reevaluate and figure out a more evidence-based approach.
GROSS: Which was?
KOPLEWICZ: Well, it turns out that a multisensory approach to learning how to read, teaching kids the sounds of the language, brother sounds, what your lips look like, and there was a program called Lindamood-Bell, which is now in 50 states, and it's very intensive. You spend 4 hours a day doing these exercises with a different tutor every hour, and then you do another 30 minutes or 40 minutes of homework. And they basically teach you how to break the code, that the rest of us are learning how to read with only one side of our brain, and they are teaching you how to read thinking that, you know, your brain thinks it's Italian or Spanish, that you're learning a foreign language. It's really a remarkable intervention.
GROSS: I'm going to stop you. What do you mean by that, that your brain thinks you're learning a foreign language?
KOPLEWICZ: When we learn a foreign language, we use both sides of our brain. When we're learning...
GROSS: We do?
KOPLEWICZ: Yes.
GROSS: (Laughter). I hadn't heard that before.
KOPLEWICZ: Right. So when we're learning our native language, we activate one side of the brain, and kids with dyslexia underactivate that brain. And so when you teach them a new way of learning, it's like teaching them a foreign language, and so when you check what's going on in a functional MRI, they're lighting up both sides of their brain. The thing that's really awful about dyslexia, as far as I'm concerned, is what it does to kids' self-esteem. You know, once a year, I get to interview someone who's struggled with it, whether it's Orlando Bloom or Ari Emanuel or, you know, Lorraine Bracco, and you hear how bad they felt about themselves.
Think about it. Every day, you go to work, and every day, you feel like a failure, so it's not surprising that you think you're stupid or that you don't want to be there. And what they - all these successful people have in common is a great mom. You know, Barbara Corcoran has it, and she told me that the nuns were really giving her a tough time in parochial school. And her mother said, don't listen to the nuns. You are not stupid. They're stupid. Well, having a mom who's telling you you're still bright or Orlando Bloom's mom, who said, let's do poetry - you know, those are these great moms who are basically saying, I'm on your side, and we're going to figure this out. But for those who don't have those moms, school is impossible. There's high school dropout rates. There are high rates of getting involved in the juvenile justice system because you're not in school. And when we look at the juvenile justice system, we see that 70% of the inmates have dyslexia.
GROSS: You know, I used to think that dyslexia was a problem with, like, reversing words, so you'd have to read slowly 'cause words would get reversed in your mind, but it's much more profound than that. Can you give us, like, the latest understanding of what dyslexia is?
KOPLEWICZ: Sure. So that's a myth, you know, the d, the b. What it really is, first of all, it's a brain-based disorder, and there's two major symptoms. One is alphabet recognition, being able to look at the A and knowing it's an A and looking at the D and knowing it's a D. And we all learned that, kind of, you know, very easily. And the other (inaudible) awareness, hearing the sounds of the language, being able to say to yourself or let your brain recognize that S-L-O-W comes out slow and S-H-O-W comes out show. And so you have to be able to hear those two different phonemes. And I will tell you that now that America is recognizing that this kind of evidence-based learning is really important, that we have to teach kids phonemes, we have to teach them how to read no matter who they are, we are really addressing this in an earlier age, so kids who have dyslexia will be picked up sooner and will be able to get interventions that are more effective, again, before it affects their self-esteem.
GROSS: So let me reintroduce you here. If you're just joining us, my guest is Doctor Harold Koplewicz. He's a child psychiatrist, author of the book "Scaffold Parenting: Raising Resilient, Self-Reliant And Secure Kids In An Age of Anxiety" and founding president of the Child Mind Institute. We'll be right back. This is FRESH AIR.
GROSS: This is FRESH AIR. Let's get back to my interview with Dr. Harold Koplewicz, the founding president of the Child Mind Institute, author of the book "Scaffold Parenting: Raising Resilient, Self-Reliant And Secure Kids In An Age Of Anxiety." He's a child psychiatrist and has been one for how many years?
KOPLEWICZ: Almost 40.
GROSS: OK. So this is a kind of personal question, but knowing what you know now - and there's so much more research that's been done into childhood, you know, behavioral problems and mental health disorders - do you think you had any undiagnosed problems as a child?
KOPLEWICZ: I don't think so, but...
GROSS: And I don't mean that, like...
KOPLEWICZ: No, no, no.
GROSS: ...I recognize symptoms in (laughter)...
KOPLEWICZ: No, no, no. Yeah.
GROSS: ...In how you're behaving...
KOPLEWICZ: I - but I know - but I would tell you that I clearly became much more of a student when I was in college than I was in high school. I had Eastern European parents. I had parents who survived the Holocaust and got to the United States in 1949. And they didn't believe that education was a journey. It was a destination. And they couldn't wait until, you know, you graduated and go to college. And so I was two years younger than everyone in elementary school. And I think that was most probably not a great idea - that most boys developed, you know, late. And so that was a problem.
And I would also tell you that, you know, the parents that I had when I was growing up were much more traumatized by the Holocaust than the parents I had later on in life, when they were in their 80s and 90s and were less anxious and the nightmares had stopped and they felt more comfortable in the United States - and also comfortable that, you know, I was going to be successful. I had graduated medical school. I had children. They - I was married. And that seemed to really calm them down.
But I do recognize that they were overly invested in my being successful because they were trying to recreate stuff that they lost. My parents were both - by the way, my father had graduated law school in 1936, and my mother was in law school in 1938. And neither one of them ever practiced law. They came to this country as immigrants. They had to start all fresh again. My father started a business. I think they struggled financially. My mother eventually went back to school and got a B.A. and then an MSW. But there was this idea of what could have been if there wouldn't have been the Holocaust. And therefore, my sister and I had to carry, you know, that weight, which is, you know, understandable but was very unpleasant when it was happening.
GROSS: Were your parents in camps?
KOPLEWICZ: My father was literally in 14 concentration camps and the Warsaw Ghetto. And how is that possible? Well, at the very first camp, they asked, who knows how to make airplanes? And my father raised his hand. And when asked about that, he said, well, they had already killed the lawyers. And he figured, well, I know how to use a screwdriver. I'll figure it out. And he went from camp to camp. And he was with one other man who kept being moved with him, and they got a little piece of metal. And the other guy was very artistic, and he engraved a sailboat and a horn of plenty. And on the other side, every time they moved from one camp to another, my father inscribed the date and the name of the camp. And they were hoping that it would be at least a record, that what they were experiencing would be recorded and documented. And that piece of metal, by the way, is at the U.S. Holocaust Museum in New York - I'm sorry, in D.C., in Washington...
GROSS: Yeah.
KOPLEWICZ: ...D.C.
GROSS: Yeah. So you mentioned your - so your mother was in camps, too?
KOPLEWICZ: No. My mother got papers as a Catholic and - false papers as a Catholic and walked out of the ghetto. And in some ways, it was more trying for her in the respect that - think about it. You have fake papers, and if the Gestapo stops you and starts really examining the papers and starts asking you questions like, what is your mother and father's name? Oh, they're dead. OK. And what was your priest's name? And where are you from? It wouldn't take very long.
So she moved around 16 different villages, outside of Warsaw, working as a maid. And she was a terrible housekeeper, so it is really amazing how she managed to do that, because she - you know, she really had a very tough time and was very isolated and just basically, you know, surviving from day to day. And it was, I think, a little more than two years where she was moving around. The war ended first in Poland. And so my father didn't come and find her until several months later.
GROSS: Oh, they were married before the war started.
KOPLEWICZ: Well, I wish I could tell you that's true, and that was the story I was told. But it turns out that when my then-12-year-old son was doing a - my wife insisted that if he was going to be bar mitzvahed, it had to be intergenerational. So he kept asking my mother her life story and recording it. And at a certain point, my son said, I don't understand, Grandma. Where was the infrastructure in the ghetto for you to get married? And my mother said, oh, you know, in the Jewish religion, you can get married and become the stars and the moon. And my son said, I don't think that's true. I think you need a contract.
KOPLEWICZ: And she said, well, August 12. It was the day I lost my virginity with your grandfather. And he came home and said, I don't know if Grandma and Grandpa ever were married. I think they're celebrating the day they had sex. So I called my mother and said, I don't understand. Why did you tell him that? She said, I never slept with anybody else, and I thought, enough. And he asked much better questions than you ever did.
KOPLEWICZ: So I think they got married when they were leaving Poland to go to a displaced persons camp in Germany. But - and I have to tell you as an example, their people - my mother was madly in love with my father before the war. You know, she lusted for him. He was very attractive, and he was a lawyer already. And then after the war, when he returned, he was skin and bones. And, you know, he was truly a different person. And she was a different person. She was no longer a bit of a princess. She was a survivor. She knew hard (ph) - and she - he came and found her. And she said, I'm going to let you come in, but I'm leaving. I've got papers to go either to Palestine or to Australia or Canada or the United States. I'm not staying here. And he said, well, I am staying here. I'm a lawyer, and we're going to make a lot of money. And she said, that's OK.
The idea that they lived together for three months and she got the papers and he decided to go with her - it's really a very romantic story that they fell in love again. And my father, every year on their anniversary, would give my mother - if they had money, he gave her a red rose for every year they were together and three white roses for the three years they weren't together with the same note - life had no color without you. So they really rediscovered each other and I think gave - that bond was so close. In some ways, my sister and I sometimes felt out of it because they were such a partnership that that's what carried them through later on.
GROSS: What impact do you think it had on you as a child to know that they were having these nightmares, these concentration camp...
KOPLEWICZ: Oh, it was nightmares.
GROSS: ...Or posing-as-a-Catholic kind of nightmares? Did they tell you about that? Could you sense it? And in the same mode there, like, did they let on what they had experienced and how traumatic it was?
KOPLEWICZ: So the stories were never consistent or chronological, so you only got bits and pieces. You know, something about the showers - right? - that one of my grandmothers died in the showers. You know, I hate to tell you that they didn't explain the camps to me, but you also knew that they were so upset by it that you didn't pursue it. You didn't ask them a lot of things. And I can certainly tell you that since they weren't very Jewish by education or training, the holidays were just terrible. I mean, you know, most people light a memorial candle for all the people that have died in their family. Well, all their brothers and sisters and their parents and their cousins, so that, you know, there were, like, 10 yahrzeit candles, these memorial candles, but they weren't kept in the kitchen. Like, all the ghosts were on the dining room table for Rosh Hashanah or Yom Kippur. And it's kind of amazing the transformation they made over time - that, you know, they were literally able to become more stable and calmer and more effective as adults.
GROSS: You must have grown up with a very dark view of life.
KOPLEWICZ: At times, yes. You know, at time, yes. And yet the amazing part about my parents were they couldn't care less about material things. So other kids would live in houses near us in Queens and then in Nassau County, where the slip covers, plastic slip covers were put on the furniture, and my mother would say, What are they waiting for? You know, they'll be dead. If something broke in our house, my mother never cared about it. I mean, it really gave them a whole different attitude about what was important, and certainly, material things were not important to my parents. They had lost a lot because they stayed. You know, I used to say, why didn't you come to America, for God's sakes? and my mother would say, Al Capone and peasants - they came to America, not - you know, not the intelligentsia. You know, she's kind of snobby about, you know, her academic credentials and who her family was, but, you know, they lost a lot because they didn't want to leave property or whatever it was or the life that they had.
GROSS: So one last question. You know, some parents really want to be their children's best friend, and some parents really want to maintain their stature as the authority figure, not the best friend. And in terms of being a parent yourself, I'm curious where you fit on that spectrum, if you are comfortable talking about that.
KOPLEWICZ: Sure. Well, I'm not my kid's best friend, you know, and that's OK, because even though they're all adults now, which is a whole different kind of relationship... I mean, my children are 41, 37, and 35. It really is frightening...
KOPLEWICZ: ...To see that one of my kids has gray hair. You know, it's like, how did this happen? Because I'm still 35. You know, but all along, I think there is this pull that you certainly want your kids to love you because you love them so much, but it's OK for them not to like you because you do have to protect them. And when you protect them, there are certain things that they want to do that you know are dangerous for them or are just not good for them or not healthy for them. And so I think it's very hard, if not impossible, to be a friend, which is be a peer - right? - and share the same point of view and not have control. Your friend does not have control over you. It's much more equal. And I don't think that's possible as a parent. I think the best type of parenting, by the way, is an authoritative parent who has a lot of warmth but has a lot of control. So both the kid and the parent know, at the end of the day, the parent is going to make the decision, maybe with input from the child. But at the end of the day, it's not a democracy. It's going to be the parent who has the responsibility to make those decisions.
GROSS: Dr. Harold Koplewicz, thank you so much for talking with us.
KOPLEWICZ: Oh, it's been a pleasure, Terry.
GROSS: Dr. Harold Koplewicz is the founding president of the Child Mind Institute. His latest book is titled "Scaffold Parenting." After we take a short break, Justin Chang reviews what he describes as a marvelous new movie. This is FRESH AIR.
(SOUNDBITE OF BABO VALDES TRIO'S "LAMENTO CUBANO")
Copyright © 2024 NPR. All rights reserved. Visit our website terms of use and permissions pages at www.npr.org for further information.
NPR transcripts are created on a rush deadline by an NPR contractor. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of NPR’s programming is the audio record.

IMAGES
VIDEO
COMMENTS
Smoking can cause harm throughout the body, including the heart, brain, and lungs. This article discusses why smoking is bad for health and reasons to quit.
Smoking is like a slow death. There are various examples of the harms of smoking. Such as smoking causes lung cancer, heart disease, stroke, asthma, and a wide variety of other diseases. You might be interested: Essay on Why Trees are Important in our Life. Smokers have more coughs and colds than non-smokers.
Smoking is the practice of inhaling smoke from burning plant material. Nicotine works on your brain to create a relaxing, pleasurable feeling that makes it tough to quit. But smoking tobacco puts you at risk for cancer, stroke, heart attack, lung disease and other health issues. Nicotine replacements and lifestyle changes may help you quit.
500 Words Essay On Smoking. One of the most common problems we are facing in today's world which is killing people is smoking. A lot of people pick up this habit because of stress, personal issues and more. In fact, some even begin showing it off. When someone smokes a cigarette, they not only hurt themselves but everyone around them.
Introduction. More and more people become addicted to smoking every year. However, few of them are aware of the health damages all smokers may face in a long-term perspective. Smoking causes such incurable diseases as cancer, diabetes, asthma, or blindness. That is why many people nowadays substitute tobacco cigarettes with something they ...
Smoking causes stroke and coronary heart disease, which are among the leading causes of death in the United States. 1,3. Even people who smoke fewer than five cigarettes a day can have early signs of cardiovascular disease. 1. Smoking damages blood vessels and can make them thicken and grow narrower.
Background and objectives: Despite reductions in prevalence in recent years, tobacco smoking remains one of the main preventable causes of ill-health and premature death worldwide.This paper reviews the extent and nature of harms caused by smoking, the benefits of stopping, patterns of smoking, psychological, pharmacological and social factors that contribute to uptake and maintenance of ...
This damages the blood vessels. Smoking can result in stroke and heart attacks since it hinders blood flow, interrupting oxygen to various parts of the body, such as feet and hands. Introduction of cigarettes with low tar does not reduce these effects since smokers often prefer deeper puffs and hold the smoke in lungs for a long period.
Even among smokers who have quit, chronic lung disease still accounts for 50% of smoking-related conditions. 4. Smoking harms nearly every organ in the body, and is a main cause of lung cancer and COPD. It also is a cause of coronary heart disease, stroke and a host of other cancers and diseases. 1See more of the health effects caused by smoking.
Almost 35 years ago, the Office of the Surgeon General of the United States Health Service reviewed over 7000 research papers on the topic of smoking and health, and publicly recognized the role of smoking in various diseases, including lung cancer. Since then, numerous studies have been published that substantiate the strong association of ...
250 Words Essay on Negative Effects Of Smoking Introduction. Smoking is a harmful habit that many people around the world have. It is bad for our health and the environment. This essay will talk about the negative effects of smoking. Damages to Health. Smoking hurts our bodies in many ways. It is the main cause of lung cancer.
Health Effects. Smoking leads to disease and disability and harms nearly every organ of the body. More than 16 million Americans are living with a disease caused by smoking. For every person who dies because of smoking, at least 30 people live with a serious smoking-related illness. Smoking causes cancer, heart disease, stroke, lung diseases ...
Smoking and Its Negative Effects on Human Beings. Therefore, people need to be made aware of dental and other health problems they are likely to experience as a result of smoking. Hookah Smoking and Its Risks. The third component of a hookah is the hose. This is located at the bottom of the hookah and acts as a base.
Tobacco use is a global epidemic among young people. As with adults, it poses a serious health threat to youth and young adults in the United States and has significant implications for this nation's public and economic health in the future (Perry et al. 1994; Kessler 1995). The impact of cigarette smoking and other tobacco use on chronic disease, which accounts for 75% of American spending ...
It can also kill your family. You can die from cancer by smoking. Every time you smoke you are exposing toxic chemicals to the air which somebody else is going to breath and possibly die from. For example, you are putting people at risk every time you smoke. Because not only can it harm other people who inhale it, it also harms the people who ...
Persuasive Essay Examples About Smoking. Smoking is one of the leading causes of preventable death in the world. It leads to adverse health effects, including lung cancer, heart disease, and damage to the respiratory tract. However, the number of people who smoke cigarettes has been on the rise globally. A lot has been written on topics related ...
Smoking has a multitude of detrimental physiological, psychological, and social effects that can have a significant negative impact on a person's life. Smoking can have a negative impact on our health. Smoking has a major negative influence on the lungs. Smoking is the primary cause of one-third of all cancer cases.
Smoking can bring about lethal infections, for example, pneumonia, lung growth and emphysema. Additionally smoking causes 83% of deaths from chronic obstructive pulmonary disease (COPD) and smoking causes 84% of deaths from lung cancer (NHS , 2017) . However, there is a considerable measure of terrible illnesses connected to smoking cigarettes.
Essays on Smoking. Essay-writers in each smoking essay emphasize the dangers of smoking, and fairly so. After all, smoking is one of the most widespread bad habits in the world - there are about 2 billion smokers worldwide. It is a detrimental habit, as cigarette smoke contains more than 30 toxic components - you can go into them one by one ...
CNN —. Mark another point against smoking: It may cause an increase in a type of body fat linked to serious disease, according to a new study. Both starting smoking and spending a lifetime ...
Smoking: Causes and Effects Essay. Among numerous bad habits of modern society smoking seems to be of the greatest importance. Not only does it affect the person who smokes, but also those who are around him. Many people argue about the appropriate definition of smoking, whether it is a disease or just a bad habit.
Experts especially worry about the mental health impacts for teenagers. Some 17 percent of tenth graders report using cannabis, even though no state has legalized the drug for anyone under 21.
As a leading behavioral risk factor for numerous health outcomes, smoking is a major ongoing public health challenge. Although evidence on the health effects of smoking has been widely reported, few attempts have evaluated the dose-response relationship between smoking and a diverse range of health outcomes systematically and comprehensively.
Smoking. Multiple studies have found that smoking is associated with premature aging of skin. The chemicals in cigarettes have been found to accelerate skin aging, which causes your skin to become ...
If you're wondering whether edibles are a better bet than smoking weed…yes, but they still pose a risk to your heart. They pay me to tell you the bad news, so, straightforwardly: Maybe a ...
By MATTHEW PERRONE (AP Health Writer) WASHINGTON (AP) — Anti-smoking groups sued the U.S. government Tuesday over a long-awaited ban on menthol cigarettes, which has been idling at the White …
41%. Percentage of teens with the highest social media use who rate their overall mental health as poor or very poor, compared with 23% of those with the lowest use. For example, 10% of the highest use group expressed suicidal intent or self-harm in the past 12 months compared with 5% of the lowest use group, and 17% of the highest users expressed poor body image compared with 6% of the lowest ...
The topic of passive or involuntary smoking was first addressed in the 1972 U.S. Surgeon General's report (The Health Consequences of Smoking, U.S. Department of Health, Education, and Welfare [USDHEW] 1972), only eight years after the first Surgeon General's report on the health consequences of active smoking (USDHEW 1964). Surgeon General Dr. Jesse Steinfeld had raised concerns about ...
But LaKosky and others think something else may be at play, too: Drug users are shifting from injecting to smoking. A recent CDC report found that between early 2020 and late 2022, the percentage ...
So I want to be clear that social media is not like smoking. It doesn't - it's not terrible for everyone. But it is particularly bad for kids who have mental health disorders.