Essay on Addiction for Students and Children
500 words essay on addiction.
As we all know that excess of anything can be very dangerous, the same way, addiction of any kind can hamper the life quality of an individual. The phrase states that addiction is a family disease as one person uses and the whole family suffers. The above statement stands true in all its essence as the addict does not merely suffer but the people around him suffer greatly too. However, that does not mean they can’t be helped. Addiction is curable and we must not give up on the person who is addicted, rather help them out for a better life.


Cost of Addiction
Addiction comes at a great cost and we need to be able to recognize its harmful consequences to not let ourselves or anyone become an addict. Firstly, addiction has major health hazards. Intake of anything is bad for our body , and it does not matter what type of addiction it is, it will always impact the mental and physical health of a person.
For instance, if you are addicted to drugs or food, you will get various diseases and illnesses. Similarly, if you are addicted to video games, your mental health will also suffer along with physical health.
Moreover, people who are addicts usually face monetary issues. As they use that thing in excess, they spend loads of money on it. People become obsessed with spending all their fortunes on that one thing to satisfy their addiction. Thus, all these addictions of drugs , alcohol , gambling, and more drain the finances of a person and they usually end up in debt or even worse.
Furthermore, the personal and professional relationships of addicts suffer the most. They end up doing things or making decisions that do not work in their favor. This constraint the relationships of people and they drift apart.
Moreover, it also hampers their studies or work life. When you are spending all your money and time on your addiction, naturally your concentration levels in other things will drop. However, all this is not impossible to beat. There are many ways through which one can beat their addiction.
Get the huge list of more than 500 Essay Topics and Ideas
Beat Your Addiction
It is best to work towards beating your addiction rather than getting beat by it. One can try many ways to do so. Firstly, recognize and identify that you have an addiction problem. That is the first step to getting cured. You need to take some time and understand the symptoms in order to treat them. Motivate yourself to do better.
After that, understand that the journey will be long but worthwhile. Identify the triggers in your life and try to stay away from them as far as possible. There is no shame in asking for professional help. Always remember that professionals can always help you get better. Enroll yourself in rehabilitation programs and try to make the most out of them.
Most importantly, do not be hesitant in talking to your loved ones. Approach them and talk it out as they care most about you. They will surely help you get on the right path and help you in beating addiction for better health and life.
Q.1 What are the consequences of addiction?
A.1 Addiction has very severe consequences. Some of them are health hazards, monetary issues, relationship problems, adverse problems on studies and work of a person. It seriously hampers the quality of life of a person.
Q.2 How can one get rid of addiction?
A.2 A little help can go a long way. One can get rid of addiction by enrolling in rehabilitation programs and opening up about their struggle. Try to take professional help and talk with your close ones to become better.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 22 February 2021
Addiction as a brain disease revised: why it still matters, and the need for consilience
- Markus Heilig 1 ,
- James MacKillop ORCID: orcid.org/0000-0003-4118-9500 2 , 3 ,
- Diana Martinez 4 ,
- Jürgen Rehm ORCID: orcid.org/0000-0001-5665-0385 5 , 6 , 7 , 8 ,
- Lorenzo Leggio ORCID: orcid.org/0000-0001-7284-8754 9 &
- Louk J. M. J. Vanderschuren ORCID: orcid.org/0000-0002-5379-0363 10
Neuropsychopharmacology volume 46 , pages 1715–1723 ( 2021 ) Cite this article
84k Accesses
95 Citations
321 Altmetric
Metrics details
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that the brain disease view is deterministic, fails to account for heterogeneity in remission and recovery, places too much emphasis on a compulsive dimension of addiction, and that a specific neural signature of addiction has not been identified. We acknowledge that some of these criticisms have merit, but assert that the foundational premise that addiction has a neurobiological basis is fundamentally sound. We also emphasize that denying that addiction is a brain disease is a harmful standpoint since it contributes to reducing access to healthcare and treatment, the consequences of which are catastrophic. Here, we therefore address these criticisms, and in doing so provide a contemporary update of the brain disease view of addiction. We provide arguments to support this view, discuss why apparently spontaneous remission does not negate it, and how seemingly compulsive behaviors can co-exist with the sensitivity to alternative reinforcement in addiction. Most importantly, we argue that the brain is the biological substrate from which both addiction and the capacity for behavior change arise, arguing for an intensified neuroscientific study of recovery. More broadly, we propose that these disagreements reveal the need for multidisciplinary research that integrates neuroscientific, behavioral, clinical, and sociocultural perspectives.
Similar content being viewed by others
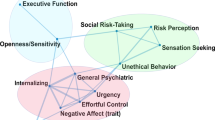
Subtypes in addiction and their neurobehavioral profiles across three functional domains
Gunner Drossel, Leyla R. Brucar, … Anna Zilverstand

Drug addiction: from bench to bedside
Julian Cheron & Alban de Kerchove d’Exaerde

The neurobiology of drug addiction: cross-species insights into the dysfunction and recovery of the prefrontal cortex
Ahmet O. Ceceli, Charles W. Bradberry & Rita Z. Goldstein
Introduction
Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that “addiction is a brain disease”, articulated a set of implications of this position, and outlined an agenda for realizing its promise [ 1 ]. The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the efforts of researchers, and resource allocation by funding agencies. A subsequent 2000 paper by McLellan et al. [ 2 ] examined whether data justify distinguishing addiction from other conditions for which a disease label is rarely questioned, such as diabetes, hypertension or asthma. It concluded that neither genetic risk, the role of personal choices, nor the influence of environmental factors differentiated addiction in a manner that would warrant viewing it differently; neither did relapse rates, nor compliance with treatment. The authors outlined an agenda closely related to that put forward by Leshner, but with a more clinical focus. Their conclusion was that addiction should be insured, treated, and evaluated like other diseases. This paper, too, has been exceptionally influential by academic standards, as witnessed by its ~3000 citations to date. What may be less appreciated among scientists is that its impact in the real world of addiction treatment has remained more limited, with large numbers of patients still not receiving evidence-based treatments.
In recent years, the conceptualization of addiction as a brain disease has come under increasing criticism. When first put forward, the brain disease view was mainly an attempt to articulate an effective response to prevailing nonscientific, moralizing, and stigmatizing attitudes to addiction. According to these attitudes, addiction was simply the result of a person’s moral failing or weakness of character, rather than a “real” disease [ 3 ]. These attitudes created barriers for people with substance use problems to access evidence-based treatments, both those available at the time, such as opioid agonist maintenance, cognitive behavioral therapy-based relapse prevention, community reinforcement or contingency management, and those that could result from research. To promote patient access to treatments, scientists needed to argue that there is a biological basis beneath the challenging behaviors of individuals suffering from addiction. This argument was particularly targeted to the public, policymakers and health care professionals, many of whom held that since addiction was a misery people brought upon themselves, it fell beyond the scope of medicine, and was neither amenable to treatment, nor warranted the use of taxpayer money.
Present-day criticism directed at the conceptualization of addiction as a brain disease is of a very different nature. It originates from within the scientific community itself, and asserts that this conceptualization is neither supported by data, nor helpful for people with substance use problems [ 4 , 5 , 6 , 7 , 8 ]. Addressing these critiques requires a very different perspective, and is the objective of our paper. We readily acknowledge that in some cases, recent critiques of the notion of addiction as a brain disease as postulated originally have merit, and that those critiques require the postulates to be re-assessed and refined. In other cases, we believe the arguments have less validity, but still provide an opportunity to update the position of addiction as a brain disease. Our overarching concern is that questionable arguments against the notion of addiction as a brain disease may harm patients, by impeding access to care, and slowing development of novel treatments.
A premise of our argument is that any useful conceptualization of addiction requires an understanding both of the brains involved, and of environmental factors that interact with those brains [ 9 ]. These environmental factors critically include availability of drugs, but also of healthy alternative rewards and opportunities. As we will show, stating that brain mechanisms are critical for understanding and treating addiction in no way negates the role of psychological, social and socioeconomic processes as both causes and consequences of substance use. To reflect this complex nature of addiction, we have assembled a team with expertise that spans from molecular neuroscience, through animal models of addiction, human brain imaging, clinical addiction medicine, to epidemiology. What brings us together is a passionate commitment to improving the lives of people with substance use problems through science and science-based treatments, with empirical evidence as the guiding principle.
To achieve this goal, we first discuss the nature of the disease concept itself, and why we believe it is important for the science and treatment of addiction. This is followed by a discussion of the main points raised when the notion of addiction as a brain disease has come under criticism. Key among those are claims that spontaneous remission rates are high; that a specific brain pathology is lacking; and that people suffering from addiction, rather than behaving “compulsively”, in fact show a preserved ability to make informed and advantageous choices. In the process of discussing these issues, we also address the common criticism that viewing addiction as a brain disease is a fully deterministic theory of addiction. For our argument, we use the term “addiction” as originally used by Leshner [ 1 ]; in Box 1 , we map out and discuss how this construct may relate to the current diagnostic categories, such as Substance Use Disorder (SUD) and its different levels of severity (Fig. 1) .
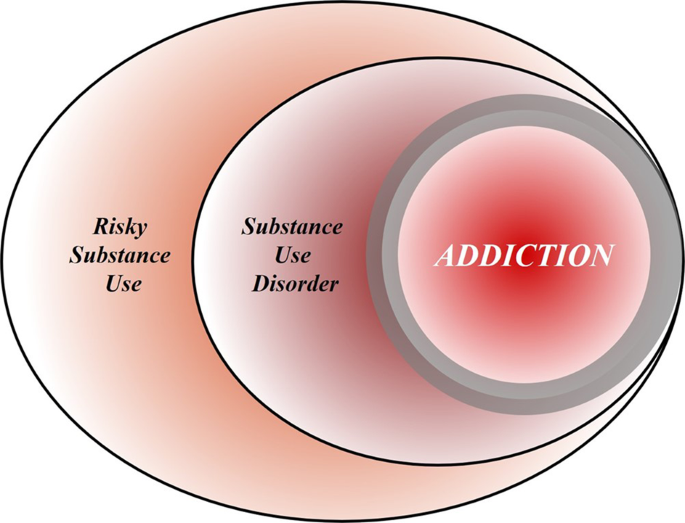
Risky (hazardous) substance use refers to quantity/frequency indicators of consumption; SUD refers to individuals who meet criteria for a DSM-5 diagnosis (mild, moderate, or severe); and addiction refers to individuals who exhibit persistent difficulties with self-regulation of drug consumption. Among high-risk individuals, a subgroup will meet criteria for SUD and, among those who have an SUD, a further subgroup would be considered to be addicted to the drug. However, the boundary for addiction is intentionally blurred to reflect that the dividing line for defining addiction within the category of SUD remains an open empirical question.
Box 1 What’s in a name? Differentiating hazardous use, substance use disorder, and addiction
Although our principal focus is on the brain disease model of addiction, the definition of addiction itself is a source of ambiguity. Here, we provide a perspective on the major forms of terminology in the field.
Hazardous Substance Use
Hazardous (risky) substance use refers to quantitative levels of consumption that increase an individual’s risk for adverse health consequences. In practice, this pertains to alcohol use [ 110 , 111 ]. Clinically, alcohol consumption that exceeds guidelines for moderate drinking has been used to prompt brief interventions or referral for specialist care [ 112 ]. More recently, a reduction in these quantitative levels has been validated as treatment endpoints [ 113 ].
Substance Use Disorder
SUD refers to the DSM-5 diagnosis category that encompasses significant impairment or distress resulting from specific categories of psychoactive drug use. The diagnosis of SUD is operationalized as 2 or more of 11 symptoms over the past year. As a result, the diagnosis is heterogenous, with more than 1100 symptom permutations possible. The diagnosis in DSM-5 is the result of combining two diagnoses from the DSM-IV, abuse and dependence, which proved to be less valid than a single dimensional approach [ 114 ]. Critically, SUD includes three levels of severity: mild (2–3 symptoms), moderate (4–5 symptoms), and severe (6+ symptoms). The International Classification of Diseases (ICD) system retains two diagnoses, harmful use (lower severity) and substance dependence (higher severity).
Addiction is a natural language concept, etymologically meaning enslavement, with the contemporary meaning traceable to the Middle and Late Roman Republic periods [ 115 ]. As a scientific construct, drug addiction can be defined as a state in which an individual exhibits an inability to self-regulate consumption of a substance, although it does not have an operational definition. Regarding clinical diagnosis, as it is typically used in scientific and clinical parlance, addiction is not synonymous with the simple presence of SUD. Nowhere in DSM-5 is it articulated that the diagnostic threshold (or any specific number/type of symptoms) should be interpreted as reflecting addiction, which inherently connotes a high degree of severity. Indeed, concerns were raised about setting the diagnostic standard too low because of the issue of potentially conflating a low-severity SUD with addiction [ 116 ]. In scientific and clinical usage, addiction typically refers to individuals at a moderate or high severity of SUD. This is consistent with the fact that moderate-to-severe SUD has the closest correspondence with the more severe diagnosis in ICD [ 117 , 118 , 119 ]. Nonetheless, akin to the undefined overlap between hazardous use and SUD, the field has not identified the exact thresholds of SUD symptoms above which addiction would be definitively present.
Integration
The ambiguous relationships among these terms contribute to misunderstandings and disagreements. Figure 1 provides a simple working model of how these terms overlap. Fundamentally, we consider that these terms represent successive dimensions of severity, clinical “nesting dolls”. Not all individuals consuming substances at hazardous levels have an SUD, but a subgroup do. Not all individuals with a SUD are addicted to the drug in question, but a subgroup are. At the severe end of the spectrum, these domains converge (heavy consumption, numerous symptoms, the unambiguous presence of addiction), but at low severity, the overlap is more modest. The exact mapping of addiction onto SUD is an open empirical question, warranting systematic study among scientists, clinicians, and patients with lived experience. No less important will be future research situating our definition of SUD using more objective indicators (e.g., [ 55 , 120 ]), brain-based and otherwise, and more precisely in relation to clinical needs [ 121 ]. Finally, such work should ultimately be codified in both the DSM and ICD systems to demarcate clearly where the attribution of addiction belongs within the clinical nosology, and to foster greater clarity and specificity in scientific discourse.
What is a disease?
In his classic 1960 book “The Disease Concept of Alcoholism”, Jellinek noted that in the alcohol field, the debate over the disease concept was plagued by too many definitions of “alcoholism” and too few definitions of “disease” [ 10 ]. He suggested that the addiction field needed to follow the rest of medicine in moving away from viewing disease as an “entity”, i.e., something that has “its own independent existence, apart from other things” [ 11 ]. To modern medicine, he pointed out, a disease is simply a label that is agreed upon to describe a cluster of substantial, deteriorating changes in the structure or function of the human body, and the accompanying deterioration in biopsychosocial functioning. Thus, he concluded that alcoholism can simply be defined as changes in structure or function of the body due to drinking that cause disability or death. A disease label is useful to identify groups of people with commonly co-occurring constellations of problems—syndromes—that significantly impair function, and that lead to clinically significant distress, harm, or both. This convention allows a systematic study of the condition, and of whether group members benefit from a specific intervention.
It is not trivial to delineate the exact category of harmful substance use for which a label such as addiction is warranted (See Box 1 ). Challenges to diagnostic categorization are not unique to addiction, however. Throughout clinical medicine, diagnostic cut-offs are set by consensus, commonly based on an evolving understanding of thresholds above which people tend to benefit from available interventions. Because assessing benefits in large patient groups over time is difficult, diagnostic thresholds are always subject to debate and adjustments. It can be debated whether diagnostic thresholds “merely” capture the extreme of a single underlying population, or actually identify a subpopulation that is at some level distinct. Resolving this issue remains challenging in addiction, but once again, this is not different from other areas of medicine [see e.g., [ 12 ] for type 2 diabetes]. Longitudinal studies that track patient trajectories over time may have a better ability to identify subpopulations than cross-sectional assessments [ 13 ].
By this pragmatic, clinical understanding of the disease concept, it is difficult to argue that “addiction” is unjustified as a disease label. Among people who use drugs or alcohol, some progress to using with a quantity and frequency that results in impaired function and often death, making substance use a major cause of global disease burden [ 14 ]. In these people, use occurs with a pattern that in milder forms may be challenging to capture by current diagnostic criteria (See Box 1 ), but is readily recognized by patients, their families and treatment providers when it reaches a severity that is clinically significant [see [ 15 ] for a classical discussion]. In some cases, such as opioid addiction, those who receive the diagnosis stand to obtain some of the greatest benefits from medical treatments in all of clinical medicine [ 16 , 17 ]. Although effect sizes of available treatments are more modest in nicotine [ 18 ] and alcohol addiction [ 19 ], the evidence supporting their efficacy is also indisputable. A view of addiction as a disease is justified, because it is beneficial: a failure to diagnose addiction drastically increases the risk of a failure to treat it [ 20 ].
Of course, establishing a diagnosis is not a requirement for interventions to be meaningful. People with hazardous or harmful substance use who have not (yet) developed addiction should also be identified, and interventions should be initiated to address their substance-related risks. This is particularly relevant for alcohol, where even in the absence of addiction, use is frequently associated with risks or harm to self, e.g., through cardiovascular disease, liver disease or cancer, and to others, e.g., through accidents or violence [ 21 ]. Interventions to reduce hazardous or harmful substance use in people who have not developed addiction are in fact particularly appealing. In these individuals, limited interventions are able to achieve robust and meaningful benefits [ 22 ], presumably because patterns of misuse have not yet become entrenched.
Thus, as originally pointed out by McLellan and colleagues, most of the criticisms of addiction as a disease could equally be applied to other medical conditions [ 2 ]. This type of criticism could also be applied to other psychiatric disorders, and that has indeed been the case historically [ 23 , 24 ]. Today, there is broad consensus that those criticisms were misguided. Few, if any healthcare professionals continue to maintain that schizophrenia, rather than being a disease, is a normal response to societal conditions. Why, then, do people continue to question if addiction is a disease, but not whether schizophrenia, major depressive disorder or post-traumatic stress disorder are diseases? This is particularly troubling given the decades of data showing high co-morbidity of addiction with these conditions [ 25 , 26 ]. We argue that it comes down to stigma. Dysregulated substance use continues to be perceived as a self-inflicted condition characterized by a lack of willpower, thus falling outside the scope of medicine and into that of morality [ 3 ].
Chronic and relapsing, developmentally-limited, or spontaneously remitting?
Much of the critique targeted at the conceptualization of addiction as a brain disease focuses on its original assertion that addiction is a chronic and relapsing condition. Epidemiological data are cited in support of the notion that large proportions of individuals achieve remission [ 27 ], frequently without any formal treatment [ 28 , 29 ] and in some cases resuming low risk substance use [ 30 ]. For instance, based on data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) study [ 27 ], it has been pointed out that a significant proportion of people with an addictive disorder quit each year, and that most afflicted individuals ultimately remit. These spontaneous remission rates are argued to invalidate the concept of a chronic, relapsing disease [ 4 ].
Interpreting these and similar data is complicated by several methodological and conceptual issues. First, people may appear to remit spontaneously because they actually do, but also because of limited test–retest reliability of the diagnosis [ 31 ]. For instance, using a validated diagnostic interview and trained interviewers, the Collaborative Studies on Genetics of Alcoholism examined the likelihood that an individual diagnosed with a lifetime history of substance dependence would retain this classification after 5 years. This is obviously a diagnosis that, once met, by definition cannot truly remit. Lifetime alcohol dependence was indeed stable in individuals recruited from addiction treatment units, ~90% for women, and 95% for men. In contrast, in a community-based sample similar to that used in the NESARC [ 27 ], stability was only ~30% and 65% for women and men, respectively. The most important characteristic that determined diagnostic stability was severity. Diagnosis was stable in severe, treatment-seeking cases, but not in general population cases of alcohol dependence.
These data suggest that commonly used diagnostic criteria alone are simply over-inclusive for a reliable, clinically meaningful diagnosis of addiction. They do identify a core group of treatment seeking individuals with a reliable diagnosis, but, if applied to nonclinical populations, also flag as “cases” a considerable halo of individuals for whom the diagnostic categorization is unreliable. Any meaningful discussion of remission rates needs to take this into account, and specify which of these two populations that is being discussed. Unfortunately, the DSM-5 has not made this task easier. With only 2 out of 11 symptoms being sufficient for a diagnosis of SUD, it captures under a single diagnostic label individuals in a “mild” category, whose diagnosis is likely to have very low test–retest reliability, and who are unlikely to exhibit a chronic relapsing course, together with people at the severe end of the spectrum, whose diagnosis is reliable, many of whom do show a chronic relapsing course.
The NESARC data nevertheless show that close to 10% of people in the general population who are diagnosed with alcohol addiction (here equated with DSM-IV “dependence” used in the NESARC study) never remitted throughout their participation in the survey. The base life-time prevalence of alcohol dependence in NESARC was 12.5% [ 32 ]. Thus, the data cited against the concept of addiction as a chronic relapsing disease in fact indicate that over 1% of the US population develops an alcohol-related condition that is associated with high morbidity and mortality, and whose chronic and/or relapsing nature cannot be disputed, since it does not remit.
Secondly, the analysis of NESARC data [ 4 , 27 ] omits opioid addiction, which, together with alcohol and tobacco, is the largest addiction-related public health problem in the US [ 33 ]. This is probably the addictive condition where an analysis of cumulative evidence most strikingly supports the notion of a chronic disorder with frequent relapses in a large proportion of people affected [ 34 ]. Of course, a large number of people with opioid addiction are unable to express the chronic, relapsing course of their disease, because over the long term, their mortality rate is about 15 times greater than that of the general population [ 35 ]. However, even among those who remain alive, the prevalence of stable abstinence from opioid use after 10–30 years of observation is <30%. Remission may not always require abstinence, for instance in the case of alcohol addiction, but is a reasonable proxy for remission with opioids, where return to controlled use is rare. Embedded in these data is a message of literally vital importance: when opioid addiction is diagnosed and treated as a chronic relapsing disease, outcomes are markedly improved, and retention in treatment is associated with a greater likelihood of abstinence.
The fact that significant numbers of individuals exhibit a chronic relapsing course does not negate that even larger numbers of individuals with SUD according to current diagnostic criteria do not. For instance, in many countries, the highest prevalence of substance use problems is found among young adults, aged 18–25 [ 36 ], and a majority of these ‘age out’ of excessive substance use [ 37 ]. It is also well documented that many individuals with SUD achieve longstanding remission, in many cases without any formal treatment (see e.g., [ 27 , 30 , 38 ]).
Collectively, the data show that the course of SUD, as defined by current diagnostic criteria, is highly heterogeneous. Accordingly, we do not maintain that a chronic relapsing course is a defining feature of SUD. When present in a patient, however, such as course is of clinical significance, because it identifies a need for long-term disease management [ 2 ], rather than expectations of a recovery that may not be within the individual’s reach [ 39 ]. From a conceptual standpoint, however, a chronic relapsing course is neither necessary nor implied in a view that addiction is a brain disease. This view also does not mean that it is irreversible and hopeless. Human neuroscience documents restoration of functioning after abstinence [ 40 , 41 ] and reveals predictors of clinical success [ 42 ]. If anything, this evidence suggests a need to increase efforts devoted to neuroscientific research on addiction recovery [ 40 , 43 ].
Lessons from genetics
For alcohol addiction, meta-analysis of twin and adoption studies has estimated heritability at ~50%, while estimates for opioid addiction are even higher [ 44 , 45 ]. Genetic risk factors are to a large extent shared across substances [ 46 ]. It has been argued that a genetic contribution cannot support a disease view of a behavior, because most behavioral traits, including religious and political inclinations, have a genetic contribution [ 4 ]. This statement, while correct in pointing out broad heritability of behavioral traits, misses a fundamental point. Genetic architecture is much like organ structure. The fact that normal anatomy shapes healthy organ function does not negate that an altered structure can contribute to pathophysiology of disease. The structure of the genetic landscape is no different. Critics further state that a “genetic predisposition is not a recipe for compulsion”, but no neuroscientist or geneticist would claim that genetic risk is “a recipe for compulsion”. Genetic risk is probabilistic, not deterministic. However, as we will see below, in the case of addiction, it contributes to large, consistent probability shifts towards maladaptive behavior.
In dismissing the relevance of genetic risk for addiction, Hall writes that “a large number of alleles are involved in the genetic susceptibility to addiction and individually these alleles might very weakly predict a risk of addiction”. He goes on to conclude that “generally, genetic prediction of the risk of disease (even with whole-genome sequencing data) is unlikely to be informative for most people who have a so-called average risk of developing an addiction disorder” [ 7 ]. This reflects a fundamental misunderstanding of polygenic risk. It is true that a large number of risk alleles are involved, and that the explanatory power of currently available polygenic risk scores for addictive disorders lags behind those for e.g., schizophrenia or major depression [ 47 , 48 ]. The only implication of this, however, is that low average effect sizes of risk alleles in addiction necessitate larger study samples to construct polygenic scores that account for a large proportion of the known heritability.
However, a heritability of addiction of ~50% indicates that DNA sequence variation accounts for 50% of the risk for this condition. Once whole genome sequencing is readily available, it is likely that it will be possible to identify most of that DNA variation. For clinical purposes, those polygenic scores will of course not replace an understanding of the intricate web of biological and social factors that promote or prevent expression of addiction in an individual case; rather, they will add to it [ 49 ]. Meanwhile, however, genome-wide association studies in addiction have already provided important information. For instance, they have established that the genetic underpinnings of alcohol addiction only partially overlap with those for alcohol consumption, underscoring the genetic distinction between pathological and nonpathological drinking behaviors [ 50 ].
It thus seems that, rather than negating a rationale for a disease view of addiction, the important implication of the polygenic nature of addiction risk is a very different one. Genome-wide association studies of complex traits have largely confirmed the century old “infinitisemal model” in which Fisher reconciled Mendelian and polygenic traits [ 51 ]. A key implication of this model is that genetic susceptibility for a complex, polygenic trait is continuously distributed in the population. This may seem antithetical to a view of addiction as a distinct disease category, but the contradiction is only apparent, and one that has long been familiar to quantitative genetics. Viewing addiction susceptibility as a polygenic quantitative trait, and addiction as a disease category is entirely in line with Falconer’s theorem, according to which, in a given set of environmental conditions, a certain level of genetic susceptibility will determine a threshold above which disease will arise.
A brain disease? Then show me the brain lesion!
The notion of addiction as a brain disease is commonly criticized with the argument that a specific pathognomonic brain lesion has not been identified. Indeed, brain imaging findings in addiction (perhaps with the exception of extensive neurotoxic gray matter loss in advanced alcohol addiction) are nowhere near the level of specificity and sensitivity required of clinical diagnostic tests. However, this criticism neglects the fact that neuroimaging is not used to diagnose many neurologic and psychiatric disorders, including epilepsy, ALS, migraine, Huntington’s disease, bipolar disorder, or schizophrenia. Even among conditions where signs of disease can be detected using brain imaging, such as Alzheimer’s and Parkinson’s disease, a scan is best used in conjunction with clinical acumen when making the diagnosis. Thus, the requirement that addiction be detectable with a brain scan in order to be classified as a disease does not recognize the role of neuroimaging in the clinic.
For the foreseeable future, the main objective of imaging in addiction research is not to diagnose addiction, but rather to improve our understanding of mechanisms that underlie it. The hope is that mechanistic insights will help bring forward new treatments, by identifying candidate targets for them, by pointing to treatment-responsive biomarkers, or both [ 52 ]. Developing innovative treatments is essential to address unmet treatment needs, in particular in stimulant and cannabis addiction, where no approved medications are currently available. Although the task to develop novel treatments is challenging, promising candidates await evaluation [ 53 ]. A particular opportunity for imaging-based research is related to the complex and heterogeneous nature of addictive disorders. Imaging-based biomarkers hold the promise of allowing this complexity to be deconstructed into specific functional domains, as proposed by the RDoC initiative [ 54 ] and its application to addiction [ 55 , 56 ]. This can ultimately guide the development of personalized medicine strategies to addiction treatment.
Countless imaging studies have reported differences in brain structure and function between people with addictive disorders and those without them. Meta-analyses of structural data show that alcohol addiction is associated with gray matter losses in the prefrontal cortex, dorsal striatum, insula, and posterior cingulate cortex [ 57 ], and similar results have been obtained in stimulant-addicted individuals [ 58 ]. Meta-analysis of functional imaging studies has demonstrated common alterations in dorsal striatal, and frontal circuits engaged in reward and salience processing, habit formation, and executive control, across different substances and task-paradigms [ 59 ]. Molecular imaging studies have shown that large and fast increases in dopamine are associated with the reinforcing effects of drugs of abuse, but that after chronic drug use and during withdrawal, brain dopamine function is markedly decreased and that these decreases are associated with dysfunction of prefrontal regions [ 60 ]. Collectively, these findings have given rise to a widely held view of addiction as a disorder of fronto-striatal circuitry that mediates top-down regulation of behavior [ 61 ].
Critics reply that none of the brain imaging findings are sufficiently specific to distinguish between addiction and its absence, and that they are typically obtained in cross-sectional studies that can at best establish correlative rather than causal links. In this, they are largely right, and an updated version of a conceptualization of addiction as a brain disease needs to acknowledge this. Many of the structural brain findings reported are not specific for addiction, but rather shared across psychiatric disorders [ 62 ]. Also, for now, the most sophisticated tools of human brain imaging remain crude in face of complex neural circuit function. Importantly however, a vast literature from animal studies also documents functional changes in fronto-striatal circuits, as well their limbic and midbrain inputs, associated with addictive behaviors [ 63 , 64 , 65 , 66 , 67 , 68 ]. These are circuits akin to those identified by neuroimaging studies in humans, implicated in positive and negative emotions, learning processes and executive functions, altered function of which is thought to underlie addiction. These animal studies, by virtue of their cellular and molecular level resolution, and their ability to establish causality under experimental control, are therefore an important complement to human neuroimaging work.
Nevertheless, factors that seem remote from the activity of brain circuits, such as policies, substance availability and cost, as well as socioeconomic factors, also are critically important determinants of substance use. In this complex landscape, is the brain really a defensible focal point for research and treatment? The answer is “yes”. As powerfully articulated by Francis Crick [ 69 ], “You, your joys and your sorrows, your memories and your ambitions, your sense of personal identity and free will, are in fact no more than the behavior of a vast assembly of nerve cells and their associated molecules”. Social and interpersonal factors are critically important in addiction, but they can only exert their influences by impacting neural processes. They must be encoded as sensory data, represented together with memories of the past and predictions about the future, and combined with representations of interoceptive and other influences to provide inputs to the valuation machinery of the brain. Collectively, these inputs drive action selection and execution of behavior—say, to drink or not to drink, and then, within an episode, to stop drinking or keep drinking. Stating that the pathophysiology of addiction is largely about the brain does not ignore the role of other influences. It is just the opposite: it is attempting to understand how those important influences contribute to drug seeking and taking in the context of the brain, and vice versa.
But if the criticism is one of emphasis rather than of principle—i.e., too much brain, too little social and environmental factors – then neuroscientists need to acknowledge that they are in part guilty as charged. Brain-centric accounts of addiction have for a long time failed to pay enough attention to the inputs that social factors provide to neural processing behind drug seeking and taking [ 9 ]. This landscape is, however, rapidly changing. For instance, using animal models, scientists are finding that lack of social play early in life increases the motivation to take addictive substances in adulthood [ 70 ]. Others find that the opportunity to interact with a fellow rat is protective against addiction-like behaviors [ 71 ]. In humans, a relationship has been found between perceived social support, socioeconomic status, and the availability of dopamine D2 receptors [ 72 , 73 ], a biological marker of addiction vulnerability. Those findings in turn provided translation of data from nonhuman primates, which showed that D2 receptor availability can be altered by changes in social hierarchy, and that these changes are associated with the motivation to obtain cocaine [ 74 ].
Epidemiologically, it is well established that social determinants of health, including major racial and ethnic disparities, play a significant role in the risk for addiction [ 75 , 76 ]. Contemporary neuroscience is illuminating how those factors penetrate the brain [ 77 ] and, in some cases, reveals pathways of resilience [ 78 ] and how evidence-based prevention can interrupt those adverse consequences [ 79 , 80 ]. In other words, from our perspective, viewing addiction as a brain disease in no way negates the importance of social determinants of health or societal inequalities as critical influences. In fact, as shown by the studies correlating dopamine receptors with social experience, imaging is capable of capturing the impact of the social environment on brain function. This provides a platform for understanding how those influences become embedded in the biology of the brain, which provides a biological roadmap for prevention and intervention.
We therefore argue that a contemporary view of addiction as a brain disease does not deny the influence of social, environmental, developmental, or socioeconomic processes, but rather proposes that the brain is the underlying material substrate upon which those factors impinge and from which the responses originate. Because of this, neurobiology is a critical level of analysis for understanding addiction, although certainly not the only one. It is recognized throughout modern medicine that a host of biological and non-biological factors give rise to disease; understanding the biological pathophysiology is critical for understanding etiology and informing treatment.
Is a view of addiction as a brain disease deterministic?
A common criticism of the notion that addiction is a brain disease is that it is reductionist and in the end therefore deterministic [ 81 , 82 ]. This is a fundamental misrepresentation. As indicated above, viewing addiction as a brain disease simply states that neurobiology is an undeniable component of addiction. A reason for deterministic interpretations may be that modern neuroscience emphasizes an understanding of proximal causality within research designs (e.g., whether an observed link between biological processes is mediated by a specific mechanism). That does not in any way reflect a superordinate assumption that neuroscience will achieve global causality. On the contrary, since we realize that addiction involves interactions between biology, environment and society, ultimate (complete) prediction of behavior based on an understanding of neural processes alone is neither expected, nor a goal.
A fairer representation of a contemporary neuroscience view is that it believes insights from neurobiology allow useful probabilistic models to be developed of the inherently stochastic processes involved in behavior [see [ 83 ] for an elegant recent example]. Changes in brain function and structure in addiction exert a powerful probabilistic influence over a person’s behavior, but one that is highly multifactorial, variable, and thus stochastic. Philosophically, this is best understood as being aligned with indeterminism, a perspective that has a deep history in philosophy and psychology [ 84 ]. In modern neuroscience, it refers to the position that the dynamic complexity of the brain, given the probabilistic threshold-gated nature of its biology (e.g., action potential depolarization, ion channel gating), means that behavior cannot be definitively predicted in any individual instance [ 85 , 86 ].
Driven by compulsion, or free to choose?
A major criticism of the brain disease view of addiction, and one that is related to the issue of determinism vs indeterminism, centers around the term “compulsivity” [ 6 , 87 , 88 , 89 , 90 ] and the different meanings it is given. Prominent addiction theories state that addiction is characterized by a transition from controlled to “compulsive” drug seeking and taking [ 91 , 92 , 93 , 94 , 95 ], but allocate somewhat different meanings to “compulsivity”. By some accounts, compulsive substance use is habitual and insensitive to its outcomes [ 92 , 94 , 96 ]. Others refer to compulsive use as a result of increasing incentive value of drug associated cues [ 97 ], while others view it as driven by a recruitment of systems that encode negative affective states [ 95 , 98 ].
The prototype for compulsive behavior is provided by obsessive-compulsive disorder (OCD), where compulsion refers to repeatedly and stereotypically carrying out actions that in themselves may be meaningful, but lose their purpose and become harmful when performed in excess, such as persistent handwashing until skin injuries result. Crucially, this happens despite a conscious desire to do otherwise. Attempts to resist these compulsions result in increasing and ultimately intractable anxiety [ 99 ]. This is in important ways different from the meaning of compulsivity as commonly used in addiction theories. In the addiction field, compulsive drug use typically refers to inflexible, drug-centered behavior in which substance use is insensitive to adverse consequences [ 100 ]. Although this phenomenon is not necessarily present in every patient, it reflects important symptoms of clinical addiction, and is captured by several DSM-5 criteria for SUD [ 101 ]. Examples are needle-sharing despite knowledge of a risk to contract HIV or Hepatitis C, drinking despite a knowledge of having liver cirrhosis, but also the neglect of social and professional activities that previously were more important than substance use. While these behaviors do show similarities with the compulsions of OCD, there are also important differences. For example, “compulsive” substance use is not necessarily accompanied by a conscious desire to withhold the behavior, nor is addictive behavior consistently impervious to change.
Critics question the existence of compulsivity in addiction altogether [ 5 , 6 , 7 , 89 ], typically using a literal interpretation, i.e., that a person who uses alcohol or drugs simply can not do otherwise. Were that the intended meaning in theories of addiction—which it is not—it would clearly be invalidated by observations of preserved sensitivity of behavior to contingencies in addiction. Indeed, substance use is influenced both by the availability of alternative reinforcers, and the state of the organism. The roots of this insight date back to 1940, when Spragg found that chimpanzees would normally choose a banana over morphine. However, when physically dependent and in a state of withdrawal, their choice preference would reverse [ 102 ]. The critical role of alternative reinforcers was elegantly brought into modern neuroscience by Ahmed et al., who showed that rats extensively trained to self-administer cocaine would readily forego the drug if offered a sweet solution as an alternative [ 103 ]. This was later also found to be the case for heroin [ 103 ], methamphetamine [ 104 ] and alcohol [ 105 ]. Early residential laboratory studies on alcohol use disorder indeed revealed orderly operant control over alcohol consumption [ 106 ]. Furthermore, efficacy of treatment approaches such as contingency management, which provides systematic incentives for abstinence [ 107 ], supports the notion that behavioral choices in patients with addictions remain sensitive to reward contingencies.
Evidence that a capacity for choosing advantageously is preserved in addiction provides a valid argument against a narrow concept of “compulsivity” as rigid, immutable behavior that applies to all patients. It does not, however, provide an argument against addiction as a brain disease. If not from the brain, from where do the healthy and unhealthy choices people make originate? The critical question is whether addictive behaviors—for the most part—result from healthy brains responding normally to externally determined contingencies; or rather from a pathology of brain circuits that, through probabilistic shifts, promotes the likelihood of maladaptive choices even when reward contingencies are within a normal range. To resolve this question, it is critical to understand that the ability to choose advantageously is not an all-or-nothing phenomenon, but rather is about probabilities and their shifts, multiple faculties within human cognition, and their interaction. Yes, it is clear that most people whom we would consider to suffer from addiction remain able to choose advantageously much, if not most, of the time. However, it is also clear that the probability of them choosing to their own disadvantage, even when more salutary options are available and sometimes at the expense of losing their life, is systematically and quantifiably increased. There is a freedom of choice, yet there is a shift of prevailing choices that nevertheless can kill.
Synthesized, the notion of addiction as a disease of choice and addiction as a brain disease can be understood as two sides of the same coin. Both of these perspectives are informative, and they are complementary. Viewed this way, addiction is a brain disease in which a person’s choice faculties become profoundly compromised. To articulate it more specifically, embedded in and principally executed by the central nervous system, addiction can be understood as a disorder of choice preferences, preferences that overvalue immediate reinforcement (both positive and negative), preferences for drug-reinforcement in spite of costs, and preferences that are unstable ( “I’ll never drink like that again;” “this will be my last cigarette” ), prone to reversals in the form of lapses and relapse. From a contemporary neuroscience perspective, pre-existing vulnerabilities and persistent drug use lead to a vicious circle of substantive disruptions in the brain that impair and undermine choice capacities for adaptive behavior, but do not annihilate them. Evidence of generally intact decision making does not fundamentally contradict addiction as a brain disease.
Conclusions
The present paper is a response to the increasing number of criticisms of the view that addiction is a chronic relapsing brain disease. In many cases, we show that those criticisms target tenets that are neither needed nor held by a contemporary version of this view. Common themes are that viewing addiction as a brain disease is criticized for being both too narrow (addiction is only a brain disease; no other perspectives or factors are important) or too far reaching (it purports to discover the final causes of addiction). With regard to disease course, we propose that viewing addiction as a chronic relapsing disease is appropriate for some populations, and much less so for others, simply necessitating better ways of delineating the populations being discussed. We argue that when considering addiction as a disease, the lens of neurobiology is valuable to use. It is not the only lens, and it does not have supremacy over other scientific approaches. We agree that critiques of neuroscience are warranted [ 108 ] and that critical thinking is essential to avoid deterministic language and scientific overreach.
Beyond making the case for a view of addiction as a brain disease, perhaps the more important question is when a specific level of analysis is most useful. For understanding the biology of addiction and designing biological interventions, a neurobiological view is almost certainly the most appropriate level of analysis, in particular when informed by an understanding of the behavioral manifestations. In contrast, for understanding the psychology of addiction and designing psychological interventions, behavioral science is the natural realm, but one that can often benefit from an understanding of the underlying neurobiology. For designing policies, such as taxation and regulation of access, economics and public administration provide the most pertinent perspectives, but these also benefit from biological and behavioral science insights.
Finally, we argue that progress would come from integration of these scientific perspectives and traditions. E.O. Wilson has argued more broadly for greater consilience [ 109 ], unity of knowledge, in science. We believe that addiction is among the areas where consilience is most needed. A plurality of disciplines brings important and trenchant insights to bear on this condition; it is the exclusive remit of no single perspective or field. Addiction inherently and necessarily requires multidisciplinary examination. Moreover, those who suffer from addiction will benefit most from the application of the full armamentarium of scientific perspectives.
Funding and disclosures
Supported by the Swedish Research Council grants 2013-07434, 2019-01138 (MH); Netherlands Organisation for Health Research and Development (ZonMw) under project number 912.14.093 (LJMJV); NIDA and NIAAA intramural research programs (LL; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health); the Peter Boris Chair in Addictions Research, Homewood Research Institute, and the National Institute on Alcohol Abuse and Alcoholism grants AA025911, AA024930, AA025849, AA027679 (JM; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health).
MH has received consulting fees, research support or other compensation from Indivior, Camurus, BrainsWay, Aelis Farma, and Janssen Pharmaceuticals. JM is a Principal and Senior Scientist at BEAM Diagnostics, Inc. DM, JR, LL, and LJMJV declare no conflict of interest.
Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278:45–7.
Article CAS PubMed Google Scholar
McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–95.
Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The stigma of alcohol dependence compared with other mental disorders: a review of population studies. Alcohol Alcohol. 2011;46:105–12.
Heyman GM. Addiction and choice: theory and new data. Front Psychiatry. 2013;4:31.
Article PubMed PubMed Central Google Scholar
Heather N, Best D, Kawalek A, Field M, Lewis M, Rotgers F, et al. Challenging the brain disease model of addiction: European launch of the addiction theory network. Addict Res Theory. 2018;26:249–55.
Article Google Scholar
Pickard H, Ahmed SH, Foddy B. Alternative models of addiction. Front Psychiatr.y 2015;6:20.
Google Scholar
Hall W, Carter A, Forlini C. The brain disease model of addiction: is it supported by the evidence and has it delivered on its promises? Lancet Psychiatr. 2015;2:105–10.
Hart CL. Viewing addiction as a brain disease promotes social injustice. Nat Hum Behav. 2017;1:0055.
Heilig M, Epstein DH, Nader MA, Shaham Y. Time to connect: bringing social context into addiction neuroscience. Nat Rev Neurosc.i 2016;17:592–9.
Article CAS Google Scholar
Jellinek EM. The disease concept of alcoholism. Hillhouse Press on behalf of the Christopher J. Smithers Foundation: New Haven, CT; 1960.
Stevenson A. Oxford dictionary of English. 3 ed. New York, NY: Oxford University Press; 2010.
Fan J, May SJ, Zhou Y, Barrett-Connor E. Bimodality of 2-h plasma glucose distributions in whites: the Rancho Bernardo study. Diabetes Care 2005;28:1451–6.
King AC, Vena A, Hasin D, De Wit D, O’Connor CJ, Cao D. Subjective responses to alcohol in the development and maintenance of alcohol use disorder (AUD). Am J Psychiatry. 2021. https://doi.org/10.1176/appi.ajp.2020.20030247 .
GBD. 2016 Alcohol and Drug Use Collaborators. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5:987–1012.
Edwards G, Gross MM. Alcohol dependence: provisional description of a clinical syndrome. Br Med J. 1976;1:1058–61.
Article CAS PubMed PubMed Central Google Scholar
Epstein DH, Heilig M, Shaham Y. Science-based actions can help address the opioid crisis. Trends Pharm Sci. 2018;39:911–16.
Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: available evidence to inform clinical practice and research. J Subst Abus Treat. 2005;28:321–9.
Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Datab System Rev. 2013;5:CD009329.
Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings a systematic review and meta-analysis. JAMA. 2014;311:1889–900.
Article PubMed CAS Google Scholar
Mark TL, Kranzler HR, Song X. Understanding US addiction physicians’ low rate of naltrexone prescription. Drug Alcohol Depend. 2003;71:219–28.
Article PubMed Google Scholar
Nutt DJ, King LA, Phillips LD. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010;376:1558–65.
Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12:274–83.
Laing RD. The divided self; a study of sanity and madness. London: Tavistock Publications; 1960.
Foucault M, Khalfa J. History of madness. New York: Routledge; 2006.
Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL. et al.Comorbidity of mental disorders with alcohol and other drug abuse. Results Epidemiologic Catchment Area (ECA) study.JAMA. 1990;264:2511–8.
Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–16.
Lopez-Quintero C, Hasin DS, de Los Cobos JP, Pines A, Wang S, Grant BF, et al. Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addiction. 2011;106:657–69.
Humphreys K. Addiction treatment professionals are not the gatekeepers of recovery. Subst Use Misuse. 2015;50:1024–7.
Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2007;86:214–21.
Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am J Public Health. 1996;86:966–72.
Culverhouse R, Bucholz KK, Crowe RR, Hesselbrock V, Nurnberger JI Jr, Porjesz B, et al. Long-term stability of alcohol and other substance dependence diagnoses and habitual smoking: an evaluation after 5 years. Arch Gen Psychiatry. 2005;62:753–60.
Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–42.
Skolnick P. The opioid epidemic: crisis and solutions. Annu Rev Pharm Toxicol. 2018;58:143–59.
Hser YI, Evans E, Grella C, Ling W, Anglin D. Long-term course of opioid addiction. Harv Rev Psychiatry. 2015;23:76–89.
Mathers BM, Degenhardt L, Bucello C, Lemon J, Wiessing L, Hickman M. Mortality among people who inject drugs: a systematic review and meta-analysis. Bull World Health Organ. 2013;91:102–23.
Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–66.
Article PubMed PubMed Central CAS Google Scholar
Lee MR, Sher KJ. “Maturing Out” of binge and problem drinking. Alcohol Res: Curr Rev. 2018;39:31–42.
Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100:281–92.
Berridge V. The rise, fall, and revival of recovery in drug policy. Lancet. 2012;379:22–23.
Parvaz MA, Moeller SJ, d’Oleire Uquillas F, Pflumm A, Maloney T, Alia-Klein N, et al. Prefrontal gray matter volume recovery in treatment-seeking cocaine-addicted individuals: a longitudinal study. Addict Biol. 2017;22:1391–401.
Korponay C, Kosson DS, Decety J, Kiehl KA, Koenigs M. Brain volume correlates with duration of abstinence from substance abuse in a region-specific and substance-specific manner. Biol Psychiatry Cogn Neurosci Neuroimaging. 2017;2:626–35.
PubMed PubMed Central Google Scholar
Janes AC, Datko M, Roy A, Barton B, Druker S, Neal C, et al. Quitting starts in the brain: a randomized controlled trial of app-based mindfulness shows decreases in neural responses to smoking cues that predict reductions in smoking. Neuropsychopharmacology. 2019;44:1631–38.
Humphreys K, Bickel WK. Toward a neuroscience of long-term recovery from addiction. JAMA Psychiatry. 2018;75:875–76.
Verhulst B, Neale MC, Kendler KS. The heritability of alcohol use disorders: a meta-analysis of twin and adoption studies. Psychol Med. 2015;45:1061–72.
Goldman D, Oroszi G, Ducci F. The genetics of addictions: uncovering the genes. Nat Rev Genet. 2005;6:521–32.
Kendler KS, Jacobson KC, Prescott CA, Neale MC. Specificity of genetic and environmental risk factors for use and abuse/dependence of cannabis, cocaine, hallucinogens, sedatives, stimulants, and opiates in male twins. AJ Psychiatry. 2003;160:687–95.
Schizophrenia Working Group of the Psychiatric Genomics C. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–7.
Wray NR, Ripke S, Mattheisen M, Trzaskowski M, Byrne EM, Abdellaoui A, et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat Genet. 2018;50:668–81.
Wray NR, Lin T, Austin J, McGrath JJ, Hickie IB, Murray GK, et al. From basic science to clinical application of polygenic risk scores: a primer. JAMA Psychiatry. 2021;78:101–9.
Walters RK, Polimanti R, Johnson EC, McClintick JN, Adams MJ, Adkins AE, et al. Transancestral GWAS of alcohol dependence reveals common genetic underpinnings with psychiatric disorders. Nat Neurosci. 2018;21:1656–69.
Visscher PM, Wray NR. Concepts and misconceptions about the polygenic additive model applied to disease. Hum Hered. 2015;80:165–70.
Heilig M, Leggio L. What the alcohol doctor ordered from the neuroscientist: theragnostic biomarkers for personalized treatments. Prog Brain Res. 2016;224:401–18.
Rasmussen K, White DA, Acri JB. NIDA’s medication development priorities in response to the Opioid Crisis: ten most wanted. Neuropsychopharmacology. 2019;44:657–59.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. AJ Psychiatry. 2010;167:748–51.
Kwako LE, Schwandt ML, Ramchandani VA, Diazgranados N, Koob GF, Volkow ND, et al. Neurofunctional domains derived from deep behavioral phenotyping in alcohol use disorder. AJ Psychiatry. 2019;176:744–53.
Kwako LE, Bickel WK, Goldman D. Addiction biomarkers: dimensional approaches to understanding addiction. Trends Mol Med. 2018;24:121–28.
Xiao P, Dai Z, Zhong J, Zhu Y, Shi H, Pan P. Regional gray matter deficits in alcohol dependence: a meta-analysis of voxel-based morphometry studies. Drug Alcohol Depend. 2015;153:22–8.
Ersche KD, Williams GB, Robbins TW, Bullmore ET. Meta-analysis of structural brain abnormalities associated with stimulant drug dependence and neuroimaging of addiction vulnerability and resilience. Curr Opin Neurobiol. 2013;23:615–24.
Klugah-Brown B, Di X, Zweerings J, Mathiak K, Becker B, Biswal B. Common and separable neural alterations in substance use disorders: a coordinate-based meta-analyses of functional neuroimaging studies in humans. Hum Brain Mapp. 2020;41:4459–77.
Volkow ND, Fowler JS, Wang GJ. The addicted human brain: insights from imaging studies. J Clin Investig. 2003;111:1444–51.
Goldstein RZ, Volkow ND. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat Rev Neurosci. 2011;12:652–69.
Goodkind M, Eickhoff SB, Oathes DJ, Jiang Y, Chang A, Jones-Hagata LB, et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry. 2015;72:305–15.
Scofield MD, Heinsbroek JA, Gipson CD, Kupchik YM, Spencer S, Smith AC, et al. The nucleus accumbens: mechanisms of addiction across drug classes reflect the importance of glutamate homeostasis. Pharm Rev. 2016;68:816–71.
Korpi ER, den Hollander B, Farooq U, Vashchinkina E, Rajkumar R, Nutt DJ, et al. Mechanisms of action and persistent neuroplasticity by drugs of abuse. Pharm Rev. 2015;67:872–1004.
Luscher C, Malenka RC. Drug-evoked synaptic plasticity in addiction: from molecular changes to circuit remodeling. Neuron. 2011;69:650–63.
Everitt BJ. Neural and psychological mechanisms underlying compulsive drug seeking habits and drug memories–indications for novel treatments of addiction. Eur J Neurosci. 2014;40:2163–82.
Lesscher HM, Vanderschuren LJ. Compulsive drug use and its neural substrates. Rev Neurosci. 2012;23:731–45.
Cruz FC, Koya E, Guez-Barber DH, Bossert JM, Lupica CR, Shaham Y, et al. New technologies for examining the role of neuronal ensembles in drug addiction and fear. Nat Rev Neurosci. 2013;14:743–54.
Crick F. The astonishing hypothesis: the scientific search for the soul. Scribner; Maxwell Macmillan International: New York, NY; 1994.
Vanderschuren LJ, Achterberg EJ, Trezza V. The neurobiology of social play and its rewarding value in rats. Neurosci Biobehav Rev. 2016;70:86–105.
Venniro M, Zhang M, Caprioli D, Hoots JK, Golden SA, Heins C, et al. Volitional social interaction prevents drug addiction in rat models. Nat Neurosci. 2018;21:1520–29.
Martinez D, Orlowska D, Narendran R, Slifstein M, Liu F, Kumar D, et al. Dopamine type 2/3 receptor availability in the striatum and social status in human volunteers. Biol Psychiatry. 2010;67:275–8.
Wiers CE, Shokri-Kojori E, Cabrera E, Cunningham S, Wong C, Tomasi D, et al. Socioeconomic status is associated with striatal dopamine D2/D3 receptors in healthy volunteers but not in cocaine abusers. Neurosci Lett. 2016;617:27–31.
Morgan D, Grant KA, Gage HD, Mach RH, Kaplan JR, Prioleau O, et al. Social dominance in monkeys: dopamine D2 receptors and cocaine self-administration. Nat Neurosci. 2002;5:169–74.
Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e356–e66.
Gilbert PA, Zemore SE. Discrimination and drinking: a systematic review of the evidence. Soc Sci Med 2016;161:178–94.
Oshri A, Gray JC, Owens MM, Liu S, Duprey EB, Sweet LH, et al. Adverse childhood experiences and amygdalar reduction: high-resolution segmentation reveals associations with subnuclei and psychiatric outcomes. Child Maltreat. 2019;24:400–10.
Holmes CJ, Barton AW, MacKillop J, Galván A, Owens MM, McCormick MJ, et al. Parenting and salience network connectivity among African Americans: a protective pathway for health-risk behaviors. Biol Psychiatry. 2018;84:365–71.
Brody GH, Gray JC, Yu T, Barton AW, Beach SR, Galván A, et al. Protective prevention effects on the association of poverty with brain development. JAMA Pediatr. 2017;171:46–52.
Hanson JL, Gillmore AD, Yu T, Holmes CJ, Hallowell ES, Barton AW, et al. A family focused intervention influences hippocampal-prefrontal connectivity through gains in self-regulation. Child Dev. 2019;90:1389–401.
Borsboom D, Cramer A, Kalis A. Brain disorders? Not really… why network structures block reductionism in psychopathology research. Behav Brain Sci. 2018;42:1–54.
Field M, Heather N, Wiers RW. Indeed, not really a brain disorder: Implications for reductionist accounts of addiction. Behav Brain Sci. 2019;42:e9.
Pascoli V, Hiver A, Van Zessen R, Loureiro M, Achargui R, Harada M, et al. Stochastic synaptic plasticity underlying compulsion in a model of addiction. Nature. 2018;564:366–71.
James W. The dilemma of determinism. Whitefish, MT: Kessinger Publishing; 2005.
Gessell B. Indeterminism in the brain. Biol Philos. 2017;32:1205–23.
Jedlicka P. Revisiting the quantum brain hypothesis: toward quantum (neuro)biology? Front Mol Neurosci. 2017;10:366.
Heyman GM. Addiction: a disorder of choice. Cambridge, MA: Harvard University Press; 2010.
Heather NQ. Is addiction a brain disease or a moral failing? A: Neither. Neuroethics. 2017;10:115–24.
Ahmed SH, Lenoir M, Guillem K. Neurobiology of addiction versus drug use driven by lack of choice. Curr Opin Neurobiol. 2013;23:581–7.
Hogarth L, Lam-Cassettari C, Pacitti H, Currah T, Mahlberg J, Hartley L, et al. Intact goal-directed control in treatment-seeking drug users indexed by outcome-devaluation and Pavlovian to instrumental transfer: critique of habit theory. Eur J Neurosci. 2019;50:2513–25.
Mathis V, Kenny PJ. From controlled to compulsive drug-taking: the role of the habenula in addiction. Neurosci Biobehav Rev. 2019;106:102–11.
Luscher C, Robbins TW, Everitt BJ. The transition to compulsion in addiction. Nat Rev Neurosci. 2020;21:247–63.
Robinson TE, Berridge KC. Addiction. Annu Rev Psychol. 2003;54:25–53.
Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci. 2005;8:1481–89.
Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–38.
Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychol Rev. 1990;97:147–68.
Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Rev. 1993;18:247–91.
Koob GF, Le Moal M. Plasticity of reward neurocircuitry and the ‘dark side’ of drug addiction. Nat Neurosci. 2005;8:1442–4.
Stein DJ, Costa DLC, Lochner C, Miguel EC, Reddy YCJ, Shavitt RG, et al. Obsessive-compulsive disorder. Nat Rev Dis Prim. 2019;5:52.
Vanderschuren LJ, Everitt BJ. Drug seeking becomes compulsive after prolonged cocaine self-administration. Science 2004;305:1017–9.
American_Psychiatric_Association. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed. Arlington, VA, US: American Psychiatric Publishing, Inc; 2013.
Book Google Scholar
Spragg SDS. Morphine addiction in chimpanzees. Comp Psychol Monogr. 1940;15:132–32.
Lenoir M, Cantin L, Vanhille N, Serre F, Ahmed SH. Extended heroin access increases heroin choices over a potent nondrug alternative. Neuropsychopharmacology. 2013;38:1209–20.
Caprioli D, Venniro M, Zeric T, Li X, Adhikary S, Madangopal R, et al. Effect of the novel positive allosteric modulator of metabotropic glutamate receptor 2 AZD8529 on incubation of methamphetamine craving after prolonged voluntary abstinence in a rat model. Biol Psychiatry. 2015;78:463–73.
Augier E, Barbier E, Dulman RS, Licheri V, Augier G, Domi E, et al. A molecular mechanism for choosing alcohol over an alternative reward. Science. 2018;360:1321–26.
Bigelow GE. An operant behavioral perspective on alcohol abuse and dependence. In: Heather N, Peters TJ, Stockwell T, editors. International handbook of alcohol dependence and problems. John Wiley & Sons Ltd; 2001. p. 299–315.
Higgins ST, Heil SH, Lussier JP. Clinical implications of reinforcement as a determinant of substance use disorders. Annu Rev Psychol. 2004;55:431–61.
Satel S, Lilienfeld SO. Brainwashed: the seductive appeal of mindless neuroscience. New York, NY: Basic Books; 2015.
Wilson EO. Consilience: the unity of knowledge. New York, NY: Vintage Books; 1999.
Saunders JB, Degenhardt L, Reed GM, Poznyak V. Alcohol use disorders in ICD-11: past, present, and future. Alcohol Clin Exp Res 2019;43:1617–31.
Organization. WH. ICD-11 for mortality and morbidity statistics. 2018. https://icd.who.int/browse11/l-m/en . Accessed 21 Oct 2020.
Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, brief intervention, and referral to treatment (SBIRT): toward a public health approach to the management of substance abuse. Subst Abus. 2007;28:7–30.
Witkiewitz K, Hallgren KA, Kranzler HR, Mann KF, Hasin DS, Falk DE, et al. Clinical validation of reduced alcohol consumption after treatment for alcohol dependence using the World Health Organization risk drinking levels. Alcohol Clin Exp Res 2017;41:179–86.
Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. AJ Psychiatry. 2013;170:834–51.
Rosenthal RJ, Faris SB. The etymology and early history of ‘addiction’. Addict Res Theory. 2019;27:437–49.
Martin CS, Steinley DL, Verges A, Sher KJ. The proposed 2/11 symptom algorithm for DSM-5 substance-use disorders is too lenient. Psychol Med. 2011;41:2008–10.
Degenhardt L, Bharat C, Bruno R, Glantz MD, Sampson NA, Lago L, et al. Concordance between the diagnostic guidelines for alcohol and cannabis use disorders in the draft ICD-11 and other classification systems: analysis of data from the WHO’s World Mental Health Surveys. Addiction. 2019;114:534–52.
PubMed Google Scholar
Lago L, Bruno R, Degenhardt L. Concordance of ICD-11 and DSM-5 definitions of alcohol and cannabis use disorders: a population survey. Lancet Psychiatry. 2016;3:673–84.
Lundin A, Hallgren M, Forsman M, Forsell Y. Comparison of DSM-5 classifications of alcohol use disorders with those of DSM-IV, DSM-III-R, and ICD-10 in a general population sample in Sweden. J Stud Alcohol Drugs. 2015;76:773–80.
Kwako LE, Momenan R, Litten RZ, Koob GF, Goldman D. Addictions neuroclinical assessment: a neuroscience-based framework for addictive disorders. Biol Psychiatry. 2016;80:179–89.
Rehm J, Heilig M, Gual A. ICD-11 for alcohol use disorders: not a convincing answer to the challenges. Alcohol Clin Exp Res. 2019;43:2296–300.
Download references
Acknowledgements
The authors want to acknowledge comments by Drs. David Epstein, Kenneth Kendler and Naomi Wray.
Author information
Authors and affiliations.
Center for Social and Affective Neuroscience, Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
Markus Heilig
Peter Boris Centre for Addictions Research, McMaster University and St. Joseph’s Healthcare Hamilton, Hamilton, ON, Canada
- James MacKillop
Homewood Research Institute, Guelph, ON, Canada
New York State Psychiatric Institute and Columbia University Irving Medical Center, New York, NY, USA
Diana Martinez
Institute for Mental Health Policy Research & Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health (CAMH), Toronto, ON, Canada
Jürgen Rehm
Dalla Lana School of Public Health and Department of Psychiatry, University of Toronto (UofT), Toronto, ON, Canada
Klinische Psychologie & Psychotherapie, Technische Universität Dresden, Dresden, Germany
Department of International Health Projects, Institute for Leadership and Health Management, I.M. Sechenov First Moscow State Medical University, Moscow, Russia
Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, Translational Addiction Medicine Branch, National Institute on Drug Abuse Intramural Research Program and National Institute on Alcohol Abuse and Alcoholism Division of Intramural Clinical and Biological Research, National Institutes of Health, Baltimore and Bethesda, MD, USA
Lorenzo Leggio
Department of Population Health Sciences, Unit Animals in Science and Society, Faculty of Veterinary Medicine, Utrecht University, Utrecht, the Netherlands
Louk J. M. J. Vanderschuren
You can also search for this author in PubMed Google Scholar
Contributions
All authors jointly drafted the paper.
Corresponding author
Correspondence to Markus Heilig .
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Heilig, M., MacKillop, J., Martinez, D. et al. Addiction as a brain disease revised: why it still matters, and the need for consilience. Neuropsychopharmacol. 46 , 1715–1723 (2021). https://doi.org/10.1038/s41386-020-00950-y
Download citation
Received : 10 November 2020
Revised : 11 December 2020
Accepted : 14 December 2020
Published : 22 February 2021
Issue Date : September 2021
DOI : https://doi.org/10.1038/s41386-020-00950-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Persistent impacts of smoking on resting-state eeg in male chronic smokers and past-smokers with 20 years of abstinence.
- Yoonji Jeon
- Dongil Chung
Scientific Reports (2023)
A contextualized reinforcer pathology approach to addiction
- Samuel F. Acuff
- James G. Murphy
Nature Reviews Psychology (2023)
Functional genomic mechanisms of opioid action and opioid use disorder: a systematic review of animal models and human studies
- Camille Falconnier
- Alba Caparros-Roissard
- Pierre-Eric Lutz
Molecular Psychiatry (2023)
A neuromarker for drug and food craving distinguishes drug users from non-users
- Leonie Koban
- Tor D. Wager
Nature Neuroscience (2023)
Does a Survivorship Model of Opioid Use Disorder Improve Public Stigma or Policy Support? A General Population Randomized Experiment
- Jarratt D. Pytell
- Geetanjali Chander
- Emma E. McGinty
Journal of General Internal Medicine (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Substance Use Disorders and Addiction: Mechanisms, Trends, and Treatment Implications
- Ned H. Kalin , M.D.
Search for more papers by this author
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health ( 1 ) suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol. When considering other substances, the report estimated that 4.4 million individuals had a marijuana use disorder and that 2 million people suffered from an opiate use disorder. It is well known that stress is associated with an increase in the use of alcohol and other substances, and this is particularly relevant today in relation to the chronic uncertainty and distress associated with the COVID-19 pandemic along with the traumatic effects of racism and social injustice. In part related to stress, substance use disorders are highly comorbid with other psychiatric illnesses: 9.2 million adults were estimated to have a 1-year prevalence of both a mental illness and at least one substance use disorder. Although they may not necessarily meet criteria for a substance use disorder, it is well known that psychiatric patients have increased usage of alcohol, cigarettes, and other illicit substances. As an example, the survey estimated that over the preceding month, 37.2% of individuals with serious mental illnesses were cigarette smokers, compared with 16.3% of individuals without mental illnesses. Substance use frequently accompanies suicide and suicide attempts, and substance use disorders are associated with a long-term increased risk of suicide.
Addiction is the key process that underlies substance use disorders, and research using animal models and humans has revealed important insights into the neural circuits and molecules that mediate addiction. More specifically, research has shed light onto mechanisms underlying the critical components of addiction and relapse: reinforcement and reward, tolerance, withdrawal, negative affect, craving, and stress sensitization. In addition, clinical research has been instrumental in developing an evidence base for the use of pharmacological agents in the treatment of substance use disorders, which, in combination with psychosocial approaches, can provide effective treatments. However, despite the existence of therapeutic tools, relapse is common, and substance use disorders remain grossly undertreated. For example, whether at an inpatient hospital treatment facility or at a drug or alcohol rehabilitation program, it was estimated that only 11% of individuals needing treatment for substance use received appropriate care in 2018. Additionally, it is worth emphasizing that current practice frequently does not effectively integrate dual diagnosis treatment approaches, which is important because psychiatric and substance use disorders are highly comorbid. The barriers to receiving treatment are numerous and directly interact with existing health care inequities. It is imperative that as a field we overcome the obstacles to treatment, including the lack of resources at the individual level, a dearth of trained providers and appropriate treatment facilities, racial biases, and the marked stigmatization that is focused on individuals with addictions.
This issue of the Journal is focused on understanding factors contributing to substance use disorders and their comorbidity with psychiatric disorders, the effects of prenatal alcohol use on preadolescents, and brain mechanisms that are associated with addiction and relapse. An important theme that emerges from this issue is the necessity for understanding maladaptive substance use and its treatment in relation to health care inequities. This highlights the imperative to focus resources and treatment efforts on underprivileged and marginalized populations. The centerpiece of this issue is an overview on addiction written by Dr. George Koob, the director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and coauthors Drs. Patricia Powell (NIAAA deputy director) and Aaron White ( 2 ). This outstanding article will serve as a foundational knowledge base for those interested in understanding the complex factors that mediate drug addiction. Of particular interest to the practice of psychiatry is the emphasis on the negative affect state “hyperkatifeia” as a major driver of addictive behavior and relapse. This places the dysphoria and psychological distress that are associated with prolonged withdrawal at the heart of treatment and underscores the importance of treating not only maladaptive drug-related behaviors but also the prolonged dysphoria and negative affect associated with addiction. It also speaks to why it is crucial to concurrently treat psychiatric comorbidities that commonly accompany substance use disorders.
Insights Into Mechanisms Related to Cocaine Addiction Using a Novel Imaging Method for Dopamine Neurons
Cassidy et al. ( 3 ) introduce a relatively new imaging technique that allows for an estimation of dopamine integrity and function in the substantia nigra, the site of origin of dopamine neurons that project to the striatum. Capitalizing on the high levels of neuromelanin that are found in substantia nigra dopamine neurons and the interaction between neuromelanin and intracellular iron, this MRI technique, termed neuromelanin-sensitive MRI (NM-MRI), shows promise in studying the involvement of substantia nigra dopamine neurons in neurodegenerative diseases and psychiatric illnesses. The authors used this technique to assess dopamine function in active cocaine users with the aim of exploring the hypothesis that cocaine use disorder is associated with blunted presynaptic striatal dopamine function that would be reflected in decreased “integrity” of the substantia nigra dopamine system. Surprisingly, NM-MRI revealed evidence for increased dopamine in the substantia nigra of individuals using cocaine. The authors suggest that this finding, in conjunction with prior work suggesting a blunted dopamine response, points to the possibility that cocaine use is associated with an altered intracellular distribution of dopamine. Specifically, the idea is that dopamine is shifted from being concentrated in releasable, functional vesicles at the synapse to a nonreleasable cytosolic pool. In addition to providing an intriguing alternative hypothesis underlying the cocaine-related alterations observed in substantia nigra dopamine function, this article highlights an innovative imaging method that can be used in further investigations involving the role of substantia nigra dopamine systems in neuropsychiatric disorders. Dr. Charles Bradberry, chief of the Preclinical Pharmacology Section at the National Institute on Drug Abuse, contributes an editorial that further explains the use of NM-MRI and discusses the theoretical implications of these unexpected findings in relation to cocaine use ( 4 ).
Treatment Implications of Understanding Brain Function During Early Abstinence in Patients With Alcohol Use Disorder
Developing a better understanding of the neural processes that are associated with substance use disorders is critical for conceptualizing improved treatment approaches. Blaine et al. ( 5 ) present neuroimaging data collected during early abstinence in patients with alcohol use disorder and link these data to relapses occurring during treatment. Of note, the findings from this study dovetail with the neural circuit schema Koob et al. provide in this issue’s overview on addiction ( 2 ). The first study in the Blaine et al. article uses 44 patients and 43 control subjects to demonstrate that patients with alcohol use disorder have a blunted neural response to the presentation of stress- and alcohol-related cues. This blunting was observed mainly in the ventromedial prefrontal cortex, a key prefrontal regulatory region, as well as in subcortical regions associated with reward processing, specifically the ventral striatum. Importantly, this finding was replicated in a second study in which 69 patients were studied in relation to their length of abstinence prior to treatment and treatment outcomes. The results demonstrated that individuals with the shortest abstinence times had greater alterations in neural responses to stress and alcohol cues. The authors also found that an individual’s length of abstinence prior to treatment, independent of the number of days of abstinence, was a predictor of relapse and that the magnitude of an individual’s neural alterations predicted the amount of heavy drinking occurring early in treatment. Although relapse is an all too common outcome in patients with substance use disorders, this study highlights an approach that has the potential to refine and develop new treatments that are based on addiction- and abstinence-related brain changes. In her thoughtful editorial, Dr. Edith Sullivan from Stanford University comments on the details of the study, the value of studying patients during early abstinence, and the implications of these findings for new treatment development ( 6 ).
Relatively Low Amounts of Alcohol Intake During Pregnancy Are Associated With Subtle Neurodevelopmental Effects in Preadolescent Offspring
Excessive substance use not only affects the user and their immediate family but also has transgenerational effects that can be mediated in utero. Lees et al. ( 7 ) present data suggesting that even the consumption of relatively low amounts of alcohol by expectant mothers can affect brain development, cognition, and emotion in their offspring. The researchers used data from the Adolescent Brain Cognitive Development Study, a large national community-based study, which allowed them to assess brain structure and function as well as behavioral, cognitive, and psychological outcomes in 9,719 preadolescents. The mothers of 2,518 of the subjects in this study reported some alcohol use during pregnancy, albeit at relatively low levels (0 to 80 drinks throughout pregnancy). Interestingly, and opposite of that expected in relation to data from individuals with fetal alcohol spectrum disorders, increases in brain volume and surface area were found in offspring of mothers who consumed the relatively low amounts of alcohol. Notably, any prenatal alcohol exposure was associated with small but significant increases in psychological problems that included increases in separation anxiety disorder and oppositional defiant disorder. Additionally, a dose-response effect was found for internalizing psychopathology, somatic complaints, and attentional deficits. While subtle, these findings point to neurodevelopmental alterations that may be mediated by even small amounts of prenatal alcohol consumption. Drs. Clare McCormack and Catherine Monk from Columbia University contribute an editorial that provides an in-depth assessment of these findings in relation to other studies, including those assessing severe deficits in individuals with fetal alcohol syndrome ( 8 ). McCormack and Monk emphasize that the behavioral and psychological effects reported in the Lees et al. article would not be clinically meaningful. However, it is feasible that the influences of these low amounts of alcohol could interact with other predisposing factors that might lead to more substantial negative outcomes.
Increased Comorbidity Between Substance Use and Psychiatric Disorders in Sexual Identity Minorities
There is no question that victims of societal marginalization experience disproportionate adversity and stress. Evans-Polce et al. ( 9 ) focus on this concern in relation to individuals who identify as sexual minorities by comparing their incidence of comorbid substance use and psychiatric disorders with that of individuals who identify as heterosexual. By using 2012−2013 data from 36,309 participants in the National Epidemiologic Study on Alcohol and Related Conditions–III, the authors examine the incidence of comorbid alcohol and tobacco use disorders with anxiety, mood disorders, and posttraumatic stress disorder (PTSD). The findings demonstrate increased incidences of substance use and psychiatric disorders in individuals who identified as bisexual or as gay or lesbian compared with those who identified as heterosexual. For example, a fourfold increase in the prevalence of PTSD was found in bisexual individuals compared with heterosexual individuals. In addition, the authors found an increased prevalence of substance use and psychiatric comorbidities in individuals who identified as bisexual and as gay or lesbian compared with individuals who identified as heterosexual. This was most prominent in women who identified as bisexual. For example, of the bisexual women who had an alcohol use disorder, 60.5% also had a psychiatric comorbidity, compared with 44.6% of heterosexual women. Additionally, the amount of reported sexual orientation discrimination and number of lifetime stressful events were associated with a greater likelihood of having comorbid substance use and psychiatric disorders. These findings are important but not surprising, as sexual minority individuals have a history of increased early-life trauma and throughout their lives may experience the painful and unwarranted consequences of bias and denigration. Nonetheless, these findings underscore the strong negative societal impacts experienced by minority groups and should sensitize providers to the additional needs of these individuals.
Trends in Nicotine Use and Dependence From 2001–2002 to 2012–2013
Although considerable efforts over earlier years have curbed the use of tobacco and nicotine, the use of these substances continues to be a significant public health problem. As noted above, individuals with psychiatric disorders are particularly vulnerable. Grant et al. ( 10 ) use data from the National Epidemiologic Survey on Alcohol and Related Conditions collected from a very large cohort to characterize trends in nicotine use and dependence over time. Results from their analysis support the so-called hardening hypothesis, which posits that although intervention-related reductions in nicotine use may have occurred over time, the impact of these interventions is less potent in individuals with more severe addictive behavior (i.e., nicotine dependence). When adjusted for sociodemographic factors, the results demonstrated a small but significant increase in nicotine use from 2001–2002 to 2012–2013. However, a much greater increase in nicotine dependence (46.1% to 52%) was observed over this time frame in individuals who had used nicotine during the preceding 12 months. The increases in nicotine use and dependence were associated with factors related to socioeconomic status, such as lower income and lower educational attainment. The authors interpret these findings as evidence for the hardening hypothesis, suggesting that despite the impression that nicotine use has plateaued, there is a growing number of highly dependent nicotine users who would benefit from nicotine dependence intervention programs. Dr. Kathleen Brady, from the Medical University of South Carolina, provides an editorial ( 11 ) that reviews the consequences of tobacco use and the history of the public measures that were initially taken to combat its use. Importantly, her editorial emphasizes the need to address health care inequity issues that affect individuals of lower socioeconomic status by devoting resources to develop and deploy effective smoking cessation interventions for at-risk and underresourced populations.
Conclusions
Maladaptive substance use and substance use disorders are highly prevalent and are among the most significant public health problems. Substance use is commonly comorbid with psychiatric disorders, and treatment efforts need to concurrently address both. The papers in this issue highlight new findings that are directly relevant to understanding, treating, and developing policies to better serve those afflicted with addictions. While treatments exist, the need for more effective treatments is clear, especially those focused on decreasing relapse rates. The negative affective state, hyperkatifeia, that accompanies longer-term abstinence is an important treatment target that should be emphasized in current practice as well as in new treatment development. In addition to developing a better understanding of the neurobiology of addictions and abstinence, it is necessary to ensure that there is equitable access to currently available treatments and treatment programs. Additional resources must be allocated to this cause. This depends on the recognition that health care inequities and societal barriers are major contributors to the continued high prevalence of substance use disorders, the individual suffering they inflict, and the huge toll that they incur at a societal level.
Disclosures of Editors’ financial relationships appear in the April 2020 issue of the Journal .
1 US Department of Health and Human Services: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality: National Survey on Drug Use and Health 2018. Rockville, Md, SAMHSA, 2019 ( https://www.samhsa.gov/data/nsduh/reports-detailed-tables-2018-NSDUH ) Google Scholar
2 Koob GF, Powell P, White A : Addiction as a coping response: hyperkatifeia, deaths of despair, and COVID-19 . Am J Psychiatry 2020 ; 177:1031–1037 Link , Google Scholar
3 Cassidy CM, Carpenter KM, Konova AB, et al. : Evidence for dopamine abnormalities in the substantia nigra in cocaine addiction revealed by neuromelanin-sensitive MRI . Am J Psychiatry 2020 ; 177:1038–1047 Link , Google Scholar
4 Bradberry CW : Neuromelanin MRI: dark substance shines a light on dopamine dysfunction and cocaine use (editorial). Am J Psychiatry 2020 ; 177:1019–1021 Abstract , Google Scholar
5 Blaine SK, Wemm S, Fogelman N, et al. : Association of prefrontal-striatal functional pathology with alcohol abstinence days at treatment initiation and heavy drinking after treatment initiation . Am J Psychiatry 2020 ; 177:1048–1059 Abstract , Google Scholar
6 Sullivan EV : Why timing matters in alcohol use disorder recovery (editorial). Am J Psychiatry 2020 ; 177:1022–1024 Abstract , Google Scholar
7 Lees B, Mewton L, Jacobus J, et al. : Association of prenatal alcohol exposure with psychological, behavioral, and neurodevelopmental outcomes in children from the Adolescent Brain Cognitive Development Study . Am J Psychiatry 2020 ; 177:1060–1072 Link , Google Scholar
8 McCormack C, Monk C : Considering prenatal alcohol exposure in a developmental origins of health and disease framework (editorial). Am J Psychiatry 2020 ; 177:1025–1028 Abstract , Google Scholar
9 Evans-Polce RJ, Kcomt L, Veliz PT, et al. : Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates . Am J Psychiatry 2020 ; 177:1073–1081 Abstract , Google Scholar
10 Grant BF, Shmulewitz D, Compton WM : Nicotine use and DSM-IV nicotine dependence in the United States, 2001–2002 and 2012–2013 . Am J Psychiatry 2020 ; 177:1082–1090 Link , Google Scholar
11 Brady KT : Social determinants of health and smoking cessation: a challenge (editorial). Am J Psychiatry 2020 ; 177:1029–1030 Abstract , Google Scholar
- Cited by None
- Substance-Related and Addictive Disorders
- Addiction Psychiatry
- Transgender (LGBT) Issues
239 Addiction Essay Topic Ideas & Examples
🏆 best addiction topic ideas & essay examples, 👍 good essay topics on addiction, 📌 simple & easy addiction essay titles, 💡 most interesting addiction topics to write about, 📑 good research topics about addiction, ✍️ addiction essay topics for college.
- Addiction to Online Gaming: A Review of Literature The present paper is an overview of scholarly sources on online gaming addiction and the analysis of narrative inquiry as the most suitable qualitative research method to use for the investigation of this problem.
- Smartphone Addiction Problem Statement Uncontrolled use of smartphone requires users to review the need to respond to smartphone alerts, deactivate the alerts, and consult their colleagues rather than the phone because such actions can reduce anxiety. Smartphone addiction is […] We will write a custom essay specifically for you by our professional experts 808 writers online Learn More
- Problems of Internet Addiction Disorder Another possible cause of a reduction in the brain capabilities is the kind of the materials that one is exposed to on the Internet.
- Problems of Pornography Addiction This paper provides you with a deep insight into the issues related to pornography including the factors leading to wide spread of this, the various perspective and attitudes towards the matter, and lastly, discuss its […]
- The Concept of Addiction The recent developments in psychology, as well as intensive studies in the concept of addiction, has drawn considerable debates and concerns on the issue of relationships between the legal system and addiction.
- Symbolic Interactionism on Drug Addiction Genetic factors in addiction include the number of receptors in the brain that influence the perception of drugs and other substances.
- Online Gambling Addiction Gambling is an addiction as one becomes dependent on the activity; he cannot do without it, it becomes a necessity to him. Online gambling is more of an addiction than a game to the players.
- Facebook Addiction in the Modern Society As a result of these occurrences, it has been proposed that Facebook is addictive since people appear to be hooked to the site and cannot keep away from it even considering the negative consequences.
- Phone Addiction Among Adolescents The ethical principle that the paper will base on is the principle of nonmaleficence, which aims to weigh the benefits versus the harms of phone addiction. However, it is ethical to be addicted to smartphone […]
- The Qualitative and Quantitative Research Strategies: Drug Addiction This is why another purpose of this paper is to evaluate what kind of research strategy is more effective and better in regards to the topic of drug addiction.
- Jim Carroll’s Drug Addiction in the Movie “The Basketball Diaries” by Leonardo Dicaprio After the bursting of Jim and apprehending of his friends, using drugs red handed by the couch, disintegration starts taking place in the group and most of the boys lose their essence for being thrown […]
- Online Video Games Addiction The changes are far-reaching: the definition of online video game; the nature of the information ‘commons’ for the citizen; the right of privacy in communicated expressions; the regulation of information infrastructures; the definition of information […]
- Effects of Internet Addiction on Family Relationships Among Teenagers In the modern society, cyber bullying refers to the instances where the individual uses the internet to interfere with the rights and freedoms of others.
- “A Star Is Born”: Addiction Analysis From the BPS+ Perspective Most importantly, the movie points to the presence of a much more significant factor that pushes Jack toward the abuse of alcohol and the use of drugs.
- Internet Addiction Among College Students It is definitely advisable that the schedule include at least a few hours to login to Facebook because at the end of the day the aim is not to put the person in total isolation.
- Social Media Addiction in Society The person takes the substance, or in case of social media, keeps checking and updating online status or website on and on.
- College Students: Internet Addiction The authors also note that the use and access of the internet have increased in the past decades. Additionally, the authors argue that conflicts between parents and young individuals are likely to result in internet […]
- On Internet Addiction in Swift’s Satirical Style In the modern world, it is difficult to find any person who is unfamiliar with the Internet. People began to abuse the Internet and live a virtual life, forgetting the real world.
- Women’s Addiction in All Its Manifestations Analysis In the Substance Addiction category, women usually indulge in Food, Alcohol, and Drugs in that order of priority; however, addiction of women to alcohol and drugs is more prevalent in Western countries {albeit to a […]
- The Intervention of Positive Coping and Drug Addiction The intervention in question is based on the three domains that are referred to as “the pleasant life”, “the engaged life” and “the meaningful life”.
- The Theme of Addiction in Tennessee Williams’ Plays Apart from that, one can mention that addiction is depicted as a force that ruins the family of the characters. This is one of the points that should be distinguished.
- Amy Winehouse: Addiction Case Study The singer’s relationships with her dad and husband serve as the representation of the abuse she had to face as a pop-star.
- Video Games Addiction: Is It Real? Addiction is associated with the need of substance while in some cases a behaviour which someone finds hard to move on without it, where the unavailability to a way out leads to abnormality.
- The Effect of Internet Addiction on Students’ Emotional and Academic Performance The participants will be told the goals and objectives of the study, and their experience of Internet addiction will be clarified.
- The Role Play in Drug Addiction Treatment Moreover, the client believes that everyone in the law field uses coke, including his father, and this is the culture of the sphere.
- Likecoholic: Social Media Addiction Modern scholars have started likening the addiction to the use of social media to smoking, stating that companies such as Facebook must be regulated “exactly the same way you regulated the cigarette industry,” in which […]
- Social Work and Addiction in Family Settings The patient experiences urges to use drugs regardless of the apparent negative consequences of this practice. Therapists and clients consider this stage to be the most difficult.
- Deviant Behavior: Drug Addiction Drug addiction as a form of deviant behavior is seen as a loss of a person’s former moral and spiritual values, which leads to intellectual degradation and a reduced desire to function as a member […]
- Mental Health Care in Cannabis Addiction Case Based on the experience of studying the stories of juvenile delinquents, Bowlby revealed the influence of early separation from the mother and the experiences of loss and separation associated with it on the violation of […]
- Alcohol Addiction and Psychological Assistance Smith is a supporter of the Democratic Party like most people in her family and among her friends and colleagues. Smith was asked what goals she wanted to achieve in the course of her treatment.
- Addiction of Whitney Houston This paper looks at the causes of addiction, hindrances to recovery, and the causes of relapse or successful recovery using the life of Whitney Houston as a model.
- Drug Addiction and Its Effects The main cause of drug addiction is, obviously, the use of drugs but there are specific predictors making some people engage in drug abuse. Another sign of addiction is the need to use drugs in […]
- Online Gaming Addiction Analysis For example, in World of Warcraft, there are 10 million players around the world who pay about $15 a month to blitz around the world of Azeroth.
- Opioids Addiction in the United States The growing addiction, abuse, and overdose of opioids in the United States are some of the main concerns among the federal agencies involved in safeguarding public health.
- Online Gaming Addiction Intervention HC’s philosophical stand is to stop the addiction, meaning that he is motivated and hopes that the obsession will end. The addiction process started at a very young age of 7 years, back when HC […]
- Caffeine Addiction as a Mental Disorder And it is a rather pragmatic question stipulated by the professionals need to debate about, but not by the addiction nature itself.
- Addiction Assessment Tool Evaluation The purpose of the present paper is to conduct a review of the 10-item yes/no Drug Abuse Screening Test to evaluate its benefits and limitations.
- Social Cognitive Theory Against Addiction All the sources are closely related to the problem of alcohol addiction and, therefore, are included in the research. The study aimed to investigate the effect of the social cognitive theory implementation on people willing […]
- Theories of Substance Addiction The risk is confounded when these factors occur in combination; thus, the more the risk factors, the higher the probability that the use of substances can result into addiction.
- Psychodrama in Treating Trauma and Addiction In all cases, it is problematic for the individual to reconcile with the anxiety they feel and to cope with the problems with trust.
- Society’s Obligation to Help People With Addiction The first and foremost point is that the group approach shifts treatment to the natural environment and reconnects addiction therapy to a more comprehensive and long-lasting recovery process.
- Men and Porn Addiction Discussion Watching porn trains men to differentiate reality from acting, implying that it does not alter men’s perception of women in real life.
- Impaired Nurses: Prescription Drug Addiction Work with drugs and psychotropic substances in medical organizations is constantly in the field of view of law enforcement agencies for the control of drug trafficking and health authorities.
- Psilocybin as a Smoking Addiction Remedy Additionally, the biotech company hopes to seek approval from FDA for psilocybin-based therapy treatment as a cigarette smoking addiction long-term remedy.
- Advocacy Programs to Address Disparities in Mental Health and Addiction Management Due to the absence of coverage offered by state Medicaid programs, the problem with the community’s overall health likely resides in a population segment that is unable to receive care, especially individuals with mental health […]
- The History of ADHD Treatment: Drug Addiction Disorders Therefore, the gathered data would be classified by year, treatment type, and gender to better comprehend the statistical distribution of the prevalence of drug addiction.
- Teen Vaping: The New Wave of Nicotine Addiction It might have a significant effect if state officials asked the region’s health authority to ban all flavored vape goods in reaction to this issue to safeguard the youth’s well-being.
- The Epidemic of Opioid Addiction in the US Although the author presents facts about kratom benefits, the article still lacks scientific evidence, likely due to insufficient research in this area, so it may not convince the reader that this herb should be legal.
- Opioid Addiction and Pharmacological Treatment LAAM has several merits over the use of methadone, particularly regarding its use of three doses per week, which can reduce the potential of contracting HIV/AIDS, improve the relationship between the patients and the clinicians, […]
- Misconceptions About Addiction In addition, addicts are not always drug abusers, as addiction is a treatable disorder, and people seeking help can recover and become productive.
- Smartphone Addiction in the United States With the advent of phones that have the function of many other gadgets, people began to move away from the real world into the virtual one. This paper examines the essence of the issue of […]
- The Truth About Food Addiction in Society One of the most important tasks is understanding the reality of food addiction. The first line of food addiction prevention is the decision people have to make.
- The Opium Addiction Treatment Above all, the main problem is the reluctance of pharmaceutical companies to find a common approach and method of facing opium addiction since the first thing to think about is profits, just like any other […]
- Discussion: Social Media Addiction Social media use impacts the nerves in the brain and can cause psychological and physical addiction. The brain gets used to the rewards from such channels, and it becomes automatic for the person to use […]
- Opioid Addiction in Adults: A Group Counselling Plan A group leader ensures that the group is led in a healthy discussion and that the group’s objectives are achieved. When this culture is properly outlined, and members are aware of their targets, the group’s […]
- Tackling Drug: Addiction Among Youth Drug addiction is a serious problem, and while it spreads to less marginalized parts of society, this problem affects more people.
- The Nature of Addiction The purpose of this critical writing is to understand why people begin to want to get rid of the shackles of addictive behavior.
- Tobacco Addictions Among Teenagers This makes it urgent to fight all forms of tobacco and nicotine use in order to preserve the health of adolescents.
- Program to Tackle Drug Addiction Among Youth The core area of emphasis will be training the students on different ways to avoid the temptations of using drugs in order to lower the rate of addiction.
- Parental Role in Adolescents’ Phone Addiction In other words, the connection between the guardian and the teenagers is critical and should be maintained to allow children experience the love of their parents.
- A Manifesto on the Phone Addiction Issue It seems to be common knowledge that being too attached to one’s phone is bad for mental and physical health, and the dangers may be greater for the younger generation.
- Discussion of Tobacco Addiction in Miami The problem analyzed in the presentation is related to the increased risk of tobacco use among adults associated with nicotine dependence.
- Lysergic Acid Diethylamide (LCD): Addiction, Treatment, and Prevention The problems are not only depicted in the area of concentration but also in the suburbs that are out of the stereotypical view of intoxication of the drug.
- Drug and Alcohol Addiction: Abby’s Case The amounts of money Abby spends weekly on fulfilling her addictive desires and her long history of drug usage imply that she has an addiction problem.
- Drug Addiction in Teenagers: Smoking and Other Lifestyles In the first part of this assignment, the health problem of drug addiction was considered among teens and the most vulnerable group was established.
- Instagram Addiction and Impact on Self-Esteem The effect of social media use is reported to have a mixed effect on the user. First, social media addiction may have a varying effect on self-esteem depending on the type of use.
- Comprehensive Addiction and Recovery Act The policy authorizes the secretary to award grants to states with a higher rate of substances and drugs as this indicates the state of mental health.
- How Alvin Ailey’s Dances Help With Drug Addiction Ailey is the founder of the famous theater in New York and is known for popularizing modern dance and mixing it with ballet, jazz and elements of African culture.
- Molecular Dynamics Modeling: Treating Addiction The resulting mechanism of the three sites provides the separation of antagonists from the agonists and explains the selectivity of the subtypes.
- Drug Addiction Treatment for a Pregnant Woman The drug has affected various aspects of her life, causing her to lose her job and making her turn to crime to afford the drugs.
- You Are What You Eat: How Does Food Become an Addiction One of the most important problems that arouse the interest of researchers is the influence of advertising on the formation of models of food behavior and, above all, its involvement in the formation of food […]
- Instagram Addiction and Self-Esteem in Kuwaiti High School Students Besides, the study will explore the impact of social media and reveal the possible ways to resolve the social media addiction issues affecting the youth.
- Instagram Addiction and Self-Esteem in High School Students To test the relationship between social media Instagram addiction and self-esteem in American high school students, a descriptive survey where students will be enrolled in an online, blinded survey will apply.
- Tobacco as a Chemical Addiction Chemical addiction is a global disease of the mind, soul, and body. It is necessary to remove the mechanism of a disease-dependent state of origin and engage all the spheres of human life to overcome […]
- Drug Addiction: Overview of the Main Principles and Recovery Plan On the one hand, the term’ drug addiction is specifically defined by NIDA as “characterized by intense and, at times, uncontrollable drug craving, along with compulsive drug seeking and use that persist even in the […]
- How Opioid Addiction Affects the United States Addicted people have a constant desire to increase the dose, which is a severe medical and social problem. The crisis has acquired enormous proportions and become a brake on the economy and a threat to […]
- Drug and Alcohol Addiction in Atlantic City The prevalent part of the population of Atlantic City consists of African-Americans and Caucasians. Because of this, alcohol and drugs are very popular among residents, which may pose a community health issue and is applicable […]
- The Role of Mitochondria in Cocaine Addiction In many instances, the drug users tend to sniff it, and the powder gets through the nasal materials to the bloodstream.
- Why Addiction Develops and How a Person Can Overcome It The interview process was good; I called the interviewee at a scheduled time and asked her the questions from the list.
- Preventing Childhood Exposure to Addiction-Forming Factors The implementation of the method relied on the use of advanced questionnaire that provided the researchers with sufficient data to reflect and address the children’s inclination toward any form of addiction. Evidently, the role of […]
- History and Social Side of Drug Addiction Heroin and fentanyl are the most dangerous drugs created on the basis of papaver somniferum due to produced effects and the outcomes for the body.
- Drug and Substance Addiction Standardization has to be used to ensure that patients’ experiences and different clinical services are the same, regardless of the process.
- My Personal Beliefs About People With Addictions Therefore, in my opinion, the main reason people get addicted is related to the desire to forget about the problems of this reality and feel differently.
- Biopsychological and Spiritual Models in Addiction Studies More specifically, it is the “simplification” of the real-world conditions provides an opportunity to neglect different factors to provide a qualitative conclusion concerning the object of learning.
- Device Addiction: Consequences and Solutions One of the essential traits of smartphone addiction is tolerance which is defined as “a gradual increase in the mobile phone use to obtain the same level of satisfaction”.
- Economic Inequality During COVID-19: Correlation With Depression and Addiction Thus, during the pandemic, people with lower incomes experienced depression and increased their addictive behaviors to cope with the stress of COVID-19.
- Opioid Use and Addiction in Afghanistan and Iraq Veterans My chosen topic integrates the welfare of veterans of recent wars, such as conflicts in Iraq and Afghanistan, the prescription of opioids for trauma, general mental well-being, and adaptation to civilian and even academic life.
- Tobacco Addiction: Causes and Effects However, it has also been proven that, in general, smoking has causal roots in human genetics, with different percentages of the message affecting, respectively, the start of smoking, the duration of the experience, and the […]
- Drug Addiction and Problems Related to It It is one of the main sources of dopamine, and other pleasure hormones, which are essential for a person to feel joy in their life.
- Chemical Dependency and Crisis of Addiction The scope of the damaging effects of alcohol abuse on the well-being of the person is astounding. Based on the WHO’s data, socio-cultural determinants of health are the issues that are linked to culture and […]
- Social Facet of Substance Addiction Even though the determination of the hazardous society is important for analyzing the social facet of drug addiction, it is crucial to fundamentally understand the society’s influential factors of engaging a person in drug addiction.
- Alcohol Addiction: Biological & Social Perspective At the same time, the UK is one of the most drinking countries, as the average number of liters of alcohol per person there was 11. In addition, taking acetaldehyde dehydrogenase inhibitors allows to break […]
- Drug and Alcohol Addiction Crisis Among Adults in Baltimore While a lot of the violence in Baltimore is related to the drug trade, the drugs themselves killed at least 180 more people than homicides in the city as of 2019.
- Addiction in Sexton’s, Marshall’s, Flynn’s Poems The poems The Addict by Anne Sexton, Habitual by Nate Marshall, and Philip Seymour Hoffman by Nick Flynn, address the issue from the psychological perspective as an inner struggle within a person.
- John S. McCain Opioid Addiction Prevention Act’s Analysis Anderson, the President and Chief Executive Officer of the National Association of Chain Drug Stores, backed the legislation enactment believing in its potential to reduce opioid abuse and addiction.
- Alcohol Addiction and the Role of a Community New Horizons Group of Alcoholics Anonymous is a local fellowship to support men and women with alcoholic problems in Miami Springs.
- Analysis of the Addiction’s Aspects Addiction in the modern world is one of the phenomena that occur in the vast majority of people. However, if the goal is not achieved, there will be a sharp decline in this hormone, and […]
- Workout and Addiction: Review As a result of personal factors and the presence of eating or image disorders, an individual can be unable to stop exercising even when it is detrimental to their life.
- Counseling of a Client With Heroin Addiction Although he has a son, he does not maintain any relationship with him, and his son does not try to communicate with Dante. First, the client did not address this aspect and was unwilling to […]
- Drug Addiction and Drug Legalization Rosenthal views drug addiction as slavery and the idea for drug legalization is revolting because most of the victims of addiction are adolescents and children. Without honesty and responsibility, legalization of drugs is just a […]
- The Issue of Opioid Abuse and Addiction in Treatment The project will primarily focus on the issue of opioid abuse and addiction to treat and minimize the effects of pain through the given pharmacological method of pain management.
- Fundamental Determination of Substance Abuse and Addiction and Their Difference Due to the difference in regularity and intensity of drug absorption, substance abuse and addiction can be correctly separated from another so that there is a concrete measure that identifies an abuse and an addiction […]
- Alcohol Addiction Among Women Women are a population of interest because of the increased mortality rates from alcohol-related health complications and the effect of this substance on childbearing. Similarly, to the previous organization, Alcove is a recovery facility that […]
- Drug Addiction Treatment Approaches In this way, some state that the objectives and aims of treatment should be to entirely drug-free the drug addict and that treatment should include drug-free techniques of achieving this aim.
- Drug Addiction From Pharmacological Perspective In the history of human society, drug addiction is almost always spoken of as a crime. Understanding drug effects allow criminologists and sociologists to recognize the relationship between drug addiction and crime.
- Drug Addiction Problem Among Homeless People There is a need to fill the data gap regarding the issues of magnitude, location, period, severity, and changeability of the SUD in the Skid Row community.
- Nuances of Alcohol Using Addiction Despite the traced co-occurrence of criminal activities and alcohol consumption, people argue that there are many positive aspects of drinking moderately, such as relaxation that is useful in many social environments. Goode argues that “for […]
- Systemic Interventions Overview: Cocaine Addiction She shared her recovery story in the Portrait of Addiction, and though she was successful on her way to a normal life, a systemic intervention approach would make it much easier and more comfortable for […]
- Substance Addiction Challenges for American Indians In the case presented by Paul et al, the distinctions between male and female addicts can be seen in the cultural features and traits of the American Indian population.
- Loneliness and Social Networking Addiction in Students The hypothesis of the study was as follows: the higher the level of loneliness, the higher the likelihood of social networking addiction; conversely, the lower the level of loneliness, the lower the likelihood of social […]
- Warm Hand-off for Overdose Survivors to Addiction Treatment The first responders facilitate the identification of survivors needing emergency health care systems House Bill 424 of the General Assembly of Pennsylvania, known as the Warm Hand-Off to Treatment Act, provides a comprehensive initiative that […]
- Reasons of Alcohol Addiction in Teenagers Given the clinical diagnoses, the wide-spread nature of the problem, and the severe consequences impacting the life and health of millions of people, the in-depth investigation of the causes of the disorder is of critical […]
- The John Muir Health Facility’s Addiction Medicine Recovery Services The aim of this evaluation plan is to establish the effectiveness of the program in addressing patients’ behavioral and attitudinal issues affecting their commitment to sobriety.
- Impact of Digital Drug and Electronic Addiction on UAE Youth Therefore, the primary purpose of this dissertation is to determine the impact of digital drugs and the electronic addiction they cause on the youth of the UAE to highlight the existing problem in society.
- Criticism of Injecting Rooms – Drug Addiction Supporters of injecting rooms claim that injecting rooms are beneficial to the society and that the ones which are in existence have saved many lives especially from the dangers of drug overdosing.
- Drug Addiction: Importance of Policy Change Drug addiction and abuse are the issues that have to be discussed and analyzed from different aspects to make sure that the policy change and offered practices can work effectively to reduce the number of […]
- Mobile Addiction and Anxiety: The Relationship Analysis The purpose of the study is to establish the nature of the relationship that exists between mobile addiction and anxiety among students.
- The Drug Addiction and Clonidine As soon as it gets to the brain, it reacts by binding on the a2 receptors, a process that leads to a reduction in the levels of presynaptic calcium.
- How Serotonin Affects the Brain and Addictions The purpose of this paper is to discuss the effects that serotonin has in the brain and how it interacts with other chemicals in the body Serotonin is an indoleamine chemical secreted by the brain […]
- Impacts of Internet on Children Health and Addiction Among the worst hit are children, who find themselves addicted to it given that they are in the process of development. To help nurture children’s behavior, parents should educate them on the safety and risks […]
- Searching the Web for Research Evidence: Drug Addiction Among School Aged Children Defining the topic in the form of a question or statement and separating the question into specific logical components or concepts is the principal strategy to search the CINAHL database.
- Caffeine Addiction and Negative Effects The thesis of this paper is that scientists need to reclassify caffeine as a potentially addictive stimulant drug. In addition to the potential to cause addictive behavior, caffeine can have an adverse effect on the […]
- The Case of Katie’s Addiction Katie became one of the unfortunate people who had to deal with chronic pain, which led her to develop an addiction to the medication which was supposed to benefit her and relieve the car accident’s […]
- Valium and Heroin Addiction: Compare and Contrast The purpose of this paper is to contrast and compare Valium and heroin from a point of view of addiction and withdrawal.
- Mental Health Nursing of Cocaine Addiction The 1983 Mental Health Act is an Act of the Parliament of the United Kingdom that applies to the residents of England and Wales.
- Refraining From Diet Coke: Substance Use Addiction Speaking of my plans on the use of diet coke, I would like to emphasize that I do not plan to drink it.
- Addiction in the Elderly: Structured Critical Review Therefore, it is in the interest of national and global communities to prioritize the needs of the elderly and investigate the particularities of their addiction to substances.
- DSM-5 and Introduction of Behavioral Addictions The combination of substance abuse and behavioral addiction is another point that is widely debated to be recognized in the DSM-5.
- Symptoms of Addiction: Case Analysis Second, the inability to fall asleep without alcohol or a sleeping pill is a definite sign of addiction. Third, the client initially takes large doses of alcohol, which is a sign of increased tolerance.
- Team of Professionals: Addiction Case Analysis Second, the client needs to undergo a thorough medical assessment to understand if he presents the signs of comorbidities. Considering that the client may find it difficult to organize and keep track of all appointments, […]
- Anxiety Among Us: How and Why, Drug Addiction As the effects of the drug are not long-lasting, people who take phenobarbital tend to use the medicine more often than it is allowed in the drug prescription.
- Addiction Treatment: Challenges in Case Management Settings Case management has a vital role in addiction treatment as it helps to adopt a holistic approach and empower the client. According to the US Department of Health and Human Services (HHS, 2004), “substance abusers have better treatment outcomes if their other problems are addressed concurrently” (pp.1-2). Case management aims at planning and coordinating health […]
- Adolescent Substance Abuse, Addiction, and Dependence And while overall statistics show a decrease in the number of unique and persistent cases of substance abuse in Western countries in general and in the US in particular, this problem is still extremely urgent.
- Alcoholic Anonymous Organization Fighting Addiction By accepting the problem and causes, a participant can try to resolve. In the program, participants have to admit their past wrongs and errors to a group and receive support to change.
- Food Addiction and Obesity in Children and Teens Many turn to comfort eating to cope with this stress, to the point where it takes on the characteristics of an addiction. Overeating and obesity can also become a vicious cycle: children would eat to […]
- Shopping Addiction: Personal Experiences She realized that she had wasted most of her life and she was heading to destruction. She began thinking of taking a positive turn in her life; although she knew it would not be easy […]
- Drug Abuse and Addiction Holimon has succeeded in reviving some of her family relations, and she is still putting a lot of effort to get ahead in this area to the fullest extent possible.
- Facebook Addiction Problem Overview This paper is an in-depth analysis of the risks that Facebook poses to children and the steps that parents should take to ensure that their children do not become victims of Facebook use.
- Facebook: The Latest Addiction Most delegates had laptops in the room connected to the internet and my surprise a good number of them were misusing the privileges of the internet provided by the UN by accessing Facebook and other […]
- Psychoactive Substances and Addiction Substances that could easily lead to addiction are the elements that directly motivate the dopaminergic system such as marijuana, cocaine, nicotine, and heroin.
- The Development of Phobias and Addictions On the other hand, addictions are the behavioral pattern that is characterized by either psychological or physical reliance on substances abuse which is known to have negative impacts on the health and the life of […]
- Addictions and Emotions in Biopsychology The impulse sent to the brain in response to the stimuli is sent to two different parts of the brain: cortex and thalamus.
- The Addiction From Cocaine Main Aspects The impact of the cocaine on the human brain can be explained by the chemical dopamine and its variations in the brain of the drug addict, as well as by three main areas of the […]
- Drug Addiction Treatment: Variety of the Methods Basing on the importance of the learning process in the development of drug addiction practice, CBT makes use of the learning process, firstly, in helping the patients to recognize the conditions which stimulate them to […]
- Addiction: Is It a Disease or Moral Failing? According to the journal article of clinical and research news, a disease can be defined as a complicated relationship existing between the environment of an individual and the general genetic makeup that combines together resulting […]
- The Problem of Gambling in the Modern Society as the Type of Addiction Old people and adolescents, rich and poor, all of them may become the prisoners of this addiction and the only way out may be the treatment, serious psychological treatment, as gambling addiction is the disease […]
- Behavioral Change: Drugs and Addiction The reasons for such usage could vary according to the substance used and to the life rhythm of the addicted person.
- Computer Addiction: Side Effects and Possible Solutions Since that time humanity started to speak of different signs of “computer addiction” the term stands to emphasize the seriousness of the problem and implies the possibility of drastic consequences that computer mania might have.
- Drug Addiction: A General View of New Concepts Users who are weak-minded or peer adulating, tend to imitate others and use the drug not because they really want to, but in order to appear ‘cool’ and ‘one of the group.’ This is a […]
- Antidepressant Addiction and Abuse Depressed addicts need to have a proper examination of their addictive behavior to be able to abstain from processes and substances for altering moods fully.
- Sexual Addiction, Compulsivity, or Problematic Behavior Sex, in general, is most common among the male, they are the ones who can have many ladies just to have sex with them, and they will never think of sex as being sacred or […]
- Alcohol Addiction Issue in USA In order to do well in the group of Alcoholics Anonymous, it is better if the individual is talkative and open to conversations, as the main way of psychological therapy is telling stories about their […]
- The Reality TV Shows Addiction: Cause-Effect The viewers feel like the actors are just in the same scenario as them and every development is a success to both the actor and his viewer.
- Advanced Addiction Psychology Contemporary Perspectives The aptest critique of the test is provided by the discussion that Cox has provided when they suggest that the test should be considered along with the connectionist model.
- Opium Addiction: Cause and Effect The traffic of opium became unlawful only at the beginning of the 20th century when the scientists discovered the real properties of this drug and found out that it causes addiction.
- Methamphetamine and Cocaine Addiction Treatment In fact, by doing so, people subconsciously try to prove that aggressiveness, anxiety, and panic attacks are not implications of drug dependence but the states they medicate with the help of methamphetamine.
- Addictions Assessment Process The first four stages are designed to assist in making the correct diagnosis and determining the level of care to ensure further rehabilitation of the client. The psychiatrist attended to the PTSD and mental issues […]
- Addiction Assessment Tools Terrance is to use two assessment tools: the Drug Abuse Screening Test and the Alcohol Use Disorders Identification Test. In short, Terrance is recommended to use these two tools for a quick and low-cost assessment […]
- Alcohol Addiction: Opting for a Correct Referral Method The psychological content of codependency is evidence of the uniqueness of health disorders and personal functioning of a family member as compared with alcohol-related disorders.
- Relevant Therapy Approaches: Probationers With Alcohol Addiction In the case of substance abuse, this type of therapy can help to pinpoint the root cause of a habit and substitute it with a healthier pattern.
- How Does Addiction Affect Families
- Hallucinogens: Addiction and Treatment
- Clinical and Addictions Assessment Tools
- Models of Addiction and the Assessment Process
- Ethical Codes and Principles in Addictions: Implications of Labeling
- Ethical Codes and Principles in Addictions Assessment
- Food Addiction: How to Overcome It?
- Addiction as Moral Defect From Cultural Perspective
- Heroin Addiction and Its Biological Aspect
- The Crisis of Opiate Addiction
- Drug Addiction in Australia and Management Methods
- Addiction in Adolescences: Factors and Treatments
- Alcohol Addiction as a Learned Behavior
- Drug Addiction Diagnostics and Therapy Prescription
- The Psychology of Addiction and Addictive Behaviors
- Conditioning in Phobias and Addictions
- Connecticut Community for Addiction Recovery
- Drug and Alcohol Addiction: Athletes and Student Leaders
- Addiction Counseling and Certification in Arizona
- The Opioid Crisis: Preventing Addiction
- Addictions in Cultural Groups: Study Challenges
- Addiction Recovery and Its Ethical Risks
- Substance Addiction Treatment in Students
- Heroin Addiction Educational and Preventive Program
- Stop Heroin Addiction: Service Delivery Program
- Primary Care Providers Treating Opiate Addiction
- Addiction History and Concepts
- Nicotine Addiction Research and Assessment
- Addictions: Treatment and Prevention
- Addiction Prevention Programs in Miami-Dade County
- Addiction Occurrence and Reduction in Adolescence
- Addictions in Free Markets
- Video Game Addiction and Maslow’s Hierarchy of Needs
- Second Life Games Addiction and Its Reasons
- Drug Addiction Issues in The Corner Miniseries
- Alcohol Addiction and Its Societal Influence
- Disease Harm Reduction Addiction Treatment Model
- Addiction’s Etiology: Models and Theories
- Addiction: Methods and Approaches
- Gambling and Addiction’s Effects on Neuroplasticity
- Martyrdom as Addiction to Offset the Injustice
- Caffeine: Carriers, Addiction and Diseases
- Cognitive Therapy for Anxiety and Addiction Withdrawal
- Gender Identity and Addiction Treatment
- Drug Addiction History in Urban Areas Since the 1970s
- Social Issues: Alcoholism as a Mode of Addiction
- Breaking the Chains of Cocaine Addiction
- Addiction Counseling and Psychosocial Crisis in Elderly
- Gambling Addiction Research Approaches
- “Breaking the Chains of Cocaine: Black Male Addiction and Recovery” Book
- Adolescent Risk: Substance and Addiction
- Methamphetamine Addiction and Prevention
- Biblical Word Study: Counseling and Addiction Categories
- Drug Addictions Counseling: Assessment and Diagnosing
- Attachment Dimensions and Adolescence Drug Addiction in Relation to School Counseling
- Case Management: Drug Addiction
- Peculiarities of the Addiction Treatments
- Link Between Environment and Addiction
- Theories of Addiction: General Counseling Methods
- Addiction to an Experience
- The Role of Spirituality in Overcoming Addictions
- Problem of Hydrocodone Addiction in US
- Literature Review and Research Methodology Draft: Effects of Internet Addiction on Family Relationships Among Teenagers
- Definition of Alcohol Misuse (Alcohol Abuse and Addiction) in Youth Population Age 18-29
- Computer Addiction in Modern Society
- Pharmaceutical Drug Addiction Among African American Male Adolescents
- Addiction of Digital Media in Society
- “Cocaine: Abuse and Addiction” by National Institute on Drug Abuse
- Understanding Drug & Alcohol Addiction
- Substance Abuse, Addiction and Dependency Among Adolescents
- Is Drug (Legal or Illegal) Addiction and or Abuse Individual Responsibility or Societies Responsibility?
- Analyzing Love and Love Addiction in Relationships
- Addiction Severity Index
- Fast Food, Quick Problem Emergence, Rapid Addiction and Slow Recovery Process
- Internet Addiction in Modern Society
- Sex Addiction as a Psychological Disorder
- Comparison of Theories of Addiction: The Biological Model and the Genetic Model
- Where Does the Path to Smoking Addiction Start?
- Problems of Everyday Addictions in Society
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, March 2). 239 Addiction Essay Topic Ideas & Examples. https://ivypanda.com/essays/topic/addiction-essay-topics/
"239 Addiction Essay Topic Ideas & Examples." IvyPanda , 2 Mar. 2024, ivypanda.com/essays/topic/addiction-essay-topics/.
IvyPanda . (2024) '239 Addiction Essay Topic Ideas & Examples'. 2 March.
IvyPanda . 2024. "239 Addiction Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/addiction-essay-topics/.
1. IvyPanda . "239 Addiction Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/addiction-essay-topics/.
Bibliography
IvyPanda . "239 Addiction Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/addiction-essay-topics/.
- Alcohol Essay Titles
- Abnormal Psychology Paper Topics
- Drug Abuse Research Topics
- Smoking Research Topics
- Alcohol Abuse Paper Topics
- Cognitive Behavioral Therapy Topics
- Gambling Essay Titles
- Drugs Titles
- Eating Disorders Questions
- Alcoholism Essay Titles
- Developmental Psychology Essay Ideas
- Epigenetics Essay Titles
- Mental Disorder Essay Topics
- Neuropsychology Topics
- Criminal Behavior Essay Topics
Causes of Addiction
Reviewed by Psychology Today Staff
There are many theories about the causes of addiction, the use and abuse of legal and illegal psychoactive substances. Biology, psychology, and social and cultural elements all play a role in the enormously complex causal bouquet that results in addiction , and different theories weight the elements differently. Together they reflect the fact that there is no one path to addiction, and no one factor makes addiction an inevitable outcome. Addiction can’t happen without exposure to agents, but that is hardly the determining factor. Addiction is not a property of the substance ingested or activity engaged in.
Instead, research indicates that it is more related to what else is, or isn’t, going on in a person’s life that makes the sensation a substance induces so attractive. Among the many factors that have been shown to influence the development of an addiction are feelings about oneself, emotional state, quality of family relationships, social ties, community attributes, employment status, stress reactivity and coping skills, physical or emotional pain, personality traits, educational opportunities, compelling goals and progress toward them, opportunities for and access to rewards in life, as well as physiological responses. While no factor predominates, each exerts some degree of influence.
On This Page
- What are the most common causes of addiction?
- What are the most common substances of abuse?
- Are some substances more addictive than others?
- Are there risk factors for addiction?
- Do genes play a role in addiction?
- What biological factors influence addiction?
- What environmental factors influence addiction?
- Does stress play a role in addiction?
- What role does childhood trauma play in addiction?
- Is there a brain malfunction that causes addiction?
- If a family member was addicted, will I become addicted?
- Is there an addictive personality?
- Why do some people become addicted while others do not?
- Can someone get addicted by using a substance once?
- Can drug addiction be prevented?
There are no substances (or activities) that universally or uniformly cause people to become addicted. And the vast majority of people exposed to most substances (or activities) considered addictive do not in fact develop addiction to them. Rather, a very complex array of cultural factors, social factors, and situational factors mingle with psychological factors, biological factors, and even personal values to influence the possibility of addiction.
Many different theories of addiction exist because they weight the role of contributing factors differently. Some current models of addiction emphasize the causative role of individual variations in biology or genes that make a substance or experience feel more or less pleasurable. Many models of addiction highlight the causative role of individual psychological factors, whether personality factors such as impulsiveness or sensation-seeking, or psychopathology such as the negative effects of early trauma. Other models of addiction emphasize the role that social and economic factors play in shaping behavior, such as the strength of family and peer relationships and the presence of absence of educational and employment opportunities.
Around the world and in the U.S., nicotine is the most widely used addictive substance; tobacco causes a reported 40 million deaths worldwide. According to the National Institute of Drug Abuse, smoking kills more than 1,000 Americans every day, and although tobacco use is generally declining in the U.S. its use is increasing among some groups of young people, especially in the form of vaping, or inhaling nicotine vapors .
Alcohol in some form is widely used for pleasurable purposes and is an important part of the social fabric worldwide, today as in ancient times. Nevertheless, according to the National Institute on Alcohol Abuse and Alcoholism, 14.6 million U.S. adults over the age of 18 have alcohol use disorder, marked by uncontrolled drinking. Around the world, 240 million people are reportedly dependent on alcohol; alcohol abuse is most prevalent in Eastern Europe and least prevalent among Asians.
Painkillers including prescription opiates such as oxycodone and fentanyl and the illegal drug heroin account for more than 10 percent of all addictions in the U.S, affecting more than 2.5 million people, according to the American Society of Addiction Medicine.
Cocaine is a stimulant that is often taken intranasally (snorted) or injected intravenously but is considered to have the most potential for addiction because of the fast, intense high when smoked in the form of “crack.” Other stimulants that are subject to abuse are amphetamines, widely prescribed to combat attention deficit hyperactivity disorder and to foster alertness and energy.
Depressive agents such as sedatives and tranquilizers are widely used medically to combat stress, anxiety, and sleep disorders , but NIDA reports that 3.5 to 5 percent of the population uses tranquilizers and sleeping pills nonmedically.
The synthetic stimulant methamphetamine is widely considered one of the most addictive agents. Often inhaled, it directly affects the dopamine and other neurotransmitter systems system to produce an extremely fast and intense—but short-lived—high, with an altered sense of energy and power. Further, by changing the responsiveness of dopamine receptors, methamphetamine blunts the experience of reward from normal sources of pleasure.
Crack cocaine is also considered highly addictive. Cocaine processed so that it can be smoked, it enters the blood stream rapidly and produces a rapid “rush” of a high; the immediate response becomes powerfully reinforcing, driving the motivation to repeat the experience.
There are many risk factors for addiction, from individual factors such as stress tolerance and personality makeup to social factors such as friendships and educational and job opportunities. They interact in dynamic ways unique to each person. But what addiction may come down to for everyone is the emotional and physical appeal of a substance at a particular moment in a person’s life. The effects of drugs are pleasurable and rewarding only in relation to how a person feels emotionally and physically in the context of his or her relationships and social life and other opportunities for development and reward.
Some studies show that genes can account for as much as 50 percent of a person’s risk for addiction, although the degree of genetic influence shifts in importance over time. For example, environmental factors such as family and social relationships are more strongly tied to use of alcohol and nicotine in adolescence than later in life. Nevertheless, there is no single gene for addiction nor even a group of genes.
However, there are a number of personality traits, each of which is partly genetically influenced, that contribute to the risk of addiction. These include impulsiveness, frustration tolerance, and sensitivity to rejection. Impulsivity is thought to play its strongest role in the early stages of addiction, driving the motivation for seeking drugs.
Biology contributes to addiction in ways beyond genes. How the body metabolizes, or breaks down and eliminates, foreign substances such as drugs or alcohol is heavily dependent on the presence of various enzymes, and they may vary significantly between individuals and even between ethnic groups.
For example, research shows that the Japanese have unique variations of certain alcohol-metabolizing enzymes that are not present in other populations, deterring alcohol consumption— and alcoholism—because it quickly gives rise to uncomfortable body sensations. Biological factors such as enzyme profile can influence the amount of alcohol people ingest, the pleasantness of the experience, harmful effects on the body, and the development of disease.
There are many factors that influence addiction beyond genes and biology. One of the most significant is t he family milieu and early life experiences . Family interactions, parenting style, and levels of supervision all play a role in development of coping skills and susceptibility to mental health problems. Studies have linked authoritarian or neglectful parenting, family violence, and divorce to increased likelihood of substance use problems later in life. Growing up with strong ties to and a sense of belonging—to a family, to a belief tradition, to a culture—are known to be protective against addiction.
Peers play an enormous role in addiction susceptibility, especially among teens and young adults; most people use drugs for the first time as teenagers. Misuse of prescription drugs, for example, is highest among young adults aged 18 to 25, according to the National Institute of Drug Abuse. Alcohol is the most commonly abused drug among adolescents in the United States. The behavior patterns of friends influence everyone in the group. Further, psychological distress, especially depression and anxiety , has been shown to play an important role in such substance use.
Stress is a risk factor for many kinds of nonadaptive behavior, and addiction is one. Researchers have long linked the effects of chronic stress to alcohol use. Stress relief may enhance the pleasurable effect of any substance. There is some research to support the view that adverse events in childhood and in adulthood change the responsiveness of brain systems. Adverse early life events and cumulative negative events in adulthood—especially those that are both unpredictable and emotionally distressing—alter reactivity of brain structures that govern learning, motivation, the control of distress and control of impulsiveness to increase susceptibility to addiction and to influence the risk of relapse. Stress also increases the risk of mood and anxiety disorders, which are linked to addiction.
Adverse childhood experiences (ACEs) such as trauma, especially combined with an unpredictable and chaotic childhood, pose a risk factor for many kinds of maladaptive behaviors and poor health outcomes . Studies show that having multiple ACEs puts children at risk of poor school performance, unemployment, and high-risk health behaviors including smoking and drug use.
Prolonged stress during childhood dysregulates the normal stress response and, through overproduction of cortisol, is especially harmful to the brain’s hippocampus, impairing memory and learning. Severe or sustained early life adversity shifts the course of brain development and can lastingly impair emotion regulation and cognitive development. What is more, it can sensitize the stress response system so that it overresponds to minimal levels of threat, making people feel easily overwhelmed by life’s normal difficulties. Research shows a strong link between ACEs and opioid drug abuse as well as alcoholism.
The common but mistaken view of addiction as a brain disease suggests that there is some malfunction in the brain that leads to addiction. But that is not the case. Studies show that repeated use of a substance (or an activity), encouraged by a surge in dopamine, creates changes in the wiring of the brain—and those changes are reversible after drug use stops.
Neuroscience research supports the idea that addiction is a habit that becomes deeply entrenched and self-perpetuating , rewiring the circuitry of the brain as it is repeated. The repetition of a highly pleasurable experience—drugs, gambling—alters neurons; they adjust their wiring to become increasingly efficient at the experience. They prune away their capacity to respond to other inputs. It is a form of deeply engraved learning. As drug use stops, engaging in other rewarding activities rewires the brain to find interest and pleasure in non-drug pursuits.
The vast majority of children whose parents abuse alcohol or drugs do not grow up to do the same. However, they are at some increased risk for doing so, and there are a number of reasons why. For one, they are exposed to those substances, and exposure during early adolescence may especially influence substance use.
For another, they may inherit whatever genetic or biological vulnerabilities laid the groundwork for a parental addiction. But they may also be more prone to addiction because they suffer from cognitive, emotional, or behavioral problems known to arise in children as a consequence of growing up in a home marked by substance use; for example, as children they are at increased risk of neglect, abuse, or a poor quality parent-child relationship .
It is a myth that there is some personality factor that is specific for the development of addiction and makes addiction likely. There are a number of personality traits widely shared in the population that contribute to the risk of developing an addiction, usually in indirect ways. For example, people prone to thrill-seeking may be more likely than others to find themselves in situations where drugs are used or to experiment with any number of activities—think: bungee jumping, base-jumping—or substances that provide outsize rewards.
Studies show that those who are high in the trait of neuroticism—they are prone to experiencing negative emotions—are overwhelmed by minor frustrations and interpret ordinary situations as stressful. Neuroticism is linked to a wide array of mental health problems, including anxiety, depression, and eating disorders as well as substance abuse. Neuroticism is also linked to a diminished quality of life, another factor that could increase the allure of substance use.
There is some evidence that natural variation in genetic makeup of the dopamine system may influence who gets addicted. Dopamine is the neurotransmitter activated by rewarding activities as a way of increasing the likelihood of engaging in such activities in the future. Having a relationship, getting a promotion, doing something creative—those are normal ways of stimulating the reward system. Illicit drug use short-circuits that process and directly boosts dopamine levels.
Some people may be more prone to addiction because they feel less pleasure through natural routes, such as from work, friendships, and romance. Their genetic makeup inclines them to develop such personality traits as thrill-seeking. Their craving for risk and novelty takes the fear out of drug use and the huge dopamine boost powerfully reinforces the motivation to seek the reward over and over again.
A person cannot get addicted to a substance without exposure to the substance, but exposure alone does not lead to addiction. Addiction develops only after repeated use of a substance. One use of a substance can produce a pleasurable effect that motivates interest in repeating the experience. But the experience of pleasure is relative; it hinges in part on biology and very much on what else there is going on in a persons life that is meaningful or rewarding.
In its simplest form, drug addiction can be seen as a way of hacking the brain —of finding a shortcut to feelings of emotional reward by bypassing the normal activities that stimulate such sensations and directly manipulating the neurochemicals responsible for them. To a very large degree, brain hacks become appealing when there are restricted opportunities for meaning and for pleasure other than the response to drugs.
Just as recovery from addiction requires focusing on rewarding activities other than drug use , so does prevention. The definition of a meaningful life varies from person to person, but psychology has long identified its components—feelings of self-respect; meaningful relationships that create a sense of belonging; opportunities for growth and development; work that is engaging or rewarding; opportunities for enjoyment and pleasure.

The death rate is rising—and it's rising fastest among women and young people. Here's what to know, and how to protect yourself.

Desires and cravings can often trap us in the grip of unhealthy addictions or relationships. Fortunately, there's a surprisingly simple way to rewire your brain and get free.

Medical interventions for addiction have been life-saving, yet we should be wary of the "medicalization" of addiction.

Problem gambling devastates millions of lives through betting apps and mobile games. If the system is rigged so the house always wins, we have to start playing a new game.

New studies show the risk of cannabis use disorder is the same for medicinal and recreational cannabis users. How would the brain know the difference?

Personal Perspective: Have you ever felt that changes in your workplace have accelerated to the point where it becomes almost impossible to do your job?

Threats to maintaining abstinence from alcohol and other drugs can arise at any time. Here's how to guard against them.

Doctors who are suspected of having substance use disorders are often required to undergo evaluations that require them to pass polygraphs if they want to keep practicing medicine.

Delta-8 is legal under federal law because it is derived from hemp CBD, but its effects are similar to marijuana's THC.

Discover the intricate link between genetics and addiction, unraveling pathways that shape susceptibility and empowering informed choices.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience

Essay on Addiction
Addiction is a complex and multifaceted phenomenon that impacts individuals, families, and society at large. It transcends the mere act of indulging excessively in substances or behaviors; it is a chronic disorder involving brain mechanisms and psychological elements. This essay delves into the nature of addiction, its causes, effects, and potential solutions, offering a comprehensive understanding crucial for students preparing for essay writing competitions.
Addiction is often misconceived as a lack of willpower or moral failing, but in reality, it is a chronic medical condition. It is characterized by compulsive engagement in rewarding stimuli, despite adverse consequences. Addictions can be substance-related, like alcohol, drugs, and nicotine, or behavioral, such as gambling or internet usage.
The Brain and Addiction
At the core of addiction lies the brain’s reward system. Substances like drugs or activities like gambling trigger a surge in dopamine, a neurotransmitter associated with pleasure. Repeated exposure alters the brain’s chemistry, leading to dependency and tolerance, where more of the substance or behavior is needed to achieve the same effect.
Causes of Addiction
Addiction arises from a combination of various factors:
- Biological Factors: Genetics and an individual’s brain chemistry can play a significant role in addiction. Some people may have a genetic predisposition that makes them more susceptible to addiction, while others may have imbalances in neurotransmitters that affect their impulse control and reward-seeking behavior.
- Psychological Factors: Certain psychological factors can contribute to addiction. These include stress, trauma, depression, anxiety, and other mental health issues. Substance abuse may be an attempt to self-medicate or cope with these underlying emotional or psychological issues.
- Environmental Influences: The environment in which a person grows up and lives can have a substantial impact on addiction risk. Exposure to substance abuse, peer pressure, a lack of parental supervision, or living in a community with high drug availability can increase the likelihood of addiction.
- Social and Peer Pressure: Peer pressure, especially during adolescence and young adulthood, can be a significant factor leading to addiction. The desire to fit in or be accepted by a particular social group can lead individuals to experiment with drugs or alcohol.
- Early Exposure: Early experimentation with substances at a young age can increase the risk of addiction. The developing brain may be more vulnerable to the effects of drugs and alcohol, making it easier for addiction to take hold.
- Physical Pain and Prescription Medications: Chronic pain or medical conditions that require prescription medications can sometimes lead to addiction when individuals misuse or become dependent on these drugs.
- Easy Access: The availability and accessibility of addictive substances can contribute to addiction. If drugs or alcohol are readily available, it can be harder for individuals to resist temptation.
- Peer and Family History: A family history of addiction can increase an individual’s susceptibility to addiction. Children of parents with substance abuse issues may have a higher genetic risk and be exposed to a lifestyle that normalizes substance use.
- Socioeconomic Factors: Socioeconomic status can also play a role. Economic stressors and lack of access to resources or support can increase the likelihood of addiction.
- Lack of Coping Skills: Some individuals may lack effective coping skills to deal with life’s challenges and stressors. They may turn to substances as a way to escape or numb emotional pain.
Effects of Addiction
The ramifications of addiction are far-reaching:
- Physical Health Decline: Addiction to substances like drugs or alcohol can lead to severe physical health problems, including organ damage, infections, and an increased risk of chronic diseases.
- Mental Health Issues: Addiction often co-occurs with mental health disorders like depression and anxiety, exacerbating these conditions and making recovery more challenging.
- Financial Consequences: Addiction can drain an individual’s financial resources, leading to financial instability, debt, and even homelessness in extreme cases.
- Relationship Strain: Addicted individuals often face strained relationships with family, friends, and partners due to lying, broken promises, and erratic behavior associated with addiction.
- Legal Problems: Some addictions may lead to legal issues, including arrests and incarceration, further complicating one’s life and future prospects.
- Loss of Employment: Maintaining employment can become difficult for those struggling with addiction, leading to job loss, reduced earning potential, and economic instability.
- Social Isolation: Addiction can result in social isolation as individuals prioritize substance use over social interactions, leading to loneliness and a lack of support.
- Physical Harm: Reckless behavior associated with addiction can result in accidents, injuries, and even overdose, which can be life-threatening.
- Neglect of Responsibilities: Addiction often causes individuals to neglect their responsibilities at home, work, and in their personal lives, leading to a decline in overall functioning.
- Tolerance and Withdrawal: Over time, addicts may develop tolerance to the substance, requiring larger amounts to achieve the desired effect. This can lead to withdrawal symptoms when the substance is not available.
- Loss of Control: One of the defining characteristics of addiction is the loss of control over substance use, where individuals find it nearly impossible to stop despite negative consequences.
- Healthcare Costs: Treating the physical and mental health issues arising from addiction can result in substantial healthcare costs for both the individual and society as a whole.
- Impact on Education: For young people, addiction can disrupt their education, leading to poor academic performance and limited future opportunities.
- Stigmatization: There is often a stigma associated with addiction, which can deter individuals from seeking help and support, further exacerbating their problems.
- Cycle of Relapse: Addiction is characterized by a cycle of relapse and remission, making recovery a challenging and ongoing process.
- Effects on Family: Addiction can have profound effects on family members, causing emotional distress, financial strain, and a breakdown of trust within the family unit.
- Healthcare Burden: The healthcare system may be burdened by the demands of treating addiction-related health issues, diverting resources from other medical needs.
- Community Impact: Addiction can have a broader impact on communities through increased crime rates, accidents, and the strain on social services.
Addiction and Society
Addiction also has a profound societal impact. It increases healthcare costs, contributes to crime rates, and reduces productivity. Moreover, it perpetuates a cycle of poverty and inequality, as those in disadvantaged communities often have limited access to addiction treatment.
Treating Addiction
Treating addiction is challenging but possible. It requires a holistic approach:
- Medical Treatment : Detoxification, medication, and therapy are essential components of addiction treatment.
- Counseling and Behavioral Therapies : These therapies help in understanding the root causes of addiction and developing coping strategies.
- Support Groups : Groups like Alcoholics Anonymous provide community support and accountability.
- Preventive Measures : Education and awareness programs are vital in preventing the onset of addictive behaviors.
In conclusion, Addiction is a complex issue that requires compassion, understanding, and a multi-faceted approach for treatment and prevention. As we understand more about the causes and effects of addiction, it becomes imperative to develop comprehensive strategies to address this crisis. For students participating in essay writing competitions, discussing addiction offers a chance to explore a significant societal issue, emphasizing the need for empathy and informed intervention in tackling this persistent challenge.

Essay Generator
Text prompt
- Instructive
- Professional
Generate an essay on the importance of extracurricular activities for student development
Write an essay discussing the role of technology in modern education.
Home — Essay Samples — Nursing & Health — Substance Abuse — Impact of Drug Addiction on Society
Impact of Drug Addiction on Society
- Categories: Drug Addiction Substance Abuse
About this sample

Words: 904 |
Published: Feb 12, 2024
Words: 904 | Pages: 2 | 5 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!

Related Essays
1 pages / 657 words
1 pages / 661 words
5 pages / 1590 words
3 pages / 1162 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Substance Abuse
Pleasure Unwoven is a documentary film produced by Dr. Kevin McCauley that explores the complex nature of addiction and the underlying neurobiology behind it. The film delves into the concept of pleasure and how it relates to [...]
Millions of individuals are affected by the devastating consequences of substance abuse, making it a significant public health concern worldwide. As societies strive to address this issue, innovations in technology have emerged [...]
Addiction is a complex and pervasive issue that affects individuals from all walks of life. In this essay, we will explore the addictions of Terry and Leon, two individuals who are in need of intervention in order to address [...]
Substance abuse continues to be a pressing global issue, with far-reaching consequences for individuals, families, communities, economies, and public health systems. This essay delves into the multifaceted impact of substance [...]
Teenage drug abuse is a deeply concerning issue that continues to cast a shadow over the lives of young Americans and their communities. As we grapple with this persistent challenge, it is essential to conduct an in-depth [...]
Motivational interviewing (MI) is a counseling technique which assists the interviewee in identifying the internal motivation to change the client’s behavior by resolving ambivalence and insecurities. The term holds similar [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- About Project
- Testimonials
Business Management Ideas

- Essay on Addiction

Introduction
Essay on drug addiction in youth, essay on solutions to drug addiction, essay on internet addiction, essay on tv addiction, essay on computer addiction, essay on addiction to social networking sites, essay on addiction to video games, essay on addiction to facebook, essay on addiction to pornography, essay on addiction to gambling, essay on addiction to smartphones, essay in addiction to video games.
- Introduction:
- Prevention:
- Conclusion:
Addiction to Social Networking Sites
There are several factors leading to addiction. Some of the most common ones are, if one has a genetic predisposition, then there is a high possibility of falling for substance abuse. Another reason is trying to escape a tragic experience or stress. An easy access to cheap and commonly available drugs or cues like going to bar with friends also contribute to forming an addictive behavior. Nonetheless, if a person sees someone in the family history, like mother, father, or uncle taking drugs, alcohol, or going for compulsive behaviors like gambling, or betting sort of things, he/she is most likely to inherit that addiction.
Research has proved that addiction to any form, especially to physical substances, have effects on the wiring of certain neural patterns in the brain, specifically those related to reward, pleasure, motivation, impulse control, and decision-making. Due to this, the situation keeps getting worse and the addiction becomes more severe. The effects and consequences are a disturbed family life, social isolation, financial troubles, affected work life, serious health problems. All these things add to the embarrassment, shame, repentance, and even depression in that person. To counter and overcome these negative feelings, the addict may further take help of the drugs, that are causing the problem in the first place.
Usually, in treating the addiction, preventive measures involve therapy and use of medications. But, taking these measures is only possible when there is acceptance of problem instead of denial. Family support plays a crucial role because the addict may need a lot of emotional and psychological support during the withdrawal stage. It is important to create a clean and drug-free surrounding and this may happen by hospitalizing the patient, confining him to a therapy center for some time. Various support groups help a lot in overcoming the addiction. The therapists also explain to the concerned person, the reasons and special situations which trigger his impulse for drugs. This helps the person in observing and curbing his behavior in future.
Addiction is an involuntary process. It may not be fair to associate a person’s addictive behavior with his moral standards or character. The brain response to an addict changes in such a way that he continues to live with the bad habits and addictions in spite of understanding its dangerous implications. Apart from therapy and medicines, the person requires a lot of love, affection, support, and motivation to get over with the addiction.
The drug addiction in youth today is a world-wide problem and more common than one can imagine. Teens are trying alcohol, marijuana, cigarettes, and heroin etc. even before they have turned 15. Just like any adult addict, the brain-working and neuron patterns of young drug addicts also show the same changes. Once the drugs and substance abuse take over their mind, their personality gradually begins to deform in a very strange way. Teens constitute an important part of our society. Imagining them to fall into the trap of substance abuse at such young age only points towards the seriousness of this issue.
The most common causes of drug addiction in youth are mainly an urge to experiment and experience something new. Then, there is peer pressure, lack of communication between parents and teens, low self-esteem, and a tendency towards seeking pleasure. Genetics and family history of substance abuse also contributed to drug addiction in teenagers. After trying the drugs once, the cycle goes on. It becomes an involuntary process and giving in to the harmful urges becomes a natural habit. The biggest reason behind the inability of our young ones to get out the drug addiction is denial and secrecy amongst both teens and their parents.
Talking about the effects of drug addiction in youth, the list goes on to a great length. A long exposure to habit-forming substance abuse gives birth to poor memory, low self-confidence, serious health troubles, and even violent behaviors. The addicted teenagers are also more prone to having accidents, mood swings, poor sleep, and developing psychological disorders like schizophrenia and bipolar syndrome. The drug abuse may happen at a crucial time of their career-making and ruin the future despite having brilliant talents. The regret, however, may not always be reversible, leading to mental breakdown and suicidal tendencies in the teenagers.
The first and foremost step towards dealing with drug addiction in youth is recognizing the denial mode and getting it out of the way. A healthy and supportive atmosphere of trust and love is a must between the parents and their young ones. For parents, blaming themselves or their kids is of no help. Instead, opting to meet a therapist, taking their teens and visiting a self-help center along with effective medicines may really do wonders. Parents also need to be vigilant of any such friends or relatives who themselves are suffering from addiction, as they may act as triggers and damage all the efforts being made. Maintaining a distance with such persons and unhealthy surroundings is equally essential during the whole process.
Our young ones are the future of our society. Watching them fall into this dark pit of drug addiction is the last thing that we need. With the help of open communication, observation, and positive mindset, we as adults can prevent such cases. Nonetheless, in case of drug abuse, there should not be any need to feel ashamed and helpless. Delaying the treatment worsens the case. That is why, once the drug abuse in the youth is confirmed, it is better to take prompt steps and receive help from self-help groups and therapists.
In such times, when drug addiction is emerging as one of the most common and harmful problems in our youth, searching for proper and effective solutions to drug addiction is the need of the hour. Drug addiction cannot be get ridden of overnight. It is a long process and requires the support of the addict’s family and friends at various levels like emotionally, physically, mentally, and psychologically. Through step by step treatments and therapies, one can successfully get out of the dark traps of drug abuse and eventually start a fresh and healthy life.
The solutions to drug addiction can only be found when the reasons have been discovered. Especially among teens, the basic and usual reasons behind substance abuse are seen to be a mere curiosity, experiments, peer pressure. However, the most substantial cause is having a genetic predisposition to drug abuse. That means, if the person has a family history of drug addiction then the teenager can easily fall for the same addiction. The other reasons include stress, lack of communication, inability to cope up with other kinds of pressures, etc. Only after understanding the cause, we could begin the effective treatment of the concerned person.
Needless to say, the effects of drug addiction are disastrous. A long-term exposure to substance abuse initiates a chain of other severe problems. The first thing that happens is feeling guilt and shame all the time. The drug addiction plays with the wiring of the nervous system. It can cause more stress and lead to serious depression. Apart from social isolation, it never stops to just one addiction. In fact, there are high chances of one substance abuse leading to newer ones. Both mental and physical health of the person is severely affected and more delay in getting the treatment may mean lesser effectiveness of the treatment.
It has been observed that creating a healthy and safe environment for the young people is important. This may mean staying away from even those family members, friends, or relatives who themselves are stuck into the addiction. Open communication between parents and young ones plays a crucial role. It is important to not judge the teenagers who are into drug addiction. An intelligent way to curb this issue is to create a movement in the society by conducting awareness sessions at schools, colleges, and social institutions, which would explain the harmful effects of drugs and other narcotics.
Medicines are necessary to make the treatment effective. Psychological therapies work well in the minds of the drug addict and gradually helps in creating more self-confidence in the youth. Parents of those youth who are into drug addiction should be well-aware of the withdrawal symptoms so that they are prepared from before itself and know how to handle such situations. For a young and healthy society, strict steps should be taken in order to control and eliminate the supply and transactions of such harmful elements. Special measures need to be taken to prevent the young ones to have any kind of access to these drugs.
Unfortunately, we as a world, are living in an era of internet addiction. And the compulsion to stay stuck to the mobile screens, laptops, and desktops has become so much a part of our lives, that now it doesn’t even count as an addiction for most of us. The truth is if one is unable to voluntarily stop himself from checking the phone or going online all the time, then he is suffering from internet addiction. Internet addiction has many other names such as Internet Addiction Disorder, Problematic Internet Disorder, or Compulsive Internet Use.
The causes of internet addiction are both obvious and subtle. First of all, the pleasures one receives from browsing the internet, logging on social media etc are quite similar to any other kind of addiction like substance abuse, gambling, alcohol etc. This pleasure/reward-seeking creates a loop and the addict cannot help but look at the screen time and again. Another major reason is that every single thing or service is available on the internet, regardless of what time of the day it is, which includes shopping online, playing games, watching movies, making friends, learning something, booking tickets and many other important and unimportant things.
Internet addiction has serious effects on our body, mind, and personal lives. Surprisingly, the internet addiction disorder does the same to the wiring of our neurons as is caused by any other addiction to drug or alcohol. Our thought process becomes blurred, decision-making and priorities are hampered. Nothing seems important when compared to staying online. The social damages caused include confinement of virtual relationships with friends and family. Faceless conversations are taking over our lives. Going out for a walk to the nearby local grocery stores has become a thing of past. This means sticking to the chair for a longer time, with no physical activity and no fresh air, leading to weight gain and depression. Other physical and mental troubles consist of a headache, insomnia, spinal problems, boredom, dry eyes, and mood swings.
Denial is the biggest hurdle in treating any disorder. So, being honest about internet addiction may be a nice start. Planning physical workouts in groups, spending more time in the real world, meeting friends, or planning a small trip or outing with family are some of the small yet effective steps that one can take. In severe cases, therapy groups and cognitive behavior therapy may help a lot. Keeping a track of limited online time and being accountable for it to a loved one works great in order to curb the internet addiction. If one is self-aware and willing to get out of this disorder, then sometimes the problem dissolves on its own.
Dealing with internet addiction is challenging because it is available to us all the time. However, limiting the online hours, being self-aware, including a daily work out in the routine, using apps that warn you when you have exceeded the daily limit of internet usage would really help in creating an internet-free atmosphere around you and bring the life on a healthy and positive track.
Gone are the days, when television was treated as a special event. It used to be played for particular shows and specific hours. With time, the number of channels has been growing tremendously and with them, countless programmes have been flourishing like mushrooms. The result is in front of us in the form of TV addiction. To our dismay, not only adults are affected by it. In fact, TV addiction starts at a very early age, especially the kids. It is painful to imagine the horror and imagine our kids going through the same craving as any other drug addict.
TV has become a 24*7 form of entertainment and this is actually a tragedy. In case of adults, the ideal time and lack of creative activities are the main reasons for TV addiction. The spicy nature of serials, reality shows, or even game shows makes it quite difficult to switch off the TV and continue with other departments of life. The innocent and tender minds of kids are continuously being served with ample cartoon channels. To make it worse, they are topped up with advertisements of chocolates, snacks, and many unhealthy products, which are specially tailored for kids.
The harmless-looking TV addiction comes at a very high cost. It is stealing away from kids, their rights to play outside, to experience physical activities, and spend time with nature. Both kids and adults are glued to their chairs all the time. The consequences are poor eyesight, lack of concentration, headache, irritation, mood swings. Due to lack of activity and binge-eating as a result of TV addiction, weight gain is being observed in both kids and adults. The creative side of the minds are left unused and people behave like zombies, doing and eating whatever is being presented on the TV as the latest trend.
Hours should be fixed for watching TV, whether it is for adults or for children. Another alternative is to select one or two favorite programmes that one wants to watch and then simply turn the TV off. Use of timer or alarm is also very effective in limiting the screen time. Strict rules should be made and followed in the family. Apart from these, positive reinforcements like indulging in more creative activities like exercising, joining a dance class, or a gym, prioritizing the daily chores can really help in getting rid of the TV addiction. Kids should be encouraged to play and interact with their friends in natural surroundings like parks or go for family picnics. Books and colors are great ways to keep them occupied for long happy hours.
The first thing in order to get out of TV addiction loop is to take a step back and observe in what ways TV is harming the old and new generation. Substituting the addiction time for something creative and fun makes the whole process easy and doable. It is important to understand and remember that we should use the TV as just a form of entertainment and must not allow it to govern our everyday life.
Computer addiction is basically found to be of two types. The compulsive disorder can make one stick to the computer either offline or online. The offline addiction may happen due to keeping busy with the downloaded versions of games or watching movies continuously. Online computer addiction is more common than offline and there are multiple kinds of options that keep people glued to the screen. The examples of online computer addiction are playing games, uncontrollable email checking, watching videos and movies on the loop, checking notifications of every other social media accounts, unnecessary shopping, or simple random browsing on the internet.
Computer addiction has mainly been observed in males. Depression and anxiety are the prime reasons for any person to suffer from computer addiction, regardless of age and gender. The games, TV series, and videos are crafted in such a way that all of these things prime the person’s mind to watch more and more. Switching the computer may ultimately give a feeling of missing out something important. The adrenalin rush running through one’s body and mind after watching a game or a super-exciting episode turns the situation into a highly addictive one. The taste of instant gratification and freeness of interacting in the virtual world are other reasons working behind the computer addiction.
Those who are suffering from anxiety and depression in an unknown way are more prone to become addicted to the computer. Nonetheless, looking for a relieving solace in the wrong place like online or offline computer world actually worsens the case, leading to even more severe forms of depression. Longer hours of screen time have harmful effects on the health of eyes, poor brain activities, sleep disorders, feeling lonely, lost, and irritated. Once the computer is shut down, life would seem dull to an addict as there is no drama or rush of such levels in the real life. Urgent and important issues of personal life such as health, spending time with family, work-life etc look mundane and one might lose interest in all these aspects of life.
The best measure to reduce and eliminate computer addiction from the life is using outside helps like behavioral therapy, joining self-help groups. One can also take stronger actions like restricting the computer use to purely important purposes, like work, bill-payments etc. Noting down the logged hours may also help in tracking and limiting the computer use. Participating more in real-life activities, accepting help and support from friends and family are some of the other wonderful ideas that actually work. Instead of keeping the computer in the sleep mode, it is safer to shut it down after the necessary work has been done. Starting the computer would require much effort and act as a good reminder to not use it for trivial purposes.
For a better mental, physical, and social health, it is very crucial to recognize the computer addiction which is spreading like a sweet poison in the society. There is no shame in seeking help from others. Addiction to the computer should be taken seriously as it does the same damages as alcohol, drug or any other form of addiction.
The craze for going hit on various social media is enough to point towards the addiction to social networking sites in every age group. Whether an adult or a kid, social media has blessed everyone with a (false) celebrity-like status. The mindset has become such that people can’t keep away from their social media updates for more than a few minutes. An addiction that has reached from our dining room to the bedroom and instead of its potential dangers, it is being welcomed in every house. It couldn’t get worse as for the solution to occur, the problem needs to exist according to the people, which is obviously not the case with today’s world.
There are many strong reasons and rewards working behind such blind addiction to social networking sites. One that tops the list is gaining fame. Hundreds of likes and followers give a false impression of feeling like a celebrity. Instant notification facility has made the situation even more pathetic. There are light app versions of almost every social networking site, which allows for a quick access anytime anywhere. It has become a huge market for showing off along with hollow and made-up compliments, where the phrase, ‘you scratch my back and I would scratch yours’ has become quite true.
The addiction to social networking sites breathes in the houses and bedrooms of the people. As a result, it is one of the leading causes of relationship break-ups and privacy disruption. The trend for gaining attention is making people more self-obsessed. Their mental and physical health is suffering. People have less time for members living in the same house than they have for somebody they have never even met for once in real life. Faceless communication also paves the path for infidelity, stalking, online abuse, and many privacy-related cyber crimes, let alone the physical health problems like a headache, mood swings, depression, guilt etc.
Strong will-power and proper planning are needed if one truly wishes to get rid of the addiction to social networking sites. For those who really mean to do this, there are options like deactivating the account completely. Certain apps record your log in time and send a warning signal as a reminder when one has exceeded the set weekly or daily limits. Searching the same satisfaction in more productive things like taking care of yourself, working on the diet, taking kids out for a picnic, indulging in various recreational activities are effective means to detoxify the mind and body and bring the addiction to an end.
We will have to understand that social media is there for a particular reason. It is good for networking and interacting with long-distance friends and business relations. Beyond that, a compulsive need to be online all the time, inability to find meaning in real life without staying active online are certainly issues that are red flags. In the end, addiction to social networking sites only ruins the time and opportunities that come along in real life and hence it is important to keep a check on our online presence, so that, we could really focus on things that really matter for us.
There is an official term for the addiction to video games, it is IGD (Internet Gaming Disorder). The world of video games is not a child’s play anymore. As we can see, it is not just the kids but even adults are so badly into the spell of online games that ruining their lives and important aspects of it doesn’t concern them anymore. Almost three percent of the world’s population has lost the track of time and life due to addiction to online games. They are installed and available everywhere, including the home computers, to cyber cafes, malls, and other gaming spaces, which makes it further difficult to get out of the trap.
The programmers design everything in such a way that people cannot help but fall into the bottomless pit of addiction to video games. There are stages, rules, rewards, a particular degree of challenges so that the game is neither too easy to lose interest nor too difficult that one would want to quit. People who are facing a tough time in their lives are more likely to develop anxiety, depression, and an escaping tendency from the real world problems, which pushes them into the virtual world of gaming. Internet gaming has become a trend and many youngsters feel the peer pressure to follow what their friends are doing. The chain goes on and there seems no limit to it.
Addiction to video games is not hard to track. If it is affecting your life, preventing you from thinking about the serious departments of life, and leaving you with no time and energy to tend to your own needs and that of your family, then, it is the case of IGD. Sadly, the minds of kids and teenagers are easier to manipulate and drag them into the instant reward loop, which endangers their health and future as well. Longer hours spent playing and watching the computer screen almost withers the mind and body. Kids lose interest in the study, their career is affected, and they hardly want to go out. Adults are becoming more immune to emotional needs of their loved ones, and getting more used to the virtual sphere.
In case of addiction to video games, prevention is possible only by acknowledging the harmful effects of it. Understanding how the consistent hours of sitting ideal and playing an unproductive game are eating up all the precious time and digging a large hole into their real lives is key to curb the addiction. Kids too need to be talked about the toxic nature of this mania. They need to be explained how it is ruining their career. Spending more time away from computers and in nature’s embrace is healing and detoxifies the mind and body. Severe cases of IGD may seek the help of therapies, where CBT has been seen to work very effectively.
For the sake of our health, it is important that we don’t give the remote control of our lives into the hands of the virtual world of machines. The prices are high and too much is at stake. The young ones learn from our actions. If they see us becoming enslaved to such addiction to video games, chances are high that they would follow the same path. One should seek help as early as possible so that not much damage is done.
And here comes the talk we have always wanted to avoid, our addiction to Facebook. Facebook addiction has crossed its tipping point long time back. After all, this particular social networking platform has made updating pictures, thoughts, and flaunting the happy moments of our lives a piece of cake. A large number of likes and notifications give us an adrenaline rush like nothing else. The features of tagging, poking, finding an old friend, chatting make Facebook a highly tempting place that has succeeded in luring users from all kinds of age groups. And the number is growing every day.
Research has shown that addiction to Facebook is not that plain and simple. There are various reasons which intensify our constant need to check the updates on Facebook. Trying hard to get many likes by posting pictures, sharing updates, or tagging multiple people just shows a person’s attention-seeking nature. Sharing every little sad thing that is going on in the life, ranting in the status updates, or scrolling down aimlessly is indicative of lower self-esteem and a negative mindset. One also gets an opportunity to silently peek into others’ lives which instantly satiates their appetite for drama but also gives rise to comparisons.
Effects of addiction to Facebook are disastrous. First of all, it has promoted stalking to a very great level. Getting involved in useless conflicts and arguments over social media updates related to religious or political views has done no less harm. It not only consumes the time and energy but does nothing to solve the issues in reality. People really have begun to behave like drug addicts, unable to spend a day without logging in to their account. Facebook addiction disturbs the sleep cycle, and also causes backaches, dry eyes, sabotages the concentration power, along with mood swings, desire for more isolation leading to the distance from the loved ones.
The best and most effective method to deal with an addiction to Facebook is to immediately and abruptly deactivate the account. The milder steps that can be taken are self-observation, restricting and tracking the number of hours logged in to Facebook account. One should look for the reasons why he/she feels the need to check the account every other minute. Is it for popularity, for attention, for stalking, or wandering there with no apparent reason, just to kill the time. Without understanding the basic factors behind the addiction, it would be quite hard to stop oneself from going back there time and again.
Once the reasons responsible for the addiction to Facebook come into the limelight, one should try to work and resolve those issues in a healthy way. Facebook addiction is only a reflection of other deeper and hidden issues of our minds that need to be taken care of. Taking care of one’s mental and physical health should be the top priority for all of us. And getting out of the addiction to Facebook would be a big milestone in that journey.
Sex is one of the most primitive and basic natural instincts of human beings, thus making the addiction to pornography an obvious one in comparison to other ones. In a way, people have always been keen to learn more about sex, but indulgence in pornography is a not a healthy way to do that. The luring nature of pornography makes it quite seamless to get a hold on the person’s mind. The compulsive appetite for watching porn destroys the family, relationships, and health of the addict.
Youngsters are more vulnerable and feel excited to gain uninhibited access to porns. The rush is new to them, expectancy and curiosity make it quite irresistible to them. Adults are equally prone to have this disorder. A significant reason responsible for the addiction to porn is boredom and eagerness to experience something that is less likely to happen in the real life. Loneliness, lack of interesting activities in the life, isolation from other family members, depression and anxiety are some of the most common factors which result in spending a heavy amount of time on watching porn.
The leading problems associated with addiction to porn are erectile dysfunction, loss of intimacy between the partners, irritability in case of not getting access to pornography. The addicts also develop a tendency to compulsively lie in order to hide their addiction. Porn addicts are more likely to cheat and behave dishonestly with their partners. For them, everything else takes a back seat. Even those parts of their life which need attention become secondary to them. This creates an atmosphere of distrust and frustration in the family. An attitude of carelessness creeps into the person towards his work. Moreover, porn gives rise to many sexual fantasies which have elements of violence, aggression leading to more and more sexual assault cases.
Out of many steps that can be taken to deal with the addiction to porns, one of the most effective has been seen to be CBT. The cognitive behavior therapy helps the person get comfortable with his own addictions and fantasies. One can express the guilt and weakness in front of the therapist without the fear of being judged. Apart from getting outside help, realizing that the addiction exists and will-power to get out of it, is an essential step towards solving the issue. For the family members, it is necessary to understand that the problem would not dissolve in few days. A healthy support of love and affection from the family members means a lot to the person struggling with the porn addiction.
A society where most of the adults and teenagers are getting into the trap of addiction to porns, a concern for their health becomes obvious. Watching pornography not only kills time in a very destructive manner, it also desensitizes the mass and pulls them into sexually aggressive and violent actions, which may threaten the other genders or even kids. Addiction to pornography is a prevalent problem and needs our attention. Dealing with it in a non-judgmental way and with patience is the only way out.
Addiction to gambling is not new. Even in historical times, it used to be a passion of many royal families. We have also read about the disasters it caused to their rulings and damages that came along with it. Centuries later, the situation is still the same, even worse than before. Due to the appearance of internet, virtual gambling has become a part of many lives and the detriments are not limited to just financial aspects now. Addiction to gambling has been considered of the same nature as any other addiction to drugs, alcohol, etc.
The basic cause that drives one to fall for addiction to gambling is the need for perpetual excitement. The zest for making quick and easy money is the main pull for investing in gambling. People fall for the cycle of winning, losing, and then the possibility of winning some more, which keeps the cycle on. Even after they have lost a large sum of money, they would still want to give it multiple tries just in the hope of making up the losses. Research has proved that addiction to gambling is also a common way to deal with anxiety, depression, sadness, and the need to work for survival.
To the addict, there is an endless chain of realizing the problem, then deciding to quit, and again start gambling after a while. In case of addiction to gambling, it becomes very hard for one to quit it even after suffering great personal and financial losses. The normal life looks dull to the person and the entire family is affected. This may give birth to guilt, shame, and even anger in the addict. The work life of the person gets troubled. There is a possibility of going into the debts that may continue forever. Even after understanding the serious nature of such consequences, it might not be possible for one to get over the addiction.
Facing the truth is important for both the addict and the family members of him/her. And the reality is, addiction to gambling cannot be dealt with overnight. The temptations and impulses of gambling may reappear time and again. Thus, it requires a great deal of patience, affection, and care to handle the long-term problem. Ignoring, taunting, or making loose comments about the addict tends to worsen the situation and push him away. Therapy should be considered keeping in mind that things won’t change the next day.
A healthy way of living needs to be pursued. If one is in some kind of financial crisis, then, keeping the expenditures in control may reduce the pressure. Talking to friends and family members and sharing about the addiction to gambling is helpful in curbing the spell. Gambling has wide nature of negative consequences. It not only ruins the bank balance, but also makes the kids, partners, and parents go through a lot. With a combined support and help, addiction to gambling can be minimized gradually and one might be able to live a normal and healthy life.
We cannot imagine our daily routine without our phones, we have such kind of addiction to smartphones. It has completely taken the control over our lives. The irony is we don’t see it as a problem. Most of the people would justify their phone usage by using excuses like work, networking, business needs, or for fun. But there is a difference between using a device and depending so much on it that one begins to feel anxious without it. In most of the cases, latter is the story. We feel desperate and anxious if we are made to stay away from the smartphone for more than a while. This compulsive habit is simply indicative of an addiction to smartphones.
Many psychological disorders like depression, anxiety, self-obsession, low self-esteem work behind the addiction to smartphones. The constant need to stay surrounded by updates, triggers, notifications, and approvals are also some of the major factors responsible for the condition. People trying to avoid some long-term stressful situations in their lives or those with attention-seeking tendencies are also very likely to suffer the same problem. Those living a life of loneliness, or having difficulty in a face-to-face interaction also feel the need to use phones more in comparison to others. The fear of missing out and feeling left-out is another reason for the phone addiction.
The biggest damage that addiction to smartphones has caused is dissolving the culture of personal meetings and interactions. Kids, youngsters, or adults prefer to talk over text or chat instead of going out and sitting together at some place. Adults are more locked with their smartphones due to consistent nagging by work emails and messages. Basically, the phones have hypnotized people into doing one thing or the other on a continuous basis, whether it is essential or not. The physical and mental symptoms include the ringing of ears, numb mind, further anxiety and depression, insomnia, and lower emotional states.
Prevention is better than cure. In order to prevent the development of addiction to smartphones in kids, phones should strictly be prohibited for them at least up to a certain age. Even for teenagers, there should be an accountability for how much phone usage is allowed to them on a daily basis. For adults as well, a time should be fixed after which they would put the phone on silent mode and look at it only the next day. A good idea is to follow some fun rules, like not using the phone while eating, not letting the phone disturb you while you are asleep or having quality time with your family.
Apart from ruining one’s social, mental, and physical health, the addiction to smartphones has been responsible for many fatal accidents too. A habit which looks so harmless conceals within many serious troubles. Smartphones are even hampering the relationships and bonding between two people. More usage also results in lack of warmth, indifference, and anxiety. For regaining the healthier version of society, it is important to limit the use of phones.
Introduction :
Addiction to video games is considered a behavioral addiction that can be characterized by an excessive use of video games (in the computer, tablet or smartphone), interfering with everyday activities. People who suffer from this addiction are compulsive gamers, then to isolate themselves from social activities, have frequent mood swings, less imagination, they are obsessed with the game achievements and then to underestimate events in their own life’s.
Video game addiction has different causes, the main reason might be the fact that the games are designed to be like that, making people want to play more. The video game industry is worried about their profits and are constantly trying to improve the games to make more people to play them and keep playing constantly. The idea is to make challenging games that take time and effort to get to the achievements, but there is also a worry to not make the game so difficult that the gamer would easily give up on playing. Addicted gamers never feel accomplished and are always searching for playing more and reaching new objectives, similar behavior in other addictions (like gambling addiction).
Being addicted to video games affect people’s life in many ways and depend on people’s age. There are 5 main problems associated with video games addiction like emotional problems (usually addicted gamers struggle with depression, social anxiety, loneliness, anger and sometimes shame for spending so much time playing games), financial problems (more common in adults and adolescents, that spend enormous amounts of money in video games and specific equipment’s to play), health problems (people addicted to video games develop poor sleeping habits, can neglect personal hygiene, don’t get physical activity and make poor choices eating) and social problems (as the addiction develops, most addicts spend less time with family, friends and significant others, prejudicing the relationships).
Prevention :
The first step to prevent an addiction is to avoid being exposed to the agent that leads to it. When the addiction is already installed treatment is the best way to get rid of those unhealthy habits, there are 4 main options to treat video games addiction, they are one-to-one counselling with a professional (specialist can have a better approach to treat each case differently), family therapy (by modifying the family systems, interactions and dynamics can help to treat video games addiction but it is necessary commitment from the family member in the entire process), attend video games addiction centers (in these centers there are various programs defined by mental health professionals, although they are extremely expensive), wilderness therapy (by removing the individual from environments were they can play video games, it is commonly used to treat various types of child and adolescent behavioral problems and has been showing to have good results against this addiction),
Conclusion :
Video games addiction is not considered (yet) a diagnosable disorder, although it is a real disorder with increasing expansion. Specialists consider that early interventions are necessary to control this disorder and it should be treated has many other.
Addiction to social networking site is a growing problem in nowadays society. Social networking sites started on 1997, but their popularity has been increasing every year, with millions of people active on websites and apps like Facebook, Instagram, Snapchat and Twitter. Every addiction is a compulsive behavior with negative consequences, for example, most people feel so compelled to anything that it starts taking over the productivity at work or school and let them affect their everyday life.
Being addicted to social media is these terms corresponds with a compulsion to use excessively social networks; the need to check for any news frequently, the need to always be online to be the first one to know about the gossiping, posting everything about their days and life’s or even stalking people’s profiles for hours.
There are many types of social networking addiction. It can be manifested using instant messaging with apps like WhatsApp, Facebook Messenger or even Skype. Microblogging can also be other type of social network addiction, people tend to tell about their day and thoughts in apps/sites like Twitter (the most successful platform of this kind. Gaming is another type of social networking addiction since it involves connecting with other people in game-inherent channels, popular games like World of Warcraft or League of Legends provide gamers various channels for gamers to interact. Also, online dating is a form of social network addiction since most users of apps like Tinder are looking for quick gratification (short relationships) and the ease to meet other people online.
The excessive using of social networking resulting in addiction is a huge problem between teenagers, studies performed on six countries in Europe has shown that when kids use social network more than 2 hours a day they start internalizing problems and decrease their academical performance and activity.
Addiction to social networking sites have been studied for psychologists and sociologists all over the world and they have found that the excessive use of social networks can lead to the same symptoms observed in people with substance addictions. The most common symptoms are salience, mood modification, tolerance, withdrawal, relapse and conflict to behavioral addictions. For some people (mostly shy, isolated or even too self-focused) using social networking, sharing their life’s or even stalking others is the most important activity they do during the day, making the addiction more severe. To prevent social networking addiction people should try to not engage excessively in any form of social network, remembering there is a offline world. Social networking addiction is a problem that affects people’s everyday life, if you know someone you think that suffers from this problem you should try to convince them to get help.
The manifestation of social networking is usually associated with people with maladaptive cognitions and exacerbation with external issues, that lead to an excessive use. Most of these people (who are addicted) claim that they have a tough time when comes to talk to people face to face, and feel the need of self-rewarding and satisfaction by getting the online attention they think they need. This can result in a vicious cycle where people neglect their relationships and their work to be online and feel better about themselves, then when they face the outside world they don’t feel happy or rewarded the same way they are online.
Get FREE Work-at-Home Job Leads Delivered Weekly!

Join more than 50,000 subscribers receiving regular updates! Plus, get a FREE copy of How to Make Money Blogging!
Message from Sophia!
No related posts.
No comments yet.
Leave a reply click here to cancel reply..
You must be logged in to post a comment.
Billionaires
- Donald Trump
- Warren Buffett
- Email Address
- Free Stock Photos
- Keyword Research Tools
- URL Shortener Tools
- WordPress Theme
Book Summaries
- How To Win Friends
- Rich Dad Poor Dad
- The Code of the Extraordinary Mind
- The Luck Factor
- The Millionaire Fastlane
- The ONE Thing
- Think and Grow Rich
- 100 Million Dollar Business
- Business Ideas
Digital Marketing
- Mobile Addiction
- Social Media Addiction
- Computer Addiction
- Drug Addiction
- Internet Addiction
- TV Addiction
- Healthy Habits
- Morning Rituals
- Wake up Early
- Cholesterol
- Reducing Cholesterol
- Fat Loss Diet Plan
- Reducing Hair Fall
- Sleep Apnea
- Weight Loss
Internet Marketing
- Email Marketing
Law of Attraction
- Subconscious Mind
- Vision Board
- Visualization
Law of Vibration
- Professional Life
Motivational Speakers
- Bob Proctor
- Robert Kiyosaki
- Vivek Bindra
- Inner Peace
Productivity
- Not To-do List
- Project Management Software
- Negative Energies
Relationship
- Getting Back Your Ex
Self-help 21 and 14 Days Course
Self-improvement.
- Body Language
- Complainers
- Emotional Intelligence
- Personality
Social Media
- Project Management
- Anik Singal
- Baba Ramdev
- Dwayne Johnson
- Jackie Chan
- Leonardo DiCaprio
- Narendra Modi
- Nikola Tesla
- Sachin Tendulkar
- Sandeep Maheshwari
- Shaqir Hussyin
Website Development
Wisdom post, worlds most.
- Expensive Cars
Our Portals: Gulf Canada USA Italy Gulf UK
Privacy Overview

Essay on Internet Addiction
Students are often asked to write an essay on Internet Addiction in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Internet Addiction
Introduction.
Internet addiction is a growing problem globally. It refers to excessive use of the internet, leading to negative impacts on a person’s life.
The main cause of internet addiction is the desire for online social interaction and entertainment. Online games, social media, and websites can be very engaging.
Internet addiction can lead to poor academic performance, lack of social skills, and health issues like eye strain and obesity due to physical inactivity.
It’s important to balance internet usage with other activities. Parents and teachers can help by setting limits and promoting healthy habits.
Also check:
- Paragraph on Internet Addiction
250 Words Essay on Internet Addiction
The advent of the internet has revolutionized human existence, providing limitless opportunities for learning, communication, and entertainment. However, this unprecedented access to information and connectivity has birthed a new form of dependency – internet addiction.
Understanding Internet Addiction
Internet addiction, also known as compulsive internet use, is characterized by excessive or poorly controlled preoccupations, urges, or behaviors regarding computer use and internet access. It is a psychological disorder that can lead to severe stress, anxiety, and a variety of other mental health problems.
Causes and Effects
The causes of internet addiction are multifaceted, ranging from the need for social interaction, escapism, or the thrill of exploring virtual realities. The effects, however, can be detrimental, leading to academic failure, job loss, and the breakdown of personal relationships.
Prevention and Treatment
Prevention is always better than cure. Encouraging healthy internet usage habits, promoting physical activities, and fostering real-life social interactions can help prevent this addiction. However, once addicted, professional help may be necessary. Cognitive-behavioral therapy has proven effective in treating internet addiction by helping individuals to identify and change patterns of thought that lead to compulsive behaviors.
In conclusion, while the internet has undoubtedly brought about vast benefits, it has also introduced new challenges. Internet addiction is a growing concern that requires our attention. By understanding its causes and effects, we can develop strategies to prevent and treat this modern-day affliction.
500 Words Essay on Internet Addiction
Internet addiction, also known as compulsive internet use, has emerged as a significant issue in the digital age. It is a psychological condition that involves excessive use of the internet, resulting in negative impacts on an individual’s life.
Internet addiction is characterized by an individual’s inability to control their use of the internet, which eventually interferes with their daily life, work, and relationships. It is not merely about the amount of time spent online but the obsession with internet activities to the point where it affects mental and physical health, personal relationships, and productivity.
Causes and Symptoms
The causes of internet addiction can be multifaceted. It can be a symptom of other underlying mental health issues like depression, anxiety, and stress disorders. The anonymity, ease of access, and perceived environment of acceptance and escape the internet offers can also contribute to its addictive potential. Symptoms may include preoccupation with the internet, inability to control online use, neglect of personal life, and emotional changes such as restlessness or irritability when internet use is limited.
Impacts of Internet Addiction
Internet addiction can have severe impacts. It can lead to a sedentary lifestyle, which can result in obesity, cardiovascular issues, and other health problems. It can also lead to sleep disorders due to late-night internet use. From a psychological perspective, it can increase feelings of loneliness, depression, and anxiety. It can also lead to academic or job failures due to a lack of concentration and reduced productivity.
Preventing internet addiction involves promoting healthy internet use. This can be achieved by setting time limits, taking regular breaks, and promoting a balanced lifestyle with physical activities and offline social interactions. Treatment for those already addicted often involves cognitive-behavioral therapy, which helps individuals identify problematic behaviors and develop coping strategies. In severe cases, medication may also be used under professional supervision.
In conclusion, internet addiction is a growing concern that requires attention. As we continue to embrace digital technology, it is crucial to promote healthy internet use and provide help for those struggling with addiction. It’s a call to action for researchers, mental health professionals, and society as a whole to understand and address this modern-day issue effectively.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Evolution of Internet
- Essay on Life Without Internet
- Essay on Influence of Internet on Children
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Drugs, Brains, and Behavior: The Science of Addiction Preface
How science has revolutionized the understanding of drug addiction.
For much of the past century, scientists studying drugs and drug use labored in the shadows of powerful myths and misconceptions about the nature of addiction. When scientists began to study addictive behavior in the 1930s, people with an addiction were thought to be morally flawed and lacking in willpower. Those views shaped society’s responses to drug use, treating it as a moral failing rather than a health problem, which led to an emphasis on punishment rather than prevention and treatment.
Today, thanks to science, our views and our responses to addiction and the broader spectrum of substance use disorders have changed dramatically. Groundbreaking discoveries about the brain have revolutionized our understanding of compulsive drug use, enabling us to respond effectively to the problem.
As a result of scientific research, we know that addiction is a medical disorder that affects the brain and changes behavior. We have identified many of the biological and environmental risk factors and are beginning to search for the genetic variations that contribute to the development and progression of the disorder. Scientists use this knowledge to develop effective prevention and treatment approaches that reduce the toll drug use takes on individuals, families, and communities.
Despite these advances, we still do not fully understand why some people develop an addiction to drugs or how drugs change the brain to foster compulsive drug use. This booklet aims to fill that knowledge gap by providing scientific information about the disorder of drug addiction, including the many harmful consequences of drug use and the basic approaches that have been developed to prevent and treat substance use disorders.
At the National Institute on Drug Abuse (NIDA), we believe that increased understanding of the basics of addiction will empower people to make informed choices in their own lives, adopt science-based policies and programs that reduce drug use and addiction in their communities, and support scientific research that improves the Nation’s well-being.
Nora D. Volkow, M.D. Director National Institute on Drug Abuse
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Neuropsychopharmacology
- v.46(10); 2021 Sep
Addiction as a brain disease revised: why it still matters, and the need for consilience
Markus heilig.
1 Center for Social and Affective Neuroscience, Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
James MacKillop
2 Peter Boris Centre for Addictions Research, McMaster University and St. Joseph’s Healthcare Hamilton, Hamilton, ON Canada
3 Homewood Research Institute, Guelph, ON Canada
Diana Martinez
4 New York State Psychiatric Institute and Columbia University Irving Medical Center, New York, NY USA
Jürgen Rehm
5 Institute for Mental Health Policy Research & Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health (CAMH), Toronto, ON Canada
6 Dalla Lana School of Public Health and Department of Psychiatry, University of Toronto (UofT), Toronto, ON Canada
7 Klinische Psychologie & Psychotherapie, Technische Universität Dresden, Dresden, Germany
8 Department of International Health Projects, Institute for Leadership and Health Management, I.M. Sechenov First Moscow State Medical University, Moscow, Russia
Lorenzo Leggio
9 Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, Translational Addiction Medicine Branch, National Institute on Drug Abuse Intramural Research Program and National Institute on Alcohol Abuse and Alcoholism Division of Intramural Clinical and Biological Research, National Institutes of Health, Baltimore and Bethesda, MD USA
Louk J. M. J. Vanderschuren
10 Department of Population Health Sciences, Unit Animals in Science and Society, Faculty of Veterinary Medicine, Utrecht University, Utrecht, the Netherlands
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that the brain disease view is deterministic, fails to account for heterogeneity in remission and recovery, places too much emphasis on a compulsive dimension of addiction, and that a specific neural signature of addiction has not been identified. We acknowledge that some of these criticisms have merit, but assert that the foundational premise that addiction has a neurobiological basis is fundamentally sound. We also emphasize that denying that addiction is a brain disease is a harmful standpoint since it contributes to reducing access to healthcare and treatment, the consequences of which are catastrophic. Here, we therefore address these criticisms, and in doing so provide a contemporary update of the brain disease view of addiction. We provide arguments to support this view, discuss why apparently spontaneous remission does not negate it, and how seemingly compulsive behaviors can co-exist with the sensitivity to alternative reinforcement in addiction. Most importantly, we argue that the brain is the biological substrate from which both addiction and the capacity for behavior change arise, arguing for an intensified neuroscientific study of recovery. More broadly, we propose that these disagreements reveal the need for multidisciplinary research that integrates neuroscientific, behavioral, clinical, and sociocultural perspectives.
Introduction
Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that “addiction is a brain disease”, articulated a set of implications of this position, and outlined an agenda for realizing its promise [ 1 ]. The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the efforts of researchers, and resource allocation by funding agencies. A subsequent 2000 paper by McLellan et al. [ 2 ] examined whether data justify distinguishing addiction from other conditions for which a disease label is rarely questioned, such as diabetes, hypertension or asthma. It concluded that neither genetic risk, the role of personal choices, nor the influence of environmental factors differentiated addiction in a manner that would warrant viewing it differently; neither did relapse rates, nor compliance with treatment. The authors outlined an agenda closely related to that put forward by Leshner, but with a more clinical focus. Their conclusion was that addiction should be insured, treated, and evaluated like other diseases. This paper, too, has been exceptionally influential by academic standards, as witnessed by its ~3000 citations to date. What may be less appreciated among scientists is that its impact in the real world of addiction treatment has remained more limited, with large numbers of patients still not receiving evidence-based treatments.
In recent years, the conceptualization of addiction as a brain disease has come under increasing criticism. When first put forward, the brain disease view was mainly an attempt to articulate an effective response to prevailing nonscientific, moralizing, and stigmatizing attitudes to addiction. According to these attitudes, addiction was simply the result of a person’s moral failing or weakness of character, rather than a “real” disease [ 3 ]. These attitudes created barriers for people with substance use problems to access evidence-based treatments, both those available at the time, such as opioid agonist maintenance, cognitive behavioral therapy-based relapse prevention, community reinforcement or contingency management, and those that could result from research. To promote patient access to treatments, scientists needed to argue that there is a biological basis beneath the challenging behaviors of individuals suffering from addiction. This argument was particularly targeted to the public, policymakers and health care professionals, many of whom held that since addiction was a misery people brought upon themselves, it fell beyond the scope of medicine, and was neither amenable to treatment, nor warranted the use of taxpayer money.
Present-day criticism directed at the conceptualization of addiction as a brain disease is of a very different nature. It originates from within the scientific community itself, and asserts that this conceptualization is neither supported by data, nor helpful for people with substance use problems [ 4 – 8 ]. Addressing these critiques requires a very different perspective, and is the objective of our paper. We readily acknowledge that in some cases, recent critiques of the notion of addiction as a brain disease as postulated originally have merit, and that those critiques require the postulates to be re-assessed and refined. In other cases, we believe the arguments have less validity, but still provide an opportunity to update the position of addiction as a brain disease. Our overarching concern is that questionable arguments against the notion of addiction as a brain disease may harm patients, by impeding access to care, and slowing development of novel treatments.
A premise of our argument is that any useful conceptualization of addiction requires an understanding both of the brains involved, and of environmental factors that interact with those brains [ 9 ]. These environmental factors critically include availability of drugs, but also of healthy alternative rewards and opportunities. As we will show, stating that brain mechanisms are critical for understanding and treating addiction in no way negates the role of psychological, social and socioeconomic processes as both causes and consequences of substance use. To reflect this complex nature of addiction, we have assembled a team with expertise that spans from molecular neuroscience, through animal models of addiction, human brain imaging, clinical addiction medicine, to epidemiology. What brings us together is a passionate commitment to improving the lives of people with substance use problems through science and science-based treatments, with empirical evidence as the guiding principle.
To achieve this goal, we first discuss the nature of the disease concept itself, and why we believe it is important for the science and treatment of addiction. This is followed by a discussion of the main points raised when the notion of addiction as a brain disease has come under criticism. Key among those are claims that spontaneous remission rates are high; that a specific brain pathology is lacking; and that people suffering from addiction, rather than behaving “compulsively”, in fact show a preserved ability to make informed and advantageous choices. In the process of discussing these issues, we also address the common criticism that viewing addiction as a brain disease is a fully deterministic theory of addiction. For our argument, we use the term “addiction” as originally used by Leshner [ 1 ]; in Box 1 , we map out and discuss how this construct may relate to the current diagnostic categories, such as Substance Use Disorder (SUD) and its different levels of severity (Fig. 1) .

Risky (hazardous) substance use refers to quantity/frequency indicators of consumption; SUD refers to individuals who meet criteria for a DSM-5 diagnosis (mild, moderate, or severe); and addiction refers to individuals who exhibit persistent difficulties with self-regulation of drug consumption. Among high-risk individuals, a subgroup will meet criteria for SUD and, among those who have an SUD, a further subgroup would be considered to be addicted to the drug. However, the boundary for addiction is intentionally blurred to reflect that the dividing line for defining addiction within the category of SUD remains an open empirical question.
Box 1 What’s in a name? Differentiating hazardous use, substance use disorder, and addiction
Although our principal focus is on the brain disease model of addiction, the definition of addiction itself is a source of ambiguity. Here, we provide a perspective on the major forms of terminology in the field.
Hazardous Substance Use
Hazardous (risky) substance use refers to quantitative levels of consumption that increase an individual’s risk for adverse health consequences. In practice, this pertains to alcohol use [ 110 , 111 ]. Clinically, alcohol consumption that exceeds guidelines for moderate drinking has been used to prompt brief interventions or referral for specialist care [ 112 ]. More recently, a reduction in these quantitative levels has been validated as treatment endpoints [ 113 ].
Substance Use Disorder
SUD refers to the DSM-5 diagnosis category that encompasses significant impairment or distress resulting from specific categories of psychoactive drug use. The diagnosis of SUD is operationalized as 2 or more of 11 symptoms over the past year. As a result, the diagnosis is heterogenous, with more than 1100 symptom permutations possible. The diagnosis in DSM-5 is the result of combining two diagnoses from the DSM-IV, abuse and dependence, which proved to be less valid than a single dimensional approach [ 114 ]. Critically, SUD includes three levels of severity: mild (2–3 symptoms), moderate (4–5 symptoms), and severe (6+ symptoms). The International Classification of Diseases (ICD) system retains two diagnoses, harmful use (lower severity) and substance dependence (higher severity).
Addiction is a natural language concept, etymologically meaning enslavement, with the contemporary meaning traceable to the Middle and Late Roman Republic periods [ 115 ]. As a scientific construct, drug addiction can be defined as a state in which an individual exhibits an inability to self-regulate consumption of a substance, although it does not have an operational definition. Regarding clinical diagnosis, as it is typically used in scientific and clinical parlance, addiction is not synonymous with the simple presence of SUD. Nowhere in DSM-5 is it articulated that the diagnostic threshold (or any specific number/type of symptoms) should be interpreted as reflecting addiction, which inherently connotes a high degree of severity. Indeed, concerns were raised about setting the diagnostic standard too low because of the issue of potentially conflating a low-severity SUD with addiction [ 116 ]. In scientific and clinical usage, addiction typically refers to individuals at a moderate or high severity of SUD. This is consistent with the fact that moderate-to-severe SUD has the closest correspondence with the more severe diagnosis in ICD [ 117 – 119 ]. Nonetheless, akin to the undefined overlap between hazardous use and SUD, the field has not identified the exact thresholds of SUD symptoms above which addiction would be definitively present.
Integration
The ambiguous relationships among these terms contribute to misunderstandings and disagreements. Figure 1 provides a simple working model of how these terms overlap. Fundamentally, we consider that these terms represent successive dimensions of severity, clinical “nesting dolls”. Not all individuals consuming substances at hazardous levels have an SUD, but a subgroup do. Not all individuals with a SUD are addicted to the drug in question, but a subgroup are. At the severe end of the spectrum, these domains converge (heavy consumption, numerous symptoms, the unambiguous presence of addiction), but at low severity, the overlap is more modest. The exact mapping of addiction onto SUD is an open empirical question, warranting systematic study among scientists, clinicians, and patients with lived experience. No less important will be future research situating our definition of SUD using more objective indicators (e.g., [ 55 , 120 ]), brain-based and otherwise, and more precisely in relation to clinical needs [ 121 ]. Finally, such work should ultimately be codified in both the DSM and ICD systems to demarcate clearly where the attribution of addiction belongs within the clinical nosology, and to foster greater clarity and specificity in scientific discourse.
What is a disease?
In his classic 1960 book “The Disease Concept of Alcoholism”, Jellinek noted that in the alcohol field, the debate over the disease concept was plagued by too many definitions of “alcoholism” and too few definitions of “disease” [ 10 ]. He suggested that the addiction field needed to follow the rest of medicine in moving away from viewing disease as an “entity”, i.e., something that has “its own independent existence, apart from other things” [ 11 ]. To modern medicine, he pointed out, a disease is simply a label that is agreed upon to describe a cluster of substantial, deteriorating changes in the structure or function of the human body, and the accompanying deterioration in biopsychosocial functioning. Thus, he concluded that alcoholism can simply be defined as changes in structure or function of the body due to drinking that cause disability or death. A disease label is useful to identify groups of people with commonly co-occurring constellations of problems—syndromes—that significantly impair function, and that lead to clinically significant distress, harm, or both. This convention allows a systematic study of the condition, and of whether group members benefit from a specific intervention.
It is not trivial to delineate the exact category of harmful substance use for which a label such as addiction is warranted (See Box 1 ). Challenges to diagnostic categorization are not unique to addiction, however. Throughout clinical medicine, diagnostic cut-offs are set by consensus, commonly based on an evolving understanding of thresholds above which people tend to benefit from available interventions. Because assessing benefits in large patient groups over time is difficult, diagnostic thresholds are always subject to debate and adjustments. It can be debated whether diagnostic thresholds “merely” capture the extreme of a single underlying population, or actually identify a subpopulation that is at some level distinct. Resolving this issue remains challenging in addiction, but once again, this is not different from other areas of medicine [see e.g., [ 12 ] for type 2 diabetes]. Longitudinal studies that track patient trajectories over time may have a better ability to identify subpopulations than cross-sectional assessments [ 13 ].
By this pragmatic, clinical understanding of the disease concept, it is difficult to argue that “addiction” is unjustified as a disease label. Among people who use drugs or alcohol, some progress to using with a quantity and frequency that results in impaired function and often death, making substance use a major cause of global disease burden [ 14 ]. In these people, use occurs with a pattern that in milder forms may be challenging to capture by current diagnostic criteria (See Box 1 ), but is readily recognized by patients, their families and treatment providers when it reaches a severity that is clinically significant [see [ 15 ] for a classical discussion]. In some cases, such as opioid addiction, those who receive the diagnosis stand to obtain some of the greatest benefits from medical treatments in all of clinical medicine [ 16 , 17 ]. Although effect sizes of available treatments are more modest in nicotine [ 18 ] and alcohol addiction [ 19 ], the evidence supporting their efficacy is also indisputable. A view of addiction as a disease is justified, because it is beneficial: a failure to diagnose addiction drastically increases the risk of a failure to treat it [ 20 ].
Of course, establishing a diagnosis is not a requirement for interventions to be meaningful. People with hazardous or harmful substance use who have not (yet) developed addiction should also be identified, and interventions should be initiated to address their substance-related risks. This is particularly relevant for alcohol, where even in the absence of addiction, use is frequently associated with risks or harm to self, e.g., through cardiovascular disease, liver disease or cancer, and to others, e.g., through accidents or violence [ 21 ]. Interventions to reduce hazardous or harmful substance use in people who have not developed addiction are in fact particularly appealing. In these individuals, limited interventions are able to achieve robust and meaningful benefits [ 22 ], presumably because patterns of misuse have not yet become entrenched.
Thus, as originally pointed out by McLellan and colleagues, most of the criticisms of addiction as a disease could equally be applied to other medical conditions [ 2 ]. This type of criticism could also be applied to other psychiatric disorders, and that has indeed been the case historically [ 23 , 24 ]. Today, there is broad consensus that those criticisms were misguided. Few, if any healthcare professionals continue to maintain that schizophrenia, rather than being a disease, is a normal response to societal conditions. Why, then, do people continue to question if addiction is a disease, but not whether schizophrenia, major depressive disorder or post-traumatic stress disorder are diseases? This is particularly troubling given the decades of data showing high co-morbidity of addiction with these conditions [ 25 , 26 ]. We argue that it comes down to stigma. Dysregulated substance use continues to be perceived as a self-inflicted condition characterized by a lack of willpower, thus falling outside the scope of medicine and into that of morality [ 3 ].
Chronic and relapsing, developmentally-limited, or spontaneously remitting?
Much of the critique targeted at the conceptualization of addiction as a brain disease focuses on its original assertion that addiction is a chronic and relapsing condition. Epidemiological data are cited in support of the notion that large proportions of individuals achieve remission [ 27 ], frequently without any formal treatment [ 28 , 29 ] and in some cases resuming low risk substance use [ 30 ]. For instance, based on data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) study [ 27 ], it has been pointed out that a significant proportion of people with an addictive disorder quit each year, and that most afflicted individuals ultimately remit. These spontaneous remission rates are argued to invalidate the concept of a chronic, relapsing disease [ 4 ].
Interpreting these and similar data is complicated by several methodological and conceptual issues. First, people may appear to remit spontaneously because they actually do, but also because of limited test–retest reliability of the diagnosis [ 31 ]. For instance, using a validated diagnostic interview and trained interviewers, the Collaborative Studies on Genetics of Alcoholism examined the likelihood that an individual diagnosed with a lifetime history of substance dependence would retain this classification after 5 years. This is obviously a diagnosis that, once met, by definition cannot truly remit. Lifetime alcohol dependence was indeed stable in individuals recruited from addiction treatment units, ~90% for women, and 95% for men. In contrast, in a community-based sample similar to that used in the NESARC [ 27 ], stability was only ~30% and 65% for women and men, respectively. The most important characteristic that determined diagnostic stability was severity. Diagnosis was stable in severe, treatment-seeking cases, but not in general population cases of alcohol dependence.
These data suggest that commonly used diagnostic criteria alone are simply over-inclusive for a reliable, clinically meaningful diagnosis of addiction. They do identify a core group of treatment seeking individuals with a reliable diagnosis, but, if applied to nonclinical populations, also flag as “cases” a considerable halo of individuals for whom the diagnostic categorization is unreliable. Any meaningful discussion of remission rates needs to take this into account, and specify which of these two populations that is being discussed. Unfortunately, the DSM-5 has not made this task easier. With only 2 out of 11 symptoms being sufficient for a diagnosis of SUD, it captures under a single diagnostic label individuals in a “mild” category, whose diagnosis is likely to have very low test–retest reliability, and who are unlikely to exhibit a chronic relapsing course, together with people at the severe end of the spectrum, whose diagnosis is reliable, many of whom do show a chronic relapsing course.
The NESARC data nevertheless show that close to 10% of people in the general population who are diagnosed with alcohol addiction (here equated with DSM-IV “dependence” used in the NESARC study) never remitted throughout their participation in the survey. The base life-time prevalence of alcohol dependence in NESARC was 12.5% [ 32 ]. Thus, the data cited against the concept of addiction as a chronic relapsing disease in fact indicate that over 1% of the US population develops an alcohol-related condition that is associated with high morbidity and mortality, and whose chronic and/or relapsing nature cannot be disputed, since it does not remit.
Secondly, the analysis of NESARC data [ 4 , 27 ] omits opioid addiction, which, together with alcohol and tobacco, is the largest addiction-related public health problem in the US [ 33 ]. This is probably the addictive condition where an analysis of cumulative evidence most strikingly supports the notion of a chronic disorder with frequent relapses in a large proportion of people affected [ 34 ]. Of course, a large number of people with opioid addiction are unable to express the chronic, relapsing course of their disease, because over the long term, their mortality rate is about 15 times greater than that of the general population [ 35 ]. However, even among those who remain alive, the prevalence of stable abstinence from opioid use after 10–30 years of observation is <30%. Remission may not always require abstinence, for instance in the case of alcohol addiction, but is a reasonable proxy for remission with opioids, where return to controlled use is rare. Embedded in these data is a message of literally vital importance: when opioid addiction is diagnosed and treated as a chronic relapsing disease, outcomes are markedly improved, and retention in treatment is associated with a greater likelihood of abstinence.
The fact that significant numbers of individuals exhibit a chronic relapsing course does not negate that even larger numbers of individuals with SUD according to current diagnostic criteria do not. For instance, in many countries, the highest prevalence of substance use problems is found among young adults, aged 18–25 [ 36 ], and a majority of these ‘age out’ of excessive substance use [ 37 ]. It is also well documented that many individuals with SUD achieve longstanding remission, in many cases without any formal treatment (see e.g., [ 27 , 30 , 38 ]).
Collectively, the data show that the course of SUD, as defined by current diagnostic criteria, is highly heterogeneous. Accordingly, we do not maintain that a chronic relapsing course is a defining feature of SUD. When present in a patient, however, such as course is of clinical significance, because it identifies a need for long-term disease management [ 2 ], rather than expectations of a recovery that may not be within the individual’s reach [ 39 ]. From a conceptual standpoint, however, a chronic relapsing course is neither necessary nor implied in a view that addiction is a brain disease. This view also does not mean that it is irreversible and hopeless. Human neuroscience documents restoration of functioning after abstinence [ 40 , 41 ] and reveals predictors of clinical success [ 42 ]. If anything, this evidence suggests a need to increase efforts devoted to neuroscientific research on addiction recovery [ 40 , 43 ].
Lessons from genetics
For alcohol addiction, meta-analysis of twin and adoption studies has estimated heritability at ~50%, while estimates for opioid addiction are even higher [ 44 , 45 ]. Genetic risk factors are to a large extent shared across substances [ 46 ]. It has been argued that a genetic contribution cannot support a disease view of a behavior, because most behavioral traits, including religious and political inclinations, have a genetic contribution [ 4 ]. This statement, while correct in pointing out broad heritability of behavioral traits, misses a fundamental point. Genetic architecture is much like organ structure. The fact that normal anatomy shapes healthy organ function does not negate that an altered structure can contribute to pathophysiology of disease. The structure of the genetic landscape is no different. Critics further state that a “genetic predisposition is not a recipe for compulsion”, but no neuroscientist or geneticist would claim that genetic risk is “a recipe for compulsion”. Genetic risk is probabilistic, not deterministic. However, as we will see below, in the case of addiction, it contributes to large, consistent probability shifts towards maladaptive behavior.
In dismissing the relevance of genetic risk for addiction, Hall writes that “a large number of alleles are involved in the genetic susceptibility to addiction and individually these alleles might very weakly predict a risk of addiction”. He goes on to conclude that “generally, genetic prediction of the risk of disease (even with whole-genome sequencing data) is unlikely to be informative for most people who have a so-called average risk of developing an addiction disorder” [ 7 ]. This reflects a fundamental misunderstanding of polygenic risk. It is true that a large number of risk alleles are involved, and that the explanatory power of currently available polygenic risk scores for addictive disorders lags behind those for e.g., schizophrenia or major depression [ 47 , 48 ]. The only implication of this, however, is that low average effect sizes of risk alleles in addiction necessitate larger study samples to construct polygenic scores that account for a large proportion of the known heritability.
However, a heritability of addiction of ~50% indicates that DNA sequence variation accounts for 50% of the risk for this condition. Once whole genome sequencing is readily available, it is likely that it will be possible to identify most of that DNA variation. For clinical purposes, those polygenic scores will of course not replace an understanding of the intricate web of biological and social factors that promote or prevent expression of addiction in an individual case; rather, they will add to it [ 49 ]. Meanwhile, however, genome-wide association studies in addiction have already provided important information. For instance, they have established that the genetic underpinnings of alcohol addiction only partially overlap with those for alcohol consumption, underscoring the genetic distinction between pathological and nonpathological drinking behaviors [ 50 ].
It thus seems that, rather than negating a rationale for a disease view of addiction, the important implication of the polygenic nature of addiction risk is a very different one. Genome-wide association studies of complex traits have largely confirmed the century old “infinitisemal model” in which Fisher reconciled Mendelian and polygenic traits [ 51 ]. A key implication of this model is that genetic susceptibility for a complex, polygenic trait is continuously distributed in the population. This may seem antithetical to a view of addiction as a distinct disease category, but the contradiction is only apparent, and one that has long been familiar to quantitative genetics. Viewing addiction susceptibility as a polygenic quantitative trait, and addiction as a disease category is entirely in line with Falconer’s theorem, according to which, in a given set of environmental conditions, a certain level of genetic susceptibility will determine a threshold above which disease will arise.
A brain disease? Then show me the brain lesion!
The notion of addiction as a brain disease is commonly criticized with the argument that a specific pathognomonic brain lesion has not been identified. Indeed, brain imaging findings in addiction (perhaps with the exception of extensive neurotoxic gray matter loss in advanced alcohol addiction) are nowhere near the level of specificity and sensitivity required of clinical diagnostic tests. However, this criticism neglects the fact that neuroimaging is not used to diagnose many neurologic and psychiatric disorders, including epilepsy, ALS, migraine, Huntington’s disease, bipolar disorder, or schizophrenia. Even among conditions where signs of disease can be detected using brain imaging, such as Alzheimer’s and Parkinson’s disease, a scan is best used in conjunction with clinical acumen when making the diagnosis. Thus, the requirement that addiction be detectable with a brain scan in order to be classified as a disease does not recognize the role of neuroimaging in the clinic.
For the foreseeable future, the main objective of imaging in addiction research is not to diagnose addiction, but rather to improve our understanding of mechanisms that underlie it. The hope is that mechanistic insights will help bring forward new treatments, by identifying candidate targets for them, by pointing to treatment-responsive biomarkers, or both [ 52 ]. Developing innovative treatments is essential to address unmet treatment needs, in particular in stimulant and cannabis addiction, where no approved medications are currently available. Although the task to develop novel treatments is challenging, promising candidates await evaluation [ 53 ]. A particular opportunity for imaging-based research is related to the complex and heterogeneous nature of addictive disorders. Imaging-based biomarkers hold the promise of allowing this complexity to be deconstructed into specific functional domains, as proposed by the RDoC initiative [ 54 ] and its application to addiction [ 55 , 56 ]. This can ultimately guide the development of personalized medicine strategies to addiction treatment.
Countless imaging studies have reported differences in brain structure and function between people with addictive disorders and those without them. Meta-analyses of structural data show that alcohol addiction is associated with gray matter losses in the prefrontal cortex, dorsal striatum, insula, and posterior cingulate cortex [ 57 ], and similar results have been obtained in stimulant-addicted individuals [ 58 ]. Meta-analysis of functional imaging studies has demonstrated common alterations in dorsal striatal, and frontal circuits engaged in reward and salience processing, habit formation, and executive control, across different substances and task-paradigms [ 59 ]. Molecular imaging studies have shown that large and fast increases in dopamine are associated with the reinforcing effects of drugs of abuse, but that after chronic drug use and during withdrawal, brain dopamine function is markedly decreased and that these decreases are associated with dysfunction of prefrontal regions [ 60 ]. Collectively, these findings have given rise to a widely held view of addiction as a disorder of fronto-striatal circuitry that mediates top-down regulation of behavior [ 61 ].
Critics reply that none of the brain imaging findings are sufficiently specific to distinguish between addiction and its absence, and that they are typically obtained in cross-sectional studies that can at best establish correlative rather than causal links. In this, they are largely right, and an updated version of a conceptualization of addiction as a brain disease needs to acknowledge this. Many of the structural brain findings reported are not specific for addiction, but rather shared across psychiatric disorders [ 62 ]. Also, for now, the most sophisticated tools of human brain imaging remain crude in face of complex neural circuit function. Importantly however, a vast literature from animal studies also documents functional changes in fronto-striatal circuits, as well their limbic and midbrain inputs, associated with addictive behaviors [ 63 – 68 ]. These are circuits akin to those identified by neuroimaging studies in humans, implicated in positive and negative emotions, learning processes and executive functions, altered function of which is thought to underlie addiction. These animal studies, by virtue of their cellular and molecular level resolution, and their ability to establish causality under experimental control, are therefore an important complement to human neuroimaging work.
Nevertheless, factors that seem remote from the activity of brain circuits, such as policies, substance availability and cost, as well as socioeconomic factors, also are critically important determinants of substance use. In this complex landscape, is the brain really a defensible focal point for research and treatment? The answer is “yes”. As powerfully articulated by Francis Crick [ 69 ], “You, your joys and your sorrows, your memories and your ambitions, your sense of personal identity and free will, are in fact no more than the behavior of a vast assembly of nerve cells and their associated molecules”. Social and interpersonal factors are critically important in addiction, but they can only exert their influences by impacting neural processes. They must be encoded as sensory data, represented together with memories of the past and predictions about the future, and combined with representations of interoceptive and other influences to provide inputs to the valuation machinery of the brain. Collectively, these inputs drive action selection and execution of behavior—say, to drink or not to drink, and then, within an episode, to stop drinking or keep drinking. Stating that the pathophysiology of addiction is largely about the brain does not ignore the role of other influences. It is just the opposite: it is attempting to understand how those important influences contribute to drug seeking and taking in the context of the brain, and vice versa.
But if the criticism is one of emphasis rather than of principle—i.e., too much brain, too little social and environmental factors – then neuroscientists need to acknowledge that they are in part guilty as charged. Brain-centric accounts of addiction have for a long time failed to pay enough attention to the inputs that social factors provide to neural processing behind drug seeking and taking [ 9 ]. This landscape is, however, rapidly changing. For instance, using animal models, scientists are finding that lack of social play early in life increases the motivation to take addictive substances in adulthood [ 70 ]. Others find that the opportunity to interact with a fellow rat is protective against addiction-like behaviors [ 71 ]. In humans, a relationship has been found between perceived social support, socioeconomic status, and the availability of dopamine D2 receptors [ 72 , 73 ], a biological marker of addiction vulnerability. Those findings in turn provided translation of data from nonhuman primates, which showed that D2 receptor availability can be altered by changes in social hierarchy, and that these changes are associated with the motivation to obtain cocaine [ 74 ].
Epidemiologically, it is well established that social determinants of health, including major racial and ethnic disparities, play a significant role in the risk for addiction [ 75 , 76 ]. Contemporary neuroscience is illuminating how those factors penetrate the brain [ 77 ] and, in some cases, reveals pathways of resilience [ 78 ] and how evidence-based prevention can interrupt those adverse consequences [ 79 , 80 ]. In other words, from our perspective, viewing addiction as a brain disease in no way negates the importance of social determinants of health or societal inequalities as critical influences. In fact, as shown by the studies correlating dopamine receptors with social experience, imaging is capable of capturing the impact of the social environment on brain function. This provides a platform for understanding how those influences become embedded in the biology of the brain, which provides a biological roadmap for prevention and intervention.
We therefore argue that a contemporary view of addiction as a brain disease does not deny the influence of social, environmental, developmental, or socioeconomic processes, but rather proposes that the brain is the underlying material substrate upon which those factors impinge and from which the responses originate. Because of this, neurobiology is a critical level of analysis for understanding addiction, although certainly not the only one. It is recognized throughout modern medicine that a host of biological and non-biological factors give rise to disease; understanding the biological pathophysiology is critical for understanding etiology and informing treatment.
Is a view of addiction as a brain disease deterministic?
A common criticism of the notion that addiction is a brain disease is that it is reductionist and in the end therefore deterministic [ 81 , 82 ]. This is a fundamental misrepresentation. As indicated above, viewing addiction as a brain disease simply states that neurobiology is an undeniable component of addiction. A reason for deterministic interpretations may be that modern neuroscience emphasizes an understanding of proximal causality within research designs (e.g., whether an observed link between biological processes is mediated by a specific mechanism). That does not in any way reflect a superordinate assumption that neuroscience will achieve global causality. On the contrary, since we realize that addiction involves interactions between biology, environment and society, ultimate (complete) prediction of behavior based on an understanding of neural processes alone is neither expected, nor a goal.
A fairer representation of a contemporary neuroscience view is that it believes insights from neurobiology allow useful probabilistic models to be developed of the inherently stochastic processes involved in behavior [see [ 83 ] for an elegant recent example]. Changes in brain function and structure in addiction exert a powerful probabilistic influence over a person’s behavior, but one that is highly multifactorial, variable, and thus stochastic. Philosophically, this is best understood as being aligned with indeterminism, a perspective that has a deep history in philosophy and psychology [ 84 ]. In modern neuroscience, it refers to the position that the dynamic complexity of the brain, given the probabilistic threshold-gated nature of its biology (e.g., action potential depolarization, ion channel gating), means that behavior cannot be definitively predicted in any individual instance [ 85 , 86 ].
Driven by compulsion, or free to choose?
A major criticism of the brain disease view of addiction, and one that is related to the issue of determinism vs indeterminism, centers around the term “compulsivity” [ 6 , 87 – 90 ] and the different meanings it is given. Prominent addiction theories state that addiction is characterized by a transition from controlled to “compulsive” drug seeking and taking [ 91 – 95 ], but allocate somewhat different meanings to “compulsivity”. By some accounts, compulsive substance use is habitual and insensitive to its outcomes [ 92 , 94 , 96 ]. Others refer to compulsive use as a result of increasing incentive value of drug associated cues [ 97 ], while others view it as driven by a recruitment of systems that encode negative affective states [ 95 , 98 ].
The prototype for compulsive behavior is provided by obsessive-compulsive disorder (OCD), where compulsion refers to repeatedly and stereotypically carrying out actions that in themselves may be meaningful, but lose their purpose and become harmful when performed in excess, such as persistent handwashing until skin injuries result. Crucially, this happens despite a conscious desire to do otherwise. Attempts to resist these compulsions result in increasing and ultimately intractable anxiety [ 99 ]. This is in important ways different from the meaning of compulsivity as commonly used in addiction theories. In the addiction field, compulsive drug use typically refers to inflexible, drug-centered behavior in which substance use is insensitive to adverse consequences [ 100 ]. Although this phenomenon is not necessarily present in every patient, it reflects important symptoms of clinical addiction, and is captured by several DSM-5 criteria for SUD [ 101 ]. Examples are needle-sharing despite knowledge of a risk to contract HIV or Hepatitis C, drinking despite a knowledge of having liver cirrhosis, but also the neglect of social and professional activities that previously were more important than substance use. While these behaviors do show similarities with the compulsions of OCD, there are also important differences. For example, “compulsive” substance use is not necessarily accompanied by a conscious desire to withhold the behavior, nor is addictive behavior consistently impervious to change.
Critics question the existence of compulsivity in addiction altogether [ 5 – 7 , 89 ], typically using a literal interpretation, i.e., that a person who uses alcohol or drugs simply can not do otherwise. Were that the intended meaning in theories of addiction—which it is not—it would clearly be invalidated by observations of preserved sensitivity of behavior to contingencies in addiction. Indeed, substance use is influenced both by the availability of alternative reinforcers, and the state of the organism. The roots of this insight date back to 1940, when Spragg found that chimpanzees would normally choose a banana over morphine. However, when physically dependent and in a state of withdrawal, their choice preference would reverse [ 102 ]. The critical role of alternative reinforcers was elegantly brought into modern neuroscience by Ahmed et al., who showed that rats extensively trained to self-administer cocaine would readily forego the drug if offered a sweet solution as an alternative [ 103 ]. This was later also found to be the case for heroin [ 103 ], methamphetamine [ 104 ] and alcohol [ 105 ]. Early residential laboratory studies on alcohol use disorder indeed revealed orderly operant control over alcohol consumption [ 106 ]. Furthermore, efficacy of treatment approaches such as contingency management, which provides systematic incentives for abstinence [ 107 ], supports the notion that behavioral choices in patients with addictions remain sensitive to reward contingencies.
Evidence that a capacity for choosing advantageously is preserved in addiction provides a valid argument against a narrow concept of “compulsivity” as rigid, immutable behavior that applies to all patients. It does not, however, provide an argument against addiction as a brain disease. If not from the brain, from where do the healthy and unhealthy choices people make originate? The critical question is whether addictive behaviors—for the most part—result from healthy brains responding normally to externally determined contingencies; or rather from a pathology of brain circuits that, through probabilistic shifts, promotes the likelihood of maladaptive choices even when reward contingencies are within a normal range. To resolve this question, it is critical to understand that the ability to choose advantageously is not an all-or-nothing phenomenon, but rather is about probabilities and their shifts, multiple faculties within human cognition, and their interaction. Yes, it is clear that most people whom we would consider to suffer from addiction remain able to choose advantageously much, if not most, of the time. However, it is also clear that the probability of them choosing to their own disadvantage, even when more salutary options are available and sometimes at the expense of losing their life, is systematically and quantifiably increased. There is a freedom of choice, yet there is a shift of prevailing choices that nevertheless can kill.
Synthesized, the notion of addiction as a disease of choice and addiction as a brain disease can be understood as two sides of the same coin. Both of these perspectives are informative, and they are complementary. Viewed this way, addiction is a brain disease in which a person’s choice faculties become profoundly compromised. To articulate it more specifically, embedded in and principally executed by the central nervous system, addiction can be understood as a disorder of choice preferences, preferences that overvalue immediate reinforcement (both positive and negative), preferences for drug-reinforcement in spite of costs, and preferences that are unstable ( “I’ll never drink like that again;” “this will be my last cigarette” ), prone to reversals in the form of lapses and relapse. From a contemporary neuroscience perspective, pre-existing vulnerabilities and persistent drug use lead to a vicious circle of substantive disruptions in the brain that impair and undermine choice capacities for adaptive behavior, but do not annihilate them. Evidence of generally intact decision making does not fundamentally contradict addiction as a brain disease.
Conclusions
The present paper is a response to the increasing number of criticisms of the view that addiction is a chronic relapsing brain disease. In many cases, we show that those criticisms target tenets that are neither needed nor held by a contemporary version of this view. Common themes are that viewing addiction as a brain disease is criticized for being both too narrow (addiction is only a brain disease; no other perspectives or factors are important) or too far reaching (it purports to discover the final causes of addiction). With regard to disease course, we propose that viewing addiction as a chronic relapsing disease is appropriate for some populations, and much less so for others, simply necessitating better ways of delineating the populations being discussed. We argue that when considering addiction as a disease, the lens of neurobiology is valuable to use. It is not the only lens, and it does not have supremacy over other scientific approaches. We agree that critiques of neuroscience are warranted [ 108 ] and that critical thinking is essential to avoid deterministic language and scientific overreach.
Beyond making the case for a view of addiction as a brain disease, perhaps the more important question is when a specific level of analysis is most useful. For understanding the biology of addiction and designing biological interventions, a neurobiological view is almost certainly the most appropriate level of analysis, in particular when informed by an understanding of the behavioral manifestations. In contrast, for understanding the psychology of addiction and designing psychological interventions, behavioral science is the natural realm, but one that can often benefit from an understanding of the underlying neurobiology. For designing policies, such as taxation and regulation of access, economics and public administration provide the most pertinent perspectives, but these also benefit from biological and behavioral science insights.
Finally, we argue that progress would come from integration of these scientific perspectives and traditions. E.O. Wilson has argued more broadly for greater consilience [ 109 ], unity of knowledge, in science. We believe that addiction is among the areas where consilience is most needed. A plurality of disciplines brings important and trenchant insights to bear on this condition; it is the exclusive remit of no single perspective or field. Addiction inherently and necessarily requires multidisciplinary examination. Moreover, those who suffer from addiction will benefit most from the application of the full armamentarium of scientific perspectives.
Funding and disclosures
Supported by the Swedish Research Council grants 2013-07434, 2019-01138 (MH); Netherlands Organisation for Health Research and Development (ZonMw) under project number 912.14.093 (LJMJV); NIDA and NIAAA intramural research programs (LL; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health); the Peter Boris Chair in Addictions Research, Homewood Research Institute, and the National Institute on Alcohol Abuse and Alcoholism grants AA025911, AA024930, AA025849, AA027679 (JM; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health).
MH has received consulting fees, research support or other compensation from Indivior, Camurus, BrainsWay, Aelis Farma, and Janssen Pharmaceuticals. JM is a Principal and Senior Scientist at BEAM Diagnostics, Inc. DM, JR, LL, and LJMJV declare no conflict of interest.
Acknowledgements
The authors want to acknowledge comments by Drs. David Epstein, Kenneth Kendler and Naomi Wray.
Author contributions
All authors jointly drafted the paper.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Share full article
Advertisement
Supported by
Guest Essay
Mass Tech Layoffs? Just Another Day in the Corporate Blender.

By Ashley Goodall
Mr. Goodall, who previously worked as an executive at Deloitte and at Cisco Systems, is the author of the forthcoming book “The Problem With Change.”
Silicon Valley, home of so many technological and workplace innovations, is rolling out another one: the unnecessary layoff.
After shedding over 260,000 jobs last year, the greatest carnage since the dot-com meltdown more than two decades ago, the major tech companies show little sign of letting up in 2024 despite being mostly profitable, in some cases handsomely so. In their words, the tech companies are letting people go to further the continuing process of aligning their structure to their key priorities , or “transformation” or becoming “ future ready .” Behind these generalities, however, some tech companies are using what has hitherto been an extreme measure in order to engineer a short-term bump in market sentiment.
Investors are indeed thrilled . Meta’s shares are up over 170 percent amid its downsizing talk. And where stock prices go, chief executives will generally follow, which means it is not likely to be long before the unnecessary layoff makes its appearance at another publicly traded company near you.
These layoffs are part of a tide of disruption that is continually churning the work days in corporations everywhere. If you’ve spent any amount of time working at a company of pretty much any size, you’ll be familiar with what I call the resulting “life in the blender”: the unrelenting uncertainty and the upheaval that have become constant features of business life today. A new leader comes in, promptly begins a reorganization and upends the reporting relationships you’re familiar with. Or a consultant suggests a new strategy, which takes up everyone’s time and attention for months until it’s back to business as usual, only with a new mission statement and slideware. Or, everyone’s favorite: A merger is announced and leads to all of these and more.
Now, no business prospers by standing still, and there is no improvement without change. Course corrections, re-orgs and strategic pivots are all necessary from time to time. Technological changes continue to demand the restructuring of major industries. But over the last quarter-century or so, the idea of disruption has also metastasized into a sort of cult, the credo of which holds that everything is to be disrupted, all the time, and that if you’re not changing everything, you’re losing.
You can take courses in disruption at the business schools of Stanford, Cornell, Columbia and Harvard. You can read, on the cover of a leading business magazine, about how to “Build a Leadership Team for Transformation: Your Organization’s Future Depends on It.” And if it is the catechism of chaos you’re after, you can buy the inspirational posters and chant the slogans: Fail fast; disrupt or be disrupted; move fast and break things. Part of this, of course, is a product of the hubris of the Silicon Valley technologists. But part, too, is the belief that the fundamental task of a leader is to instigate change. It is hard to remember a time when there was any other idea about how to manage a company.
Moreover, because a majority of corporate executives — together with the consultants and bankers who advise them, the activist investors who spur them on and the financial analysts who evaluate their efforts — have been raised according to this change credo, the constant churn becomes a sort of flywheel. A leader instigates some change, because that’s what a leader does. The advisers and investors and analysts respond positively, because they’ve been taught that change is always good. There’s a quick uptick in reputation or stock price or both, the executives — paid, remember, mostly in stock — feel they have been appropriately rewarded for maximizing shareholder value, and then everyone moves on to the next change.
But it’s hardly clear that this is having the desired result. Studies of merger and acquisition activity have pegged the rate at which they destroy — rather than increase — shareholder value at something between 60 and 90 percent; a Stanford business school professor, Jeffrey Pfeffer, has argued that layoffs seldom result in lower costs, increased productivity or a remedy for the underlying problems in a business; and few of us who have lived through re-orgs remember them as the occasion for a sudden blossoming of productivity and creativity.
Seen through the eyes of the people on the front lines, the reason for this gap between intent and outcome comes into tighter focus. After all, when the people around you are being “transitioned out,” or when you find yourself suddenly working for a new boss who has yet to be convinced of your competence, it’s a stretch to persuade yourself that all this change and disruption is leading to much improvement at all.
“It’s exhausting,” one person I spoke to about change at work told me. “It’s soul-sucking,” said another. One person told me that after the combination of two departments, his people were like deer in the headlights, unsure of what they should be working on. Another had 19 managers in 10 years. Another told me that perpetual change drained the energy from work: “You say the right things in the meetings, but you don’t necessarily do what needs to be done to make it happen.” Another learned to watch the managers and be alert when they stopped dropping by or communicating: “It is like before a tsunami, when the water goes. You don’t see the water, and then the tsunami comes — all of a sudden, it comes, hard. When everything is calm, I worry.”
Of the dozens of people I spoke to, every single one had some sort of change-gone-bad story to share. And these sorts of reactions are about more than simple frustration or discontent. They are rooted in the psychological response we humans experience when our sense of stability is shattered and our future feels uncertain, and indeed the scientific literature has much light to shed on exactly why life in the blender is so hard on us. Experimenters have found, for example, that our stress is greatest when uncertainty , not discomfort, is at its peak — and uncertainty is the calling card of change at work. Then there is the question of agency: a well-known series of experiments conducted by Steven Maier and Martin Seligman in the 1960s discovered that when we sense we are not in control of a situation we give up trying to make things better — this is “learned helplessness” setting in.
Other researchers have described our fundamental need, as a species, for belonging , and the importance of our social groupings — which helps to explain why we don’t like it when our teams are disassembled, reshuffled and reassembled. And others still have shown that we have — perhaps unsurprisingly! — a deep-seated need for things to make sense in our environment, a need that is so often thwarted by the generic C.E.O. statements and exaggerated cheer-speak with which most change initiatives are communicated.
But while the essential response of the human animal to uncertainty and disruption is hard-wired, the degree of change we introduce into our workplaces isn’t. It’s often a choice. We’ve reached this point because the business world seems to have decided that change is an unalloyed good, and so there is no amount of it that is too much, and no cost of it that is too great.
Were more leaders to be guided by the science of change, or by the stories that people on the front lines share, they would quickly discover that it is stability that is the foundation of improvement. Only once we begin to honor people’s psychological needs at work, by thinking twice before launching into the next shiny change initiative and by paying more heed to the rituals and relationships that allow all of us to point our efforts in a useful direction, can we begin to do justice to the idea that a company must be, first, a platform for human contribution if it is to be anything else at all.
Ashley Goodall, who previously worked as an executive at Deloitte and at Cisco Systems, is the author of the forthcoming book “The Problem With Change.”
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , X and Threads .
FutureVU: Sustainability

Vanderbilt creates Center for Sustainability, Energy and Climate
Posted by hamiltcl on Monday, April 1, 2024 in featured , FutureVU , GHG , Research .
Vanderbilt University will harness its global expertise in scientific discovery, technological innovation, public policy, law and education to launch the Vanderbilt Center for Sustainability, Energy and Climate (VSEC).
The multimillion-dollar investment follows a recommendation by an interdisciplinary working group to address the crucial societal challenge of ensuring a sustainable world. It is the latest center to be launched through Discovery Vanderbilt , an initiative of the Office of the Provost and one of three pathways in the university’s Dare to Grow campaign to support and extend the resources underpinning Vanderbilt’s most innovative research and education.
Previously announced centers include the Vanderbilt Center for Addiction Research , the Vanderbilt Policy Accelerator , and the Vanderbilt Center for Research on Inequality and Health .
“One of the defining hallmarks of Vanderbilt is our spirit of ‘radical collaboration’ where researchers across a wide range of disciplines join together with local and global partners to tackle some the most urgent issues of our time,” Provost C. Cybele Raver. “VSEC exemplifies this spirit, where this group of brilliant faculty members are taking on and solving complex and pressing challenges for climate, energy, and sustainability. It makes me so proud to see Vanderbilt so powerfully positioned to make tremendous contributions in these areas.”
Raver added that the university is embarking on a global search for an accomplished researcher and administrative leader to direct the center.
VSEC’s primary mission will focus on advancing multidisciplinary research that includes partnerships with communities, government, industry, national laboratories and other research universities. The center will also engage Vanderbilt’s world-class engineering, science, law, policy and education expertise to investigate areas such as:
- Energy Integration
- Resource Sustainability
- Climate Change Mitigation and Adaptation
- Systems Risk, Reliability, and Resilience
“Vanderbilt’s School of Engineering is the ideal setting for this forward-thinking cross-disciplinary center,” said Hiba Baroud , who co-led the strategic planning committee that recommended the creation of VSEC and who is serving as its interim director, said the center is unique because it tackles complex challenges that require advances in basic science as well as broad interdisciplinary applied research.
“We are taking a holistic approach to achieve sustainable development by examining how different aspects of climate change mitigation and adaptation affect each other,” said Baroud, who is the A. James and Alice B. Clark Foundation Faculty Fellow and Associate Chair of the Department of Civil Engineering. “We envision the center doing this not just in terms of making advances in different focus areas, but by pairing scientific discoveries and transformative technologies with implementation and policy adoption.”
Jonathan Gilligan , who was vice chair of the strategic planning committee and is director of the Vanderbilt Climate and Society Grand Challenge Initiative, said it is imperative for VSEC to view sustainability solutions through a wide lens, engaging all the schools and disciplines of the university on equal footing, as well as connecting with community, industry, and government partners.
“VSEC’s success will be measured by how deeply it engages the expertise of the entire university, including engineering, natural and social sciences, humanities, and professional disciplines such as law, management, and healthcare,” said Gilligan, professor of Earth and Environmental Sciences whose work explores the intersection of the natural sciences, social sciences, engineering, and public policy. “Its success will not be measured solely by the number of academic papers published or the amount of grant money it attracts, but on its ability to draw upon Vanderbilt’s distinctive strengths in trans-institutional and trans-disciplinary collaboration in order to advance the frontiers of transdisciplinary research on sustainability, to provide students with a world-class holistic education on climate change and environmental sustainability, and to apply the results of its research to delivering tangible benefits to society.”
Already, the center’s strategic planning committee has identified opportunities to perform rigorous testing of novel concepts and technologies by leveraging existing testbeds at Vanderbilt and developing new ones that address sustainable transportation, materials science, microgrid energy development and biomanufacturing.
The university seeks to hire a permanent director. Interested candidates should contact [email protected] .
Tags: climate change , featured , FutureVU , GHG , Research
Comments are closed
- Annual Report
- What You Can Do
- Subscribe to Newsletter
Quick Links
- PeopleFinder

IMAGES
VIDEO
COMMENTS
500 Words Essay on Addiction Understanding Addiction. Addiction is a serious issue that affects many people around the world. It is a state where a person cannot stop using a substance or engaging in a behavior, even if it is harmful. The person becomes dependent on the substance or the activity to feel good or normal. Types of Addiction
Addiction is an illness that requires, for most, professional help and that once you are an addict you are always an addict. Addiction is everywhere, from celebrity tabloids, to television, and possibly to a family member or close friend. There is alcoholism, drug abuse, and gambling. 2651 Words. 11 Pages.
500 Words Essay on Addiction. As we all know that excess of anything can be very dangerous, the same way, addiction of any kind can hamper the life quality of an individual. The phrase states that addiction is a family disease as one person uses and the whole family suffers. The above statement stands true in all its essence as the addict does ...
The view that addiction is a disease makes it an individual problem. That's dangerous. ... Guest Essay. It's Misleading to Call Addiction a Disease. Jan. 15, 2022
Drug addiction is a chronic disease characterized by drug seeking and use that is compulsive, or difficult to control, despite harmful consequences. Brain changes that occur over time with drug use challenge an addicted person's self-control and interfere with their ability to resist intense urges to take drugs.
Essay on Addiction: Addiction is an illness- be it a drug, habit, or a person, that changes the way our brain thinks, functions, and processes information. Addiction leads to compulsive behaviour that provides temporary pleasure but holds long-term harmful effects on an addict's life. The scientific panel defines addiction as a neural disorder where a […]
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that ...
This essay was also published by Health Affairs on January 3, 2022. ... Drug addiction is a chronic but treatable disorder with well-understood genetic and social contributors. It is not a sign of a person's weakness or bad character. Continued or intermittent use of drugs, even by people who know they have a disorder and are trying hard to ...
We will write a custom essay on your topic. Generally, addiction has led to broken morals, malpractices, distorted relationships, as well as significant health problems. It is notable that most addicts might not be aware of their deviant characters. Contextually, physical addiction incorporates a biological condition where an individual adjusts ...
Addiction is the key process that underlies substance use disorders, and research using animal models and humans has revealed important insights into the neural circuits and molecules that mediate addiction. ... The papers in this issue highlight new findings that are directly relevant to understanding, treating, and developing policies to ...
1 page / 621 words. Addiction is a complex and pervasive issue that affects individuals from all walks of life. In this essay, we will explore the addictions of Terry and Leon, two individuals who are in need of intervention in order to address their substance abuse problems. By examining... Substance Abuse.
Caffeine Addiction and Negative Effects. The thesis of this paper is that scientists need to reclassify caffeine as a potentially addictive stimulant drug. In addition to the potential to cause addictive behavior, caffeine can have an adverse effect on the […] The Case of Katie's Addiction.
Drug addiction is a complex and contentious issue that has sparked debates for decades. At the heart of this debate is the question of whether drug addiction should be viewed as a choice made by individuals or as a disease that requires medical treatment. This essay will explore the multifaceted nature of drug addiction, examining both the ...
There are many theories about the causes of addiction, the use and abuse of legal and illegal psychoactive substances. Biology, psychology, and social and cultural elements all play a role in the ...
the hallmark of addiction. Brain imaging studies of people with addiction show physical changes in areas of the brain that are critical to judgment, decision making, learning and memory, and behavior control.7Scientists believe that these changes alter the way the brain works and may help explain the compulsive and destructive behaviors of ...
Essay on Drug Addiction: Addiction refers to the harmful need to consume substances that have damaging consequences on the user. Addiction affects not just the body but also on the person's mental health and soundness of mind. Addiction is one of the most severe health problems faced around the world and is termed as a chronic disease.
Essay on Addiction. Addiction is a complex and multifaceted phenomenon that impacts individuals, families, and society at large. It transcends the mere act of indulging excessively in substances or behaviors; it is a chronic disorder involving brain mechanisms and psychological elements. This essay delves into the nature of addiction, its ...
Impact of Drug Addiction on Society. Drug addiction has been a significant issue worldwide for many decades, impacting not only individuals addicted to illegal substances but also the society surrounding them. This essay aims to explore the influence of drug addiction on society at the local, national, and global scale.
Essay on Addiction Introduction This essay on addiction throws light on all such compulsive behaviors which give pleasure on a temporary basis but have long-term harmful effects on a person's lives. In scientific terms, it is a neural disorder. The addictive behaviors may include but are not confined to substance abuse, like alcohol, marijuana, drugs like cocaine, excessive work, or even ...
Students are often asked to write an essay on Internet Addiction in their schools and colleges. And if you're also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic. Let's take a look… 100 Words Essay on Internet Addiction Introduction. Internet addiction is a growing problem globally.
For much of the past century, scientists studying drugs and drug use labored in the shadows of powerful myths and misconceptions about the nature of addiction. When scientists began to study addictive behavior in the 1930s, people with an addiction were thought to be morally flawed and lacking in willpower. Those views shaped society's ...
Another major flaw within the justice system is the overcriminalization of drug possession. The mistreatment of addiction in America leads to countless cases of people's lives being ruined by the disease. Data shows that addiction rates are twice as high among people struggling with poverty and unemployment (Correa).
Introduction. Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that "addiction is a brain disease", articulated a set of implications of this position, and outlined an agenda for realizing its promise [].The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the ...
The wave of unnecessary layoffs sweeping Silicon Valley is the latest evidence of corporate America's addiction to change for change's sake.
Diversity, equity and inclusion helps transcend barriers between patients and doctors. Republican efforts to undo DEI will make bridging biases in medicine still harder.
Previously announced centers include the Vanderbilt Center for Addiction Research, the ... "Its success will not be measured solely by the number of academic papers published or the amount of grant money it attracts, but on its ability to draw upon Vanderbilt's distinctive strengths in trans-institutional and trans-disciplinary ...