An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychol

Child and Adolescent Depression: A Review of Theories, Evaluation Instruments, Prevention Programs, and Treatments
Elena bernaras.
1 Developmental and Educational Department, University of the Basque Country, Donostia/San Sebastián, Spain
Joana Jaureguizar
2 Developmental and Educational Psychology Department, University of the Basque Country, Lejona, Spain
Maite Garaigordobil
3 Personality, Evaluation and Psychological Treatments Department, University of the Basque Country, Donostia/San Sebastián, Spain
Depression is the principal cause of illness and disability in the world. Studies charting the prevalence of depression among children and adolescents report high percentages of youngsters in both groups with depressive symptoms. This review analyzes the construct and explanatory theories of depression and offers a succinct overview of the main evaluation instruments used to measure this disorder in children and adolescents, as well as the prevention programs developed for the school environment and the different types of clinical treatment provided. The analysis reveals that in mental classifications, the child depression construct is no different from the adult one, and that multiple explanatory theories must be taken into account in order to arrive at a full understanding of depression. Consequently, both treatment and prevention should also be multifactorial in nature. Although universal programs may be more appropriate due to their broad scope of application, the results are inconclusive and fail to demonstrate any solid long-term efficacy. In conclusion, we can state that: (1) There are biological factors (such as tryptophan—a building block for serotonin-depletion, for example) which strongly influence the appearance of depressive disorders; (2) Currently, negative interpersonal relations and relations with one's environment, coupled with social-cultural changes, may explain the increase observed in the prevalence of depression; (3) Many instruments can be used to evaluate depression, but it is necessary to continue to adapt tests for diagnosing the condition at an early age; (4) Prevention programs should be developed for and implemented at an early age; and (5) The majority of treatments are becoming increasingly rigorous and effective. Given that initial manifestations of depression may occur from a very early age, further and more in-depth research is required into the biological, psychological and social factors that, in an interrelated manner, may explain the appearance, development, and treatment of depression.
Introduction
Depression is the principal cause of illness and disability in the world. The World Health Organization (WHO) has been issuing warnings about this pathology for years, given that it affects over 300 million people all over the world and is characterized by a high risk of suicide (the second most common cause of death in those aged between 15 and 29) [World Health Organization (WHO), 2017 ]. Studies on the child population which use self-reports to evaluate severe symptoms of depression, specifically the Children's Depression Inventory (CDI, Kovacs, 1992 ) and the Children's Depression Scale (CDS, Lang and Tisher, 1978 ), have observed prevalence rates of, for example, 4% in Spain (Demir et al., 2011 ; Bernaras et al., 2013 ), 6% in Finland (Puura et al., 1997 ), 8% in Greece (Kleftaras and Didaskalou, 2006 ), 10% in Australia (McCabe et al., 2011 ), and 25% in Colombia (Vinaccia et al., 2006 ). The main classifications of mental disorders are the Diagnostic and Statistical Manual of Mental Disorders, DSM-5 (American Psychiatric Association, 2014 ), published by the American Psychiatric Association, which has become a key reference in clinical practice, and version 10 of the International Classification of Diseases (ICD-10, 1992), published by the WHO, which classifies and codifies all diseases, although initially its aim was to chart mortality rates. The new ICD-11 classification will be presented for approval to Member States at the World Health Assembly in May 2019, and is expected to come into effect on January 1, 2022 [World Health Organization (WHO), 2018 ]. The two classifications offer different categorizations of depressive disorders, although certain similarities do exist, and it should be borne in mind also that both have been criticized for hardly distinguishing at all between child and adult depression.
Throughout history, there have been many different explanatory theories of depression. Biological and psychological theories are the ones which have mainly tried to explain the origin of this mental disorder. Biological theories have, from a variety of different perspectives, postulated that depression may occur due to noradrenalin deficits (e.g., Schildkraut, 1965 ; Narbona, 2014 ), endocrine disorders (e.g. Birmaher et al., 1996 ), sleep-related disorders (e.g., Sivertsen et al., 2014 ; Pariante, 2017 ), alterations in brain structure (Whittle et al., 2014 ), or the influence of genetics (Scourfield et al., 2003 ). Psychological theories have attempted to explain depression on the basis of psychoanalysis and, more specifically, in terms of attachment theories (e.g., Bowlby, 1976 ; Ainsworth et al., 1978 ; Blatt, 2004 ; Bigelow et al., 2018 ), behavioral models (e.g., Skinner, 1953 ; Ferster, 1966 ; Lewinsohn, 1975 ), cognitive models (e.g., Seligman, 1975 ; Abramson et al., 1978 ; Beck, 1987 ), the self-control model (e.g., Rehm, 1977 ; Rehm et al., 1979 ), interpersonal theory (e.g., Markowitz and Weissman, 1995 ; Milrod et al., 2014 ), stressful life events (e.g., Reinherz et al., 1993 ; Frank et al., 1994 ), and sociocultural models (e.g., Lorenzo-Blanco et al., 2012 ; Chang et al., 2013 ; Reeves et al., 2014 ).
Evaluating depression accurately has been another concern upon which psychology has focused, with attention being centered specifically around diagnosing this pathology in childhood and adolescence. Although many diagnostic instruments have been developed and validated, mainly for the adolescent and adult stages of life, it is still difficult to find diagnostic tests for evaluating depression in children. Preventing depression is another aspect to which much importance is attached by the World Health Organization (WHO) ( 2017 ), which argues that school programs, interventions aimed at parents and specific exercises for the elderly population help reduce the prevalence of this pathology. Depression prevention programs do exist, but they are mainly targeted at adolescents and very few focus on children under the age of 10.
The treatment of depression is another aspect that should not be overlooked. In 2016, the WHO and the World Bank announced that investing in the treatment of depression and anxiety leads to four-fold returns, since these pathologies cost the global economy one trillion US dollars each year. Furthermore, they claimed that humanitarian emergencies and conflicts highlight a pressing need to broaden current therapeutic options. In this sense, the multiple different explanatory theories of depression have given rise to a plethora of different treatments (psychotherapeutic, behavioral, cognitive-behavioral, interpersonal, etc.) which are currently being analyzed with a high degree of precision and scientific rigor.
In light of the different aspects related to depression outlined above, the present study has the following aims: (1) To analyze the construct of depression offered by the two main mental disorder classifications (DSM-5 and ICD-10); (2) To provide an overview of the main explanatory theories of depression; (3) To outline the child and adolescent depression evaluation instruments most commonly used in scientific literature; (4) To provide a brief overview of child and adolescent depression prevention programs in the school environment; and (5) To describe the most scientifically rigorous and effective clinical treatments for this mental disorder.
The databases used for carrying out the searches were PubMed, PsycINFO, Web of Science, Scopus, Science Direct and Google Scholar, along with a range of different manuscripts. With the constant key word being depression, the search for information cross-referenced a series of other key words also, namely: childhood, adolescence, explanatory theories, etiology, evaluation instruments, prevention programs, and treatment. Searches were conducted for information published between 1970 and 2017.
Thus, first we describe the construct of depression and summarize the main explanatory theories. Next, we present the main evaluation instruments used to measure child and adolescent depression and report the results of a bibliographical review of prevention programs in school settings. Finally, we outline the main clinical treatments used nowadays to treat child and adolescent depression.
The Construct of Depression: DSM-5 and ICD-10
Depression features in both of the two most important global classifications: the DSM-5 and the ICD-10. As stated earlier in the introduction, the new ICD-11 classification will be presented for approval to Member States at the World Health Assembly in May 2019, and is expected to come into effect on January 1, 2022. The presentation of the new classification in 2019 will enable countries to plan for its implementation, prepare the necessary translations and train professionals accordingly [World Health Organization (WHO), 2018 ]. In texts published by WHO collaborators (Luciano, 2017 ), it has been suggested that the ICD-11 will include mood disorders within the mental and behavioral disorder category. However, until the final version is published, this information cannot be fully verified.
The two classifications (DSM-5 e IDC-10) offer different categorizations of depressive disorders, as shown in Table 1 . The WHO includes depressive disorders in the mood disorders category, although this review only focuses on Sections F32, F33, F34, and F38, which include the most frequent depressive disorders and which, in turn, contain subsections that will be further specified later on.
Depressive disorders according to the DSM-5 and the ICD-10.
According to the DSM-5, depressive disorders all have one common feature, namely the presence of sad, empty or irritable mood, accompanied by somatic and cognitive changes that significantly affect the individual's capacity to function (DSM-5). They may become a serious health problem if allowed to persist for long periods of time and occur with a moderate-to-severe degree of intensity. One important consequence of depression is the risk of suicide, which is, according the World Health Organization (WHO) ( 2017 ), the second most common cause of death among young people aged between 15 and 29.
The main novelty offered by the DSM-5 in its section on depressive disorders is the introduction to Disruptive mood dysregulation disorder (which should not be diagnosed before the age of 6 or after the age of 18). This disorder is characterized by severe recurrent temper outbursts manifested verbally (e.g., verbal rages) and/or behaviorally (e.g., physical aggression toward people or property). These outbursts often occur as the result of frustration and in order to be considered a diagnostic criterion must be inconsistent with the individual's developmental level, occur three or more times per week for at least a year in a number of different settings (at home, at school, etc.) and be severe in at least one of these. This disorder was added to the DSM-5 due to doubts arising in relation to how to classify and treat children presenting with chronic persistent irritability as opposed to other related disorders, specifically pediatric bipolar disorder. The prevalence of this disorder has been estimated at between 2 and 5%, with male children and teenage boys being more likely to suffer from it than their female counterparts.
Major Depressive Disorder
Major depressive disorder is characterized by a depressed mood most of the day, nearly every day, although in children and adolescents this mood may be irritable rather than depressed. The disorder causes a markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day, significant weight loss or gain, insomnia or hypersomnia, psychomotor agitation or retardation, fatigue or loss of energy, feelings of worthlessness, or excessive or inappropriate guilt, diminished ability to think or concentrate, recurrent thoughts of death, recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide. These symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. In the United States, the 12-month prevalence is ~7%, although it is three times higher among those aged between 18 and 29 than among those aged 60 or over. Moreover, the prevalence rates for women are ~1.5–3 times higher than for men.
Persistent Depressive Disorder (Dysthymia)
Persistent depressive disorder (dysthymia) is a consolidation of DSM-5-defined chronic major depressive disorder and dysthymic disorder, and is characterized by a depressed mood for most of the day, for more days than not, for at least 2 years. In children and adolescents, mood can be irritable and duration must be at least 1 year. The DSM-5 specifies that patients presenting symptoms that comply with the diagnostic criteria for major depressive disorder for 2 years should also be diagnosed with persistent depressive disorder. When the individual in question is experiencing a depressive mood episode, they must also present at least two of the following symptoms: poor appetite or overeating, insomnia or hypersomnia, low energy or fatigue, low self-esteem, poor concentration, or difficulty making decisions and feelings of hopelessness. The prevalence of this disorder in the United States is 0.5%.
Premenstrual Dysphoric Disorder
The diagnostic criterion for premenstrual dysphoric disorder states that, in the majority of menstrual cycles, at least five symptoms must be present during the last week before the start of menstruation, and individuals should start to feel better a few days later, with all symptoms disappearing completely or almost completely during the week after menstruation. The most important characteristics of this disorder are affective lability, intense irritability or anger, or increased interpersonal conflicts, markedly depressed mood and/or over-excitation, and symptoms of anxiety which may be accompanied by behavioral and somatic symptoms. Symptoms must be present during most menstrual cycles during the past year and must negatively affect occupational and social functioning. The most rigorous estimations of the prevalence of this disorder claim that 1.8% of women comply with the criterion but have no functional impairment, while 1.3% comply with the criterion and suffer functional impairment and other concomitant symptoms of another mental disorder.
Substance/Medication-Induced Depressive Disorder
Substance/medication-induced depressive disorder is characterized by the presence of the symptoms of a depressive disorder, such as major depressive disorder, induced by the consumption, inhalation or injection of a substance, with said symptoms persisting after the physiological effects or the effects of intoxication or withdrawal have disappeared. Some medication may generate depressive symptoms, which is why it is important to determine whether the symptoms were actually induced by the taking of the drug or whether the depressive disorder simply appeared during the period in which the medication was being taken. The prevalence of this disorder in the United States is 0.26%.
Depressive Disorder Due to Another Medical Condition
Depressive disorder due to another medical condition is characterized by the appearance of a depressed mood and a markedly diminished interest or pleasure in all activities within the context of another medical condition. The DSM-5 offers no information about the prevalence of this disorder.
The category Other specified depressive disorder is used when the symptoms characteristic of a depressive disorder appear and cause significant distress or impairment in social, occupational or other areas of functioning but do not comply with all the criteria of any depressive disorder, and the clinician opts to communicate the specific reason for this. In the Other unspecified depressive disorder category , on the other hand, the difference is that the clinician prefers not to specify the reason why the presentation fails to comply with all the criteria of a specific disorder and includes presentations about which there is insufficient information for giving a more specific diagnosis.
In the ICD-10, depressive disorders are included within the mood disorders category. The following disorders are analyzed below: single depressive episode, recurrent depressive disorder, and persistent mood (affective) disorders.
Single Depressive Episode
The classification Single depressive episode distinguishes between depressive episodes of varying severity: mild, moderate, and severe without psychotic symptoms. Characteristics common to all of them include lowering of mood, reduction of energy, and decrease in daily activity. There is a loss of interest in formerly pleasurable pursuits, a decrease in the capacity for concentration, and an increase in tiredness, even during activities requiring minimum effort. Changes occur in appetite, sleep is disturbed, self-esteem and self-confidence drop, ideas of guilt or worthlessness are present and the symptoms vary little from day to day. In its mildest form, two or three of the symptoms described above may be present, and the patient is able to continue with most of their daily activities. When the episode is moderate, four or more of the symptoms are usually present and the patient is likely to have difficulty continuing with ordinary activities. In its most severe form, several of the symptoms are marked and distressing, typically loss of self-esteem and ideas of worthlessness or guilt. Suicidal thoughts and acts are common and a number of somatic symptoms are usually present. If the depressive episode is with psychotic symptoms, it is characterized by the presence of hallucinations, delusions, psychomotor retardation, or stupor so severe that ordinary social activities are impossible; there may be danger to life from suicide, dehydration, or starvation.
Recurrent Depressive Disorder
Recurrent depressive disorder is characterized by repeated episodes of depression similar to those described above for single depressive episodes without mania. There may be brief episodes of mild mood elevation and over activity (hypomania) immediately after a depressive episode, sometimes precipitated by antidepressant treatment. The more severe forms of this disorder are very similar to manic-depressive depression, melancholia, vital depression, and endogenous depression. The first episode may occur at any age, from childhood to old age. The onset may be either acute or insidious and can last from a few weeks to many months. Recurrent depressive disorder can be mild or moderate, but in neither of these is there any history of mania. This section also includes recurrent depressive disorder currently in remission, in which the patient may have had two or more depressive episodes in the past, but has been free from depressive symptoms for several months.
Persistent Mood [Affective] Disorders
Persistent mood [affective] disorders are persistent and usually fluctuating disorders in which the majority of episodes are not sufficiently severe to warrant being diagnosed as hypomanic or mild depressive episodes. Since they last for many years and affect the patient's normal life, they involve considerable distress and disability. This section also includes cyclothymia and dysthymia. Cyclothymia is a persistent instability of mood involving numerous periods of depression and mild elation, none of which are sufficiently prolonged to justify a diagnosis of bipolar affective disorder or recurrent depressive disorder. This disorder is frequently found among the relatives of patients with bipolar affective disorder and some patients with cyclothymia eventually develop bipolar affective disorder. For its part, dysthymia is a chronic depression of mood, lasting at least several years, which is not sufficiently severe, or in which individual episodes are not sufficiently prolonged, to justify a diagnosis of mild, moderate, or severe recurrent depressive disorder.
Other Mood (Affective) Disorders
Finally, other mood (affective) disorders include any mood disorders that do not fall into the categories described above because they are not of sufficient severity or duration. They may be single, recurrent (brief), or specified episodes.
The manifestations and symptoms of depression vary in accordance with age and level of development. However, it is clear that the DSM-5 and the ICD-10 do not distinguish between adult and child depression, although by including disruptive mood dysregulation disorder, the DSM-5 does take into account the fact that children and young people aged between 7 and 18 may express their distress in other ways, through chronic, severe, and recurrent irritability manifested verbally and/or behaviorally. Similarly, major depressive disorder specifies that in children the mood may be irritable rather than depressed. However, no distinctions of this kind are found in the ICD-10, an absence which may lead to the faulty inference that the characteristics of child and adolescent depression are similar to those of adult depression.
Explanatory Theories of Depression
Depressive disorders cannot be explained by any single theory, since many different variables are involved in their onset and persistence. The principal biological and psychological theories were therefore taken as the main references for this section. Subsequently, the contributions made by each of these theories regarding depression were studied by conducting searches in PubMed, Web of Science, Science direct, and Google Scholar. With the constant key words being depression, child depression and adolescent depression, the search for information cross-referenced a series of other key words also in accordance with the specific theory in question. Due to the importance of some seminal works in relation to the development of psychological theories of depression, certain authors have remained key references for decades. A total of 64 bibliographical references were used. The following is a summary of the various explanations for the onset of depression, according to the different theoretical frameworks.
Biological Theories
If a mood disorder cannot be explained by family history or stressful life events, then it may be that the child or adolescent in question is suffering from a neurological disease. In such a case, depressive symptoms may manifest early in children and adolescents as epileptic syndromes, sleep disorders, chronic recurrent cephalalgias, several neurometabolic diseases, and intracranial tumors (Narbona, 2014 ).
Noradrenalin Deficit
Serotonin is a monoamine linked to adrenaline, norepinephrine, and dopamine which plays a key role, particularly in the brain, since it is involved in important life regulation functions (appetite, sleep, memory, learning, temperature regulation, and social behaviors, etc.), as well as many psychiatric pathologies (Nique et al., 2014 ). Serotonin modulates neuroplasticity, particularly during the early years of life, and dysfunctions in both systems contribute to the physiopathology of depression (Kraus et al., 2017 ). MRI tests in animals have revealed that a reduction in neuron density and size, as well as a reduction in hippocampal volume among depressive patients may be due to serotonergic neuroplasticity changes. Branchi ( 2011 ), however, argues that improving serotonin levels may increase the likelihood of both developing and recovering from the psychopathology, and underscores the role played by the social environment in this process. In this sense, Curley et al. ( 2011 ) point out that the quality of the social environment may influence the development and activity of neural systems, which in turn have an impact on behavioral, physiological, and emotional responses.
Endocrine Alterations
Age-related changes and the presence of biological risk factors, including endocrine, inflammatory or immune, cardiovascular and neuroanatomical factors, make people more vulnerable to depression (Clarke and Currie, 2009 ). Indeed, some studies suggest that depression may be linked to endocrine alterations: nocturnal cortisol secretions (Birmaher et al., 1996 ), nocturnal growth hormone secretion (Ryan et al., 1994 ), thyroid stimulating hormone secretion (Puig-Antich, 1987 ), melatonin and prolactin secretions (Waterman et al., 1994 ), high cortisol levels (Herane-Vives et al., 2018 ), or decreased growth hormone production (Dahl et al., 2000 ). Puberty and the accompanying hormonal and physical changes require special attention because it has been proposed that they could be associated with an increased incidence of depression (Reinecke and Simons, 2005 ).
Sleep Disorders
Sleep problems are often associated with situations of social deprivation, unemployment, or stressful life events (divorce, bad life habits, or poor working conditions) (Garbarino et al., 2016 ). It also seems, however, that sleep disorders are linked to the development of depression. This relationship occurs as a result of how insufficient sleep affects the hippocampus, heightening neural sensitivity to excitotoxic insult and vulnerability to neurotoxic challenges, resulting in a net decrease in gray matter in the hippocampus in the left orbitofrontal cortex (Novati et al., 2012 ).
For their part, Franzen and Buysse ( 2008 ) state that bidirectional associations between sleep disturbances (particularly insomnia) and depression make it more difficult to distinguish cause-effect relations between them. It is therefore unclear whether depression causes sleep disturbances or whether chronic sleep disturbances lead to the appearance of depression. What does seem clear, however, is that treating sleep disturbances (both insomnia and hypersomnia) may help reduce the severity of depression and accelerate recovery (Franzen and Buysse, 2008 ).
Longitudinal studies have identified insomnia as a risk factor for the onset or recurrence of depression in young people and adults (Sivertsen et al., 2014 ). In comparison with the non-clinical population, depressed children and adolescents report both trouble sleeping and longer sleep duration (Accardo et al., 2012 ).
For their part, Foley and Weinraub ( 2017 ) observed that, among preadolescent girls, early and later sleep problems directly or indirectly predicted a wide variety of social and emotional adjustment disorders (depressive symptoms, low school competence, poor emotion regulation, and risk-taking behaviors).
Altered Neurotransmission
Studies conducted over the past 20 years have shown that increased inflammation and hyperactivity of the hypothalamic–pituitary–adrenal (HPA) axis may explain major depression (Pariante, 2017 ). Some of the pathophysiological mechanisms of depression include altered neurotransmission, HPA axis abnormalities involved in chronic stress, inflammation, reduced neuroplasticity, and network dysfunction (Dean and Keshavan, 2017 ). Other studies report alterations in the brain structure: smaller hippocampus, amygdala, and frontal lobe (Whittle et al., 2014 ). Nevertheless, the underlying molecular and clinical mechanisms have yet to be discovered (Pariante, 2017 ). Major depressive disorder in children and adolescents has been associated with increased intracortical facilitation, a direct neurophysiological result of excessive glutamatergic neurotransmission. However, contrary to the findings in adults with depression, no deficits in cortical inhibition were found in children and adolescents with major depressive disorder (Croarkin et al., 2013 ).
Genetic Factors
Other studies have highlighted the importance of genetics in the onset of depression (40%) (Scourfield et al., 2003 ). It is important to recognize that a genetic predisposition to an excessive amygdala response to stress, or a hyperactive HPA axis (moderate hyperphenylalaninemia) due to stress during early childhood may trigger an excessive effect or alter an otherwise healthy psychological system (Dean and Keshavan, 2017 ). Kaufman et al. ( 2018 ) support a potential role for genes related to the homeobox 2 gene of Orthodenticle (OTX2) and to the OTX2-related gene in the physiopathology of stress-related depressive disorders in children. Furthermore, genetic anomalies in serotonergic transmission have been linked to depression. The serotonin-linked polymorphic region (5-HTTLPR) is a degenerate repeat in the gene which codes for the serotonin transporter (SLC6A4). The s/s genotype of this region is associated with a reduction serotonin expression, in turn linked to greater vulnerability to depression (Caspi et al., 2010 ).
For their part, Oken et al. ( 2015 ) claim that psychological disturbances may trigger changes in physiological parameters, such as DNA transcription, or may result in epigenetic modifications which alter the sensitivity of the neurotransmitter receptor.
Psychological Theories
This section outlines the different psychological theories which have attempted to explain the phenomenon of depression. Depression is a highly complex disorder influenced by multiple factors, and it is clear that no single theory can fully explain its etiology and persistence. It is likely that a more eclectic outlook must be adopted if we are to make any progress in determining the origin, development, and maintenance of this pathology.
Attachment-Informed Theories
Attachment theory was the term used by Bowlby ( 1976 ) to refer to a specific conceptualization of human beings' propensity to establish strong and long-lasting affective ties with other people. Bowlby ( 1969 , 1973 ) proposes that consistency, nurturance, protectiveness, and responsiveness in early interactions with caregivers contribute to the development of schemas or mental representations about the relationships of oneself with others, and that these schemas serve as models for later relationships. Bowlby's ethological model of attachment postulates that vulnerability to depression stems from early experiences which failed to satisfy the child's need for security, care and comfort, as well as from the current state of their intimate relations (Bowlby, 1969 , 1973 , 1988 ). Adverse early experiences can contribute to disturbances in early attachments, which may be associated with vulnerability for depression (Cummings and Cicchetti, 1990 ; Joiner and Coyne, 1999 ). Associations between insecure attachment among children and negative self-concept, sensitivity to loss, and an increased risk of depression in childhood and adolescence have been reported (Armsden et al., 1990 ; Koback et al., 1991 ; Kenny et al., 1993 ; Roelofs et al., 2006 ; Allen et al., 2007 ; Chorot et al., 2017 ). Relationships between secure attachment and depression seem also to be mediated by the development of maladaptive beliefs or schemas (Roberts et al., 1996 ; Reinecke and Rogers, 2001 ).
Thus, attachment theory has become a useful construct for conceptualizing many different disorders and provides valuable information for the treatment of depression (Reinecke and Simons, 2005 ).
Ainsworth described three attachment styles, in accordance with the child's response to the presence, absence, and return of the mother (or main caregiver): secure, anxious-avoidant, and anxious-resistant (Ainsworth et al., 1978 ). The least secure attachment styles may give rise to traumatic experiences during childhood, which in turn may result in the appearance of depressive symptoms.
Similarly, Hesse and Main ( 2000 ) argued that the central mechanism regulating infant emotional survival was proximity to attachment figures, i.e., those figures who help the child cope with frightening situations. Using Ainsworth's strange situation procedure, Main ( 1996 ) found that abused children engaged in more disorganized, disruptive, aggressive, and dissociative behaviors during both childhood and adolescence. Main ( 1996 ) also found that many people with clinical disorders have insecure attachment and that psychological-disoriented and disorganized children are more vulnerable.
For his part, Blatt ( 2004 ) explored the nature of depression and the life experiences which contribute to its appearance in more depth, identifying two types of depression which, despite a common set of symptoms, nevertheless have very different roots: (1) anaclitic depression, which arises from feelings of loneliness and abandonment; and (2) introjective depression, which stems from feelings of failure and worthlessness. This distinction is consistent with psychoanalytical formulations, since it considers defenselessness/dependency and desperation/negative feelings about oneself to be two key issues in depression.
Brazelton et al. ( 1975 ) found that at age 3 weeks, babies demonstrate a series of interactive behaviors during face-to-face mother-infant interactions. These behaviors were not found to be present in more disturbed interactions, which may trigger infant anxiety.
In a longitudinal study focusing on the relationship between risk of maternal depression and infant attachment behavior, Bigelow et al. ( 2018 ) analyzed babies at age 6 weeks, 4 and 12 months, finding that mothers at risk of depression soon after the birth of their child may have difficulty responding appropriately to their infant's attachment needs, giving rise to disorganized attachment, with all the psychological consequences that this may involve. Similarly, Beeghly et al. ( 2017 ) found that among infants aged between 2 and 18 months, greater maternal social support was linked to decreasing levels of maternal depressive symptoms over time, and that boys were more vulnerable than girls to early caregiving risks such as maternal depression, with negative consequences for mother-child attachment security during toddlerhood.
Authors such as Shedler and Westen ( 2004 ) have attempted to find solutions to the problems arising in relation to the DSM diagnostic categories, developing the Shedler Westen Assessment Procedure (SWAP-200) to capture the wealth and complexity of clinical personality descriptions and to identify possible diagnostic criteria which may better define personality disorders.
For their part, Ju and Lee ( 2018 ) argue that peer attachment reduces depression levels in at-risk children, and also highlight the curative aspect of attachment between adolescent peers.
Behavioral Models
The first explanations proposed by this model argued that depression occurs due to the lack of reinforcement of previously reinforced behaviors (Skinner, 1953 ; Ferster, 1966 ; Lewinsohn, 1975 ), an excess of avoidance behaviors and the lack of positive reinforcement (Ferster, 1966 ) or the loss of efficiency of positive reinforcements (Costello, 1972 ). A child with depression initially receives a lot of attention from his social environment (family, friends…), and behaviors such as crying, complaints or expressions of guilt are reinforced. When these depressive behaviors increase, the relationship with the child becomes aversive, and the people who used to accompany the child avoid being with him, which contributes to aggravating his depression (Lewinsohn, 1974 ). Low reinforcement rates can be explained by maternal rejection and lower parental support (Simons and Miller, 1987 ), by a lower rate of reinforcement offered to their children by mothers of depressed children (Cole and Rehm, 1986 ), or by low social competence (Shah and Morgan, 1996 ).
Depression is mainly a learned phenomenon, related to negative interactions between the individual and his or her environment (e.g., low rate of reinforcement or unsatisfactory social relations). These interactions are influenced by cognitions, behaviors and emotions (Antonuccio et al., 1989 ).
Cognitive Models
The attributional reformulation of the learned helplessness model (Abramson et al., 1978 ) and Beck's cognitive theory (Beck et al., 1979 ) are the two most widely-accepted cognitive theories among contemporary cognitive models of depression (Vázquez et al., 2000 ).
Learned helplessness is related to cognitive attributions, which can be specific/global, internal/external, and stable/unstable (Hiroto and Seligman, 1975 ; Abramson et al., 1978 ). Global attribution implies the conviction that the negative event is contextually consistent rather than specific to a particular circumstance. Internal attribution is related to the belief that the aversive situation occurs due to individual conditions rather than to external circumstances. Stable attribution is the belief that the aversive situation is unchanging over time (Miller and Seligman, 1975 ). People prone to depression attribute negative events to internal, stable and global factors and make external, unstable, and specific attributions for success (Abramson et al., 1978 ; Peterson et al., 1993 ), a cognitive style also present in children and adolescents with depression (Gladstone and Kaslow, 1995 ).
The Information Processing model (Beck, 1967 ; Beck et al., 1979 ) postulates that depression is caused by particular stresses that evoke the activation of a schema that screens and codes the depressed individual's experience in a negative fashion (Ingram, 1984 , p. 443). Beck suggests that this distortion of reality is expressed in three areas, which he calls the “cognitive triad”: negative views about oneself, the world and the future as a result of their learning history (Beck et al., 1983 ). These beliefs are triggered by life events which hold special meaning for the subject (Beck and Alford, 2009 ).
Self-Control Model
This theory assumes that depression is due to deficits in the self-control process, which consists of three phases: self-monitoring, self-evaluation, and self-administration of consequences (Rehm, 1977 ; Rehm et al., 1979 ). In the self-monitoring phase, individuals attend only to negative events and tend to recognize only immediate, short-term consequences. In the self-evaluation phase, depressed individuals establish unrealistic evaluation criteria and inaccurately attribute their successes and failures. If self-evaluation is negative, in the self-administration of consequences phase the individual tends to engage very little in self-reinforcement and very frequently in self-punishment.
Both Rehm's self-control model (Rehm, 1977 ) and Bandura's conception of child depression (Bandura, 1977 ) assume that children internalize external control guidelines. These guidelines are related to family interaction patterns and both may contribute to the etiology or persistence of depression in children.
In a study conducted with children aged between 8 and 12 years, Kaslow et al. ( 1988 ) found that depressed children had a more depressive attributional style and more self-control problems.
Interpersonal Theory
This model, which is closely linked to attachment theories, aims to identify and find solutions for an individual's problems with depression in their interpersonal functioning. It suggests that the difficulties experienced are linked to unresolved grief, interpersonal disputes, transition roles and interpersonal deficits (Markowitz and Weissman, 1995 ).
Milrod et al. ( 2014 ) argue that pathological attachment during early childhood has serious consequences for adults' ability to experience and internalize positive relationships.
Similarly, various different studies have highlighted the fact that one of the variables that best predicts depression in children is peer relations (Bernaras et al., 2013 ; Garaigordobil et al., 2017 ).
Stressful Life Events
Studies focusing on the adult population have reported that between 60 and 70% of depressed adults experienced one or more stressful events during the year prior to the onset of major depression (Frank et al., 1994 ). In children and adolescents, modest associations have been found between stressful life events and depression (Williamson et al., 1995 ). For their part, Shapero et al. ( 2013 ) found that people who had suffered severe emotional abuse during childhood experienced higher levels of depressive symptoms when faced with current stressors. Sokratous et al. ( 2013 ) argue that the onset of depression is not only triggered by major stressful events, but rather, minor life events (dropping out of school, your father losing his job, financial difficulties in the family, losing friends, or the illness of a family member) may also influence the appearance of depressive symptoms.
Events such as the loss of loved ones, divorce of parents, mourning or exposure to suicide (either individually or collectively) have all been associated with the onset of depression in childhood (Reinherz et al., 1993 ). Factors such as a history of additional interpersonal losses, added stress factors, a history of psychiatric problems in the family and prior psychopathology (including depression) increase the risk of depression in adolescents (Brent et al., 1993 ). Birmaher et al. ( 1996 ) found that prior research into stressful life events in relation to early-onset depression had been based on data obtained from self-reports, making it difficult to determine the causal relationship, since events may be both the cause and consequence of depression.
However, not everyone exposed to this kind of traumatic experience becomes depressed. Personality and the moment at which events occur are both involved in the relationship between depression and stressful life events, although biological factors such as serotonergic functioning (Caspi et al., 2010 ) also exert an influence.
Sociocultural Models
These models postulate that cultural variables are responsible for the appearance of depressive symptoms. These variables are mainly acculturation and enculturation. In acculturation, structural changes are observed (economic, political, and demographic), along with changes in people's psychological behavior (Casullo, 2001 ). Some studies link increased suicide rates with economic recession (Chang et al., 2013 ; Reeves et al., 2014 ). Enculturation occurs when the older generation invites, induces or forces the younger generation to adopt traditional mindsets and behaviors.
In an attempt to better understand the influence of culture and family on depressive symptoms, Lorenzo-Blanco et al. ( 2012 ) tested an acculturation, cultural values and family functioning model with Hispanic students born in the United States. The results revealed that both family conflict and family cohesion were related to depressive symptoms.
Another study carried out with girls aged 7–10 years (Evans et al., 2013 ) observed that internalizing an unrealistically thin ideal body predicted disordered eating attitudes through body dissatisfaction, dietary restraint and depression.
Finally, the importance of family interactions in the onset of depressive symptoms cannot be overlooked. Parenting style has been identified as a key factor in children's and adolescents' psychosocial adjustment (Lengua and Kovacs, 2005 ). Parental behavior has been studied from two different perspectives: warmth and control. Warmth is linked to aspects such as engagement and expression of affection, respect, and positive concern by parents and/or principal caregivers (Rohner and Khaleque, 2003 ). In this sense, prior studies have identified a significant association between parental warmth and positive adjustment among adolescents (Barber et al., 2005 ; Heider et al., 2006 ). Rohner and Khaleque ( 2003 ) argue that children's psychological adjustment is closely linked to their perception of being accepted or rejected by their principal caregivers, and other studies have found that weaker support from parents is associated with higher levels of depression and anxiety among adolescents (Yap et al., 2014 ).
Similarly, Jaureguizar et al. ( 2018 ) found that a low level of perceived parental warmth was linked to high levels of clinical and school maladjustment, and that the weaker the parental control, the greater the clinical maladjustment. These authors also found that young people with negligent mothers and authoritarian fathers had higher levels of clinical maladjustment.
In short, according to the different theories, depression may be due to (1) biological reasons; (2) insecure attachment; (3) lack of reinforcement of previously-reinforced behaviors; (4) negative interpersonal relations and relations with one's environment and the resulting negative consequences; (5) attributions made by individuals about themselves, the world and their future; and (6) sociocultural changes. It is likely that no single theory can fully explain the genesis and persistence of depression, although currently, negative interpersonal relations and relations with one's environment and sociocultural changes (economic, political, and demographic) may explain the observed increase in the prevalence of depression.
Evaluation Instruments
Many different evaluation instruments can be used to measure child and adolescent depression. Tables 2 , ,3 3 outline the ones most commonly used in scientific literature. Table 2 summarizes the main self-administered tests that specifically measure child and adolescent depression, while Table 3 presents tests that measure child and adolescent depression among other aspects (i.e., broader or more general tests). Finally, Table 4 summarizes the main hetero-administered psychometric tests for assessing this pathology.
Self-administered psychometric tests designed specifically for evaluating child and adolescent depression.
KR-20, Kuder-Richardson coefficient (formula 20); κ, Cohen's kappa reliability co-efficient; PPV, Positive predictive value; NPV, Negative predictive value; AUC, Area under the Receiver Operating Characteristic Curve (AUC) .
Self-administered general psychometric tests which, among other variables, also assess child and adolescent depression.
Hetero-administered psychometric tests for assessing child and adolescent depression.
As shown in the tables above, there are several self-administered instruments that can be used with children from age 6 to 7 onwards, although their duration should be taken into consideration in order to avoid overtiring subjects. While it is clear that an effort has been made to design shorter measures (compare, for example, the 66 items of the CDS with the 16 items of the longest version of the KADS), the duration of the test should not be the only aspect taken into account when selecting an evaluation instrument.
One of the most widely used instruments to measure child depression in the scientific literature is the Children's Depression Inventory-CDI (Kovacs, 1985 ), which is based on the Beck Depression Inventory-BDI (Beck and Beamesderfer, 1974 ). Thus, it is based on Beck's cognitive theory of depression. Following this same theoretical line, the Children's Depression Scale-CDS (Lang and Tisher, 1978 ) was designed, but in this case, this instrument was not created based on another instrument previously designed for adult population (as in the case of the CDI), but instead from its beginnings, it was conceived exclusively to assess child depression. Chorpita et al. ( 2005 ) explain that the CDI measures a broader construct of negative affectivity rather than depression as a separate construct, and that it may be useful for screening for trait dimensions or personality features, whereas other instruments, such as the Revised Child Anxiety and Depression Scale-RCADS (Chorpita et al., 2000 ), measure a specific clinical syndrome.
Table 2 describes many other instruments that are very useful as screening tests for depression and depressive disorder, such as the Center for Epidemiological Studies Depression Scale for Children-CES-DC (Weissman et al., 1980 ) (based on the Center for Epidemiological Studies Depression Scale for Adults, CES-D; Radloff, 1977 ), the Mood and Feelings Questionnaire-MFQ (Angold et al., 1995 ), or the Depression Self-Rating Scale for Children-DSRS (Birleson, 1981 ). This last one, for example, is useful to measure moderate to severe depression in childhood and is based on the operational definition of depressive disorder, that is, a specific affective-behavior pattern that implies an impairment of a child's or adolescent's ability to function effectively in his/her environment (Birleson, 1981 ).
The cognitive and affective component of depression is the one that is most present in the instruments described in Table 2 . In fact, for example, the Short Mood and Feelings Questionnaire (SMFQ) includes the cognitive and affective items from the original MFQ item pool, in addition to some items related to tiredness, restlessness, and poor concentration (Angold et al., 1995 ). In the SMFQ, more than half of the items from the MFQ were removed, and even so, high correlations between the MFQ and the SMFQ were found (Angold and Costello, 1995 ), which may be indicating that the really important items were the cognitive and affective items that were maintained. Reynolds et al. ( 1985 ) defended that children could accurately report their cognitive and affective characteristics, so “ if one wishes to know how a child feels, ask the child” (Reynolds et al., 1985 , p. 524).
Depending on the specific aim of the evaluation or research study, a broader diagnostic measure, such as those outlined in Table 3 , may also provide valuable information. Finally, it is worth noting that only two hetero-administered instruments were found for teachers, with all others being clearly oriented toward the clinical field. In this sense, special emphasis should be placed on the need to develop valid and reliable instruments for teachers, since they may be key agents for detecting symptoms among their students. While it is important to train teachers in this sense, it is also important to provide them with instruments to help them assess their students. The instruments that are currently available have produced very different results as regards their correlation with students' self-reported symptoms, although in general, teachers tend to underestimate their students' depressive symptoms (Jaureguizar et al., 2017 ).
Child and Adolescent Depression Prevention Programs in the School Environment
Extant scientific literature was reviewed in order to summarize the main depression prevention programs for children and adolescents in school settings. The databases used for conducting the searches were PubMed, PsycINFO, Web of Science, Scopus, Science Direct, and Google Scholar, along with a range of different manuscripts. With the constant key word being depression, the search for information cross-referenced a series of other key words also, namely: “child * OR adolescent * ,” “prevent * program,” and “school OR school-based.” Searches were conducted for information published between January 1, 1970 and December 31, 2017.
First, articles were screened (i.e., their titles and abstracts were read and a decision was made regarding their possible interest for the review study). The inclusion criteria were that the study analyzed all the research subjects of the review study (depression, childhood, or adolescence and prevention programs in school settings), that study participants were aged between 6 and 18, that the study was published in a peer-reviewed journal and that it was written in either English or Spanish. Review studies and their references were also analyzed. Studies focusing mainly on psychiatric disorders other than depression were excluded.
Finally, 39 studies were selected for the review, which explored 8 prevention programs that are outlined in Table 5 . In general terms, child depression prevention programs are divided into two main categories: universal programs for the general population, and targeted programs aimed at either the at-risk population or those with a clear diagnosis. Although scientific literature reports that targeted programs obtain better outcomes than universal ones, the latter type nevertheless offer certain advantages, since they reach a larger number of people without the social stigma attached to having been specially selected (Roberts et al., 2003 ; Huggins et al., 2008 ). Thus, the ideal context for instigating universal child depression prevention programs is the school environment.
School-based child and adolescent depression prevention programs.
Type: T, targeted; U, universal .
Table 5 outlines the most important child depression prevention programs carried out in the school context. They are all cognitive-behavioral programs implemented either by psychologists or teachers with specialist training, consisting of between 8 and 15 sessions. Only a few universal programs designed to prevent the symptoms of depression focus on younger children, since most are targeted mainly at the adolescent population (Gillham et al., 1995 ; Barrett and Turner, 2001 ; Farrell and Barrett, 2007 ; Essau et al., 2012 ; Gallegos et al., 2013 ; Rooney et al., 2013 ). Indeed, in the present review, only four universal child depression prevention programs were found that were aimed at a younger age group (between 8 and 12): the Penn Resiliency Program, FRIENDS, the Aussie Optimism Program, and FORTIUS (see Table 5 ).
As shown in the table, the results of the various programs outlined are not particularly positive, since on many occasions the effects (if there are any) are not sustained over time or are limited in scope (being dependent on who applies the program or on the sex of the participant, etc.). Nor is the distinction between universal and targeted programs particularly clear as regards their effects, since although targeted programs may initially appear to be more effective, their impact is not found to be sustained in the long term.
Greenberg et al. ( 2001 ) argue that researchers should explain whether their prevention programs focus on one or various microsystems (basically family and school), mesosystems or exosystems, etc. (following the model described by Bronfenbrenner, 1979 ), or are centered exclusively on the individual and his or her environment, since this will influence the results reported. These same authors conclude that programs focused exclusively on children and adolescents themselves are less effective than those which aim to “educate” subjects and bring about positive changes in their family and school environments.
As Calear and Christensen ( 2010 ) point out in their review, some authors suggest that the fact that some targeted programs are aimed at people with high levels of depressive symptoms entails a broader range of possibilities for change; however, this does not help us understand why these changes are not sustained over time. Thus, further research is required in this field in order to identify what specific components of those programs observed to be effective actually have a positive impact on the level of depressive symptoms, how these programs are developed, who implements them and whether or not their effects are sustained in the short, medium, and long term.
Clinical Treatments for Depression
In order to draft this section, a search was conducted for the most commonly-used therapies with proven efficacy for treating depression. The databases used were PubMed, Web of Science, Science direct, and Google Scholar. The key words used in the search were treatment, depression, child depression, and adolescent depression. A total of 30 bibliographic references were used in the drafting of this summary, including the major contribution made by The American Psychological Association's Society of Clinical Psychology (American Psychological Association, Society of Clinical Psychology (APA), 2017 ) regarding the most effective psychological methods for treating depression.
Although the World Health Organization (WHO) ( 2017 ) claims that prevention programs reduce the risk of suffering from depression, it has yet to be ascertained what type of programs and what contents are the most effective. The WHO also states that there are effective treatments for moderate and severe depression, such as psychological treatments (behavioral activation, cognitive behavioral therapy, and interpersonal psychotherapy) and antidepressant drugs (although it also warns of adverse effects), as well as psychosocial treatments for cases of mild depression. Moreover, a study conducted with adolescents by Foster and Mohler-Kuo ( 2018 ) found that the combination of cognitive-behavioral therapy and fluoxetine (antidepressant drug) was more effective than drug therapy alone.
The efficacy of treatment with antidepressants has been called into question for some years now. Iruela et al. ( 2009 ) claim that tricyclic antidepressants (imipramine, clomipramine, amitriptyline) are not recommended in childhood and adolescence since no benefits other than the placebo effect have been proven and furthermore, they generate major side effects due to their cardiotoxicity. They are therefore particularly dangerous in cases of attempted suicide. These same authors also advise against the use of monoamine oxidase inhibitors (MAOIs) due to dietary restrictions, interactions with other medication and the lack of clinical trials with sufficiently large groups which guarantee their efficacy. SSRIs or serotonergic antidepressants are the ones that have been most extensively studied in this population. The most effective is fluoxetine, the use of which is recommended in association with cognitive psychotherapy for cases of moderate and severe child depression.
On another hand, Wagner and Ambrosini ( 2001 ) analyzed the efficacy of pharmacological treatment in children and adolescents and stated that, at best, antidepressant therapy for depressed youth was moderately effective. Peiró et al. ( 2005 ) indicate that there is a great debate about the safety of selective serotonin reuptake inhibitors (SSRIs) in childhood. SSRIs, except for fluoxetine in the United States, have never been authorized by any agency for use in children or adolescents, mainly because of the risk of suicide to which they are associated. In 1991, the Food and Drugs Administration (FDA) claimed that there was insufficient evidence to confirm a causal association between SSRIs and suicide. Vitiello and Ordoñez ( 2016 ) conducted a systematic review of the topic and found more than 30 controlled clinical trials in adolescents and a few studies with children. Most studies found no differences between studies that administered drugs and those that used placebo, but they did find fluoxetine to be effective. They noted that antidepressants increased the risk of suicide (suicidal ideation and behaviors) compared to studies that had used placebos. The authors recommend using antidepressants with caution in young people and limiting them to patients with moderate to severe depression, especially when psychosocial interventions are not effective or are not feasible.
As regards the effectiveness of psychodynamic treatments, Luyten and Blatt ( 2012 ) advocate the inclusion of psychoanalytic therapy in the treatment of child, adolescent and adult depression. After conducting a review of both the theoretical assumptions of psychodynamic treatments of depression and the evidence supporting the efficacy of these interventions, these authors concluded that brief psychoanalytic therapy (BPT) is as effective in treating depression as other active psychotherapeutic treatments or pharmacotherapy, and its effects tend to be maintained in the longer term. They also observed that the combination of BPT and medication obtained better results than medication alone. Longer-term psychoanalytic treatment (LTPT) was found to be effective for patients suffering from chronic depression and co-morbid personality problems. Together, the authors argue, these findings justify the inclusion of psychoanalytic therapy as a first-line treatment in adult, child, and adolescent depression.
In a qualitative study carried out by Brown ( 2018 ) on parents' expectations regarding the recovery of their depressed children, a direct relationship was observed between said expectations and type of attachment. Parents who remained more passive and expected expert helpers to fix their child experienced reduced hope months after finishing the program. However, when parents changed their interactions with their child and adopted more positive expectations regarding their cure, they felt a more sustained sense of hope. Moreover, when parents themselves participated in therapy sessions, as part of their child's treatment, they felt greater hope and effectiveness in contributing to their child's recovery.
The American Psychological Association's Society of Clinical Psychology [American Psychological Association, Society of Clinical Psychology (APA), 2017 ] has published a list of psychological treatments that have been tested with the most scientific rigor and which, moreover, have been found to be most effective in treating depression. These treatments are as follows:
- – Self-Management/Self-Control Therapy (Kanfer, 1970 ). Depression is due to selective attention to negative events and immediate consequences of events, inaccurate attributions of responsibility for events, insufficient self-reinforcement, and excessive self-punishment. During therapy, the patient is provided with information about depression and taught skills they can use in their everyday life. This 10-session program can be delivered either in group or individual formats, at any age.
- – Cognitive Therapy (Beck, 1987 ). Individuals suffering from depression are taught cognitive and behavioral skills to help them develop more positive beliefs about themselves, others, and the world. Méndez ( 1998 ) argues that therapists working with depressed children should pursue three changes: (1) Learn to value their own feelings; (2) Replace behaviors which generate negative feelings with more appropriate behaviors; and (3) Modify distorted thoughts and inaccurate reasoning. The number of sessions varies between 8 and 16 in patients with mild symptoms. Those with more severe symptoms show improvement after 16 sessions.
- – Interpersonal Therapy (Klerman et al., 1984 ). García and Palazón ( 2010 ) identified four typical focal points for tension in depression, related to loss (complicated mourning), conflicts (interpersonal disputes), change (life transitions), and deficits in relations with others (interpersonal deficits), which generate and maintain a depressive state. It uses certain behavioral strategies such as problem solving and social skills training and lasts between 12 and 16 sessions in the most severe cases, and between 3 and 8 sessions in milder cases.
- – Cognitive Behavioral Analysis System of Psychotherapy (McCullough, 2000 ). This therapy combines components of cognitive, behavioral, interpersonal, and psychodynamic therapies. According to McCullough ( 2003 ), it is the only therapy developed specifically to treat chronic depression. Patients undergoing this therapy generate more empathic behaviors and identify, change and heal interpersonal patterns related to depression. Patients are recommended to combine the therapy with a regime of antidepressant medication.
- – Behavior Therapy/Behavioral Activation (BA) (Martell et al., 2013 ). Depression prompts sufferers to disengage from their routines and become increasingly isolated. Over time, this isolation exacerbates their depressive symptoms. Depressed individuals lose opportunities to be positively reinforced through pleasant experiences or social activities. The therapy aims to increase patients' chances of being positively reinforced by increasing their activity levels and improving their social relations. The therapy usually lasts between 20 and 24 sessions, with the brief version consisting of between 8 and 15 sessions.
- – Problem-Solving Therapy (Nezu et al., 2013 ). The aim is to enhance patients' personal adjustment to their problems and stress using affective, cognitive, and behavioral strategies. The therapy usually comprises around 12 sessions, although substantial changes are generally observed from the fourth session onwards. This therapy is widely used in primary care. It is an adaptation that is easy to apply in general medicine by personnel working in those contexts, and can be completed in around 6 weeks (Areán, 2000 ).
The treatments that, according to the American Psychological Association, Society of Clinical Psychology (APA) ( 2017 ), have modest research support and could be used with children are as follows:
- – Rational Emotive Behavioral Therapy (Ellis, 1994 ). This short-term, present-focused therapy works on changing the thinking which contributes to emotional and behavioral problems using an active-directive, philosophical and empirical intervention model. Using the A-B-C model (A: events observed by the individual; B: Individual's interpretation of the observed event; C: Emotional consequences of the interpretations made), the aim is to bring about the cognitive restructuring of erroneous thoughts, so as to replace them with more rational ones. The most commonly used techniques are cognitive, behavioral, and emotional.
- – Self-System Therapy (Higgins, 1997 ). Depression occurs as the result of the individual's chronic failure to achieve their established goals. During therapy, patients review their situation, analyze their beliefs and, on the basis of the results, alter their regulation style and move toward a new vision of themselves. Therapy generally consists of between 20 and 25 sessions.
- – Short-Term Psychodynamic Therapy (Hilsenroth et al., 2003 ). The aim of this therapy is to help patients understand that past experiences influence current functioning, and to analyze affect and the expression of emotion. The therapy focuses on the therapeutic relationship, the facilitation of insight, the avoidance of uncomfortable topics and the identification of core conflictual relationship themes. It is usually combined with pharmacological treatment to alleviate depressive episodes.
- – Emotion-Focused Therapy (emotion regulation therapy or Greenberg's experiential therapy) (Greenberg, 2004 ). According to Greenberg et al. ( 2015 ), this therapy combines elements of client-based practices (Rogers, 1961 ), Gestalt therapy (Perls et al., 1951 ), the theory of emotions and a dialectic-constructivist meta-theory. The aim is to create a safe environment in which the individual's anxiety is reduced, thereby enabling them to confront difficult emotions, raising their awareness of said emotions, exploring their emotional experiences in more depth and identifying maladaptive emotional responses. The therapy is delivered in 8–20 sessions.
- – Acceptance and Commitment Therapy (Hayes, 2005 ). This theory has become increasingly popular over recent years and is the contextual or third-generation therapy that is supported by the largest body of empirical evidence. It is based on a realization of the importance of human language in experience and behavior and aims to change the relationship individuals have with depression and their own thoughts, feelings, memories, and physical sensations that are feared or avoided. Strategies are used to teach patients to decrease avoidance and negative cognitions, and to increase focus on the present. The aim is not to modify the content of the patient's thoughts, but rather to teach them how to change the way they analyze them, since any attempt to correct thoughts may, paradoxically, only serve to intensify them (Hayes, 2005 ).
Ferdon and Kaslow ( 2008 ), for their part, in a theoretical review of the treatment of depression in children and adolescents, concluded that the cognitive-behavioral-therapy-based specific programs of the Penn Prevention program meet the criteria to conduct effective interventions in children with depression. In adolescent depression, the cognitive-behavioral therapy and the Interpersonal Therapy–Adolescent seem to have a well-established efficacy. Weersing et al. ( 2017 ), in this same line, state that, although the efficacy of treatments in children is rather weak, cognitive-behavioral therapy is probably the most effective therapy. They also confirm that, in depressed adolescents, cognitive behavioral therapy, and interpersonal psychotherapy are appropriate interventions.
There are other studies also which focus on treatments for depression in childhood. For example, Crowe and McKay ( 2017 ) carried out a meta-analysis of the effects of Cognitive Behavioral Therapy (CBT) on children suffering from anxiety and depression, concluding that CBT can be considered an effective treatment for child depression. According to these authors, the majority of protocols for children have been adapted from protocols for adults, and the most common techniques are psychoeducation, self-monitoring, identification of emotions, problem solving, coping skills, and reward plans. Similarly, cognitive strategies include the identification of cognitive errors, also known as cognitive restructuring. In another meta-analysis conducted to analyze the efficacy and acceptability of CBT in cases of child depression, Yang et al. ( 2017 ) observed that, in comparison with the control groups that did not receive treatment, the experimental groups showed significant improvement, although they also pointed out that the relevance of this finding was limited due to the small size of the trial groups.
Another study carried out in Saudi Arabia concluded that student counseling in schools may help combat and directly reduce anxiety and depression levels among Saudi children and adolescents (Alotaibi, 2015 ).
Family-based treatment may also be effective in treating the interpersonal problems and symptoms observed among depressed children. The data indicate that the characteristics of the family environment predict recovery from persistent depression among depressed children (Tompson et al., 2016 ). In this sense, Tompson et al. ( 2017 ) compared the effects of a family-focused treatment for child depression (TCF-DI) with those of individual supportive psychotherapy among children aged 7–14 with depressive disorders. The results revealed that incorporating the family into the therapy resulted in a significant improvement in depressive symptoms, global response, functioning, and social adjustment.
To conclude this section, it can be stated that treatment for depression should be multifactorial and should bear in mind the personal characteristics of the patient, their coping strategy for problems, the type of relationship they have with themselves and the type of relationship they establish with their environment (friends, school, family, etc.). Thus, in order for the individual to attain the highest possible level of psychological wellbeing, attention should focus on both these and other related aspects.
Conclusions
The present review aims to shed some light on the complex and broad-ranging field of child and adolescent depression, starting with a review of the construct itself and its explanatory theories, before continuing on to analyze existing evaluation instruments, the main prevention programs currently being implemented and the various treatments currently being applied. All these aspects are intrinsically linked: how the concept is defined depends on the explanatory variables upon which said definition is based, and this in turn influences how we measure it and the variables we define as being key elements for its prevention and treatment.
It is interesting to note the low level of specificity of both the construct itself and the explanatory theories offered by child and adolescent psychology, which suggest that child depression can be understood on the basis of the adult version of the pathology. This may well be a basic error in our approach to depression among younger age groups. The fact that universal prevention programs specifically designed for children are obtaining only modest results may indicate that we have perhaps failed to correctly identify the key variables involved in the genesis and maintenance of child and adolescent depression.
The review of current child and adolescent depression prevention programs revealed that the vast majority coincide in adopting a cognitive-behavioral approach, with contents including social skills and problem solving training, emotional education, cognitive restructuring, and strategies for coping with anxiety. These contents are probably included because they are important elements in the treatment of depression, as shown in this review. But if their inclusion is important and effective in the treatment of depression, why do they not seem to be so effective in preventing this pathology? There are probably many factors linked to prevention programs which, in one way or another, influence their efficacy: who implements the program and what prior training they receive; the characteristics of the target group; group dynamics; how sessions are run; how the program is evaluated; and if the proposed goals are really attained (e.g., training in social skills may be key, but perhaps we are not training students correctly). Moreover, in universal prevention programs carried out in schools, the intervention focuses on students themselves rather than adopting a more holistic approach, as recommended by certain authors such as Greenberg et al. ( 2001 ). But, if we accept that depression is multifactorial and that risk and protection factors may be found not only in the school environment but also in the family and social contexts, should prevention not also be multifactorial?
There is therefore still much work to be done in order to fully understand child and adolescent depression and its causes, and so design more effective evaluation instruments and prevention and treatment programs. Given the important social and health implications of this disorder, we need to make a concerted effort to further our research in this field.
Author Contributions
MG designed the study and wrote the protocol. EB and JJ conducted literature review and provided summaries of previous research studies, and wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding. The Research Project was sponsored by the Alicia Koplowitz Foundation, with grant number FP15/62.
- Abramson L. Y., Seligman M. E. P., Teasdale J. D. (1978). Learned helplessness in humans: critique and reformulation . J. Abnorm. Psychol. 87 , 49–74. 10.1037/0021-843X.87.1.49 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Accardo J., Marcus C. L., Leonard M. B., Shults J., Meltzer L. J., Elia J. (2012). Associations between psychiatric comorbidities and sleep disturbances in children with attention-deficit/hyperactivity disorder . J. Dev. Behav. Pediatr. 33 , 97–105. 10.1097/DBP.0b013e31823f6853 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Achenbach T. M., Edelbrock C. S. (1985). Manual for the Child Behavior Checklist and Revised Child Behavior Profile . Burlington, VT: University Associates in Psychiatry. [ Google Scholar ]
- Ainsworth M., Blehar M., Waters E., Wall S. (1978). Patterns of Attachment . Hillsdale, NJ: Erlbaum. [ Google Scholar ]
- Allen J. P., Porter M., McFarland C., McElhaney K. B., Marsh P. (2007). The relation of attachment security to adolescents' paternal and peer relationships, depression, and externalizing behavior . Child Dev. 78 , 1222–1239. 10.1111/j.1467-8624.2007.01062.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alotaibi T. (2015). Combating anxiety and depression among school children and adolescents through student counselling in Saudi Arabia . Proc. Soc. Behav. Sci. 205 , 18–29. 10.1016/j.sbspro.2015.09.006 [ CrossRef ] [ Google Scholar ]
- American Psychiatric Association (2014). Manual Diagnóstico y Estad í stico de los Trastornos Mentales (DSM-5) [Diagnostic and Statistical Manual of Mental Disorders (DSM − 5)] Madrid: Médica Panamericana. [ Google Scholar ]
- American Psychological Association Society of Clinical Psychology (APA). (2017). Depression . Available online at: http://www.div12.org/psychological-treatments/disorders/depression/
- Angold A., Costello E. J. (1995). A test-retest reliability study of child-reported psychiatric symptoms and diagnoses using the Child and Adolescent Psychiatric Assessment (CAPA-C) . Psychol. Med. 25 , 755–762. [ PubMed ] [ Google Scholar ]
- Angold A., Costello E. J., Messer S. C., Pickles A., Winder F., Silver D. (1995). The development of a short questionnaire for use in epidemiological studies of depression in children and adolescents . Int. J. Methods Psychiatr. Res. 5 , 237–249. [ Google Scholar ]
- Antonuccio D. O., Ward C. H., Tearnan B. H. (1989). The behavioral treatment of unipolar depression in adult outpatients , in Progress in Behavior Modification , eds Hersen M., Eisler R. M., Miller P. M. (Newbury Park, CA: Sage; ), 152–191. [ PubMed ] [ Google Scholar ]
- Areán P. A. (2000). Terapia de solución de problemas para la depresión: teoría, investigación y aplicaciones [Therapy for the solution of depression problems: theory, research and implementations] . Psicol. Conduct. 8 , 547–559. [ Google Scholar ]
- Armsden G., McCauley E., Greenberg M., Burke E., Mitchell J. (1990). Parent and peer attachment in early adolescent depression . J. Abnorm. Child Psychol. 18 , 683–698. 10.1007/BF01342754 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bandura A. (1977). Social learning theory of aggression . J. Commun. 8 , 12–29. [ PubMed ] [ Google Scholar ]
- Barber B. K., Stolz H. E., Olsen J. A. (2005). Parental support, psychological control, and behavioral control: assessing relevance across time, culture, and method . Monogr. Soc. Res. Child Dev. 70 , 1–137. 10.1111/j.1540-5834.2005.00365.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Barrett P., Turner C. (2001). Prevention of anxiety symptoms in primary school children: preliminary results from a universal school-based trial . Br. J. Clin. Psychol. 40 , 399–410. 10.1348/014466501163887 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bath H. J., Middleton M. R. (1985). The Children's Depression Scale: psychometric properties and factor structure . Aust. J. Psychol. 37 , 81–88. [ Google Scholar ]
- Beck A. T. (1967). Depression: Clinical, Experimental and Theoretical Aspects . New York, NY: Hoeber. [ Google Scholar ]
- Beck A. T. (1987). Cognitive models of depression . J. Cogn. Psychother. 1 , 5–37. [ Google Scholar ]
- Beck A. T., Alford B. A. (2009). Depression: Causes and Treatment, 2nd Edn . Philadelphia, PA: University of Pennsylbania Press. [ Google Scholar ]
- Beck A. T., Beamesderfer A. (1974). Assessment of depression: the depression inventory , in Psychological Measurements in Psychopharmacology , eds Pichot P., Olivier-Martin R. (Oxford: Karger Publishers; ). 10.1159/000395074 [ CrossRef ] [ Google Scholar ]
- Beck A. T., Epstein N., Harrison R. (1983). Cognitions, attitudes and personality dimensions in depression . Br. J. Cogn. Psychother. 1 , 1–16. [ Google Scholar ]
- Beck A. T., Rush A. J., Shaw B. F., Emery G. (1979). Cognitive therapy of depression . Aust. N.Z. J. Psychiatry 36 , 272–275. [ Google Scholar ]
- Beck A. T., Steer R. A., Brown G. K. (1996). Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation. [ Google Scholar ]
- Beck J. S., Beck A. T., Jolly J. B., Steer R. A. (2005). The Beck Youth Inventories, 2nd Edn. San Antonio, TX: Psychological Corporation. [ Google Scholar ]
- Beeghly M., Partridge T., Tronick E., Muzik M., Mashhadi M. R., Boeve J., et al.. (2017). Associations between early maternal depressive symptom trajectories and toddlers' felt security at 18 months: are boys and girls at differential risk? Infant Ment. Health J. 38 , 53–67. 10.1002/imhj.21617 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bernaras E., Jaureguizar J., Soroa M., Ibabe I., de las Cuevas M. C. (2013). Evaluación de la sintomatología depresiva en el contexto escolar y variables asociadas [Evaluation of depressive symptomatology and the related variables in the school context] . Anal. Psicol. 29 , 131–140. 10.6018/analesps.29.1.137831 [ CrossRef ] [ Google Scholar ]
- Bigelow A. E., Beebe B., Power M., Stafford A. L., Ewing J., Egleson A., et al.. (2018). Longitudinal relations among maternal depressive symptoms, maternal mind-mindedness, and infant attachment behavior . Infant Behav. Dev. 51 , 33–44. 10.1016/j.infbeh.2018.02.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Birleson P. (1981). The validity of depressive disorder in childhood and the development of a self-rating scale: a research report . J. Child Psychol. Psychiatry 22 , 73–88. 10.1111/j.1469-7610.1981.tb00533.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Birleson P., Hudson I., Grey-Buchanan D., Wolff S. (1987). Clinical evaluation of a self-rating scale for depressive disorder in childhood (Depression Self-Rating Scale) . J. Child Psychol. Psychiatry 28 , 43–60. 10.1111/j.1469-7610.1987.tb00651.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Birmaher B., Ryan N. D., Williamson D. E., Brent D. A., Kaufman J., Dahl R. E., et al. (1996). Childhood and adolescent depression: a review of the past 10 years. Part I . J. Am. Acad. Child Adolesc. Psychiatry 5 , 1427–1439. 10.1097/00004583-199611000-00011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blatt S. J. (2004). Experiences of Depression: Theoretical, Clinical, and Research Perspectives . Washington, DC: American Psychological Association; 10.1037/10749-000 [ CrossRef ] [ Google Scholar ]
- Bowlby J. (1969). Attachment and Loss: Attachment . New York, NY: Basic Books. [ Google Scholar ]
- Bowlby J. (1973). Attachment and Loss: Separation, Anxiety, and Anger . New York, NY: Basic Books. [ Google Scholar ]
- Bowlby J. (1976). Attachment and Loss (II). La Separación Afectiva . Buenos Aires: Paidós. [ Google Scholar ]
- Bowlby J. (1988). Developmental psychiatry comes of age . Am. J. Psychiatry 145 , 1–10. 10.1176/ajp.145.1.1 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Branchi I. (2011). The double edged sword of neural plasticity: increasing serotonin levels leads to both greater vulnerability to depression and improved capacity to recover . Psychoneuroendocrinology 36 , 339–351. 10.1016/j.psyneuen.2010.08.011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bravo M., Ribera J., Rubio-Stipec M., Canino G., Shrout P., Ramírez R., et al.. (2001). Test retest reliability of the Spanish version of the Diagnostic Interview Schedule for Children (DISC IV) . J. Abnorm. Child Psychol. 29 , 433–444. 10.1023/A:1010499520090 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brazelton T. B., Tronick E., Adamson L., Als H., Wise S. (1975). Early mother-infant reciprocity . Ciba Found. Symp. 33 , 137–154. 10.1002/9780470720158.ch9 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brent D. A., Perper J. A., Moritz G., Allman C., Schweers J., Roth C., et al.. (1993). Psychiatric sequelae to the loss of an adolescent peer to suicide . J. Am. Acad. Child Adolesc. Psychiatry 32 , 509–517. 10.1097/00004583-199305000-00004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bronfenbrenner U. (1979). The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press. [ Google Scholar ]
- Brooks S. J., Krulewicz S. P., Kutcher S. (2003). The Kutcher Adolescent Depression Scale: assessment of its evaluative properties over the course of an 8-week pediatric pharmacotherapy trial . J. Child Adolesc. Psychopharmacol. 13 , 337–349. 10.1089/104454603322572679 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brown J. (2018). Parents' experiences of their adolescent's mental health treatment: helplessness or agency-based hope . Clin. Child Psychol. Psychiatry 23 , 644–662. 10.1177/1359104518778330 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Calear A. L., Christensen H. (2010). Systematic review of school-based prevention and early intervention programs for depression . J. Adolesc. 33 , 429–438. 10.1016/j.adolescence.2009.07.004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cardemil E. V., Reivich K. J., Beevers C. G., Seligman M. E. P., James J. (2007). The prevention of depressive symptoms in low-income, minority children: two year follow-up . Behav. Res. Ther. 45 , 313–327. 10.1016/j.brat.2006.03.010 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Caspi A., Hariri A. R., Holmes A., Uher R., Moffitt T. E. (2010). Genetic sensitivity to the environment: the case of the serotonin transporter gene and its implications for studying complex diseases and traits . Am. J. Psychiatry 167 , 509–527. 10.1176/appi.ajp.2010.09101452 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Casullo M. M. (2001). Depresión y suicidio en la adolescencia [Depression and suicide in adolescence] , in Detección y Prevención en el Aula de Los Problemas del Adolescente [Detection and Prevention of Adolescent's Problems in the Classroom] , ed C. Saldaña (Madrid: Pirámide; ), 83–99. [ Google Scholar ]
- Chang S. S., Stuckler D., Yip P., Gunnel D. (2013). Impact of 2008 global economic crisis on suicide: time trend study in 54 countries . BMJ 347 , 1–16. 10.1136/bmj.f5239 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chaplin T. M., Gillham J. E., Reivich K., Elkon A. G. L., Samuels B., Freres D. R., et al.. (2006). Depression prevention for early adolescent girls: a pilot study of all girls versus co-ed groups . J. Early Adolesc. 26 , 110–126. 10.1177/0272431605282655 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chorot P., Valiente R. M., Magaz A. M., Santed M. A., Sadin B. (2017). Perceived parental child rearing and attachment as predictors of anxiety and depressive disorder symptoms in children: the mediational role of attachment . Psychiatry Res. 253 , 287–295. 10.1016/j.psychres.2017.04.015 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chorpita B. F., Moffitt C. E., Gray J. (2005). Psychometric properties of the Revised Child Anxiety and Depression Scale in a clinical sample . Behav. Res. Ther. 43 , 309–322. 10.1016/j.brat.2004.02.004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chorpita B. F., Yim L. M., Moffitt C. E., Umemoto L. A., Francis S. E. (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: a Revised Child Anxiety and Depression Scale . Behav. Res. Ther. 38 , 835–855. 10.1016/S0005-7967(99)00130-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cianchetti C., Sannio Fascello G. (2001). Scale Psichiatriche di Autosomministrazione per Fanciulli e Adolescenti (SAFA) [Psychiatric Scales of Self-Administration for Children and Adolescents] . Firenze: Organizzazioni Speciali. [ Google Scholar ]
- Clarke D. M., Currie K. C. (2009). Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence . Med. J. Aust. 190 , 54–60. [ PubMed ] [ Google Scholar ]
- Clarke G. N., Hawkins W., Murphy M., Sheeber L. B., Lewinsohn P. M., Seeley J. R. (1995). Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: a randomized trial of a group cognitive intervention . J. Am. Acad. Child Adolesc. Psychiatry 34 , 312–321. 10.1097/00004583-199503000-00016 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Clarke G. N., Hornbrook M., Lynch F., Polen M., Gale J., Beardslee W., et al.. (2001). A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents . Arch. Gen. Psychiatry 58 , 1127–1134. 10.1001/archpsyc.58.12.1127 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cole D., Rehm L. P. (1986). Family interaction patterns and childhood depression . J. Abnorm. Child Psychol. 14 , 297–314. 10.1007/BF00915448 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Costello C. G. (1972). Depression: loss of reinforcers or loss of reinforcer effectiveness? Behav. Ther. 3 , 240–247. 10.1016/S0005-7894(72)80084-4 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Croarkin P. E., Nakonezny P. A., Husain M. M., Melton T., Buyukdura J. S., Kennard B. D., et al.. (2013). Evidence for increased glutamatergic cortical facilitation in children and adolescents with major depressive disorder . JAMA Psychiatry 70 , 291–299. 10.1001/2013.jamapsychiatry.24 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Crowe K., McKay D. (2017). Efficacy of cognitive-behavioral therapy for childhood anxiety and depression . J. Anxiety Disord. 49 , 76–87. 10.1016/j.janxdis.2017.04.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cummings E. M., Cicchetti D. (1990). Toward a transactional model of relations between attachment and depression , in The John D. and Catherine T. MacArthur Foundation Series on Mental Health and Development. Attachment in the Preschool Years: Theory, Research, and Intervention , eds Greenberg M. T., Cicchetti D., Cummings E. M. (Chicago, IL: University of Chicago Press; ), 339–372. [ Google Scholar ]
- Curley J. P., Jensen C. L., Mashoodh R., Campagne F. A. (2011). Social influences on neurobiology and behavior: epigenetic effects during development . Psychoneuroendocrinology 36 , 352–371. 10.1016/j.psyneuen.2010.06.005 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dahl R. E., Birmaher B., Williamson D. E., Dorn L., Perel J., Kaufman J., et al.. (2000). Low growth hormone response to growth hormone–releasing hormone in child depression . Biol. Psychiatry 48 , 981–988. 10.1016/S0006-3223(00)00932-X [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dean J., Keshavan M. (2017). The neurobiology of depression: an integrative view . Asian J. Psychiatr. 27 , 101–111. 10.1016/j.ajp.2017.01.025 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Del Barrio V., Carrasco M. A. (2004). Adaptación del CDI, Inventario de Depresión Infantil de Maria Kovacs . Madrid: TEA. [ Google Scholar ]
- Del Barrio V., Colondrón M. F., de Pablo C., Roa M. L. (1996). Primera adaptación española de las escalas de depresión de Reynolds RCDS y RADS a población española [First Spanish adaptation of the Reynolds depression scales RCDS and RADS to the Spanish population] . RIDEP 2 ,75–100. [ Google Scholar ]
- Demir T., Karacetin G., Demir D. E., Uysal O. (2011). Epidemiology of depression in an urban population of Turkish children and adolescents . J. Affect. Disord. 134 , 168–176. 10.1016/j.jad.2011.05.041 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Derogatis L. R., Cleary P. A. (1977). Confirmation of the dimensional structure of the SCL-90: a study in construct validation . J. Clin. Psychol. 33 , 981–989. 10.1002/1097-4679(197710)33:4<981::AID-JCLP2270330412>3.0.CO;2-0 [ CrossRef ] [ Google Scholar ]
- Domènech-Llaberia E., Polaino-Lorente A. (1990). La escala ESDM como instrumento adicional en el diagnóstico de la depresión infantil [ESDM scale as an additional instrument in the diagnosis of child-depression] . Rev. Psiquiatr. Fac. Med. Barc. 17 , 105–113. [ Google Scholar ]
- Ellis A. (1994). Reason and Emotion in Psychotherapy, Rev. Edn. Secaucus, NJ: Birch Lane. [ Google Scholar ]
- Ellis A., Harper R. A. (1961). A Guide to Rational Living. Oxford: Prentice-Hall. [ Google Scholar ]
- Essau C. A., Conradt J., Sasagawa S., Ollendick T. H. (2012). Prevention of anxiety symptoms in children: results from a universal school-based trial . Behav. Ther. 43 , 450–464. 10.1016/j.beth.2011.08.003 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Evans E., Tovee M. J., Boothroyd L. G., Drewett R. F. (2013). Body dissatisfaction and disordered eating attitudes in 7- to 11-year-old girls: testing a sociocultural model . Body Image 10 , 8–15. 10.1016/j.bodyim.2012.10.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ezpeleta L., de la Osa M., Doménech J. M., Navarro J. B., Losilla J. M. (1995). Diagnostic Interview for Children and Adolescent-DICA-R: acuerdo diagnóstico entre niños/adolescentes y sus padres [Diagnostic Interview for Children and Adolescent-DICA-R: diagnostic agreement between children/adolescents and their parents] . Rev. Psiquiatr. Fac. Med. Barc. 22 , 153–163. [ Google Scholar ]
- Farrell L. J., Barrett P. M. (2007). Prevention of childhood emotional disorders: reducing the burden of suffering associated with anxiety and depression . Child Adolesc. Ment. Health 12 , 58–65. 10.1111/j.1475-3588.2006.00430.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ferdon C. D., Kaslow N. J. (2008). Evidence-based psychosocial treatments for child and adolescent depression . J. Clin. Child Adolesc. Psychol. 37 , 62–104, 10.1080/15374410701817865 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ferster C. B. (1966). Animal behavior and mental illness . Psychol. Rec. 16 , 345–356. 10.1007/BF03393678 [ CrossRef ] [ Google Scholar ]
- Figueras A., Amador J. A., Guàrdia J. (2008). Psychometric properties of the Reynolds Child Depression Scale in community and clinical samples . Span. J. Psychol. 11 , 641–649. [ PubMed ] [ Google Scholar ]
- Foley J. E., Weinraub M. (2017). Sleep, affect, and social competence from preschool to preadolescence: distinct pathways to emotional and social adjustment for boys and for girls . Front. Psychol. 8 :711. 10.3389/fpsyg.2017.00711 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Foster S., Mohler-Kuo M. (2018). Treating a broader range of depressed adolescents with combined therapy . J. Affect. Disord. 241 , 417–424. 10.1016/j.jad.2018.08.027 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Frank E., Anderson B., Reynold C. F., Ritenour A., Kupfer D. J. (1994). Life events and the research diagnostic criteria endogenous subtype. A confirmation of the distinction using the Bellford College methods . Arch. Gen. Psychiatry 51 , 519–524. 10.1001/archpsyc.1994.03950070011005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Franzen P. L., Buysse D. J. (2008). Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications . Dialogues Clin. Neurosci. 10 , 473–481. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gallegos J., Linan-Thompson S., Stark K., Ruvalcaba N. (2013). Preventing childhood anxiety and depression: testing the effectiveness of a school-based program in Mexico . Psicol. Educ. 19 , 37–44. 10.5093/ed2013a6 [ CrossRef ] [ Google Scholar ]
- Garaigordobil M., Bernaras E., Jaureguizar J., Matxinbarrena J. M. (2017). Childhood depression: relation to adaptative, clinical and predictor variables . Front. Psychol. 8 :821 10.3389/fpsyg.2017.00821 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Garaigordobil M., Maganto C. (2012). SPECI: Screening de Problemas Emocionales y de Conducta Infantiles [Screening of Emotional and Behavioral Problems During Childhood]. Madrid: TEA. [ Google Scholar ]
- Garbarino S., Lanteri P., Durando P., Magnavita N., Sannita W. G. (2016). Co-morbidity, mortality, quality of life and the healthcare/welfare/social costs of disordered sleep: a rapid review . Int. J. Environ. Res. Public Health 13 :831. 10.3390/ijerph13080831 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Garber J., Clarke G. N., Robin Weersing V., Beardslee W. R., Brent D. A., Gladstone T. R. G., et al.. (2009). Prevention of depression in at-risk adolescents: a randomized controlled trial . JAMA J. Am. Med. Assoc. 301 , 2215–2224. 10.1001/jama.2009.788 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- García J., Palazón P. (2010). Afronta tu Depresión con Terapia Interpersonal [Face Your Depression with Interpersonal Therapy] . Bilbao: Desclée de Brouwer. [ Google Scholar ]
- Gillham J. E. (1994). Preventing Depressive Symptoms in School Children . Doctoral dissertation, University of Pennsylvania. [ Google Scholar ]
- Gillham J. E., Hamilton J., Freres D. R., Patton K., Gallop R. (2006). Preventing depression among early adolescents in the primary care setting: a randomized controlled study of the Penn Resiliency Program . J. Abnorm. Child Psychol. 34 , 203–219. 10.1007/s10802-005-9014-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gillham J. E., Jaycox L. H., Reivich K. J., Seligman M. E. P., Silver T. (1990). The Penn Resiliency Program. Unpublished manuscript, University of Pennsylvania. [ Google Scholar ]
- Gillham J. E., Reivich K. J. (1999). Prevention of depressive symptoms in school children: a research update . Psychol. Sci. 10 , 461–462. 10.1111/1467-9280.00188 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gillham J. E., Reivich K. J., Freres D. R., Chaplin T. M., Shatt,é A. J., Samuels B., et al.. (2007). School-based prevention of depressive symptoms: a randomized controlled study of the effectiveness and specificity of the Penn Resiliency Program . J. Consult. Clin. Psychol. 75 , 9–19. 10.1037/0022-006X.75.1.9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gillham J. E., Reivich K. J., Jaycox L. H., Seligman M. E. P. (1995). Prevention of depressive symptoms in schoolchildren: two-year follow-up . Psychol. Sci. 6 , 343–351. 10.1111/j.1467-9280.1995.tb00524.x“ [ CrossRef ] [ Google Scholar ]
- Gladstone T. R. G., Kaslow N. J. (1995). Depression and attributions in children and adolescents: a meta-analytic review . J. Abnorm. Child Psychol. 23 , 597–606. 10.1007/BF01447664 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- González De Rivera J. L., De Las Cuevas C., Rodríguez-Abuín M. J., Rodríguez-Pulido F. (2002). El Cuestionario de 90 S í ntomas (Adaptación Española del SCL-90R de L. R. Derogatis) [THE 90 Symptoms Checklist (Spanish Adaptation of the SCL-90R of L. R. Derogatis] Madrid: TEA [ Google Scholar ]
- González J., Fernández S., Pérez E., Santamaría P. (2004). Adaptación Española del Sistema de Evaluación de la Conducta en Niños y Adolescentes: BASC [Spanish Adaptation of the Behavior Assessment System for Children]. Madrid: TEA. [ Google Scholar ]
- Greenberg L., Elliot R., Pos A. (2015). La teoría focalizada en las emociones: una visión de conjunto [The theory focused on emotions: the joint vission] . Mental. Rev. Psicoanál. Psicoter. 5 , 1–19. [ Google Scholar ]
- Greenberg L. S. (2004). Emotion-focused therapy . Clin. Psychol. Psychother. 11 , 3–16. 10.1002/cpp.388 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Greenberg M. T., Domitrovich C., Bumbarger B. (2001). The prevention of mental disorders in school-aged children: current state of the field . Prevent. Treat. 4 , 1–59. 10.1037/1522-3736.4.1.41a [ CrossRef ] [ Google Scholar ]
- Hayes S. C. (2005). Get Out of Your Mind and Into Your Life: The New Acceptance and Commitment Therapy . New York, NY: New Harbinger Publications. [ Google Scholar ]
- Heider D., Matschinger H., Bernet S., Alonso J., Angermeyer M. (2006). Relationship between parental bonding and mood disorder in six European countries . Psychiatry Res. 143 , 89–98. 10.1016/j.psychres.2005.08.015 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Herane-Vives A., Fischer S., de Angel V., Wise T., Cheung E., Chua K. C., et al.. (2018). Elevated fingernail cortisol levels in major depressive episodes . Psychoneuroendocrinology 88 , 17–23. 10.1016/j.psyneuen.2017.10.026 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hesse E., Main M. (2000). Disorganized infant, child, and adult attachment: collapse in behavioral and attentional strategies . J. Am. Psychoanal. Assoc. 48 , 1097–1127. 10.1177/00030651000480041101 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Higgins E. (1997). Beyond pleasure and pain . Am. Psychol. 52 , 1280–1300. 10.1037/0003-066X.52.12.1280 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hilsenroth M. J., Ackerman S. J., Blagys M. D., Baity M. R., Mooney M. A. (2003). Short-term psychodynamic psychotherapy for depression: an examination of statistical, clinically significant, and technique-specific change . J. Nerv. Mental Dis. 191 , 349–357. 10.1097/01.NMD.0000071582.11781.67 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hiroto D. S., Seligman M. E. P. (1975). Generality of learned helplessness in man . J. Pers. Soc. Psychol. 31 , 311–327. 10.1037/h0076270 [ CrossRef ] [ Google Scholar ]
- Horowitz J. L., Garber J., Ciesla J. A., Young J. F., Mufson L. (2007). Prevention of depressive symptoms in adolescents: a randomized trial of cognitive-behavioral and interpersonal prevention programs . J. Consult. Clin. Psychol. 75 :693. 10.1037/0022-006X.75.5.693 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Huggins L., Davis M. C., Rooney R. M., Kane R. T. (2008). Socially prescribed and self-orientated perfectionism as predictors of depressive diagnosis in preadolescents . Aust. J. Guid. Couns. 18 , 182–194. 10.1375/ajgc.18.2.182 [ CrossRef ] [ Google Scholar ]
- Ingram R. E. (1984). Toward and information-processing analysis of depression . Cogn. Ther. Res. 8 , 443–478. 10.1007/BF01173284 [ CrossRef ] [ Google Scholar ]
- Iruela L. M., Picazo J., Peláez C. (2009). Tratamiento farmacológico de la depresión en niños y adolescentes [Pharmacological treatment of depression in children and adolescents] . Inf. Técnico Sist. Nac. Salud 33 , 35–38. [ Google Scholar ]
- Jaureguizar J., Bernaras E., Bully P., Garaigordobil M. (2018). Perceived parenting and adolescents' adjustment . Psicol. Reflex. Crítica 31 :8 10.1186/s41155-018-0088-x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jaureguizar J., Bernaras E., Garaigordobil M. (2017). Child depression: prevalence and comparison between self-reports and teacher reports . Span. J. Psychol. 20 , 1–10. 10.1017/sjp.2017.14 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jellinek M., Evans N., Knight R. B. (1979). Use of a behavior checklist on a pediatric inpatient unit . J. Pediatr. 94 , 156–158. 10.1016/S0022-3476(79)80386-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Joiner T., Coyne J. C. (1999). The Interactional Nature of Depression. Washington, DC: American Psychological Association. [ Google Scholar ]
- Ju S., Lee Y. (2018). Developmental trajectories and longitudinal mediation effects of self-esteem, peer attachment, child maltreatment and depression on early adolescents . Child Abuse Negl. 76 , 353–363. 10.1016/j.chiabu.2017.11.015 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kanfer F. H. (1970). Self-regulation: research, issues and speculations , in Behavior Modification in Clinical Psychology , eds Neuringer C., Michael J. L. (New York, NY: Appleton-Century-Crofts; ), 178–220. [ Google Scholar ]
- Kaslow N., Rehm L. P., Pollack S. L., Siegel A. W. (1988). Attributional style and self-control behavior in depressed and nondepressed children and their parents . J. Abnorm. Child Psychol. 16 , 163–175. 10.1007/BF00913592 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kaufman J., Birmaher B., Brent D., Rao U., Ryan N. (1996). The Schedule for Affective Disorders and Schizophrenia for School-Age Children. Pittsburgh, PA: University of Pittsburgh Medical Center. [ PubMed ] [ Google Scholar ]
- Kaufman J., Wymbs N. F., Montalvo-Ortiz J. L., Orr C., Albaugh M. D., Althoff R., et al.. (2018). Methylation in OTX2 and related genes, maltreatment, and depression in children . Neuropsychopharmacology 43 , 2204–2211. 10.1038/s41386-018-0157-y [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kenny M., Moilanen D., Lomax R., Brabeck M. (1993). Contributions of parental attachments to view of self and depressive symptoms among early adolescents . J. Early Adolesc. 13 , 408–430. 10.1177/0272431693013004004 [ CrossRef ] [ Google Scholar ]
- Kleftaras G., Didaskalou E. (2006). Incidence and teachers' perceived causation of depression in primary school children in Greece . Sch. Psychol. Int. 27 , 296–314. 10.1177/0143034306067284 [ CrossRef ] [ Google Scholar ]
- Klerman G. L., Weissman M. M., Rounsaville B. J., Chevron E. S. (1984). Interpersonal Psychotherapy of Depression . New York, NY: Basic Books. [ Google Scholar ]
- Koback R., Sudler N., Gamble W. (1991). Attachment and depressive symptoms during adolescence: a developmental pathways analysis . Dev. Psychopathol. 3 , 461–474. 10.1017/S095457940000763X [ CrossRef ] [ Google Scholar ]
- Kovacs M. (1985). The children's depression inventory (CDI) . Psychopharmacol. Bull. 21 , 995–998. [ PubMed ] [ Google Scholar ]
- Kovacs M. (1992). The Children's Depression Inventory Manual . New York, NY: Multi-Health Systems, Inc. [ Google Scholar ]
- Kowalenko N., Rapee R. M., Simmons J., Wignall A., Hoge R., Whitefield K., et al. (2005). Short-term effectiveness of a school-based early intervention program for adolescent depression . Clin. Child Psychol. Psychiatry 10 , 493–507. 10.1177/1359104505056311 [ CrossRef ] [ Google Scholar ]
- Kraus C., Castrén E., Kasper S., Lanzenberger R. (2017). Serotonin and neuroplasticity – links between molecular, functional and structural pathophysiology in depression . Neurosci. Biobehav. Rev. 77 , 317–326. 10.1016/j.neubiorev.2017.03.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Krefetz D. G., Steer R. A., Gulab N. A., Beck A. T. (2002). Convergent validity of the beck depression inventory-II with the Reynolds Adolescent Depression Scale in psychiatric inpatients . J. Pers. Assess. 78 , 451–460. 10.1207/S15327752JPA7803_05 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lang M., Tisher M. (1978). Children's Depression Scale. Camberbell, VIC: Australian Council for Educational Research. [ Google Scholar ]
- Lauth B., Arnkelsson G. B., Magnússon P., Skarphedinsson G. A., Ferrari P., Pétursson H. (2010). Validity of K-SADS-PL (Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime version) depression diagnoses in an adolescent clinical population . Nord. J. Psychiatry 64 , 409–420. 10.3109/08039481003777484 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Leblanc J. C., Almudevar A., Brooks S. J. (2002). Screening for adolescent depression: comparison of the Kutcher Adolescent Scale with the beck depression inventory . J. Child Adolesc. Psychopharmacol. 12 , 113–126. 10.1089/104454602760219153 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lemos S., Fidalgo A. M., Calvo P., Menéndez P. (1992). Estructura factorial de la prueba YSR y su utilidad en psicopatología infanto-juvenil [Factorial structure of YSR scale and its utility in child-youth psychopathology] . Anál. Modif. Conduct. 3 , 183–194. [ Google Scholar ]
- Lengua L. J., Kovacs E. A. (2005). Bidirectional associations between temperament and parenting and the prediction of adjustment problems in middle childhood . Appl. Dev. Psychol. 26 , 21–38. 10.1016/j.appdev.2004.10.001 [ CrossRef ] [ Google Scholar ]
- Lewinsohn P. M. (1974). Clinical and theoretical aspects of depression , in Innovative Treatment Methods in Psychopathology , eds Calhoun K. S., Adams H. E., Mitchel K. M. (New York, NY: Wiley; ), 63–120. [ Google Scholar ]
- Lewinsohn P. M. (1975). Clinical and theoretical aspects of depression , in Innovative Treatment Methods of Psychopathology , eds Calhoun K. S., Adams H. E., Mitchell K. M. (New York, NY: Wiley; ), 63–120. [ Google Scholar ]
- Lock S., Barrett P. M. (2003). A longitudinal study of developmental differences in universal preventive intervention for child anxiety . Behav. Change 20 , 183–199. 10.1375/bech.20.4.183.29383 [ CrossRef ] [ Google Scholar ]
- Lorenzo-Blanco E. I., Unger J. B., Baezconde-Garbatani L.A, Soto D. (2012). Acculturation, enculturation, and symptoms of depression in hispanic youth: the roles of gender, hispanic cultural values, and family functioning . J. Youth Adolesc. 41, 1350–1365. 10.1007/s10964-012-9774-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lowry-Webster H., Barrett P. M., Dadds M. R. (2001). A universal prevention trial of anxiety and depressive symptomatology in childhood: preliminary data from an Australian study . Behav. Change 18 , 36–50. 10.1375/bech.18.1.36 [ CrossRef ] [ Google Scholar ]
- Lozano L., García-Cueto E., Lozano L. M. (2007). Cuestionario Educativo Cl í nico de Ansiedad y Depresión [Educative and Clinical Questionnaire of Anxiety and Depression] Madrid: TEA Ediciones. [ Google Scholar ]
- Luciano M. (2017). Versiones provisionales del capítulo de la CIE-11 sobre trastornos mentales . Actas Españolas Psiquiatr. 45 , 79–88. [ Google Scholar ]
- Luyten P., Blatt S. J. (2012). Psychodynamic treatment of depression . Psychiatr. Clin. North Am. 35 , 111 10.1016/j.psc.2012.01.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Main M. (1996). Introduction to the special section on attachment and psychopathology. 2. Overview of the field of attachment . J. Consult. Clin. Psychol. 64 , 237–243. 10.1037/0022-006X.64.2.237 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Markowitz J. C., Weissman M. M. (1995). Interpersonal psychotherapy , in Handbook of Depression , eds Beckham E., Leber W. R. (New York, NY: Guilford; ), 376–390. [ Google Scholar ]
- Martell C. R., Dimidjian S., Herman-Dunn (2013). Behavioral Activation for Depression. A Clinician's Guide . New York, NY: Guilford. [ Google Scholar ]
- McCabe M., Ricciardelli L., Banfield S. (2011). Depressive symptoms and psychosocial functioning in preadolescent children . Depress. Res. Treat. 2011 , 1–7. 10.1155/2011/548034 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McConaughy S. H., Achenbach T. M. (1994). Manual for the Semistructured Clinical Interview for Children and Adolescents . Burlington, NJ: Department of Psychiatry; University of Vermont. [ Google Scholar ]
- McCullough J. P. (2000). Treatment for Chronic Depression: Cognitive Behavioral Analysis System of Psychotherapy (CBASP) . New York, NY: Guilford. [ Google Scholar ]
- McCullough J. P. (2003). Treatment for chronic depression using Cognitive Behavioral Analysis System of Psychotherapy (CBASP) . J. Clin. Psychol. 59 , 833–846. 10.1002/jclp.10176 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Méndez F. X. (1998). El niño que no sonr í e. Estrategias Para Superar la Tristeza y la Depresión Infantil [The Child that Does not Smile. Strategies to Face the Sadness and Child Depression] . Madrid: Pirámide. [ Google Scholar ]
- Méndez F. X., Llavona L. M., Espada J. P., Orgilés M. (2013). Programa Fortius. Fortaleza Psicológica y Prevención de las Dificultades Emocionales [Fortius Program. Psychological Strength and Prevention of Emotional Difficulties]. Madrid: Pirámide. [ Google Scholar ]
- Merry S., McDowell H., Wild C. J., Bir J., Cunliffe R. (2004). A randomized placebo-controlled trial of a school-based depression prevention program . J. Am. Acad. Child Adolesc. Psychiatry 43 , 538–547. 10.1097/00004583-200405000-00007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Miller W. R., Seligman M. E. (1975). Depression and learned helplessness in man . J. Abnorm. Psychol. 84 , 228–238. 10.1037/h0076720 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Milrod B., Markowitz J. C., Gerber A. J., Cyranowski J., Altemus M., Shapiro T., et al.. (2014). Childhood separation anxiety and the pathogenesis and treatment of adult anxiety . Am J Psychiatry 171 , 34–43. 10.1176/appi.ajp.2013.13060781. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Narbona J. (2014). Depressive phenomenology at the outset of neuropaediatric diseases . Rev. Neurol. 58 ( Suppl. 1 ), S71–S75. [ PubMed ] [ Google Scholar ]
- Nezu A. M., Nezu C. M., D'Zurilla T. J. (2013). Problem-Solving Therapy. A Treatment Manual . New York, NY: Springer Publishing Company. [ Google Scholar ]
- Nique S., Fournis G., El_Hage W., Nabhan-Abou N., Garr,é J.-B., Gohier B. (2014). Transporteur de la sérotonine, troubles ansieux et dépression: revue de la littérature . Eur. Psychiatry 29 , 544–545. 10.1016/j.eurpsy.2014.09.328 [ CrossRef ] [ Google Scholar ]
- Novati A., Hulshof H. J., Granic I., Meerlo P. (2012). Chronic partial sleep deprivation reduces brain sensitivity to glutamate N -methyl-d-aspartate receptor-mediated neurotoxicity . J. Sleep Res. 21 , 3–9. 10.1111/j.1365-2869.2011.00932.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Oken B., Chamine I., Wakelan W. (2015). A systems approach to stress, stressors and resilience in humans . Behav. Brain Res. 282 , 144–154. 10.1016/j.bbr.2014.12.047 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Orenes A. M. (2015). Evaluación de la Ansiedad por Separación y Prevención Escolar de las Dificultades Emocionales [Evaluation of Separation Anxiety and School Prevention of Emotional Difficulties] . Doctoral dissertation, University of Murcia, Murcia. [ Google Scholar ]
- Pariante C. M. (2017). Why are depressed patients inflamed? A reflection on 20 years of research on depression, glucocorticoid resistance and inflammation . Eur. Neuropscychopharmacol. 27 , 554–559. 10.1016/j.euroneuro.2017.04.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pattison C., Lynd-Stevenson R. M. (2001). The prevention of depressive symptoms in children: The immediate and long-term outcomes of a school based program . Behav. Change 18 , 92–102. 10.1375/bech.18.2.92 [ CrossRef ] [ Google Scholar ]
- Peiró S., Cervera P., Bernal-Delgado E. (2005). Los inhibidores selectivos de la recaptación de serotonina en la depresión infantil: un “culebrón” que refleja importantes problemas de seguridad de los medicamentos [Selective inhibitors of serotonine reuptake in child depression: a “soap opera” that reflects important safety problems of medication]. Gac. Sanit . 19 . Available online at: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0213–91112005000500010 [ PubMed ]
- Perls F., Hefferline R. F., Goodman P. (1951). Gestalt Therapy . New York, NY: Dell. [ Google Scholar ]
- Peterson C., Maier S. F., Seligman M. E. (1993). Learned Helplessness. A Theory for the Age of Personal Control . New York, NY: Oxford University Press. [ Google Scholar ]
- Poznanski E. O., Cook S. C., Carroll B. J. (1979). A depression rating scale for children . Pediatrics 64 , 442–450. [ PubMed ] [ Google Scholar ]
- Puig-Antich J. (1987). Affective disorder in children and adolescents: diagnosis, validity and psychobiology , in Psychopharmacology: The Third Generation of Progress , ed Meltzer H. Y. (New York, NY: Raven Press; ), 843–860. [ Google Scholar ]
- Puura K., Tamminen T., Almqvist F., Kresanov K., Kumpulainen K., Moilanen I., et al. (1997). Should depression in young-children be diagnosed with different criteria? Eur. Child Adolesc. Psychiatry 6 , 12–19. 10.1007/BF00573635 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Quayle D., Dzuirawiec S., Roberts C., Kane R., Ebsworthy G. (2001). The effect of an optimism and lifeskills program on depressive symptoms in preadolescence . Behav. Change 18 , 194–203. 10.1375/bech.18.4.194 [ CrossRef ] [ Google Scholar ]
- Radloff L. S. (1977). A CES-D scale: a self-report depression scale for research in the general population . Appl. Psychol. Meas. 1 , 385–401. 10.1177/014662167700100306 [ CrossRef ] [ Google Scholar ]
- Reeves A., McKee M., Stuckler D. (2014). Economic suicides in the great recession in Europe and North America . Br. J. Psychiatry J. Mental Sci. 205 , 246–247. 10.1192/bjp.bp.114.144766 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rehm L. P. (1977). A self-control model of depression . Behav. Ther. 8 , 787–804. 10.1016/S0005-7894(77)80150-0 [ CrossRef ] [ Google Scholar ]
- Rehm L. P., Fuchs C. Z., Roth D. M., Kornblith S. J., Romano J. (1979). A comparison of self-control and social skills treatments of depression . Behav. Ther. 10 :4442 10.1016/S0005-7894(79)80048-9 [ CrossRef ] [ Google Scholar ]
- Reich W., Shayka J. J., Taibleson C. H. (1991). Diagnostic Interview Schedule for Children and Adolescen-DICA-R. Unpublished manuscript, Washington University, Division of Child Psychiatry. [ Google Scholar ]
- Reinecke M. A., Rogers G. M. (2001). Dysfunctional attitudes and attachment style among clinically depressed adults . Behav. Cogn. Psychother. 29 , 129–141. 10.1017/S1352465801002016 [ CrossRef ] [ Google Scholar ]
- Reinecke M. A., Simons A. (2005). Vulnerability to depression among adolescents: Implications for cognitive-behavioral treatment . Cogn. Behav. Pract. 12 , 166–176. 10.1016/S1077-7229(05)80022-7 [ CrossRef ] [ Google Scholar ]
- Reinherz H. Z., Giaconia R. M., Palus B., Silverman A. B., Frost A. K., Lefkowitz E. S. (1993). Psychosocial risks for major depression in late adolescence: a longitudinal community study . J. Am. Acad. Child Adolesc. Psychiatry 32 , 1155–1163. 10.1097/00004583-199311000-00007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Reynolds C. R., Kamphaus R. W. (1992). Behavior Assessment System for Children (BASC). Circle Pines, MN: American Guidance Services. [ Google Scholar ]
- Reynolds W. M. (1987). Reynolds Adolescent Depression Scale. Professional manual. Odessa, FL: Psychological Assessment Resources. [ Google Scholar ]
- Reynolds W. M. (1989). Reynolds Child Depression Scale. Professional manual. Odessa, FL: Psychological Assessment Resources. [ Google Scholar ]
- Reynolds W. M., Anderson G., Bartell N. (1985). Measuring depression in children: a multimethod assessment investigation . J. Abnorm. Child Psychol. 13 , 513–526. 10.1007/BF00923138 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roberts C., Kane R., Bishop B., Matthews H., Thomson H. (2004). The prevention of depressive symptoms in rural school children: a follow-up study . Int. J. Mental Health Promot. 6 , 4–16. 10.1080/14623730.2004.9721934 [ CrossRef ] [ Google Scholar ]
- Roberts C., Kane R., Thomson H., Bishop B., Hart B. (2003a). The prevention of depressive symptoms in rural school children: a randomized controlled trial . J. Consult. Clin. Psychol. 71 , 622–628. 10.1037/0022-006X.71.3.622 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roberts C. M., Mazzucchelli T., Taylor K., Reid R. (2003). Early intervention for children with challenging behavior and developmental disabilities . Int. J. Disabil. Dev. Educ. 50 , 275–292. 10.1080/1034912032000120453 [ CrossRef ] [ Google Scholar ]
- Roberts J., Gotlib I., Kassel J. (1996). Adult attachment security and symptoms of depression: the mediating roles of dysfunctional attitudes and low self-esteem . J. Pers. Soc. Psychol. 70 , 310–320. 10.1037/0022-3514.70.2.310 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roelofs J., Meesters C., ter Huurne M., Bamelis L., Muris P. (2006). On the links between attachment style, parental rearing behaviors, and internalizing and externalizing problems in non-clinical children . J. Child Fam. Stud. 15 , 319–332. 10.1007/s10826-006-9025-1 [ CrossRef ] [ Google Scholar ]
- Rogers C. R. (1961). On Becoming a Person: A Psychotherapists View of Psychotherapy . Boston, MA: Houghton Mifflin. [ Google Scholar ]
- Rohner R. P., Khaleque A. (2003). Reliability and validity of the parental control scale: a meta-analysis of cross-cultural and intracultural studies . J. Cross Cult. Psychol. 34 , 643–649. 10.1177/0022022103255650 [ CrossRef ] [ Google Scholar ]
- Rooney R., Hassan S., Kane R., Roberts C. M., Nesa M. (2013). Reducing depression in 9-10 year old children in low SES schools: a longitudinal universal randomized controlled trial . Behav. Res. Ther. 51 , 845–854. 10.1016/j.brat.2013.09.005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rooney R., Pike L., Roberts C. (2000). The Positive Thinking Program: Prevention Manual. Unpublished manuscript, Curtin University of Technology. [ Google Scholar ]
- Rooney R., Roberts C., Kane R., Pike L., Winsor A., White J., et al. (2006). The prevention of depression in 8- to 9-year-old children: a pilot study . Aust. J. Guid. Couns. 16 , 76–90. 10.1375/ajgc.16.1.76 [ CrossRef ] [ Google Scholar ]
- Rubio-Stipec M., Bird H., Canino G., Gould M. (1990). The internal consistency and concurrent validity of a Spanish translation of the child behavior checklist . J. Abnorm. Child Psychol. 18 , 393–406. 10.1007/BF00917642 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ryan N. D., Dahl R. E., Birmaher B., Williamson D. E., Iyendar S., Nelson B., et al. (1994). Stimulatory test of growth hormone secretion in prepuberal major depression: depressed versus normal children . J. Am. Acad. Child Adolesc. Psychiatry 33 , 824–833. 10.1097/00004583-199407000-00008 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sandín B., Chorot P., Valiente R. M., Chorpita B. F. (2010). Development of a 30-item version of the Revised Child Anxiety and Depression Scale . Rev. Psicopatol. Psicol. Clín. 15 , 165–178. 10.5944/rppc.vol.15.num.3.2010.4095 [ CrossRef ] [ Google Scholar ]
- Sandín B., Valiente R. M., Chorot P. (2009). RCADS: evaluación de los síntomas de trastornos de ansiedad y depresión en niños y adolescentes [RCADS: evaluation of symptoms of anxiety and depression disorders in children and adolescents] . Rev. Psicopatol. Psicol. Clín. 14 , 193–206. 10.5944/rppc.vol.14.num.3.2009.4078 [ CrossRef ] [ Google Scholar ]
- Sanz J., Vázquez C. (1998). Fiabilidad, validez y datos normativos del Inventario para la Depresión de Beck [Reliability, validity and normative data of the Beck Depression Inventory] . Psicothema 10 , 303–318. [ Google Scholar ]
- Schildkraut J. J. (1965). The catecholamine hypothesis of affective disorders: a review of supporting evidence . Am. J. Psychiatr. 122 , 509–522. 10.1176/ajp.122.5.509 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Scourfield J., Rice F., Thapar A., Harold G., Martin N., McGuffin P. (2003). Depressive symptoms in children and adolescents: changing aetiological influences with development . J. Child Psychol. Psychiatry 44 , 968–976. 10.1111/1469-7610.00181 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Seisdedos N. (2003). Cuestionario de Depresión para Niños [Child Depression Scale], 7th Edn. Manual. Madrid: TEA. [ Google Scholar ]
- Seligman M. E. P. (1975). Helplessness. On Depression, Development, and Death. San Francisco, CA: Freeman. [ Google Scholar ]
- Shaffer D., Fisher P., Lucas C., Dulcan M. K., Schwab-Stone M. (2000). NIMH Diagnostic Interview Schedule for Children, Version IV (NIMH DISC-IV): description, differences from previous versions and reliability of some common diagnoses . J. Am. Acad. Child Adolesc. Psychiatry 39 , 28–38. 10.1097/00004583-200001000-00014 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shah F., Morgan S. B. (1996). Teachers' ratings of social competence of children with high versus low levels of depressive symptoms . J. Sch. Psychol. 34 , 337–349. [ Google Scholar ]
- Shapero B. G., Black S. K., Liu R. T., Klugman J., Bender R. E., Abramson L. Y., et al.. (2013). Stressful life events and depression symptoms: the effect of childhood emotional abuse on stress reactivity . J. Clin. Psychol. 70 , 209–223. 10.1002/jclp.22011 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shedler J., Westen D. (2004). Dimensions of personality pathology: an alternative to the five-factor model . Am. J. Psychiatry 161 , 1743–1754. 10.1176/ajp.161.10.1743 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sheffield J. K., Spence S. H., Rapee R. M., Kowalenko N., Wignall A., Davis A., et al.. (2006). Evaluation of universal, indicated, and combined cognitive-behavioral approaches to the prevention of depression among adolescents . J. Consult. Clin. Psychol. 74 :66. 10.1037/0022-006X.74.1.66 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shochet I. M., Dadds M. R., Holland D., Whitefield K., Harnett P. H., Osgarby S. M. (2001). The efficacy of a universal school-based program to prevent adolescent depression . J. Clin. Child Psychol. 30 , 303–315. 10.1207/S15374424JCCP3003_3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Simons R. L., Miller M. G. (1987). Adolescent depression: assessing the impact of negative cognitions and socioenvironmental problems . Soc. Work 32 , 326–330. 10.1093/sw/32.4.326 [ CrossRef ] [ Google Scholar ]
- Sivertsen B., Harvey A., Lundrevold A. J., Hysing M. (2014). Sleep problems and depression in adolescence: results from a large population-based study of Norwegian adolescents aged 16-18 years . Eur. Child Adolesc. Psychiatry 23 , 681–689. 10.1007/s00787-013-0502-y [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Skinner B. F. (1953). Science and Human Behavior . New York, NY: Macmillan Company. [ Google Scholar ]
- Sokratous S., Merkouris A., Middeleton N., Karanikola M. (2013). The association between stressful life events and depressive symptoms among Cypriot university students: a cross-sectional descriptive correlational study . Bio. Med. Central Public Health 13 :1121. 10.1186/1471-2458-13-1121 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Soler J., Pérez-Sola V., Puigdemont D., Pérez-Blanco J., Figueres M., Álvarez E. (1997). Estudio de validación del Center for Epidemiologic Studies-Depression (CES-D) en una población española de pacientes con trastornos afectivos [A validity study of the Center for Epidemiologic Studies-Depression (CES-D) in a Spanish population of patients with affective disorders] . Actas Luso Esp. Neurol. Psiquiatr. Cien Afines 25 , 243–294. [ PubMed ] [ Google Scholar ]
- Spence S. H., Sheffield J. K., Donovan C. L. (2003). Preventing adolescent depression: an evaluation of the problem solving for life program . J. Consult. Clin. Psychol. 71 , 3–13. 10.1037/0022-006X.71.1.3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Spence S. H., Sheffield J. K., Donovan C. L. (2005). Long-term outcome of a school-based, universal approach to prevention of depression in adolescents . J. Consult. Clin. Psychol. 73 , 160–167. 10.1037/0022-006X.73.1.160 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stockings E., Degenhardt L., Lee Y. Y., Mihalopoulos C., Liu A., Hobbs M., et al.. (2015). Symptom screening scales for detecting major depressive disorder in children and adolescents: a systematic review and meta-analysis of reliability, validity and diagnostic utility . J. Affect. Disord. 174 , 447–463. 10.1016/j.jad.2014.11.061 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thabrew H., Stasiak K., Bavin L. M., Frampton C., Merry S. (2017). Validation of the Mood and Feelings Questionnaire (MFQ) and Short Mood and Feelings Questionnaire (SMFQ) in New Zealand help-seeking adolescents . Int. J. Methods Psychiatr. Res. 27 :e1610. 10.1002/mpr.1610 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tisher M., Lang-Takac E., Lang M. (1992). The Children's Depression Scale: review of Australian and overseas experience . Aust. J. Psychol. 44,27–35. [ Google Scholar ]
- Tompson M. C., Langer D. A., Hughes J. L., Asarnow J. R. (2016). Family-focused treatment for childhood depression: model and case illustrations . Cogn. Behav. Pract. 24 , 269–287. 10.1016/j.cbpra.2016.06.003 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tompson M. C., Sugar C. A., Langer D., Asarnow J. R. (2017). A randomized clinical trial comparing family-focused treatment and individual supportive therapy for depression in childhood and early adolescence . J. Am. Acad. Child Adolesc. Psychiatry 56 , 515–523. 10.1016/j.jaac.2017.03.018 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vázquez F. L., Muñoz R. F., Becoña E. (2000). Depresión: diagnóstico, modelos teóricos y tratamiento a finales del siglo XX [Depression: diagnosis, theoretical models and treatments on the verge of 20th century] . Psicol. Conduct. 8 , 417–449. [ Google Scholar ]
- Vinaccia S., Gaviria A. M., Atehortúa L. F., Martínez P. H., Trujillo C., Quiceno J. M. (2006). Prevalencia de la depresión en niños escolarizados entre 8 y 12 años del oriente antioqueño a partir del “Child depression inventory”-CDI- [Prevalence of depression in 8-12 years-old children in east Antioquia using the “Child depression inventory”-CDI-] . Rev. Divers. Perspect. Psicol. 2 , 217–227. 10.15332/s1794-9998.2006.0002.03 [ CrossRef ] [ Google Scholar ]
- Vitiello B., Ordoñez A. E. (2016). Pharmacological treatment of children and adolescents with depression . Expert Opin. Pharmacother. 17 , 2273–2279. 10.1080/14656566.2016.1244530 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wagner K. D., Ambrosini P. J. (2001). Childhood depression: pharmacological therapy/treatment (pharmacotherapy of childhood depression) . J. Clin. Child Adolesc. Psychol. 30 , 88–97. 10.1207/S15374424JCCP3001_10 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Waterman G. S., Dahl R. E., Birmaher B., Ambrosini P., Rabinovich H., Williamson D. E., et al.. (1994). The 24-hour pattern of prolactin secretion in depressed and normal adolescents . Biol. Psychiatry 35 , 440–445. 10.1016/0006-3223(94)90041-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weersing V. R., Jeffreys M., Do M.-C. T., Schwartz K. T. G., Bolano C. (2017). Evidence base update of psychosocial treatments for child and adolescent depression . J. Clin. Child Adolesc. Psychol. 46 , 11–43, 10.1080/15374416.2016.1220310 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weissman M. M., Orvaschel H., Padian N. (1980). Children's symptom and social functioning self-report scales: comparison of mothers' and children's reports . J. Nerv. Mental Disord. 168 , 736–740. [ PubMed ] [ Google Scholar ]
- Whittle S., Lichter R., Dennison M., Vijayakumar N., Schwartz O., Byrne M. L., et al.. (2014). Structural brain development and depression onset during adolescence: a prospective longitudinal study . Am. J. Psychiatry 171 , 564–571. 10.1176/appi.ajp.2013.13070920 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Williamson D. E., Birmaher B., Anderson B. P., Al-Shabbout M., Ryan N. D. (1995). Stressful life events in depressed adolescents: the role of dependent events during the depressive episode . Am. Acad. Child Adolesc. Psychiatry 33 , 591–598. 10.1097/00004583-199505000-00011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization (WHO) (2017). Depression. Fact sheet . Available online at: http://www.who.int/mediacentre/factsheets/fs369/en/
- World Health Organization (WHO) (2018). WHO Releases New International Classification of Diseases (ICD 11) . Available online at: http://www.who.int/news-room/detail/18-06-2018-who-releases-new-international-classification-of-diseases-(icd-11)
- Yang L., Zhou X., Zhou CH., Zhang Y., Pu. J, Liu L., Gong X., et al.. (2017). Efficacy and acceptability of cognitive behavioral therapy for depression in children: a systematic review and meta-analysis . Acad. Pediatr. 17 , 9–16. 10.1016/j.acap.2016.08.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yap M. B., Pilkington P. D., Ryan S. M., Jorm A. F. (2014). Parental factors associated with depression and anxiety in young people: a systematic review and meta-analysis . J. Affect. Disord. 156 , 8–23. 10.1016/j.jad.2013.11.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Young J. F., Mufson L. (2003). Manual for Interpersonal Psychotherapy-Adolescent Skills Training (IPT-AST) . New York, NY: Columbia University. [ Google Scholar ]
- Young J. F., Mufson L., Gallop R. (2010). Preventing depression: a randomized trial of interpersonal psychotherapy adolescent skills training . Depress. Anxiety 27 , 426–433. 10.1002/da.20664 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zhou H., Hao N., Liu Y., Sui Y., Wang Y., Ciu Y., et al. (2016). Reliability and validity of the eleven item Kutcher Adolescent Depression Scale, Chinese Version (KADS-11CV) . J. Child Adolesc. Behav. 4 :4 10.4172/2375-4494.1000308 [ CrossRef ] [ Google Scholar ]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 07 August 2023
A global mental health approach to depression in adolescence
- Ana Paula Donnelly 1
Nature Mental Health volume 1 , pages 527–528 ( 2023 ) Cite this article
151 Accesses
4 Altmetric
Metrics details
Adolescence is one of the most important transition periods in life, in which self-esteem and identity are being shaped and individuals experience profound social and physical transformations. In recent years, a concerning increase in the prevalence of mental health disorders in adolescents has been documented, prompting the mental health research community to prioritize understanding the risks of developing psychiatric disorders as well as factors that might be protective. Nature Mental Health spoke about depression in adolescence with Christian Kieling , an associate professor of child and adolescent psychiatry at the School of Medicine at the Federal University of Rio Grande do Sul in Brazil. Kieling is leading an international project called ‘Identifying depression early in adolescence ( IDEA )’ that brings a global health approach to the topic.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
55,14 € per year
only 4,60 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Author information
Authors and affiliations.
Nature Mental Health https://www.nature.com/natmentalhealth/
Ana Paula Donnelly
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ana Paula Donnelly .
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Donnelly, A.P. A global mental health approach to depression in adolescence. Nat. Mental Health 1 , 527–528 (2023). https://doi.org/10.1038/s44220-023-00107-y
Download citation
Published : 07 August 2023
Issue Date : August 2023
DOI : https://doi.org/10.1038/s44220-023-00107-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Anxiety, Depression, and Suicide in Youth
- Ned H. Kalin , M.D.
Search for more papers by this author
Anxiety disorders and depression are among the most common psychiatric illnesses affecting youth. Anxiety disorders typically begin in childhood, whereas the onset of depression frequently occurs later during adolescence or early adulthood. These illnesses are highly comorbid, with pathological anxiety regularly preceding the development of depression. The lifetime prevalence of anxiety disorders when assessed in adolescents is reported to be as high as 32% ( 1 ), whereas the estimated 12-month prevalence of major depression in adolescents is approximately 13% ( 2 ). Prior to adolescence, the incidence of these disorders is the same between boys and girls; however, as girls mature and go through puberty, they are approximately twice as likely as boys to be diagnosed with anxiety and major depression. In addition to causing considerable suffering and impaired functioning, when severe, these illnesses can be life threatening. Tragically, 6,200 suicide deaths were reported in 2017 among U.S. adolescents and young adults from 15 to 24 years of age ( 3 ), and suicide is the second leading cause of death among individuals 10–34 years of age ( 4 ).
As with other psychiatric illnesses, the risks for developing anxiety disorders and major depression are due to interactions between heritable and nonheritable factors. It is estimated that the heritability of anxiety and major depression is between 30% and 40%, leaving a considerable amount of the risk to potentially modifiable environmental factors. Genome-wide association studies with increasingly large sample sizes continue to identify genes that help explain a portion of the heritability for anxiety and depression ( 5 ). However, it is important to note that a recent study has provided evidence questioning the validity of previous findings that have linked a number of the familiar, “usual suspect” candidate genes (e.g., polymorphisms of the gene for the serotonin transporter protein) to be strongly associated with anxiety and depression ( 6 ). Early life trauma, neglect, inadequate parenting, and ongoing stress are among the environmental factors that contribute to the likelihood of developing anxiety, depression, and other stress-related disorders. Adolescence is a particularly vulnerable period, as the psychosocial challenges of adolescence converge with rapid and substantial developmental changes in the brain and in hormones. Prior to the onset of anxiety disorders and major depression, at-risk phenotypes or personality traits such as behavioral inhibition ( 7 ) and neuroticism ( 8 ), which are also partially heritable, can be identified and provide an opportunity for developing early intervention strategies for children at risk.
Two now classic clinical trials have evaluated the efficacy of selective serotonin reuptake inhibitors and cognitive therapies for the treatment of major depression and anxiety disorders in youth. The Treatment for Adolescents With Depression Study was a randomized 12-week trial involving 439 adolescents with major depression in which fluoxetine, cognitive-behavioral therapy (CBT), CBT plus fluoxetine, and placebo were compared ( 9 ). Results demonstrated that fluoxetine plus CBT and fluoxetine alone were significantly better than placebo, with the combination outperforming fluoxetine alone. CBT by itself did not statistically differ from placebo (fluoxetine plus CBT, 71% response; fluoxetine alone, 60.6% response; CBT alone, 43.2% response; placebo, 34.8% response). With continued treatment, rates of response remained high for up to 36 months ( 10 ). The Child/Adolescent Anxiety Multimodal Study was a randomized clinical trial comparing 14 CBT sessions with 12 weeks of sertraline plus CBT, sertraline alone, or placebo in 488 children and adolescents (7–17 years old) with separation anxiety disorder, generalized anxiety disorder, or social phobia ( 11 ). Results demonstrated that all therapies were more effective than placebo and that the combination of sertraline plus CBT was superior to the other active treatments (sertraline plus CBT, 80.7% response; CBT, 59.7% response; sertraline alone, 54.9% response; placebo, 23.7% response). Long-term follow-up of 319 of these children revealed that only 22% were in stable remission, whereas the remainder were either chronically ill or had relapsed ( 12 ). Taken together, these studies highlight the efficacy of relatively short-term interventions and point to the need for treatments that can fundamentally affect childhood developmental trajectories that will enable initial interventions to have long-lasting positive effects.
In this regard, a more complete understanding of the pathophysiology underlying anxiety disorders and major depression in youth is necessary to advance the development of new early intervention strategies. Neuroimaging studies suggest that anxiety and depression share alterations in the function of prefrontal-limbic circuits that underlie the adaptive regulation of emotion and the processing of anxiety ( 13 ), and studies also show alterations in reward-related processing to be associated with both anxiety and depression ( 14 , 15 ). However, to move beyond the associations between brain and behavior that have been identified with neuroimaging, preclinical studies are critical to elucidate potential mechanisms that underlie anxiety- and depression-related pathophysiology. For various reasons, developing valid preclinical animal models of depression has been challenging. In contrast, anxiety and fear can be effectively modeled in rodents and nonhuman primates ( 13 , 16 ), and such research has led to a deep understanding of the circuits, cells, and molecules that are mechanistically involved in mediating adaptive and pathological anxiety. The evolutionary expansion of the primate prefrontal cortex makes nonhuman primates particularly valuable for modeling human anxiety, as the expanded primate prefrontal cortex is prominently involved in mediating internal emotional experiences and cognitive processes that are unique to primate species and that, when aberrant, contribute to psychopathology.
The neural circuitry underlying fear and anxiety includes subcortical structures such as specific amygdala nuclei, the bed nucleus of the stria terminalis, the anterior hippocampus, and brainstem regions such as the periaqueductal gray ( 17 ). These subcortical regions, via their synaptic connectivity, work in concert with the ventromedial prefrontal cortex, the anterior insular cortex, the anterior cingulate cortex, and other regions of the posterior orbitofrontal cortex to regulate and process anxiety. In relation to major depression, the presence of anhedonia is a clinical feature that clearly distinguishes depression from anxiety. This diminished capacity to enjoy and engage with one’s world is in part mediated by altered function of the brain’s reward circuitry. For exam-ple, neuroimaging studies in adolescents with depression demonstrate altered reward-related responsivity of various components of this system, including the nucleus accumbens and striatum, as well as cortical regions such as the insular and the anterior cingulate cortices ( 14 ).
This issue of the Journal focuses on depression and anxiety during childhood and adolescence and importantly includes two articles that address mental health issues in disadvantaged youth living in poverty. We include four research articles that address critical treatment areas, including the use of CBT for treating childhood grief, ketamine for treatment-resistant adolescent depression, the use of neuroimaging in anxious youth to predict treatment response, and a preschool intervention for preventing psychopathology in disadvantaged children. Another article that is relevant to the health of disadvantaged and underresourced populations presents research that combines measures of inflammation with neuroimaging to better understand factors that may underlie physical health problems in children living in poverty. Other articles in this issue are focused on understanding underlying pathophysiology (capitalizing on neuroimaging data from the large Adolescent Brain Cognitive Development [ABCD] database), examining neuroimaging measures associated with suicidal thoughts, and examining reward-related neural processing in relation to disruptive behavior disorders.
Treating Prolonged Grief in Children and Adolescents
The loss of a loved one during childhood is traumatic and increases the risk to develop stress-related psychiatric illnesses such as depression and posttraumatic stress disorder (PTSD). Boelen and coauthors ( 18 ) present data from a randomized clinical trial comparing CBT aimed at coping with grief with an intervention employing supportive counseling in 134 children and adolescents who met criteria for prolonged grief disorder. Prolonged grief disorder, which was recently added to ICD-11, is defined by the presence of significant and interfering grief symptoms that last beyond the first 6 months after a loss. Although it is not in DSM-5, prolonged grief disorder is similar to the DSM-5 diagnosis of persistent complex bereavement disorder. In this study, each participant received nine sessions of the respective therapies, and their parents or caregivers received five therapy sessions focused on supporting their children and strengthening their relationship with their child. Results demonstrated that, when assessed at 3, 6, and 9 months posttreatment, both treatments had positive effects. However, the CBT group demonstrated greater decreases in grief symptoms at all posttreatment time points, and at 6 and 12 months, CBT considerably outperformed counseling in the domains of depression and PTSD symptoms. Margaret Crane and Lesley Norris, Ph.D. candidates, along with Dr. Philip Kendall from Temple University, contribute an editorial that speaks to moving beyond the findings presented in this study toward developing personalized treatment approaches for prolonged grief and modifying current treatment strategies to make them more widely accessible to suffering youth ( 19 ).
An Intervention in Children Living in Poverty Aimed at Reducing the Later Development of Psychopathology
Poverty is associated with numerous factors that are stressful and traumatic. To assess the extent to which an early school intervention can make a difference for impoverished children, Bierman et al. ( 20 ) report data from a randomized clinical trial examining the effects of an evidence-based intervention on the development of psychopathology, when assessed years later during adolescence. In this study, 356 4-year-old children from low-income families received an intervention consisting of a social-emotional learning program combined with an interactive reading program that was compared with usual educational practices. The children were recruited from three counties in Pennsylvania and came from families with a median annual income of $15,000. While differences between the interventions were not apparent when children were in the 7th grade, significant differences were observed when children reached 9th grade. For example, significantly fewer conduct problems, emotional symptoms, and peer problems were present in the 9th graders who, at 4 years of age, had participated in the social-emotional learning program. This study underscores the need to view the societal issue of poverty as stressful and traumatic, the disparities in health care associated with poverty, and the profound effects poverty can have on families and children. The findings are encouraging, with important public health implications, and clearly support early interventions aimed at promoting healthy social, emotional, and cognitive development in children facing the chronic adversity of growing up in poverty.
Enhanced Linkages Between Neural Activation and Inflammation in Impoverished Children
Miller and coauthors present data from a sample of early adolescents supporting an enhanced association between brain activation and peripheral inflammation that is selective to children living in poverty ( 21 ). The findings may shed light onto why underprivileged children have increased vulnerabilities to develop psychiatric and physical illnesses. The study was performed in 207 12- to 14-year-old children from the Chicago area who came from families across the socioeconomic spectrum. To explore a link between peripheral inflammation and neural function, the investigators correlated blood inflammatory markers (C-reactive protein, tumor necrosis factor-α, and interleukins-6, -8, and -10) with functional neuroimaging measures that assessed threat- and reward-related neural activation. First, the authors found that children living in poverty had higher levels of inflammation than children from higher socioeconomic backgrounds. In addition, the results demonstrated that in impoverished children, the inflammatory markers were positively correlated with both threat-related amygdala and reward-related striatal activation. The authors speculate that this enhanced coupling between neural and inflammatory processes may be due to the developmental impact of chronic adversity and may be a mechanism linking poverty to increased stress reactivity and illness. Interestingly, the positive relation between inflammatory markers and striatal activation was not in the predicted direction. Dr. Charles Nemeroff, from the University of Texas at Austin, contributes an editorial that emphasizes the deleterious effects of poverty on poor health and mental illness and further elaborates on the immune and neural alterations found in children who grow up in such impoverished and unfortunate conditions ( 22 ).
Neuroimaging Measures Are Not Good Predictors of Childhood Suicidal Ideation and Behavior
Vidal-Ribas and coworkers ( 23 ) use the large ABCD multimodal imaging database to comprehensively assess the usefulness of structural and functional brain measures in predicting childhood suicidal thoughts and behaviors. In a sample of 7,994 9- to 10-year-old children, the researchers found that 14.3% of the sample, or 1,140 children, had suicidal ideation or behaviors as reported by themselves or by caregivers. The occurrence of suicidal thoughts and behaviors was associated with increased levels of psychopathology and psychosocial adversity. Of the more than 5,000 statistical tests that were performed with multiple imaging measures (to assess cortical thickness, resting-state functional connectivity, and task-related functional activation), only one test survived correction for multiple comparisons. This finding revealed a relation between reduced thickness of the left bank of the superior temporal sulcus and caregiver-reported suicidal thoughts and behaviors. The authors draw the conclusion from these overall negative findings that current neuroimaging methods are not useful in reflecting the biological underpinnings of suicidal ideation and behavior in youth. In their editorial, Dr. Randy Auerbach from Columbia University and Drs. Henry Chase and David Brent from the University of Pittsburgh discuss the comprehensive and thorough nature of the study, the potential meaning of the superior temporal sulcus finding, and other critical aspects worth considering in future studies aimed at understanding the factors underlying youth suicide ( 24 ).
Reward-Related Functional Brain Alterations in Children With Disruptive Behavior Disorders and Callous-Unemotional Traits
Hawes et al. examine the extent to which children with disruptive behavior disorders (DBDs) (e.g., oppositional defiant disorder and conduct disorder) have alterations in neural responses to the anticipation and actual receipt of a reward ( 25 ). As in the Vidal-Ribas et al. study ( 23 ), these investigators used the ABCD neuroimaging database to provide a large sample size. Alterations in reward processing characterized by difficulties in delaying gratification and overvaluation of immediate rewards have been hypothesized to underlie externalizing phenotypes. In this study, reward-related brain activation in response to a monetary incentive delay task was examined in youth with DBDs who were subdivided into those with DBDs only (N=276) and those with DBDs with callous-unemotional traits (N=198), a characteristic that is more likely to be associated with antisocial behavior. The data from these children were compared with neuroimaging data from 693 typically developing youth. The children were, on average, 9.5 years old when studied. The findings from the study demonstrated that regardless of the presence of callous-unemotional traits, youth with DBDs exhibited decreased dorsal anterior cingulate activation in response to reward anticipation and increased orbitofrontal cortical and nucleus accumbens activation during reward receipt. Some neural activation differences between the DBD-only group and the DBD callous-unemotional trait group were also observed. Taken together, these findings shed light on the cortical control systems and subcortical reward-related neural substrates that may underlie the maladaptive behaviors characteristic of youth with DBDs.
Pretreatment Reward-Related Brain Activation Is Associated With Response to Psychotherapy in Youth With Anxiety Disorders
Sequeira and coworkers ( 26 ) explore the use of pretreatment functional imaging measures to predict treatment responses to psychotherapy in 9- to 14-year-old children with anxiety disorders (i.e., separation anxiety disorder, generalized anxiety disorder, or social anxiety disorder). Similar to other articles in this issue, this study probed reward-related brain activation. In this case, activation of brain regions encompassing the medial prefrontal cortex and the striatum was compared between the conditions of winning a reward relative to the experience of losing. The study included 50 children treated with 16 sessions of CBT, 22 children treated with child-centered therapy, and 37 healthy comparison youth. The intervention was effective, as 67% of the patients, regardless of treatment, responded to the intervention. Prior to treatment, greater activation of the medial prefrontal cortex was found in the patients with anxiety compared with the control subjects. However, the authors note that this difference in medial prefrontal activation could be accounted for by the co-occurrence of depressive symptoms in the anxiety group. Importantly, the authors found that as a group, treatment responders compared with nonresponders had increased pretreatment activation of regions encompassing the subgenual anterior cingulate cortex and the nucleus accumbens. These initial findings point to the potential importance of understanding reward-related brain systems in relation to psychotherapeutic outcomes in youth with anxiety. The authors speculate that increased striatal responsivity to rewards prior to treatment could be associated with increased motivation and engagement with therapy.
A Proof-of-Concept Trial Assessing Ketamine for Depression in Adolescents
Dwyer and colleagues ( 27 ) report the results of a small randomized double-blind single-dose crossover study in 17 adolescents with major depression who had not responded to at least one adequate trial of an antidepressant. In this trial, intravenous ketamine (0.5 mg/kg) or intravenous midazolam (0.045 mg/kg) was administered to each patient in a crossover design with a 2-week interval between treatments. Patients remained on their current psychiatric medications throughout the study. Sixteen patients completed both treatments, and the primary outcome was depression severity measured with the Montgomery-Åsberg Depression Rating Scale (MADRS) 24 hours after the infusion. Results demonstrated that 24 hours after infusion, ketamine had a significantly greater effect than midazolam in reducing depressive symptoms. For the midazolam infusion, the average pretreatment MADRS score was 31.88, and 24 hours later it was 24.13. For the ketamine infusion, the average pretreatment MADRS score was 30.56, and 24 hours later it was 15.44. Responders were defined by a 50% reduction in the MADRS score, and it was found that ketamine was associated with a response in 77% of the patients, with 35% of patients responding to midazolam (five of six of these participants also responded to ketamine). Compared with midazolam, the ketamine infusions were associated with reduced MADRS scores at all time points measured up to 14 days postinfusion. Ketamine was associated with dissociative side effects that were transient as well as with transient changes in blood pressure and heart rate. In their editorial ( 28 ), Drs. Parikh and Walkup from Northwestern University discuss the potential importance of this finding in relation to treating adolescent depression, but they also put into context such issues as the small sample size, the difficulty maintaining blinding because of ketamine’s dissociative effects, and concerns raised by others regarding the role of opiates in mediating ketamine’s effects in relation to its addiction potential ( 29 ).
Conclusions
Many psychiatric disorders have their origins early in life, which is clearly the case with anxiety and depression. In addition, the adolescent transition period is a time of increased risk during which psychiatric illnesses, especially depression, tend to emerge. Although there are adequate treatments for youth with anxiety and depressive disorders, many individuals do not respond to current treatments, and it is important to emphasize that many young people with psychiatric illnesses do not have access to available treatments. There is no question that we need better treatments and better access for children suffering from these disorders. This issue of the Journal highlights recent insights and clinical advances related to the treatment of anxiety disorders and major depression. Findings with the potential to directly affect the clinical care of youth include: demonstration of the efficacy of CBT in treating prolonged grief; early school socioemotional and cognitive interventions in disadvantaged children that prevent adolescent psychopathology; the rapid efficacy and safety of ketamine in reducing depressive symptoms in youth with treatment-resistant depression; and the promise of using functional neuroimaging to inform treatment choice and predict outcomes in youth with anxiety disorders. Other articles in this issue address pathophysiology, demonstrating increased coupling between brain and peripheral inflammatory markers in impoverished youth, altered reward-related brain activation in youth with DBDs, and a lack of association between structural and functional neuroimaging measures with suicidal ideation and behavior in youth. Continued research focused on a better understanding of the mechanisms underlying the early life risk to develop anxiety disorders and major depression is critical for the development of novel, improved treatment strategies. Efforts should be devoted to developing treatments that have the potential to positively affect the at-risk neurodevelopmental trajectories of vulnerable children. Such early life interventions provide the hope of moving beyond symptomatic treatment and toward prevention strategies.
Disclosures of Editors’ financial relationships appear in the April 2021 issue of the Journal .
1 Merikangas KR, He JP, Burstein M, et al. : Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) . J Am Acad Child Adolesc Psychiatry 2010 ; 49:980–989 Crossref , Medline , Google Scholar
2 Substance Abuse and Mental Health Services Administration (SAMHSA) : National Survey on Drug Use and Health . SAMHSA, Rockville, Md, 2017 Google Scholar
3 America’s Health Rankings : Teen suicide. https://www.americashealthrankings.org/explore/health-of-women-and-children/measure/teen_suicide/state/ALL Google Scholar
4 Centers for Disease Control and Prevention (CDC) : WISQARS Leading Causes of Death Reports . CDC, Atlanta, 2018 Google Scholar
5 Levey DF, Gelernter J, Polimanti R, et al. : Reproducible genetic risk loci for anxiety: results from ∼200,000 participants in the Million Veteran Program . Am J Psychiatry 2020 ; 177:223–232 Link , Google Scholar
6 Border R, Johnson EC, Evans LM, et al. : No support for historical candidate gene or candidate gene-by-interaction hypotheses for major depression across multiple large samples . Am J Psychiatry 2019 ; 176:376–387 Link , Google Scholar
7 Clauss JA, Blackford JU : Behavioral inhibition and risk for developing social anxiety disorder: a meta-analytic study . J Am Acad Child Adolesc Psychiatry 2012 ; 51:1066–1075.e1 Crossref , Medline , Google Scholar
8 Akingbuwa WA, Hammerschlag AR, Jami ES, et al. : Genetic associations between childhood psychopathology and adult depression and associated traits in 42 998 individuals: a meta-analysis . JAMA Psychiatry 2020 ; 77:715–728 Crossref , Medline , Google Scholar
9 March J, Silva S, Petrycki S, et al. : Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial . JAMA 2004 ; 292:807–820 Crossref , Medline , Google Scholar
10 Reinecke MA, Curry JF, March JS : Findings from the Treatment for Adolescents with Depression Study (TADS): what have we learned? What do we need to know? J Clin Child Adolesc Psychol 2009 ; 38:761–767 Crossref , Medline , Google Scholar
11 Walkup JT, Albano AM, Piacentini J, et al. : Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety . N Engl J Med 2008 ; 359:2753–2766 Crossref , Medline , Google Scholar
12 Ginsburg GS, Becker-Haimes EM, Keeton C, et al. : Results from the Child/Adolescent Anxiety Multimodal Extended Long-Term Study (CAMELS): primary anxiety outcomes . J Am Acad Child Adolesc Psychiatry 2018 ; 57:471–480 Crossref , Medline , Google Scholar
13 Kovner R, Oler JA, Kalin NH : Cortico-limbic interactions mediate adaptive and maladaptive responses relevant to psychopathology . Am J Psychiatry 2019 ; 176:987–999 Link , Google Scholar
14 Rappaport BI, Kandala S, Luby JL, et al. : Brain reward system dysfunction in adolescence: current, cumulative, and developmental periods of depression . Am J Psychiatry 2020 ; 177:754–763 Link , Google Scholar
15 Lahat A, Benson BE, Pine DS, et al. : Neural responses to reward in childhood: relations to early behavioral inhibition and social anxiety . Soc Cogn Affect Neurosci 2018 ; 13:281–289 Medline , Google Scholar
16 Fox AS, Kalin NH : A translational neuroscience approach to understanding the development of social anxiety disorder and its pathophysiology . Am J Psychiatry 2014 ; 171:1162–1173 Link , Google Scholar
17 Fox AS, Oler JA, Shackman AJ, et al. : Intergenerational neural mediators of early-life anxious temperament . Proc Natl Acad Sci USA 2015 ; 112:9118–9122 Crossref , Medline , Google Scholar
18 Boelen PA, Lenferink LIM, Spuij M : CBT for prolonged grief in children and adolescents: a randomized clinical trial . Am J Psychiatry 2021 ; 178:294–304 Abstract , Google Scholar
19 Kendall PC, Norris LA, Crane ME : Personalizing and delivering treatment for prolonged grief in youths (editorial). Am J Psychiatry 2021 ; 178:280–281 Abstract , Google Scholar
20 Bierman KL, Heinrichs BS, Welsh JA, et al. : Reducing adolescent psychopathology in socioeconomically disadvantaged children with a preschool intervention: a randomized controlled trial . Am J Psychiatry 2021 ; 178:305–312 Abstract , Google Scholar
21 Miller GE, White SF, Chen E, et al. : Association of inflammatory activity with larger neural responses to threat and reward among children living in poverty . Am J Psychiatry 2021 ; 178:313–320 Abstract , Google Scholar
22 Nemeroff CB : The trifecta of misery and disease vulnerability: poverty, childhood maltreatment, and inflammation (editorial). Am J Psychiatry 2021 ; 178:282–284 Abstract , Google Scholar
23 Vidal-Ribas P, Janiri D, Doucet GE, et al. : Multimodal neuroimaging of suicidal thoughts and behaviors in a U.S. population-based sample of school-age children . Am J Psychiatry 2021 ; 178:321–332 Abstract , Google Scholar
24 Auerbach RP, Chase HW, Brent DA : The elusive phenotype of preadolescent suicidal thoughts and behaviors: can neuroimaging deliver on its promise? (editorial). Am J Psychiatry 2021 ; 178:285–287 Abstract , Google Scholar
25 Hawes SW, Waller R, Byrd AL, et al. : Reward processing in children with disruptive behavior disorders and callous-unemotional traits in the ABCD study . Am J Psychiatry 2021 ; 178:333–342 Abstract , Google Scholar
26 Sequeira SL, Silk JS, Ladouceur CD, et al. : Association of neural reward circuitry function with response to psychotherapy in youths with anxiety disorders . Am J Psychiatry 2021 ; 178:343–351 Link , Google Scholar
27 Dwyer JB, Landeros-Weisenberger A, Johnson JA, et al. : Efficacy of intravenous ketamine in adolescent treatment-resistant depression: a randomized midazolam-controlled trial . Am J Psychiatry 2021 ; 178:352–362 Link , Google Scholar
28 Parikh T, Walkup JT : The future of ketamine in the treatment of teen depression (editorial). Am J Psychiatry 2021 ; 178:288–289 Abstract , Google Scholar
29 Williams NR, Heifets BD, Blasey C, et al. : Attenuation of antidepressant effects of ketamine by opioid receptor antagonism . Am J Psychiatry 2018 ; 175:1205–1215 Link , Google Scholar
- Cited by None
- Anxiety Disorders
- Depressive Disorders
- Suicide and Self-Harm
- Child/Adolescent Psychiatry
- Open access
- Published: 02 April 2024
Potential mental health-related harms associated with the universal screening of anxiety and depressive symptoms in Australian secondary schools
- Taylor A. Braund 1 , 2 ,
- Simon T. E. Baker 3 ,
- Mirjana Subotic-Kerry 1 , 2 ,
- Gabriel Tillman 4 ,
- Nathan J. Evans 5 ,
- Andrew Mackinnon 1 ,
- Helen Christensen 1 , 2 &
- Bridianne O’Dea 1 , 2
Child and Adolescent Psychiatry and Mental Health volume 18 , Article number: 46 ( 2024 ) Cite this article
29 Accesses
4 Altmetric
Metrics details
Anxiety and depressive disorders typically emerge in adolescence and can be chronic and disabling if not identified and treated early. School-based universal mental health screening may identify young people in need of mental health support and facilitate access to treatment. However, few studies have assessed the potential harms of this approach. This paper examines some of the potential mental health-related harms associated with the universal screening of anxiety and depression administered in Australian secondary schools.
A total of 1802 adolescent students from 22 secondary schools in New South Wales, Australia, were cluster randomised (at the school level) to receive either an intensive screening procedure (intervention) or a light touch screening procedure (control). Participants in the intensive screening condition received supervised self-report web-based screening questionnaires for anxiety, depression and suicidality with the follow-up care matched to their symptom severity. Participants in the light touch condition received unsupervised web-based screening for anxiety and depression only, followed by generalised advice on help-seeking. No other care was provided in this condition. Study outcomes included the increased risk of anxiety, depression, psychological distress, decreased risk of help-seeking, increased risk of mental health stigma, determined from measures assessed at baseline, 6 weeks post-baseline, and 12 weeks post-baseline. Differences between groups were analysed using mixed effect models.
Participants in the intensive screening group were not adversely affected when compared to the light touch screening condition across a range of potential harms. Rather, participants in the intensive screening group were found to have a decreased risk of inhibited help-seeking behaviour compared to the light touch screening condition.
Conclusions
The intensive screening procedure did not appear to adversely impact adolescents’ mental health relative to the light touch procedure. Future studies should examine other school-based approaches that may be more effective and efficient than universal screening for reducing mental health burden among students.
Trial registration Australian and New Zealand Clinical Trials Registry (ACTRN12618001539224) https://anzctr.org.au/Trial/Registration/TrialReview.aspx?id=375821 .
Introduction
Anxiety and depressive disorders can be chronic and disabling if not identified and treated early in the course of illness [ 21 ]. Universal mental health screening of adolescents has emerged as one potential method of the timely identification of young people in need of mental healthcare and support. By using validated questionnaires, screening can identify adolescents who may (a) have an increased risk of these illnesses or are experiencing subsyndromal symptoms so that preventive action can be taken, or (b) have undiagnosed, clinically significant levels of illness so that treatment can be administered. Using screening to triage adolescents into appropriate treatments may help to reduce symptoms and accelerate recovery, leading to improved future health outcomes [ 38 ]. There has been growing calls internationally for the broader uptake of mental health screening in settings where young people frequent, including health services and schools [ 16 , 19 , 48 ]. In 2016, the U.S. Preventive Services Task Force (USPSTF) recommended screening for major depressive disorder in adolescents aged 12 to 18 years [ 38 ] and recently [ 46 ] expanded this advice to include the screening for anxiety [ 45 ]. In Australia, the Federal government also recently invested over $10 million Australian dollars in a universal mental health and wellbeing screening tool for schools [ 9 ]. Conversely, the Royal Australian College of General Practitioners do not recommend routine screening for depression in adolescents in primary care [ 31 ]. While evidence-based practice calls for high quality evidence, a major challenge for policy makers in this domain is the limited informativeness of past trials for determining the potential harms of mental health screening in adolescents.
There is limited evidence from RCTs on the overall benefits of mental health screening programs in improving health outcomes, and an even greater gap in understanding the potential harms related to the screening process. The USPSTF recommendations were based on a review of 80 studies that evaluated the benefits or harms of screening for depression, anxiety, and suicide risk compared to ‘no screening’ or ‘usual care’. The evidence considered by the USPSTF primarily focused on the benefits and harms of exposing youth to anxiety and depression treatments and the accuracy of screening questionnaires, rather than the harms associated with other aspects of the screening processes such as the level of supervision, support, and intervention offered to participating youth [ 49 ]. Two systematic reviews Williams et al. [ 50 ] and Roseman et al. [ 36 ]) found no RCTs examining the effects of depression screening on outcomes for children and adolescents. This lack of evidence was further confirmed in a later review by Anderson et al. [ 2 ], who found only one RCT examining the utility of universal screening programs for youth mental health. Some recent RCTs have examined various screening approaches in schools, with mixed findings [ 14 , 20 , 27 , 37 ]. Sekhar et al. [ 37 ] found that adolescents who underwent universal screening for depression at school were 5.9 times more likely to be detected, 3.3 times more likely to confirm the need for treatment, and 2.1 times more likely to start, when compared to targeted screening [ 14 , 20 , 27 , 37 ]. This is consistent with Husky et al. [ 14 ], who also found that universal screening in schools led to a significantly greater proportion of youth being identified and referred to services than targeted screening. In a large, multi-site trial across six middle schools in the United States, Makover et al. [ 20 ] showed that universal screening was an effective method of detecting students who would benefit from a targeted depression intervention. In Australia, O'Dea et al. [ 27 ] found that a web-based screening platform with stepped-care interventions for depression and anxiety significantly improved adolescents’ likelihood of seeking help, but had no effect on their depressive symptoms. However, none of these studies explicitly examined the potential harms that may be associated with screening processes in adolescents.
When undertaken without adequate supervision and support, universal screening for depression and anxiety may induce distress through emotional activation and increased self-awareness of negative symptoms [ 35 , 39 ]. Inaccurate screening results may fail to identify all those in need or may lead to unnecessary intervention and overtreatment, wasted time and resources, victimisation, stigma, isolation, shame, and negative stereotyping [ 2 , 10 , 35 , 41 ]. Although universal mental health screening in schools is generally supported by parents and teachers [ 23 , 28 , 40 ], one in 10 parents have reported perceived harms due to lack of trained staff, and potential discomfort and stigmatisation of the student [ 40 ]. School counsellors have also reported specific concerns about parental agreement, students’ readiness for follow-up, and adequate resourcing of counsellors to care for all students in need [ 6 , 26 , 28 ]. These concerns have were validated in Sekhar and colleagues [ 37 ] large ( n > 12 k) school-based screening trial for depression, which found that the primary reason for failure of treatment initiation among students was lack of parent or individual consent. Screening may provide schools with important data on the need for mental health programs and help to guide decision-makers in selecting and targeting such programs. For example, a US County Schools Mental Health Coalition uses the prevalence of positive cases identified through screening to determine whether universal (prevalence rate > 20%) or selective programs (prevalence rate < 15%) are required [ 32 ]. However, the level of potential harm associated with different screening procedures and components remains unclear. A growing number of research trials have shown that some school-based mental health programs do result in iatrogenic effects [ 4 , 12 , 22 ]. As school-based screening programs are resource intensive, in terms of time, personnel, infrastructure, equipment and training [ 13 , 41 ], it is important for schools to carefully consider the suitability of these activities, to ensure that limited resources are being used effectively and efficiently to maximize benefits for students. It is vital for researchers and service designers to explicitly examine the potential harms of school-based screening with student mental health outcomes of paramount importance.
Objectives of the current paper
This paper explores some of the potential mental health-related harms associated with the universal screening of anxiety and depression administered in Australian secondary schools as part of a cluster RCT that examined the effectiveness of a digital mental health service for improving adolescents’ help-seeking [ 25 , 27 , 29 ]. This paper presents a secondary data analysis of this recent RCT as its design presents a unique opportunity to compare whether a more intensive screening procedure for anxiety and depression is associated with greater risk of potential mental health-related harms when compared to a control condition that involved a light touch screening procedure (see Fig. 1 ). For example, schools have mandatory reporting procedures that are initiated when a person reports suicidality. As a result, the use of this additional measure may lead unintended harm to students by initiating this process.
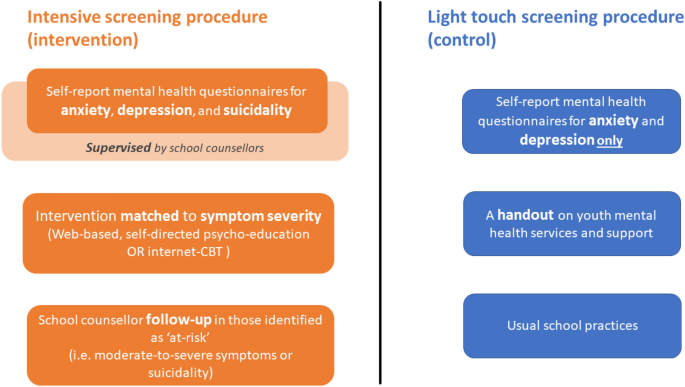
Brief overview of screening procedures examined in current study
In contrast to past work, this paper explicitly defines and measures student-level harms that are relevant to decision-makers wishing to compare school-based screening processes. In the current paper, the potential mental health-related harms examined were:
The increased risk of anxiety and depressive symptoms and psychological distress;
The increased risk of deterioration in help-seeking and daily functioning;
The increased risk of mental health stigma.
Hypotheses were framed in terms of the more intensive screening procedure (i.e., intervention condition) being no worse than the light touch screening procedure (i.e., control condition) and inferences were primarily based on point estimates and confidence intervals rather than significance to determine the risk of harms [ 11 , 44 ]. Based on previous findings [ 3 , 35 , 41 ], it was hypothesised that students who received the more intensive screening procedure would show no increase in risk of harm compared to students who received the ‘light touch’ procedure. These findings sought to provide the first evidence from an RCT on the potential mental health-related harms of universal screening and subsequent intervention for symptoms of anxiety and depression in the secondary school setting.
This paper is a secondary analysis of a two-arm 12 week cluster RCT. The trial was undertaken between February and December 2018 in secondary schools in New South Wales, Australia. Schools were the clusters and individual students were the participants [ 25 , 27 ]. The full trial protocol [ 25 ] and primary outcomes [ 27 ] have been published elsewhere. All mental health-related harms examined in this paper pertain to the individual participant level.
Participants
Secondary school adolescents (age range: 11–19 years) from grades (7–12) who attended participating schools were eligible to take part. A total of 1098 students from 12 schools were allocated to the control condition and 704 students from 10 schools were allocated to the intervention (CONSORT chart provided in Additional file 1 : Fig. S1). Participation was voluntary and parents/guardians who did not wish for their child to take part were instructed to notify the school or research team prior to the baseline assessment. Students provided informed online consent during the baseline assessment in the presence of the research team and a school representative.
Screening procedures
Intensive screening procedure (intervention condition).
As outlined in Fig. 1 and described in Additional file 1 the intensive screening procedure offered schools a comprehensive approach to universal screening, intervention and monitoring for anxiety and depression. Students in this condition completed the self-report screening measures for generalised anxiety and depressive symptoms using a web-based service platform called ‘Smooth Sailing’. This screening procedure involved an additional depressive symptom scale (Patient Health Questionnaire—9—Adolescent version, PHQ-9; [ 17 ], which included one item to assess students’ suicidality (i.e., thoughts of death and/or self-harm). Upon completion of the self-report screeners, the service then automatically recommended students complete activities that were matched to their symptom severity. The recommended activities were displayed to students on a personalised dashboard within the Smooth Sailing platform, which also provided generalised feedback on symptom severity. Using the thresholds of the GAD-7 and PHQ-9 screeners, students with ‘nil’ to ‘mild’ symptoms were recommended to complete a series of interactive, online, self-directed psycho-education modules that were hosted within the web-based platform. Students with ‘mild’ to ‘moderate’ symptoms were recommended to complete MoodGYM or BRAVE Online (two online, evidence-based, self-directed cognitive behavioural therapy programs for depression and anxiety in youth). Students with ‘moderately severe’ to ‘severe’ symptoms or who reported suicidality received an in-person follow-up with a school counsellor within 48 h. After 6 weeks, students repeated the mental health screening, and the level of intervention was then ‘stepped up’ in response to students’ deterioration. In this condition, all three screening sessions were conducted in the presence of a researcher, teacher, and school counsellor. The school counsellor was required to be onsite for 2 days after the screening sessions to ensure all students in need were attended to. School counsellors were given access to a purpose-built, secure online platform that enabled them to log in to identify and monitor the identified students. School counsellors were also provided with a list of local mental health service and supports that they could refer students to. The research team contacted all participating school counsellors after 48 h of the screening sessions to ensure all follow-ups had been conducted.
Light touch screening procedure (Control condition)
Students in this condition completed the screening measures using an identical web-based platform to the screening procedure 1; however, the PHQ-9 scale (which included the measure on suicidality) was not administered. Upon completion of the screening measures, students in this condition were not given access to any of the additional processes or components (i.e., symptom feedback, psycho-education modules, online cognitive behavioural therapy program, follow-ups with the school counsellor). Instead, all students were displayed information on a range of different youth mental health services and support (including in-person, web-based and telephone services). This information was also provided to students as a one-page printed handout. In this arm, the screening procedure was conducted in the presence of a researcher and schoolteacher. The school counsellor was required to be onsite only on the day of screening but did not attend the screening sessions. No additional contact was made with the schools after each screening session. No limitations were placed on these students’ mental healthcare activities, practices, or help-seeking during the study period.
Measures of mental health-related harms
Depressive symptoms.
Depressive symptoms were measured using the Centre for Epidemiologic Studies Depression Scale—Child version (CES-DC) [ 34 ]. This 20-item self-report scale was administered at baseline and 12 weeks post-baseline. Item scores were summed, with higher scores indicative of greater depressive symptoms. For the sample included in this paper, participants’ total scores ranged from 0 to 60 and Cronbach’s alpha was 0.93. For this paper, total scores ≥ 16 were classified as clinically meaningful cases and ‘new’ cases were participants who emerged as a case only at week 12.
Anxiety symptoms
Anxiety symptoms were measured using the Generalised Anxiety Disorder Questionnaire (GAD-7) [ 42 ]. This 7-item self-report scale was administered at baseline and 12 weeks post-baseline. Item scores were summed, with higher scores indicative of greater anxiety with the following score descriptors: ‘nil to mild’ (0–9), ‘moderate’ (10–14), or ‘moderately severe to severe’ (≥ 15). For the sample included in this paper, participants’ total scores ranged from 0 to 21 and the Cronbach’s alpha was 0.89. For this paper, total scores ≥ 10 were classified as clinically meaningful cases and ‘new’ cases were participants who emerged as a case only at week 12.
Psychological distress
Psychological distress was measured using the Distress Questionnaire-5 (DQ5) [ 5 ]. This 5-item self-report scale was administered at baseline and 12 weeks post-baseline. Item scores were summed, with higher scores indicative of greater psychological distress. For the sample included in this paper, total scores ranged from 5 to 25 and the Cronbach’s alpha was 0.88. For this paper, total scores ≥ 14 were classified as clinically meaningful cases [ 5 ] and ‘new’ cases were participants who emerged as a case only at week 12.
Help-seeking intentions and behaviour
The General Help-Seeking Questionnaire (GHSQ) [ 51 ] was used to measure participants’ intentions to seek help for general mental health problems. This was administered at baseline and 12 weeks post-baseline. Using a 5-point Likert scale, participants were asked to rate how likely they were to seek help from 13 sources when having a tough time with their mental health. Item scores were summed, with higher scores indicative of greater intentions to seek help. For the sample included in this paper, the total scores ranged from 13 to 65 and the Cronbach’s alpha was 0.87. The Actual Help-Seeking Questionnaire (AHSQ) [ 33 ] was used to measure help-seeking behaviour for mental health among participants. Participants were asked whether they had turned to the same list of sources outlined in the GHSQ for help with any mental health issue in the past three months (answered yes or no). For this paper, the 12-week assessment was utilised and participants were classified as an ‘inhibited help-seeker’ based on whether they self-identified as needing support for their mental health but did not seek help from anyone (i.e. those who answered yes to the final item of AHSQ “I needed support but I did not seek help from anyone”).
Mental health stigma
This was measured using the Mental Health Literacy Scale (MHLS) [ 24 ]. This 13-item composite scale measured students’ confidence in seeking help (4 items) and their level of stigmatising attitudes towards mental illness (9 items) at baseline and 12 weeks post-baseline. Items were rated on a 5-point Likert scale. Item scores were summed, with higher total scores indicative of greater confidence in help-seeking and lower levels of stigma. The MHLS has demonstrated good internal and test–retest reliability and has been used in school-based mental health research [ 47 ]. For the sample included in this paper, participants’ scores ranged from 13 to 65 and the Cronbach’s alpha was 0.71.
Daily functioning
To determine the functional impairment caused by their mental health problems, participants were asked to rate “how difficult have your mental health problems made it for you to do your schoolwork, take care of things at home, or get along with your mates and family?” using a 4-point Likert scale with answers ranging from “not difficult at all” to “extremely difficult”. This question is a supplementary item within the adolescent version of the PHQ-9 scale [ 17 ]. In this sample, participants scores ranged from 0 to 3. For this paper, the 12-week assessment was utilised and participants were classified as ‘Not impaired’ (i.e., those who responded, “not difficult at all” or “somewhat difficult”) or ‘Impaired’ (i.e., those who responded, “very difficult” or “extremely difficult”).
Reliable change scores
As the GHSQ and MHLS do not have established cut-points, reliable change (RC) scores were calculated to assess meaningful individual-level change. Individual difference scores were calculated by subtracting the total score at baseline ( \({{\text{X}}}_{1}\) ) from the total score at 12 weeks post-baseline ( \({{\text{X}}}_{2}\) ). These difference scores were then used to calculate RC scores (for formulas used to calculate RC scores, see Additional file 1 : Text S2). \({\text{RC}}\le -1.96\) and \({\text{RC}}\ge 1.96\) indicate a statistically significant difference from the average difference score and therefore reflect a “reliable change.”
Harms analysis
Case classification, reliable change, and other classifications were then used to calculate several measures such as risk ratios and risk differences. Equations for each of these measures are presented in Additional file 1 : Table S1 and were computed for each outcome by comparing the occurrence of that outcome among students in the screening condition (i.e., Experimental Event Rate [EER]) to its occurrence among students in the control condition (i.e., Control Event Rate [CER]).
Statistical analyses
All analyses were conducted using Stata 17.0 [ 43 ]. Group differences between the conditions at baseline were examined using mixed linear or logit models. Baseline characteristics were included as the dependent variables, condition was included as a fixed effect, and school was included as a cluster random effect. Poisson generalised linear models with robust standard errors were used to estimate the relative risk of harmful outcomes between the conditions, which have shown to outperform log binomial models when calculating risk ratios [ 8 , 52 ]. Outcomes (i.e., case classifications, reliable change scores, and other classifications) were included as the dependent variables, condition was included as a fixed effect, and school was included as a cluster random effect. Population average estimates were used instead of cluster specific estimates to control for the effects over clusters. Intracluster correlation coefficients (ICC) were calculated to examine the impact of clustering. The ∞ component of the confidence intervals for relative risk of harmful outcomes indicates instances where the statistical test is non-significant. Specifically, these instances occur when transforming both positive and negative values (and hence spans zero), resulting in confidence intervals that encompass two disjointed regions (e.g., NNTB to ∞, NNTH to ∞). As a result, confidence intervals were expressed as number needed to treat for harm (NNTH) to ∞ to number need to treat for benefit (NNTB) for continuity, in line with Altman [ 1 ].
Participant characteristics are presented in Table 1 . No significant differences were found between the intensive screening group and light touch group on baseline sample characteristics. Case classification frequencies are presented in Table 2 and reliable change and other classification frequencies are presented in Table 3 .
Risk measures
Event rates and risk indices for each outcome classification are presented in Table 4 . Intensive screening was associated with a decreased risk of experiencing inhibited help-seeking behaviour (Relative Risk Reduction = 50%, 95% CI [27%, 74%]; Absolute Risk Reduction = 9%, 95% CI [3%, 15%]) with the NNTB indicating that 11 (95% CI [3, 19]) students needed to be screened to prevent 1 case of inhibited help-seeking behaviour. No other confidence intervals crossed the 0 threshold for risk ratios or ∞ for NNTB.
This paper examined some of the potential mental health-related harms associated with two types of universal school-based screening procedures for anxiety and depression in Australian adolescents using data from a cluster RCT. Given the lack of research in this field, this investigation aimed to provide additional insights to help policy-makers and researchers determine best-practice for school-based mental health screening in Australia and worldwide. Notably, there were a high number of cases of anxiety, depression, and psychological distress in the whole sample at baseline, which offers some support to the USPSTF’s recommendation of the need for universal screening for depression and anxiety in adolescents. In the current study, students who received the more intensive screening procedure were not adversely affected when compared to those who received the light touch procedure on a range of potential mental health-related harms, including the increased risk of clinically significant symptoms of anxiety, depression, and psychological distress or the deterioration in help-seeking intentions or mental health stigma. This is an important finding, given the more intensive screening procedure involved the assessment of suicidality, the provision of symptom feedback, and mandated follow-ups with school counsellors, which may have introduced the potential for greater risk. Overall, these findings suggest that the more intensive procedure did not appear to harm students on the measures collected.
In this paper, we investigated two types of screening procedures that differed in the intensity of care and intervention provided to students as well as the resources required by the schools. We found that the more intensive screening procedure resulted in a significantly lower risk of inhibited help-seeking behaviour in students. This is consistent with the primary outcomes of the effectiveness trial [ 27 ] and is an important finding given that inhibited help-seeking behaviour (i.e., having a self-identified need for mental health support but not actively seeking help) prolongs mental distress and delays treatment gains. This finding is consistent with Sekhar et al. [ 37 ] and indicates that direct links to accessible care are required for universal screening programs to shift help-seeking outcomes in adolescents. As the positive impacts of screening on health outcomes are mitigated by individuals’ willingness to engage in the treatment provided [ 15 ], careful consideration must also be given to the interventions recommended by adolescent screening programs. In this study, adolescents’ preferences for digital therapies (e.g., increased privacy, accessibility, autonomy) may have moderated the positive effects of the intensive screening procedure on help-seeking [ 30 ]. Different levels of harm may be found when the integrated treatments do not align with adolescents’ expectations, needs and or accessibility requirements. Furthermore, the interventions provided by screening programs may also have indirect effects on adolescent mental health. In this study, the intense screening procedure may have increased students’ awareness to and openness to other school-based supports (e.g. the school counsellor) but inverse effects may be found with different screening procedures. Future trials would also benefit from extrapolating the direct and indirect effects of screening processes on adolescent health outcomes and using qualitative inquiry to capture other types of experiences that are not easily measured through questionnaires.
While students who received the more intensive screening procedure were not adversely affected on any of the mental health harms examined when compared to the light touch procedure, the more intensive procedure required significantly more resources from both the students and schools, even with the integration of self-directed digital interventions. For example, students needed to allocate more time to this approach and required ongoing access to a computer and the Internet for completion of the digital content. School counsellors were also required to allocate significantly more time to completing training on the screening procedure and portal, supervising the screening practices, and following up all students who required it. As time, resources and costs impede the uptake of school-based mental health identification programs [ 13 , 41 ], the intensive procedure may therefore not be feasible for all schools, despite low levels of harm. The few studies (none from Australia) that have examined the cost-effectiveness of school-based mental health screening approaches have had mixed findings [ 2 , 7 , 18 ]. Future studies should therefore aim to quantify the direct costs of universal screening programs for mental health in the Australian context, in comparison with other initiatives, so that schools are better placed to evaluate program affordability, sustainability and cost versus benefits.
Limitations
This study was a secondary analysis of a cluster RCT and was not specifically designed to test for harms. As such, the findings are exploratory in nature. Further, as screening is likely to generate greatest benefit when delivered ‘en masse’, different levels of harms may emerge when larger samples from more schools are exposed to universal screening. Notably, data on other important potential harms (e.g., impact of false-positive and false-negative results, lack of treatment uptake and non-adherence, negative treatment effects) were not available for this study. While a single item was used to assess daily functioning for brevity and minimal participant burden, a more comprehensive assessment would benefit from the possibility of deeper insights into how their symptoms have impacted their daily life and relationships. The relatively short study period also limited the examination of long-term harms. There may be flow on effects of the negative experiences of universal screening on students, such as disengagement in care and reluctance to participate in other school-based mental health programs. In addition, as this study relied on voluntary participation, different levels of harms may emerge when screening is compulsory. Lastly, as suggested by Foulkes and Stringaris [ 12 ], there may be subgroups of adolescents who will experience harms from screening-related interventions, which may be masked when findings are averaged. There may also be harms associated with the different components of universal screening programs, such as the types of treatment young people are referred to, that are better captured through qualitative research.
Our findings suggest that the intensive screening procedure examined by this paper did not appear to increase mental health-related harms for adolescents when compared to the light touch procedure. The intensive screening procedure may offer a beneficial approach for improving aspects of help-seeking behaviour. These results may alleviate some of the concerns held by schools, parents, and students on the benefits of screening and may facilitate greater participation in these procedures. However, given the high resource burden of the intensive screening, future studies are needed to determine whether this approach is superior to other school-based interventions for improving adolescents’ mental health. Moreover, future studies on school-based mental health screening should routinely define, assess, and report on potential harms over extended periods to comprehensively evaluate the impact and net benefit for students.
Availability of data and materials
The data collected and analysed in the current trial is not currently available to researchers outside of the approved team due to constraints placed on the project by the various ethics bodies. Additional related project documents are currently available from the web-based Australian and New Zealand Clinical Trials Registry.
Altman DG. Confidence intervals for the number needed to treat. BMJ. 1998;317(7168):1309–12. https://doi.org/10.1136/bmj.317.7168.1309 .
Article CAS PubMed PubMed Central Google Scholar
Anderson JK, Ford T, Soneson E, Coon JT, Humphrey A, Rogers M, Moore D, Jones PB, Clarke E, Howarth E. A systematic review of effectiveness and cost-effectiveness of school-based identification of children and young people at risk of, or currently experiencing mental health difficulties. Psychol Med. 2019;49(1):9–19. https://doi.org/10.1017/s0033291718002490 .
Article PubMed Google Scholar
Anderson JK, Ford T, Soneson E, Coon JT, Humphrey A, Rogers M, Moore D, Jones PB, Clarke E, Howarth E. A systematic review of effectiveness and cost-effectiveness of school-based identification of children and young people at risk of, or currently experiencing mental health difficulties. Psychol Med. 2019;49(1):9–19. https://doi.org/10.1017/S0033291718002490 .
Andrews JL, Birrell L, Chapman C, Teesson M, Newton N, Allsop S, McBride N, Hides L, Andrews G, Olsen N, Mewton L, Slade T. Evaluating the effectiveness of a universal eHealth school-based prevention programme for depression and anxiety, and the moderating role of friendship network characteristics. Psychol Med. 2022. https://doi.org/10.1017/s0033291722002033 .
Article PubMed PubMed Central Google Scholar
Batterham PJ, Sunderland M, Carragher N, Calear AL, Mackinnon AJ, Slade T. The distress questionnaire-5: population screener for psychological distress was more accurate than the K6/K10. J Clin Epidemiol. 2016;71:35–42. https://doi.org/10.1016/j.jclinepi.2015.10.005 .
Burns JR, Rapee RM. Barriers to universal mental health screening in schools: the perspective of school psychologists. J App School Psychol. 2022;38(3):223–40. https://doi.org/10.1080/15377903.2021.1941470 .
Article Google Scholar
Chatterji P, Caffray CM, Crowe M, Freeman L, Jensen P. Cost Assessment of a school-based mental health screening and treatment program in New York City. Ment Health Serv Res. 2004;6(3):155–66. https://doi.org/10.1023/B:MHSR.0000036489.50470.cb .
Chen W, Qian L, Shi J, Franklin M. Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med Res Methodol. 2018;18(1):63. https://doi.org/10.1186/s12874-018-0519-5 .
Clare J, McBride E. Half a billion dollar investment into student wellbeing . 2023. https://ministers.education.gov.au/clare/half-billion-dollar-investment-student-wellbeing#:~:text=%24192%20million%20in%20additional%20one,get%20the%20support%20they%20need .
Cosgrove L, Karter JM, Vaswani A, Thombs BD. Unexamined assumptions and unintended consequences of routine screening for depression. J Psychosom Res. 2018;109:9–11. https://doi.org/10.1016/j.jpsychores.2018.03.007 .
Dunn DT, Copas AJ, Brocklehurst P. Superiority and non-inferiority: two sides of the same coin? Trials. 2018;19(1):499. https://doi.org/10.1186/s13063-018-2885-z .
Foulkes L, Stringaris A. Do no harm: can school mental health interventions cause iatrogenic harm? BJPsych Bull. 2023. https://doi.org/10.1192/bjb.2023.9 .
Garbacz SA, Godfrey E, Twombly T, Collins B, Porter J, Davis E, Fischer K, Albers CA. Principal perspectives on addressing youth mental health within schools. School Ment Health. 2023. https://doi.org/10.1007/s12310-023-09588-9 .
Husky MM, Kaplan A, McGuire L, Flynn L, Chrostowski C, Olfson M. Identifying adolescents at risk through voluntary school-based mental health screening. J Adolesc. 2011;34(3):505–11. https://doi.org/10.1016/j.adolescence.2010.05.018 .
Iragorri N, Spackman E. Assessing the value of screening tools: reviewing the challenges and opportunities of cost-effectiveness analysis. Public Health Rev. 2018;39(1):17. https://doi.org/10.1186/s40985-018-0093-8 .
Kass M, Alexander L, Moskowitz K, James N, Salum GA, Leventhal B, Merikangas K, Milham MP. Parental preferences for mental health screening of youths from a multinational survey. JAMA Netw Open. 2023;6(6):e2318892–e2318892. https://doi.org/10.1001/jamanetworkopen.2023.18892 .
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x .
Kuo E, Vander Stoep A, McCauley E, Kernic MA. Cost-effectiveness of a school-based emotional health screening program. J Sch Health. 2009;79(6):277–85. https://doi.org/10.1111/j.1746-1561.2009.00410.x .
Lustig S, Kaess M, Schnyder N, Michel C, Brunner R, Tubiana A, Kahn J-P, Sarchiapone M, Hoven CW, Barzilay S, Apter A, Balazs J, Bobes J, Saiz PA, Cozman D, Cotter P, Kereszteny A, Podlogar T, Postuvan V, Värnik A, Resch F, Carli V, Wasserman D. The impact of school-based screening on service use in adolescents at risk for mental health problems and risk-behaviour. Eur Child Adolesc Psychiatry. 2023;32(9):1745–54. https://doi.org/10.1007/s00787-022-01990-z .
Makover H, Adrian M, Wilks C, Read K, Stoep AV, McCauley E. Indicated prevention for depression at the transition to high school: outcomes for depression and anxiety. Prev Sci. 2019;20(4):499–509. https://doi.org/10.1007/s11121-019-01005-5 .
Merikangas KR, Cui L, Kattan G, Carlson GA, Youngstrom EA, Angst J. Mania with and without depression in a community sample of US adolescents. Arch Gen Psychiatry. 2012;69(9):943–51. https://doi.org/10.1001/archgenpsychiatry.2012.38 .
Montero-Marin J, Allwood M, Ball S, Crane C, De Wilde K, Hinze V, Jones B, Lord L, Nuthall E, Raja A, Taylor L, Tudor K, Blakemore SJ, Byford S, Dalgleish T, Ford T, Greenberg MT, Ukoumunne OC, Williams JMG, Kuyken W. School-based mindfulness training in early adolescence: what works, for whom and how in the MYRIAD trial? Evid Based Ment Health. 2022;25(3):117–24. https://doi.org/10.1136/ebmental-2022-300439 .
Moore SA, Dowdy E, Hinton T, DiStefano C, Greer FW. Moving toward implementation of universal mental health screening by examining attitudes toward school-based practices. Behavioral Disord. 2020;47(3):166–75. https://doi.org/10.1177/0198742920982591 .
O’Connor M, Casey L. The mental health literacy scale (MHLS): a new scale-based measure of mental health literacy. Psychiatry Res. 2015;229(1–2):511–6. https://doi.org/10.1016/j.psychres.2015.05.064 .
O’Dea B, King C, Subotic-Kerry M, Anderson M, Achilles MR, Parker B, Mackinnon A, Anderson J, Cockayne N, Christensen H. Evaluating a web-based mental health service for secondary school students in Australia: protocol for a cluster randomized controlled trial. JMIR Res Protoc. 2019;8(5): e12892. https://doi.org/10.2196/12892 .
O’Dea B, King C, Subotic-Kerry M, O’Moore K, Christensen H. School counselors’ perspectives of a web-based stepped care mental health service for schools: cross-sectional online survey. JMIR Ment Health. 2017;4(4): e55. https://doi.org/10.2196/mental.8369 .
O’Dea B, Subotic-Kerry M, King C, Mackinnon AJ, Achilles MR, Anderson M, Parker B, Werner-Seidler A, Torok M, Cockayne N, Baker STE, Christensen H.2021 A cluster randomised controlled trial of a web-based youth mental health service in Australian schools. The Lancet Regional Health—Western Pacific, doi: https://doi.org/10.1016/j.lanwpc.2021.100178
O’Dea B, King C, Achilles MR, Calear AL, Subotic-Kerry M. Delivering a digital mental health service in Australian secondary schools: understanding school counsellors’ and parents’ experiences. Health Services Insights. 2021;14:11786329211017688. https://doi.org/10.1177/11786329211017689 .
O’Dea B, King C, Subotic-Kerry M, Achilles MR, Cockayne N, Christensen H. Smooth sailing: a pilot study of an online, school-based, mental health service for depression and anxiety [Original Research]. Front Psychiatry. 2019. https://doi.org/10.3389/fpsyt.2019.00574 .
Pretorius C, Chambers D, Coyle D. Young People’s Online Help-Seeking and mental health difficulties: systematic narrative review. J Med Internet Res. 2019;21(11): e13873. https://doi.org/10.2196/13873 .
RACGP. (2016). RACGP Guidelines for preventive activities in general practice 9th edition . The RACGP. https://www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/guidelines-for-preventive-activities-in-general-pr/psychosocial/depression#ref-num-31
Reinke WM, Thompson A, Herman KC, Holmes S, Owens S, Cohen D, Tanner-Jones LA, Henry L, Green A, Copeland C. The county schools mental health coalition: a model for community-level impact. School Mental Health. 2018;10(2):173–80. https://doi.org/10.1007/s12310-017-9227-2 .
Rickwood D, Deane FP, Wilson CJ, Ciarrochi J. Young people’s help-seeking for mental health problems. Aust e-J Advancement Mental Health. 2005;4(3):218–51. https://doi.org/10.5172/jamh.4.3.218 .
Roberts RE, Andrews JA, Lewinsohn PM, Hops H. Assessment of depression in adolescents using the Center for Epidemiologic Studies Depression Scale. Psychol Assess: A J Consult Clin Psychol. 1990;2(2):122–8. https://doi.org/10.1037/1040-3590.2.2.122 .
Robinson J, Pan Yuen H, Martin C, Hughes A, Baksheev GN, Dodd S, Bapat S, Schwass W, McGorry P, Yung AR. Does screening high school students for psychological distress, deliberate self-harm, or suicidal ideation cause distress—and is it acceptable? Crisis. 2011;32(5):254–63. https://doi.org/10.1027/0227-5910/a000087 .
Roseman M, Saadat N, Riehm KE, Kloda LA, Boruff J, Ickowicz A, Baltzer F, Katz LY, Patten SB, Rousseau C, Thombs BD. Depression screening and health outcomes in children and adolescents: a systematic review. Can J Psychiatry. 2017;62(12):813–7. https://doi.org/10.1177/0706743717727243 .
Sekhar DL, Schaefer EW, Waxmonsky JG, Walker-Harding LR, Pattison KL, Molinari A, Rosen P, Kraschnewski JL. Screening in high schools to identify, evaluate, and lower depression among adolescents: a randomized clinical trial. JAMA Netw Open. 2021;4(11):e2131836–e2131836. https://doi.org/10.1001/jamanetworkopen.2021.31836 .
Siu AL, Force USPST. Screening for depression in children and adolescents: U.S. preventive services task force recommendation statement. Ann Intern Med. 2016;164(5):360–6. https://doi.org/10.7326/M15-2957 .
Skar A-MS, Ormhaug SM, Jensen TK. Reported levels of upset in youth after routine trauma screening at mental health clinics. JAMA Netw Open. 2019;2(5):e194003–e194003. https://doi.org/10.1001/jamanetworkopen.2019.4003 .
Soneson E, Childs-Fegredo J, Anderson JK, Stochl J, Fazel M, Ford T, Humphrey A, Jones PB, Howarth E. Acceptability of screening for mental health difficulties in primary schools: a survey of UK parents. BMC public health. 2018;18(1):1404. https://doi.org/10.1186/s12889-018-6279-7 .
Soneson E, Howarth E, Ford T, Humphrey A, Jones PB, Thompson Coon J, Rogers M, Anderson JK. Feasibility of school-based identification of children and adolescents experiencing, or at-risk of developing, mental health difficulties: a systematic review. Prev Sci. 2020;21(5):581–603. https://doi.org/10.1007/s11121-020-01095-6 .
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7. https://doi.org/10.1001/archinte.166.10.1092 .
StataCorp. (2021). Stata Statistical Software: Release 17 . StataCorp LP.
Sterne JAC, Cox DR, Smith GD. <span hwp:id="article-title-1" class="article-title">Sifting the evidence—what's wrong with significance tests?</span><span hwp:id="article-title-36" class="sub-article-title">Another comment on the role of statistical methods</span>. BMJ, 2001:322(7280), 226. https://doi.org/10.1136/bmj.322.7280.226
US Preventive Services Task Force. Screening for anxiety in children and adolescents: us preventive services task force recommendation statement. JAMA. 2022;328(14):1438–44. https://doi.org/10.1001/jama.2022.16936 .
US Preventive Services Task Force. Screening for depression and suicide risk in children and adolescents: us preventive services task force recommendation statement. JAMA. 2022;328(15):1534–42. https://doi.org/10.1001/jama.2022.16946 .
Vella SA, Swann C, Batterham M, Boydell KM, Eckermann S, Fogarty A, Hurley D, Liddle SK, Lonsdale C, Miller A, Noetel M, Okely AD, Sanders T, Telenta J, Deane FP. Ahead of the game protocol: a multi-component, community sport-based program targeting prevention, promotion and early intervention for mental health among adolescent males. BMC public health. 2018;18(1):390. https://doi.org/10.1186/s12889-018-5319-7 .
Villarreal V, Castro-Villarreal F, Peterson LS, Bear M, Cortes DM, Escobedo T. Meta-analysis of proportions of students screened and identified in mental health multiple-gate screening research. School Psychol Rev. 2023;52(2):130–43. https://doi.org/10.1080/2372966X.2022.2106155 .
Viswanathan M, Wallace I, Middleton CJ , Kennedy SM, McKeeman J, Hudson K, Rains C, Schaaf EBV, Kahwati L. Screening for Depression, Anxiety, and Suicide Risk in Children and Adolescents: An Evidence Review for the U.S. Preventive Services Task Force. 2022; https://www.uspreventiveservicestaskforce.org/uspstf/document/draft-evidence-review/screening-anxiety-children-adolescents
Williams SB, O’Connor EA, Eder M, Whitlock EP. Screening for child and adolescent depression in primary care settings: a systematic evidence review for the US Preventive Services Task Force. Pediatrics. 2009;123(4):e716-735. https://doi.org/10.1542/peds.2008-2415 .
Wilson CJ, Deane FP, Ciarrochi J, Rickwood D. Measuring help-seeking intentions: properties of the general help-seeking questionnaire. Can J Couns. 2005;39(1):15–28.
Google Scholar
Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–6. https://doi.org/10.1093/aje/kwh090 .
Download references
Acknowledgements
The authors would like to acknowledge the Black Dog Institute IT team who supported the build and implementation of the web-based service and research trial. The authors would like to acknowledge the Trial Steering Committee for their oversight, guidance, and support throughout the design and evaluation of the Smooth Sailing service model.
This work was supported by HSBC and the Graf Foundation from a non-competitive philanthropic research grant donation to the Black Dog Institute. The funders had no role in the design, execution, analyses, data interpretation, authorship or the decision to submit the paper for publication.
Author information
Authors and affiliations.
Black Dog Institute, University of New South Wales, Randwick, NSW, Australia
Taylor A. Braund, Mirjana Subotic-Kerry, Andrew Mackinnon, Helen Christensen & Bridianne O’Dea
Faculty of Medicine and Health, University of New South Wales, Sydney, NSW, Australia
Taylor A. Braund, Mirjana Subotic-Kerry, Helen Christensen & Bridianne O’Dea
Orygen, University of Melbourne, Melbourne, VIC, Australia
Simon T. E. Baker
Institute of Health and Wellbeing, Federation University, Ballarat, VIC, Australia
Gabriel Tillman
School of Psychology, University of Queensland, St Lucia, QLD, Australia
Nathan J. Evans
You can also search for this author in PubMed Google Scholar
Contributions
TAB: Analysis, interpretation, knowledge, authorship and editing. STEB: Conception, interpretation, knowledge, authorship and editing. MSK: Recruitment, data collection, interpretation, knowledge, authorship and editing. GT: Interpretation, knowledge, authorship and editing. NJE: Interpretation, knowledge, authorship and editing. AM: Analysis, Interpretation, knowledge, authorship and editing. HC: Interpretation, knowledge, authorship and editing. BOD: Conception, recruitment, data collection, interpretation, knowledge, authorship and editing.
Corresponding author
Correspondence to Taylor A. Braund .
Ethics declarations
Ethics approval and consent to participate.
Ethics approvals were obtained from the University of New South Wales Human Research Ethics Committee (HC17910), the State Education Research Applications Process for the New South Wales Department of Education (2016471), the Sydney Catholic Schools Research Centre (20186), and the Catholic Schools Office Diocese of Maitland-Newcastle. The trial was registered with the Australian and New Zealand Clinical Trials Registry (ACTRN12618001539224). Students gave their informed consent to participate on the day of the baseline assessment via a signed PICF that was witnessed by the research team (for full details, see [ 27 ].
Consent for publication
Not applicable.
Competing interests
BOD and HC reports philanthropic non-competitive research grants from HSBC and the Graf Foundation during the conduct of the trial. BOD reports speaker fees and travel reimbursements from the New South Wales and Queensland Departments of Education, paid to the Black Dog Institute for educational training seminars, that were outside the submitted work. All other authors have no conflicts to disclose.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file1: figure s1..
Consort Chart. Table S1. Risk Measures and Equations. Text S1. Description of Smooth Sailing. Text S2. RC Score Calculation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Braund, T.A., Baker, S.T.E., Subotic-Kerry, M. et al. Potential mental health-related harms associated with the universal screening of anxiety and depressive symptoms in Australian secondary schools. Child Adolesc Psychiatry Ment Health 18 , 46 (2024). https://doi.org/10.1186/s13034-024-00734-y
Download citation
Received : 18 December 2023
Accepted : 15 March 2024
Published : 02 April 2024
DOI : https://doi.org/10.1186/s13034-024-00734-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Intervention

Child and Adolescent Psychiatry and Mental Health
ISSN: 1753-2000
- Submission enquiries: [email protected]
- Patient Care & Health Information
- Diseases & Conditions
- Teen depression
Teen depression is a serious mental health problem that causes a persistent feeling of sadness and loss of interest in activities. It affects how your teenager thinks, feels and behaves, and it can cause emotional, functional and physical problems. Although depression can occur at any time in life, symptoms may be different between teens and adults.
Issues such as peer pressure, academic expectations and changing bodies can bring a lot of ups and downs for teens. But for some teens, the lows are more than just temporary feelings — they're a symptom of depression.
Teen depression isn't a weakness or something that can be overcome with willpower — it can have serious consequences and requires long-term treatment. For most teens, depression symptoms ease with treatment such as medication and psychological counseling.
Products & Services
- A Book: A Practical Guide to Help Kids of All Ages Thrive
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Teen depression signs and symptoms include a change from the teenager's previous attitude and behavior that can cause significant distress and problems at school or home, in social activities, or in other areas of life.
Depression symptoms can vary in severity, but changes in your teen's emotions and behavior may include the examples below.
Emotional changes
Be alert for emotional changes, such as:
- Feelings of sadness, which can include crying spells for no apparent reason
- Frustration or feelings of anger, even over small matters
- Feeling hopeless or empty
- Irritable or annoyed mood
- Loss of interest or pleasure in usual activities
- Loss of interest in, or conflict with, family and friends
- Low self-esteem
- Feelings of worthlessness or guilt
- Fixation on past failures or exaggerated self-blame or self-criticism
- Extreme sensitivity to rejection or failure, and the need for excessive reassurance
- Trouble thinking, concentrating, making decisions and remembering things
- Ongoing sense that life and the future are grim and bleak
- Frequent thoughts of death, dying or suicide
Behavioral changes
Watch for changes in behavior, such as:
- Tiredness and loss of energy
- Insomnia or sleeping too much
- Changes in appetite — decreased appetite and weight loss, or increased cravings for food and weight gain
- Use of alcohol or drugs
- Agitation or restlessness — for example, pacing, hand-wringing or an inability to sit still
- Slowed thinking, speaking or body movements
- Frequent complaints of unexplained body aches and headaches, which may include frequent visits to the school nurse
- Social isolation
- Poor school performance or frequent absences from school
- Less attention to personal hygiene or appearance
- Angry outbursts, disruptive or risky behavior, or other acting-out behaviors
- Self-harm — for example, cutting or burning
- Making a suicide plan or a suicide attempt
What's normal and what's not
It can be difficult to tell the difference between ups and downs that are just part of being a teenager and teen depression. Talk with your teen. Try to determine whether he or she seems capable of managing challenging feelings, or if life seems overwhelming.
When to see a doctor
If depression signs and symptoms continue, begin to interfere in your teen's life, or cause you to have concerns about suicide or your teen's safety, talk to a doctor or a mental health professional trained to work with adolescents. Your teen's family doctor or pediatrician is a good place to start. Or your teen's school may recommend someone.
Depression symptoms likely won't get better on their own — and they may get worse or lead to other problems if untreated. Depressed teenagers may be at risk of suicide, even if signs and symptoms don't appear to be severe.
If you're a teen and you think you may be depressed — or you have a friend who may be depressed — don't wait to get help. Talk to a health care provider such as your doctor or school nurse. Share your concerns with a parent, a close friend, a spiritual leader, a teacher or someone else you trust.
Suicide is often associated with depression. If you think you may hurt yourself or attempt suicide, call 911 or your local emergency number immediately.
Also consider these options if you're having suicidal thoughts:
- Call your mental health professional.
- In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . The Spanish language phone line is 1-888-628-9454 (toll-free). Services are free and confidential.
- Or contact a crisis service for teenagers in the U.S. called TXT 4 HELP : Text the word "safe" and your current location to 4HELP (44357) for immediate help, with the option for interactive texting.
- Seek help from your primary care doctor or other health care provider.
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader or someone else in your faith community.
If a loved one or friend is in danger of attempting suicide or has made an attempt:
- Make sure someone stays with that person.
- Call 911 or your local emergency number immediately.
- Or, if you can do so safely, take the person to the nearest hospital emergency room.
Never ignore comments or concerns about suicide. Always take action to get help.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
It's not known exactly what causes depression, but a variety of issues may be involved. These include:
- Brain chemistry. Neurotransmitters are naturally occurring brain chemicals that carry signals to other parts of your brain and body. When these chemicals are abnormal or impaired, the function of nerve receptors and nerve systems changes, leading to depression.
- Hormones. Changes in the body's balance of hormones may be involved in causing or triggering depression.
- Inherited traits. Depression is more common in people whose blood relatives — such as a parent or grandparent — also have the condition.
- Early childhood trauma. Traumatic events during childhood, such as physical or emotional abuse, or loss of a parent, may cause changes in the brain that increase the risk of depression.
- Learned patterns of negative thinking. Teen depression may be linked to learning to feel helpless — rather than learning to feel capable of finding solutions for life's challenges.
Risk factors
Many factors increase the risk of developing or triggering teen depression, including:
- Having issues that negatively impact self-esteem, such as obesity, peer problems, long-term bullying or academic problems
- Having been the victim or witness of violence, such as physical or sexual abuse
- Having other mental health conditions, such as bipolar disorder, an anxiety disorder, a personality disorder, anorexia or bulimia
- Having a learning disability or attention-deficit/hyperactivity disorder (ADHD)
- Having ongoing pain or a chronic physical illness such as cancer, diabetes or asthma
- Having certain personality traits, such as low self-esteem or being overly dependent, self-critical or pessimistic
- Abusing alcohol, nicotine or other drugs
- Being gay, lesbian, bisexual or transgender in an unsupportive environment
Family history and issues with family or others may also increase your teenager's risk of depression, such as:
- Having a parent, grandparent or other blood relative with depression, bipolar disorder or alcohol use problems
- Having a family member who died by suicide
- Having a family with major communication and relationship problems
- Having experienced recent stressful life events, such as parental divorce, parental military service or the death of a loved one
Complications
Untreated depression can result in emotional, behavioral and health problems that affect every area of your teenager's life. Complications related to teen depression may include, for example:
- Alcohol and drug misuse
- Academic problems
- Family conflicts and relationship difficulties
- Suicide attempts or suicide
There's no sure way to prevent depression. However, these strategies may help. Encourage your teenager to:
- Take steps to control stress, increase resilience and boost self-esteem to help handle issues when they arise
- Practice self-care, for example by creating a healthy sleep routine and using electronics responsibly and in moderation
- Reach out for friendship and social support, especially in times of crisis
- Get treatment at the earliest sign of a problem to help prevent depression from worsening
- Maintain ongoing treatment, if recommended, even after symptoms let up, to help prevent a relapse of depression symptoms
Teen depression care at Mayo Clinic
- Depressive disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. American Psychiatric Association; 2013. https://dsm.psychiatryonline.org. Accessed May 4, 2021.
- Bipolar and related disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. American Psychiatric Association; 2013. https://dsm.psychiatryonline.org. Accessed May 4, 2021.
- Brown AY. Allscripts EPSi. Mayo Clinic. April 9, 2021.
- Teen depression. National Institute of Mental Health. https://www.nimh.nih.gov/health/publications/teen-depression/. Accessed March 30, 2022.
- Depression in children and teens. American Academy of Child and Adolescent Psychiatry. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/The-Depressed-Child-004.aspx. Accessed May 4, 2021.
- Psychotherapy for children and adolescents: Different types. American Academy of Child and Adolescent Psychiatry. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Psychotherapies-For-Children-And-Adolescents-086.aspx. Accessed May 4, 2021.
- Suicidality in children and adolescents being treated with antidepressant medications. U.S. Food and Drug Administration. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/suicidality-children-and-adolescents-being-treated-antidepressant-medications. Accessed May 4, 2021.
- Depression medicines. U.S. Food and Drug Administration. https://www.fda.gov/consumers/free-publications-women/depression-medicines. Accessed May 4, 2021.
- Building your resilience. American Psychological Association. https://www.apa.org/topics/resilience. Accessed May 4, 2021.
- Psychiatric medications for children and adolescents: Part I ― How medications are used. American Academy of Child and Adolescent Psychiatry. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Psychiatric-Medication-For-Children-And-Adolescents-Part-I-How-Medications-Are-Used-021.aspx. Accessed May 4, 2021.
- Psychiatric medications for children and adolescents: Part II ― Types of medications. American Academy of Child and Adolescent Psychiatry. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Psychiatric-Medication-For-Children-And-Adolescents-Part-II-Types-Of-Medications-029.aspx. Accessed May 5, 2021.
- Weersing VR, et al. Evidence-base update of psychosocial treatments for child and adolescent depression. Journal of Clinical Child and Adolescent Psychology. 2017; doi:10.1080/15374416.2016.1220310.
- Zuckerbrot RA, et al. Guidelines for adolescent depression in primary care (GLAD-PC): Part I. Practice preparation, identification, assessment, and initial management. Pediatrics. 2018; doi:10.1542/peds.2017-4081.
- Cheung AH, et al. Guidelines for adolescent depression in primary care (GLAD-PC): Part II. Treatment and ongoing management. Pediatrics. 2018; doi:10.1542/peds.2017-4082.
- Resilience guide for parents and teachers. American Psychological Association. https://www.apa.org/topics/resilience/guide-parents-teachers. Accessed May 4, 2021.
- Rice F, et al. Adolescent and adult differences in major depression symptoms profiles. Journal of Affective Disorders. 2019; doi:10.1016/j.jad.2018.09.015.
- Haller H, et al. Complementary therapies for clinical depression: An overview of systemic reviews. BMJ Open. 2019; doi:10.1136/bmjopen-2018-028527.
- Ng JY, et al. Complementary and alternative medicine recommendations for depression: A systematic review and assessment of clinical practice guidelines. BMC Complementary Medicine and Therapeutics. 2020; doi:10.1186/s12906-020-03085-1.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 92: Use of psychiatric medications during pregnancy and lactation. Obstetrics & Gynecology. 2008; doi:10.1097/AOG.0b013e31816fd910. Reaffirmed 2019.
- Neavin DR, et al. Treatment of major depressive disorder in pediatric populations. Diseases. 2018; doi:10.3390/diseases6020048.
- Vande Voort JL (expert opinion). Mayo Clinic. June 29, 2021.
- Safe Place: TXT 4 HELP. https://www.nationalsafeplace.org/ txt-4-help. Accessed March 30, 2022.
- Antidepressants for children and teens
Associated Procedures
- Acupuncture
- Cognitive behavioral therapy
- Psychotherapy
News from Mayo Clinic
- Mayo Clinic Minute: Know the difference between adult and teen depression April 15, 2022, 04:00 p.m. CDT
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Psychiatry hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Open access
- Published: 03 April 2024
Depression, stress, and anxiety versus internet addiction in early and middle adolescent groups: the mediating roles of family and school environments
- Maryam Aziz ORCID: orcid.org/0000-0002-5031-4951 1 ,
- Khansa Chemnad ORCID: orcid.org/0000-0001-5052-9285 1 ,
- Sanaa Al-Harahsheh 2 ,
- Azza O. Abdelmoneium 3 ,
- Ahmed Baghdady 4 &
- Raian Ali ORCID: orcid.org/0000-0002-5285-7829 1
BMC Psychology volume 12 , Article number: 184 ( 2024 ) Cite this article
Metrics details
Family and school environment play a crucial role across the different developmental stages of adolescence. This paper investigates the potential mediating role of family and school environments in the relationship between the three psychosocial predictors of depression, anxiety, stress, and Internet addiction (IA). Specifically, it focuses on the two stages of early and middle adolescence.
The study involved a survey of 407 adolescents from Qatar, comprising 250 early adolescents and 157 middle adolescents. Inclusion criteria for the study included adolescents between the ages of 10 to 17 years old, residents of Qatar and studying in a Qatar-based school. To assess the constructs of the three psychosocial predictors, IA, family environment, the study utilized the Depression, Stress, and Anxiety Scale (DASS), the Internet Addiction Diagnostic Questionnaire (IADQ), and the Brief Family Relationship Scale, respectively. School environment was measured using questions from the “Health Behavior in School-aged Children: WHO Collaborative Cross-National survey/study (HBSC) 2013–2014. The study applied standard mediation analysis between the DASS components and IA with family and school environment as the mediators.
Results from the mediation analysis reveal insights into the relationships between psychosocial predictors and IA. The findings indicate that family and school environments partially mediated the relationship with regards to depression, stress, and anxiety in early adolescents. In middle adolescents, family environment partially mediated the relationship with depression and stress and fully mediating the relationship with anxiety. Meanwhile, school environment only exhibited partial mediation in the relationship with anxiety in middle adolescence.
Conclusions
These results highlight the crucial role parents and schools play in addressing problematic technology usage that develops as a response to depression, anxiety, and stress among adolescents. Moreover, the study reveals nuances in the mediating role of family and school environment in early and middle adolescence. This highlights the evolving nature of these influences across the different stages of development. Notably, this study contributes to the literature by moving beyond the conventional focus on the so-called WEIRD population, and offering valuable insights from a region that is underrepresented in current research.
Peer Review reports
The excessive use of the Internet in daily lives is leading to growing public concerns towards adolescent Internet Addiction (IA). High prevalence rates of adolescent IA have been estimated in several countries including 26.5% in China [ 1 ], 20.6% in the United States [ 2 ], 23.7% in Japan [ 3 ] and 17.7% in Turkey [ 4 ]. The direct comparisons between these rates should be approached with caution due to subtle differences in the time of study, sampling methods, and measurement tools used in each research. While IA is not officially recognized as a mental disorder by the American Psychiatric Association (APA) [ 5 ], gaming disorder is formally included in the 11th version of the International Classification of Diseases (ICD-11) by WHO in 2018 [ 6 ]. As of yet, no clear and definitive definition exists of IA [ 7 ], however, several broad definitions have been mentioned in literature. IA, also known as “problematic Internet use”, “compulsive Internet use”, and “pathological Internet use” is defined as the excessive or uncontrollable use of the Internet leading to symptoms of withdrawal, tolerance, and negative psychological concerns by Young [ 8 ]. Lai & Kwan [ 9 ] gave an alternative perspective on IA defining it as “the excessive use of the Internet that causes disturbances or harm to the individual”.Click or tap here to enter text. Furthermore, previous literature has also widely debated on the constructs of IA. Baggio et al. [ 10 ] found problematic online behaviors manifested through problematic Internet use, occurred as separate but related issues. Despite no official diagnostic criteria existing for IA, Young [ 8 ] defined the diagnostic criteria for IA based on the extreme gambling criteria suggested in DSM-IV. The four characteristics of addictive behaviors mentioned in DSM-IV: excessive use, withdrawal, tolerance, and adverse psychological consequences are frequently observed in internet-addicted individuals [ 11 ]. As such, the Young’s Internet Addiction Scale is an adaptation of the DSM-IV symptoms for addictive behaviors. Adolescents, particularly, are vulnerable to IA as the sensitivity of their developing brains to signals of excitement causes them difficulties in controlling their Internet use [ 12 ]. IA in adolescents has also been linked to other maladaptive behaviors such as aggressiveness [ 13 , 14 ], impulsivity [ 14 ] and suicidal behavior [ 15 ]. This makes it crucial to identify and understand the factors of IA and their underlying mechanisms.
Adolescent IA and psychosocial predictors
IA has been repeatedly associated with negative psychosocial conditions in adolescents. Several studies have demonstrated that depression [ 16 , 17 , 18 ], stress [ 17 , 18 , 19 ], and anxiety [ 16 , 17 ] were positively related with IA in adolescents. IA can be both a result of a psychological state or condition and a way to mitigate and cope with it. Adolescents may turn to the Internet as a way to cope with negative emotional problems [ 20 ]. This may be explained by the mood enhancement hypothesis that states that individuals facing psychosocial problems are more likely to turn to recreational activities including technology use to alleviate their mood [ 21 ]. Online interactions may also provide a sense of comfort with reduced perceived threat compared to face-to-face interactions due to the anonymity involved. While adolescents’ sensitivity to excitement may cause them to feel temporary happiness and relief when using the Internet, they may not understand that it is a means of escape rather than the solution to their emotional state. The temporary change from negative to positive emotions with internet use may lead the adolescents to assume that increased internet use leads to increased happiness. However, they may end up being trapped in the cycle of continued Internet use to lessen negative emotions and improve positive emotions without realizing that they no longer experience the same level of change from negative to positive emotion over time [ 22 ].
WEIRD vs. Non-WEIRD Population: sampling considerations
Most literature in psychology relies on the western, educated, industrialized, rich, and democratic (WEIRD) population creating the so-called replication crisis in psychology and sampling bias [ 23 ]. In contrast, studies aimed at the non-WEIRD population are limited. Henrich et al. [ 23 ] argues that the WEIRD population constitutes to about 12% of the world’s population hence the results from the WEIRD-dominated population cannot be generalized to the rest of the world. Since adolescent IA is a global concern with Asian countries reportedly having higher prevalence rates compared to Western countries [ 24 ], it is essential to conduct studies inclusive of the non-WEIRD population. Studies show that adolescents IA is impacted by academic pressure [ 25 ], cultural differences [ 26 ], and social aspects [ 11 ]. It is important to note that the WEIRD and non-WEIRD population may differ in these educational, cultural, and social domains. This raises the need to study adolescent IA with a focus on the non-WEIRD population. Our study adds to the literature on non-WEIRD population and adolescent IA by utilizing a sample from the population resident to Qatar.
Developmental changes and adolescence period
During the adolescence period, individuals experience major developmental changes including physical, emotional, and cognitive transitions. This phase also involves the development of one’s ability to reflect on their own and other’s behaviors with strong reflective functioning being a protective factor against risky behaviors [ 27 ]. These developmental changes differ amongst the various stages of adolescence. Early adolescence period is marked by dramatic physical, cognitive, and social changes. Along with the shift from childlike features to a more adult appearance, early adolescents also see a change in their social relationships and cognitive thinking [ 28 ]. Social relationships in this period expand beyond their families to include peer groups. The early adolescence period also involves individuals experiencing rapid cognitive growth and struggling with their sense of identity and ability to regulate emotions [ 29 ]. The middle adolescence period sees a continuing physical growth along with an increasing need to find one’s unique competence, which is the abilities and interests that become a part of their identity [ 30 ]. Past literature has suggested that adolescents’ identity development may be linked to the development of problematic behaviors [ 31 ].
Socioecological influences: family and school environment
The socioecological model by Bronfenbrenner [ 32 ] states that developing individuals are influenced by the various levels of ecological systems surrounding them and their interactions with these systems. The model places parents and schools as the central part of an individual’s immediate environment, that is one that has the most influence on them during the development phase. According to the attachment theory by Bowlby [ 33 ], when parents provide children with a secure environment, they tend to be more confident, and develop better social and emotional skills. With the onset of adolescence period introducing difficult developmental changes, family environment can play a center role towards the development of problem behaviors [ 34 ]. Having a negative family environment prone to parental conflicts, hostility, and inconsistency can negatively impact adolescent mental health. A study by Wang et al. [ 35 ] found family dysfunction was positively related to depression and anxiety in Chinese early adolescents. Another longitudinal study on Chinese adolescents found that family dysfunction was positively associated with anxiety levels in adolescents [ 36 ]. Family environment also plays an essential role in how adolescents develop effective coping strategies [ 37 ]. A survey on adolescents in China found the quality of family relationships posed as risk factor for adolescent Internet addiction [ 1 ]. Another survey conducted on early adolescents in Central Taiwan found family functionality and depression as predictors of adolescent IA where adolescents with poor family atmosphere and high depression were more prone to Internet addiction [ 38 ]. In addition, a study by Aziz et al., [ 39 ] surveyed parents in Qatar and looked at the interplay between adolescent IA and the family-related factors of parents’ IA, frequency of parents’ serious arguments with adolescent on excessive Internet use and parenting styles. Their results identified three different interactions between adolescent IA and the family factors namely assertive, aggressive, and lenient interactions. Research on the relation between parental IA and adolescent IA in Chemnad et al. [ 40 ] utilized the same dataset used in [ 39 ] and showed that adolescents were highly likely to be dependent Internet users when their parents were also dependent Internet users showing the important role of family in adolescent IA. This leads us to propose the following hypothesis:
Family environment mediates the relationship between depression, stress, and anxiety (DAS), and IA in adolescents.
Adolescents spend a significant amount of time in schools, making it a key environment setting that can strongly influence their psychological and emotional well-being [ 41 ]. Factors of school environment, such as academic pressure, have been shown to impact adolescent mental health negatively. For instance, a study by Frӧjd et al. [ 42 ] revealed that middle adolescents experiencing problems with school performance and assignments reported higher levels of depression. Similarly, a survey conducted by Ogilvie et al. [ 43 ] found significant associations between school-related issues, such as school difficulties, engagement, and avoidance, and psychological and emotional problems in adolescents. Academic challenges, including struggling with homework completion and unnecessary pressure to keep up with the class, can lead to frustration, feelings of inadequacy, and contribute to elevated levels of stress and anxiety.
School environment has also been associated with maladaptive behavior in adolescents. The study by Chemnad et al. [ 44 ] indicated that a positive school environment was linked to lower levels of IA among adolescents, suggesting that a supportive and nurturing school setting can be beneficial for their well-being. On the other hand, a cross-sectional study by Zhai et al. [ 45 ] found that adolescents who perceived their school climate negatively were more likely to report higher levels of Internet addiction. This highlights the significant role schools play in shaping adolescent behavior and the importance of creating a positive and conducive learning environment to promote healthier outcomes. Thus, we propose the following hypothesis:
School environment mediates the relationship between depression, stress, and anxiety (DAS), and IA in adolescents.
Research gap and study rationale
On the context of adolescent IA, several studies reported levels of IA differed amongst the different age groups of adolescents with IA level increasing as age progresses in adolescents [ 19 ]. While both early and middle adolescents are vulnerable to IA, their different developmental stages may lead them to being exposed to different IA related risk and protective factors. For example, a study by Badenes-Ribera et al. [ 46 ] found levels of Facebook addiction in early adolescents was influenced by parental attachment whereas in middle adolescents Facebook addiction levels were impacted by peer relationships. The middle adolescence period also sees an increasing reliance on peer groups and a need to separate from familial relations [ 29 ]. Technology access also differs among early and middle adolescents. A survey conducted on late adolescents in United States found almost 16% reported receiving smartphones in early adolescent stage whereas approximately 61% reported receiving smartphones in middle adolescence period [ 47 ]. This makes it crucial to study early and middle adolescents individually and the impact that different risk factors of IA may have on them. By studying them independently, interventions and prevention approaches can be effectively tailored to each adolescent phase taking into consideration the differences due to their developmental changes, relationship dynamics and family influences.
Family and school environment play a central role in an adolescent’s life and are key to understanding adolescent IA and mental health. A major gap in the literature relates to the limited studies on the role of family and school environment when discussing DAS and adolescent IA. Moreover, prior studies did not make a clear distinction between the early and middle adolescence stages in that context. In addition, most literature on adolescent IA predominantly utilized a WEIRD sample whereas limited research is conducted on the non-WEIRD sample. Hence, our research aims to add to the literature on DAS and adolescent IA by studying the mediating role of family and school environment in a sample of early and middle adolescents that are resident to Qatar.
Participants
Participants for this study were recruited through an online survey administered using SurveyMonkey. The link to the survey was shared with the students at 16 schools selected randomly. The survey period lasted 3 months between March 2022 and May 2022. Prior approval was obtained from the Institutional Review Board (IRB) of Hamad Bin Khalifa University (No. QBRI-IRB 2021-05-094) and the study was carried out according to the guidelines stated in the Declaration of Helsinki. In addition, school permissions were also acquired to distribute the survey and informed consent was obtained from both parents and adolescents. Participation in the study was voluntary.
Inclusion criteria for this study comprised of adolescents between the ages of 10 to 17 years old, residents of Qatar and studying in a Qatar-based school. Participants that did not meet the inclusion criteria were excluded from the study. We did not include the technology penetration criteria in our inclusion criteria as technology penetration in Qatar is already high bordering at 99% [ 48 ]. Of the 586 participants who responded, those who gave incomplete and hasty answers were removed. As such, 407 participants were included in the final study which met the criteria of 5% margin of error at the 95% confidence interval.
The survey collected information regarding participants’ demographics, digital technology usage and IA. Data regarding participants’ physical and psychological health status were also gathered. The survey was administered in both English and Arabic. The Arabic survey was generated using the back-translation method [ 49 ] to ensure the quality of translation and the preservation of the original meaning is maintained.
Internet Addiction Diagnostic Questionnaire (IADQ)
The Internet Addiction Diagnostic Questionnaire (IADQ) was used to assess adolescent IA level. The IADQ comprised of eight closed-ended questions (yes/no) where the IA score is the total number of questions the participant responded to in affirmative. Each question represents a different symptom of IA that are preoccupation with internet, tolerance, unsuccessful efforts to control Internet use repeatedly, withdrawal, staying online longer than intended, risk/loss of relationships and opportunities because of the Internet use, lies to conceal the extent of involvement and dysfunctional coping. Participants were asked to answer the questionnaire based on their non-essential internet use, (non-business or non-academic use). The IADQ total score ranges between 0 and 8, where Young [ 8 ] suggests that a score of 5 or higher classifies the participant as a dependent internet user. In line with the suggestion by Young [ 8 ], we classified participants who scored 5 or above as dependent users and below 5 as non-dependent users. Previous literature on IADQ states the Cronbach’s alpha to be within the range of 0.60 and 0.72 [ 50 ]. The Cronbach’s alpha for the present sample was 0.64.
Depression, anxiety, stress scale – 21 (DASS-21)
The Depression, Anxiety, Stress Scale – 21 items is a set of three self-report scales that are used to assess the degree of depression, anxiety, and stress in individuals [ 51 ]. The three subscales each have seven items that measure a negative emotional symptom. The depression scale rates symptoms of dysphoria, helplessness, life devaluation, self-deprecation, loss of interest, anhedonia, and lethargy. The autonomic arousal, skeletal muscle effects, situational anxiety, and subjective sensation of anxious affect are all measured by the anxiety scale. The stress scale evaluates issues with relaxation, nervousness, irritability, overreacting, and impatience. The scores for the relevant questions are added up to determine the scores for depression, anxiety, and stress and then scaled up by 2. Each subscale ranges from 0 to 42 and the cutoff scores for the severity categories (normal, mild, moderate, severe, and extremely severe) are unique to each subscale. Cronbach’s alpha for depression scale was found to be 0.94 in literature, 0.87 for the anxiety scale and 0.91 for the stress scale [ 52 ]. For the present study, the Cronbach’s alpha for depression, anxiety and stress scale was determined to be at 0.88, 0.87, and 0.85 respectively which indicates a very good reliability [ 53 ].
Brief family relationship scale (BFRS)
The Brief Family Relationship Scale is a 16-item scale that measures three dimensions of family functioning that is cohesion, expressiveness, and conflict. The BFRS is used to examine youth perceptions of family. The scale uses a 3–point Likert scale where 1 = not at all, 2 = sometimes, and 3 = a lot. The total score is the sum of the 16 questions and participants can accumulate a maximum possible score of 48 where the higher the score the less family functioning is experience. The Cronbach alpha was reported as 0.88 [ 54 ] in literature whereas for the present study it was found to be 0.89, a very good level of reliability [ 53 ].
School environment
The school environment variable was measured using questions from the “Health Behavior in School-aged Children: WHO Collaborative Cross- National survey/study (HBSC) 2013–2014” [ 55 ]. The HBSC is an international collaboration project between research groups across North America and Europe aimed at understanding adolescents’ health and wellbeing behaviors. The questions were adapted from the section on school settings in HSBC. Three items assessed the school environment: (1) “how do you feel about school at present?”, (2) “how pressured do you feel by the schoolwork/homework you have to do?”, and (3) “how much of a problem have you had getting your schoolwork/homework done on time?”. Responses for the school feeling were 1= “I don’t like it at all”, 2= “I don’t like it very much”, 3= “I like it a bit” and 4= “I like it a lot”. The possible responses for school pressure were 1= “A lot”, 2= “Some”, 3= “A little” and 4= “Not at all”. For schoolwork problems, the possible responses were 1= “A serious problem”, 2= “A considerable problem”, 3= “Some problem” and 4= “No problem”.
Statistical analysis
Descriptive statistics were computed for all variables. The statistical analysis for this study was performed using JASP 0.16.3 [ 56 ]. Exploratory factor analysis was employed with an orthogonal varimax rotation to discover the underlying structure of the school environment variables. The number of factors to retain was determined by the following criteria: (1) The scree plot needed to align with the number of factors extracted, and (2) the resulting factors lead to a meaningful interpretation. Mediation analysis was conducted using the standard mediation method available in the JASP software. JASP utilizes the product of coefficient approach [ 57 ] to implement mediation analysis. This method provides more robust statical power and accurate Type I error rates. The standardized values for DAS, family environment, school environment and internet addiction scores were used for the mediation analysis. It is also worth noting that typical mediation analysis means that changes in the predictor, DASS components, lead to changes in the mediator, family, or school environment, which in turns leads to changes in the outcome, IA. However, in our specific research context, we are employing an approach known as exploratory mediation analysis [ 58 ] where the mediator explains the relation between the predictor and the outcome without implying causality and does not vary with changes in the predictor. The mediator in this analysis is used to better understand and describe the relations between the predictor and outcome without establishing any causality. For instance, in the case of school environment, adolescents may resort to using the Internet excessively if the environment is not supportive. On the other hand, a supportive environment may help them utilize better coping strategies. Statistical significance for this study was accepted at p < .05.
The final sample had 407 participants with the mean age of 13.2 years (SD = 1.24). The sample consisted of 330 (81.1%) females and 77 (18.9%) males. Two of the schools that highly responded to the survey were predominantly female schools. The sample also included 250 early adolescents (10–13 years old) and 157 middle adolescents (14–17 years old). Of the middle adolescents, only four participants were aged 17 years.
Descriptive statistics
Table 1 summarizes the descriptive statistics of the sample for this study. The participants were all residents of Qatar. The sample included 75.2% Arabs, 16.5% from Eastern backgrounds, and 8.3% from Western backgrounds. Additionally, the sample comprised 70% non-Qataris and 30% Qataris.
Factor analysis of school environment
Exploratory factor analysis on the sample resulted in the grouping of the three items into a single variable of school environment. We measured the Kaiser-Meyer-Olkin (KMO) to measure the sample adequacy for factor analysis. The overall KMO measure was 0.66 with individual KMO measures between the range of 0.64 and 0.71. As per [ 59 ], the KMO measures fall into the categories of ‘mediocre’ to ‘middling’. Bartlett’s test of sphericity was statistically significant ( p < .001), indicating that the variables are unrelated and suitable for factor analysis.
The factor analysis resulted in one component which accounted for 44% of the variance. The resulting scree plot also aligned with the one-factor solution. This one factor was interpreted as representing the school environment. Table 2 presents the component loadings and uniqueness of the factor. In addition, the derived school environment variable was calculated by taking the average of the individual items.
Correlation between sample variables for early and middle adolescents
As shown in Tables 3 and 4 , all variables are correlated in the analysis for early and middle adolescents respectively.
Mediation analysis of family environment in early and middle adolescents
The mediation analysis included stress, depression and anxiety as the independent variables, and IA as the dependent variable. The family environment variable was included as a potential mediator. The model met the assumptions of continuous variables, correlation between dependent, mediating, and independent variables, multicollinearity, and outliers [ 60 ].
The mediation model of stress as independent variable, family environment as mediator and IA as dependent variable showed a significant total effect of stress on IA (β = 0.51, SE = 0.054, p < .001). The direct effect was also significant (β = 0.43, SE = 0.061, p < .001). Additionally, the indirect effect of family environment was significant (β = 0.085, SE = 0.031, p = .007). These findings indicate that family environment partially mediated the effect of stress on IA for early adolescents (see Fig. 1 ).
For middle adolescents, the mediation model showed a significant total effect of stress on IA (β = 0.46, SE = 0.073, p < .001). The direct effect was also significant (β = 0.28, SE = 0.080, p < .001). Additionally, the indirect effect of family environment was significant (β = 0.18, SE = 0.047, p < .001). These findings indicate that family environment partially mediated the effect of stress on IA for middle adolescents as shown in Fig. 1 .
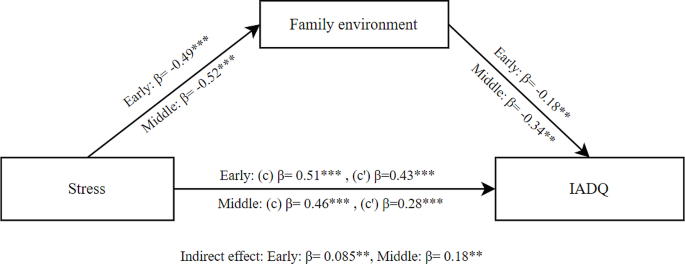
Mediation model between stress and IADQ through family environment for early and middle adolescents; (c) Total effect, (c’) Direct effect; * p < .05; ** p < .01; *** p < .001
The mediation results for depression as independent variable, family environment as mediator and IA as dependent variable showed a significant total effect of depression on IA (β = 0.50, SE = 0.054, p < .001) in early adolescents. The direct effect was also significant (β = 0.41, SE = 0.061, p < .001). Additionally, the indirect effect of family environment was significant (β = 0.089, SE = 0.031, p = .004). These findings indicate that family environment partially mediated the effect of depression on IA for early adolescents as shown in Fig. 2 .
For middle adolescents, the mediation results showed a significant total effect of depression on IA (β = 0.42, SE = 0.069, p < .001). The direct effect was also significant (β = 0.24, SE = 0.079, p = .003). Additionally, the indirect effect of family environment was significant (β = 0.18, SE = 0.049, p < .001). These findings indicate that family environment partially mediated the effect of depression on IA for middle adolescents (see Fig. 2 ).
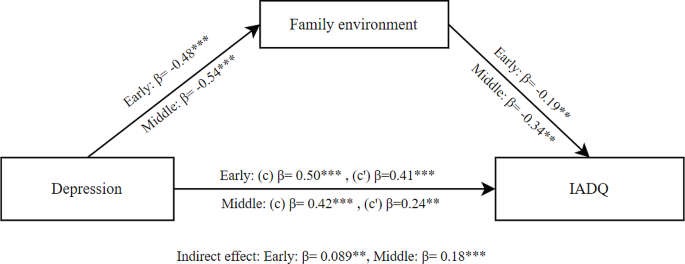
Mediation model between depression and IADQ through family environment for early and middle adolescents; (c) Total effect, (c’) Direct effect; * p < .05; ** p < .01; *** p < .001
The mediation results for anxiety as independent variable, family environment as mediator and IA as dependent variable showed a significant total effect of anxiety on IA (β = 0.49, SE = 0.055, p < .001) in early adolescents. The direct effect was also significant (β = 0.40, SE = 0.058, p < .001). Additionally, the indirect effect of family environment was significant (β = 0.089, SE = 0.026, p < .001). These findings indicate that family environment partially mediated the effect of anxiety on IA for early adolescents as shown in Fig. 3 .
For middle adolescents, the mediation results also showed a significant total effect of anxiety on IA (β = 0.32, SE = 0.075, p < .001). However, the direct effect was not significant (β = 0.14, SE = 0.076, p = .063). The indirect effect of family environment was significant (β = 0.17, SE = 0.044, p < .001). These findings indicate that family environment fully mediated the effect of anxiety on IA for middle adolescents as shown in Fig. 3 .
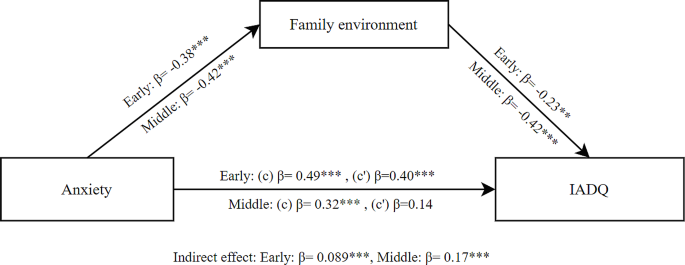
Mediation model between anxiety and IADQ through family environment for early and middle adolescents; (c) Total effect, (c’) Direct effect; * p < .05; ** p < .01; *** p < .001
Mediation analysis of school environment in early and middle adolescents
The mediation analysis included stress, depression and anxiety as the independent variables, and IA as the dependent variable. The school environment variable was included as a potential mediator. The model met the assumptions of continuous variables, correlation between dependent, mediating, and independent variables, multicollinearity, and outliers.
The mediation model of stress as independent variable, school environment as mediator and IA as dependent variable showed a significant total effect of stress on IA (β = 0.51, SE = 0.054, p < .001) in early adolescents. The direct effect was also significant (β = 0.45, SE = 0.061, p < .001). We also found the indirect effect of school environment was significant (β = 0.062, SE = 0.030, p = .040). These findings indicate that school environment partially mediated the effect of stress on IA for early adolescents as shown in Fig. 4 .
For middle adolescents, the mediation model showed a significant total effect of stress on IA (β = 0.46, SE = 0.073, p < .001). The direct effect was also significant (β = 0.39, SE = 0.080, p < .001). However, the indirect effect of school environment was not significant (β = 0.069, SE = 0.037, p = .065). These findings indicate that school environment did not mediate the effect of stress on IA for middle adolescents.

Mediation model between stress and IADQ through school environment for early and middle adolescents; (c) Total effect, (c’) Direct effect; * p < .05; ** p < .01; *** p < .001
The mediation results for depression as independent variable, school environment as mediator and IA as dependent variable showed a significant total effect of depression on IA (β = 0.50, SE = 0.054, p < .001) in early adolescents. The direct effect was also significant (β = 0.43, SE = 0.061, p < .001). Additionally, the indirect effect of school environment was significant (β = 0.066, SE = 0.031, p =.033). These findings indicate that school environment partially mediated the effect of depression on IA for early adolescents as shown in Fig. 5 .
The mediation results for middle adolescents showed a significant total effect of depression on IA (β = 0.42, SE = 0.069, p < .001). The direct effect was also significant (β = 0.35, SE = 0.079, p < .001). However, the indirect effect of the school environment was not significant (β = 0.066, SE = 0.040, p =.094). These findings indicate that school environment did not mediate the effect of depression on IA for middle adolescents.
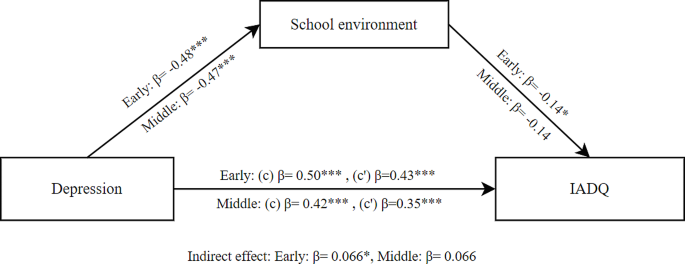
Mediation model between depression and IADQ through school environment for early and middle adolescents; (c) Total effect, (c’) Direct effect; * p < .05; ** p < .01; *** p < .001
The mediation results for anxiety as independent variable, school environment as mediator and IA as dependent variable showed a significant total effect of anxiety on IA (β = 0.49, SE = 0.055, p < .001) in early adolescents. The direct effect was also significant (β = 0.42, SE = 0.060, p < .001). Additionally, the indirect effect of school environment was significant (β = 0.073, SE = 0.027, p =.007). These findings indicate that school environment partially mediated the effect of anxiety on IA for early adolescents as shown in Fig. 6 .
The mediation results for middle adolescents showed a significant total effect of anxiety on IA (β = 0.32, SE = 0.075, p < .001). The direct effect was also significant (β = 0.22, SE = 0.082, p =.009). Additionally, the indirect effect of school environment was significant (β = 0.099, SE = 0.040, p =.013). These findings indicate that school environment partially mediated the effect of anxiety on IA for middle adolescents as shown in Fig. 6 .
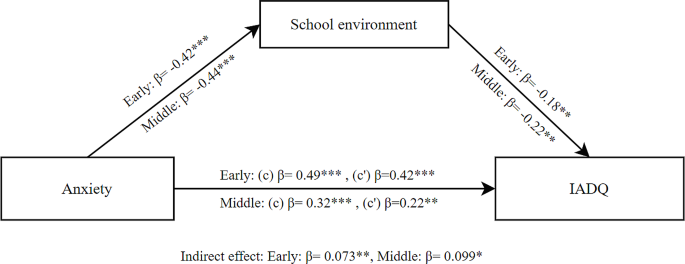
Mediation model between anxiety and IADQ through school environment for early and middle adolescents; (c) Total effect, (c’) Direct effect; * p < .05; ** p < .01; *** p < .001
This study explored the underlying role of family and school environment in the relationship between depression, stress, and anxiety and IA in early and middle adolescents. The main findings of this study are threefold. First, family environment mediates the relationship between DAS and IA in early and middle adolescents. Second, school environment partially mediates the relationship between DAS and IA in early adolescents. Third, school environment partially mediates the relationship between anxiety and IA in middle adolescents but does not mediate the relationship between depression and IA and between stress and IA.
In line with our first hypothesis, we observed an indirect effect of DAS on adolescent IA through the family environment in both early and middle adolescents. This implies the significant role of family environment in prevention and intervention efforts for adolescent IA. Further, our findings revealed that family environment fully mediates the relationship between anxiety and IA in middle adolescents, indicating that anxiety does not directly impact IA but rather affects it indirectly through the family environment. These results suggest that family dynamics can influence adolescents’ susceptibility to DAS and subsequent engagement in IA.
Our findings align with the Bronfenbrenner model [ 32 ] suggesting that being in a negative family environment can lead to adolescents looking for alternative sources of emotional support and developing maladaptive coping mechanisms such as IA. Adolescents living in a healthy environment rely on their parents for emotional support, reducing the need for maladaptive coping strategies. The attachment theory proposed by Bowlby [ 33 ] also supports this idea, as it suggests that healthy parental attachments foster the development of healthy coping skills in adolescents. Wang et al. [ 61 ] reported that good parent-adolescent relationship was positively related with adolescents’ emotion regulation ability, which in turn was negatively related with IA. Conversely, living in a dysfunctional family environment may lead to an impaired sense of security, increasing the risk of psychological and behavioral problems [ 20 ]. Factors like parental conflict, family discord, and lack of communication may magnify the impact of DAS on adolescents, potentially driving them towards excessive internet use as a means of escape, and ultimately contributing to the development of IA. This behavior is commonly seen in other addictions as well for example, a study conducted in Qatar found a bidirectional relationship between family relationships and adolescent substance addiction that is adolescents living in dysfunctional family environment may resort to substance addiction which may then further negatively impact the family environment [ 62 ].
Our findings partly support our second hypothesis indicating that the school environment partially mediated the relationship between DAS and IA in early adolescents. However, for middle adolescents, the school environment only partially mediated the relationship between anxiety, without showing significant effects on depression and stress with IA. These findings emphasize the nuanced role of the school environment during different developmental stages in adolescence.
During early adolescence, students undergo significant academic transitions, moving from primary to middle school [ 63 ]. This transition along with the increased hormonal changes and social pressures may impact the mental health struggles of early adolescents. They may be more susceptible to external stressors such as academic pressure and schoolwork difficulties. Furthermore, early adolescents disengaged from school and experiencing negative school feelings, such as a lack of belonging and support, are at a higher risk for psychological distress and involvement in risky behaviors [ 64 ]. A survey carried out by Oberle [ 65 ] revealed a direct relation between a supportive classroom environment and the emotional well-being of early adolescents. The connection was also influenced indirectly through positive social interactions and self-perception. Early adolescents also lack effective coping skills as they are less trained in evaluating circumstances and formulating effective approaches to manage [ 66 ]. This lack of coping skills may make them susceptible to maladaptive behavioral patterns. These findings also align with the Bronfenbrenner model [ 32 ] for school environment suggesting that having a school environment that lacks effective support may further reinforce adolescents’ feelings of inadequacy and failure, thus driving them towards seeking relief through the internet and adopt dysfunctional coping mechanisms, one of the symptoms of the IADQ scale. As such, the school environment may either alleviate or aggravate their psychological distress.
On the other hand, middle adolescents show a different pattern. While the school environment still plays a role in mediating anxiety and IA, they have better coping skills and a stronger sense of emotional competence [ 66 ]. Having already adjusted to their school environment, they may experience less negative school-related feelings compared to early adolescents. Conversely, middle adolescents encounter a more demanding and competitive learning environment compared to early adolescents. Middle adolescents are confronted with elevated parental expectations and heightened academic stress, factors that can significantly influence their level of academic involvement [ 67 ]. Simultaneously, these middle adolescents may also grapple with anxiety stemming from the increased pressure to excel academically as they move from high school to college.
Our results also showed that family and school environment were both negatively related with DASS and IA for both early and middle adolescents. This suggests that a positive and supportive family and school environment is related to lower levels of IA and DAS in adolescents. These results align with previous literature on family and school environment with IA where a negative family and school environment were reported as possible risk factors for adolescent IA [ 1 ]. A study on depression and anxiety also found family dysfunction positively predicted depression and anxiety in adolescents [ 35 ]. Further, a systematic literature review reported that school environment is related to adolescent mental health [ 68 ]. Our results further reinforce the existing body of literature highlighting the impact of family and school environments.
With Qatar having one of the highest internet penetration rates in the world at 99% [ 48 ], the culture of convenience in addition to the hot weather during most of the year, leads to people spending most of their indoors. Sedentary behavior in adolescents is also associated with negative psychosocial factors of depression, stress, and anxiety [ 69 ]. A study by Al-Kaabi et al. [ 70 ] found that almost 34% of Qatari adolescents in secondary schools reported experiencing symptoms of depression. Their results also showed that relationships with family, peers and teachers were significantly related to symptoms of depression. Furthermore, while the majority of Qatar’s population is immigrants, the family-wise cultural differences in family structure and norms between Qataris and other Arab countries is relatively low, and our sample comprised of approximately 75% Arab population (including Qataris). The Arab cultures holds hierarchical family atmosphere where parents and elderly in general are respected and seen as a source of authority and point of reference [ 71 ]. These cultural differences may impact the coping strategies adolescents adopt and the level of emotional support available to them in the familial context. Further research is needed to understand the impact the hierarchical family structure may have on mitigating the impact of DAS on IA in adolescents. We also note that the parent’s marital life and support of domestic helps may impact the results however due to sensitivity issues these questions were avoided. Regardless, we have measured the school environment which is based on the UNICEF scale that accounts for the global conditions of family environment and school environment and family environment through the BFRS scale which was validated for Arab population.
Our study is subject to certain limitations that need to be considered when interpreting the findings. Although mediation analysis typically establishes causal relations and is based on a longitudinal research design, our research design adopts a cross-sectional approach, making the establishment of causal relations impossible. Furthermore, we are employing exploratory mediation analysis where the mediator explains the relation between the predictor and the outcome without implying causality and does not vary with changes in the predictor. Additionally, the reliance on self-reported data introduces potential biases that could impact the accuracy of the outcomes. For instance, there is a possibility of recall bias influencing participants’ recollection and reporting of their online activities. A relevant study conducted by Zurbriggen et al. [ 72 ] revealed that early adolescents tend to overestimate positive affect, whereas middle adolescents tend to overestimate negative affect when recalling emotional experiences. Another significant source of potential bias is social desirability, wherein respondents might feel inclined to provide socially acceptable responses rather than completely accurate ones. This phenomenon might have affected the accuracy of participants’ reporting, particularly in relation to aspects such as internet addiction and psychological distress. Moreover, it is important to note that our data collection took place during exam periods, which led to a limited number of schools willing to participate. In addition, we received majority of responses from two girls’ schools resulting in approximately 80% female participants. This limited our ability to draw conclusions about potential gender-based differences in adolescents’ internet addiction. While there is limited research on how family and school environment explain the relationship between DAS and adolescent IA, our results should be interpreted with caution when it comes to gender related differences and be seen closer to females than males given the approximately 80% female population. Our sample is also not nationally representative due to certain logistical limitation of administering the survey again in other times of the year as it could lead to bias due to the time of year, and academic calendars amongst other factors.
Despite these limitations, the results of our study have both theoretical and practical implications. From a theoretical perspective, the present study provides empirical evidence of the mediating effect of both family and school environment in the context of internet addiction. Furthermore, our study indicates the distinct impacts that both environments have on psychological distress and internet addiction among early and middle adolescents, particularly regarding anxiety. These findings contribute to the existing literature on adolescent internet addiction and emphasize the necessity of tailoring research to each phase of adolescence. From a practical perspective, our findings demonstrate that both family and school environments are crucial when dealing with adolescent Internet addiction. This corresponds with Bronfenbrenner’s socioecological model, which proposes that individuals are shaped by the immediate environments they inhabit and by the interactions occurring within and between these environments [ 32 ]. Abdelrahman et al. [ 73 ] reported that parents’ activities with their children and coping strategies were positively related to their children’s mental health in a sample from Qatar that is how parents handle their mental health impacts their children’s mental health as well. Evidence-based prevention and interventions strategies should be rooted in evidence and consider the unique influence of family and school settings, as well as the specific phase of adolescence. A study on the interaction between adolescent IA and family environment factors showed the need to train parents on effective prevention and intervention strategies for adolescent IA [ 39 ]. While the family environment bears importance for early and middle adolescents, our findings showed that school environment played a larger role in early adolescents compared to middle adolescents. A systematic literature review on prevention of IA revealed that effective prevention interventions should engage individuals who are integral to the formative environment of at-risk adolescents [ 74 ]. This highlights the collective responsibility of parents and schools in cultivating a healthy climate that aids adolescents in developing effective coping mechanisms, thereby mitigating the risk of internet addiction.
Our study did not find a mediating effect of school environment on the relationship between depression and IA or between stress and IA in middle adolescents. The family environment, however, did partially mediate the relationship between depression and stress and adolescent IA. This suggests that the influence of depression and stress on adolescent IA might operate through distinct underlying mechanisms. Future research could explore other potential mediator factors, such as environmental-level factors. For instance, a study by Chung et al. [ 13 ] indicated that factors like higher accessibility to PC cafes and Internet game advertising had a greater influence on adolescent internet addiction than family and school environment. Another study conducted in Qatar found time and mood management also impacted internet addiction in their sample [ 75 ]. It is also worth noting that this study was from the perspective of adolescents, future research may also include the parental and teacher perspectives to provide a comprehensive view of the relationship between DAS and IA. Our previous work in [ 39 ] and [ 40 ] shed light into the perspective of parents. We aim to be collecting data from the same household both from the adolescents and their parents to be able to compare perspectives and study how family environment and parent-child relation affect both views. Future research could also employ structural equation modeling to test and establish causal relationships among DAS, family environment, school environment, and adolescent IA. By contrasting different models and incorporating longitudinal and cross-cultural analyses, the study may provide a further nuanced understanding of the complex relationships involved. This would also help in guiding the development of targeted interventions for adolescent internet addiction and mental health. Literature on gender-based differences have no fixed consensus on gender differences in IA. Studies in literature have reported conflicting results with some reporting males as having higher IA levels than females [ 2 , 76 ] while others reporting females as having higher IA levels [ 77 , 78 ]. Some have even reported no differences amongst the two genders when it comes to IA [ 79 , 80 ]. Given that our sample was predominantly female, future studies could benefit from a larger and more balanced sample to investigate the role of gender in adolescent internet addiction. It is also worth noting that adolescents in Qatar can attend private or public schools. Public schools are funded and managed by the government in Qatar whereas private schools are funded by tuition fees and managed by private organizations. Public schools typically follow the Qatari curriculum. Private schools, on the other hand, offer various international curricula that are reviewed by the government. Public schools are generally attended by Qatari citizens. Expatriates are more likely to be enrolled in private schools than public. This is due to the language of instruction in public schools predominantly being Arabic and the access to free education for Qataris. Furthermore, socioeconomic status greatly impacts the literacy across the different school types [ 81 ] with higher fees of enrollment to private schools related to more selective curricula and education. While our current research had a sample predominantly from public schools, our future research could look into the impact of the school environment in the different school types on DAS and adolescents’ IA.
In conclusion, our study provides significant insights into the mediating role of family and school environments on the relationship between DAS and adolescent IA. The findings also highlight the influence of these environments across the two developmental stages of early and middle adolescence.
The family environment emerged as a significant mediator, fully mediating the relationship between DAS and IA. This underscores the importance of family dynamics in shaping adolescents’ susceptibility to psychological distress and subsequent engagement in maladaptive coping mechanisms, such as excessive internet use. Aligning with ecological models and attachment theory, our results suggest that a healthy family environment provides a crucial buffer against IA by fostering positive coping skills and emotional support.
The school environment, while playing a nuanced role, was found to partially mediate the relationship between DAS and IA, with variations between early and middle adolescents. Early adolescents, undergoing significant academic transitions, were more susceptible to negative school-related feelings, contributing to psychological distress and IA. In contrast, middle adolescents, equipped with better coping skills, faced heightened academic stress, revealing a more demanding learning environment.
Limitations
Despite the valuable insights gained, our study is not without limitations. The cross-sectional design restricts our ability to establish causal relationships, emphasizing the need for future longitudinal studies. The reliance on self-reported data introduces potential biases, including recall bias and social desirability. The predominantly female sample raises questions about gender-related differences, necessitating more balanced participant demographics in future research.
Additionally, our study took place during exam periods, limiting the number of participating schools and potentially influencing responses. The exclusion of certain sensitive questions, such as those related to parental martial life, may have left gaps in our understanding of the family environment’s full impact. Further research is needed to explore the cultural nuances of hierarchical family structures and their potential mitigating effects on the relationship between DAS and IA in adolescents.
Future research prospects
Looking ahead, future research could delve into additional mediator factors, such as environmental-level variables, to enhance our understanding of the complex dynamics at play. Employing structural equation modeling could help establish causal relationships among DAS, family environment, school environment, and adolescent IA. Exploring cross-cultural and longitudinal analyses would provide a more nuanced understanding of these relationships.
Furthermore, given the observed impact of school environments on IA, future studies could investigate the influence of different school types on psychological distress and IA among adolescents. A more balanced sample that includes both public and private school attendees would contribute to a more comprehensive understanding of the role of the school environment.
Implications
The study has both theoretical and practical implications. Theoretically, the study contributes to the existing literature by demonstrating the mediating effects of both family and school environments on the relationship between DAS and adolescent IA. The findings also emphasize the importance of tailoring interventions to each adolescence phase. Practically, the study highlights the collective responsibility of parents and schools in addressing adolescent IA. Evidence-based prevention and intervention strategies should consider the influence of family and school settings. Engaging parents in effective prevention strategies and fostering a supportive school environment are crucial components of mitigating internet addiction risks.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Abbreviations
Internet Addiction
Internet Addiction Diagnostic Questionnaire
Western, Educated, Industrialized, Rich, Democratic
Depression, Anxiety, and Stress Scale
Brief Family Relationship Scale
Kaiser-Meyer-Olkin
Standard Error
Xin M, Xing J, Pengfei W, Houru L, Mengcheng W, Hong Z. Online activities, prevalence of internet addiction and risk factors related to family and school among adolescents in China. Addict Behav Rep. 2018;7:14–8.
PubMed Google Scholar
Chi X, Hong X, Chen X. Profiles and sociodemographic correlates of internet addiction in early adolescents in southern China. Addict Behav. 2020;106:106385.
Article PubMed Google Scholar
Kawabe K, Horiuchi F, Oka Y, Ueno SI. Association between Sleep Habits and Problems and Internet Addiction in Adolescents. Psychiatry Investig [Internet]. 2019 Aug 1 [cited 2023 Dec 12];16(8):581–7. Available from: http://www.psychiatryinvestigation.org/journal/view.php?doi=10.30773/pi .2019.03.21.2.
Bener A, Yildirim E, Torun P, Çatan F, Bolat E, Alıç S et al. Internet Addiction, Fatigue, and Sleep Problems Among Adolescent Students: a Large-Scale Study. Int J Ment Health Addict [Internet]. 2019 Aug 15 [cited 2022 Mar 9];17(4):959–69. Available from: https://link.springer.com/article/ https://doi.org/10.1007/s11469-018-9937-1 .
Kuss DJ, Lopez-Fernandez O. Internet addiction and problematic Internet use: A systematic review of clinical research. World J Psychiatry [Internet]. 2016 [cited 2022 Feb 2];6(1):143. Available from: /pmc/articles/PMC4804263/.
Poznyak V. Inclusion of gaming disorder in ICD-11. World Health Organization [Internet]. 2018 Sep 14 [cited 2022 Apr 9]; Available from: https://www.who.int/news/item/14-09-2018-inclusion-of-gaming-disorder-in-icd-11 .
Musetti A, Cattivelli R, Giacobbi M, Zuglian P, Ceccarini M, Capelli F et al. Challenges in internet addiction disorder: Is a diagnosis feasible or not? Front Psychol. 2016;7(JUN):177995.
Young KS. Internet Addiction: The Emergence of a New Clinical Disorder. CyberPsychology & Behavior [Internet]. 1998 [cited 2022 Jan 29];1(3):237–44. Available from: https://www.liebertpub.com/doi/abs/ https://doi.org/10.1089/cpb.1998.1.237 .
Lai FTT, Kwan JLY. Socioeconomic influence on adolescent problematic internet use through school-related psychosocial factors and pattern of internet use. Comput Hum Behav. 2017;68:121–36.
Article Google Scholar
Baggio S, Starcevic V, Billieux J, King DL, Gainsbury SM, Eslick GD, et al. Testing the spectrum hypothesis of problematic online behaviors: a network analysis approach. Addict Behav. 2022;135:107451.
Fumero A, Marrero RJ, Voltes D, Peñate W. Personal and social factors involved in internet addiction among adolescents: a meta-analysis. Comput Hum Behav. 2018;86:387–400.
Zhao Q, Huang Y, Li C. Does adolescents’ Internet addiction trigger depressive symptoms and aggressive behavior, or vice versa? The moderating roles of peer relationships and gender. Comput Human Behav [Internet]. 2022 Apr 1 [cited 2022 Jan 29];129:107143. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0747563221004660 .
Chung S, Lee J, Lee HK, Personal, Factors. Internet Characteristics, and Environmental Factors Contributing to Adolescent Internet Addiction: A Public Health Perspective. International Journal of Environmental Research and Public Health 2019, Vol 16, Page 4635 [Internet]. 2019 Nov 21 [cited 2023 Aug 7];16(23):4635. Available from: https://www.mdpi.com/1660-4601/16/23/4635/htm .
Obeid S, Saade S, Haddad C, Sacre H, Khansa W, Al Hajj R et al. Internet Addiction among Lebanese Adolescents: The Role of Self-Esteem, Anger, Depression, Anxiety, Social Anxiety and Fear, Impulsivity, and Aggression - A Cross-Sectional Study. Journal of Nervous and Mental Disease [Internet]. 2019 Oct 1 [cited 2023 Dec 12];207(10):838–46. Available from: https://journals.lww.com/jonmd/fulltext/2019/10000/internet_addiction_among_lebanese_adolescents__the.5.aspx .
Pan PY, Yeh C, Bin. Internet addiction among adolescents may predict Self-Harm/Suicidal behavior: a prospective study. J Pediatr. 2018;197:262–7.
Olivier E, Morin AJS, Tardif-Grenier K, Archambault I, Dupéré V, Hébert C. Profiles of Anxious and Depressive Symptoms Among Adolescent Boys and Girls: Associations with Coping Strategies. J Youth Adolesc [Internet]. 2022 Mar 1 [cited 2023 Jul 8];51(3):570–84. Available from: https://link.springer.com/article/10.1007/s10964-022-01572-x .
Gao M, Teng Z, Wei Z, Jin K, Xiao J, Tang H, et al. Internet addiction among teenagers in a Chinese population: prevalence, risk factors, and its relationship with obsessive-compulsive symptoms. J Psychiatr Res. 2022;153:134–40.
Saikia AM, Das J, Barman P, Bharali MD. Internet Addiction and its Relationships with Depression, Anxiety, and Stress in Urban Adolescents of Kamrup District, Assam. J Family Community Med [Internet]. 2019 May 1 [cited 2023 Dec 12];26(2):108. Available from: /pmc/articles/PMC6515762/.
Feng Y, Ma Y, Zhong Q. The Relationship between adolescents’ stress and internet addiction: a mediated-moderation model. Front Psychol. 2019;10:483355.
Gao T, Meng X, Qin Z, Zhang H, Gao J, Kong Y, et al. Association between parental marital conflict and internet addiction: a moderated mediation analysis. J Affect Disord. 2018;240:27–32.
Bryant J, Zillmann D. Using television to alleviate boredom and stress: Selective exposure as a function of induced excitational states. Journal of Broadcasting [Internet]. 2009 May [cited 2023 Jul 8];28(1):1–20. Available from: https://www.tandfonline.com/doi/abs/10.1080/08838158409386511 .
Longstreet P, Brooks S, Gonzalez ES. Internet addiction: when the positive emotions are not so positive. Technol Soc. 2019;57:76–85.
Henrich J, Heine SJ, Norenzayan A. Most people are not WEIRD. Nature [Internet]. 2010 Jun 30 [cited 2023 Jul 8];466(7302):29–29. Available from: https://www.nature.com/articles/466029a .
Li J, Li D, Jia J, Li X, Wang Y, Li Y. Family functioning and internet addiction among adolescent males and females: a moderated mediation analysis. Child Youth Serv Rev. 2018;91:289–97.
Jun S, Choi E. Academic stress and internet addiction from general strain theory framework. Comput Hum Behav. 2015;49:282–7.
Lozano-Blasco R, Latorre-Martínez MP, Cortés-Pascual A. Screen addicts: a meta-analysis of internet addiction in adolescence. Child Youth Serv Rev. 2022;135:106373.
Musetti A, Starcevic V, Boursier V, Corsano P, Billieux J, Schimmenti A. Childhood emotional abuse and problematic social networking sites use in a sample of Italian adolescents: The mediating role of deficiencies in self-other differentiation and uncertain reflective functioning. J Clin Psychol [Internet]. 2021 Jul 1 [cited 2023 Dec 20];77(7):1666–84. Available from: https://onlinelibrary.wiley.com/doi/full/ https://doi.org/10.1002/jclp.23138 .
Blum RW, Astone NM, Decker MR, Mouli VC. A conceptual framework for early adolescence: A platform for research. Int J Adolesc Med Health [Internet]. 2014 Aug 1 [cited 2023 Jul 15];26(3):321–31. Available from: https://www.degruyter.com/document/doi/ https://doi.org/10.1515/ijamh-2013-0327/html .
Sawyer SM, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC et al. Adolescence: a foundation for future health. The Lancet [Internet]. 2012 Apr 28 [cited 2023 Jul 14];379(9826):1630–40. Available from: http://www.thelancet.com/article/S0140673612600725/fulltext .
Barrett DE. The Three Stages of Adolescence. The High School Journal [Internet]. 1996 Apr [cited 2023 Jul 15];79(4):333–9. Available from: https://www.jstor.org/stable/40364502 .
Imperato C, Mancini T, Musetti A. Exploring the Role of Problematic Social Network Site Use in the Link Between Reflective Functioning and Identity Processes in Adolescents. Int J Ment Health Addict [Internet]. 2023 Oct 1 [cited 2023 Dec 20];21(5):3430–45. Available from: https://link.springer.com/article/ https://doi.org/10.1007/s11469-022-00800-6 .
Bronfenbrenner U. The ecology of human development: experiments by nature and design. Harvard University Press; 1979.
Bowlby J. Attachment and Loss: Retrospect and Prospect. American Journal of Orthopsychiatry [Internet]. 1982 Oct 1 [cited 2023 Jul 8];52(4):664–78. Available from: https://onlinelibrary.wiley.com/doi/full/ https://doi.org/10.1111/j.1939-0025.1982.tb01456.x .
Kim HJ, Min JY, Min KB, Lee TJ, Yoo S. Relationship among family environment, self-control, friendship quality, and adolescents’ smartphone addiction in South Korea: Findings from nationwide data. PLoS One [Internet]. 2018 Feb 1 [cited 2023 Dec 12];13(2):e0190896. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0190896 .
Wang Y, Tian L, Guo L, Huebner ES. Family dysfunction and adolescents’ anxiety and depression: a multiple mediation model. J Appl Dev Psychol. 2020;66:101090.
Guo L, Tian L, Scott Huebner E. Family dysfunction and anxiety in adolescents: a moderated mediation model of self-esteem and perceived school stress. J Sch Psychol. 2018;69:16–27.
Yen JY, Yen CF, Chen CC, Chen SH, Ko CH. Family Factors of Internet Addiction and Substance Use Experience in Taiwanese Adolescents. Cyberpsychology and Behavior [Internet]. 2007 Jun 26 [cited 2023 Jul 15];10(3):323–9. Available from: https://www.liebertpub.com/doi/ https://doi.org/10.1089/cpb.2006.9948 .
Chen HC, Wang JY, Lin YL, Yang SY. Association of Internet Addiction with Family Functionality, Depression, Self-Efficacy and Self-Esteem among Early Adolescents. Int J Environ Res Public Health [Internet]. 2020 Dec 1 [cited 2023 Jul 15];17(23):1–13. Available from: https://pubmed.ncbi.nlm.nih.gov/33260988/ .
Aziz M, Erbad A, Brahim Belhaouari S, Abdelmoneium AO, Al-Harahsheh S, Bagdady A et al. The interplay between adolescents’ Internet addiction and family-related factors: three common patterns. Int J Adolesc Youth [Internet]. 2022 [cited 2022 Oct 6];27(1):418–31. Available from: https://www.tandfonline.com/doi/abs/ https://doi.org/10.1080/02673843.2022.2115307 .
Chemnad K, Alshakhsi S, Al-Harahsheh S, Abdelmoneium AO, Al-Khalaf MS, Baghdady A et al. Is it Contagious? Does Parents’ Internet Addiction Impact Their Adolescents’ Internet Addiction? Soc Sci Comput Rev [Internet]. 2022 Aug 5 [cited 2022 Oct 6]; Available from: https://journals.sagepub.com/doi/abs/ https://doi.org/10.1177/08944393221117408 .
Cavioni V, Grazzani I, Ornaghi V, Agliati A, Pepe A, Adolescents. ’ Mental Health at School: The Mediating Role of Life Satisfaction. Front Psychol [Internet]. 2021 Aug 18 [cited 2023 Jul 16];12. Available from: /pmc/articles/PMC8416350/.
Fröjd SA, Nissinen ES, Pelkonen MUI, Marttunen MJ, Koivisto AM, Kaltiala-Heino R. Depression and school performance in middle adolescent boys and girls. J Adolesc. 2008;31(4):485–98.
Ogilvie S, Head S, Parekh S, Heintzman J, Preyde M. Association of School Engagement, Academic Difficulties and School Avoidance with Psychological Difficulties Among Adolescents Admitted to a Psychiatric Inpatient Unit. Child and Adolescent Social Work Journal [Internet]. 2019 Aug 15 [cited 2023 Jul 15];36(4):419–27. Available from: https://link.springer.com/article/ https://doi.org/10.1007/s10560-018-0570-4 .
Chemnad K, Aziz M, Abdelmoneium AO, Al-Harahsheh S, Baghdady A, Al Motawaa FY et al. Adolescents’ Internet addiction: Does it all begin with their environment? Child Adolesc Psychiatry Ment Health [Internet]. 2023 Dec 1 [cited 2023 Jul 16];17(1):1–14. Available from: https://capmh.biomedcentral.com/articles/ https://doi.org/10.1186/s13034-023-00626-7 .
Zhai B, Li D, Li X, Liu Y, Zhang J, Sun W, et al. Perceived school climate and problematic internet use among adolescents: mediating roles of school belonging and depressive symptoms. Addict Behav. 2020;110:106501.
Badenes-Ribera L, Fabris MA, Gastaldi FGM, Prino LE, Longobardi C. Parent and peer attachment as predictors of facebook addiction symptoms in different developmental stages (early adolescents and adolescents). Addict Behav. 2019;95:226–32.
Vaterlaus JM, Aylward A, Tarabochia D, Martin JD. A smartphone made my life easier: an exploratory study on age of adolescent smartphone acquisition and well-being. Comput Hum Behav. 2021;114:106563.
Kemp S, Digital. 2022: Qatar — DataReportal– Global Digital Insights [Internet]. 2022 [cited 2022 Dec 24]. Available from: https://datareportal.com/reports/digital-2022-qatar .
Brislin RW. Back-translation for cross-cultural research. J Cross Cult Psychol. 1970;1(3):185–216.
Young K. Internet Addiction Test (IAT) [Internet]. Bkp. Stoelting; 2015 [cited 2022 Feb 2]. 1–5 p. Available from: https://books.google.com/books/about/Internet_Addiction_Test_IAT.html?id=vaRaDwAAQBAJ .
Lovibond SH, Lovibond PF. Manual for the Depression Anxiety & Stress Scales [Internet]. 2nd ed. Psychology Foundation of Australia; 1995. Available from: https://www.worldcat.org/title/Manual-for-the-depression-anxiety-stress-scales/oclc/222009504 .
Antony MM, Cox BJ, Enns MW, Bieling PJ, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression anxiety stress scales in clinical groups and a community sample. Psychol Assess. 1998;10(2):176–81.
Ursachi G, Horodnic IA, Zait A. How Reliable are Measurement Scales? External factors with indirect influence on reliability estimators. Procedia Econ Finance. 2015;20:679–86.
Fok CCT, Allen J, Henry D, Team PA. The Brief Family Relationship Scale: A Brief Measure of the Relationship Dimension in Family Functioning. Assessment [Internet]. 2014 Feb [cited 2023 Aug 13];21(1):67. Available from: /pmc/articles/PMC3292682/.
Currie C, Inchley J, Molcho M, Lenzi M, Veselska Z. Health behaviour in school-aged children (HBSC) study protocol: background, methodology and mandatory items for the 2013/14 survey [Internet]. 2014 [cited 2023 Jul 8]. Available from: https://researchonline.gcu.ac.uk/en/publications/health-behaviour-in-school-aged-children-hbsc-study-protocol-back .
JASP. JASP. [cited 2021 Nov 29]. JASP - A Fresh Way to Do Statistics. Available from: https://jasp-stats.org/ .
MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods [Internet]. 2002 [cited 2023 Nov 3];7(1):83–104. Available from: https://pubmed.ncbi.nlm.nih.gov/11928892/ .
van Kesteren EJ, Oberski DL. Exploratory Mediation Analysis with Many Potential Mediators. Struct Equ Modeling [Internet]. 2019 Sep 3 [cited 2023 Nov 4];26(5):710–23. Available from: https://www.tandfonline.com/doi/abs/ https://doi.org/10.1080/10705511.2019.1588124 .
Kaiser HF. An index of factorial simplicity. Psychometrika [Internet]. 1974 Mar [cited 2023 Jul 8];39(1):31–6. Available from: https://link-springer-com.eres.qnl.qa/article/10.1007/BF02291575 .
Fein EC, Gilmour J, Machin T, Hendry L. Statistics for Research Students: An Open Access Resource with Self-Tests and Illustrative Examples [Internet]. University of Southern Queensland; 2022 [cited 2023 Jul 8]. 1–101 p. Available from: https://open.umn.edu/opentextbooks/textbooks/1191 .
Wang W, Li D, Li X, Wang Y, Sun W, Zhao L, et al. Parent-adolescent relationship and adolescent internet addiction: a moderated mediation model. Addict Behav. 2018;84:171–7.
Hamza EGA, Gladding S, Moustafa AA. The Impact of Adolescent Substance Abuse on Family Quality of Life, Marital Satisfaction, and Mental Health in Qatar. Family Journal [Internet]. 2022 Jan 1 [cited 2023 Oct 31];30(1):85–90. Available from: https://journals.sagepub.com/doi/ https://doi.org/10.1177/10664807211000720 .
Chung H, Elias M, Schneider K. Patterns of Individual Adjustment Changes during Middle School Transition. J Sch Psychol. 1998;36(1):83–101.
McLaughlin C, Clarke B. Relational matters: a review of the impact of school experience on mental health in early adolescence. Educational Child Psychol. 2010;27(1):91–103.
Oberle E. Early Adolescents’ Emotional Well-Being in the Classroom: The Role of Personal and Contextual Assets. Journal of School Health [Internet]. 2018 Feb 1 [cited 2023 Aug 5];88(2):101–11. Available from: https://onlinelibrary.wiley.com/doi/full/ https://doi.org/10.1111/josh.12585 .
Williams K, Lisi AMG, De. Coping strategies in adolescents. J Appl Dev Psychol. 1999;20(4):537–49.
Liu S, Zou S, Zhang D, Wang X, Wu X. Problematic internet use and academic engagement during the COVID-19 lockdown: the indirect effects of depression, anxiety, and insomnia in early, middle, and late adolescence. J Affect Disord. 2022;309:9–18.
Article PubMed PubMed Central Google Scholar
Aldridge JM, McChesney K. The relationships between school climate and adolescent mental health and wellbeing: a systematic literature review. Int J Educ Res. 2018;88:121–45.
Saller FVI, Khaled SM. Potential psychosocial influences on gender differences in physical activity among Qatari adolescents: a first insight through descriptive observation. Int J Adolesc Youth [Internet]. 2019 Apr 3 [cited 2023 Oct 31];24(2):234–51. Available from: https://www.tandfonline.com/doi/abs/ https://doi.org/10.1080/02673843.2018.1515087 .
Al-Kaabi N, Selim NAA, Singh R, Almudahka H, Salem M. Prevalence and Determinants of Depression among Qatari Adolescents in Secondary Schools. Fam Med Med Sci Res [Internet]. 2017 [cited 2023 Oct 31];6(3):1–8. Available from: https://www.longdom.org/open-access/prevalence-and-determinants-of-depression-among-qatari-adolescents-in-secondary-schools-16729.html .
Al-Khani AM, Saquib J, Rajab AM, Khalifa MA, Almazrou A, Saquib N. Internet addiction in Gulf countries: A systematic review and meta-analysis. J Behav Addict [Internet]. 2021 Sep 6 [cited 2023 Sep 14];10(3):601–10. Available from: https://akjournals.com/view/journals/2006/10/3/article-p601.xml .
Zurbriggen CLA, Jendryczko D, Nussbeck FW. Rosy or blue? Change in Recall Bias of Students’ affective experiences during early adolescence. Emotion. 2021;21(8):1637–49.
Abdelrahman M, Al-Adwan D, Hasan Y. Impact of Social Distancing on the Mental Health of Parents and Children in Qatar. Int J Ment Health Addict [Internet]. 2022 Oct 1 [cited 2023 Oct 31];20(5):2894–905. Available from: https://link.springer.com/article/ https://doi.org/10.1007/s11469-021-00555-6 .
Vondráčková P, Gabrhelík R. Prevention of Internet addiction: A systematic review. J Behav Addict [Internet]. 2016 Dec 20 [cited 2023 Aug 13];5(4):568–79. Available from: https://akjournals.com/view/journals/2006/5/4/article-p568.xml .
Khan HU, Awan MA. Possible factors affecting internet addiction: a case study of higher education students of Qatar. Int J Bus Inf Syst. 2017;26(2):261–76.
Google Scholar
Mo PKH, Chan VWY, Wang X, Lau JTF. Gender difference in the association between internet addiction, self-esteem and academic aspirations among adolescents: a structural equation modelling. Comput Educ. 2020;155:103921.
Peris M, de la Barrera U, Schoeps K, Montoya-Castilla I. Psychological Risk Factors that Predict Social Networking and Internet Addiction in Adolescents. International Journal of Environmental Research and Public Health. 2020, Vol 17, Page 4598 [Internet]. 2020 Jun 26 [cited 2023 Aug 7];17(12):4598. Available from: https://www.mdpi.com/1660-4601/17/12/4598/htm .
Casaló LV, Escario JJ. Predictors of excessive internet use among adolescents in Spain: the relevance of the relationship between parents and their children. Comput Hum Behav. 2019;92:344–51.
Li Q, Dai W, Zhong Y, Wang L, Dai B, Liu X. The mediating role of coping styles on impulsivity, behavioral inhibition/approach system, and internet addiction in adolescents from a gender perspective. Front Psychol. 2019;10(OCT):476845.
Peterka-Bonetta J, Sindermann C, Elhai JD, Montag C. Personality associations with smartphone and internet use disorder: a comparison study including links to impulsivity and social anxiety. Front Public Health. 2019;7(JUN):453335.
Cheema JR. Public versus private schools in Qatar: Is there a literacy gap? http://dx.doi.org/107227/RIE0017 [Internet]. 2015 Jan 1 [cited 2023 Oct 31];95(1):5–18. Available from: https://journals.sagepub.com/doi/10.7227/RIE.0017 .
Download references
Acknowledgements
“Technology Overuse Amongst Adolescents in Qatar: current status, challenges, and recommendations for policy”, is a joint project between three members of Qatar Foundation for Education, Science and Community Development (QF), the Doha International Family Institute (DIFI), the World Innovation Summit for Education (WISE), and the Word Innovation Summit for Health (WISH). The statements made herein are solely the responsibility of the authors, and do not reflect statements/opinions of the institutes.
Open Access funding provided by the Qatar National Library. This publication was supported by NPRP 14 Cluster Grant # NPRP 14 C-0916-210015 from the Qatar National Research Fund (a member of Qatar Foundation). The findings herein reflect the work and are solely the responsibility of the authors.
Author information
Authors and affiliations.
College of Science and Engineering, Hamad Bin Khalifa University, Doha, Qatar
Maryam Aziz, Khansa Chemnad & Raian Ali
World Innovation Summit for Health, Qatar Foundation, Doha, Qatar
Sanaa Al-Harahsheh
Doha International Family Institute, Qatar Foundation, Doha, Qatar
Azza O. Abdelmoneium
World Innovation Summit for Education, Qatar Foundation, Doha, Qatar
Ahmed Baghdady
You can also search for this author in PubMed Google Scholar
Contributions
MA conceptualized the paper, prepared, and analyzed the data and wrote the first draft. KC helped with the data preparation and verified the statistical analysis. AA, SA, and AB participated in the study conceptualization and design and conducted the data collection. RA participated in all stages and supervised the research. All authors reviewed the paper and provided feedback on it. All authors approved the final version of the paper.
Corresponding authors
Correspondence to Maryam Aziz or Raian Ali .
Ethics declarations
Ethical approval and consent to participate.
The study was approved by the Institutional Review Board (IRB) of Hamad Bin Khalifa University (No. QBRI-IRB 2021-05-094) and school permissions were obtained to distribute the survey. The research was performed according to the guidelines stated in the Declaration of Helsinki. The parents and adolescents were informed beforehand of the study and their informed consent and assent were collected.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Aziz, M., Chemnad, K., Al-Harahsheh, S. et al. Depression, stress, and anxiety versus internet addiction in early and middle adolescent groups: the mediating roles of family and school environments. BMC Psychol 12 , 184 (2024). https://doi.org/10.1186/s40359-024-01659-z
Download citation
Received : 13 August 2023
Accepted : 13 March 2024
Published : 03 April 2024
DOI : https://doi.org/10.1186/s40359-024-01659-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescence
- Internet addiction
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
Depression in Adolescents
Affiliation.
- 1 From the Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine (L.M., J.V.C.), and the Kennedy Krieger Institute (J.V.C.) - both in Baltimore.
- PMID: 34320289
- DOI: 10.1056/NEJMra2033475
Publication types
- Antidepressive Agents / adverse effects
- Antidepressive Agents / therapeutic use*
- Depressive Disorder* / epidemiology
- Depressive Disorder* / etiology
- Depressive Disorder* / therapy
- Depressive Disorder, Major / diagnosis
- Psychotherapy*
- Selective Serotonin Reuptake Inhibitors / therapeutic use
- Suicide / psychology
- Antidepressive Agents
- Serotonin Uptake Inhibitors

- Weather
Search location by ZIP code
U.s. surgeon general visits central iowa, talks about mental health.
- Copy Link Copy {copyShortcut} to copy Link copied!

GET LOCAL BREAKING NEWS ALERTS
The latest breaking updates, delivered straight to your email inbox.
The U.S. Surgeon General visited central Iowa on Wednesday to speak about the rise in mental health issues.
Dr. Vivek Murthy was the keynote speaker for the 2024 Harkin on Wellness Symposium at Drake University. This year's event focused on mental health in children and young people, much of which he says is rooted in excessive social media use.
Adolescents using social media for three or more hours a day face double the risk of depression and anxiety symptoms, he said.
Murthy says he's calling on Congress to create safety standards to protect young people from harmful content. He's also encouraging schools to move toward phone-free learning to help students focus.
» Download the free KCCI app to get updates on the go: Apple | Google Play
Get the latest headlines from KCCI
Analysis of social media language using AI models predicts depression severity for white Americans, but not Black Americans
NIH-supported study also found Black people with depression used different language than white people to express their thoughts on Facebook

Researchers were able to predict depression severity for white people, but not for Black people using standard language-based computer models to analyze Facebook posts. Words and phrases associated with depression, such as first-person pronouns and negative emotion words, were around three times more predictive of depression severity for white people than for Black people. The study , published today in the Proceedings of the National Academy of Sciences , is co-authored by researchers at the University of Pennsylvania, Philadelphia, and the National Institute on Drug Abuse (NIDA), part of the National Institutes of Health (NIH), which also funded the study.
While previous research has indicated that social media language could provide useful information as part of mental health assessments, the findings from this study point to potential limitations in generalizing this practice by highlighting key demographic differences in language used by people with depression. The results also highlight the importance of including diverse pools of data to ensure accuracy as machine learning models, an application of artificial intelligence (AI) language models, are developed.
“As society explores the use of AI and other technologies to help deliver much-needed mental health care, we must ensure no one is left behind or misrepresented,” said Nora Volkow, M.D., NIDA director. “More diverse datasets are essential to ensure that healthcare disparities are not perpetuated by AI and that these new technologies can help tailor more effective health care interventions.”
The study, which recruited 868 consenting participants who identified themselves as Black or white, demonstrated that models trained on Facebook language used by white participants with self-reported depression showed strong predictive performance when tested on the white participants. However, when the same models were trained on Facebook language from Black participants, they performed poorly when tested on the Black participants, and showed only slightly better performance when tested on white participants.
While depression severity was associated with increased use of first-person singular pronouns (“I,” “me,” “my”) in white participants, this correlation was absent in Black participants. Additionally, white people used more language to describe feelings of belongingness (“weirdo,” “creep”), self-criticism (“mess,” “wreck”), being an anxious-outsider (“terrified,” “misunderstood”), self-deprecation (“worthless,” “crap”), and despair (“begging,” “hollow”) as depression severity increased, but there was no such correlation for Black people. For decades, clinicians have been aware of demographic differences in how people express depressive symptoms, and this study now demonstrates how this can play out in social media.
Language-based models hold promise as personalized, scalable, and affordable tools to screen for mental health disorders. For example, excessive self-referential language, such as the use of first-person pronouns, and negative emotions, such as self-deprecating language, are often regarded as clinical indicators of depression. However, there has been a notable absence of racial and ethnic consideration in assessing mental disorders through language, an exclusion that leads to inaccurate computer models. Despite evidence showing that demographic factors influence the language people use, previous studies have not systematically explored how race and ethnicity influence the relationship between depression and language expression.
Researchers set up this study to help bridge this gap. They analyzed past Facebook posts from Black and white people who self-reported depression severity through the Patient Health Questionnaire (PHQ-9) – a standard self-report tool used by clinicians to screen for possible depression. The participants consented to share their Facebook status updates. Participants were primarily female (76%) and ranged from 18 to 72 years old. The researchers matched Black and white participants on age and sex so that data from the two groups would be comparable.
The study’s findings challenge assumptions about the link between the use of certain words and depression, particularly among Black participants. Current clinical practices in mental health that have not accounted for racial and ethnic nuances may be less relevant, or even irrelevant, to populations historically excluded from mental health research, the researchers note. They also hypothesize that depression may not manifest in language in the same way for some Black people – for example, tone or speech rate, instead of word selection, may relate more to depression among this population.
“Our research represents a step forward in building more inclusive language models. We must make sure that AI models incorporate everyone's voice to make technology fair for everyone,” said Brenda Curtis, Ph.D., MsPH, chief of the Technology and Translational Research Unit in the Translational Addiction Medicine Branch at NIDA’s Intramural Research Program and one of the study’s senior authors. “Paying attention to the racial nuances in how mental health is expressed lets medical professionals better understand when an individual needs help and provide more personalized interventions.”
Future studies will need to examine differences across other races and demographic features, using various social media platforms, the authors say. They also caveat that social media language is not analogous to everyday language, so future work on language-based models must take this into account.
“It’s important to note that social media language and language-based AI models are not able to diagnose mental health disorders – nor are they replacements for psychologists or therapists – but they do show immense promise to aid in screening and informing personalized interventions,” said the study’s lead author, Sunny Rai, Ph.D., a postdoctoral researcher in Computer and Information Science at the University of Pennsylvania. “Many improvements are needed before we can integrate AI into research or clinical practice, and the use of diverse, representative data is one of the most critical.”
For more information on substance and mental health treatment programs in your area, call the free and confidential National Helpline 1-800-662-HELP (4357) or visit FindTreatment.gov . Anyone who needs assistance with the first steps in pursuing help can find guidance at FindSupport.gov .
If you or someone you know is in crisis and needs immediate help, call the 988 Suicide & Crisis Lifeline at 988. Learn more about suicide prevention and ways you can help someone who might be at risk for self-harm.
- S Rai, et al. Key Language Markers of Depression on Social Media Depend on Race . The Proceedings of the National Academy of Sciences . DOI: 10.1073/pnas.2319837121 (2024).
About the National Institute on Drug Abuse (NIDA): NIDA is a component of the National Institutes of Health, U.S. Department of Health and Human Services. NIDA supports most of the world’s research on the health aspects of drug use and addiction. The Institute carries out a large variety of programs to inform policy, improve practice, and advance addiction science. For more information about NIDA and its programs, visit www.nida.nih.gov .
About the National Institutes of Health (NIH): NIH, the nation’s medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
About substance use disorders: Substance use disorders are chronic, treatable conditions from which people can recover. In 2022, nearly 49 million people in the United States had at least one substance use disorder. Substance use disorders are defined in part by continued use of substances despite negative consequences. They are also relapsing conditions, in which periods of abstinence (not using substances) can be followed by a return to use. Stigma can make individuals with substance use disorders less likely to seek treatment. Using preferred language can help accurately report on substance use and addiction. View NIDA’s online guide .
NIH…Turning Discovery Into Health®
Related Articles

Law enforcement seizures of psilocybin mushrooms rose dramatically between 2017-2022

Reduced drug use is a meaningful treatment outcome for people with stimulant use disorders

Residential addiction treatment for adolescents is scarce and expensive
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Research Identifies Characteristics of Cities That Would Support Young People’s Mental Health
Survey responses from global panel that included young people provide insights into what would make cities mental health-friendly for youth
As cities around the world continue to draw young people for work, education, and social opportunities, a new study identifies characteristics that would support young urban dwellers’ mental health. The findings, based on survey responses from a global panel that included adolescents and young adults, provide a set of priorities that city planners can adopt to build urban environments that are safe, equitable, and inclusive.
To determine city characteristics that could bolster youth mental health, researchers administered an initial survey to a panel of more than 400, including young people and a multidisciplinary group of researchers, practitioners, and advocates. Through two subsequent surveys, participants prioritized six characteristics that would support young city dwellers’ mental health: opportunities to build life skills; age-friendly environments that accept young people’s feelings and values; free and safe public spaces where young people can connect; employment and job security; interventions that address the social determinants of health; and urban design with youth input and priorities in mind.
The paper was published online February 21 in Nature .
The study’s lead author is Pamela Collins, MD, MPH, chair of the Johns Hopkins Bloomberg School of Public Health’s Department of Mental Health. The study was conducted while Collins was on the faculty at the University of Washington. The paper was written by an international, interdisciplinary team, including citiesRISE, a global nonprofit that works to transform mental health policy and practice in cities, especially for young people.
Cities have long been a draw for young people. Research by UNICEF projects that cities will be home to 70 percent of the world’s children by 2050. Although urban environments influence a broad range of health outcomes, both positive and negative, their impacts manifest unequally. Mental disorders are the leading causes of disability among 10- to 24-year-olds globally. Exposure to urban inequality, violence, lack of green space, and fear of displacement disproportionately affects marginalized groups, increasing risk for poor mental health among urban youth.
“Right now, we are living with the largest population of adolescents in the world’s history, so this is an incredibly important group of people for global attention,” says Collins. “Investing in young people is an investment in their present well-being and future potential, and it’s an investment in the next generation—the children they will bear.”
Data collection for the study began in April 2020 at the start of the COVID-19 pandemic. To capture its possible impacts, researchers added an open-ended survey question asking panelists how the pandemic influenced their perceptions of youth mental health in cities. The panelists reported that the pandemic either shed new light on the inequality and uneven distribution of resources experienced by marginalized communities in urban areas, or confirmed their preconceptions of how social vulnerability exacerbates health outcomes.
For their study, the researchers recruited a panel of more than 400 individuals from 53 countries, including 327 young people ages 14 to 25, from a cross-section of fields, including education, advocacy, adolescent health, mental health and substance use, urban planning and development, data and technology, housing, and criminal justice. The researchers administered three sequential surveys to panelists beginning in April 2020 that asked panelists to identify elements of urban life that would support mental health for young people.
The top 37 characteristics were then grouped into six domains: intrapersonal, interpersonal, community, organizational, policy, and environment. Within these domains, panelists ranked characteristics based on immediacy of impact on youth mental health, ability to help youth thrive, and ease or feasibility of implementation.
Taken together, the characteristics identified in the study provide a comprehensive set of priorities that policymakers and urban planners can use as a guide to improve young city dwellers' mental health. Among them: Youth-focused mental health and educational services could support young people’s emotional development and self-efficacy. Investment in spaces that facilitate social connection may help alleviate young people’s experiences of isolation and support their need for healthy, trusting relationships. Creating employment opportunities and job security could undo the economic losses that young people and their families experienced during the pandemic and help cities retain residents after a COVID-era exodus from urban centers.
The findings suggest that creating a mental health-friendly city for young people requires investments across multiple interconnected sectors like transportation, housing, employment, health, and urban planning, with a central focus on social and economic equity. They also require urban planning policy approaches that commit to systemic and sustained collaboration, without magnifying existing privileges through initiatives like gentrification and developing green spaces at the expense of marginalized communities in need of affordable housing.
The authors say this framework underscores that responses by cities should include young people in the planning and design of interventions that directly impact their mental health and well-being.
“ Making cities mental health friendly for adolescents and young adults ” was co-authored by an international, interdisciplinary team of 31 researchers led by the University of Washington Consortium for Global Mental Health, Urban@UW, the University of Melbourne, and citiesRISE. Author funding is listed in the Acknowledgements section of the paper.
Related Content

Student Spotlight: Glendedora Dolce

Study Estimates Nearly 70 Percent of Children Under Six in Chicago May Be Exposed to Lead-Contaminated Tap Water

Hidden Food Insecurity: The Adolescents Who Aren’t Getting Enough to Eat

A Zero-Emissions Transition Would Save Kids’ Lives

Child Diarrhea Has a Cheap and Easy Fix—Why Isn’t It Reaching Patients?
- Open access
- Published: 02 October 2020
Depression in adolescence: a review
- Diogo Beirão ORCID: orcid.org/0000-0001-5612-8941 1 ,
- Helena Monte 1 ,
- Marta Amaral 1 ,
- Alice Longras 1 ,
- Carla Matos 1 , 2 &
- Francisca Villas-Boas 1
Middle East Current Psychiatry volume 27 , Article number: 50 ( 2020 ) Cite this article
48k Accesses
15 Citations
13 Altmetric
Metrics details
Depression is a common mental health disease, especially in mid to late adolescence that, due to its particularities, is a challenge and requires an effective diagnosis. Primary care providers are often the first line of contact for adolescents, being crucial in identifying and managing this pathology. Besides, several entities also recommend screening for depression on this period. Thus, the main purpose of this article is to review the scientific data regarding screening, diagnosis and management of depression in adolescence, mainly on primary care settings.
Comprehension of the pathogenesis of depression in adolescents is a challenging task, with both environmental and genetic factors being associated to its development. Although there are some screening tests and diagnostic criteria, its clinical manifestations are wide, making its diagnosis a huge challenge. Besides, it can be mistakenly diagnosed with other psychiatric disorders, making necessary to roll-out several differential diagnoses. Treatment options can include psychotherapy (cognitive behavioural therapy and interpersonal therapy) and/or pharmacotherapy (mainly fluoxetine), depending on severity, associated risk factors and available resources. In any case, treatment must include psychoeducation, supportive approach and family involvement. Preventive programs play an important role not only in reducing the prevalence of this condition but also in improving the health of populations.
Depression in adolescence is a relevant condition to the medical community, due to its uncertain clinical course and underdiagnosis worldwide. General practitioners can provide early identification, treatment initiation and referral to mental health specialists when necessary.
Adolescence is an important period in developing knowledge and skills, learning how to manage emotions and relationships and acquiring attributes and abilities for adulthood. Depression in adolescence is a common mental health disease with a prevalence of 4–5% in mid to late adolescence [ 1 ]. It is a major risk factor for suicide and can also lead to social and educational impairments. Consequently, identifying and treating this disorder is crucial.
General practitioners and primary care providers are frequently the first line of contact for adolescents in times of distress and can be crucial to identify mental health issues amongst these patients. They can facilitate early identification of depression, initiate treatment and refer the adolescents for mental health specialists [ 2 ]. It is vital to make a timely and accurate diagnosis of depression in adolescence and a correct differential diagnosis from other psychiatric disorders, due to the recurrent nature of this condition and its association with poor academic performance, functional impairment and problematic relationships with parents, siblings and peers. Furthermore, depression at this age is strongly related to suicidal ideation and attempts [ 2 ].
The US Preventive Services Task Force (USPSTF) recommends screening adolescents for depressive disorder by the General Practitioners [ 2 , 3 ]. Guidelines from the American Academy of Pediatrics (AAP) state that adolescent patients should be screened annually for depression in Primary Care with a formal self-report screening tool [ 4 ]. AAP recommends that Primary Care clinicians should evaluate for depression in those who screen positive on the screening tool, in those who present with any emotional problem as the chief complaint and in those in whom depression is highly suspected despite a negative screen result [ 4 ].
The present work consists of a review on the depression in the adolescent, summarizing data published in scientific papers in the last years, regarding the epidemiology of the disease, its pathogenesis and risk factors, screening and diagnosis tools and its management and treatment. Our research focused on research papers published between January 2010 and March 2020 in the area. Other research papers not included in this first search were included due to their interest and value to the subject. The keywords, used in different permutations and combinations, included the following: depression, adolescence, overview, pathophysiology, diagnosis and treatment.
Epidemiology
The prevalence of depression is significantly linked to age, being low in children (< 1%) and increasing throughout childhood and adolescence. Nevertheless, the prevalence of depression in adolescence varies significantly between studies and reports. A reported prevalence in Great Britain was 4%, whereas in the USA was 2.1% and in France was 11.0% [ 5 , 6 , 7 ]. Nevertheless, a systematic review from 2013 stated the life prevalence of depression varies from 1.1 to 14.6% [ 8 ].
A possible factor for the reported increase during adolescence is the set of social and biological changes characteristic of post-pubertal phase, such as enhanced social understanding and self-awareness, brain circuits changes involved in responses to reward and danger and increased reported stress levels [ 9 , 10 , 11 ].
Regarding differences between genders, while no significant differences are found in depression during childhood, depression during adolescence has a strong female preponderance, similar to adulthood [ 12 , 13 , 14 ]. This difference is still observed between distinct epidemiological and clinical samples and across various methods of assessment. As such, it is unlikely due to differences in help-seeking or reporting of symptoms and more closely tied to female hormonal changes, which suggests a direct link to hormone-brain relations [ 15 ].
Pathogenesis
Comprehension of the pathogenesis of depression in adolescents is a challenging task, due to its heterogeneous clinical presentation and diverse causes.
Putative risk factors, potentially modifiable during adolescence without professional intervention, are substance use (alcohol, cannabis and other illicit drugs, tobacco), diet and weight [ 16 ].
Alcohol use is known to have neurotoxic effects during this developmentally sensitive period. Cannabis and other illicit drugs can have an impact on serotonin and other neurotransmitters causing an increase in depressive symptoms. Furthermore, alcohol, cannabis and other illicit drug use have various deleterious social and academic consequences for the adolescent which could increase their risk for depression [ 16 ].
The relationship between tobacco use and depression is unclear. However, it has been proposed that this linkage may arise from the effects of nicotine on neurotransmitter activity in the brain, causing changes to neurotransmitter activity [ 17 ]. Overweight can have a negative impact on self-image which elevates the risk for depression. Moreover, depressed people may lead a less healthy lifestyle and suffer from deregulation in the stress response system, which may contribute to weight gain [ 16 ].
Association between depression and environmental factors, such as exposures to acute stressful events (personal injury, bereavement) and chronic adversity (maltreatment, family discord, bullying by peers, poverty, physical illness), has been subject of papers. Stressful life events seem more strongly associated with first onset rather than recurrence, and risk is considerably greater in girls and in adolescents who have multiple negative life events. The most important factors are chronic and severe relationship stressors [ 18 ]. A significant interaction was found between exposure to maternal threatening behaviours and deficits in emotional clarity in relation to depressive symptom severity [ 19 ].
Genetic factors can also play a very important role in the pathogenesis. Many reports suggest that a variant (5-HTTLPR) in the serotonin transporter gene might increase the risk of depression, but only in the presence of adverse life stressors or early maltreatment. The findings are less robust in adolescent boys than girls. This gene variant has also been reported to affect fear-related and danger-related brain circuitry, which is altered in depression. However, such findings seem to vary not only by genotype but also by age, sex, and severity of symptoms, and are also reliant on good quality measures of adversity and depression [ 18 , 20 ].
Two interrelated neural circuits and associated modulatory systems have been closely linked to risk for depression. One circuit connects the amygdala to the hippocampus and ventral expanses of the prefrontal cortex (PFC) and is linked to hypothalamic-pituitary-adrenal (HPA) axis activity. Disruption of this circuit links depression to stress-related enhancements in HPA-stress systems, such as higher than expected cortisol concentrations, and activity in the serotonergic system. Psychosocial stress, sex hormones and development have also been linked to changing activity in this circuit, with evidence that this circuit matures after adolescence. High concentrations of sex steroid receptors have been identified within this circuit and might provide a biological mechanism for why girls have higher risk of depression than boys. The other key circuit implicated in depression encompasses the striatum and its connection to both the PFC and ventral dopamine-based systems. Like the first circuit, this one also continues to mature through adolescence. Sex differences emerge in both circuits. Research into this reward circuit implies that reduced activity is linked with expression of and risk for depression. Reduced striatal and PFC activity during tasks involving rewards has been recorded both in individuals with major depression and in those with depressed parents. Both inherited factors and stress-related perturbations seem to contribute to these changes [ 18 , 21 ].
Temperament and character traits are also important factors in the pathogenesis of depression in adolescence. According to Cloninger, temperament is responsible for automatic and emotional responses to environmental stimuli and encompasses four dimensions: novelty seeking, exploratory activity, harm avoidance, reward dependence and persistence [ 22 ]. In contrast, character develops across the lifespan and is influenced by social and cultural experiences. Three dimensions are distinguished: self-directedness, cooperativeness and self-transcendence [ 23 ]. Studies showed that depressed patients present higher novelty seeking, harm avoidance and lower reward dependence, persistence, self-directedness and cooperativeness compared to healthy individuals [ 23 , 24 ].
Primary care providers are frequently the first contact during times of distress and can be crucial to identify mental health issues allowing for an earlier depression diagnosis, treatment and referral [ 2 ].
The symptoms can differ from the adult population. In comparison to it, adolescents tend to have more frequently somatic symptoms, anxiety, disruptive behaviour and personality disorders [ 25 ].
The fact that these symptoms are common in other disorders such as hypothyroidism, anaemia, sleep apnoea or other chronic diseases makes the diagnosis more challenging to establish in these subjects [ 26 ].
Screening tools
The screening of adolescents for depression is an essential tool for early detection of this disorder. USPSTF and AAP recommend the screening of adolescents in primary care settings [ 2 , 3 , 4 , 25 , 26 , 27 ].
The Beck Depression Inventory (BDI) and Patient Health Questionnaire for Adolescents (PHQ-A) are the most commonly used, outperforming other screening tools in the identification of major depressive disorder among adolescents [ 2 , 28 ].
Originally developed as a depression symptom rating scale for the adult population, BDI is widely used among adults and adolescents and mainly in research. It is a 21-item self-report measure of depressive symptoms, scored from “0” to “3”. Participants are asked to respond to each item based on their experiences within the past 2 weeks. The total score can range from 0 to 63, with higher scores meaning higher levels of depressive symptoms [ 29 ]. In primary care settings, an adapted version (BDI-PC) is often used, which consists of a 7-item self-report instrument, with a cut-off of 4 points for major depression [ 30 ]. Good performance has also been shown using BDI, with sensitivity ranging from 84 to 90% and specificity ranging from 81 to 86% [ 3 ].
The PHQ-A is the depression module of a 67-item questionnaire that can be used to screen for depression among adolescent primary care patients. Composed of 9 questions, it can be entirely self-administered by the patient and evaluates symptoms experienced in the 2 weeks prior. It measures functional impairment and inquiries about suicidal ideation and suicide attempts [ 31 ]. The PHQ-A study had the highest positive predictive value, as well as a sensitivity and specificity of 73% and 94%, respectively [ 3 ].
Diagnostic tools
Diagnosis of depression in adolescents is established through the criteria described in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [ 32 ]. The evaluation of patients should be made through interviews, alone and with the patient’s family and/or caregivers and should include an assessment of functional impairment in different domains and other existing psychiatric conditions [ 4 ].
DSM-5 establishes the diagnosis of major depressive disorder as a period of at least 2 weeks during which there is a depressed mood or the loss of interest or pleasure in nearly all activities, and, additionally, at least four additional symptoms from a list that includes changes in weight, sleep disturbances, changes in psychomotor activity, fatigue, feelings of worthlessness or guilt, impaired concentration or ability to make decisions, or suicidal ideation. Additionally, it states that, in adolescents, depressed mood can be replaced by irritability or crankiness, a sign that can be neglected during assessment or by caregivers. This presentation should be differentiated from a pattern of irritability when frustrated [ 33 ]. Children diagnosed with disruptive mood dysregulation disorder, a new diagnosis referring persistent irritability and frequent episodes of extreme behaviour, typically develop unipolar depressive or anxiety disorders as they mature into adolescence [ 32 ]. Clinical presentation differs between genders, with female adolescents reporting feelings of sadness, loneliness, irritability, pessimism, self-hatred and eating disorders, while males present with somatic complaints, reduced ability to think or concentrate, lacking decision making skills, restlessness and anhedonia [ 34 , 35 ].
The severity of depressive disorders can be based on symptom count or intensity, and/or level of impairment. Mild depression can be defined as 5 to 6 symptoms that are mild in severity, with mild impairment in functioning. Severe depression exists when a patient experiences all depressive symptoms listed in the DSM-5 or severe impairment in functioning and, also, with at least 5 criteria and a specific suicide plan, clear intent or recent suicide attempt, psychotic symptoms or family history of first-degree relatives with bipolar disorder. Moderate depression falls between these two categories [ 4 ].
Differential diagnosis
Despite its well-defined diagnostic criteria, depression during adolescence can often be misdiagnosed, with the main differential diagnoses being adjustment disorder, dysthymic disorder, bipolar disorder and schizophrenia. However, it is crucial to establish the correct diagnosis as different psychiatric disorders involve distinct treatment and prognosis.
Adjustment disorder is classified as depressed mood in response to an identifiable psychosocial stressor. It arises within 3 months of the onset of a stressor and persists up to 6 months after stressor resolution. It is characterized by low mood, tearfulness, or hopelessness associated with a significant distress that exceeds what would be expected given the nature of the stressor, or impaired social or occupational functioning. On the other hand, dysthymic disorder is a pattern of chronic symptoms of depression that are present for most of the time on most days with a minimum duration of 1 year for children and adolescents [ 32 ].
Bipolar disorder and schizophrenia are much less common in adolescents compared to depression disorder. However, they have different prognosis and require different treatments. Consequently, when establishing the diagnosis of depressive disorder in adolescence, it is important to bear in mind that the first symptomatic episode may also represent the beginning of a bipolar disorder [ 36 , 37 ].
Management and treatment
The treatment of depression in adolescence can include psychotherapy, pharmacotherapy or both [ 38 ]. Treatment should be selected based on the severity of the condition, the preference of the patient/family, associated risk factors, family support and the availability of each therapy [ 39 , 40 ]. On first approach, it is essential to comprehensively explain the therapeutic strategy and involve both patients and family members to assure close follow-up of progress, treatment adjustment according to symptoms and prevention of relapse [ 41 ]. Adolescents with moderate to severe depression, substance abuse, psychiatric disorders, suicidal ideation or resistance to treatment should be referred for specialized evaluation [ 42 ].
Treatment may be divided into three phases: acute (obtain response and remission), continuation (consolidate the response) and maintenance (avoid recurrences) [ 39 ]. Each of them must include psychoeducation, supportive approach and family involvement [ 39 , 40 ].
In mild depression, psychotherapy may be the first option, complemented with pharmacotherapy if there is no response [ 42 , 43 ]. The AAP recommends starting with active support, symptom monitoring and close follow-up for 6–8 weeks [ 44 ]. These measures are also useful when patients refuse more interventional treatments. The National Institute for Health and Care Excellence (NICE) has a slightly stricter approach, in which it recommends psychotherapy after absence of improvement after 2 weeks of watchful waiting [ 45 ]. In adolescents with moderate to severe depression, treatment is based on combined psychotherapy and pharmacotherapy [ 42 , 43 ]. NICE recommends psychotherapy for the minimum of 3 months, followed by fluoxetine if necessary. AAP has a similar approach [ 44 , 45 ]. Other strategies such as physical exercise, sleep hygiene and adequate nutrition have been referred as treatment adjuvants [ 44 , 46 , 47 ].
Both NICE and AAP recommend treatment for at least 6 months after remission of symptoms to consolidate the response and prevent relapse (continuation phase). In addition, both organizations also recommend maintaining follow-up during 1 year or, in cases of recurrent depression, 2 years [ 44 , 45 ].
Psychotherapy
In this area, Cognitive Behavioural Therapy (CBT) and Interpersonal Therapy (IPT) have shown effectiveness [ 40 , 48 ].
CBT is a brief psychotherapy, carried out individually or in groups, based on the relationship between thoughts, feelings and behaviours [ 40 ]. CBT focuses on cognitive distortions associated with depressive mood and the development of behavioural activation techniques, coping strategies and problem solving [ 42 ]. When used in acute depression, it has been shown to have a moderate effect [ 40 ]. CBT seems to be useful in preventing relapses and suicidal ideation, in the treatment of resistant depression and in adolescents with long-term physical conditions [ 49 , 50 , 51 ]. Moreover, the combination of psychotherapy and pharmacotherapy, in particular fluoxetine, has shown promising results [ 52 ]. Within the different psychotherapy approaches, behavioural activation, challenging thoughts and involvement of caregivers have a higher success rate [ 53 ].
IPT assumes depression association with disruptive relationships, based on the negative impact of symptoms on interpersonal relationships and vice-versa [ 40 ]. This approach may be useful especially when there is a well-established relational factor as the cause of the depressive condition [ 54 ]. Most studies have compared only IPT with placebo groups or with other psychotherapy, showing favourable results for IPT [ 48 , 55 ].
Psychotherapy should be considered first line of treatment in adolescents afraid of or with contraindications for medication, with identified stress factors or those with poor response to other approaches [ 56 ]. There are no contraindications to psychotherapy, though it has a limited effect in cases of cognitive delay [ 40 ].
Pharmacotherapy
Even though psychotherapy is an important component, pharmacotherapy can be used as an addition. When psychotherapy is not available or cannot be applied, pharmacotherapy can be an alternative [ 39 , 41 ].
Fluoxetine is widely regarded as the first-line drug for this age group given its efficacy [ 2 , 38 , 57 , 58 , 59 ]. Besides fluoxetine, escitalopram has also shown to be particularly effective, especially for ages between 12 and 17 years [ 38 , 60 , 61 , 62 ]. The main side effects of selective serotonin receptor inhibitors (SSRIs) include abdominal pain, agitation, jitteriness, restlessness, diarrhoea, headache, nausea and changes in sleep patterns. However, these effects are dose dependent and tend to decrease over time [ 39 ].
Given the efficacy of fluoxetine and escitalopram, many studies have focused on other SSRIs, such as sertraline, citalopram, paroxetine and fluvoxamine. Citalopram must be carefully evaluated as side effects include prolongation of the QT interval, which can lead to arrhythmia [ 63 , 64 ]. Paroxetine and fluvoxamine are not commonly used due to a lack of efficacy in this age group [ 65 , 66 ]. Regarding serotonin noradrenaline receptor inhibitors (SNRIs), venlafaxine appears to have a similar efficacy to SSRIs in resistant depression and no significant differences in adverse effects [ 49 ]. However, because hypertension is a possible side effect, this parameter must be periodically evaluated [ 41 , 64 ]. In Table 1 , the main drugs used in the treatment of depression in adolescents are displayed.
Bupropion and duloxetine have also been studied as alternatives but the evidence of its use in adolescents is limited. Bupropion can be useful in the treatment of overweight patients or those who intend to quit smoking. The main side effects are insomnia, agitation and seizures [ 41 ]. Bupropion is contraindicated in patients suffering from eating disorders. Duloxetine can be used for comorbid depression and pain in adolescents [ 67 ].
Tricyclic antidepressants do not have any demonstrated benefit in the treatment of depression in adolescents [ 42 , 68 , 69 ]. This drug class has significant side effects such as dry mouth, orthostatic hypotension, tremors and vertigo and can increase PR interval and QRS duration. Moreover, it is highly lethal in overdose [ 69 ].
At the time of writing, only fluoxetine (ages 8 years and older) and escitalopram (ages 12 years and older) are approved by the Food and Drug Administration for the treatment of depression in children and adolescents [ 70 , 71 ].
Several studies suggest an association between antidepressants and increased suicidal risk [ 18 , 58 ]. However, the risks and benefits of this strategy should be evaluated. Adolescents should be closely monitored, and, if suicidal thoughts arise during treatment, parents should seek care as soon as possible, to adjust dosage, change antidepressant or discontinue it [ 42 ].
Finally, the treatment strategies proposed in this age group are illustrated in Fig. 1 .
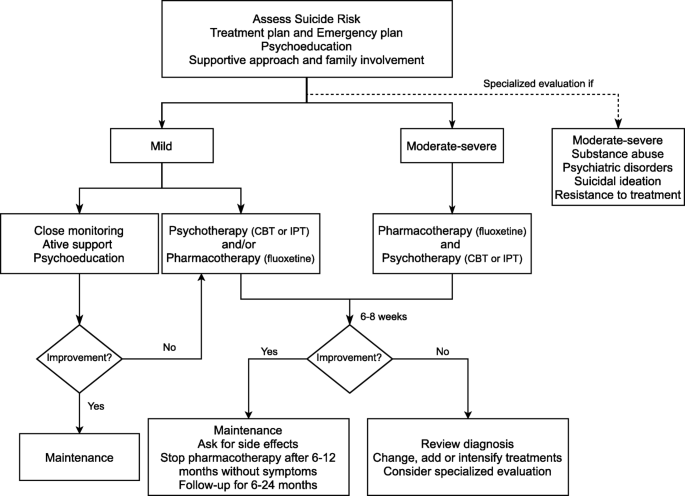
Algorithm for the management and treatment of depression in adolescents
Prevention is crucial to depression management, consequence of the impact on the population and inequal quality health care access [ 72 ]. In addition, it prevents the onset of other possible comorbidities, as well as reduces the impact on the patient and their families [ 73 , 74 , 75 ].
It is important to understand which different risk factors and protective factors intervene in the development of the disease. The risk factors can be divided into specific and non-specific for depression. Regarding the specific ones, parent depression history increases the risk between 2 and 4 times [ 76 ]. Among the non-specific, poverty, domestic violence and child abuse also increase the risk. On the other hand, protective factors are good family support, emotional skills or coping ability [ 77 ].
Depression prevention can be divided into 3 types: universal, selective and indicated. Universal interventions target the adolescent population group in general. Selective interventions target adolescents who are at risk for developing depression. Finally, indicated interventions target adolescents with subclinical symptoms of depression [ 78 ].
With regard to universal interventions, the efficacy of prevention programs through therapy for problem solving and overcoming traumatic situations has been demonstrated in multiple studies [ 79 , 80 ]. Although it has been shown that adolescents under these programs experience decreased depressive symptoms, the long-term usefulness of these programs was not unanimous. The inclusion of parents to these programs provided no additional advantage [ 81 ]. Furthermore, no significant difference between adolescents who received an intervention program and those who did not was found, although improvements in school environment were reported [ 82 ].
Concerning selective interventions, interpersonal communication skills and optimistic thinking programs have shown to be effective in decreasing anxiety and depression [ 83 ]. Contrary to universal interventions, the inclusion of parents in programs was demonstrated as beneficial [ 83 , 84 , 85 ]. However, it had no benefit to adolescents, but improved the parents’ perception of children’s behaviour [ 86 ].
Finally, in indicated interventions, psychoeducation and skill development programs to overcome interpersonal issues and role disputes among adolescents have been carried out [ 87 , 88 ]. It was shown that symptoms improved significantly compared at the end of the program [ 87 ]. Additionally, the number of adolescents with suicidal ideations decreased.
Comparing different groups of programs, various meta-analyses have found that selective and indicated programs are more effective than universal ones [ 89 , 90 ]. These prevention programs are more effective when started between the ages of 11 and 15 [ 78 ]. However, their superiority is not unanimous [ 91 ].
Depression in adolescence can be a complex diagnosis and requires individual and oriented treatment. For this reason, early identification, treatment initiation and prompt referral to mental health specialists is crucial for the prognosis of these patients.
Due to the variety of its main clinical manifestations and the lack of diagnostic tests that fully and accurately establish the definite diagnosis, this process can be particularly challenging. Additionally, several differential diagnoses must be made to provide an accurate course of treatment.
Treatment options can include both psychotherapy (CBT or IPT) and pharmacotherapy. The most promising results are observed with the combination of psychotherapy and pharmacotherapy, mainly fluoxetine.
Nevertheless, the authors would like to highlight certain aspects that require improvement and implementation in daily practice in comparison with the presented recommendations in this publication. First, although Cognitive Behavioral Therapy is one of the most studied therapeutic orientations, the reproducibility of performance among professionals is limited and relies on the relationship established between the mental health professional and the patient, in a deeper way compared to pharmacotherapy. The scarce number of professionals and the absence of choice by the user may not allow the development of this interpersonal bond. This limitation is particularly important in the case of children and adolescents, who are in a period of transition in their physical and mental development, and whose psychological intervention can have a significant positive or negative impact with potential future repercussions. Second, most of the prevention programs described in the literature are not currently implemented. Finally, approaching the family environment is essential in the implementation of effective long-term therapeutic interventions, especially in the presence of a dysfunctional structure. Although recommended, its practical application is often difficult due to the need of active participation of family members, inside and outside the clinical office. Prevention, early diagnosis and treatment of depression in adolescence should be considered worldwide objectives, and the implementation of straightforward, effective and cost-conscious strategies for achieving such purposes is essential. Amongst these objectives, prevention is of utter importance and must be a priority when defining political strategies and governmental programs related to mental health.
Availability of data and materials
Not applicable.
Abbreviations
US Preventive Services Task Force
American Academy of Pediatrics
Prefrontal cortex
Hypothalamic-pituitary-adrenal
Beck Depression Inventory
Patient Health Questionnaire for Adolescents
Beck Depression Inventory for Primary Care
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
Cognitive Behavioral Therapy
Interpersonal Therapy
Selective Serotonin Reuptake Inhibitors
Costello EJ, Egger H, Angold A (2005) 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry 44(10):972–986. https://doi.org/10.1097/01.chi.0000172552.41596.6f
Article PubMed Google Scholar
Forman-Hoffman V, McClure E, McKeeman J, Wood CT, Middleton JC, Skinner AC, Perrin EM, Viswanathan M (2016) Screening for major depressive disorder in children and adolescents: a systematic review for the US preventive services task force. Ann Intern Med 164(5):342. https://doi.org/10.7326/m15-2259
Siu AL, USPSTF (2016) Screening for depression in children and adolescents: US preventive services task force recommendation statement. Pediatrics 137(3). https://doi.org/10.1542/peds.2015-4467
Zuckerbrot RA, Cheung A, Jensen PS, Stein REK, Laraque D (2018) Guidelines for adolescent depression in primary care (GLAD-PC): part I - practice preparation, identification, assessment, and initial management. Pediatrics 141 (3):pii:e20174081. https://doi.org/10.1542/peds.2017-4081
Costello EJ, Foley DL, Angold A (2006) 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: II. Developmental epidemiology. J Am Acad Child Adolesc Psychiatry 45(1):8–25. https://doi.org/10.1097/01.chi.0000184929.41423.c0
Green H, McGinnity A, Meltzer H, Ford T, Goodman R (2005) Mental health of children and young people in Great Britain, 2004. Palgrave Macmillan, Hampshire
Book Google Scholar
Perou R, Bitsko RH, Blumberg SJ, Pastor P, Ghandour RM, Gfroerer JC, Hedden SL, Crosby AE, Visser SN, Schieve LA, Parks SE, Hall JE, Brody D, Simile CM, Thompson WW, Baio J, Avenevoli S, Kogan MD, Huang LN (2013) Mental health surveillance among children - United States, 2005-2011. MMWR Suppl 62(2):1–35
PubMed Google Scholar
Wesselhoeft R, Sorensen MJ, Heiervang ER, Bilenberg N (2013) Subthreshold depression in children and adolescents - a systematic review. J Affect Disord 151(1):7–22. https://doi.org/10.1016/j.jad.2013.06.010
Blakemore SJ (2008) The social brain in adolescence. Nat Rev Neurosci 9(4):267–277. https://doi.org/10.1038/nrn2353
Article CAS PubMed Google Scholar
Nelson EE, Leibenluft E, McClure EB, Pine DS (2005) The social re-orientation of adolescence: a neuroscience perspective on the process and its relation to psychopathology. Psychol Med 35(2):163–174. https://doi.org/10.1017/s0033291704003915
Patton GC, Viner R (2007) Pubertal transitions in health. Lancet 369(9567):1130–1139. https://doi.org/10.1016/s0140-6736(07)60366-3
Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR (2015) Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry 54 (1):37-44.e32. https://doi.org/10.1016/j.jaac.2014.10.010
Hyde JS, Mezulis AH, Abramson LY (2008) The ABCs of depression: integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol Rev 115(2):291–313. https://doi.org/10.1037/0033-295x.115.2.291
Seedat S, Scott KM, Angermeyer MC, Berglund P, Bromet EJ, Brugha TS, Demyttenaere K, de Girolamo G, Haro JM, Jin R, Karam EG, Kovess-Masfety V, Levinson D, Medina Mora ME, Ono Y, Ormel J, Pennell BE, Posada-Villa J, Sampson NA, Williams D, Kessler RC (2009) Cross-national associations between gender and mental disorders in the world health organization world mental health surveys. Arch Gen Psychiatry 66(7):785–795. https://doi.org/10.1001/archgenpsychiatry.2009.36
Article PubMed PubMed Central Google Scholar
Angold A, Costello EJ, Erkanli A, Worthman CM (1999) Pubertal changes in hormone levels and depression in girls. Psychol Med 29(5):1043–1053. https://doi.org/10.1017/s0033291799008946
Cairns KE, Yap MB, Pilkington PD, Jorm AF (2014) Risk and protective factors for depression that adolescents can modify: a systematic review and meta-analysis of longitudinal studies. J Affect Disord 169:61–75. https://doi.org/10.1016/j.jad.2014.08.006
Boden JM, Fergusson DM, Horwood LJ (2010) Cigarette smoking and depression: tests of causal linkages using a longitudinal birth cohort. Br J Psychiatry 196(6):440–446. https://doi.org/10.1192/bjp.bp.109.065912
Thapar A, Collishaw S, Pine DS, Thapar AK (2012) Depression in adolescence. Lancet 379(9820):1056–1067. https://doi.org/10.1016/S0140-6736(11)60871-4
Trent ES, Viana AG, Raines EM, Woodward EC, Storch EA, Zvolensky MJ (2019) Parental threats and adolescent depression: the role of emotion dysregulation. Psychiatry Res 276:18–24. https://doi.org/10.1016/j.psychres.2019.04.009
Risch N, Herrell R, Lehner T, Liang KY, Eaves L, Hoh J, Griem A, Kovacs M, Ott J, Merikangas KR (2009) Interaction between the serotonin transporter gene (5-HTTLPR), stressful life events, and risk of depression: a meta-analysis. JAMA 301(23):2462–2471. https://doi.org/10.1001/jama.2009.878
Article CAS PubMed PubMed Central Google Scholar
Forbes EE, Dahl RE (2005) Neural systems of positive affect: relevance to understanding child and adolescent depression? Dev Psychopathol 17(3):827–850. https://doi.org/10.1017/s095457940505039x
Cloninger CR, Svrakic DM, Przybeck TR (1993) A psychobiological model of temperament and character. Arch Gen Psychiatry 50(12):975–990. https://doi.org/10.1001/archpsyc.1993.01820240059008
Nogueira BS, Fraguas R Júnior, Benseñor IM, Lotufo PA, Brunoni AR (2017) Temperament and character traits in major depressive disorder: a case control study. Sao Paulo Med J 135 (5)469-74. https://doi.org/10.1590/1516-3180.2017.0063250517
Zappitelli MC, Bordin IA, Hatch JP, Caetano SC, Zunta-Soares G, Olvera RL, Soares JC (2013) Temperament and character traits in children and adolescents with major depressive disorder: a case-control study. Compr Psychiatry 54(4):346–353. https://doi.org/10.1016/j.comppsych.2012.10.009
Nardi B, Francesconi G, Catena-Dell'Osso M, Bellantuono C (2013) Adolescent depression: clinical features and therapeutic strategies. Eur Rev Med Pharmacol Sci 17(11):1546–1551
CAS PubMed Google Scholar
Bilello JA (2016) Seeking an objective diagnosis of depression. Biomark Med 10(8):861–875. https://doi.org/10.2217/bmm-2016-0076
Mäki M, Mustalahti K, Kokkonen J, Kulmala P, Haapalahti M, Karttunen T, Ilonen J, Laurila K, Dahlbom I, Hansson T, Höpfl P, Knip M (2003) Prevalence of Celiac disease among children in Finland. N Engl J Med 348(25):2517–2524. https://doi.org/10.1056/NEJMoa021687
Maurer DM, Raymond TJ, Davis BN (2018) Depression: screening and diagnosis. Am Fam Physician 98(8):508–515
Stockings E, Degenhardt L, Lee YY, Mihalopoulos C, Liu A, Hobbs M, Patton G (2015) Symptom screening scales for detecting major depressive disorder in children and adolescents: a systematic review and meta-analysis of reliability, validity and diagnostic utility. J Affect Disord 174:447–463. https://doi.org/10.1016/j.jad.2014.11.061
Beck AT, Guth D, Steer RA, Ball R (1997) Screening for major depression disorders in medical inpatients with the beck depression inventory for primary care. Behav Res Ther 35(8):785–791. https://doi.org/10.1016/s0005-7967(97)00025-9
Johnson JG, Harris ES, Spitzer RL, Williams JBW (2002) The patient health questionnaire for adolescents: validation of an instrument for the assessment of mental disorders among adolescent primary care patients. J Adolesc Health 30(3):196–204. https://doi.org/10.1016/s1054-139x(01)00333-0
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th edition: DSM-5 (2013). 5th edn. American Psychiatric Publishing, Arlington.
Orchard F, Pass L, Marshall T, Reynolds S (2017) Clinical characteristics of adolescents referred for treatment of depressive disorders. Child Adolesc Ment Health 22(2):61–68. https://doi.org/10.1111/camh.12178
Kovacs M, Obrosky DS, Sherrill J (2003) Developmental changes in the phenomenology of depression in girls compared to boys from childhood onward. J Affect Disord 74(1):33–48. https://doi.org/10.1016/s0165-0327(02)00429-9
Price RB, Rosen D, Siegle GJ, Ladouceur CD, Tang K, Allen KB, Ryan ND, Dahl RE, Forbes EE, Silk JS (2016) From anxious youth to depressed adolescents: prospective prediction of 2-year depression symptoms via attentional bias measures. J Abnorm Psychol 125(2):267–278. https://doi.org/10.1037/abn0000127
Lewinsohn PM, Klein DN, Seeley JR (1995) Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry 34(4):454–463
Article CAS Google Scholar
Thapar A, Pine D, Leckman JF, Scott S, Snowling MJ, Taylor EA (2017) Rutter’s child and adolescent psychiatry, 6th edn. Wiley-Blackwell, Oxford, UK
Google Scholar
Selph SS, McDonagh MS (2019) Depression in children and adolescents: evaluation and treatment. Am Fam Physician 100(10):609–617
Birmaher B, Brent D (2007) Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry 46(11):1503–1526. https://doi.org/10.1097/chi.0b013e318145ae1c
Cheung AH, Kozloff N, Sacks D (2013) Pediatric depression: an evidence-based update on treatment interventions. Curr Psychiatry Rep 15(8):381. https://doi.org/10.1007/s11920-013-0381-4
Richardson LP, Katzenellenbogen R (2005) Childhood and adolescent depression: the role of primary care providers in diagnosis and treatment. Curr Probl Pediatr Adolesc Health Care 35(1):6–24. https://doi.org/10.1016/j.cppeds.2004.09.001
Clark MS, Jansen KL, Cloy JA (2012) Treatment of childhood and adolescent depression. Am Fam Physician 86(5):442–448
Lewandowski RE, Acri MC, Hoagwood KE, Olfson M, Clarke G, Gardner W, Scholle SH, Byron S, Kelleher K, Pincus HA, Frank S, Horwitz SM (2013) Evidence for the management of adolescent depression. Pediatrics 132(4):e996–e1009. https://doi.org/10.1542/peds.2013-0600
Cheung AH, Zuckerbrot RA, Jensen PS, Laraque D, Stein REK (2018) Guidelines for adolescent depression in primary care (GLAD-PC): part II - treatment and ongoing management. Pediatrics 141(3):e20174082. https://doi.org/10.1542/peds.2017-4082
National Institute for Health and Care Excellence (2019) Depression in children and young people: identification and management (NICE Guideline 134). Available at: https://www.nice.org.uk/guidance/ng134 [].
Bailey AP, Hetrick SE, Rosenbaum S, Purcell R, Parker AG (2018) Treating depression with physical activity in adolescents and young adults: a systematic review and meta-analysis of randomised controlled trials. Psychol Med 48(7):1068–1083. https://doi.org/10.1017/s0033291717002653
Radovic S, Gordon MS, Melvin GA (2017) Should we recommend exercise to adolescents with depressive symptoms? A meta-analysis. J Paediatr Child Health 53(3):214–220. https://doi.org/10.1111/jpc.13426
Zhou X, Hetrick SE, Cuijpers P, Qin B, Barth J, Whittington CJ, Cohen D, Del Giovane C, Liu Y, Michael KD, Zhang Y, Weisz JR, Xie P (2015) Comparative efficacy and acceptability of psychotherapies for depression in children and adolescents: a systematic review and network meta-analysis. World Psychiatry 14(2):207–222. https://doi.org/10.1002/wps.20217
Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, Vitiello B, Ritz L, Iyengar S, Abebe K, Birmaher B, Ryan N, Kennard B, Hughes C, DeBar L, McCracken J, Strober M, Suddath R, Spirito A, Leonard H, Melhem N, Porta G, Onorato M, Zelazny J (2008) Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA 299(8):901–913. https://doi.org/10.1001/jama.299.8.901
Thabrew H, Stasiak K, Hetrick SE, Donkin L, Huss JH, Highlander A, Wong S, Merry SN (2018) Psychological therapies for anxiety and depression in children and adolescents with long-term physical conditions. Cochrane Database Syst Rev 12:CD012488. https://doi.org/10.1002/14651858.CD012488.pub2
Vitiello B, Brent DA, Greenhill LL, Emslie G, Wells K, Walkup JT, Stanley B, Bukstein O, Kennard BD, Compton S, Coffey B, Cwik MF, Posner K, Wagner A, March JS, Riddle M, Goldstein T, Curry J, Capasso L, Mayes T, Shen S, Gugga SS, Turner JB, Barnett S, Zelazny J (2009) Depressive symptoms and clinical status during the treatment of adolescent suicide attempters (TASA) study. J Am Acad Child Adolesc Psychiatry 48(10):997–1004. https://doi.org/10.1097/CHI.0b013e3181b5db66
March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, Burns B, Domino M, McNulty S, Vitiello B, Severe J (2004) Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA 292(7):807–820. https://doi.org/10.1001/jama.292.7.807
Oud M, de Winter L, Vermeulen-Smit E, Bodden D, Nauta M, Stone L, van den Heuvel M, Taher RA, de Graaf I, Kendall T, Engels R, Stikkelbroek Y (2019) Effectiveness of CBT for children and adolescents with depression: a systematic review and meta-regression analysis. European psychiatry 57:33–45. https://doi.org/10.1016/j.eurpsy.2018.12.008
Brunstein-Klomek A, Zalsman G, Mufson L (2007) Interpersonal psychotherapy for depressed adolescents (IPT-A). Isr J Psychiatry Relat Sci 44(1):40–46
Mufson L, Dorta KP, Wickramaratne P, Nomura Y, Olfson M, Weissman MM (2004) A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry 61(6):577–584. https://doi.org/10.1001/archpsyc.61.6.577
Tompson MC, McNeil FM, Rea MM, Asarnow JR (2000) Identifying and treating adolescent depression. West J Med 172(3):172–176. https://doi.org/10.1136/ewjm.172.3.172
Cipriani A, Zhou X, Del Giovane C, Hetrick SE, Qin B, Whittington C, Coghill D, Zhang Y, Hazell P, Leucht S, Cuijpers P, Pu J, Cohen D, Ravindran AV, Liu Y, Michael KD, Yang L, Liu L, Xie P (2016) Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis. Lancet 388(10047):881–890. https://doi.org/10.1016/S0140-6736(16)30385-3
Hetrick SE, Merry SN, McKenzie J, Sindahl P, Proctor M (2007) Selective serotonin reuptake inhibitors (SSRIs) for depressive disorders in children and adolescents. Cochrane Database Syst Rev 3:CD004851. https://doi.org/10.1002/14651858.CD004851.pub2
Article Google Scholar
Ignaszewski MJ, Waslick B (2018) Update on randomized placebo-controlled trials in the past decade for treatment of major depressive disorder in child and adolescent patients: a systematic review. J Child Adolesc Psychopharmacol 28(10):668–675. https://doi.org/10.1089/cap.2017.0174
Bridge JA, Iyengar S, Salary CB, Barbe RP, Birmaher B, Pincus HA, Ren L, Brent DA (2007) Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA 297(15):1683–1696. https://doi.org/10.1001/jama.297.15.1683
Findling RL, Robb A, Bose A (2013) Escitalopram in the treatment of adolescent depression: a randomized, double-blind, placebo-controlled extension trial. J Child Adolesc Psychopharmacol 23(7):468–480. https://doi.org/10.1089/cap.2012.0023
Mullen S (2018) Major depressive disorder in children and adolescents. Ment Health Clin 8(6):275–283. https://doi.org/10.9740/mhc.2018.11.275
Czaja AS, Valuck RJ, Anderson HD (2013) Comparative safety of selective serotonin reuptake inhibitors among pediatric users with respect to adverse cardiac events. Pharmacoepidemiol Drug Saf 22(6):607–614. https://doi.org/10.1002/pds.3420
DeFilippis M, Wagner KD (2014) Management of treatment-resistant depression in children and adolescents. Pediatric Drugs 16(5):353–361. https://doi.org/10.1007/s40272-014-0088-y
Hetrick SE, McKenzie JE, Cox GR, Simmons MB, Merry SN (2012) Newer generation antidepressants for depressive disorders in children and adolescents. Cochrane Database Syst Rev 11:CD004851. https://doi.org/10.1002/14651858.CD004851.pub3
Walkup JT, Labellarte MJ, Riddle MA, Pine DS, Greenhill L, Klein R, Davies M, Sweeney M, Abikoff H, Hack S (2001) Fluvoxamine for the treatment of anxiety disorders in children and adolescents. N Engl J Med 344(17):1279–1285. https://doi.org/10.1056/NEJM200104263441703
Meighen KG (2007) Duloxetine treatment of pediatric chronic pain and co-morbid major depressive disorder. J Child Adolesc Psychopharmacol 17(1):121–127. https://doi.org/10.1089/cap.2006.0042
Hazell P, Connell D, Heathcote D, Robertson J, Henry D (1995) Efficacy of tricyclic drugs in treating child and adolescent depression: a meta-analysis. BMJ 310(6984):897. https://doi.org/10.1136/bmj.310.6984.897
Hazell P, Mirzaie M (2013) Tricyclic drugs for depression in children and adolescents. Cochrane Database Syst Rev 6:CD002317. https://doi.org/10.1002/14651858.CD002317.pub2
Eli Lilly and Company. Prozac (Fluoxetina) [Capsules]. U.S. Food and Drug Administration website https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/018936s108lbl.pdf . Revised 2017. Accessed 20 July, 2020.
H. Lundbeck A/S. Lexapro (Escitalopram) [Tablets]. U.S. Food and Drug Adminstration website https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/021323s047lbl.pdf . Revised 2017. Accessed 20 July, 2020.
Kakuma R, Minas H, Van Ginneken N, Dal Poz MR, Desiraju K, Morris JE, Saxena S, Scheffler RM (2011) Human resources for mental health care: current situation and strategies for action. The Lancet 378(9803):1654–1663. https://doi.org/10.1016/S0140-6736(11)61093-3
Cuijpers P, van Straten A, Smit F, Mihalopoulos C, Beekman A (2008) Preventing the onset of depressive disorders: a meta-analytic review of psychological interventions. Am J Psychiatry 165(10):1272–1280. https://doi.org/10.1176/appi.ajp.2008.07091422
Judd LL (1997) The clinical course of unipolar major depressive disorders. Arch Gen Psychiatry 54(11):989–991. https://doi.org/10.1001/archpsyc.1997.01830230015002
Panel DG (1994) Depression in primary care: detection, diagnosis, and treatment. J Am Assoc Nurse Pract 6(5):224–238. https://doi.org/10.1111/j.1745-7599.1994.tb00946.x
Evans DL, Andrews LW (2005) Adolescent mental health initiative. In: If your adolescent has depression or bipolar disorder: an essential resource for parents. Press, Oxford University
England MJ, Sim LJ, Council NR (2009) The etiology of depression. In: Depression in parents, parenting, and children: opportunities to improve identification, treatment, and prevention. National Academies Press (US), pp 73-118
O’Connell ME, Boat T, Warner KE (2009) Preventing mental, emotional, and behavioral disorders among young people: progress and possibilities, vol 7. National Academies Press, Washington, DC
Spence SH, Sheffield JK, Donovan CL (2003) Preventing adolescent depression: an evaluation of the problem solving for life program. J Clin Child Psychol 71(1):3–13. https://doi.org/10.1037//0022-006x.71.1.3
Spence SH, Sheffield JK, Donovan CL (2005) Long-term outcome of a school-based, universal approach to prevention of depression in adolescents. J Consult Clin Psychol 73(1):160–167. https://doi.org/10.1037/0022-006X.73.1.160
Shochet IM, Dadds MR, Holland D, Whitefield K, Harnett PH, Osgarby SM (2001) The efficacy of a universal school-based program to prevent adolescent depression. J Clin Child Psychol 30(3):303–315. https://doi.org/10.1207/S15374424JCCP3003_3
Sawyer MG, Pfeiffer S, Spence SH, Bond L, Graetz B, Kay D, Patton G, Sheffield J (2010) School-based prevention of depression: a randomised controlled study of the beyondblue schools research initiative. J Child Psychol Psychiatry 51(2):199–209. https://doi.org/10.1111/j.1469-7610.2009.02136.x
Gillham JE, Reivich KJ, Freres DR, Lascher M, Litzinger S, Shatté A, Seligman ME (2006b) School-based prevention of depression and anxiety symptoms in early adolescence: a pilot of a parent intervention component. Sch Psychol Q 21(3):323–348. https://doi.org/10.1521/scpq.2006.21.3.323
Gillham JE, Brunwasser SM, Freres DR (2008) Preventing depression in early adolescence: the penn resiliency program. In: Handbook of depression in children and adolescents. The Guilford Press, New York, NY, US, pp 309–322
Gillham JE, Hamilton J, Freres DR, Patton K, Gallop R (2006a) Preventing depression among early adolescents in the primary care setting: a randomized controlled study of the Penn Resiliency Program. J Abnorm Child Psychol 34(2):203–219. https://doi.org/10.1007/s10802-005-9014-7
Roberts C, Ballantyne F, Van Der Klift P (2003) Aussie optimism. Curtin University of Technology, Perth, Australia, Social life skills. Teacher resource
Thompson EA, Eggert LL, Herting JR (2000) Mediating effects of an indicated prevention program for reducing youth depression and suicide risk behaviors. Suicide Life Threat Behav 30(3):252–271. https://doi.org/10.1111/j.1943-278X.2000.tb00990.x
Young JF, Mufson L, Davies M (2006) Efficacy of interpersonal psychotherapy-adolescent skills training: an indicated preventive intervention for depression. J Child Psychol Psychiatry 47(12):1254–1262. https://doi.org/10.1111/j.1469-7610.2006.01667.x
Horowitz JL, Garber J (2006) The prevention of depressive symptoms in children and adolescents: a meta-analytic review. J Consult Clin Psychol 74(3):401–415. https://doi.org/10.1037/0022-006X.74.3.401
Stice E, Shaw H, Bohon C, Marti CN, Rohde P (2009) A meta-analytic review of depression prevention programs for children and adolescents: factors that predict magnitude of intervention effects. J Consult Clin Psychol 77(3):486–503. https://doi.org/10.1037/a0015168
Merry SN, Hetrick SE, Cox GR, Brudevold-Iversen T, Bir JJ, McDowell H (2011) Psychological and educational interventions for preventing depression in children and adolescents. Cochrane Database Syst Rev 7(12):CD003380. https://doi.org/10.1002/14651858.CD003380.pub3
Download references
Acknowledgments
The authors would like to thank Dilermando Sobral, MD, Sónia Almeida, MD and Paula Assunção, MD for their guidance.
No sources of funding were required.
Author information
Authors and affiliations.
Family Health Unit of Ramalde, Health Centres Grouping of Porto Ocidental, Porto, Portugal
Diogo Beirão, Helena Monte, Marta Amaral, Alice Longras, Carla Matos & Francisca Villas-Boas
FP-ENAS-Energy, Environment and Health Research Unit/CEBIMED- Centro de Estudos em Biomedicina, Fernando Pessoa University, Porto, Portugal
Carla Matos
You can also search for this author in PubMed Google Scholar
Contributions
DB conceived the original idea of this work and took the lead in writing the manuscript. All authors contributed equally in the literature review and writing of the manuscript. DB was responsible for the section on epidemiology and comorbidities. HM was responsible for the sections on the background and pharmacological treatment. MA was responsible for the abstract, non-pharmacological treatment and the conclusion. AL was responsible for the sections on methods and pathogenesis. CM was responsible for the sections on diagnosis and background, and FVB for the section on prevention. DB and HM were responsible for the construction of the final version of the manuscript which was reviewed and approved by all co-authors.
Corresponding author
Correspondence to Diogo Beirão .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Beirão, D., Monte, H., Amaral, M. et al. Depression in adolescence: a review. Middle East Curr Psychiatry 27 , 50 (2020). https://doi.org/10.1186/s43045-020-00050-z
Download citation
Received : 12 June 2020
Accepted : 21 August 2020
Published : 02 October 2020
DOI : https://doi.org/10.1186/s43045-020-00050-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescence

IMAGES
VIDEO
COMMENTS
In adolescent depression, the cognitive-behavioral therapy and the Interpersonal Therapy-Adolescent seem to have a well-established efficacy. Weersing et al. , in this same line, state that, although the efficacy of treatments in children is rather weak, cognitive-behavioral therapy is probably the most effective therapy. They also confirm ...
Certain profiles of depression are more com-mon in adolescence than in adulthood. Although depressed mood is the most common symptom in adolescents and adults with major depressive disorder ...
Epidemiologic Features. Although the prevalence of depression has increased across all age groups, the increase among adolescents has outpaced that among adults. 3 The lifetime prevalence of major ...
Kieling is leading an international project called 'Identifying depression early in adolescence (IDEA)' that brings a global health approach to the topic. As your main area of research is ...
Depression rates in young people have risen sharply in the past decade, especially in females, which is of concern . because adolescence is a period of rapid social, emotional, and cognitive development and key life transitions. Adverse outcomes associated with depression in young people include depression recurrence; the onset of other psychiatric
Background: Depression is a common mental health disease, especially in mid to late adolescence that, due to its. particularities, is a challenge and requires an effective diagnosis. Primary care ...
Abstract. Depression often first develops during adolescence, with its rate sharply increasing after puberty and often running a chronic, recurring course thereafter. The development of depression is associated with difficulties in the lives of adolescents and their families, reduced academic achievement, suicide, and increased socio-economic ...
Depression in adolescence is a common mental health disease with a prevalence of 4-5% in mid to late adolescence [1]. It is a major risk factor for sui-cide and can also lead to social and educational impair-ments. Consequently, identifying and treating this disorder is crucial.
Tragically, 6,200 suicide deaths were reported in 2017 among U.S. adolescents and young adults from 15 to 24 years of age ( 3 ), and suicide is the second leading cause of death among individuals 10-34 years of age ( 4 ). As with other psychiatric illnesses, the risks for developing anxiety disorders and major depression are due to ...
A broad biopsychosocial perspective on adolescent depression is recommended, and possible directions for future integrative research are proposed, implications for research, program, and national policy are considered. Adolescence is an important developmental period for understanding the nature, course, and treatment of depression. Recent research concerned with depressive mood, syndromes ...
Similarly, Appel, Gerlach, and Crusius (Citation 2016) found that passive Facebook use predicts social comparison and envy, which in turn lead to depression. Adolescence is the period of personal and social identity formation (Erikson, Citation 1950), and much of this development is now reliant on social media. Due to their limited capacity for ...
This paper explores some of the potential mental health-related harms associated with the universal screening of anxiety and depression administered in Australian secondary schools as part of a cluster RCT that examined the effectiveness of a digital mental health service for improving adolescents' help-seeking [25, 27, 29].This paper presents a secondary data analysis of this recent RCT as ...
Teen depression is a serious mental health problem that causes a persistent feeling of sadness and loss of interest in activities. It affects how your teenager thinks, feels and behaves, and it can cause emotional, functional and physical problems. Although depression can occur at any time in life, symptoms may be different between teens and ...
Background Family and school environment play a crucial role across the different developmental stages of adolescence. This paper investigates the potential mediating role of family and school environments in the relationship between the three psychosocial predictors of depression, anxiety, stress, and Internet addiction (IA). Specifically, it focuses on the two stages of early and middle ...
Unipolar depressive disorder is a common mental health problem in adolescents worldwide,1 with an estimated 1 year prevalence of 4-5% in mid to late adolescence.2,3 Depression in adolescents is a major risk factor for suicide, the second-to-third leading cause of death in this age group,4 with more than half of adolescent suicide victims ...
Depression in Adolescents. Depression in Adolescents. Depression in Adolescents N Engl J Med. 2021 Jul 29;385(5):445-449. doi: 10.1056/NEJMra2033475. Authors Leslie Miller 1 , John V Campo 1 Affiliation 1 From the Department of Psychiatry and Behavioral ...
Adolescence can be a challenging time of life for developmental reasons. Social, emotional, and physical maturity increase during adolescence, and adolescent brains continue to develop. Adolescence is also a period in which new social and physical challenges emerge, including sensation seeking, risk-taking behaviors, and navigating peer influence.
Advertisement. Adolescents using social media for three or more hours a day face double the risk of depression and anxiety symptoms, he said. Murthy says he's calling on Congress to create safety ...
Black people with depression used different language than white people to express their thoughts on Facebook ... Residential addiction treatment for adolescents is scarce and expensive. Cite this article. APA Style MLA Style AMA Style. NIDA. 2024, March 26. Analysis of social media language using AI models predicts depression severity for white ...
The study was conducted while Collins was on the faculty at the University of Washington. The paper was written by an international, interdisciplinary team, including citiesRISE, a global nonprofit that works to transform mental health policy and practice in cities, especially for young people. Cities have long been a draw for young people.
Depression in adolescence is a relevant condition to the medical community, due to its uncertain clinical course and underdiagnosis worldwide. ... The present work consists of a review on the depression in the adolescent, summarizing data published in scientific papers in the last years, regarding the epidemiology of the disease, its ...
The considerable differences seen in the IAHS thematic focus as compared with the leading causes of fatal and non-fatal disease burden in adolescents in India, and in the availability of population-level data to monitor the outcome indicators of the IAHS can pose substantial limitations for improving adolescent health in India.
Depression Screening and Follow-Up for Adolescents and Adults (DSF-E) HEDIS ® (Healthcare Effectiveness Data Information Set) is a widely used set of performance measures developed and maintained by NCQA. These are used to drive improvement efforts surrounding best practices. The HEDIS quality measures reported using the electronic clinical ...