Compassion: what it is and why it matters in medicine

'Many medical students are demoralised by an impersonal system before they even begin'

.chakra .wef-1c7l3mo{-webkit-transition:all 0.15s ease-out;transition:all 0.15s ease-out;cursor:pointer;-webkit-text-decoration:none;text-decoration:none;outline:none;color:inherit;}.chakra .wef-1c7l3mo:hover,.chakra .wef-1c7l3mo[data-hover]{-webkit-text-decoration:underline;text-decoration:underline;}.chakra .wef-1c7l3mo:focus,.chakra .wef-1c7l3mo[data-focus]{box-shadow:0 0 0 3px rgba(168,203,251,0.5);} Mara Fiorese
Stefano alice.

.chakra .wef-1nk5u5d{margin-top:16px;margin-bottom:16px;line-height:1.388;color:#2846F8;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-1nk5u5d{font-size:1.125rem;}} Get involved .chakra .wef-9dduvl{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-9dduvl{font-size:1.125rem;}} with our crowdsourced digital platform to deliver impact at scale
If you were to comb through scientific literature, you may notice that there’s something capable of reducing post-operative pain, boosting the survival chance of cancer patients , lowering the mortality rate in high risk cardiac patients and cutting the hospitalization rate for diabetics . As if that wasn’t enough, it also boosts the immune system .
So what is this mysterious substance? It’s compassion, or better still, compassionate doctors. Before you stop reading, don’t make the mistake of confusing compassion with pity or commiseration.
Compassion isn't a single, sympathetic utterance, but is rather made up of presence and engagement that suffuses an entire conversation .
The importance of compassion may unsettle doctors who think their duty is to be technically proficient and up-to-date, those who think that it’s a natural quality you either have or don’t have, as well as certain ethicists who think that doctors need to maintain a professional distance from their patients.
But it is central to the welfare of patients. Dr. Robert Youngson, an anaesthesiologist, has launched a campaign to make healthcare more compassionate. According to his research , there are two type of doctors who fit the profile:
1) Empathetic doctors: those who naturally grasp that the whole point of empathy is to focus attention on the patient.
2) Doctors who have successfully attended a doctor patient communication skills course. Communication skills can be taught.
For example, a good technique for showing compassion, is simple: 3 T’s. Talk or listen, take time and touch. Merely taking the time to talk and listen to patients is comforting, as is a doctor’s touch .
Moreover, we must leave our empathetic abilities to guide us through our work, we should develop our compassion as a gift everyone can use.
How many doctors have become cold and distant after losing their freedom and being forced to work as small cogs in a big machine? How many students have become unenthusiastic or demotivated before even getting their medical degree? This is a pedagogical mistake due to a depersonalizing education system: unconcerned and unable to give full support to students, leaving them alone and without a role model.
Scientific literature proves that this argument can be applied both to single professionals and organisations. Personality, values and behaviour reflect individual performances, which are the road to failure or success for each organisation. The doctor-patient relationship is part of the healing process.
Biologically speaking, empathy can be explained by " Mirror neurons ." These are a type of brain cell that fires when someone performs an action, and also when a person watches someone else performing the same action.
They were discovered back in the 90s, by a team of Italian researchers who found individual neurons in the brains of monkeys that fired both when the monkeys grabbed an object and also when the monkeys watched another primate grab the same object.
But mirror neurons also exist in the brain areas that are in charge of emotions.
This means that we are able to recognize other people’s emotions simply by observing them. When we observe someone, these mirror neurons are activated and allow us to at least partly feel the emotions that the person we are observing is feeling.
These “empathic” mirrors are triggered both when we experience an emotion and when we observe somebody who is experiencing the same emotion. This extraordinary achievement provides the neurophysiological grounds for empathy.
“It’s the relationship that heals”, says Dr. Irvin D. Yalom, Psychiatry professor at Stanford University; he underlines the importance of qualitative relationships over theory. A relationship is strictly personal, a good relationship is based on care and the will to relieve patients’ suffering.
According to the American psychologist Carl Rogers, there are three main ingredients to a good doctor-patient relationship: empathy, honesty and genuineness .
Rollo May, psychologist and theologian, applies the Greek word “agape” or the Latin “caritas” to compassion to underline what is essential in a therapeutic relationship: an emotion of regard and affection (it applies to both “agape” and “caritas”). He shares the Royal College of General Practitioners’ (RCGP) point of view, whose motto is: “Cum Scientia caritas - Compassion with Knowledge”. It all seems to fit.
If we work on patient-centered care, if the patient himself feels that he’s taken seriously and the doctor addresses his needs, this will lead to reduced healthcare waste .
Our purpose is to stimulate a debate on how to improve medical training, given the positive results of the researches; a debate on being both up-to-date and compassionate.
At the edge of the Fourth Industrial Revolution, a wave of digital-era change, compassion is still a valuable tool for those who want to shape innovations rather than being overwhelmed by them.
Have you read?
In the machine age, only one type of organization will thrive: a human one, can a city be mindful and which cities do it best, people or process: which does your company put first, don't miss any update on this topic.
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
The Agenda .chakra .wef-n7bacu{margin-top:16px;margin-bottom:16px;line-height:1.388;font-weight:400;} Weekly
A weekly update of the most important issues driving the global agenda
- Open access
- Published: 15 March 2024
Cultivating compassion in medicine: a toolkit for medical students to improve self-kindness and enhance clinical care
- Krisha K. Mehta 1 ,
- Shafkat Salam 2 ,
- Austin Hake 2 ,
- Rebecca Jennings 2 ,
- Afra Rahman 2 &
- Stephen G. Post 2
BMC Medical Education volume 24 , Article number: 291 ( 2024 ) Cite this article
378 Accesses
Metrics details
Compassionate care lies at the foundation of good patient care and is a quality that patients and providers continue to value in the fast-paced setting of contemporary medicine. Compassion is often discussed superficially in medical school curricula, but the practical aspect of learning this skill is often not taught using a formal framework. In the present work, the authors present an 8-session curriculum with a mindfulness-based approach to compassion that addresses this need. It is hypothesized that students in this curriculum will improve in their levels of compassion based on validated scales.
The curriculum was delivered to fourth-year medical students at Renaissance School of Medicine at Stony Brook University who had just completed their clerkship year. It was developed as a customizable set of modules that could be delivered in various ways. The students were taught with evidence-based cognitive exercises followed by group discussions and written reflections based on compassion-focused thematic questions. All students completed a pre- and post-Self-Compassion Scale, Compassion Scale, and Toronto Mindfulness Scale. Students in this course were compared with students in different courses about non-clinical topics delivered at the same time. Wilcoxon Signed Rank tests and Mann Whitney U tests were used to assess potential associations between pre- and post-survey responses for the validated scales and subscales.
17 fourth-year medical students completed pre- and post-course tests, 11 participated in the compassion curriculum while 6 participated from the other courses. Before any of the courses began, all students performed similarly on the pre-test across all scales. The students in the compassion curriculum demonstrated a significant increase in their total Self-Compassion score by 8.7 [95% CI 4.3 to 13.2] points ( p = 0.008), total Compassion score by 6.0 [95% CI 1.4 to 10.6] points ( p = 0.012), and the curiosity component of the Toronto Mindfulness Scale by 4.4 [95% CI 1.0 to 7.7] points ( p = 0.012). There was no statistically significant difference between pre- and post-tests among the non-compassion curriculum students in the aforementioned scales ( p = 0.461, p = 0.144, p = 0.785, respectively).
Conclusions
Our results indicate that the students in our course developed an enhanced ability to engage in self-compassion, to understand the shared human experience, and to be motivated to act to alleviate suffering. Regardless of a program’s existing compassion education, this customizable model allows for easy integration into a medical student’s crowded curriculum. Furthermore, although teaching compassion early and often in a clinician’s training is desirable, our study that targeted fourth-year medical students suggests an additional benefit of rekindling the loss of compassion well described in a medical student’s clinical years.
Peer Review reports
Introduction
Compassion is defined as experiencing an authentic desire to help another person secondary to an emotional response to that person’s pain or suffering. Not only is compassion about feeling the desire, but also in enacting such a will. Although it seems unquestionable that compassionate care lies at the foundation of medicine and should be employed with all patients, there remains an obvious deficit in applying compassionate care in clinical medicine [ 1 ]. A 2010 national survey of 800 hospitalized patients and 510 physicians showed that nearly half of the patients and physicians felt that compassionate care is missing from the current healthcare system, signaling an incredibly urgent “compassion crisis” [ 2 ].
A consensus on nomenclature is required to advance our understanding and eventual education of this subject. Empathy involves two stages: the affective stage is the sharing of the emotion by the other and the feeling of the emotional state of the other and cognitive stage is the development of a mental representation of the emotional state. Compassion on the hand is a feeling of concern for another’s suffering combined with a motivation and an action to relieve the other’s suffering. Research has shown that there are distinct neural circuits for empathy and compassion - empathy was shown to activate the pathway involved with experiences of negative emotions and pain and compassion was shown to activate the pathway involved with positive affect and affiliation [ 3 ]. As such, it is important to delineate the terms used in literature as training in compassionate care will promote a pro-social state.
There is a stark absence of experimental studies testing interventions that increase compassionate behaviors and their impact on various outcomes such as patient benefit, provider benefit, healthcare system and payer benefit, and healthcare system cultural benefit [ 1 ]. Although other similar interventions to this study found significant changes in outcomes, many were complicated and impractical given their lengthy time requirement for implementation in hospitals and medical schools. For example, one study tested an intervention that included students participating in a once-a-week course; which included interviews with patients/physicians, supervised visits to the hospital, didactics and discussions of videotaped simulated consultations, over a four-month period [ 4 ]. Introducing longitudinal curricula such as this one may prove burdensome for already-crowded curricula at well-established medical schools.
Medical students and doctors experience high rates of psychological distress, including burnout, anxiety and depression [ 5 , 6 ]. As such, there has been increasing interest in incorporating mindfulness-based interventions for student well-being. Based on improvements in psychological well-being and self-compassion, one narrative review concluded that mindfulness-based toolkits are indeed beneficial for medical students [ 7 ]. Mindfulness is the act of engaging in the non-judgmental awareness of the relevant aspects of an experience. It allows for moment-to-moment awareness while disengaging from “strong attachment to beliefs, thoughts, or emotions to experience emotional regulation and clarity in thinking [ 8 ]. As described, there is strong evidence to suggest that training medical students and physicians in compassion correlates with positive changes in at least one outcome measure, which can either be for the patient or the provider themselves [ 9 ]. Although this has been known for years, many medical schools have failed to implement compassion training for medical students, leading to the current “compassion crisis” we live in. While reasons for this failure have not been specifically delineated, it’s possible that traditional medical educators assumed compassion is inherently present in medical students. This assumption, though not completely deniable, is unlikely given the recent evidence that compassion is deficient in medical students [ 9 ]. Further research about compassionate care in medicine could demonstrate that compassion can be taught and developed in medical students without requiring burdensome training programs or seminars.
Currently, there is a gap in the literature for easily implementable, effective interventions to increase compassion in health care providers and students. This research aims to fill that gap by utilizing a mindfulness-focused approach to compassion to provide students with a “toolkit” to promote compassionate care.
IRB approval
This study was approved and granted a notice of exemption on 03/09/2022 by the Institutional Review Board at Stony Brook University (IRB2022-0119). Due to this exemption, informed consent did not need to be obtained for the study participants.
Intervention
The intervention, the compassion selective, taught evidence-based cognitive exercises and practices followed by group discussions and written reflections based on thematic questions about those experiences. This selective was one option for a curricular requirement in the fourth year of medical school, amongst other courses described below. The intervention was designed in the following stepwise manner: understand what compassion means as a concept and as a practice via shared experiences, learn how to settle the mind through mindfulness-based practices, reflect on the emotions experienced by the self, reflect on the personal needs the self has and what corresponding behavior/activity do they engage, understand shared needs and values as a way to connect with others, learn what the barriers to connectedness are and how the stereotypes may influence our interactions with others, understand the concept of shared common humanity through mental exercises, and learn how to practice these on the go in a clinical setting.
The intervention included several exercises designed to cultivate compassion including: 1)asking the students to reflect in writing on common emotions and on the regulatory processes used to address those emotions; 2) reflecting in writing on the needs that underlie their behaviors; and 3) listening to another person’s story and reflecting on shared values, needs, and emotions.
The course was taught by a medical school faculty member from the Center for Medical Humanities, Compassionate Care and Bioethics and a 4th year medical student. The course was held over 40 h in 4 weeks − 16 h for lectures and small group discussions (2 h a day, 2 days a week for 4 weeks) and 24 h for self-study and assignments. The self-study included reading and analyzing papers related to the thematic topics being reviewed in class and reading chapters from The Art and Science of Compassion by Dr. Anges Wong [ 3 ]. The assignments included weekly self-reflections at the end of the week to discuss what was learned and how it may be implemented in their lives and an end-of-course project to create a presentation on an evidence-based article on compassion education.
Study tools
The survey included demographic data, the Self-Compassion Scale short form, the Compassion Scale, and the Toronto Mindfulness Scale. The Self-Compassion Scale (26-item scale 5 point Likert scale; validated in 20 diverse samples N = 11,685 by Neff et al.) measures one’s ability for self-compassion [ 10 ]. The Compassion Scale (16-item 5-point Likert scale; validated in 20 diverse samples N = 11,685 by Neff et al.) entails the understanding of concepts and evaluates one’s ability to act with kindness, social connectedness, common humanity and mindfulness [ 11 ]. The Toronto Mindfulness Scale (13-item scale 5 point Likert scale; validated in one diverse sample N = 390 by Lau et al.) includes both the Curiosity subscale, which describes the ability to reflect with inquisitiveness, and the Decentering subscale, which focuses on the ability to be aware of one’s experience and distance one’s own emotions from it [ 12 ].
These scales were chosen as they are validated scales that consist of sub-scales that can examine separate components of self-compassion, compassion and mindfulness. The scales are theoretically coherent and allow brevity and flexibility of use in a classroom setting. The brief structure of the scales also allows for higher compliance and completion rates for the survey itself.
Data collection
We anonymously surveyed medical students enrolled in the selective courses: Cultivating Compassion in Medicine, Addiction and Pain, Lifestyle Medicine, Telehealth Medicine, and Recognizing the Acutely-Ill Patient. The participants of these courses were fourth-year medical students enrolled to fulfill medical school requirements, and the courses ran from April 5th to April 28th, 2022. Students were surveyed using the online Qualtrics platform; pre- and post-course responses were collected over one week at the beginning of the course and one week at the end of the course. All the courses, including our selective, was taught at the Renaissance School of Medicine at Stony Brook University.
Data analysis
For this project the Cultivating Compassion in Medicine course was our intervention, and students enrolled in courses that were not Cultivating Compassion in Medicine were designated as controls - Addiction and Pain, Lifestyle Medicine, Telehealth Medicine, and Recognizing the Acutely-Ill Patient. The results from the other courses, i.e. non-compassion selectives were pooled together for analysis. We conducted independent t-tests to assess potential associations between the pre-test responses for the validated scales between the groups (intervention and control), to determine whether there were any differences at baseline. We conducted independent t-tests to assess potential associations between the pre-test responses for the validated scales between the groups (intervention and control) to determine whether there were any differences at baseline. Since we had a small sample size we determined whether our variables followed a normal distribution in order to choose an appropriate statistical test. A Shapiro-Wilk test was performed and showed that the distribution of some of our variables departed significantly from normality. Therefore, we conducted Wilcoxon Signed Rank tests to compare paired samples and to assess potential associations within groups (intervention or control) between the pre- and post-survey responses for the validated scales and subscales that were utilized. Mann-Whitney U tests were used to compare non-paired samples, to determine whether there were any baseline differences between groups for the validated scales. The minimum criterion for significance was set at p < 0.05. Statistical analysis was performed using SPSS 28.0 statistical software (IBM Corporation).
Participation in the study is described in Table 1 . The 11 paired responses for Cultivating Compassion in Medicine were compared with the control group of the 6 paired responses for the other courses. The students were of varying demographic backgrounds, including age, ethnic group and gender. Before the start of the courses, no significant difference was found between the participants in the Cultivating Compassion in Medicine course and the pooled participants responses from the control courses for any of the four main measures: compassion (U = 67.5, p = 0.816), self-compassion (U = 68.5, p = 0.862), curiosity (U = 60.5, p = 0.522), or decentering (U = 62, p = 0.581). Tables 2 , 3 and 4 demonstrates that students in the compassion course achieved a significant difference in self-compassion scores, compassion scores and the decentering component of the Toronto Mindfulness Scale.
Self-compassion scale
The students in the compassion course achieved a significant (Z= -2.654, p = 0.008) increase in their total Self-Compassion score of 8.7 [95% CI 4.3 to 13.2] points. There was no statistically significant difference among the control course students (Z= -0.736, p = 0.461). The sub-components of this scale are shown in Table 2 .
Compassion scale
The students in the compassion course achieved a significant (Z= -2.499, p = 0.012) increase in their total compassion score of 6.0 [95% CI 1.4 to 10.6] points. There was no statistically significant difference among the control course students (Z= -1.461, p = 0.144). The sub-components of this scale are shown in Table 3 .
Toronto mindfulness scale
The students in the compassion course achieved a significant (Z= -2.505, p = 0.012) increase in the curiosity component of the Toronto Mindfulness Scale of 4.4 [95% CI 1.0 to 7.7] points. There was no statistically significant difference in the decentering component of the scale (Z= -1.585, p = 0.113). There was no statistically significant difference among the control course students in either the curiosity component (Z= -0.272, p = 0.785) or the decentering component (Z= -0.921, p = 0.357). The sub-components of this scale are shown in Table 4 .
Medical school is an environment in which many medical students and trainees experience intense stress, which, for some students, culminates into increased depression symptoms and suicidal ideation, as well as a low sense of personal accomplishment [ 5 , 6 ]. Amidst all this, medical curricula demand students to practice self-care and compassionate care while providing little instruction on how to do so in practice [ 13 ]. Studies of medical trainees (residents and medical students) have found that mindfulness and meditation practices can influence a medical trainee’s levels of compassion, and many different methods have been employed to achieve this. An abridged mindfulness intervention to support wellness in first-year medical students showed a significant increase in self-compassion scores at the conclusion of the study and at six months [ 14 ]. Similarly, an 8-week mindfulness-based yoga intervention studying residents and medical students led to increased perceived compassion towards others post-intervention [ 15 ]. In this research, we set out to find if using a mindfulness-focused approach to compassion by providing medical students with a practical “toolkit” would, in fact, promote compassionate care, both for self and others. Throughout this curriculum, a combination of didactics in compassionate care and mindfulness theory and practical sessions to learn different methods of mindfulness and compassion helped students develop their personal toolkit to carry forward in their careers. The results convey a significant change in the ability of medical students who took the course to practice compassion. Self-compassion score pre-study showed no differences in the groups (compassion selective vs. other selectives), indicating no difference at baseline in self-compassion between groups before the intervention, while post-study scores were significantly higher in the compassion in medicine course group than the control group. Similarly, total compassion scores were not significantly different at baseline between the groups, and there was an increase in total compassion in this selective while no increase was seen in the control group. As groups do not differ at baseline, this would indicate that this difference is due to the selection, and not because of differences in population or self-selection into a course on compassion by people who might tend to be more compassionate. Students in the compassion course also significantly increased the curiosity component of the Toronto Mindfulness Scale. One of the major aspects of the compassion course focused on mindfulness-type interventions that students could employ. The proposed intervention provides a mindfulness-focused approach that provides a cognitive pathway to promoting self-compassion. The mental exercises and narratives they engage in help individuals identify their emotions, motivations and behaviors, allowing for appropriate emotional regulation. The intervention also provides strategies to enhance self-awareness, cognitive reappraisal and attentional control.
The finding in our study of an increased total compassion score for students who took the compassion course, which was not seen in the control group courses, indicates that the students who took the compassion course appeared to evidence growth in attentional stability, building mental representation of another’s emotions, understanding the shared human experience, connecting with another’s distress, and to be motivated to act to alleviate suffering. This supports our findings that mindfulness-based training courses can be effectively utilized to increase compassion among medical trainees [ 16 , 17 ]. Our results demonstrate that a formal curriculum can aid in developing the “how” to be compassionate towards others by teaching emotional contextualization, perspective-taking and cognitive flexibility. Understanding the differences between empathy and compassion is also crucial to developing this cognitive pathway. Research from Paul Bloom states the effort involved in emotional empathy can emotionally exhaust individuals, erode relationships, and reduce our capacity to be concerned with others [ 18 ]. Instead, engaging in cognitive practices that allow reason to be present in the decision-making process for an altruistic act are better tools for the greater good [ 3 ]. The study also demonstrates that strategies using cognitive practices and constructive thinking can prime kindness, patience and prosocial attributes. Our intervention, which could be easily adapted to existing curricula that involve discussions of medical humanities and could even be taught remotely, educates students on techniques to help individuals identify personal needs and connect them to shared needs that exist in humanity.
Patients seek compassionate care; however, medical schools appear to struggle to teach future medical physicians how to nurture compassion [ 19 ]. We used certified scales to measure the effectiveness of the course on self-compassion, compassion and mindfulness. This increases the value of our intervention as a curricular tool. The framework taught in the course can be adapted to teach in a time-effective manner during multiple points of medical education.
As with all studies, there are limitations that should be noted when interpreting the results. The study found no baseline difference in compassion between the groups, but self-selection, personal motivation, and receptivity to training in compassion are confounding factors that should be addressed in a future study. Response bias should also be considered, as medical students may be pressured to answer differently due to the nature of the career they are entering into. Another limitation of the study is the small sample size. The intervention class enrolled fifteen students; however, only eleven completed the pre and post-surveys. The control group included multiple courses (sixty students taking their respective courses); however, only six completed the pre and post-surveys. While there is a large gap in study participation between groups, using a control group allowed us to address the bias of baseline differences in compassion levels due to self-motivation, as mentioned above. Our results indicate that utilizing mindfulness to foster compassion in medical students is a successful approach. Further studies focusing on our course need to be conducted with a larger sample size for additional insights into the course. A repeat post-survey course several months after the end of the course would also provide insight into the value of our course as a curricular tool.
Proposed is a novel course designed to teach medical students how to practice compassion for themselves and their patients. The course was well received by early 4th-year medical students. It can be taught to medical students during any of the four years of schooling, albeit the recommendation is to expose the tools in the course early during medical education to provide sufficient time for incorporation and practice. The course can be used as an intervention and is customizable enough to apply to medical residents and physicians alike.
Data availability
All data is available in a secure server to use for further analysis or study. The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Wear D, Zarconi J. (2008) Can compassion be taught? Let’s ask our students. J Gen Intern Med. 2008;23: 948–953. https://doi.org/10.1007/s11606-007-0501-0 .
Lown BA, Rosen J, Marttila J. An agenda for improving compassionate care: a Survey shows about half of patients say such care is missing. Health Aff. 2011;30(9):1772–8. https://doi.org/10.1377/hlthaff.2011.0539 .
Article Google Scholar
Wong AMF. The art and science of compassion, a primer: reflections of a physician-chaplain. Oxford University Press; 2020.
Schweller M, Ribeiro DL, Celeri EV, de Carvalho-Filho MA. Nurturing virtues of the medical profession: does it enhance medical students’ empathy? Int J Med Educ. 2017;8:262–7. https://doi.org/10.5116/ijme.5951.6044 . PMID: 28704203; PMCID: PMC5511746.
Article PubMed PubMed Central Google Scholar
Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, Shanafelt TD. (2014) Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89(3):443– 51.
Dyrbye LNMD, Thomas MRMD, Shanafelt TDMD. Systematic review of Depression, anxiety, and other indicators of psychological distress among U.S. and Canadian Medical Students. Acad Med. April 2006;81(4):354–73.
Polle E, Gair J. Mindfulness-Based Stress Reduction for Medical Students: A Narrative Review. Canadian Medical Education Journal, vol. 12, no. 2, 31 Mar. 2021, pp. 74–80, www.erudit.org/en/journals/cmej/1900-v1-n1-cmej06034/1077196ar/abstract/ , https://doi.org/10.36834/cmej.68406 . Accessed 2 Apr. 2023.
Ludwig DS, Kabat-Zinn J. Mindfulness Med JAMA. 2008;300(11):1350–2.
CAS Google Scholar
Patel S, Pelletier-Bui A, Smith S, Roberts MB, Kilgannon H, Trzeciak S, Roberts BW. Curricula for empathy and compassion training in medical education: a systematic review. PLoS ONE. 2019;14(8). https://doi.org/10.1371/journal.pone.0221412 .
Neff KD. Development and validation of a scale to measure self-compassion. Self Identity. 2003;2:223–50.
Pommier E, Neff KD, Tóth-Király I. The development and validation of the compassion scale. Assessment. 2020;27:21–39. https://doi.org/10.1177/1073191119874108 .
Article PubMed Google Scholar
Lau MA, Bishop SR, Segal ZV, Buis T, Anderson ND, Carlson L, Shapiro S, Carmody J, Abbey S, Devins G. (2006) The Toronto Mindfulness Scale: development and validation. J Clin Psychol. 2006;62(12):1445-67. https://doi.org/10.1002/jclp.20326 . PMID: 17019673.
Winefield HR, Chur-Hansen A. Evaluating the outcome of communication skill teaching for entry-level medical students: does knowledge of empathy increase? Med Educ. 2000;34:90–4.
Article CAS PubMed Google Scholar
Fernando AT, Skinner K, Consedine NS. Increasing Compassion in Medical Decision-Making: can a brief mindfulness intervention help? Mindfulness. 2017;8:276–85.
Ofei-Dodoo S, Cleland-Leighton A, Nilsen K, Cloward JL, Casey E. Impact of a Mindfulness-Based, Workplace Group Yoga Intervention on Burnout, Self-Care, and Compassion in Health Care professionals a pilot study. J Occup Environ Med - Volume. 2020;62(8):581–7.
Branch WT Jr, Kern D, Haidet P, et al. Teaching the human dimensions of care in clinical settings. JAMA. 2001;286(9):1067–74.
Creswell JD. Mindfulness Interventions. Annual Review of Psychology, vol. 68, no. 1, 2017, pp. 491–516, www. https://doi.org/10.1146/annurev-psych-042716-051139 .
Bloom P. Against empathy: the case for rational compassion. Ecco, an imprint of HarperCollins; 2016.
Petrou L, Mittelman E, Osibona O, Panahi M, Harvey JM, Patrick YAA, et al. The role of humanities in the medical curriculum: medical students’ perspectives. BMC Med Educ. 2021;21:179. https://doi.org/10.1186/s12909-021-02555-5 .
Danilewitz M, Koszycki D, Maclean H, Sanchez-Campos M, Gonsalves C, Archibald D, Bradwejn J. Feasibility and effectiveness of an online mindfulness meditation program for medical students. Can Med Educ J -. 2018;9(4):e15–25.
Erogul M, Singer G, McIntyre T, Stefanov D. G. Abridged mindfulness intervention to Support Wellness in First-Year Medical Students. Teach Learn Med. 2014;26(4):350–6. https://doi.org/10.1080/10401334.2014.945025 .
Jaber R, Steinhardt S, Trilling J. Explanatory models of illness: a pilot study. Family Syst Med. 1991;9(1):39–51.
Mascaro JS, Kelley S, Darcher A, Negi LT, Worthman C, Miller A, Raison C. Meditation buffers medical student compassion from the deleterious effects of depression. J Posit Psychol - Volume. 2018;13(2):133–42.
McKenna KM, Hashimoto DA, Maguire MS, Bynum WE. (2016) The missing link: connection is the key to resilience in medical education. Acad Med. 2016;91(9):1197–1199.
Menezes P, Guraya SY, Guraya SS. (2021) A systematic review of educational interventions and their impact on empathy and compassion of undergraduate medical students. Front Med. 2021;8.
Moore S, Barbour R, Ngo H et al. Determining the feasibility and effectiveness of brief online mindfulness training for rural medical students: a pilot study. BMC Med Educ 20, 104.
Pedersen R. Empathy development in medical education– a critical review. Med Teach. 2010;32(7):593–600.
Pohontsch NJ, Stark A, Ehrhardt M, Kötter T, Scherer M. Influences on students’ empathy in medical education: an exploratory interview study with medical students in their third and last year. BMC Med Educ. 2018;18(1). https://doi.org/10.1186/s12909-018-1335-7 .
Schairer CE, Tutjer J, Cannavino C, Mobley WC, Eyler L, Bloss CS. Learning to practice compassionate care: medical students discuss their most memorable lessons. J Patient Exp. 2022;9(1):1–9.
Google Scholar
Sinclair S, Norris JM, McConnell SJ, Chochinov HM, Hack TF, Hagen NA et al. (2016) Compassion: a scoping review of the healthcare literature. BMC Palliat Care. 2016;15.
Trzeciak S, Roberts BW, Mazzarelli AJ. Compassionomics: hypothesis and experimental approach. Med Hypotheses. 2017;107:92–7. https://doi.org/10.1016/j.mehy.2017.08.015 .
Download references
Not applicable.
Author information
Authors and affiliations.
Department of Medicine, Stony Brook University, Stony Brook, NY, USA
Krisha K. Mehta
Stony Brook University, Renaissance School of Medicine, Stony Brook, NY, USA
Shafkat Salam, Austin Hake, Rebecca Jennings, Afra Rahman & Stephen G. Post
You can also search for this author in PubMed Google Scholar
Contributions
KM and SS wrote the main manuscript text. RJ ran the statistical analysis and AH and AR created the data collection form, figures and tables. All authors reviewed the manuscript.
Corresponding author
Correspondence to Krisha K. Mehta .
Ethics declarations
Ethics approval and consent to participate.
This study was approved and granted a notice of exemption on 03/09/2022 by the Institutional Review Board at Stony Brook University (IRB2022-0119). The need for study approval and informed consent was waived by the Institutional Review Board at Stony Brook University (IRB2022-0119).
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mehta, K.K., Salam, S., Hake, A. et al. Cultivating compassion in medicine: a toolkit for medical students to improve self-kindness and enhance clinical care. BMC Med Educ 24 , 291 (2024). https://doi.org/10.1186/s12909-024-05270-z
Download citation
Received : 07 November 2023
Accepted : 06 March 2024
Published : 15 March 2024
DOI : https://doi.org/10.1186/s12909-024-05270-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Compassion education
- Medical education
- Medical humanities
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An Initiative of the Program for Bedside Medicine
- See us on youtube
- See us on facebook
- See us on twitter
Compassion: A Powerful Tool for Improving Patient Outcomes

The release of Compassionomics: The Revolutionary Scientific Evidence That Caring Makes a Difference , authored by physician-scientists Stephen Trzeciak and Anthony Mazzarelli, has ignited a conversation on the relationship between physician compassion and patient outcomes.
Stanford Medicine’s Emma Seppala discussed the topic with Trzeciak and Mazzarelli in a recent Q&A in the Washington Post . In the interview, the authors share findings on the link between bedside manner and healing. Among the many positive outcomes achieved by demonstrations of physician kindness, they name medication adherence, better achievement of adequate sedation before surgery and a decrease in need for opiate medication post-surgery.
And the proof is in the numbers. PubMed research cited by the Compassionomics authors reinforces their philosophy. When a healthcare provider shows compassion, studies show the following benefits:
· The likelihood that a diabetic patient has optimal blood-sugar control is 80 percent higher and odds are 41 percent lower the patient will experience serious complications related to the disease.
· Patients are less likely to utilize excessive health care services and, on average, have lower medical bills by about 50 percent.
· Patients recover more quickly from the symptom that brought them to the doctor and have fewer visits, tests and referrals. Furthermore, “the proportion of these patients who are referred to specialists is 59 percent lower and diagnostic testing is 84 percent lower.”
Research involving MRI scans further confirms that when a patient experiences “compassion — the action component of trying to alleviate another’s suffering,” a “reward” pathway in the brain is activated. The connection is quite apparent, but as Trzeciak and Mazzarelli emphasize, it’s underestimated throughout the medical community.
So how can physicians actively demonstrate compassion? Mazzarelli names four behaviors that can be practiced at the patient bedside: sitting (versus standing) while speaking; face to face communication with eye contact; taking an active interest in emotional and psychological well-being, and not interrupting. We agree that these exercises, in combination with physical exam skills, are practices vital to improving patient outcomes.
Subscribe to our mailing list
Related pages, teaching humility at the bedside, what can doctors learn from narrative medicine, interview with dr. eric topol (editor-in-chief of medscape), the internet: the elephant in the examination room.
- Dermatology
- Endocrinology
- Extremities
- Gastroenterology/Hepatology
- Gynecology/Women's Health
- Hematology/oncology
- Ophthalmology
- Perspective
- Rheumatology
Compassion in Medicine and Healthcare Research Paper
Introduction.
With scientific and technological progress, the mechanistic approach began to dominate the human touch in modern health care. Following the principles of mind-body dualism, most physicians are inclined to focus on the diseased body and its physiological mechanisms, disregarding the patients’ suffering and psychological conditions. Compassion needs to be reintroduced into modern health care practice for humanizing biomedicine and improving the quality of the provided health care services.
The moral of Christ’s parable about the Good Samaritan
Christ’s lessons about the Good Samaritan can be regarded as an example of human compassion which should be followed by everyone and especially healthcare providers who need to serve the best interests of their patients.
The discussed parable about the Good Samaritan who took care of the victim’s wounds was Jesus’ answer to a question concerning our neighbors. Through Christ’s parable does not answer the question directly, it teaches people how they should behave like neighbors. This lesson is especially valuable for healthcare providers who have the moral obligation to act by the patients’ best interests.
However, in contrast to the man lying on the side of the street whose needs were obvious to the passing Good Samaritan, modern physicians may have difficulties with understanding the needs of their clients. With the pluralism of modern society, morality is the matter of personal preference and most individuals have become moral strangers and black boxes to each other (Welie 1995, 476). Thus, analyzing the application of black-box anthropology for establishing the relationship between healthcare providers and their patients, it can be stated that the principle of distancing to show respect for the patient’s privacy as the primary principle of modern healthcare contradicts the moral of the discussed parable.
Disregarding the present decline in people’s ability to feel compassion, sharing the patients’ feelings and establishing the interpersonal rapport with them is necessary for modern healthcare providers for acting beneficently.
Various definitions of the concept of compassion
Though the concept of compassion has various definitions that make its meaning rather controversial, healthcare practitioners should nurture their ability to feel compassion as one of the greatest virtues.
Analyzing the etymology of the word “compassion”, it can be stated that it originates from the Latin “co-pati” which means “suffer with” (Thomasma and Kushner 1995, 416). The element of suffering which is bad adds shades of a negative meaning to the concept of compassion. However, taking into account its antonyms, including cruelty, indifference, hard-heartedness, it can be logically assumed that compassion is attractive at least by contrast (Comte-Sponville 2009).
By the way, the word sympathy as the synonymic doublet for compassion in modern Romance languages means “fellow feeling” which can be regarded as the more appropriate translation for compassion as well. In general, the definitions of compassion can be divided into two basic subgroups, including those which present compassion as an individual’s ability and willingness to understand person’s suffering by entering deep into his/her situation and those which define compassion as a virtue of willing to alleviate another person’s suffering if it is possible (Dougherty and Purtillo 1995, 427).
Most theoreticians treat the word compassion either as a feeling or as the moral principle and the greatest virtue of humanity. In that regard, the individual cannot be forced to feel compassion, but he/she can nurture their ability to enter the world of another person which would be especially beneficial for medical workers who need to gain knowledge on the best interests of their patients before serving them.
Compassion and medicine
The concept of compassion plays an important role in modern healthcare and has been incorporated even into the official AMA principles of Medical Ethics, saying that a physician has to provide healthcare services with compassion.
Humanizing biomedicine has become the central issue of the modern healthcare industry aimed at overcoming the current quality-of-care crisis. The shift from a mechanistic approach to healthcare in the form of logos (rationality) towards medicine based on pathos (passion) is suggested as a solution for improving the quality of modern Western medicine (Marcum 2008, 399).
Then, instead of using a solely mechanistic approach and viewing the patient’s diseased body as an object, a humane practitioner not only focuses on the inner bodily structure but also empathizes with the patient and takes into account his/her experience of suffering. In that regard, the traditional goals of modern medicine have been updated and complemented with the professional objectives to relieve patients’ suffering from maladies and care for those who cannot be cured for preventing premature death and ensuring peaceful death (“An International Project of the Hastings Center: The Goals of Medicine: Setting New Priorities”).
Integration of compassion as the basic principle of healthcare not only into official manifestations but also into educational programs and professional practice is required for humanizing modern biomedicine and improving the quality of healthcare services.
Compassion and the patient with chronic illness or the dying patient
Disregarding all the benefits of compassion for providing high-quality healthcare services, the issue concerning empathizing patients in all cases as a great challenge and a source of pressure is rather controversial.
In most cases, suffering is subjective and cannot be identified with bodily pain only (Van Hooft 1998). On the one hand, the bodily disease cannot be separated from the overall patient’s condition and modern medicine obtains a more extended view of its mission than mere treatment of physical diseases (Cassell 2004). On the other hand, in particular, situations, when the patients’ claims do not belong to the domain of medicine and cannot be solved through the implementation of healthcare intervention strategies, the doctor should draw the line. For example, the problems of managing the meaning of life and death cannot be handled through medical interventions (Callahan 2004, 101).
There are two levels of human suffering, including those of uncertainty of an ill person if he/she will be able to cope with the disease and the second level which touches upon the links between suffering and the meaning of life itself. Though the struggle against aging and death is a utopian idea, patients’ thoughts about the meaning of life and death can make patients suffer (Callahan 2009). This second level of suffering involves the solution of philosophical and religious issues which are more fundamental than psychological problems, and the physician’s interference into this level would be inappropriate.
Though relieving the suffering of dying patients is one of the central objectives of modern healthcare services, the medical workers cannot handle the issues which are outside the medical domain. It can be stated that compassion can be irrelevant in certain cases with dying patients or patients who have chronic diseases when the problems go beyond the physician’s competence.
Compassion and the physician: a virtue or a duty?
Disregarding the ethical aspect of compassion and taking into account its importance for improving the quality of modern health care services, it should become a duty of every physician.
The main argument which can support the claim that compassion should become every physician’s duty instead of a preferred virtue or an elective element of the physician-patient relationship is the strong link between compassion and physicians’ professional responsibilities (Dougherty and Purtillo 1995, 429). The changes in healthcare educational programs and medicine paradigms need to foster compassion as a part of physicians’ professional duty.
Compassion and ethics
Despite all its benefits and the fact that compassion should be made a part of physicians’ professional duties, it can conflict with other professional responsibilities of an individual physician. For example, compassion to one patient can become a hurdle for identifying and satisfying the needs of other clients. The same goes for the ethical issue of preserving the confidentiality of the patient’s information. In their professional practice, physicians make decisions concerning the appropriateness and usefulness of certain intervention strategies. However, in hard cases, when physicians regard the further treatment as useless, the decision to stop treatment is a real ethical dilemma (Chwang 2009). In general, compassion may require different conduct in various situations and cannot be identified with the rest of the physicians’ professional duties.
Characteristics of a compassionate physician
The main characteristics of a compassionate physician include the ability to obtain a humane gaze upon their patients and take into account the experience of suffering for providing high-quality health care services. A compassionate physician can establish interpersonal rapport with patients, obtain knowledge on their experience of suffering including not only physical but also psychological pain and find the most appropriate strategies for alleviating the patients’ suffering.
Another significant side is the prevention of futile treatment, taking into account the following patients’ disillusionment. Thus, in case if the treatment is not likely to work, a compassionate doctor will never prescribe it (Ten Have and Janssens, 2002, 213). Recognizing compassion as a significant element of their professional duties, compassionate physicians manage to reach a compromise between their empathy with an individual patient and the rest of their professional duties and use rational consideration for making the most appropriate professional decisions.
Benefits of compassion
Integration of compassion as one of the significant physician’s duties into the modern health care paradigm would be beneficial for humanizing biomedicine and improving the quality of the provided services. Compassion can provide a source of motivation for alleviating the patients’ suffering (Crisp, 2008, 245). Recognizing the fact that psychological conditions can have a significant impact on the patient’s overall well-being, physicians cannot separate mental suffering from the patients’ bodily pain. The main advantage of compassion for modern medicine is an opportunity to extend the mechanistic biomedical approach by taking into account the aspects of the patients’ feelings and implementing a complex approach to treatment.
Barriers to compassion
Though the benefits of making compassion one of physicians’ professional duties may seem obvious, there are certain barriers to implementing this approach in healthcare practice. First of them is the perception of compassion as a source of suffering for physicians and their natural willingness to avoid it. However, rejecting compassion, physicians deprive themselves of opportunities to develop their professional skills and see the gratitude of their clients because the interpersonal rapport is responsible for not only negative but also positive implications. “They will miss the experience of human openness and vulnerability and the chance to experience unconditional love and the power of human connection” (Connelly, 2009, 386). Physicians need to overcome the barriers to compassion for implementing a complex approach to treatment and improving the quality of healthcare services.
Teaching of compassion
Taking into account the fact that the inability to feel compassion and share emotions can harm not only physicians’ competence but also their well-being. Not responding to suffering and not acknowledging their emotions, physicians put at risk not only the quality of healthcare but even their wellbeing (Connelly, 2009, 386). It explains the importance of teaching compassion. The doctor-patient interpersonal relationship presupposes a high level of confidentiality and vulnerability. For this reason, the teaching of compassion and developing skills of finding rational consideration for selecting the most appropriate strategies are recognized as lifetime learning. Learning to recognize their emotions and respond to suffering is significant for improving the quality of healthcare services and physicians’ well-being.
In general, taking into account the drawbacks of the mechanistic approach to treatment and the integrity of physiological and psychological processes, it can be concluded that compassion should be reintroduced into healthcare educational programs and practice. As one of the physician’s professional responsibilities, compassion requires different conduct in various situations and rational consideration for selecting the most appropriate intervention strategies for improving the quality of the provided services as well as physicians’ wellbeing.
Reference List
“An International Project of the Hastings Center: The Goals of Medicine: Setting New Priorities”. Hastings Center Report 26(1996): S 1-27.
Callahan, Daniel. “Death, mourning, and medical progress”. Perspectives in Biology and Medicine 52(2009): 103-115.
Callahan, Daniel. The Troubled Dream of Life: In Search of a Peaceful Death . Georgetown University Press, 2004.
Cassell, Eric. The Nature of Suffering and the Goals of Medicine . New York: Oxford University Press, 2004.
Chwang, Eric. “Futility Clarified”. Journal of Law, Medicine & Ethics 2009: 487-495.
Comte-Sponville, André. “Compassion”, in Comte-Sponville, André. A Small Treatise on the Great Virtues . New York: Henry Holt & Company, 2001: 103-117.
Connelly, Julia. “The Avoidance of Human Suffering”. Perspectives in Biology and Medicine 52(2009): 381-391.
Crisp, Roger. “Compassion and Beyond”. Ethical Theory and Moral Practice 11 (2008): 233-246.
Dougherty, Charles and Ruth Purtilo: “Physicians’ Duty of Compassion”. Cambridge Quarterly of Healthcare Ethics 4 (1995): 426-433.
Marcum, James. “Reflections on Humanizing Biomedicine”. Perspectives in Biology and Medicine 51 (2008): 392-405.
Ten Have, Henk and Rien Janssens. “Futility, Limits and Palliative Care” in Ten Have, Henk and David Clark (eds.): The Ethics of Palliative Care. Buckingham: Open University Press, 2002.
Thomasma, David and Tomasine Kushner. “A dialogue on Compassion and Supererogation in Medicine”. Cambridge Quarterly of Healthcare Ethics 1995: 415-425.
Van Hooft, Stan. “The Meanings of Suffering”. Hastings Center Report 28(1998): 13-19.
Welie, Jos. “Sympathy as the Basis of Compassion”. Cambridge Quarterly of Healthcare Ethics 4 (1995): 476-487.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2020, July 24). Compassion in Medicine and Healthcare. https://ivypanda.com/essays/compassion-in-medicine-and-healthcare/
"Compassion in Medicine and Healthcare." IvyPanda , 24 July 2020, ivypanda.com/essays/compassion-in-medicine-and-healthcare/.
IvyPanda . (2020) 'Compassion in Medicine and Healthcare'. 24 July.
IvyPanda . 2020. "Compassion in Medicine and Healthcare." July 24, 2020. https://ivypanda.com/essays/compassion-in-medicine-and-healthcare/.
1. IvyPanda . "Compassion in Medicine and Healthcare." July 24, 2020. https://ivypanda.com/essays/compassion-in-medicine-and-healthcare/.
Bibliography
IvyPanda . "Compassion in Medicine and Healthcare." July 24, 2020. https://ivypanda.com/essays/compassion-in-medicine-and-healthcare/.
- Organic and Mechanistic Organizational Structures
- Mechanistic vs Human Relations Management
- Mechanistic vs. Organic Organizational Structure
- Compassionate Nursing Care and Its Perception
- Structural-Mechanistic vs. Organic-Humanistic Organization
- Compassion in Relation to Goals of Medicine and Healthcare
- "Compassionate Communication in Patient Care" by Engel
- Compassion in Healthcare Setting
- Caring and Compassionate Experience in Nursing
- The Risk of Compassion Fatigue in Medicine
- Ethical Issues in International Medical Research
- Biomedical Ethical Theories and Principles
- Normative Methods in Healthcare Ethics
- Truth-Telling/Confidentiality in Medical Practice
- Ethics and Deception in Psychological Research
Compassionomics: The Science and Practice of Caring
Affiliations.
- 1 From the Massachusetts Eye and Ear (I.L.), Department of Ophthalmology, Harvard Medical School, Boston, Massachusetts.
- 2 University of Utah School of Medicine (T.J.J.), Salt Lake City, Utah.
- 3 W.K. Kellogg Eye Center (M.W.J.), Department of Ophthalmology and Visual Sciences, University of Michigan, Ann Arbor, Michigan, USA. Electronic address: [email protected].
- PMID: 37923101
- DOI: 10.1016/j.ajo.2023.10.006
Purpose: To summarize the scientific evidence that compassion can measurably improve patient outcomes, health care quality and safety, and the well-being of health care providers, and to consider specific strategies for cultivating compassion and better communicating it to patients.
Design: Perspective.
Methods: We selectively reviewed the literature on compassion in health care, including obstacles to its expression and the demonstrated effects of provider compassion on patient outcomes, health care quality and cost, and provider well-being. We also review evidence regarding the trainability of compassion, discuss proven methods for cultivating individual compassion, and recommend strategies for incorporating it into routine medical practice.
Results: Compassion is the emotional response to another's pain or suffering, accompanied by a desire to alleviate it. Review of the literature shows that compassionate health care measurably improves physical and psychological patient outcomes, increases patient adherence, improves health care quality and safety, increases financial margins, and prevents physician burnout. Psychophysiological research shows that empathy and compassion can be actively cultivated through intentional practice. Validated models of compassion-based interactions can facilitate the consistent expression of compassion in daily medical practice.
Conclusions: Given its many proven benefits to patients, health care organizations, and providers, compassion should be cultivated by health care providers and systems and considered an essential component of optimal medical care.
Copyright © 2023 Elsevier Inc. All rights reserved.
Publication types
- Delivery of Health Care*
- Health Personnel
- Physicians*
Med School Applicants Should Highlight Compassion
Show admissions committees that you are committed to increasing your level of compassion as an aspiring doctor.
Premeds and Compassion in Medicine

Getty Images
Compassion is important because it's comforting to know our health care providers can relate to us when we are going through an illness.
Compassion is an important concept in medicine. This is why it is frequently discussed in medical school applications. However, compassion often is used as a buzzword without sufficient attention to what it really means and why it is so important.
Bad Signals Med School Applicants Send
Azadeh Salek, M.D. June 30, 2020

For aspiring physicians, it is worthwhile to understand what compassion means and its role in providing medical care. By taking time to think about the concept in more depth, med school applicants can write about compassion more effectively in their applications and discuss it in a more sophisticated fashion in their medical school interviews .
What Is Compassion in Medicine?
When we ask students to define compassion, we often get varied responses. Even health care providers who may have a strong grasp of the concept sometimes have difficulty expressing it in a tangible way.
A study published in the International Journal of Palliative Nursing in 2016 sought to define compassion in the context of health care by reviewing previous literature written on the topic. Not surprisingly, the investigators found that in medical literature, compassion was defined in different ways by different authors.
However, some common themes emerged from the study. Its authors examined the themes and distilled compassion into several elements. One is the ability to show sensitivity or to understand another person’s pain. In this way, they argued, compassion is similar to empathy .
However, according to the authors, there is another element to compassion that goes beyond empathy – the desire to go out of one’s way to help a suffering person. Other experts have argued that in the context of health care, compassion also involves effectively communicating with patients.
Compassion needs to be distinguished from pity because compassion is a positive attribute that comes from generosity and a desire to connect with others. Pity, on the other hand, is considered a negative emotion. One who is compassionate toward another person sees the other person as equal. By contrast, someone who feels pity for another person views the other person with condescension.
Why Is Compassion Important in Medicine?
This may seem like an obvious question. After all, most of us want to feel cared for when we experience difficulty. It is comforting to know that when we are going through an illness, our care providers can relate to us, put themselves in our shoes and do everything in their power to help us.
But beyond these self-evident reasons, there is another argument for why compassion matters. It turns out that providing compassionate medical care may lead to better patient outcomes.
Some experts argue that compassion leads patients to adhere more to medical treatments. A patient with high blood pressure , for example, may be more inclined to take his blood pressure medication regularly if he feels that his physician is compassionate.
Studies have shown that patients with diabetes whose physicians were more empathetic tended to achieve better blood sugar and blood cholesterol levels. Other examples abound in medical literature showing that compassion can improve patient care, and premed students are encouraged to go beyond this article to explore the topic.
How Can Compassion Be Acquired?
A common misconception is that compassion cannot be learned, that it is something a person either possesses or does not. However, research in this area suggests otherwise. Studies have shown that empathy, a component of compassion, can be increased through training. There is also biological evidence that training people to be compassionate may lead to positive changes in neural network activity in the brain.
Different approaches have been proposed for increasing compassion. For example, some research demonstrates a role for mindfulness meditation programs. When a group of college students were randomly assigned to either three weeks of a self-guided mindfulness meditation regimen or to a program that improved cognitive skills, those in the mindfulness meditation group displayed greater compassion toward others after the program.
To increase compassion, students should take part in service-based activities. This idea is also backed by research. For example, in a study of nursing students published in Nurse Education in Practice in 2018, participation in an activity to provide service to populations experiencing homelessness resulted in greater levels of empathy and improved attitudes toward the challenges that homeless people face.
By getting involved in community service projects where you can help those in need or working at a clinic where you can assist underserved populations with medical care, you will learn about the challenges that others face, develop greater sensitivity and become more motivated to serve. In doing so, you can show medical school admissions committees that you are striving to increase your level of compassion, in turn making you a better candidate for med school.
When writing about compassion in medical school applications as an aspiring physician, strive to explain what compassion means to you and draw on examples where you have seen compassion at play. Most importantly, view compassion as a skill that you can build on over the course of your training and your future career so that you can constantly improve the quality of care you provide to patients.
Where Famous Docs Earned Medical Degrees

Tags: medical school , graduate schools , students , education , doctors
About Medical School Admissions Doctor
Need a guide through the murky medical school admissions process? Medical School Admissions Doctor offers a roundup of expert and student voices in the field to guide prospective students in their pursuit of a medical education. The blog is currently authored by Dr. Ali Loftizadeh, Dr. Azadeh Salek and Zach Grimmett at Admissions Helpers , a provider of medical school application services; Dr. Renee Marinelli at MedSchoolCoach , a premed and med school admissions consultancy; Dr. Rachel Rizal, co-founder and CEO of the Cracking Med School Admissions consultancy; Dr. Cassie Kosarec at Varsity Tutors , an advertiser with U.S. News & World Report; Dr. Kathleen Franco, a med school emeritus professor and psychiatrist; and Liana Meffert, a fourth-year medical student at the University of Iowa's Carver College of Medicine and a writer for Admissions Helpers. Got a question? Email [email protected] .
Popular Stories
Paying for Graduate School

Medical School Admissions Doctor

Best Graduate Schools

Law Admissions Lowdown

Applying to Graduate School

You May Also Like
Mba scholarships.
Sammy Allen April 4, 2024
Special Master's Programs and Med School
Renee Marinelli, M.D. April 2, 2024
15 Famous Fulbright Scholars
Cole Claybourn April 1, 2024
When to Expect Law School Decisions
Gabriel Kuris April 1, 2024
How to Decide if an MBA Is Worth it
Sarah Wood March 27, 2024
Choosing A Major for Med School
Andrew Bauld March 26, 2024

Handling a Law School Rejection Letter
Gabriel Kuris March 25, 2024

College Majors and MBA Admissions
Anthony Todd Carlisle March 20, 2024

Tips While Awaiting Med School Decision
Zach Grimmett March 19, 2024

2024 Best Grad Schools Rankings Coming
Robert Morse and Eric Brooks March 19, 2024

Home — Essay Samples — Life — Compassion — Importance Of My Passion For Medicine

Importance of My Passion for Medicine
- Categories: Compassion
About this sample

Words: 677 |
Published: Mar 25, 2024
Words: 677 | Page: 1 | 4 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Heisenberg
Verified writer
- Expert in: Life

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 579 words
2 pages / 873 words
4 pages / 1989 words
4.5 pages / 2031 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Compassion
Charity, with its far-reaching impact, stands as a beacon of hope in a world facing multifaceted challenges. This essay delves into the profound importance of charity in fostering positive social change, emphasizing its role in [...]
Mother Teresa, a name that resonates with compassion, selflessness, and tireless dedication to serving the poorest of the poor. Born on August 26, 1910, in Skopje, now the capital of North Macedonia, Mother Teresa's life [...]
Receiving is often regarded as an essential aspect of human interactions, yet it stands in the shadow of the more celebrated act of giving. This essay delves into the dynamics of giving and receiving, examining the emotional, [...]
In the grand symphony of life, pediatrics stands as a testament to the power of compassion, growth, advocacy, teamwork, and discovery. As I embark on this noble journey, I am steadfast in my commitment to becoming a pediatrician [...]
When it involves education, reading, writing, and arithmetic, accustomed take center stage and were the quality menu of what was instructed to students beginning in school. In today’s world of education, wherever students area [...]
“On Compassion” is an essay written by Barbara Lazear Ascher. The main argument of Ascher's piece deals with acts of compassion, as well as the motives behind them. Ascher utilizes a somber tone, being a third party observer. [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
10 Successful Medical School Essays
Sponsored by.

-- Accepted to: Harvard Medical School GPA: 4.0 MCAT: 522
Sponsored by A ccepted.com : Great stats don’t assure acceptance to elite medical schools. The personal statement, most meaningful activities, activity descriptions, secondaries and interviews can determine acceptance or rejection. Since 1994, Accepted.com has guided medical applicants just like you to present compelling medical school applications. Get Accepted !
I started writing in 8th grade when a friend showed me her poetry about self-discovery and finding a voice. I was captivated by the way she used language to bring her experiences to life. We began writing together in our free time, trying to better understand ourselves by putting a pen to paper and attempting to paint a picture with words. I felt my style shift over time as I grappled with challenges that seemed to defy language. My poems became unstructured narratives, where I would use stories of events happening around me to convey my thoughts and emotions. In one of my earliest pieces, I wrote about a local boy’s suicide to try to better understand my visceral response. I discussed my frustration with the teenage social hierarchy, reflecting upon my social interactions while exploring the harms of peer pressure.
In college, as I continued to experiment with this narrative form, I discovered medical narratives. I have read everything from Manheimer’s Bellevue to Gawande’s Checklist and from Nuland’s observations about the way we die, to Kalanithi’s struggle with his own decline. I even experimented with this approach recently, writing a piece about my grandfather’s emphysema. Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love. I have augmented these narrative excursions with a clinical bioethics internship. In working with an interdisciplinary team of ethics consultants, I have learned by doing by participating in care team meetings, synthesizing discussions and paths forward in patient charts, and contributing to an ongoing legislative debate addressing the challenges of end of life care. I have also seen the ways ineffective intra-team communication and inter-personal conflicts of beliefs can compromise patient care.
Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love.
By assessing these difficult situations from all relevant perspectives and working to integrate the knowledge I’ve gained from exploring narratives, I have begun to reflect upon the impact the humanities can have on medical care. In a world that has become increasingly data driven, where patients can so easily devolve into lists of numbers and be forced into algorithmic boxes in search of an exact diagnosis, my synergistic narrative and bioethical backgrounds have taught me the importance of considering the many dimensions of the human condition. I am driven to become a physician who deeply considers a patient’s goal of care and goals of life. I want to learn to build and lead patient care teams that are oriented toward fulfilling these goals, creating an environment where family and clinician conflict can be addressed efficiently and respectfully. Above all, I look forward to using these approaches to keep the person beneath my patients in focus at each stage of my medical training, as I begin the task of translating complex basic science into excellent clinical care.
In her essay for medical school, Morgan pitches herself as a future physician with an interdisciplinary approach, given her appreciation of how the humanities can enable her to better understand her patients. Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient’s humanity at the center of her approach to clinical care.
This narrative distinguishes Morgan as a candidate for medical school effectively, as she provides specific examples of how her passions intersect with medicine. She first discusses how she used poetry to process her emotional response to a local boy’s suicide and ties in concern about teenage mental health. Then, she discusses more philosophical questions she encountered through reading medical narratives, which demonstrates her direct interest in applying writing and the humanities to medicine. By making the connection from this larger theme to her own reflections on her grandfather, Morgan provides a personal insight that will give an admissions officer a window into her character. This demonstrates her empathy for her future patients and commitment to their care.
Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient's humanity at the center of her approach to clinical care.
Furthermore, it is important to note that Morgan’s essay does not repeat anything in-depth that would otherwise be on her resume. She makes a reference to her work in care team meetings through a clinical bioethics internship, but does not focus on this because there are other places on her application where this internship can be discussed. Instead, she offers a more reflection-based perspective on the internship that goes more in-depth than a resume or CV could. This enables her to explain the reasons for interdisciplinary approach to medicine with tangible examples that range from personal to professional experiences — an approach that presents her as a well-rounded candidate for medical school.
Disclaimer: With exception of the removal of identifying details, essays are reproduced as originally submitted in applications; any errors in submissions are maintained to preserve the integrity of the piece. The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this article.
-- Accepted To: A medical school in New Jersey with a 3% acceptance rate. GPA: 3.80 MCAT: 502 and 504
Sponsored by E fiie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
"To know even one life has breathed easier because you have lived. This is to have succeeded." – Ralph Waldo Emerson.
The tribulations I've overcome in my life have manifested in the compassion, curiosity, and courage that is embedded in my personality. Even a horrific mishap in my life has not changed my core beliefs and has only added fuel to my intense desire to become a doctor. My extensive service at an animal hospital, a harrowing personal experience, and volunteering as an EMT have increased my appreciation and admiration for the medical field.
At thirteen, I accompanied my father to the Park Home Animal Hospital with our eleven-year-old dog, Brendan. He was experiencing severe pain due to an osteosarcoma, which ultimately led to the difficult decision to put him to sleep. That experience brought to light many questions regarding the idea of what constitutes a "quality of life" for an animal and what importance "dignity" plays to an animal and how that differs from owner to owner and pet to pet. Noting my curiosity and my relative maturity in the matter, the owner of the animal hospital invited me to shadow the professional staff. Ten years later, I am still part of the team, having made the transition from volunteer to veterinarian technician. Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
As my appreciation for medical professionals continued to grow, a horrible accident created an indelible moment in my life. It was a warm summer day as I jumped onto a small boat captained by my grandfather. He was on his way to refill the boat's gas tank at the local marina, and as he pulled into the dock, I proceeded to make a dire mistake. As the line was thrown from the dock, I attempted to cleat the bowline prematurely, and some of the most intense pain I've ever felt in my life ensued.
Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
"Call 911!" I screamed, half-dazed as I witnessed blood gushing out of my open wounds, splashing onto the white fiberglass deck of the boat, forming a small puddle beneath my feet. I was instructed to raise my hand to reduce the bleeding, while someone wrapped an icy towel around the wound. The EMTs arrived shortly after and quickly drove me to an open field a short distance away, where a helicopter seemed to instantaneously appear.
The medevac landed on the roof of Stony Brook Hospital before I was expeditiously wheeled into the operating room for a seven-hour surgery to reattach my severed fingers. The distal phalanges of my 3rd and 4th fingers on my left hand had been torn off by the rope tightening on the cleat. I distinctly remember the chill from the cold metal table, the bright lights of the OR, and multiple doctors and nurses scurrying around. The skill and knowledge required to execute multiple skin graft surgeries were impressive and eye-opening. My shortened fingers often raise questions by others; however, they do not impair my self-confidence or physical abilities. The positive outcome of this trial was the realization of my intense desire to become a medical professional.
Despite being the patient, I was extremely impressed with the dedication, competence, and cohesiveness of the medical team. I felt proud to be a critical member of such a skilled group. To this day, I still cannot explain the dichotomy of experiencing being the patient, and concurrently one on the professional team, committed to saving the patient. Certainly, this experience was a defining part of my life and one of the key contributors to why I became an EMT and a volunteer member of the Sample Volunteer Ambulance Corps. The startling ring of the pager, whether it is to respond to an inebriated alcoholic who is emotionally distraught or to help bring breath to a pulseless person who has been pulled from the family swimming pool, I am committed to EMS. All of these events engender the same call to action and must be reacted to with the same seriousness, intensity, and magnanimity. It may be some routine matter or a dire emergency; this is a role filled with uncertainty and ambiguity, but that is how I choose to spend my days. My motives to become a physician are deeply seeded. They permeate my personality and emanate from my desire to respond to the needs of others. Through a traumatic personal event and my experiences as both a professional and volunteer, I have witnessed firsthand the power to heal the wounded and offer hope. Each person defines success in different ways. To know even one life has been improved by my actions affords me immense gratification and meaning. That is success to me and why I want to be a doctor.
This review is provided by EFIIE Consulting Group’s Pre-Health Senior Consultant Jude Chan
This student was a joy to work with — she was also the lowest MCAT profile I ever accepted onto my roster. At 504 on the second attempt (502 on her first) it would seem impossible and unlikely to most that she would be accepted into an allopathic medical school. Even for an osteopathic medical school this score could be too low. Additionally, the student’s GPA was considered competitive at 3.80, but it was from a lower ranked, less known college, so naturally most advisors would tell this student to go on and complete a master’s or postbaccalaureate program to show that she could manage upper level science classes. Further, she needed to retake the MCAT a third time.
However, I saw many other facets to this student’s history and life that spoke volumes about the type of student she was, and this was the positioning strategy I used for her file. Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA. Although many students have greater MCAT scores than 504 and higher GPAs than 3.80, I have helped students with lower scores and still maintained our 100% match rate. You are competing with thousands of candidates. Not every student out there requires our services and we are actually grateful that we can focus on a limited amount out of the tens of thousands that do. We are also here for the students who wish to focus on learning well the organic chemistry courses and physics courses and who want to focus on their research and shadowing opportunities rather than waste time deciphering the next step in this complex process. We tailor a pathway for each student dependent on their health care career goals, and our partnerships with non-profit organizations, hospitals, physicians and research labs allow our students to focus on what matters most — the building up of their basic science knowledge and their exposure to patients and patient care.
Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA.
Even students who believe that their struggle somehow disqualifies them from their dream career in health care can be redeemed if they are willing to work for it, just like this student with 502 and 504 MCAT scores. After our first consult, I saw a way to position her to still be accepted into an MD school in the US — I would not have recommended she register to our roster if I did not believe we could make a difference. Our rosters have a waitlist each semester, and it is in our best interest to be transparent with our students and protect our 100% record — something I consider a win-win. It is unethical to ever guarantee acceptance in admissions as we simply do not control these decisions. However, we respect it, play by the rules, and help our students stay one step ahead by creating an applicant profile that would be hard for the schools to ignore.
This may be the doctor I go to one day. Or the nurse or dentist my children or my grandchildren goes to one day. That is why it is much more than gaining acceptance — it is about properly matching the student to the best options for their education. Gaining an acceptance and being incapable of getting through the next 4 or 8 years (for my MD/PhD-MSTP students) is nonsensical.
-- Accepted To: Imperial College London UCAT Score: 2740 BMAT Score: 3.9, 5.4, 3.5A
My motivation to study Medicine stems from wishing to be a cog in the remarkable machine that is universal healthcare: a system which I saw first-hand when observing surgery in both the UK and Sri Lanka. Despite the differences in sanitation and technology, the universality of compassion became evident. When volunteering at OSCE training days, I spoke to many medical students, who emphasised the importance of a genuine interest in the sciences when studying Medicine. As such, I have kept myself informed of promising developments, such as the use of monoclonal antibodies in cancer therapy. After learning about the role of HeLa cells in the development of the polio vaccine in Biology, I read 'The Immortal Life of Henrietta Lacks' to find out more. Furthermore, I read that surface protein CD4 can be added to HeLa cells, allowing them to be infected with HIV, opening the possibility of these cells being used in HIV research to produce more life-changing drugs, such as pre-exposure prophylaxis (PreP). Following my BioGrad laboratory experience in HIV testing, and time collating data for research into inflammatory markers in lung cancer, I am also interested in pursuing a career in medical research. However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude. As the surgeon explained that the cancer had metastasised to her liver, I watched him empathetically tailor his language for the patient - he avoided medical jargon and instead gave her time to come to terms with this. I have been developing my communication skills by volunteering weekly at care homes for 3 years, which has improved my ability to read body language and structure conversations to engage with the residents, most of whom have dementia.
However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude.
Jude’s essay provides a very matter-of-fact account of their experience as a pre-medical student. However, they deepen this narrative by merging two distinct cultures through some common ground: a universality of compassion. Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
From their OSCE training days to their school’s Science society, Jude connects their analytical perspective — learning about HeLa cells — to something that is relatable and human, such as a poor farmer’s notable contribution to science. This approach provides a gateway into their moral compass without having to explicitly state it, highlighting their fervent desire to learn how to interact and communicate with others when in a position of authority.
Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
Jude’s closing paragraph reminds the reader of the similarities between two countries like the UK and Sri Lanka, and the importance of having a universal healthcare system that centers around the just and “world-class” treatment of patients. Overall, this essay showcases Jude’s personal initiative to continue to learn more and do better for the people they serve.
While the essay could have benefited from better transitions to weave Jude’s experiences into a personal story, its strong grounding in Jude’s motivation makes for a compelling application essay.
-- Accepted to: Weill Cornell Medical College GPA: 3.98 MCAT: 521
Sponsored by E fie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
Following the physician’s unexpected request, we waited outside, anxiously waiting to hear the latest update on my father’s condition. It was early on in my father’s cancer progression – a change that had shaken our entire way of life overnight. During those 18 months, while my mother spent countless nights at the hospital, I took on the responsibility of caring for my brother. My social life became of minimal concern, and the majority of my studying for upcoming 12th- grade exams was done at the hospital. We were allowed back into the room as the physician walked out, and my parents updated us on the situation. Though we were a tight-knit family and my father wanted us to be present throughout his treatment, what this physician did was give my father a choice. Without making assumptions about who my father wanted in the room, he empowered him to make that choice independently in private. It was this respect directed towards my father, the subsequent efforts at caring for him, and the personal relationship of understanding they formed, that made the largest impact on him. Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
It was during this period that I became curious about the human body, as we began to learn physiology in more depth at school. In previous years, the problem-based approach I could take while learning math and chemistry were primarily what sparked my interest. However, I became intrigued by how molecular interactions translated into large-scale organ function, and how these organ systems integrated together to generate the extraordinary physiological functions we tend to under-appreciate. I began my undergraduate studies with the goal of pursuing these interests, whilst leaning towards a career in medicine. While I was surprised to find that there were upwards of 40 programs within the life sciences that I could pursue, it broadened my perspective and challenged me to explore my options within science and healthcare. I chose to study pathobiology and explore my interests through hospital volunteering and research at the end of my first year.
Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
While conducting research at St. Michael’s Hospital, I began to understand methods of data collection and analysis, and the thought process of scientific inquiry. I became acquainted with the scientific literature, and the experience transformed how I thought about the concepts I was learning in lecture. However, what stood out to me that summer was the time spent shadowing my supervisor in the neurosurgery clinic. It was where I began to fully understand what life would be like as a physician, and where the career began to truly appeal to me. What appealed to me most was the patient-oriented collaboration and discussions between my supervisor and his fellow; the physician-patient relationship that went far beyond diagnoses and treatments; and the problem solving that I experienced first-hand while being questioned on disease cases.
The day spent shadowing in the clinic was also the first time I developed a relationship with a patient. We were instructed to administer the Montreal cognitive assessment (MoCA) test to patients as they awaited the neurosurgeon. My task was to convey the instructions as clearly as possible and score each section. I did this as best I could, adapting my explanation to each patient, and paying close attention to their responses to ensure I was understood. The last patient was a challenging case, given a language barrier combined with his severe hydrocephalus. It was an emotional time for his family, seeing their father/husband struggle to complete simple tasks and subsequently give up. I encouraged him to continue trying. But I also knew my words would not remedy the condition underlying his struggles. All I could do was make attempts at lightening the atmosphere as I got to know him and his family better. Hours later, as I saw his remarkable improvement following a lumbar puncture, and the joy on his and his family’s faces at his renewed ability to walk independently, I got a glimpse of how rewarding it would be to have the ability and privilege to care for such patients. By this point, I knew I wanted to commit to a life in medicine. Two years of weekly hospital volunteering have allowed me to make a small difference in patients’ lives by keeping them company through difficult times, and listening to their concerns while striving to help in the limited way that I could. I want to have the ability to provide care and treatment on a daily basis as a physician. Moreover, my hope is that the breadth of medicine will provide me with the opportunity to make an impact on a larger scale. Whilst attending conferences on neuroscience and surgical technology, I became aware of the potential to make a difference through healthcare, and I look forward to developing the skills necessary to do so through a Master’s in Global Health. Whether through research, health innovation, or public health, I hope not only to care for patients with the same compassion with which physicians cared for my father, but to add to the daily impact I can have by tackling large-scale issues in health.
Taylor’s essay offers both a straightforward, in-depth narrative and a deep analysis of his experiences, which effectively reveals his passion and willingness to learn in the medical field. The anecdote of Taylor’s father gives the reader insight into an original instance of learning through experience and clearly articulates Taylor’s motivations for becoming a compassionate and respectful physician.
Taylor strikes an impeccable balance between discussing his accomplishments and his character. All of his life experiences — and the difficult challenges he overcame — introduce the reader to an important aspect of Taylor’s personality: his compassion, care for his family, and power of observation in reflecting on the decisions his father’s doctor makes. His description of his time volunteering at St. Michael’s Hospital is indicative of Taylor’s curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship. Moreover, he shows how his volunteer work enabled him to see how medicine goes “beyond diagnoses and treatments” — an observation that also speaks to his compassion.
His description of his time volunteering at St. Michael's Hospital is indicative of Taylor's curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship.
Finally, Taylor also tells the reader about his ambition and purpose, which is important when thinking about applying to medical school. He discusses his hope of tackling larger scale problems through any means possible in medicine. This notion of using self interest to better the world is imperative to a successful college essay, and it is nicely done here.
-- Accepted to: Washington University
Sponsored by A dmitRx : We are a group of Chicago-based medical students who realize how challenging medical school admissions can be, so we want to provide our future classmates with resources we wish we had. Our mission at AdmitRx is to provide pre-medical students with affordable, personalized, high-quality guidance towards becoming an admitted medical student.
Running has always been one of my greatest passions whether it be with friends or alone with my thoughts. My dad has always been my biggest role model and was the first to introduce me to the world of running. We entered races around the country, and one day he invited me on a run that changed my life forever. The St. Jude Run is an annual event that raises millions of dollars for St. Jude Children’s Research Hospital. My dad has led or our local team for as long as I can remember, and I had the privilege to join when I was 16. From the first step I knew this was the environment for me – people from all walks of life united with one goal of ending childhood cancer. I had an interest in medicine before the run, and with these experiences I began to consider oncology as a career. When this came up in conversations, I would invariably be faced with the question “Do you really think you could get used to working with dying kids?” My 16-year-old self responded with something noble but naïve like “It’s important work, so I’ll have to handle it”. I was 16 years young with my plan to become an oncologist at St. Jude.
As I transitioned into college my plans for oncology were alive and well. I began working in a biochemistry lab researching new anti-cancer drugs. It was a small start, but I was overjoyed to be a part of the process. I applied to work at a number of places for the summer, but the Pediatric Oncology Education program (POE) at St. Jude was my goal. One afternoon, I had just returned from class and there it was: an email listed as ‘POE Offer’. I was ecstatic and accepted the offer immediately. Finally, I could get a glimpse at what my future holds. My future PI, Dr. Q, specialized in solid tumor translational research and I couldn’t wait to get started.
I was 16 years young with my plan to become an oncologist at St. Jude.
Summer finally came, I moved to Memphis, and I was welcomed by the X lab. I loved translational research because the results are just around the corner from helping patients. We began a pre-clinical trial of a new chemotherapy regimen and the results were looking terrific. I was also able to accompany Dr. Q whenever she saw patients in the solid tumor division. Things started simple with rounds each morning before focusing on the higher risk cases. I was fortunate enough to get to know some of the patients quite well, and I could sometimes help them pass the time with a game or two on a slow afternoon between treatments. These experiences shined a very human light on a field I had previously seen only through a microscope in a lab.
I arrived one morning as usual, but Dr. Q pulled me aside before rounds. She said one of the patients we had been seeing passed away in the night. I held my composure in the moment, but I felt as though an anvil was crushing down on me. It was tragic but I knew loss was part of the job, so I told myself to push forward. A few days later, I had mostly come to terms with what happened, but then the anvil came crashing back down with the passing of another patient. I could scarcely hold back the tears this time. That moment, it didn’t matter how many miraculous successes were happening a few doors down. Nothing overshadowed the loss, and there was no way I could ‘get used to it’ as my younger self had hoped.
I was still carrying the weight of what had happened and it was showing, so I asked Dr. Q for help. How do you keep smiling each day? How do you get used to it? The questions in my head went on. What I heard next changed my perspective forever. She said you keep smiling because no matter what happened, you’re still hope for the next patient. It’s not about getting used to it. You never get used to it and you shouldn’t. Beating cancer takes lifetimes, and you can’t look passed a life’s worth of hardships. I realized that moving passed the loss of patients would never suffice, but I need to move forward with them. Through the successes and shortcomings, we constantly make progress. I like to imagine that in all our future endeavors, it is the hands of those who have gone before us that guide the way. That is why I want to attend medical school and become a physician. We may never end the sting of loss, but physicians are the bridge between the past and the future. No where else is there the chance to learn from tragedy and use that to shape a better future. If I can learn something from one loss, keep moving forward, and use that knowledge to help even a single person – save one life, bring a moment of joy, avoid a moment of pain—then that is how I want to spend my life.
The change wasn’t overnight. The next loss still brought pain, but I took solace in moving forward so that we might learn something to give hope to a future patient. I returned to campus in a new lab doing cancer research, and my passion for medicine continues to flourish. I still think about all the people I encountered at St. Jude, especially those we lost. It might be a stretch, but during the long hours at the lab bench I still picture their hands moving through mine each step of the way. I could never have foreseen where the first steps of the St. Jude Run would bring me. I’m not sure where the road to becoming a physician may lead, but with helping hands guiding the way, I won’t be running it alone.
This essay, a description of the applicant’s intellectual challenges, displays the hardships of tending to cancer patients as a milestone of experience and realization of what it takes to be a physician. The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional. In this way, the applicant gives the reader some insight into the applicant’s mindset, and their ability to think beyond the surface for ways to become better at what they do.
However, the essay fails to zero in on the applicant’s character, instead elaborating on life events that weakly illustrate the applicant’s growth as a physician. The writer’s mantra (“keep moving forward”) is feebly projected, and seems unoriginal due to the lack of a personalized connection between the experience at St. Jude and how that led to the applicant’s growth and mindset changes.
The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional.
The writer, by only focusing on grief brought from patient deaths at St. Jude, misses out on the opportunity to further describe his or her experience at the hospital and portray an original, well-rounded image of his or her strengths, weaknesses, and work ethic.
The applicant ends the essay by attempting to highlight the things they learned at St. Jude, but fails to organize the ideas into a cohesive, comprehensible section. These ideas are also too abstract, and are vague indicators of the applicant’s character that are difficult to grasp.
-- Accepted to: New York University School of Medicine
Sponsored by MedEdits : MedEdits Medical Admissions has been helping applicants get into medical schools like Harvard for more than ten years. Structured like an academic medical department, MedEdits has experts in admissions, writing, editing, medicine, and interview prep working with you collaboratively so you can earn the best admissions results possible.
“Is this the movie you were talking about Alice?” I said as I showed her the movie poster on my iPhone. “Oh my God, I haven’t seen that poster in over 70 years,” she said with her arms trembling in front of her. Immediately, I sat up straight and started to question further. We were talking for about 40 minutes, and the most exciting thing she brought up in that time was the new flavor of pudding she had for lunch. All of sudden, she’s back in 1940 talking about what it was like to see this movie after school for only 5¢ a ticket! After an engaging discussion about life in the 40’s, I knew I had to indulge her. Armed with a plethora of movie streaming sights, I went to work scouring the web. No luck. The movie, “My Son My Son,” was apparently not in high demand amongst torrenting teens. I had to entreat my older brother for his Amazon Prime account to get a working stream. However, breaking up the monotony and isolation felt at the nursing home with a simple movie was worth the pandering.
While I was glad to help a resident have some fun, I was partly motivated by how much Alice reminded me of my own grandfather. In accordance with custom, my grandfather was to stay in our house once my grandmother passed away. More specifically, he stayed in my room and my bed. Just like grandma’s passing, my sudden roommate was a rough transition. In 8th grade at the time, I considered myself to be a generally good guy. Maybe even good enough to be a doctor one day. I volunteered at the hospital, shadowed regularly, and had a genuine interest for science. However, my interest in medicine was mostly restricted to academia. To be honest, I never had a sustained exposure to the palliative side of medicine until the arrival of my new roommate.
The two years I slept on that creaky wooden bed with him was the first time my metal was tested. Sharing that room, I was the one to take care of him. I was the one to rub ointment on his back, to feed him when I came back from school, and to empty out his spittoon when it got full. It was far from glamorous, and frustrating most of the time. With 75 years separating us, and senile dementia setting in, he would often forget who I was or where he was. Having to remind him that I was his grandson threatened to erode at my resolve. Assured by my Syrian Orthodox faith, I even prayed about it; asking God for comfort and firmness on my end. Over time, I grew slow to speak and eager to listen as he started to ramble more and more about bits and pieces of the past. If I was lucky, I would be able to stich together a narrative that may or may have not been true. In any case, my patience started to bud beyond my age group.
Having to remind him that I was his grandson threatened to erode at my resolve.
Although I grew more patient with his disease, my curiosity never really quelled. Conversely, it developed further alongside my rapidly growing interest in the clinical side of medicine. Naturally, I became drawn to a neurology lab in college where I got to study pathologies ranging from atrophy associated with schizophrenia, and necrotic lesions post stroke. However, unlike my intro biology courses, my work at the neurology lab was rooted beyond the academics. Instead, I found myself driven by real people who could potentially benefit from our research. In particular, my shadowing experience with Dr. Dominger in the Veteran’s home made the patient more relevant in our research as I got to encounter geriatric patients with age related diseases, such as Alzhimer’s and Parkinson’s. Furthermore, I had the privilege of of talking to the families of a few of these patients to get an idea of the impact that these diseases had on the family structure. For me, the scut work in the lab meant a lot more with these families in mind than the tritium tracer we were using in the lab.
Despite my achievements in the lab and the classroom, my time with my grandfather still holds a special place in my life story. The more I think about him, the more confident I am in my decision to pursue a career where caring for people is just as important, if not more important, than excelling at academics. Although it was a lot of work, the years spent with him was critical in expanding my horizons both in my personal life and in the context of medicine. While I grew to be more patient around others, I also grew to appreciate medicine beyond the science. This more holistic understanding of medicine had a synergistic effect in my work as I gained a purpose behind the extra hours in the lab, sleepless nights in the library, and longer hours volunteering. I had a reason for what I was doing that may one day help me have long conversations with my own grandchildren about the price of popcorn in the 2000’s.
The most important thing to highlight in Avery’s essay is how he is able to create a duality between his interest in not only the clinical, more academic-based side of medicine, but also the field’s personal side.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather. These two experiences build up the “synergistic” relationship between caring for people and studying the science behind medicine. In this way, he is able to clearly state his passions for medicine and explain his exact motives for entering the field. Furthermore, in his discussion of her grandfather, he effectively employs imagery (“rub ointment on his back,” “feed him when I came back from school,” etc.) to describe the actual work that he does, calling it initially as “far from glamorous, and frustrating most of the time.” By first mentioning his initial impression, then transitioning into how he grew to appreciate the experience, Avery is able to demonstrate a strength of character, sense of enormous responsibility and capability, and open-minded attitude.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather.
Later in the essay, Avery is also able to relate his time caring for his grandfather to his work with Alzheimer’s and Parkinson’s patients, showcasing the social impact of his work, as the reader is likely already familiar with the biological impact of the work. This takes Avery’s essay full circle, bringing it back to how a discussion with an elderly patient about the movies reminds him of why he chose to pursue medicine.
That said, the essay does feel rushed near the end, as the writer was likely trying to remain within the word count. There could be a more developed transition before Avery introduces the last sentence about “conversations with my own grandchildren,” especially as a strong essay ending is always recommended.
-- Accepted To: Saint Louis University Medical School Direct Admission Medical Program
Sponsored by Atlas Admissions : Atlas Admissions provides expert medical school admissions consulting and test preparation services. Their experienced, physician-driven team consistently delivers top results by designing comprehensive, personalized strategies to optimize applications. Atlas Admissions is based in Boston, MA and is trusted by clients worldwide.
The tension in the office was tangible. The entire team sat silently sifting through papers as Dr. L introduced Adam, a 60-year-old morbidly obese man recently admitted for a large open wound along his chest. As Dr. L reviewed the details of the case, his prognosis became even bleaker: hypertension, diabetes, chronic kidney disease, cardiomyopathy, hyperlipidemia; the list went on and on. As the humdrum of the side-conversations came to a halt, and the shuffle of papers softened, the reality of Adam’s situation became apparent. Adam had a few months to live at best, a few days at worst. To make matters worse, Adam’s insurance would not cover his treatment costs. With no job, family, or friends, he was dying poor and alone.
I followed Dr. L out of the conference room, unsure what would happen next. “Well,” she muttered hesitantly, “We need to make sure that Adam is on the same page as us.” It’s one thing to hear bad news, and another to hear it utterly alone. Dr. L frantically reviewed all of Adam’s paperwork desperately looking for someone to console him, someone to be at his side. As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy. That empathy is exactly what I saw in Dr. L as she went out of her way to comfort a patient she met hardly 20 minutes prior.
Since high school, I’ve been fascinated by technology’s potential to improve healthcare. As a volunteer in [the] Student Ambassador program, I was fortunate enough to watch an open-heart surgery. Intrigued by the confluence of technology and medicine, I chose to study biomedical engineering. At [school], I wanted to help expand this interface, so I became involved with research through Dr. P’s lab by studying the applications of electrospun scaffolds for dermal wound healing. While still in the preliminary stages of research, I learned about the Disability Service Club (DSC) and decided to try something new by volunteering at a bowling outing.
As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy.
The DSC promotes awareness of cognitive disabilities in the community and seeks to alleviate difficulties for the disabled. During one outing, I collaborated with Arc, a local organization with a similar mission. Walking in, I was told that my role was to support the participants by providing encouragement. I decided to help a relatively quiet group of individuals assisted by only one volunteer, Mary. Mary informed me that many individuals with whom I was working were diagnosed with ASD. Suddenly, she started cheering, as one of the members of the group bowled a strike. The group went wild. Everyone was dancing, singing, and rejoicing. Then I noticed one gentleman sitting at our table, solemn-faced. I tried to start a conversation with him, but he remained unresponsive. I sat with him for the rest of the game, trying my hardest to think of questions that would elicit more than a monosyllabic response, but to no avail. As the game ended, I stood up to say bye when he mumbled, “Thanks for talking.” Then he quickly turned his head away. I walked away beaming. Although I was unable to draw out a smile or even sustain a conversation, at the end of the day, the fact that this gentleman appreciated my mere effort completely overshadowed the awkwardness of our time together. Later that day, I realized that as much as I enjoyed the thrill of research and its applications, helping other people was what I was most passionate about.
When it finally came time to tell Adam about his deteriorating condition, I was not sure how he would react. Dr. L gently greeted him and slowly let reality take its toll. He stoically turned towards Dr. L and groaned, “I don’t really care. Just leave me alone.” Dr. L gave him a concerned nod and gradually left the room. We walked to the next room where we met with a pastor from Adam’s church.
“Adam’s always been like that,” remarked the pastor, “he’s never been one to express emotion.” We sat with his pastor for over an hour discussing how we could console Adam. It turned out that Adam was part of a motorcycle club, but recently quit because of his health. So, Dr. L arranged for motorcycle pictures and other small bike trinkets to be brought to his room as a reminder of better times.
Dr. L’s simple gesture reminded me of why I want to pursue medicine. There is something sacred, empowering, about providing support when people need it the most; whether it be simple as starting a conversation, or providing support during the most trying of times. My time spent conducting research kindled my interest in the science of medicine, and my service as a volunteer allowed me to realize how much I valued human interaction. Science and technology form the foundation of medicine, but to me, empathy is the essence. It is my combined interest in science and service that inspires me to pursue medicine. It is that combined interest that makes me aspire to be a physician.
Parker’s essay focuses on one central narrative with a governing theme of compassionate and attentive care for patients, which is the key motivator for her application to medical school. Parker’s story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field. This effectively demonstrates to the reader what kind of doctor Parker wants to be in the future.
Parker’s narrative has a clear beginning, middle, and end, making it easy for the reader to follow. She intersperses the main narrative about Adam with experiences she has with other patients and reflects upon her values as she contemplates pursuing medicine as a career. Her anecdote about bowling with the patients diagnosed with ASD is another instance where she uses a story to tell the reader why she values helping people through medicine and attentive patient care, especially as she focuses on the impact her work made on one man at the event.
Parker's story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field.
All throughout the essay, the writing is engaging and Parker incorporates excellent imagery, which goes well with her varied sentence structure. The essay is also strong because it comes back full circle at its conclusion, tying the overall narrative back to the story of Dr. L and Adam, which speaks to Parker’s motives for going to medical school.
-- Accepted To: Emory School of Medicine
Growing up, I enjoyed visiting my grandparents. My grandfather was an established doctor, helping the sick and elderly in rural Taiwan until two weeks before he died at 91 years old. His clinic was located on the first floor of the residency with an exam room, treatment room, X-ray room, and small pharmacy. Curious about his work, I would follow him to see his patients. Grandpa often asked me if I want to be a doctor just like him. I always smiled, but was more interested in how to beat the latest Pokémon game. I was in 8th grade when my grandfather passed away. I flew back to Taiwan to attend his funeral. It was a gloomy day and the only street in the small village became a mourning place for the villagers. Flowers filled the streets and people came to pay their respects. An old man told me a story: 60 years ago, a village woman was in a difficult labor. My grandfather rushed into the house and delivered a baby boy. That boy was the old man and he was forever grateful. Stories of grandpa saving lives and bringing happiness to families were told during the ceremony. At that moment, I realized why my grandfather worked so tirelessly up until his death as a physician. He did it for the reward of knowing that he kept a family together and saved a life. The ability for a doctor to heal and bring happiness is the reason why I want to study medicine. Medical school is the first step on a lifelong journey of learning, but I feel that my journey leading up to now has taught me some things of what it means to be an effective physician.
With a newfound purpose, I began volunteering and shadowing at my local hospital. One situation stood out when I was a volunteer in the cardiac stress lab. As I attached EKG leads onto a patient, suddenly the patient collapsed and started gasping for air. His face turned pale, then slightly blue. The charge nurse triggered “Code Blue” and started CPR. A team of doctors and nurses came, rushing in with a defibrillator to treat and stabilize the patient. What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care. I want to be a leader as well as part of a team that can make a difference in a person’s life. I have refined these lessons about teamwork and leadership to my activities. In high school I was an 8 time varsity letter winner for swimming and tennis and captain of both of those teams. In college I have participated in many activities, but notably serving as assistant principle cellist in my school symphony as well as being a co-founding member of a quartet. From both my athletic experiences and my music experiences I learned what it was like to not only assert my position as a leader and to effectively communicate my views, but equally as important I learned how to compromise and listen to the opinions of others. Many physicians that I have observed show a unique blend of confidence and humility.
What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care.
College opened me up to new perspectives on what makes a complete physician. A concept that was preached in the Guaranteed Professional Program Admissions in Medicine (GPPA) was that medicine is both an art and a science. The art of medicine deals with a variety of aspects including patient relationships as well as ethics. Besides my strong affinity for the sciences and mathematics, I always have had interest in history. I took courses in both German literature and history, which influenced me to take a class focusing on Nazi neuroscientists. It was the ideology of seeing the disabled and different races as test subjects rather than people that led to devastating lapses in medical ethics. The most surprising fact for me was that doctors who were respected and leaders in their field disregarded the humanity of patient and rather focused on getting results from their research. Speaking with Dr. Zeidman, the professor for this course, influenced me to start my research which deals with the ethical qualms of using data derived from unethical Nazi experimentation such as the brains derived from the adult and child euthanasia programs. Today, science is so result driven, it is important to keep in mind the ethics behind research and clinical practice. Also the development of personalized genomic medicine brings into question about potential privacy violations and on the extreme end discrimination. The study of ethics no matter the time period is paramount in the medical field. The end goal should always be to put the patient first.
Teaching experiences in college inspired me to become a physician educator if I become a doctor. Post-MCAT, I was offered a job by Next Step Test Prep as a tutor to help students one on one for the MCAT. I had a student who stated he was doing well during practice, but couldn’t get the correct answer during practice tests. Working with the student, I pointed out his lack of understanding concepts and this realization helped him and improves his MCAT score. Having the ability to educate the next generation of doctors is not only necessary, but also a rewarding experience.
My experiences volunteering and shadowing doctors in the hospital as well as my understanding of what it means to be a complete physician will make me a good candidate as a medical school student. It is my goal to provide the best care to patients and to put a smile on a family’s face just as my grandfather once had. Achieving this goal does not take a special miracle, but rather hard work, dedication, and an understanding of what it means to be an effective physician.
Through reflecting on various stages of life, Quinn expresses how they found purpose in pursuing medicine. Starting as a child more interested in Pokemon than their grandfather’s patients, Quinn exhibits personal growth through recognizing the importance of their grandfather’s work saving lives and eventually gaining the maturity to work towards this goal as part of a team.
This essay opens with abundant imagery — of the grandfather’s clinic, flowers filling the streets, and the village woman’s difficult labor — which grounds Quinn’s story in their family roots. Yet, the transition from shadowing in hospitals to pursuing leadership positions in high schools is jarring, and the list of athletic and musical accomplishments reads like a laundry list of accomplishments until Quinn neatly wraps them up as evidence of leadership and teamwork skills. Similarly, the section about tutoring, while intended to demonstrate Quinn’s desire to educate future physicians, lacks the emotional resonance necessary to elevate it from another line lifted from their resume.
This essay opens with abundant imagery — of the grandfather's clinic, flowers filling the streets, and the village woman's difficult labor — which grounds Quinn's story in their family roots.
The strongest point of Quinn’s essay is the focus on their unique arts and humanities background. This equips them with a unique perspective necessary to consider issues in medicine in a new light. Through detailing how history and literature coursework informed their unique research, Quinn sets their application apart from the multitude of STEM-focused narratives. Closing the essay with the desire to help others just as their grandfather had, Quinn ties the narrative back to their personal roots.
-- Accepted To: Edinburgh University UCAT Score: 2810 BMAT Score: 4.6, 4.2, 3.5A
Exposure to the medical career from an early age by my father, who would explain diseases of the human body, sparked my interest for Medicine and drove me to seek out work experience. I witnessed the contrast between use of bone saws and drills to gain access to the brain, with subsequent use of delicate instruments and microscopes in neurosurgery. The surgeon's care to remove the tumour, ensuring minimal damage to surrounding healthy brain and his commitment to achieve the best outcome for the patient was inspiring. The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Whilst shadowing a surgical team in Texas, carrying out laparoscopic bariatric procedures, I appreciated the surgeon's dedication to continual professional development and research. I was inspired to carry out an Extended Project Qualification on whether bariatric surgery should be funded by the NHS. By researching current literature beyond my school curriculum, I learnt to assess papers for bias and use reliable sources to make a conclusion on a difficult ethical situation. I know that doctors are required to carry out research and make ethical decisions and so, I want to continue developing these skills during my time at medical school.
The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Attending an Oncology multi-disciplinary team meeting showed me the importance of teamwork in medicine. I saw each team member, with specific areas of expertise, contributing to the discussion and actively listening, and together they formed a holistic plan of action for patients. During my Young Enterprise Award, I facilitated a brainstorm where everyone pitched a product idea. Each member offered a different perspective on the idea and then voted on a product to carry forward in the competition. As a result, we came runners up in the Regional Finals. Furthermore, I started developing my leadership skills, which I improved by doing Duke of Edinburgh Silver and attending a St. John Ambulance Leadership course. In one workshop, similar to the bariatric surgeon I shadowed, I communicated instructions and delegated roles to my team to successfully solve a puzzle. These experiences highlighted the crucial need for teamwork and leadership as a doctor.
Observing a GP, I identified the importance of compassion and empathy. During a consultation with a severely depressed patient, the GP came to the patient's eye level and used a calm, non-judgmental tone of voice, easing her anxieties and allowing her to disclose more information. While volunteering at a care home weekly for two years, I adapted my communication for a resident suffering with dementia who was disconnected from others. I would take her to a quiet environment, speak slowly and in a non-threatening manner, as such, she became talkative, engaged and happier. I recognised that communication and compassion allows doctors to build rapport, gain patients' trust and improve compliance. For two weeks, I shadowed a surgeon performing multiple craniotomies a day. I appreciated the challenges facing doctors including time and stress management needed to deliver high quality care. Organisation, by prioritising patients based on urgency and creating a timetable on the ward round, was key to running the theatre effectively. Similarly, I create to-do-lists and prioritise my academics and extra-curricular activities to maintain a good work-life balance: I am currently preparing for my Grade 8 in Singing, alongside my A-level exams. I also play tennis for the 1st team to relax and enable me to refocus. I wish to continue my hobbies at university, as ways to manage stress.
Through my work experiences and voluntary work, I have gained a realistic understanding of Medicine and its challenges. I have begun to display the necessary skills that I witnessed, such as empathy, leadership and teamwork. The combination of these skills with my fascination for the human body drives me to pursue a place at medical school and a career as a doctor.
This essay traces Alex's personal exploration of medicine through different stages of life, taking a fairly traditional path to the medical school application essay. From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
Alex details how experiences conducting research and working with medical teams have confirmed his interest in medicine. Although the breadth of experiences speaks to the applicant’s interest in medicine, the essay verges on being a regurgitation of the Alex's resume, which does not provide the admissions officer with any new insights or information and ultimately takes away from the essay as a whole. As such, the writing’s lack of voice or unique perspective puts the applicant at risk of sounding middle-of-the-road.
From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
The essay’s organization, however, is one of its strengths — each paragraph provides an example of personal growth through a new experience in medicine. Further, Alex demonstrates his compassion and diligence through detailed stories, which give a reader a glimpse into his values. Through recognizing important skills necessary to be a doctor, Alex demonstrates that he has the mature perspective necessary to embark upon this journey.
What this essay lacks in a unique voice, it makes up for in professionalism and organization. Alex's earnest desire to attend medical school is what makes this essay shine.
-- Accepted To: University of Toronto MCAT Scores: Chemical and Physical Foundations of Biological Systems - 128, Critical Analysis and Reading Skills - 127, Biological and Biochemical Foundations of Living Systems - 127, Psychological, Social, and Biological Foundations of Behavior - 130, Total - 512
Moment of brilliance.
Revelation.
These are all words one would use to describe their motivation by a higher calling to achieve something great. Such an experience is often cited as the reason for students to become physicians; I was not one of these students. Instead of waiting for an event like this, I chose to get involved in the activities that I found most invigorating. Slowly but surely, my interests, hobbies, and experiences inspired me to pursue medicine.
As a medical student, one must possess a solid academic foundation to facilitate an understanding of physical health and illness. Since high school, I found science courses the most appealing and tended to devote most of my time to their exploration. I also enjoyed learning about the music, food, literature, and language of other cultures through Latin and French class. I chose the Medical Sciences program because it allowed for flexibility in course selection. I have studied several scientific disciplines in depth like physiology and pathology while taking classes in sociology, psychology, and classical studies. Such a diverse academic portfolio has strengthened my ability to consider multiple viewpoints and attack problems from several angles. I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
I was motivated to travel as much as possible by learning about other cultures in school. Exposing myself to different environments offered me perspective on universal traits that render us human. I want to pursue medicine because I believe that this principle of commonality relates to medical practice in providing objective and compassionate care for all. Combined with my love for travel, this realization took me to Nepal with Volunteer Abroad (VA) to build a school for a local orphanage (4). The project’s demands required a group of us to work closely as a team to accomplish the task. Rooted in different backgrounds, we often had conflicting perspectives; even a simple task such as bricklaying could stir up an argument because each person had their own approach. However, we discussed why we came to Nepal and reached the conclusion that all we wanted was to build a place of education for the children. Our unifying goal allowed us to reach compromises and truly appreciate the value of teamwork. These skills are vital in a clinical setting, where physicians and other health care professionals need to collaborate as a multidisciplinary team to tackle patients’ physical, emotional, social, and psychological problems.
I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
The insight I gained from my Nepal excursion encouraged me to undertake and develop the role of VA campus representative (4). Unfortunately, many students are not equipped with the resources to volunteer abroad; I raised awareness about local initiatives so everyone had a chance to do their part. I tried to avoid pushing solely for international volunteerism for this reason and also because it can undermine the work of local skilled workers and foster dependency. Nevertheless, I took on this position with VA because I felt that the potential benefits were more significant than the disadvantages. Likewise, doctors must constantly weigh out the pros and cons of a situation to help a patient make the best choice. I tried to dispel fears of traveling abroad by sharing first-hand experiences so that students could make an informed decision. When people approached me regarding unfamiliar placements, I researched their questions and provided them with both answers and a sense of security. I found great fulfillment in addressing the concerns of individuals, and I believe that similar processes could prove invaluable in the practice of medicine.
As part of the Sickkids Summer Research Program, I began to appreciate the value of experimental investigation and evidence-based medicine (23). Responsible for initiating an infant nutrition study at a downtown clinic, I was required to explain the project’s implications and daily protocol to physicians, nurses and phlebotomists. I took anthropometric measurements and blood pressure of children aged 1-10 and asked parents about their and their child’s diet, television habits, physical exercise regimen, and sunlight exposure. On a few occasions, I analyzed and presented a small set of data to my superiors through oral presentations and written documents.
With continuous medical developments, physicians must participate in lifelong learning. More importantly, they can engage in research to further improve the lives of their patients. I encountered a young mother one day at the clinic struggling to complete the study’s questionnaires. After I asked her some questions, she began to open up to me as her anxiety subsided; she then told me that her child suffered from low iron. By talking with the physician and reading a few articles, I recommended a few supplements and iron-rich foods to help her child. This experience in particular helped me realize that I enjoy clinical research and strive to address the concerns of people with whom I interact.
Research is often impeded by a lack of government and private funding. My clinical placement motivated me to become more adept in budgeting, culminating in my role as founding Co-President of the UWO Commerce Club (ICCC) (9). Together, fellow club executives and I worked diligently to get the club ratified, a process that made me aware of the bureaucratic challenges facing new organizations. Although we had a small budget, we found ways of minimizing expenditure on advertising so that we were able to host more speakers who lectured about entrepreneurship and overcoming challenges. Considering the limited space available in hospitals and the rising cost of health care, physicians, too, are often forced to prioritize and manage the needs of their patients.
No one needs a grand revelation to pursue medicine. Although passion is vital, it is irrelevant whether this comes suddenly from a life-altering event or builds up progressively through experience. I enjoyed working in Nepal, managing resources, and being a part of clinical and research teams; medicine will allow me to combine all of these aspects into one wholesome career.
I know with certainty that this is the profession for me.
Jimmy opens this essay hinting that his essay will follow a well-worn path, describing the “big moment” that made him realize why he needed to become a physician. But Jimmy quickly turns the reader’s expectation on its head by stating that he did not have one of those moments. By doing this, Jimmy commands attention and has the reader waiting for an explanation. He soon provides the explanation that doubles as the “thesis” of his essay: Jimmy thinks passion can be built progressively, and Jimmy’s life progression has led him to the medical field.
Jimmy did not make the decision to pursue a career in medicine lightly. Instead he displays through anecdotes that his separate passions — helping others, exploring different walks of life, personal responsibility, and learning constantly, among others — helped Jimmy realize that being a physician was the career for him. By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously. The ability to evaluate multiple options and make an informed, well-reasoned decision is one that bodes well for Jimmy’s medical career.
While in some cases this essay does a lot of “telling,” the comprehensive and decisive walkthrough indicates what Jimmy’s idea of a doctor is. To him, a doctor is someone who is genuinely interested in his work, someone who can empathize and related to his patients, someone who can make important decisions with a clear head, and someone who is always trying to learn more. Just like his decision to work at the VA, Jimmy has broken down the “problem” (what his career should be) and reached a sound conclusion.
By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously.
Additionally, this essay communicates Jimmy’s care for others. While it is not always advisable to list one’s volunteer efforts, each activity Jimmy lists has a direct application to his essay. Further, the sheer amount of philanthropic work that Jimmy does speaks for itself: Jimmy would not have worked at VA, spent a summer with Sickkids, or founded the UWO finance club if he were not passionate about helping others through medicine. Like the VA story, the details of Jimmy’s participation in Sickkids and the UWO continue to show how he has thought about and embodied the principles that a physician needs to be successful.
Jimmy’s essay both breaks common tropes and lives up to them. By framing his “list” of activities with his passion-happens-slowly mindset, Jimmy injects purpose and interest into what could have been a boring and braggadocious essay if it were written differently. Overall, this essay lets the reader know that Jimmy is seriously dedicated to becoming a physician, and both his thoughts and his actions inspire confidence that he will give medical school his all.
The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this content.
- Open access
- Published: 01 December 2023
Compassion fatigue in healthcare providers: a scoping review
- Anna Garnett 1 ,
- Lucy Hui 2 ,
- Christina Oleynikov 1 &
- Sheila Boamah 3
BMC Health Services Research volume 23 , Article number: 1336 ( 2023 ) Cite this article
2539 Accesses
2 Altmetric
Metrics details
The detrimental impacts of COVID-19 on healthcare providers’ psychological health and well-being continue to affect their professional roles and activities, leading to compassion fatigue. The purpose of this review was to identify and summarize published literature on compassion fatigue among healthcare providers and its impact on patient care. Six databases were searched: MEDLINE (Ovid), PsycINFO (Ovid), Embase (Ovid), CINAHL, Scopus, Web of Science, for studies on compassion fatigue in healthcare providers, published in English from the peak of the pandemic in 2020 to 2023. To expand the search, reference lists of included studies were hand searched to locate additional relevant studies. The studies primarily focused on nurses, physicians, and other allied health professionals. This scoping review was registered on Open Science Framework (OSF), using the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) extension to scoping review. From 11,715 search results, 24 met the inclusion criteria. Findings are presented using four themes: prevalence of compassion fatigue; antecedents of compassion fatigue; consequences of compassion fatigue; and interventions to address compassion fatigue. The potential antecedents of compassion fatigue are grouped under individual-, organization-, and systems-level factors. Our findings suggest that healthcare providers differ in risk for developing compassion fatigue in a country-dependent manner. Interventions such as increasing available personnel helped to minimize the occurrence of compassion fatigue. This scoping review offers important insight on the common causes and potential risks for compassion fatigue among healthcare providers and identifies potential strategies to support healthcare providers’ psychological health and well-being.
• What do we already know about this topic? The elevated and persistent mental stress associated with the COVID-19 pandemic predisposed healthcare providers (HCP) to various psychological conditions such as compassion fatigue. Declines in health providers’ mental health has been observed to negatively impact their professional performance and the quality of patient care.
• How does your research contribute to the field? This review provides an overview of the prevalence of compassion fatigue among HCPs across the globe during the COVID-19 pandemic. The main risk factors for compassion fatigue include younger age, female sex, being either a physician or a nurse, high workload, extensive work hours, and limited access to personal protective equipment (PPE). Negative behavioral intention towards patients has been identified to be a consequence of compassion fatigue. Interventions such as the provision of emotional support, increased monitoring for conditions such as stress and burnout, and increasing available personnel helped to minimize the occurrence of compassion fatigue.
• What are your research’s implications towards theory, practice, or policy? While the public health emergency associated with the COVID-19 pandemic has ended, the impact on human health resources persists. The findings of this review can inform policy decisions and implementation of evidence-based strategies to prevent, manage, and lessen the negative effects of compassion fatigue on HCPs and its subsequent impacts on patient care.
Peer Review reports
Introduction
The 2019-novel coronavirus disease (COVID-19) outbreak spread rapidly and by January 30 th , 2022 was formally proclaimed a global health emergency despite being first identified just over a month prior [ 1 ]. Although there have been five other global health emergencies associated with disease outbreaks since 2009, none has matched the scale and scope of the COVID-19 pandemic [ 2 ]. In the short-term the rapid increase in patients requiring acute care services presented unprecedented challenges for health systems. Care provision and infection control strategies were hampered by capacity limitations, staffing shortfalls and supply chain challenges [ 3 ]. As a result, healthcare providers (HCPs) encountered mounting levels of strain which have continued with little reprieve for the duration of and beyond the global COVID-19 pandemic. Limited access to personal protective equipment (PPEs) exacerbated transmission of the virus, compounding healthcare providers’ fears of contracting and spreading COVID-19 among their peers, patients and families [ 4 , 5 , 6 , 7 ]. HCPs also contracted COVID-19, became seriously ill and died with global estimates of HCP death between January 2020 and May 2021 being over 100,000. With time, the number of absences, extended sick leaves and staff turnovers increased [ 7 , 8 ]. The combination of short staffing, frequent changes to workflow and continuous care provision to patients who were gravely ill and had high mortality amplified the toll on health care providers [ 8 , 9 ]. While no longer a global health emergency, there continue to be COVID-19 cases and deaths. As of July 14, 2023 there were 767,972,961 COVID-19 cases and 6,950,655 deaths globally [ 10 ].
HCPs around the globe who treated severe COVID-19 cases, a process which necessitated in-depth compassionate engagement, became vulnerable to developing compassion fatigue as a result of their continued and in-depth involvement in the care of these severely ill patients and their families [ 11 ]. Compassion fatigue is defined as a composite of two measurements: burnout (sustained employment-related stress that compromises an individual’s desire to work) and secondary trauma (the development of traumatic symptoms resulting from the protracted exposure to the suffering of others) [ 12 , 13 ]. An individual experiencing compassion fatigue has a reduced ability for showing compassion to others, resulting from the prolonged exposure to witnessing the suffering of others without being able to relieve one’s anguish despite having the desire to do so [ 9 ]. Individuals experiencing compassion fatigue may express a range of behaviors such as increased work absences or declines in the ability to engage in work-related tasks such as decision-making. Burnout and secondary trauma are suggested to be mediated by compassion satisfaction—the pleasure that comes from helping behavior [ 11 , 12 ].
As the pandemic shifts from being a global health emergency to an endemic disease, there continues to be concern for HCP health and well-being [ 14 , 15 , 16 ]. The increased and chronic nature of the stress experienced during and beyond the COVID-19 pandemic has heightened HCPs risk for a range of negative psychological impacts such as depression, fearfulness, grief and post-traumatic stress disorder (PTSD) [ 17 ]. Prior infectious disease outbreaks (SARS-CoV-1, H1N1, MERS-CoV, Ebola) are also associated with an increased prevalence of declining mental health in HCPs [ 18 ]. A growing body of research on the COVID-19 pandemic highlights the range of psychological symptoms HCPs developed following their sustained exposure to COVID-19 including burnout, feelings of isolation, insomnia, grief, emotional exhaustion, depression, post-traumatic stress and depersonalization, some of which have persisted over time [ 14 , 17 , 19 , 20 , 21 , 22 ]. The consequences of HCPs’ declining psychological health and well-being has had impacts on the quality of patient care and indirectly on patient outcomes through inadequate staffing [ 18 ]. Compromises in HCPs’ ability to provide optimal clinical care can have serious consequences, including the worsening of patient conditions and the increased transmission of the infection from patients to others in the hospital [ 18 ]. In addition, compassion fatigue may be exacerbated by the COVID-19 pandemic, potentially leading to moral injury, decreased productivity, increased turnover, and reduced quality of care [ 23 ]. Moreover, a growing body of literature suggests that challenges across health systems will persist although COVID-19 is no longer a global health emergency [ 24 , 25 ]. As such, it is important to have a fulsome understanding of COVID-19’s toll on HCPs and tailor health system strategies accordingly.
As health care systems continue to experience a health human resources crisis, it is important to identify and understand the prevalence of compassion fatigue, identify contributing factors, and increase understanding of the consequences and actions that can be taken to address compassion fatigue among HCPs. While there has been in an increase in the body of published literature on the health and well-being of HCPs since the onset of the COVID-19 pandemic, there continues to be a knowledge gap mapping the incidence of compassion fatigue, its resultant impact on HCP well-being, and its potential influence on patient care provision [ 11 , 17 ]. A comprehensive review of the literature on compassion fatigue among HCPs can inform policy and practice initiatives to improve the current health human resources crisis experienced by many health systems. It may also aid in identifying prospective research foci.
The purpose of this scoping review was to synthesize and provide a synopsis of the literature on compassion fatigue among HCPs during the COVID-19 pandemic and to understand its broader impact. The review was guided by the following question: What is the current state of knowledge on compassion fatigue among HCPs over the course of COVID-19?
Project registration
This scoping review was registered under Open Science Framework. A project outline was submitted including the study hypotheses, design, and data collection procedures. The DOI for the registered project is as follows: https://doi.org/10.17605/OSF.IO/F4T7N . In addition, a scoping review protocol for this review has been published in a peer-reviewed journal ( https://doi.org/10.1136/bmjopen-2022-069843 ).
Study design
A systematic scoping review strategy was chosen to explore the existing body of literature pertaining to the research topic. The objective of a scoping review is to identify relevant literature on a given topic, without focusing on evaluating research quality or conducting a thorough analysis of selected studies, as systematic reviews typically do. Current gaps in research and directions for future research can be identified by means of summarizing emerging literature on compassion fatigue in HCPs.
The current scoping review used two methodological tools, namely the Arksey and O’Mally scoping review framework as well as the Joanna Briggs Institute Critical Appraisal Tools. The Arksey and O’Malley framework comprises five stages, which include: (1) formulating the research question; (2) identifying relevant studies; (3) selecting studies for inclusion; (4) extracting and organizing the data; and (5) collating, summarizing, and reporting the findings [ 26 ]. While scoping reviews typically do not require article appraisal, all articles were evaluated by one author (CO) using the methodology established by the Joanna Briggs Institute (JBI) to enhance the overall quality of the review [ 27 ]. No articles were excluded based on their quality, in accord with the Arksey and O’Malley framework [ 26 ].
Stage I: Identifying the research question(s)
The research objective and question were drafted by the authors (AG, LH, CO, SB) and can be found in the previous section under “Research aim”.
Stage II: Identifying relevant studies
As outlined by the JBI methodology, a three-step approach was used to identify relevant studies. These steps include: (1) conducting a preliminary search of at least two suitable databases; (2) identifying relevant keywords and index terms to perform a secondary search across all chosen databases; and (3) manually examining the reference lists of the included articles to discover additional relevant studies [ 28 ] (p11) .
Preliminary literature search
To establish the criteria for inclusion and exclusion, an initial and restricted search was conducted on the subject of interest. The preliminary literature exploration encompassed three scholarly electronic databases: MEDLINE (Ovid), Scopus, and Web of Science. The search employed the keywords “compassion fatigue” and incorporated the timeframe March 1, 2020, to June 15, 2022, so that the most impactful waves of the COVID-19 pandemic were represented in the included literature, resulting in 1519, 2489, and 2246 studies, from the respective databases. These three databases were selected due to their likelihood of yielding results relevant to the research topic. To construct a comprehensive search strategy, a collection of keywords and index terms were identified from the titles and abstracts of relevant articles. The search strategy was further refined in collaboration with a social science librarian.
Structured search strategy
A systematic search was conducted across six scholarly electronic databases: MEDLINE (Ovid), Embase (Ovid), CINAHL, Scopus, and Web of Science. These databases were deliberately chosen to encompass a broad range of relevant findings within the current knowledge landscape regarding the research topic. The systematic search of the literature commenced once the scoping review was peer reviewed and revisions were addressed by the authors. Using the selected vocabulary and Boolean connectors as shown in Table 1 , a string of relevant search terms was developed. The search strategy was adapted accordingly for each individual database (e.g., Medical Subject Headings [MeSH] terms for MEDLINE [Ovid]). In the final stage of the search strategy, the reference lists of all included studies were manually examined to identify additional relevant studies.
Inclusion criteria
The inclusion criteria for this review was formulated using the PCC (Population, Concept, Context) mnemonic developed by JBI (Table 1 ). The participants included in this review were HCPs who were employed across healthcare systems during the COVID-19 pandemic (e.g., physicians, registered nurses, nurse practitioners, physician assistants, and licensed clinical social workers). The concept explored in this review focused on compassion fatigue among HCPs working in healthcare systems during the COVID-19 pandemic. The context of the study encompassed various care settings where HCPs carry out their professional activities across different clinical specialties (e.g., surgery, critical care, palliative care), as well as clinical settings (e.g., inpatient and outpatient). For the purposes of this scoping review, formal healthcare settings were broadly classified as those that provided health services and were situated within and administered by healthcare institutions.
This scoping review only included articles published in English. A time filter was applied to encompass studies conducted between 2020 to 2023, spanning the period from the onset of the COVID-19 pandemic to the present. A range of study designs were included in the review (i.e., experiments, quasi-experimental studies, analytical observational studies, descriptive observational studies, mixed-methods studies, and qualitative studies).
Exclusion criteria
Through the past two decades, compassion fatigue has been defined in different ways, sometimes being considered synonymous with burnout and secondary traumatic stress, or as an outcome resulting from both components [ 12 , 13 ]. Yet recently, it has been suggested that compassion fatigue is a focal concept related to the management of traumatic situations whereas burnout is a general concept that may have multiple contributors [ 26 ]. Due to the conceptual ambiguity surrounding compassion fatigue, articles that solely examine the components of compassion fatigue, such as burnout and secondary trauma, without directly addressing compassion fatigue itself, were excluded from consideration.
Studies that failed to meet the inclusion criteria or lacked full-text availability were excluded from the review. Additionally, editorials, letters to the editor, commentaries, and reviews were also excluded as they did not offer sufficient information for addressing the research questions.
Stage III: Study selection
After the full database searches were conducted, all identified citations were compiled and uploaded into Covidence. Any duplicate citations were automatically excluded.
Three reviewers (LH, CO, AG) independently screened the titles and abstracts of the identified studies to assess their eligibility according to the pre-established inclusion and exclusion criteria. Subsequently, the full texts of 736 selected studies were evaluated to arrive at the final list of articles for data extraction. The reasons for excluding specific studies were documented. Throughout the process, any disagreements that arose at each stage of study selection were resolved through discussions with a third reviewer (AG, SB).
The outcomes of the study selection process were presented in a flow diagram adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) guidelines (Fig. 1 ) [ 29 ]. Additionally, all the included studies underwent an assessment of their risk of bias (quality) using established critical appraisal tools from the Joanna Briggs Institute (JBI) for Evidence Synthesis [ 30 ]. Although not mandatory for scoping reviews, appraisals of study quality will contribute to the subsequent implications and future steps stemming from this scoping review [ 31 ]. The JBI provides critical appraisal checklists for various study designs, encompassing experimental, quasi-experimental, randomized controlled trials, observational, and qualitative study designs. One reviewer (CO) conducted the assessments of all the included studies, and a second reviewer (AG) verified the evaluations. Any discrepancies that arose were discussed and resolved in consultation with both reviewers. In line with the methodology of scoping reviews, no studies were excluded based on their quality assessments, ensuring a comprehensive understanding of the current state of the literature on compassion fatigue among HCPs during the COVID-19 pandemic. A summary of the quality assessments were presented in the results section of the review, while the full appraisals can be found in Additional file 1 .
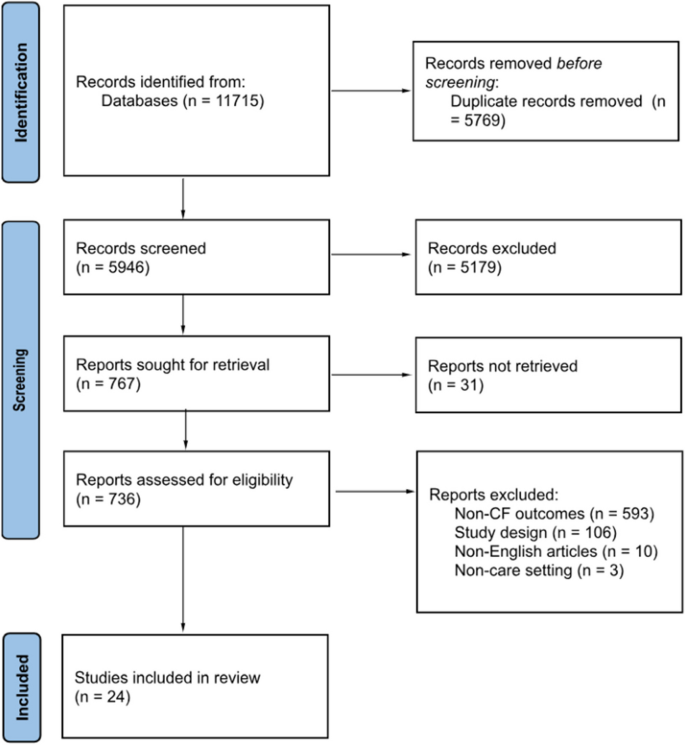
PRISMA flow chart [ 28 ]
Stage IV: Data extraction
To facilitate data extraction aligned with the research objectives, a data-extraction template was developed by one reviewer (LH). This template encompassed various aspects of the included studies (i.e., authors, publication year, study populations, country, study design, aims, sample size, assessment instruments, risk factors, protective factors, consequences of compassion fatigue, and measures to prevent/manage/reduce compassion fatigue). Utilizing Covidence, two independent reviewers (LH, CO) extracted the relevant data from the studies included in the final list of citations.
Stage V: Risk of bias
Standardized tools developed by the Joanna Briggs Institute for respective study types were used to assess risk of bias (quality) for all studies included in the review [ 27 ]. The study appraisals were conducted by one reviewer (CO) and reviewed by another reviewer (AG). Any discrepancies were discussed and resolved together. While no studies were excluded based on the appraisal scores to ensure a comprehensive presentation of the available literature on compassion fatigue among healthcare providers, the findings for the risk of bias assessments are summarized in the results section and the full appraisals are presented in Additional file 1 .
Stage VI: Collating, summarizing, and reporting the results
To summarize and synthesize the findings, the study followed a three-step approach proposed by Levac et al. [ 32 ]: (1) collating and analyzing the collected data; (2) reporting the results and outcomes to address the study objectives; and (3) discussing the potential implications that findings hold for future research and policy considerations [ 31 ]. The review process adhered to the PRISMA Extension for Scoping Reviews checklist, which provided guidance for conducting the review and reporting the findings [ 26 ].
Search results
Figure 1 displays the PRISMA-ScR flowchart of the scoping review search strategy. The search and reference list initially yielded 11,715 studies. Of these, 5769 were excluded as duplicates. Following the title and abstract screening of the remaining studies, 5179 studies were excluded as they met the exclusion criteria. Finally, the full-texts of the remaining 736 studies were screened, and 712 were excluded as they did not meet the inclusion criteria. In total, 24 eligible studies were included in the review for further analysis.
Risk of bias of included studies
The complete assessment of risk of bias of all 24 included studies is available in Additional file 1 . Within the two mixed-methods studies risk of bias primarily stemmed from the quantitative strand of the studies with a lack of clarity provided about study inclusion criteria, study setting, and identification of confounding factors [ 29 ]. Other sources of bias in other quantitative studies were vagueness around the criteria used for outcome measurement [ 30 ] and only one study identified potential cofounding factors along with strategies to manage them [ 31 ]. Further shortcomings related to the failure to provide transparency around the use of valid and reliable outcome measures [ 23 , 31 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ]. Within qualitative studies not all provided information about the researchers’ theoretical stance [ 29 , 41 , 43 ] and two studies did not provide documentation of ethics approval for the conducted research [ 43 , 44 ]. One included case report met most assessment criteria for risk of bias although more description of assessment, post-assessment condition and adverse events were warranted [ 45 ].
Characteristics of studies
Study characteristics are presented in Table 2 . Of the 24 eligible studies, 18 studies used quantitative methods [ 23 , 30 , 31 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 46 , 47 , 48 , 49 , 50 , 51 ], 3 studies used qualitative methods [ 43 , 44 , 45 ], and the remaining studies used mixed-methods approaches [ 29 , 41 , 52 ]. Additionally, 13 studies focused on the antecedents of compassion fatigue [ 23 , 29 , 33 , 34 , 35 , 36 , 40 , 41 , 42 , 45 , 46 , 47 , 48 ] and 5 studies examined the consequences of compassion fatigue [ 30 , 37 , 43 , 44 , 49 ]. Six studies were conducted in the United States, with the others being conducted in a range of countries including Ecuador, Spain, United Kingdom, Italy, Greece, Turkey, Iran, Uganda, Taiwan, Japan, Philippines, China, and India. These studies primarily focused on nurses, physicians, and other allied health professionals. The study samples included both male and female HCPs. Only one study focused exclusively on female HCPs [ 43 ].
A variety of assessment tools were used to measure compassion fatigue across included studies. Common tools included Compassion Fatigue Short Scale (CFSS) [ 33 , 47 , 48 ], Compassion Fatigue Scale (CFS) [ 30 , 49 ], Professional Quality of Life Scale Version 5 (ProQoL 5) [ 23 , 29 , 29 , 31 , 35 , 36 , 38 , 39 , 40 , 41 , 42 , 50 , 51 ], Work-Related Quality of Life Scale (WRQoL) [ 46 ], and Compassion Fatigue and Satisfaction Self-Test (CFST) [ 37 , 52 ] (Table 3 ).
The time period of the study period shows that most of the studies were conducted in the first six months of 2020, coinciding with the World Health Organization’s declaration of the COVID-19 outbreak as a pandemic [ 54 ]. No studies included in the review were conducted between March 2021 and May 2023 (Fig. 2 ).
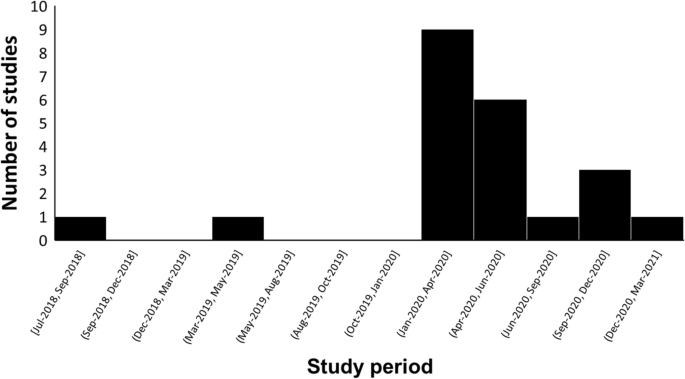
The time trend of study periods on compassion fatigue in HCPs during the COVID-19 pandemic
Findings were synthesized and presented using the following 4 themes: (1) prevalence of compassion fatigue, (2) antecedents of compassion fatigue (individual-Level, organizational-Level, and systems-level factors), (3) consequences of compassion fatigue, and (4) interventions for compassion fatigue.
Theme 1: Prevalence of compassion fatigue
Of the studies reviewed, five measured the prevalence of compassion fatigue among HCPs during the COVID-19 pandemic [ 23 , 30 , 31 , 36 , 41 ]. In a study conducted in Spain, 306 out of 506 (60.4%) HCPs reported high levels of compassion fatigue while 170 (33.6%) showed moderate levels of compassion fatigue (ProQoL 5: M = 19.9, SD = 7.6) [ 36 ]. In a sample composed of 395 Ugandan frontline nurses, 49.11% of the nurses reported high levels of compassion fatigue, while 29.6% experienced moderate levels of compassion fatigue [ 23 ]. Over half of the nurses in the study (54.94%) reported direct exposure to COVID-19 cases. A study conducted in Greece found that in a sample of 105 nurses, the majority of nurses (51.4%) experienced moderate levels of compassion fatigue (ProQoL 5: M = 22.26, SD = 6.76) [ 41 ]. In a Taiwanese study of 503 HCPs, the majority of the participants (63.2%) experienced low levels of compassion fatigue (ProQoL 5: M = 20.9, SD = 7.6) [ 31 ]. Finally, in a Filipino sample composed of 270 frontline nurses, 61.4% of the nurses reported low levels of compassion fatigue (CFS: M = 2.213, SD = 0.979) [ 30 ].
Theme 2: Antecedents of compassion fatigue
Individual-level factors.
Age and sex were key factors associated with compassion fatigue among participant HCPs. Younger HCPs with less experience were more likely to experience mental health issues and conflicting feelings with regards to providing care to COVID-19 patients [ 23 , 29 , 44 , 46 ]. Seven studies included in the review determined that female HCPs were more likely than male HCPs to experience compassion fatigue [ 23 , 35 , 36 , 38 , 40 , 50 , 52 ]. Physicians were also reported to have higher levels of compassion fatigue compared to nurses in three studies [ 36 , 38 , 39 ]. While nursing assistants had higher levels of compassion fatigue when compared to nurses in one study (ProQol 5: Nursing assistants = 29.15 ± 6.94; Nurse = 25.68 ± 5.87) [ 29 ]. Furthermore, the risk was higher in permanent workers compared to temporary workers (ProQoL 5: Permanent = 2.48 ± 1.29; Temporary = 2.11 ± 1.15; P -value < 0.05) [ 35 ]. One included study determined that marital status and education levels were not correlated with compassion fatigue [ 23 ]. Psychiatric comorbidities such as past trauma, burnout, stress, anxiety, and depression exacerbated HCPs’ psychological well-being across a number of included studies [ 31 , 33 , 36 , 38 , 39 , 41 , 49 , 50 ]. Other psychological factors such as excessive empathetic engagement, sensitive sensory processes, and overidentification from frequent witnessing of patient suffering and deaths were found to aggravate the development of compassion fatigue [ 34 , 39 , 45 ]. The inability to cope with the rapidly evolving landscape of healthcare provision and a lack of self-care contributed to increased burden and blurring of role boundaries between professional and private lives [ 29 , 41 , 43 , 44 , 51 , 52 ]. One study that used Compassion Fatigue and Satisfaction Self-Tests and a questionnaire of personal and professional characteristics found that feelings of underappreciation, insufficient compensations, and social isolation incurred psychological burden on pediatric sub-specialists [ 52 ]. Additionally, a decrease in occupational hardiness, as measured by the Occupational Hardiness Questionnaire, increased the risk of compassion fatigue among HCPs in two studies [ 42 , 50 ]. Negative outcomes to the HCPs’ families and concerns revolving around their patients’ families also predicted higher risk of experiencing compassion fatigue [ 45 , 48 , 52 ]. Finally, HCPs’ fear of COVID-19 with regards to infection and transmission was identified as a predictor of compassion fatigue [ 29 , 40 , 43 , 44 , 47 ].
Two studies identified social support from family, friends, peers, and hospital leadership as a crucial protective factor for compassion fatigue [ 43 , 52 ]. Coping mechanisms such as venting and exercising were found to help alleviate stress among HCPs [ 44 ]. Psychological qualities such as compassion satisfaction, professional satisfaction, resilience, vigor, and hardiness were found to help protect the psychological health of HCPs as well as reducing turnover intention and increasing perceived quality of care [ 30 , 34 , 36 , 37 , 39 , 40 , 42 , 46 , 50 ]. Self-care, self-awareness of limitations, and self-regulation of emotions were crucial for reducing risk of compassion fatigue in two studies comprised of physicians and nurses [ 44 , 50 ]. Lastly, spirituality, religiosity, and meditation also served as protective factors in three studies on compassion fatigue in HCPs [ 41 , 44 , 51 ].
Organizational-level factors
In five of the articles reviewed, increased workload [ 23 , 29 , 44 , 45 ], long working hours [ 23 , 29 , 44 , 45 ], and increased number of patients [ 50 ] were identified as common predictors of compassion fatigue. Furthermore, providing direct care to COVID-19 patients, which were often emotionally challenging cases, exacerbated the psychological risks to HCPs [ 23 , 36 , 46 , 48 , 50 ]. Chronic exposure to a dynamic work environment also increased the risk of compassion fatigue among HCPs [ 29 ]. Lack of access to suitable PPEs and lack of foresight from management and human resources teams regarding infection control guidelines contributed to HCPs’ distress [ 29 ]. Adjusting to the discomfort caused by wearing PPEs presented as a challenge to maintaining the efficiency of work activities [ 29 ]. Lastly, in two studies, HCPs identified that while there were plenty of wellness resources provided by healthcare organizations to support mindfulness, there was a lack of practical and pragmatic resources for social and emotional support, work-life balance, and remuneration [ 23 , 43 ].
Positive work conditions, such as a visible presence and engagement by leadership and management, as well as a positive work culture allowing HCPs to seek help without fear of judgment was found to be important protective factors against the development of compassion fatigue [ 44 ]. The social aspects of teamwork facilitated the sharing of feelings of trauma which in turn contributed to resilience and improved psychological well-being among HCPs in three studies [ 41 , 43 , 44 ]. One study observed that workplace wellness activities and a sense of feeling valued can prevent high levels of compassion fatigue [ 52 ]. Words of appreciation from supervisors boosted morale for some HCPs [ 44 ]. Attention to workplace safety in the form of PPEs and early access to vaccines alleviated the fear of infection [ 44 ]. Finally, two studies determined that adequate preparation and education to handle COVID-19 cases and increased autonomy decreased the risk of compassion fatigue and increased professional fulfillment [ 42 , 44 ].
Systems-level factors
Significant and frequently changing public health measures over the course of the pandemic presented a challenge as they were disruptive to workflow and resulted in uncertainty, feelings of inadequacy, and distress among HCPs across a range of geographical contexts [ 29 , 41 , 43 , 49 ]. Increases in the incidence of COVID-19 cases also contributed to a rise in the number of hospital admissions, aggravating HCPs’ workload [ 35 ]. Social-distancing policies precluded informal team interactions, such as sharing meals together, which posed a risk to HCPs’ psychological well-being by decreasing social support [ 43 , 52 ]. Transitions to tele-health also increased social isolation [ 43 ]. A theme that emerged was the negative impact of stigma on HCPs, with their proximity to contagion, as a possible risk factor [ 35 , 41 ]. Aggressive behaviors and verbal abuse from patients were sources of emotional stress for some HCPs [ 44 ]. Finally, negative peer pressure was identified as a barrier to HCPs engaging in self-care as they felt pressure to conform to sociocultural norms of an expected level of dedication [ 44 ]. In contrast to the impacts of stigma, a positive perception of one’s own profession is related to increased commitment and decreased compassion fatigue [ 46 ].
Theme 3: Consequences of compassion fatigue
The findings of one study suggested that compassion fatigue associated with HCP’s professional practice impacted their private lives, predicting greater parental burnout ( r = 0.542), child abuse ( r = 0.468), child neglect ( r = 0.493), spouse conflict ( r = 0.340), and substance abuse ( r = 0.298) [ 48 ]. This study identified factors such as direct care of COVID-19 patients ( r = 0.255), exposure to patient death and suffering due to COVID-19 ( r = 0.281), and family income loss due to COVID-19 ( r = 0.366) as risk factors for compassion fatigue [ 48 ]. Additionally, at an organizational-level, two studies conducted in 2020 and 2021 observed that Turkish and Filipino HCPs who reported compassion fatigue also reported lower job satisfaction and reduced professional commitment [ 30 , 46 ]. Consequently, elevated compassion fatigue also increased organizational turnover intent among Filipino HCPs (β = 0.301, P -value = 0.001) [ 30 ]. A study conducted in China found that compassion fatigue predicted negative behavioral intentions towards treating COVID-19 patients, as measured by the Attitude, Subjective Norms, and Behavioral Intention of Nurses toward Mechanically Ventilated Patients (ASIMP) questionnaire [ 33 ]. This suggests that quality of care may be adversely impacted [ 33 ]. Finally, an American study observed that compassion fatigue among HCPs was associated with deteriorating workplace culture [ 52 ].
- Patient care
The provision of care during the pandemic was impacted by the general lack of preparation for handling novel tasks experienced by many HCPs [ 23 ]. Findings from one study found that many HCPs (73%) experienced a shift in their clinical practice setting, for example, from in-personal care to virtual telehealth consults as a result of the pandemic [ 43 ]. HCPs also experienced an increase in the need to provide palliative care as a result of the negative health impacts of COVID-19, something they may have had limited prior experience with [ 43 ]. In a case study conducted in Japan, the physician reported feeling inexperienced with handling the psychological impact of the pandemic experienced by not only the patients but also the patients’ family [ 45 ]. The consequences of not being able to provide optimal care was found to exacerbate feelings of guilt, powerlessness, and frustration in HCPs [ 41 , 43 ]. In turn, study findings suggest that worsening compassion fatigue may reduce the quality of care provided by HCPs because it has been found to be a significant predictor of negative behavioral intention [ 30 , 33 , 40 , 52 ].
Theme 4: Interventions for compassion fatigue
Two studies in Japan and Uganda investigated potential interventions to support HCPs experiencing COVID-19 related compassion fatigue. On an individual-level, regularly engaging in self-care activities such as expressions of gratitude as well as learning how to recognize signs and symptoms of compassion fatigue were identified as crucial first steps in its management [ 45 , 52 ]. Emotional support from colleagues and mental health specialists was found to be effective in improving the mental health of a Japanese physician experiencing compassion fatigue [ 45 ]. Findings of two studies identified the need for a systematic approach to monitor the progression of psychological symptoms and providing tailored resources in a timely manner to HCPs to help ameliorate compassion fatigue and its consequences [ 29 , 45 ]. Suggested strategies included: facilitating regular consultations with each department [ 45 , 52 ], increasing the staffing number of HCPs in busy departments [ 23 , 45 ], and providing PPEs and vaccines in a timely manner [ 23 , 52 ]. Lastly, findings from two studies in Uganda and the United States suggested that increased remuneration may prevent or minimize compassion fatigue [ 23 , 52 ].
Key findings
This scoping review sought to provide a comprehensive summary of the literature published between January 2020 and May 2023 on the impact of the COVID-19 pandemic on compassion fatigue among HCPs and its subsequent impact on patient care. Most of the included studies were conducted in 2020 and used cross-sectional study designs. Given that the COVID-19 outbreak was declared a global health emergency in early 2020 [ 1 ], cross-sectional study designs were well-placed to provide prompt and important insights on compassion fatigue across the HCP population. Review findings were presented using four themes addressing the prevalence, antecedents, consequences, and consequences of compassion fatigue in HCPs. The prevalence of compassion fatigue was observed to vary across countries. The negative psychological outcomes reported by included studies were precipitated by individual-level factors such as age and occupational role; organizational-factors such as lack of access to PPE; and systems-level factors such as loss of social engagement and stigma. The consequences of compassion fatigue impacted HCPs’ personal and professional roles. Findings suggest an urgent need for policy makers, health managers, and team leaders to develop and implement strategies that target the potential root causes of compassion fatigue in HCPs.
Prevalence of compassion fatigue
Among the five studies that measured prevalence of compassion fatigue, results were highly variable across countries [ 23 , 30 , 31 , 36 , 41 ]. This may be attributed to differences in preparedness for infection containment and variability among health systems’ preparation and ability to respond to supply chain issues [ 53 ]. Taiwan provides an example of how digital technologies were adopted to improve disease surveillance and monitor medical supply chains [ 55 ]. Using the stringent Identify-Isolate-Inform model in conjunction with public mask-wearing and physical distancing, the spread of the disease was effectively contained in Taiwan [ 53 ]. Consequently, despite not enforcing lockdowns, Taiwan blocked the first wave of cases and slowed down subsequent outbreaks, which may contribute to the observed low prevalence of compassion fatigue among HCPs [ 56 ]. In the Philippines, responses to disease outbreaks varied across different municipalities and provinces [ 57 ]. Effective containment measures such as strict border control and early lockdowns in addition to plentiful medical supplies and personnel allowed certain regions to mount a strong response to this public health emergency, subsequently resulting in the observed low prevalence of compassion fatigue among HCPs [ 57 ]. In Uganda, there were generally low levels of preparedness with regards to the infection identification, PPE supply, access to hand-washing facilities, and establishment of isolation facilities [ 58 ]. This may have contributed to an overwhelmed healthcare system and overworked HCPs as the surge of cases was exacerbated by the shortage of disease containment resources [ 58 ]. In April 2020, Spain experienced the second highest infection incidence in the world [ 59 ]. The Spanish health system was overwhelmed by the abundance of patients due to lack of HCPs [ 60 ], hospital capacity, and material supplies [ 59 ]. An increase in compassion fatigue among HCPs was also observed in recent studies from Italy and Canada [ 61 , 62 ]. Overall, the various strategies used to address the resultant COVID-19-related public health crisis presented distinctive challenges to HCPs in different countries. Caution must be taken when interpreting the study findings given the contextual differences across various healthcare systems. The psychological burden and prevalence of compassion fatigue subsequently varied depending on the context.
Antecedents of compassion fatigue
The findings of this review suggest that individual characteristics such as age and occupational role are significant contributing factors to the development of compassion fatigue during COVID-19 [ 63 ]. Specifically, older HCPs were less likely to experience compassion fatigue than younger HCPs according to regression analyses [ 23 , 29 , 44 , 46 ]. This observation may be attributed to their increased work experience. Resilience was also positively linearly related to age [ 64 ]. Factors identified as potential contributors to the observed age-related advantage in wellbeing were access to job resources, better job security, work-life balance, and coping skills [ 64 ]. The compounding of stressors such as an increase in workload during the COVID-19 pandemic could have exacerbated the psychological health of younger HCPs. In the context of telework, older employees tended to create clear boundaries between work and non-work responsibilities [ 64 ]. The rise in telework among HCPs was mostly a consequence of the COVID-19 pandemic which may have increased the psychological burden on younger HCPs [ 65 ]. In addition, a study examining demographic predictors of resilience in nurses reported that younger nurses had less exposure to stress, and thus have fewer opportunities to develop skills in stress management [ 66 ]. As a result of these factors, the younger HCPs were at high risk for compassion fatigue during the COVID-19 pandemic. Interestingly, three of the included studies in this review also observed that physicians were at a higher risk of compassion fatigue compared to nurses [ 36 , 38 , 39 ]. This difference may be attributed to the burden of responsibility in relation to breaking bad news, a task that is often the physicians’ responsibility [ 67 ]. A study examining compassion fatigue in HCPs determined that conflict arising during patient interactions placed HCPs at a risk for compassion fatigue [ 68 ]. Delivery of bad or uncertain news also predicted a greater mental health burden in HCPs [ 68 ].
At the organizational level, findings from the studies included in this review identified that a lack of access to PPE was a contributor to compassion fatigue in HCPs during COVID-19 [ 29 , 52 ]. Specifically, one study reported that the fear of infection and transmission to patients, family, and friends added to the concern of HCPs working in high-risk environments [ 69 ]. This finding can potentially be explained by the increased vulnerability that HCPs experience following a lag in the provision of PPE. Several organizational factors were determined as potential barriers to the distribution of PPE; the unprecedented nature of the pandemic presented challenges for maintaining domestic inventories [ 70 ]. Disruptions to the PPE global supply chain also amplified the equipment shortage [ 70 ]. This finding highlights the importance of monitoring and ensuring that domestic health supplies are adequately stocked.
At the system level, loss of social engagement [ 43 , 52 ] and stigma [ 35 , 41 ] were identified in the studies included in the review as antecedents to compassion fatigue. Public policies such as social-distancing and occupancy capacity limits negatively impact social interactions which may explain the loss of social engagement in addition to worsening mental health well-being in HCPs [ 71 ]. As certain practices transition to telehealth, other studies have found increased mental fatigue and difficulty with maintaining empathetic rapport, which has important implications on patient care [ 72 , 73 ]. In addition, other studies have found that given the proximity of their role to contagion, stigma towards HCPs from patients increased during COVID-19 [ 74 , 75 ]. Consequently, the combinatorial experience of being socially isolated and stigmatized may worsen mental health outcomes [ 76 ]. This points to a need for increased access to support services for HCPs such as virtual communities.
Consequences of compassion fatigue
Review findings suggest that compassion fatigue impacted the private and professional lives of HCPs. The risk for parental burnout has increased across many occupations during the pandemic [ 77 ]. Factors related to low levels of social support, lack of leisure time, and greater parental responsibilities in face of education disruptions adds to the psychological burden of parents [ 77 ]. HCPs were placed in a unique position having to work in highly stressful environments while also balancing household responsibilities and increased challenges related to childcare [ 48 , 78 ]. This finding highlights a need for the provision of child support services for HCPs or a reduction in workload to alleviate the burden of parental and homecare responsibilities particularly in times of public health crises.
Beyond their private lives, this review has found that decreases in HCPs’ professional commitment due to compassion fatigue, may endanger the quality of patient care delivered [ 79 ]. In particular, this may be attributed to the surge in palliative care cases during the pandemic in conjunction with an unprepared workforce, creating psychological stress for HCPs [ 80 ]. In a study examining palliative care preparedness during the pandemic, a lack of core palliative care training and expertise among frontline HCPs [ 81 ] meant many felt emotionally unprepared to address cases with seriously ill patients [ 45 ]. An increased frequency of breaking bad news to patients’ families was associated with negative psychological outcomes [ 82 ]. Providing training on relevant communication skills may protect HCPs from compassion fatigue [ 83 , 84 ].
Implications
The findings of this review highlight the urgency to provide support for HCPs who may be at risk for compassion fatigue which could have subsequent impacts on the provision of patient care [ 85 ]. To address the antecedents of compassion fatigue, this scoping review has identified a need for increased staffing, recruitment, and retention efforts on the part of hospital human resources departments [ 23 , 45 ]. Interventions suggested by studies included in the review encompass the monitoring of psychological well-being among HCPs to inform timely provision of resources [ 29 , 45 ]. Specifically, structured debriefing, training on self-care routine, reduced workload, and normalization of trauma-related therapy are essential interventions [ 86 ]. Additionally, a study identified that fostering collaborative workplace culture encourages social and emotional support among staff [ 45 ]. Certain hospitals have adopted “wobble rooms” as a private unwinding and venting space for employees [ 87 ]. Studies have observed that interventions aimed at improving the well-being of HCPs resulted in enhanced quality and safety of care being delivered [ 75 ].
Strengths and limitations
There are both strengths and limitations in this review. Although some literature reviews focused on the psychological health status of HCPs (e.g., burnout, anxiety, depression), very few studies have specifically explored compassion fatigue. Reviews that considered the impact of the COVID-19 pandemic on HCPs were even more limited. It is known that compassion is a cornerstone of quality health care improvement and increases successful medical outcomes [ 88 , 89 , 90 ]. Nevertheless, prolonged exposure to distressing events by HCPs, such as patient death and suffering, results in the absorption of negative emotional responses and leads to the development of compassion fatigue [ 91 ]. This scoping review presents an extensive exploration of the current body of literature on compassion fatigue among HCPs during the COVID-19 pandemic. Another strength in this study lies in the transparency and reproducibility of the methodology. The scoping review protocol has been published in a peer-reviewed journal to establish high methodological standards for the final scoping review [ 92 ]. Additionally, the study plan was pre-registered with Open Science Framework to ensure commitment to the methodology. Double extraction was performed to ensure that a comprehensive descriptive summary of the studies was achieved.
Some limitations include the short time frame chosen for the included studies that were published since the COVID-19, which may have constrained the breadth and quality of the studies. Longitudinal studies may not be captured in the review as this study methodology requires a prolonged period of time to yield meaningful observations. More data is needed to support conclusions on the impact of compassion fatigue on patient care. Additionally, none of the studies included in the review were conducted between March 2021 and May 2023, which may miss out on meaningful trends in levels of compassion fatigue in HCPs. This scoping review only included literature published in English so studies published in other languages were not assessed. Additionally, no comparisons of compassion fatigue were made among the HCP groups in spite of potentially relevant differences such as patient exposure. There was also a lack of allied health profession representation, with the majority of the study population being nurses or physicians. Lastly, grey literature was not included in this scoping review which may delimitate the information included in the scoping review.
There were recurring themes related to limitations in the included research studies. Several studies identified sampling issues including small sample sizes, restricted sample frame, low response rate, and selection error [ 23 , 29 , 31 , 38 , 39 , 40 , 41 , 42 , 43 , 47 , 50 , 51 , 83 ]. Other studies have called for investigations into how different sociodemographic factors, other psychiatric diseases, health care settings, and workplace environment impact compassion fatigue in HCPs [ 38 , 39 , 47 , 48 , 83 ]. One study observed a lack of homogeneity in the sample due to an overrepresentation of female HCPs in the sample [ 38 ]. Lastly, many studies employed a cross-sectional study design which limits the interpretation of the data in terms of causality [ 23 , 30 , 31 , 34 , 42 , 47 , 48 , 50 ]. While there are limitations to the study, a comprehensive summary of existing literature may be useful to inform future research and policies.
Future research is needed to examine the longitudinal impacts of COVID-19 on compassion fatigue in HCPs. Moreover, research in this area could be strengthened by including a consultation phase with external experts on compassion fatigue to improve the robustness of the scoping review.
Conclusions
The COVID-19 pandemic presented a unique set of challenges to healthcare systems across the globe. This scoping review indicated that the prevalence of compassion fatigue was inconsistent across countries and may reflect the variability of pandemic preparedness among the individual countries. Primary risk factors for the development of compassion fatigue included being younger, female, a physician or nurse, and having limited access to PPE in conjunction with an excessive workload and prolonged work hours. The negative impacts of compassion fatigue were experienced at the individual and organizational level. The findings suggest there is a systemic need to assess, monitor and support health professionals’ well-being particularly during conditions of protracted health crises such as a pandemic. In addition, many health systems and sectors are facing a profound health human resources crisis and therefore ongoing efforts must be made to improve workplace environments and increase recruitment and retention efforts. Lastly, pandemic planning must include provisions to support health providers’ ability to safely do their jobs while also minimizing negative impacts to their health and well-being.
Availability of data and materials
All the material presented in the manuscript is owned by the authors and/or no permissions are required.
Coronavirus disease (COVID-19) pandemic. Accessed 16 Jan 2023. https://www.who.int/europe/emergencies/situations/covid-19
Wilder-Smith A, Osman S. Public health emergencies of international concern: a historic overview. J Travel Med. 2020;27(8):taaa227. https://doi.org/10.1093/jtm/taaa227 .
Article PubMed Google Scholar
Gristina GR, Piccinni M. COVID-19 pandemic in ICU. limited resources for many patients: approaches and criteria for triaging. Minerva Anestesiol. 2021;87(12):1367–79. https://doi.org/10.23736/S0375-9393.21.15736-0 .
Chaka EE, Mekuria M, Melesie G. Access to Essential personal safety, availability of personal protective equipment and perception of healthcare workers during the COVID-19 in public hospital in West Shoa. Infect Drug Resist. 2022;15:2315–23. https://doi.org/10.2147/IDR.S344763 .
Article PubMed PubMed Central Google Scholar
Gholami M, Fawad I, Shadan S, et al. COVID-19 and healthcare workers: a systematic review and meta-analysis. Int J Infect Dis. 2021;104:335–46. https://doi.org/10.1016/j.ijid.2021.01.013 .
Article CAS PubMed PubMed Central Google Scholar
Schug C, Geiser F, Hiebel N, et al. Sick Leave and Intention to Quit the Job among Nursing Staff in German Hospitals during the COVID-19 Pandemic. Int J Environ Res Public Health. 2022;19(4):1947. https://doi.org/10.3390/ijerph19041947 .
Lancet T. COVID-19: protecting health-care workers. Lancet Lond Engl. 2020;395(10228):922. https://doi.org/10.1016/S0140-6736(20)30644-9 .
Article Google Scholar
Beck E, Daniels J. Intolerance of uncertainty, fear of contamination and perceived social support as predictors of psychological distress in NHS healthcare workers during the COVID-19 pandemic. Psychol Health Med. Published online July 6, 2022:1–13. https://doi.org/10.1080/13548506.2022.2092762.
Nikeghbal K, Kouhnavard B, Shabani A, Zamanian Z. Covid-19 effects on the mental workload and quality of work life in Iranian nurses. Ann Glob Health. 2021;87(1):79. https://doi.org/10.5334/aogh.3386.
WHO Coronavirus (COVID-19) Dashboard. Accessed 16 Jan 2023. https://covid19.who.int
Lluch C, Galiana L, Doménech P, Sansó N. The Impact of the COVID-19 pandemic on burnout, compassion fatigue, and compassion satisfaction in healthcare personnel: a systematic review of the literature published during the first year of the pandemic. Healthcare. 2022;10(2):364. https://doi.org/10.3390/healthcare10020364 .
Salmond E, Salmond S, Ames M, Kamienski M, Holly C. Experiences of compassion fatigue in direct care nurses: a qualitative systematic review. JBI Evid Synth. 2019;17(5):682. https://doi.org/10.11124/JBISRIR-2017-003818 .
Sinclair S, Raffin-Bouchal S, Venturato L, Mijovic-Kondejewski J, Smith-MacDonald L. Compassion fatigue: A meta-narrative review of the healthcare literature. Int J Nurs Stud. 2017;69:9–24. https://doi.org/10.1016/j.ijnurstu.2017.01.003 .
Majid U, Hussain SAS, Zahid A, Haider MH, Arora R. Mental health outcomes in health care providers during the COVID-19 pandemic: an umbrella review. Health Promot Int. 2023;38(2):daad025. https://doi.org/10.1093/heapro/daad025 .
Rahmani F, Hosseinzadeh M, Gholizadeh L. Complicated grief and related factors among nursing staff during the Covid-19 pandemic: a cross-sectional study. BMC Psychiatry. 2023;23(1):73. https://doi.org/10.1186/s12888-023-04562-w .
Statement on the fifteenth meeting of the IHR (2005) Emergency Committee on the COVID-19 pandemic. Accessed July 6, 2023. https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic
Ghahramani S, Kasraei H, Hayati R, Tabrizi R, Marzaleh MA. Health care workers’ mental health in the face of COVID-19: a systematic review and meta-analysis. Int J Psychiatry Clin Pract. 2022;0(0):1–10. https://doi.org/10.1080/13651501.2022.2101927 .
Article CAS Google Scholar
Nie A, Su X, Zhang S, Guan W, Li J. Psychological impact of COVID-19 outbreak on frontline nurses: a cross-sectional survey study. J Clin Nurs. 2020;29(21–22):4217–26. https://doi.org/10.1111/jocn.15454 .
Jalili M, Niroomand M, Hadavand F, Zeinali K, Fotouhi A. Burnout among healthcare professionals during COVID-19 pandemic: a cross-sectional study. Int Arch Occup Environ Health. 2021;94(6):1345–52. https://doi.org/10.1007/s00420-021-01695-x .
Iddrisu M, Poku CA, Mensah E, Attafuah PYA, Dzansi G, Adjorlolo S. Work-related psychosocial challenges and coping strategies among nursing workforce during the COVID-19 pandemic: a scoping review. BMC Nurs. 2023;22(1):210. https://doi.org/10.1186/s12912-023-01368-9 .
Yang BJ, Yen CW, Lin SJ, et al. Emergency nurses’ burnout levels as the mediator of the relationship between stress and posttraumatic stress disorder symptoms during COVID-19 pandemic. J Adv Nurs. 2022;78(9):2861–71. https://doi.org/10.1111/jan.15214 .
Fukushima H, Imai H, Miyakoshi C, Naito A, Otani K, Matsuishi K. The sustained psychological impact of coronavirus disease 2019 pandemic on hospital workers 2 years after the outbreak: a repeated cross-sectional study in Kobe. BMC Psychiatry. 2023;23(1):313. https://doi.org/10.1186/s12888-023-04788-8 .
Amir K, Okalo P. Frontline nurses’ compassion fatigue and associated predictive factors during the second wave of COVID-19 in Kampala. Uganda Nurs Open. 2022;9(5):2390–6. https://doi.org/10.1002/nop2.1253 .
Calkins K, Guttormson J, McAndrew NS, et al. The early impact of COVID-19 on intensive care nurses’ personal and professional well-being: a qualitative study. Intensive Crit Care Nurs. 2023;76:103388. https://doi.org/10.1016/j.iccn.2023.103388 .
Sexton JB, Adair KC, Proulx J, et al. Emotional exhaustion among US health care workers before and during the COVID-19 Pandemic, 2019–2021. JAMA Netw Open. 2022;5(9):e2232748. https://doi.org/10.1001/jamanetworkopen.2022.32748 .
Slatten LA, David Carson K, Carson PP. Compassion fatigue and burnout what managers should know. Health Care Manag. 2011;30(4):325–33. https://doi.org/10.1097/HCM.0b013e31823511f7 .
Martin J. © Joanna Briggs Institute 2017 Critical Appraisal Checklist for Systematic Reviews and Research Syntheses. Published online 2017.
PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation | Annals of Internal Medicine. Accessed 16 Jan 16 2023. https://www.acpjournals.org/doi/full/ https://doi.org/10.7326/M18-0850?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
Moreno-Mulet C, Sansó N, Carrero-Planells A, et al. The Impact of the COVID-19 Pandemic on ICU healthcare professionals: a mixed methods study. Int J Environ Res Public Health. 2021;18(17):9243. https://doi.org/10.3390/ijerph18179243 .
Labrague LJ, de los Santos JAA. Resilience as a mediator between compassion fatigue, nurses’ work outcomes, and quality of care during the COVID-19 pandemic. Appl Nurs Res. 2021;61:151476.
Su PA, Lo MC, Wang CL, et al. The correlation between professional quality of life and mental health outcomes among hospital personnel during the Covid-19 pandemic in Taiwan. J Multidiscip Healthc. 2021;14:3485–95. https://doi.org/10.2147/JMDH.S330533 .
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implementation Sci. 2010;5:69. https://doi.org/10.1186/1748-5908-5-69 .
Cheng J, Cui J, Yu W, Kang H, Tian Y, Jiang X. Factors influencing nurses’ behavioral intention toward caring for COVID-19 patients on mechanical ventilation: a cross-sectional study. PLoS ONE. 2021;16(11):e0259658. https://doi.org/10.1371/journal.pone.0259658 .
Pérez-Chacón M, Chacón A, Borda-Mas M, Avargues-Navarro ML. Sensory processing sensitivity and compassion satisfaction as risk/protective factors from burnout and compassion fatigue in healthcare and education professionals. Int J Environ Res Public Health. 2021;18(2):611. https://doi.org/10.3390/ijerph18020611 .
Ramaci T, Barattucci M, Ledda C, Rapisarda V. Social Stigma during COVID-19 and its Impact on HCWs Outcomes. Sustainability. 2020;12(9):3834. https://doi.org/10.3390/su12093834 .
Ruiz-Fernández MD, Ramos-Pichardo JD, Ibáñez-Masero O, Cabrera-Troya J, Carmona-Rega MI, Ortega-Galán ÁM. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. J Clin Nurs. 2020;29(21–22):4321–30. https://doi.org/10.1111/jocn.15469 .
Kase SM, Gribben JL, Guttmann KF, Waldman ED, Weintraub AS. Compassion fatigue, burnout, and compassion satisfaction in pediatric subspecialists during the SARS-CoV-2 pandemic. Pediatr Res. 2022;91(1):143–8. https://doi.org/10.1038/s41390-021-01635-y .
Article CAS PubMed Google Scholar
Carmassi C, Dell’Oste V, Bertelloni CA, et al. Gender and occupational role differences in work-related post-traumatic stress symptoms, burnout and global functioning in emergency healthcare workers. Intensive Crit Care Nurs. 2022;69:103154. https://doi.org/10.1016/j.iccn.2021.103154 .
Ruiz-Fernández MD, Ramos-Pichardo JD, Ibáñez-Masero O, Carmona-Rega MI, Sánchez-Ruiz MJ, Ortega-Galán ÁM. Professional quality of life, self-compassion, resilience, and empathy in healthcare professionals during COVID-19 crisis in Spain. Res Nurs Health. 2021;44(4):620–32. https://doi.org/10.1002/nur.22158 .
Yılmaz A, Bay F, Erdem Ö, Özkalp B. The professional quality of life for healthcare workers during the COVID-19 Pandemic in Turkey and the influencing factors. Bezmialem Sci. 2022;10(3):361–9. https://doi.org/10.14235/bas.galenos.2021.5837 .
Missouridou E, Mangoulia P, Pavlou V, et al. Wounded healers during the COVID-19 syndemic: Compassion fatigue and compassion satisfaction among nursing care providers in Greece. Perspect Psychiatr Care. 2022;58(4):1421–32. https://doi.org/10.1111/ppc.12946 . Published online September 10, 2021.
Zakeri MA, Rahiminezhad E, Salehi F, Ganjeh H, Dehghan M. compassion satisfaction, compassion fatigue and hardiness among nurses: a comparison before and during the COVID-19 Outbreak. Front Psychol. 2022;12:815180. https://doi.org/10.3389/fpsyg.2021.815180 .
Austin EJ, Blacker A, Kalia I. “Watching the tsunami come”: a case study of female healthcare provider experiences during the COVID-19 pandemic. Appl Psychol Health Well-Being. 2021;13(4):781–97. https://doi.org/10.1111/aphw.12269 .
Kong KYC, Ganapathy S. Are we in control of our demons?: understanding compassion satisfaction, compassion fatigue and burnout in an asian pediatric emergency department in a pandemic. Pediatr Emerg Care. 2022;38(3):e1058. https://doi.org/10.1097/PEC.0000000000002656 .
Nishihara T, Ohashi A, Nakashima Y, Yamashita T, Hiyama K, Kuroiwa M. Compassion fatigue in a health care worker treating COVID-19 patients: a case report. Biopsychosoc Med. 2022;16(1):10. https://doi.org/10.1186/s13030-022-00239-0 .
Kaya ŞD, Mehmet N, Şafak K. Professional commitment, satisfaction and quality of life of nurses during the COVID-19 Pandemic in Konya. Turkey Ethiop J Health Sci. 2022;32(2):393–404. https://doi.org/10.4314/ejhs.v32i2.20 .
Kottoor AS, Chacko N. Role of entrapment in relation between fear of Covid-19 and compassion fatigue among nurses. Int J Behav Sci. 2022;15(4):250–5. https://doi.org/10.30491/ijbs.2022.288846.1573 .
Stevenson MC, Schaefer CT, Ravipati VM. COVID-19 patient care predicts nurses’ parental burnout and child abuse: Mediating effects of compassion fatigue. Child Abuse Negl. 2022;130:105458. https://doi.org/10.1016/j.chiabu.2021.105458 .
Hochwarter W, Jordan S, Kiewitz C, et al. Losing compassion for patients? The implications of COVID-19 on compassion fatigue and event-related post-traumatic stress disorder in nurses. J Manag Psychol. 2022;37(3):206–23. https://doi.org/10.1108/JMP-01-2021-0037 .
Cuartero-Castañer ME, Hidalgo-Andrade P, Cañas-Lerma AJ. professional quality of life, engagement, and self-care in healthcare professionals in Ecuador during the COVID-19 Pandemic. Healthcare. 2021;9(5):515. https://doi.org/10.3390/healthcare9050515 .
Spiridigliozzi S. Exploring the relationship between faith and the experience of burnout, compassion fatigue, and compassion satisfaction for hospice workers during a global pandemic: a multidisciplinary study. Dr Diss Proj. Published online April 1, 2022. https://digitalcommons.liberty.edu/doctoral/3572
Gribben JL, Kase SM, Guttmann KF, Waldman ED, Weintraub AS. Impact of the SARS-CoV-2 pandemic on pediatric subspecialists’ well-being and perception of workplace value. Pediatr Res. Published online January 20, 2023:1–7. https://doi.org/10.1038/s41390-023-02474-9.
Chien LC, Beÿ CK, Koenig KL. Taiwan’s Successful COVID-19 mitigation and containment strategy: achieving quasi population immunity. Disaster Med Public Health Prep.:1–4. https://doi.org/10.1017/dmp.2020.357.
Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Bio-Medica Atenei Parm. 2020;91(1):157–60. https://doi.org/10.23750/abm.v91i1.9397 .
Kuo S, Ou HT, Wang CJ. Managing medication supply chains: Lessons learned from Taiwan during the COVID-19 pandemic and preparedness planning for the future. J Am Pharm Assoc. 2021;61(1):e12–5. https://doi.org/10.1016/j.japh.2020.08.029 .
Cheng HY, Liu DP. Early Prompt Response to COVID-19 in Taiwan: Comprehensive surveillance, decisive border control, and information technology support. J Formos Med Assoc. Published online November 11, 2022. https://doi.org/10.1016/j.jfma.2022.11.002.
S. Talabis DA, Babierra AL, H. Buhat CA, Lutero DS, Quindala KM, Rabajante JF. Local government responses for COVID-19 management in the Philippines. BMC Public Health. 2021;21:1711. https://doi.org/10.1186/s12889-021-11746-0 .
Rashid N, Nazziwa A, Nanyeenya N, Madinah N, Lwere K. Preparedness, identification and care of COVID-19 cases by front line health workers in selected health facilities in mbale district uganda: a cross-sectional study. East Afr Health Res J. 2021;5(2):144–50. https://doi.org/10.24248/eahrj.v5i2.665 .
Alfonso Viguria U, Casamitjana N. Early Interventions and Impact of COVID-19 in Spain. Int J Environ Res Public Health. 2021;18(8):4026. https://doi.org/10.3390/ijerph18084026 .
Rodríguez-Almagro J, Hernández-Martínez A, Romero-Blanco C, Martínez-Arce A, Prado-Laguna MD, García-Sanchez FJ. Experiences and Perceptions of Nursing Students during the COVID-19 Crisis in Spain. Int J Environ Res Public Health. 2021;18(19):10459.
Dodek PM, Cheung EO, Burns KEA, et al. Moral distress and other wellness measures in Canadian critical care physicians. Ann Am Thorac Soc. 2021;18(8):1343–51. https://doi.org/10.1513/AnnalsATS.202009-1118OC .
Franza F, Basta R, Pellegrino F, Solomita B, Fasano V. The role of fatigue of compassion, burnout and hopelessness in healthcare: experience in the time of covid-19 outbreak. Psychiatr Danub. 32.
Coşkun Şimşek D, Günay U. Experiences of nurses who have children when caring for COVID-19 patients. Int Nurs Rev. 2021;68(2):219–27. https://doi.org/10.1111/inr.12651 .
Scheibe S, De Bloom J, Modderman T. Resilience during crisis and the role of age: involuntary telework during the COVID-19 Pandemic. Int J Environ Res Public Health. 2022;19(3):1762. https://doi.org/10.3390/ijerph19031762 .
Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: Evidence from the field. J Am Med Inform Assoc JAMIA. 2020;27(7):1132–5. https://doi.org/10.1093/jamia/ocaa072 .
Afshari D, Nourollahi-darabad M, Chinisaz N. Demographic predictors of resilience among nurses during the COVID-19 pandemic. Work. 2021;68(2):297–303. https://doi.org/10.3233/WOR-203376 .
Monden KR, Gentry L, Cox TR. Delivering bad news to patients. Proc Bayl Univ Med Cent. 2016;29(1):101–2.
Sorenson C, Bolick B, Wright K, Hamilton R. Understanding compassion fatigue in healthcare providers: a review of current literature. J Nurs Scholarsh. 2016;48(5):456–65. https://doi.org/10.1111/jnu.12229 .
Alharbi J, Jackson D, Usher K. The potential for COVID-19 to contribute to compassion fatigue in critical care nurses. J Clin Nurs. 2020;29(15–16):2762–4. https://doi.org/10.1111/jocn.15314 .
Cohen J, van der Meulen Rodgers Y. Contributing factors to personal protective equipment shortages during the COVID-19 pandemic. Prev Med. 2020;141:106263.
Institute of Professional Psychology, Bahria University Karachi Campus, Karachi, Pakistan, Waris Nawaz M, Imtiaz S, Quaid-i-Azam University Islamabad, Islamabad, Pakistan, Kausar E, Institute of Professional Psychology, Bahria University Karachi Campus, Karachi, Pakistan. self-care of frontline health care workers: during covid-19 pandemic. Psychiatr Danub. 2020;32(3–4):557–62. https://doi.org/10.24869/psyd.2020.557 .
Mano MS, Morgan G. Telehealth, social media, patient empowerment, and physician burnout: seeking middle ground. Am Soc Clin Oncol Educ Book Am Soc Clin Oncol Annu Meet. 2022;42:1–10. https://doi.org/10.1200/EDBK_100030 .
Myronuk L. Effect of telemedicine via videoconference on provider fatigue and empathy: Implications for the Quadruple Aim. Healthc Manage Forum. 2022;35(3):174–8. https://doi.org/10.1177/08404704211059944 .
Abuhammad S, Alzoubi KH, Al‐Azzam S, et al. Stigma toward healthcare providers from patients during COVID‐19 era in Jordan. Public Health Nurs Boston Mass. Published online March 25, 2022: https://doi.org/10.1111/phn.13071
Nashwan AJ, Valdez GFD, AL-Fayyadh S, et al. Stigma towards health care providers taking care of COVID-19 patients: a multi-country study. Heliyon. 2022;8(4):e09300. https://doi.org/10.1016/j.heliyon.2022.e09300 .
Shiu C, Chen WT, Hung CC, Huang EPC, Lee TSH. COVID-19 stigma associates with burnout among healthcare providers: evidence from Taiwanese physicians and nurses. J Formos Med Assoc Taiwan Yi Zhi. 2022;121(8):1384–91. https://doi.org/10.1016/j.jfma.2021.09.022 .
Griffith AK. Parental burnout and child maltreatment during the COVID-19 Pandemic. J Fam Violence. 2022;37(5):725–31. https://doi.org/10.1007/s10896-020-00172-2 .
Çakmak G, Öztürk ZA. Being both a parent and a healthcare worker in the pandemic: who could be exhausted more? Healthcare. 2021;9(5):564. https://doi.org/10.3390/healthcare9050564 .
Cavanagh N, Cockett G, Heinrich C, et al. Compassion fatigue in healthcare providers: a systematic review and meta-analysis. Nurs Ethics. 2020;27(3):639–65. https://doi.org/10.1177/0969733019889400 .
Boufkhed S, Harding R, Kutluk T, Husseini A, Pourghazian N, Shamieh O. What is the preparedness and capacity of palliative care services in Middle-Eastern and North African Countries to Respond to COVID-19? a rapid survey. J Pain Symptom Manage. 2021;61(2):e13–50. https://doi.org/10.1016/j.jpainsymman.2020.10.025 .
Gelfman LP, Morrison RS, Moreno J, Chai E. Palliative care as essential to a hospital system’s pandemic preparedness planning: how to get ready for the next wave. J Palliat Med. 2021;24(5):656–8. https://doi.org/10.1089/jpm.2020.0670 .
Messerotti A, Banchelli F, Ferrari S, et al. Investigating the association between physicians self-efficacy regarding communication skills and risk of “burnout.” Health Qual Life Outcomes. 2020;18:271. https://doi.org/10.1186/s12955-020-01504-y .
Gribben JL, Kase SM, Waldman ED, Weintraub AS. A cross-sectional analysis of compassion fatigue, burnout, and compassion satisfaction in pediatric critical care physicians in the United States. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2019;20(3):213–22. https://doi.org/10.1097/PCC.0000000000001803 .
Sengupta M, Roy A, Gupta S, Chakrabarti S, Mukhopadhyay I. Art of breaking bad news: a qualitative study in Indian healthcare perspective. Indian J Psychiatry. 2022;64(1):25–37. https://doi.org/10.4103/indianjpsychiatry.indianjpsychiatry_346_21 .
Cross LA. Compassion fatigue in palliative care nursing: a concept analysis. J Hosp Palliat Nurs. 2019;21(1):21. https://doi.org/10.1097/NJH.0000000000000477 .
Paiva-Salisbury ML, Schwanz KA. Building compassion fatigue resilience: awareness, prevention, and intervention for pre-professionals and current practitioners. J Health Serv Psychol. 2022;48(1):39–46. https://doi.org/10.1007/s42843-022-00054-9 .
Jun 8, information 2020 | For more, Corpuz-Bosshart contact L. ‘Wobble room’ provides time-out for COVID-19 frontliners. UBC News. Published June 8, 2020. Accessed 17 Jan 2023. https://news.ubc.ca/2020/06/08/making-a-difference-wobble-room-provides-time-out-for-covid-19-frontliners/
Gupta N, Dhamija S, Patil J, Chaudhari B. Impact of COVID-19 pandemic on healthcare workers. Ind Psychiatry J. 2021;30(Suppl 1):S282–4. https://doi.org/10.4103/0972-6748.328830 .
Menon GR, Yadav J, Aggarwal S, et al. Psychological distress and burnout among healthcare worker during COVID-19 pandemic in India—a cross-sectional study. PLoS ONE. 2022;17(3):e0264956. https://doi.org/10.1371/journal.pone.0264956 .
Nishimura Y, Miyoshi T, Sato A, et al. Burnout of healthcare workers amid the COVID-19 Pandemic: a follow-up study. Int J Environ Res Public Health. 2021;18(21):11581. https://doi.org/10.3390/ijerph182111581 .
Jemal K, Hailu D, Mekonnen M, Tesfa B, Bekele K, Kinati T. The importance of compassion and respectful care for the health workforce: a mixed-methods study. J Public Health. 2023;31(2):167–78. https://doi.org/10.1007/s10389-021-01495-0 .
Hui L, Garnett A, Oleyniov C, Boamah S. Compassion fatigue in health providers during the COVID-19 pandemic: A scoping review protocol. BMJ Open. 2023;13:e069843. https://doi.org/10.1136/bmjopen-2022-069843 .
Download references
Acknowledgements
I declare that the authors have no competing interests as defined by BMC, or other interests that might be perceived to influence the results and/or discussion reported in this paper.
Author information
Authors and affiliations.
Arthur Labatt Family School of Nursing, Western University, London, ON, Canada
Anna Garnett & Christina Oleynikov
Medical Sciences, Western University, London, ON, Canada
School of Nursing, McMaster University, Hamilton, ON, Canada
Sheila Boamah
You can also search for this author in PubMed Google Scholar
Contributions
AG is responsible for conception and design of the review. AG, LH, CO & SB contributed to the acquisition and analysis of the data. AG, LH & SB interpreted the data. LH drafted the manuscript and AG was a major contributor to the final version of the manuscript. AG, LH, CO & SB read, provided feedback and approved the final manuscript
Corresponding author
Correspondence to Anna Garnett .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was not required because this manuscript is a review of published literature.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Critical appraisals of included articles.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Garnett, A., Hui, L., Oleynikov, C. et al. Compassion fatigue in healthcare providers: a scoping review. BMC Health Serv Res 23 , 1336 (2023). https://doi.org/10.1186/s12913-023-10356-3
Download citation
Received : 07 August 2023
Accepted : 20 November 2023
Published : 01 December 2023
DOI : https://doi.org/10.1186/s12913-023-10356-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Compassion fatigue
- Healthcare provider
- Psychological health
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- History, Facts & Figures
- YSM Dean & Deputy Deans
- YSM Administration
- Department Chairs
- YSM Executive Group
- YSM Board of Permanent Officers
- FAC Documents
- Current FAC Members
- Appointments & Promotions Committees
- Ad Hoc Committees and Working Groups
- Chair Searches
- Leadership Searches
- Organization Charts
- Faculty Demographic Data
- Professionalism Reporting Data
- 2022 Diversity Engagement Survey
- State of the School Archive
- Faculty Climate Survey: YSM Results
- Strategic Planning
- Mission Statement & Process
- Beyond Sterling Hall
- COVID-19 Series Workshops
- Previous Workshops
- Departments & Centers
- Find People
- Biomedical Data Science
- Health Equity
- Inflammation
- Neuroscience
- Global Health
- Diabetes and Metabolism
- Policies & Procedures
- Media Relations
- A to Z YSM Lab Websites
- A-Z Faculty List
- A-Z Staff List
- A to Z Abbreviations
- Dept. Diversity Vice Chairs & Champions
- Dean’s Advisory Council on Lesbian, Gay, Bisexual, Transgender, Queer and Intersex Affairs Website
- Minority Organization for Retention and Expansion Website
- Office for Women in Medicine and Science
- Committee on the Status of Women in Medicine Website
- Director of Scientist Diversity and Inclusion
- Diversity Supplements
- Frequently Asked Questions
- Recruitment
- By Department & Program
- News & Events
- Executive Committee
- Aperture: Women in Medicine
- Self-Reflection
- Portraits of Strength
- Mindful: Mental Health Through Art
- Event Photo Galleries
- Additional Support
- MD-PhD Program
- PA Online Program
- Joint MD Programs
- How to Apply
- Advanced Health Sciences Research
- Clinical Informatics & Data Science
- Clinical Investigation
- Medical Education
- Visiting Student Programs
- Special Programs & Student Opportunities
- Residency & Fellowship Programs
- Center for Med Ed
- Organizational Chart
- Faculty Affairs Department Teams
- Committee Info (Login Required)
- Recent Appointments & Promotions
- Academic Clinician Track
- Clinician Educator-Scholar Track
- Clinican-Scientist Track
- Investigator Track
- Traditional Track
- Research Ranks
- Instructor/Lecturer
- Social Work Ranks
- Voluntary Ranks
- Adjunct Ranks
- Other Appt Types
- Appointments
- Reappointments
- Transfer of Track
- Term Extensions
- Timeline for A&P Processes
- Interfolio Faculty Search
- Interfolio A&P Processes
- Yale CV Part 1 (CV1)
- Yale CV Part 2 (CV2)
- Samples of Scholarship
- Teaching Evaluations
- Letters of Evaluation
- Dept A&P Narrative
- A&P Voting
- Faculty Affairs Staff Pages
- OAPD Faculty Workshops
- Leadership & Development Seminars
- List of Faculty Mentors
- Incoming Faculty Orientation
- Faculty Onboarding
- Past YSM Award Recipients
- Past PA Award Recipients
- Past YM Award Recipients
- International Award Recipients
- Nominations Calendar
- OAPD Newsletter
- Fostering a Shared Vision of Professionalism
- Academic Integrity
- Addressing Professionalism Concerns
- Consultation Support for Chairs & Section Chiefs
- Policies & Codes of Conduct
- Health & Well-being
- First Fridays
- Fund for Physician-Scientist Mentorship
- Grant Library
- Grant Writing Course
- Mock Study Section
- Research Paper Writing
- Funding Opportunities
- Join Our Voluntary Faculty
- Faculty Resources
- Research by Keyword
- Research by Department
- Research by Global Location
- Translational Research
- Research Cores & Services
- Program for the Promotion of Interdisciplinary Team Science (POINTS)
- CEnR Steering Committee
- Experiential Learning Subcommittee
- Goals & Objectives
- Embryonic Stem Cell Research Oversight
- COVID-19 Vaccinations in CT
- COVID-19 in Connecticut Schools
- Connecticut Towns COVID-19 Impact Dashboard
- Connecticut Town 14-Day Cases Time Lapse
- CT Correctional Facilities with COVID Cases Dashboard
- Connecticut COVID Presence Map
- CT Nursing Homes with COVID-19 Cases
- U.S. COVID Presence Map
- COVID-19 Case Density by US County
- Global Cases Dashboard
- Time-Lapse of Global Spread
- US Racial and Ethnic Disparities in COVID-19 Mortality
- Childcare Survey and Data Display
- Risk of Complications Conditional on COVID-19 Infection
- Travel Time to COVID Testing Sites in Connecticut
- Travel Time to COVID Testing Sites in the US
- Project Team
- Issues List
- Print Magazine PDFs
- Print Newsletter PDFs
- YSM Events Newsletter
- Social Media
- Patient Care
INFORMATION FOR
- Residents & Fellows
- Researchers
Call for Papers - December 2024
Call for papers - dec 2024.
call for papers for the YJBM December 2024 issue on Viruses and Autoimmunity
Call for manuscripts - Viruses and Autoimmunity Submission Deadline: June 19, 2024 Publication Date: December 2024
The Yale Journal of Biology and Medicine ( YJBM ) will be publishing an issue devoted to the topic of Viruses and Autoimmunity. We are inviting authors to submit original research articles, reviews, case reports, or perspectives within this field. Specific subtopics include:
- Molecular mechanisms
- Public health burden
- Global trends and epidemiology
- SARS-CoV-2 and Long COVID
- Treatments: existing and experimental
- Pre-existing autoimmunity, viral infection, and vaccination
- Viral evolution in immunosuppressed hosts
- Case reports
If you are unsure whether your manuscript matches with the issue topic, please reach out to Deputy Editors RuthMabel Boytz ( [email protected] ) and Evan Navori ( [email protected] ).
YJBM is a PubMed-indexed, open-access journal whose mission is to provide graduate students and medical students with experience in writing, reviewing, and publishing articles. The journal has been in publication since 1928 and is supported by an Editorial Board made up of both students and faculty members. Manuscripts are peer-reviewed by faculty in the field and there is no publication fee. The YJBM has a Scopus CiteScore of 5.4 for 2022 and an Impact Factor of 3.434 for 2021.
The length of the manuscript can vary depending on the article type. You can find guidelines for authors on our website ( https://medicine.yale.edu/yjbm/authorguidelines/index.aspx ). As part of YJBM ’s diversity efforts, we offer double-blind peer review. Reviewer bias (conscious or otherwise) should not affect the science that is published. While we encourage you to submit an anonymized manuscript, we also accept unblinded submissions for single-blind review, where only the reviewer names are kept anonymous.
- Share full article
Advertisement
Supported by
Guest Essay
The Problem With Saying ‘Sex Assigned at Birth’

By Alex Byrne and Carole K. Hooven
Mr. Byrne is a philosopher and the author of “Trouble With Gender: Sex Facts, Gender Fictions.” Ms. Hooven is an evolutionary biologist and the author of “T: The Story of Testosterone, the Hormone That Dominates and Divides Us.”
As you may have noticed, “sex” is out, and “sex assigned at birth” is in. Instead of asking for a person’s sex, some medical and camp forms these days ask for “sex assigned at birth” or “assigned sex” (often in addition to gender identity). The American Medical Association and the American Psychological Association endorse this terminology; its use has also exploded in academic articles. The Cleveland Clinic’s online glossary of diseases and conditions tells us that the “inability to achieve or maintain an erection” is a symptom of sexual dysfunction, not in “males,” but in “people assigned male at birth.”
This trend began around a decade ago, part of an increasing emphasis in society on emotional comfort and insulation from offense — what some have called “ safetyism .” “Sex” is now often seen as a biased or insensitive word because it may fail to reflect how people identify themselves. One reason for the adoption of “assigned sex,” therefore, is that it supplies respectful euphemisms, softening what to some nonbinary and transgender people, among others, can feel like a harsh biological reality. Saying that someone was “assigned female at birth” is taken to be an indirect and more polite way of communicating that the person is biologically female. The terminology can also function to signal solidarity with trans and nonbinary people, as well as convey the radical idea that our traditional understanding of sex is outdated.
The shift to “sex assigned at birth” may be well intentioned, but it is not progress. We are not against politeness or expressions of solidarity, but “sex assigned at birth” can confuse people and creates doubt about a biological fact when there shouldn’t be any. Nor is the phrase called for because our traditional understanding of sex needs correcting — it doesn’t.
This matters because sex matters. Sex is a fundamental biological feature with significant consequences for our species, so there are costs to encouraging misconceptions about it.
Sex matters for health, safety and social policy and interacts in complicated ways with culture. Women are nearly twice as likely as men to experience harmful side effects from drugs, a problem that may be ameliorated by reducing drug doses for females. Males, meanwhile, are more likely to die from Covid-19 and cancer, and commit the vast majority of homicides and sexual assaults . We aren’t suggesting that “assigned sex” will increase the death toll. However, terminology about important matters should be as clear as possible.
More generally, the interaction between sex and human culture is crucial to understanding psychological and physical differences between boys and girls, men and women. We cannot have such understanding unless we know what sex is, which means having the linguistic tools necessary to discuss it. The Associated Press cautions journalists that describing women as “female” may be objectionable because “it can be seen as emphasizing biology,” but sometimes biology is highly relevant. The heated debate about transgender women participating in female sports is an example ; whatever view one takes on the matter, biologically driven athletic differences between the sexes are real.
When influential organizations and individuals promote “sex assigned at birth,” they are encouraging a culture in which citizens can be shamed for using words like “sex,” “male” and “female” that are familiar to everyone in society, as well as necessary to discuss the implications of sex. This is not the usual kind of censoriousness, which discourages the public endorsement of certain opinions. It is more subtle, repressing the very vocabulary needed to discuss the opinions in the first place.
A proponent of the new language may object, arguing that sex is not being avoided, but merely addressed and described with greater empathy. The introduction of euphemisms to ease uncomfortable associations with old words happens all the time — for instance “plus sized” as a replacement for “overweight.” Admittedly, the effects may be short-lived , because euphemisms themselves often become offensive, and indeed “larger-bodied” is now often preferred to “plus sized.” But what’s the harm? No one gets confused, and the euphemisms allow us to express extra sensitivity. Some see “sex assigned at birth” in the same positive light: It’s a way of talking about sex that is gender-affirming and inclusive .
The problem is that “sex assigned at birth”— unlike “larger-bodied”— is very misleading. Saying that someone was “assigned female at birth” suggests that the person’s sex is at best a matter of educated guesswork. “Assigned” can connote arbitrariness — as in “assigned classroom seating” — and so “sex assigned at birth” can also suggest that there is no objective reality behind “male” and “female,” no biological categories to which the words refer.
Contrary to what we might assume, avoiding “sex” doesn’t serve the cause of inclusivity: not speaking plainly about males and females is patronizing. We sometimes sugarcoat the biological facts for children, but competent adults deserve straight talk. Nor are circumlocutions needed to secure personal protections and rights, including transgender rights. In the Supreme Court’s Bostock v. Clayton County decision in 2020, which outlawed workplace discrimination against gay and transgender people, Justice Neil Gorsuch used “sex,” not “sex assigned at birth.”
A more radical proponent of “assigned sex” will object that the very idea of sex as a biological fact is suspect. According to this view — associated with the French philosopher Michel Foucault and, more recently, the American philosopher Judith Butler — sex is somehow a cultural production, the result of labeling babies male or female. “Sex assigned at birth” should therefore be preferred over “sex,” not because it is more polite, but because it is more accurate.
This position tacitly assumes that humans are exempt from the natural order. If only! Alas, we are animals. Sexed organisms were present on Earth at least a billion years ago, and males and females would have been around even if humans had never evolved. Sex is not in any sense the result of linguistic ceremonies in the delivery room or other cultural practices. Lonesome George, the long-lived Galápagos giant tortoise , was male. He was not assigned male at birth — or rather, in George’s case, at hatching. A baby abandoned at birth may not have been assigned male or female by anyone, yet the baby still has a sex. Despite the confusion sown by some scholars, we can be confident that the sex binary is not a human invention.
Another downside of “assigned sex” is that it biases the conversation away from established biological facts and infuses it with a sociopolitical agenda, which only serves to intensify social and political divisions. We need shared language that can help us clearly state opinions and develop the best policies on medical, social and legal issues. That shared language is the starting point for mutual understanding and democratic deliberation, even if strong disagreement remains.
What can be done? The ascendance of “sex assigned at birth” is not an example of unhurried and organic linguistic change. As recently as 2012 The New York Times reported on the new fashion for gender-reveal parties, “during which expectant parents share the moment they discover their baby’s sex.” In the intervening decade, sex has gone from being “discovered” to “assigned” because so many authorities insisted on the new usage. In the face of organic change, resistance is usually futile. Fortunately, a trend that is imposed top-down is often easier to reverse.
Admittedly, no one individual, or even a small group, can turn the lumbering ship of English around. But if professional organizations change their style guides and glossaries, we can expect that their members will largely follow suit. And organizations in turn respond to lobbying from their members. Journalists, medical professionals, academics and others have the collective power to restore language that more faithfully reflects reality. We will have to wait for them to do that.
Meanwhile, we can each apply Strunk and White’s famous advice in “The Elements of Style” to “sex assigned at birth”: omit needless words.
Alex Byrne is a professor of philosophy at M.I.T. and the author of “Trouble With Gender: Sex Facts, Gender Fictions.” Carole K. Hooven is an evolutionary biologist, a nonresident senior fellow at the American Enterprise Institute, an associate in the Harvard psychology department, and the author of “T: The Story of Testosterone, the Hormone That Dominates and Divides Us.”
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow The New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Clin Med (Lond)
- v.15(2); 2015 Apr
John Saunders
A College of Health and Human Science, Swansea University, Swansea, UK; chair (2004–14), committee for ethical issues in medicine, Royal College of Physicians, London, UK; consultant physician, Nevill Hall Hospital, Abergavenny, UK
The term ‘compassion’ has been much used and little discussed. I argue that compassion is a virtue in the Aristotelian sense, one of a family of other-regarding properties and belongs to the affective qualities of a moral agent. Its exercise is an essential component of good medical care in many situations and requires grounding in moral principles. Although our dispositions vary, compassion is a quality that can be developed in all of us.
Thinking about compassion
Compassion has had a good outing recently. Compassion has been the missing factor in care. One prominent member of parliament, Ann Clwyd, raised the public profile of the lack of compassion she witnessed in the care of her dying father. She claimed an avalanche of correspondence that attested to similar experiences. 1 The Health Services ombudsman, Mrs Ann Abrahams, reported on a failure to respond with compassion in her inquiry on the care of elderly and frail patients in 2011. 2 Failures in compassionate care were also reported by the Care Quality Commission in 2011 3 and the Healthcare Commission in 2007. 4 A lack of compassion was a prominent theme in the Francis Report into failings in the Mid Staffordshire NHS Foundation Trust, 5 even advocating that training was required in compassionate care (recommendation 185) and that an aptitude test for compassion should be introduced (recommendation 188). The Royal College of Physicians emphasised that doctors should ‘display compassion in their daily work’, 6 while its Future Hospital Commission entitled one of its chapters ‘building a culture of compassion and respect’. 7 Compassion seems to be important in healthcare and its deficiency a failing.
In all this comment, there is an assumption that we all know what compassion means. Its meaning is rarely analysed. It is just assumed to be a good thing. Yet we might want to ask, is it always needed? Or can there be too much compassion? Is its demonstration always to be ‘displayed’ as part of the carer's duty or is it some sort of additional extra for those of an appropriate disposition?
Compassion features in two famous stories that have become part of our culture: the stories of the prodigal son and that of the Good Samaritan. (Even the Medical Defence Union refers to ‘emergency (Good Samaritan) acts’. 8 ) I select these stories, not because of their provenance, but simply as well known tales that illustrate what I want to say. In the former, a son takes his inheritance, spends it and, after reducing himself to misery, chooses to return. His father recognises his returning wastrel son and the writer says he ‘had compassion and ran…and kissed him. 9 ’ This translates in a standard modern text as ‘his heart went out to him. 10 ’ In the latter, the Samaritan sees a half-dead man on the road, who has been ignored by establishment figures who walk by, and ‘when he saw him, he had compassion on him. 11 ’ Again, a modern text translates this as ‘when he saw him, he was moved to pity. 12 ’ The common feature in both of these stories is that compassion features essentially as an emotional, and not a rational response. It is an expression of the character of the individuals, not the direct result of their principles. Compassion is here a virtue.
A similar conclusion is equally explicit in Aristotle's Rhetoric . 13 Although this translates as ‘pity’, it is clearly compassion to which Aristotle refers. This is defined as ‘a feeling of pain at an apparent evil, destructive or painful, which befalls one who does not deserve it, and which we might expect to befall ourselves or some friend of ours’. Again, this definition asserts compassion as part of our emotional, and not our rational, lives. In our ordinary discourse, we talk about being moved by compassion or feeling compassion. Compassion is therefore part of a moral relationship that involves moral psychology as well as moral philosophy. Aristotle says that to feel it, we must ‘obviously be capable of supposing that some evil may happen to us or some friend of ours, and moreover some such evil as is stated in our definition or is more or less of that kind.’ The central idea is ‘that could be me.’
In Snow's analysis, 14 compassion is one of a family of other-regarding emotions that include pity, sympathy and grief, all evoked in response to an object that is negative: a misfortune or loss. It therefore requires a belief about that negativity and its sufferer, making compassion a composite of belief and feeling. To take an alternative example, it would be seen as natural enough to grieve for the death of someone we love, but if we discover them to be alive, then continued grief would be irrational. Compassion has a cognitive component. We would (and should) cease to feel it, if we discover that the supposed sufferer is deliberately faking it. Psychologically it requires an imaginative indwelling into the condition of another, requiring identification with the victim. Compassion has an immediacy, a proximity and an urgency. We may feel sorrow or pity or concern for the victims of a disaster far removed from us, but we do not feel compassion. Compassion belongs at the patient's bedside or sick room, not in the office of the public health physician or epidemiologist. Those doctors qua doctors at least can do without it, for they do not deal with individual suffering patients. Compassion crosses an emotional distance between ourselves and the sufferer's plight. Snow states, ‘the ability to identify with another's distress makes the other's suffering real to those who feel compassion, and facilitates benevolent desires for the other's good.’ It also implies a relatively serious condition: we may feel sympathy for someone who has cut their finger, but not compassion. By contrast, sympathy is too weak for one who is in distress from serious illness and compassion more appropriate.
Compassion as rational?
The ability to identify with the suffering of another or to imagine ourselves in a similar state varies between individuals. (If consciousness is understood as the ability to experience the environment, internal or external to ourselves, then the unconscious cannot suffer.) Not all have the talent for imaginative indwelling well developed. Where moral action stems from altruistic concern for the benefit of another, inclination will vary according to the development of our moral appetites. It is not irrational not to feel compassion. However, the uncomfortable conclusion is then that persons could be considered of unequal instrumental value, to be valued according to how often they’re able to feel compassion and how effectively they can act for another's benefit on its basis. For Snow, a broader construal of ‘rational’ incorporates a person as rationally responding to the world on the basis of true, or at least justified, beliefs. If people have a common susceptibility to misfortune, it is rational to want a world (or a hospital) where others can be viewed as possible helpers: a kinder, gentler society.
A morality that grounds itself entirely in the virtues will leave a great deal optional in healthcare. The development of the character of the moral agent requires the grounding in defensible principles. To express that technically, virtue ethics require principlism. If compassion is something to be displayed in the doctor's daily work, it should be more than an option. Perfectionist demands may lead to ‘burnout’ but equally minimalism shouldn't be defended in saying ‘I’m just not like that’. Somehow compassion has to be brought within the ambit of duty – which is to say, within the professional's obligations and not, or not only, within the province of the supererogatory.
The difficulty of imaginative indwelling is that of transposing one's own views into another person. People vary in what constitutes suffering. Backgrounds, values, culture, needs and understanding all vary. Moreover, such understanding of another requires an intimacy with them. This will be most apparent in the management of chronic disease, especially the vulnerable and highly dependent. ‘Imaginative understanding of suffering can at times be a worthy achievement like other medical achievements. 15 ’ Compassion cannot be learned by observing the behaviour of seniors as role models – not least because not all senior figures in medicine exhibit this quality to an inspiring or even adequate degree – nor can it be permanently instilled by courses in human values, or the reflection on suitable film, literature, case studies and so on: much as these may help. Medical humanities has its place in the curriculum and the teaching of virtue ethics (see examples in the following publications 16–18 ) should certainly take its place alongside the current overemphasis on four principles. However, what can be asserted is that compassion may be snuffed out by environments that discourage its expression, a factor that is more important than individual role models. Poor behaviour can easily result from adverse political and excessively mechanical or managerial viewpoints – major factors in recent incidents.
Compassion is more than good manners, although it is hard to imagine a compassionate doctor who is ill mannered and discourteous. But compassion is not required in many situations. Much illness is minor, may be unfortunate, but hardly tragic or even upsetting for its victim. A migraine attack, an attack of influenza or a mild short-lived episode of gastroenteritis, are unpleasant; so too are long-term conditions such as an arthritic joint, strabismus or a trigger finger. Compassion as a necessary response from the health carer is then overstated. Rather what is required is respect or courtesy. Kahn 19 suggests that patients may care less about whether their doctors are reflective and empathic than whether they are respectful and attentive: good eye contact, body language, dress and manners. Whereas compassion is an emotion, etiquette is a function. Compassion concerns what is felt and etiquette, in what is done. Whether compassion can be taught has been much discussed; nobody doubts that etiquette can be taught – Kahn even proposes a check list that can be evaluated and practised. It is easier to change behaviour than attitudes.
Reconciling attitudes and behaviour
Yet these two may not be so far apart. Attitudes may owe much to our upbringing and genes; but equally, we need skills in developing and applying appropriate attitudes in clinical practice and knowledge both to assess that appropriateness and to develop those attitudes in the first place. Aristotle writes: 20
Now true virtue cannot exist without prudence any more than prudence without virtue…Virtue is not merely a disposition in conformity with the right principle but a disposition in collaboration with the principle, which in human conduct is prudence. So, while Socrates thought that the virtues are principles, we say that they work along with a principle. So we see from these arguments that it is not possible to be good in the true sense of the word without prudence or to be prudent without virtue.
And dispositions can be developed through practice. Lewis 21 uses the analogy of a tennis player:
Someone who is not a good tennis player may now and then make a good shot. What you mean by a good player is the man whose eye and muscles and nerves have been so trained by making innumerable good shots that they can now be relied on. They have a certain tone or quality which is there even when he is not playing, just as a mathematician's mind has a certain habit and outlook which is there even when he is not doing mathematics. In the same way, a man who perseveres in doing just actions gets in the end a certain quality of character. Now it is that quality rather than the particular actions which we mean when we talk of a ‘virtue’.
Dispositions are formed by repeated intentionality and right actions. Reich 22 further suggests that neglect of compassion may relate to an inability to explain the meaning of suffering for the individual. An account of compassion must begin, in his view, with a definition and an account of suffering. Suffering is different from pain.
It is an anguish which we experience on one level as a threat to our composure, our integrity, and the fulfilment of our intentions but at a deeper level as a frustration to the concrete meaning that we have found in our personal existence. It is the anguish over the injury or threat of injury to the self – and thus to the meaning of the self that is at the core of suffering.
Such anguish may include the sense of unfairness at being deprived of life's possibilities, or the sense of loss of control or the feeling of shame that might accompany dependency. Autonomy suffers whether the patient is mute or expressive in response. Compassionate others offer solidarity which can transform suffering. The iteration between the suffering patient and the compassionate person was about narrative and is only possible if the suffering can be understood. Narrative plays its part in palliative medicine in terms of interacting with patients, getting information and helping them to change their perceptions, so they are controlling circumstances and not being controlled. Recognition, review, revision and reconciliation are part of the narrative, helping to develop a new voice and a new story. Behaviour and manners matter in helping patients, but attitude is key. Compassion is a virtue.
Finding a voice
This account of how to engage with suffering is probably unfamiliar to many physicians and moves from problem solving to active listening and empowerment. The system has risks in terms of transference, countertransference, compassion fatigue and crossing personal and professional boundaries. It requires skills and supervision, but works. Sometimes, writes Reich, compassion may help to find a voice for the voiceless. RS Thomas says, 23 ‘we have all been victims of vocabulary too long.’ In her essay ‘On being ill’, Virginia Woolf writes: 24
Finally…there is the poverty of language…the merest schoolgirl when she falls in love has Shakespeare or Keats to speak her mind for her; but let a sufferer try to describe a pain in his head to a doctor and language at once runs dry. There is nothing ready made for him. He is forced to coin words himself and, taking his pain in one hand and a lump of pure sound in the other (as perhaps the people of Babel did in the beginning) so to crush them together that a brand new word drops out. Probably it will be laughable…Yet it is not only a new language that we need…but a new hierarchy of the passions; love must be deposed in favour of a temperature of 104…sleeplessness play the part of the villain and the hero become a white liquid with a sweet taste – a mighty Prince with moths eyes and feathered feet.
Compassion may need skill in language and cultural understanding to be effective. Cultural understanding and language skills can certainly be taught, even if compassion demands silence on some occasions: a waiting only. And it also demands a sense of mutuality that is difficult for those who still express the traditional paternalistic benevolence of the doctor.
Compassion often requires time. It is hard to be compassionate after several hours coping with a series of distressing emergencies: sheer physical exhaustion and continuing pressure with a limited resource puts the ideal out of reach. It may be impossible to respond adequately in the face of a tide of human misery: imagine the experience of those dealing with the victims of a bombing or a poison gas attack arriving in overwhelming numbers. Healthcare workers can only do the best in the circumstances, but in developed countries in peace time there is a responsibility of health service management to promote the conditions under which compassionate care is possible. Schulz 25 points out some of the difficulties. Programmes, such as respite care or caregiver skills training, will not impact on caregiver distress unless they impact on the patient's suffering. We would benefit from better research on the factors that contribute to patient suffering and the healthcarer's compassion: contact time, personal relationships between professional and sufferer, and resources. It cannot be accepted that because the medical profession is innovative, even radical, in terms of scientific change, that it will also be open to social change that affects its authority and autonomy. 26 In the light of recent events, medical education may have to be modified to place a greater emphasis on the personal qualities that arise in the doctor–patient relationship and less on teaching and assessment of reliably and objectively measured technical and factual knowledge. 27 The question of Plato's Meno 28 may be unanswered as to whether compassion can be taught, but we should reject Socrates’ conclusion that a virtue like compassion is merely a ‘gift of the gods’.
Acknowledgement
This paper was discussed in the Committee for Ethical Issues in Medicine, Royal College of Physicians and I am grateful for comments made there.

IMAGES
VIDEO
COMMENTS
Introduction. Compassion is one of the most important virtues in medicine, expected from medical professionals and anticipated by patients (Frampton et al., 2013; Fernando and Consedine, 2014a).Despite evidence of its centrality to effective clinical care, most research has focused on compassion fatigue and burnout (Fernando and Consedine, 2014a, b), neglecting the study of compassion itself ...
1) Empathetic doctors: those who naturally grasp that the whole point of empathy is to focus attention on the patient. 2) Doctors who have successfully attended a doctor patient communication skills course. Communication skills can be taught. For example, a good technique for showing compassion, is simple: 3 T's.
Background Compassionate care lies at the foundation of good patient care and is a quality that patients and providers continue to value in the fast-paced setting of contemporary medicine. Compassion is often discussed superficially in medical school curricula, but the practical aspect of learning this skill is often not taught using a formal framework. In the present work, the authors present ...
The release of Compassionomics: The Revolutionary Scientific Evidence That Caring Makes a Difference, authored by physician-scientists Stephen Trzeciak and Anthony Mazzarelli, has ignited a conversation on the relationship between physician compassion and patient outcomes.. Stanford Medicine's Emma Seppala discussed the topic with Trzeciak and Mazzarelli in a recent Q&A in the Washington Post.
1. INTRODUCTION. Compassion has been defined as an emotion, 1 a motivation 2 and a virtuous response. 3 At the least, it involves both feeling and action components 2 , 4 , 5 the awareness of suffering and acting to alleviate it. 6 In medicine, compassion is desired by patients, mandated by medical regulatory bodies and increasingly linked to positive outcomes for patients and families ...
Background. A previous review on compassion in healthcare (1988-2014) identified several empirical studies and their limitations. Given the large influx and the disparate nature of the topic within the healthcare literature over the past 5 years, the objective of this study was to provide an update to our original scoping review to provide a current and comprehensive map of the literature to ...
Welie, Jos. "Sympathy as the Basis of Compassion". Cambridge Quarterly of Healthcare Ethics 4 (1995): 476-487. This research paper, "Compassion in Medicine and Healthcare" is published exclusively on IvyPanda's free essay examples database. You can use it for research and reference purposes to write your own paper.
In my opinion, medical professionalism involves demonstrating humility and compassion. Modern medicine has established a culture defined by entitlement and conceit, and humility indicates weakness or false modesty. 6 Having the confidence to tackle my insecurities is paramount to my development as a doctor.
C ompassion is considered a core value in the practice of medicine and an essential cornerstone of caring for patients. Patients expect compassion from their health care providers, 1 and a recent survey found that 85% of patients and 91% of doctors value compassion. 2 Furthermore, the desire to help those suffering from disease and disability is prominently included among stated reasons for ...
While my compassion serves as the driving force behind my desire to pursue medicine, I firmly believe that a sound scientific foundation is essential for providing the highest quality of care. Throughout my undergraduate studies in biology, I have relished in the intricate details of molecular processes and the complexities of the human body.
The necessity of compassion and teamwork are recognized as essential tools to improve patient satisfaction and enhance the development of communication to solve health conditions of patients. This essay highlights the concept and significance of both 'teamwork' and 'compassion' and draws relevance as a current medical student and future ...
Results: Compassion is the emotional response to another's pain or suffering, accompanied by a desire to alleviate it. Review of the literature shows that compassionate health care measurably improves physical and psychological patient outcomes, increases patient adherence, improves health care quality and safety, increases financial margins ...
Background. Compassion is extolled as a cornerstone of quality healthcare by patients, families, clinicians, and policy makers [1-5].The necessity of compassion within healthcare is evident in the first principle of the American Medical Association [] Code of Ethics that states, "A physician shall be dedicated to providing competent medical care, with compassion and respect for human ...
Med School Applicants Should Highlight Compassion. Show admissions committees that you are committed to increasing your level of compassion as an aspiring doctor. Compassion is important because ...
The winning essays will be published in consecutive issues of Academic Medicine and the Journal of Professional Nursing in the fall/winter of 2023. The contest is named for Hope Babette Tang-Goodwin, MD, who was an assistant professor of pediatrics and an exemplar of humanism in healthcare. Her approach to medicine combined a boundless ...
Essay, Pages 6 (1303 words) Views. 494. Compassion, health disparities and social justice in health care are topics that have been discussed for decades and both have been examined from the lens of public health policies and education as well as ethics. Compassion is defined as the "sensitivity to suffering in self and others with a ...
In this essay, I will explore the importance of my passion for medicine, highlighting its significance in improving lives, advancing scientific knowledge, and fostering a culture of compassion and empathy. To fully appreciate the importance of medicine, we must first recognize its fundamental purpose: to alleviate suffering and promote well-being.
REVIEW. In her essay for medical school, Morgan pitches herself as a future physician with an interdisciplinary approach, given her appreciation of how the humanities can enable her to better ...
However, training physicians to effectively communicate compassion is challenging. This study explores how medical students experienced training focused on interacting with patients by examining students' reports of particularly memorable lessons. Six focus groups were conducted with medical students (total n = 48) in their fourth year of ...
The detrimental impacts of COVID-19 on healthcare providers' psychological health and well-being continue to affect their professional roles and activities, leading to compassion fatigue. The purpose of this review was to identify and summarize published literature on compassion fatigue among healthcare providers and its impact on patient care. Six databases were searched: MEDLINE (Ovid ...
Compassion in Medicine | Reflective Essay. Advancements in medical technology have given rise to medicalization, a process where 'non-medical' problems have become understood and treated as 'medical' issues. 1 This potentially objectifies humans, leading to "deindividuation" 2, where doctors identify patients by their disease or ...
The RCGP motto is — scientific knowledge applied with compassion. will be defined here as the open-heartedness or generosity of spirit demonstrated by a doctor or nurse when caring for a patient. It will be used synonymously with kindness, compassion, altruism, and generosity because space does not permit a more detailed exploration here.
Call for manuscripts - Viruses and Autoimmunity. Submission Deadline: June 19, 2024. Publication Date: December 2024. The Yale Journal of Biology and Medicine ( YJBM) will be publishing an issue devoted to the topic of Viruses and Autoimmunity. We are inviting authors to submit original research articles, reviews, case reports, or perspectives ...
As you may have noticed, "sex" is out, and "sex assigned at birth" is in. Instead of asking for a person's sex, some medical and camp forms these days ask for "sex assigned at birth ...
In Snow's analysis, 14 compassion is one of a family of other-regarding emotions that include pity, sympathy and grief, all evoked in response to an object that is negative: a misfortune or loss. It therefore requires a belief about that negativity and its sufferer, making compassion a composite of belief and feeling.
Compassion in Medicine | Reflective Essay. Advancements in medical technology have given rise to medicalization, a process where 'non-medical' problems have become understood and treated as 'medical' issues. 1 This potentially objectifies humans, leading to "deindividuation" 2, where doctors identify patients by their disease or ...