

How to write a Critical Analysis in Nursing – Full Guide and Examples
- Dr. Rachel Andel
- August 9, 2022
- Nursing Writing Guides
How to write a Critical Analysis in Nursing
Nursing is a demanding and highly specialized field that requires critical analysis. Whether you are a new nurse or have been working in the field for years, writing a critical analysis can be daunting. In this article, we will show you how to write a critical analysis in nursing using a step-by-step process.
What is a Critical Analysis in nursing?
A Critical Analysis is a comprehensive, in-depth analysis of a text or piece of media. It can be used to explore the author’s intentions, analyze the plot, assess the characters, and determine the overall impact of the work.
As you continue, nursingstudy.org/ has the top and most qualified writers to help with any of your assignments. All you need to do is place an order with us.
Why is it important to do a Critical Analysis?
Critical Analysis skills are essential for nurses as they work in both clinical and academic settings. They are also important for students who want to develop analytical skills and read critically. In addition, Critical Analyses provide nursing staff with insights into how other people have viewed a particular text or piece of media. This information can help nurses make informed decisions about patient care.
How do I do a Critical Analysis?
There is no one way to do a Critical Analysis. However, there are some key steps that you should take into account when undertaking this type of analysis:
1) Read the text or piece of media carefully;
2) Identify the main themes and ideas presented in the text;
3) Analyze these themes and ideas in depth;
4) Weigh each theme and idea against one another;
5) Write your analysis in an objective manner;
If you are a nursing student looking to learn how to write a critical analysis, you have come to the right place. In this article, we will teach you the basics of writing a critical analysis, including what to include and why. We will also provide some tips for how to structure your essay so that it is clear and easy to read. Finally, we will provide a sample critical analysis of a fictional novel to help you get started.
There are a few steps in writing a critical analysis of literature. In this article, we will discuss the different steps involved in writing a critical analysis and give you an example of how to go about it.
Step One: Choose Your Literature
The first step is to choose the literature you would like to analyze. This could be anything from a journal article to a novel. Once you have chosen your work, it is time to read it with an open mind. When reading any piece of literature, try to focus on the author’s purpose and message. Note what is important to them and how they communicate their ideas. After reading the work, take some time to formulate your thoughts about it in writing.
Step Two: Analyze the Text
Once you have formed your thoughts about the text, it is time to begin analyzing it. In order to do this, you will need to pay close attention to the author’s use of language and structure. Do they use specific words or phrases frequently? Why or why not? How does their choice of words affect their meaning? Are there any specific passages which stand out as particularly effective or ineffective? Once you have analyzed the text,write down your thoughts in a clear and concise manner.
Step Three: Evaluate the Theme and Ideas
Once you have analyzed the text, it is time to look at the main themes and ideas. What are they? What does the author want readers to take away from the work? Are the themes consistent throughout the text? How do the different themes connect? Once you have identified the main themes and ideas, write about them in your analysis. Do you think they are effectively communicated? Are there any elements of the text that you don’t agree with?
Step Four: Consider Your Opinion
After analyzing and evaluating the text, it is important to share your thoughts with readers. In writing a critical analysis, it is important to be objective. This means that you should not express your own opinions or biases in your writing. Instead, focus on providing readers with an objective perspective on the work. Is it worth reading? Why or why not? Is there anything else you would like to say about it?
How to format a Critical Analysis in Nursing
Critical analysis template.
Introduction
• Develop a topic sentence in which you will define the purpose of the Research Critique • Formulate a thesis statement which briefly provides a broad indication of your point of view in composing this assignment . • Include a summary outline to describe the organization and main topics you will include in the body paragraphs of the assignments (see below sections). Protection of Human Participants • Identify the benefits and risks of participation addressed by the authors. Were there benefits or risks the authors do not identify? • Was informed consent obtained from the subjects or participants? • Did it seem that the subjects participated voluntarily in the study? • Was institutional review board approval obtained from the agency in which the study was conducted?
Data Collection • Are the major variables (independent and dependent variables) identified and defined? What were these variables? • How were data collected in this study? • What rationale did the author provide for using this data collection method? • Identify the time period for data collection of the study. • Describe the sequence of data collection events for a participant.
Data Management and Analysis • Describe the data management and analysis methods used in the study. • Did the author discuss how the rigor of the process was assured? For example, does the author describe maintaining a paper trail of critical decisions that were made during the analysis of the data? Was statistical software used to ensure accuracy of the analysis? • What measures were used to minimize the effects of researcher bias (their experiences and perspectives)? For example, did two researchers independently analyze the data and compare their analyses?
Findings / Interpretation of Findings: Implications for Practice and Future Research • What is the researcher’s interpretation of findings? • Are the findings valid or an accurate reflection of reality? Do you have confidence in the findings? • What limitations of the study were identified by researchers ? • Was there a coherent logic to the presentation of findings? • What implications do the findings have for nursing practice? For example, can the study findings be applied to general nursing practice, to a specific population, to a specific area of nursing? • What suggestions are made for further studies?
Conclusion • Emphasize the importance and congruity of the thesis statement • Provide a logical wrap-up to bring the appraisal to completion and to leave a lasting impression and take-away points useful in nursing practice. • Incorporate a critical appraisal and a brief analysis of the utility and applicability of the findings to nursing practice. • Integrate a summary of the knowledge learned. Place your order now for a similar paper and have exceptional work written by our team of experts to guarantee you A Results.
Critical Analysis Essay Example Outline
Title: A critical analysis of a health promotion intervention: Diabetes effecting Schizophrenia patients
- A 2000 word essay based on a health promotion on Diabetes effecting Schizophrenia patients
- Activity that you have undertaken (or closely participated in) whilst on clinical placement.
- A rationale for the importance/necessity of the health promotion (hp) intervention that includes relevant epidemiological data and relates to contemporary health and/or social policy
- Application of a suitable health promotion model and/ or behaviour change theory to the activity undertaken.
- Critical consideration of health literacy in both the delivery of the health promotion activity and any supporting materials used.
- An evaluation of your health promotion activity.
• You need to demonstrate sound understanding of health promotion policy, evidence and theory related to your topic area. • You will not be able to address every health promotion theory, choose one model only and apply this to your topic; • Your essay should have a logical structure and have a systematic approach to care based on the Nursing Process. • Consider a paragraph for each concept and aspect of your essay.
Critical analysis requires objectivity and a critical perspective. It allows nurses to assess their own practice as well as the practices of others. To be effective, critical analysis must be structured and organized . The following steps can help you format a critical analysis:
1) Identify the purpose of the critical analysis. 2) Identify the literature that will be used in the analysis. 3) distill the information from the literature into a clear, concise, and objective statement. 4) Evaluate the strengths and weaknesses of the theory or practice being analyzed. 5) Suggest ways that the theory or practice could be improved.
The purpose of this critical analysis is to improve understanding of the strengths and weaknesses of a particular theory or practice used in nursing. The literature that will be used in this analysis includes both academic sources and clinical practice .
The information from the literature will be distilled into a clear, concise, and objective statement. The strengths and weaknesses of the theory or practice being analyzed will be evaluated. Suggestions for improving the theory or practice will be made.
How to write the introduction of a critical analysis paper
In order to write a successful introduction to your critical analysis paper, you must first establish the purpose of the paper. The purpose of this paper should be clear from the title and introduction, and should help to orient the reader towards your main points.
Once you have determined the purpose of your paper, you must introduce the reader to your main argument. You should begin by explaining why you believe that your chosen topic is important, and then provide evidence to support your claim. You may also want to mention any relevant historical or literary context, in order to give your argument a greater sense of resonance.
Finally, you should wrap up your introduction by stating how readers can use your paper as a blueprint for their own critical analysis work.
In conclusion, make sure that your introduction is concise and well-organized, so that readers will easily understand what lies ahead in the paper.
If you have any questions or would like help with writing your introduction , please don’t hesitate to reach out to one of our professional writers .
How to write the conclusion of a critical analysis paper in Nursing
The conclusion of a critical analysis paper in nursing is an important part of the paper. It should provide a summary of the main points made in the body of the essay, as well as give readers a sense of what the writer believes about the subject matter.
Capella University Nursing Quality Key Indicator Discussion
It should also provide a suggestion for future research or teaching on the topic.
When writing a conclusion for a critical analysis paper, it is important to keep in mind the purpose of the essay.
The goal is not to provide an exhaustive review of all aspects of the subject matter, but rather to provide readers with an overview of what has been discussed and to offer some ideas for further exploration. This means that conclusions should be brief and to the point.
It is also important to remember that conclusions do not have to be original or unique. In fact, they can often be based on ideas that have been introduced throughout the essay.
Rather than coming up with new ideas on their own, it can be helpful to borrow from other sources when writing a conclusion.
This will help to ensure that your argument is sound and that readers will understand your position on the subject matter.
Nursing Concept Map example pdf on RSV Bronchiolitis/Bronchiolitis
When writing the conclusion of a critical analysis paper , it is important to be concise and to provide the reader with a clear understanding of your argument. Here are some tips on how to write a conclusion that meets these goals:
– Summarize your main points and support them with evidence. – State your conclusions clearly and concisely. – Offer a solution or recommendations for future research

Working On an Assignment With Similar Concepts Or Instructions?
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started. Simply:
- Place your order ( Place Order )
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Have a subject expert Write for You Now
Have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, what you'll learn.
Working On A Paper On This Topic?
Use our nursing writing service and save your time. We guarantee high quality, on-time delivery, and 100% confidentiality.
- Nursing Careers
- Nursing Paper Solutions
- Nursing Theories
- Nursing Topics and Ideas
Related Posts
- How to become a Hospice Nurse
- How to Become a Labor and Delivery Nurse
- Role of an Intensive Care Unit Nurse: How to Become, Role and Requirements
Important Links
Knowledge base, paper examples, nursing writing services.
Nursingstudy.org helps students cope with college assignments and write papers on various topics. We deal with academic writing, creative writing, and non-word assignments.
All the materials from our website should be used with proper references. All the work should be used per the appropriate policies and applicable laws.
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Phone: +1 628 261 0844
Mail: [email protected]

We Accept:

@2015-2024, Nursingstudy.org
- Cancer Nursing Practice
- Emergency Nurse
- Evidence-Based Nursing
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- RCN Nursing Awards
- Nursing Live
- Nursing Careers and Job Fairs
- CPD webinars on-demand
- --> Advanced -->

- Clinical articles
- CPD articles
- CPD Quizzes
- Expert advice
- Clinical placements
- Study skills
- Clinical skills
- University life
- Person-centred care
- Career advice
- Revalidation
Art & Science Previous Next
Academic writing: using literature to demonstrate critical analysis, kathleen duffy senior lecturer, school of nursing, midwifery and community health, glasgow caledonian university, glasgow, elizabeth hastie senior lecturer, school of nursing, midwifery and community health, glasgow caledonian university, glasgow, jacqueline mccallum senior lecturer, school of nursing, midwifery and community health, glasgow caledonian university, glasgow, valerie ness lecturer, school of nursing, midwifery and community health, glasgow caledonian university, glasgow, lesley price lecturer, school of nursing, midwifery and community health, glasgow caledonian university, glasgow.
When writing at degree level, nurses need to demonstrate an understanding of evidence by summarising its key elements and comparing and contrasting authors’ views. Critical analysis is an important nursing skill in writing and in practice. With the advent of an all-degree profession, understanding how to develop this skill is crucial. This article examines how students can develop critical analysis skills to write at undergraduate degree level. It highlights some of the common errors when writing at this academic level and provides advice on how to avoid such mistakes.
Nursing Standard . 23, 47, 35-40. doi: 10.7748/ns2009.07.23.47.35.c7201
This article has been subject to double blind peer review
Critical appraisal - Education: methods - Literature and writing - Student nurses - Study skills
User not found
Want to read more?
Already have access log in, 3-month trial offer for £5.25/month.
- Unlimited access to all 10 RCNi Journals
- RCNi Learning featuring over 175 modules to easily earn CPD time
- NMC-compliant RCNi Revalidation Portfolio to stay on track with your progress
- Personalised newsletters tailored to your interests
- A customisable dashboard with over 200 topics
Alternatively, you can purchase access to this article for the next seven days. Buy now
Are you a student? Our student subscription has content especially for you. Find out more

29 July 2009 / Vol 23 issue 47
TABLE OF CONTENTS
DIGITAL EDITION
- LATEST ISSUE
- SIGN UP FOR E-ALERT
- WRITE FOR US
- PERMISSIONS
Share article: Academic writing: using literature to demonstrate critical analysis
We use cookies on this site to enhance your user experience.
By clicking any link on this page you are giving your consent for us to set cookies.

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

4.8: Critical Writing
- Last updated
- Save as PDF
- Page ID 16521

- Lapum et al.
- Ryerson University (Daphne Cockwell School of Nursing) via Ryerson University Library
What it is?
Have you ever been asked to write in a critical manner?
Critical writing involves critical thinking . This type of thinking develops over the course of your university program and involves learning to evaluate and reconstruct your thinking and ideas in the context of other peoples’ thinking and ideas. You may be involved in critical thinking and writing related to phenomena such as journal articles, healthcare issues, new clinical guidelines, and healthcare policy issues. See Table 4.2 .
Overall, you should use critical thinking and writing when you start breaking down your topic to develop discussion points. You will also use critical analysis when you synthesize, or blend, your ideas with those of experts. This means you will go beyond a statement of facts and take a stance , stating your view on an idea or issue and on core sources of information on that topic: you will insert your own ideas into the text’s conversation.
Table 4.2: Critical thinking and critical writing
How to do it?
The steps involved in critical writing depend on the context of your writing and what you are asked to write about. Here are some general steps:
1. Demonstrate concise and comprehensive understanding of your issue. You should contextualize the issue in relation to other work, so it will be helpful to begin with some pre-reading strategies and notetaking to understand the big picture. It will be difficult for your audience to think critically about your argument if you do not provide a clear picture of the issue , so gaps in your understanding will undermine your goal.
2. Critically evaluate the phenomenon or the text in question. This will involve identifying strengths and limitations . You don’t necessarily need to adopt a negative position in which you focus on deficits and limitations alone – it’s possible to focus on the positive aspects of a phenomenon or a combination of both negative and positive elements in your critical analysis.
3. Critical analysis demonstrates that you are able to synthesize and connect ideas , arrive at your own conclusions, and develop new directions for discussion. Move beyond simply taking another person’s ideas and spitting out facts: you should show that you have used sources to develop ideas of your own, and present alternative interpretations or perspectives through evaluation, debate, and critique.
4. You will be expected to evaluate texts related to research studies. In this case, you should ask questions like: Is the purpose of the research clear? Are the study methods clearly defined? Do the data support the research findings and conclusions? Are the nursing implications clearly identified?
What to keep in mind?
Keep these tips in mind when engaging in critical thinking:
- While summarizing an issue, it is important to adopt the language used in the original source, rather than imposing words, beliefs, or assumptions.
- Clearly and concisely argue one point at a time . An outline will help keep you on track, as each paragraph should focus on a main point.
- Highlight strengths, limitations, and recommendations in a respectful way . Severe language often can make the reader question your credibility. It is also more helpful to provide constructive feedback rather than stressing the futility of an approach. See Table 4.3 for examples of ways to avoid severe language.
Table 4.3: Severe language and better choices
Activity: Check Your Understanding
The original version of this chapter contained H5P content. You may want to remove or replace this element.
Attribution statement
This content is mainly our own original content. With editorial changes, some of this content was adapted from (specifically, the last bullet in the table in column two and item three under “how to do it?”): Writing for Success 1st Canadian Edition by Tara Horkoff is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted. Download for free at: https://opentextbc.ca/writingforsuccess/
- Help & FAQ
Academic writing: using literature to demonstrate critical analysis
Research output : Contribution to journal › Article › peer-review
- academic writing
- critical analysis
- nursing education
Documents and Links
- http://nursingstandard.rcnpublishing.co.uk/
Fingerprint
- Nursing Medicine & Life Sciences 100%
- Nurses Medicine & Life Sciences 87%
- Students Medicine & Life Sciences 84%
T1 - Academic writing: using literature to demonstrate critical analysis
AU - Duffy, Kathleen
AU - Hastie, Elizabeth
AU - McCallum, Jacqueline
AU - Ness, Val
AU - Price, Lesley
N1 - PDF available to download from publisher's website
PY - 2009/7
Y1 - 2009/7
N2 - When writing at degree level, nurses need to demonstrate an understanding of evidence by summarising its key elements and comparing and contrasting authors’ views. Critical analysis is an important nursing skill in writing and in practice. With the advent of an all-degree profession, understanding how to develop this skill is crucial. This article examines how students can develop critical analysis skills to write at undergraduate degree level.
AB - When writing at degree level, nurses need to demonstrate an understanding of evidence by summarising its key elements and comparing and contrasting authors’ views. Critical analysis is an important nursing skill in writing and in practice. With the advent of an all-degree profession, understanding how to develop this skill is crucial. This article examines how students can develop critical analysis skills to write at undergraduate degree level.
KW - academic writing
KW - literature
KW - critical analysis
KW - nursing education
M3 - Article
SN - 2047-9018
JO - Nursing Standard
JF - Nursing Standard
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Barker J, Linsley P, Kane R, 3rd edn. London: Sage; 2016
Ethical guidelines for educational research. 2018; https://tinyurl.com/c84jm5rt
Bowling A Research methods in health, 4th edn. Maidenhead: Open University Press/McGraw-Hill Education; 2014
Gliner JA, Morgan GAMahwah (NJ): Lawrence Erlbaum Associates; 2000
Critical Skills Appraisal Programme checklists. 2021; https://casp-uk.net/casp-tools-checklists
Cresswell J, 4th edn. London: Sage; 2013
Grainger A Principles of temperature monitoring. Nurs Stand. 2013; 27:(50)48-55 https://doi.org/10.7748/ns2013.08.27.50.48.e7242
Jupp VLondon: Sage; 2006
Continuing professional development (CPD). 2021; http://www.hcpc-uk.org/cpd
London: NHS England; 2017 http://www.hee.nhs.uk/our-work/advanced-clinical-practice
Kennedy M, Burnett E Hand hygiene knowledge and attitudes: comparisons between student nurses. Journal of Infection Prevention. 2011; 12:(6)246-250 https://doi.org/10.1177/1757177411411124
Lindsay-Smith G, O'Sullivan G, Eime R, Harvey J, van Ufflen JGZ A mixed methods case study exploring the impact of membership of a multi-activity, multi-centre community group on the social wellbeing of older adults. BMC Geriatrics. 2018; 18 https://bmcgeriatr.biomedcentral.com/track/pdf/10.1186/s12877-018-0913-1.pdf
Morse JM, Pooler C, Vann-Ward T Awaiting diagnosis of breast cancer: strategies of enduring for preserving self. Oncology Nursing Forum. 2014; 41:(4)350-359 https://doi.org/10.1188/14.ONF.350-359
Revalidation. 2019; http://revalidation.nmc.org.uk
Parahoo K Nursing research, principles, processes and issues, 3rd edn. Basingstoke: Palgrave Macmillan; 2014
Polit DF, Beck CT Nursing research, 10th edn. Philadelphia (PA): Wolters Kluwer; 2017
Critiquing a published healthcare research paper
Angela Grainger
Nurse Lecturer/Scholarship Lead, BPP University, and editorial board member
View articles · Email Angela

Research is defined as a ‘systematic inquiry using orderly disciplined methods to answer questions or to solve problems' ( Polit and Beck, 2017 :743). Research requires academic discipline coupled with specific research competencies so that an appropriate study is designed and conducted, leading to the drawing of relevant conclusions relating to the explicit aim/s of the study.
Relevance of research to nursing and health care
For those embarking on a higher degree such as a master's, taught doctorate, or a doctor of philosophy, the relationship between research, knowledge production and knowledge utilisation becomes clear during their research tuition and guidance from their research supervisor. But why should other busy practitioners juggling a work/home life balance find time to be interested in healthcare research? The answer lies in the relationship between the outcomes of research and its relationship to the determination of evidence-based practice (EBP).
The Health and Care Professions Council (HCPC) and the Nursing and Midwifery Council (NMC) require registered practitioners to keep their knowledge and skills up to date. This requirement incorporates being aware of the current EBP relevant to the registrant's field of practice, and to consider its application in relation to the decisions made in the delivery of patient care.
Advanced clinical practitioners (ACPs) are required to be involved in aspects of research activities ( Health Education England, 2017 ). It is for this reason that practitioners need to know how EBP is influenced by research findings and, moreover, need to be able to read and interpret a research study that relates to a particular evidence base. Reading professional peer-reviewed journals that have an impact factor (the yearly average number of citations of papers published in a previous 2-year period in a given journal is calculated by a scientometric index giving an impact factor) is evidence of continuing professional development (CPD).
CPD fulfils part of the HCPC's and the NMC's required professional revalidation process ( HCPC, 2021 ; NMC, 2019 ). For CPD in relation to revalidation, practitioners can give the publication details of a research paper, along with a critique of that paper, highlighting the relevance of the paper's findings to the registrant's field of practice.
Defining evidence-based practice
According to Barker et al (2016:4.1) EBP is the integration of research evidence and knowledge to current clinical practice and is to be used at a local level to ensure that patients receive the best quality care available. Because patients are at the receiving end of EBP it is important that the research evidence is credible. This is why a research study has to be designed and undertaken rigorously in accordance with academic and scientific discipline.
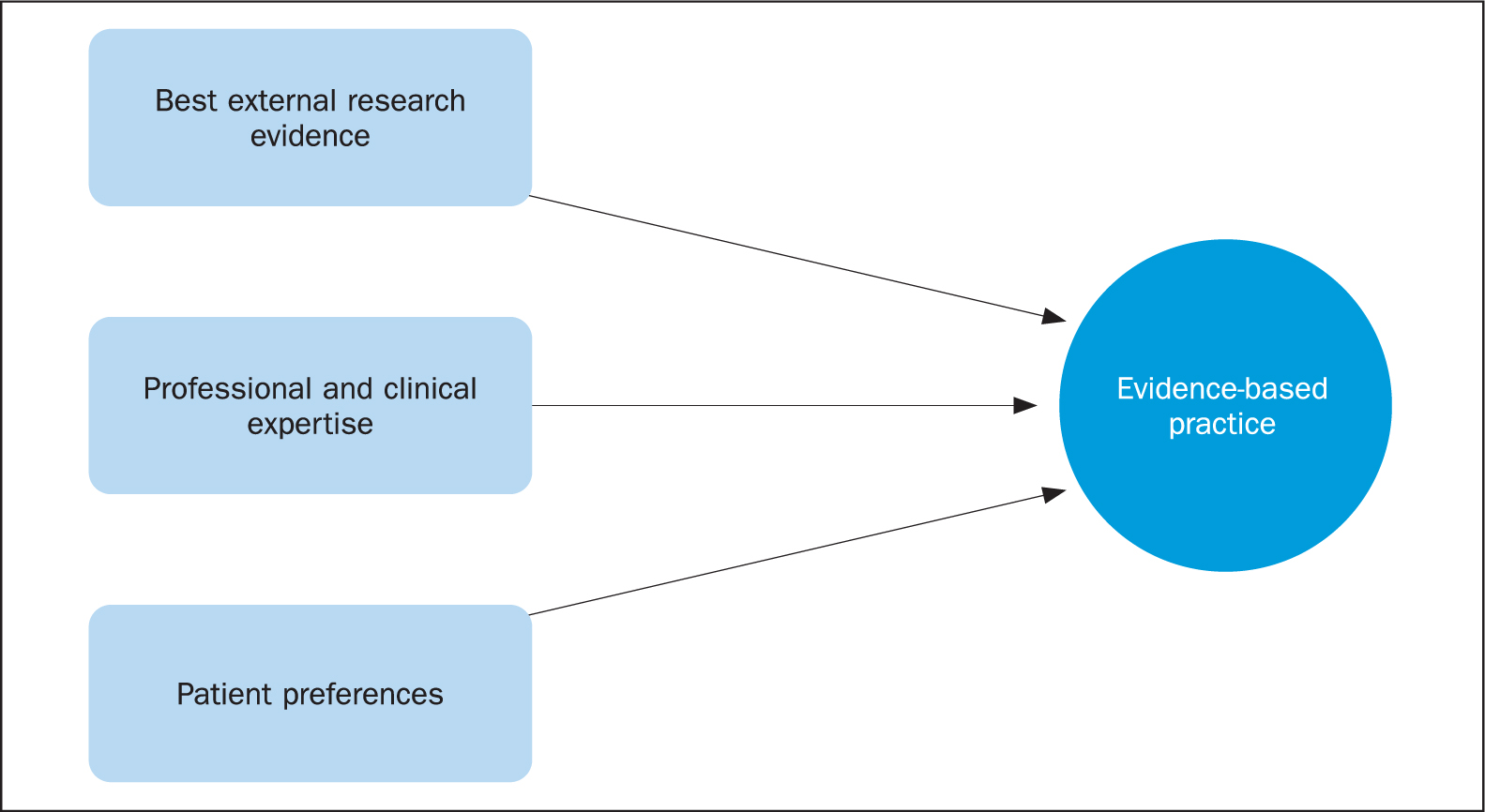
The elements of EBP
EBP comprises three elements ( Figure 1 ). The key element is research evidence, followed by the expert knowledge and professional opinion of the practitioner, which is important especially when there is no research evidence—for example, the most appropriate way to assist a patient out of bed, or perform a bed bath. Last, but in no way of least importance, is the patient's preference for a particular procedure. An example of this is the continued use of thermal screening dots for measuring a child's temperature on the forehead, or in the armpit because children find these options more acceptable than other temperature measuring devices, which, it is argued, might give a more accurate reading ( Grainger, 2013 ).
Understanding key research principles
To interpret a published research study requires an understanding of key research principles. Research authors use specific research terms in their publications to describe and to explain what they have done and why. So without an awareness of the research principles underpinning the study, how can readers know if what they are reading is credible?
Validity and reliability have long been the two pillars on which the quality of a research study has been judged ( Gliner and Morgan, 2000 ). Validity refers to how accurately a method measures what it is intended to measure. If a research study has a high validity, it means that it produces results that correspond to real properties, characteristics, and variations in the part of the physical or social world that is being studied ( Jupp, 2006 ).
Reliability is the extent to which a measuring instrument, for example, a survey using closed questions, gives the same consistent results when that survey is repeated. The measurement is considered reliable if the same result can be consistently achieved by using the same methods under the same circumstances ( Parahoo, 2014 ).
The research topic is known as the phenomenon in a singular sense, or phenomena if what is to be researched is plural. It is a key principle of research that it is the nature of the phenomenon, in association with the study's explicit research aim/s, that determines the research design. The research design refers to the overall structure or plan of the research ( Bowling, 2014 :166).
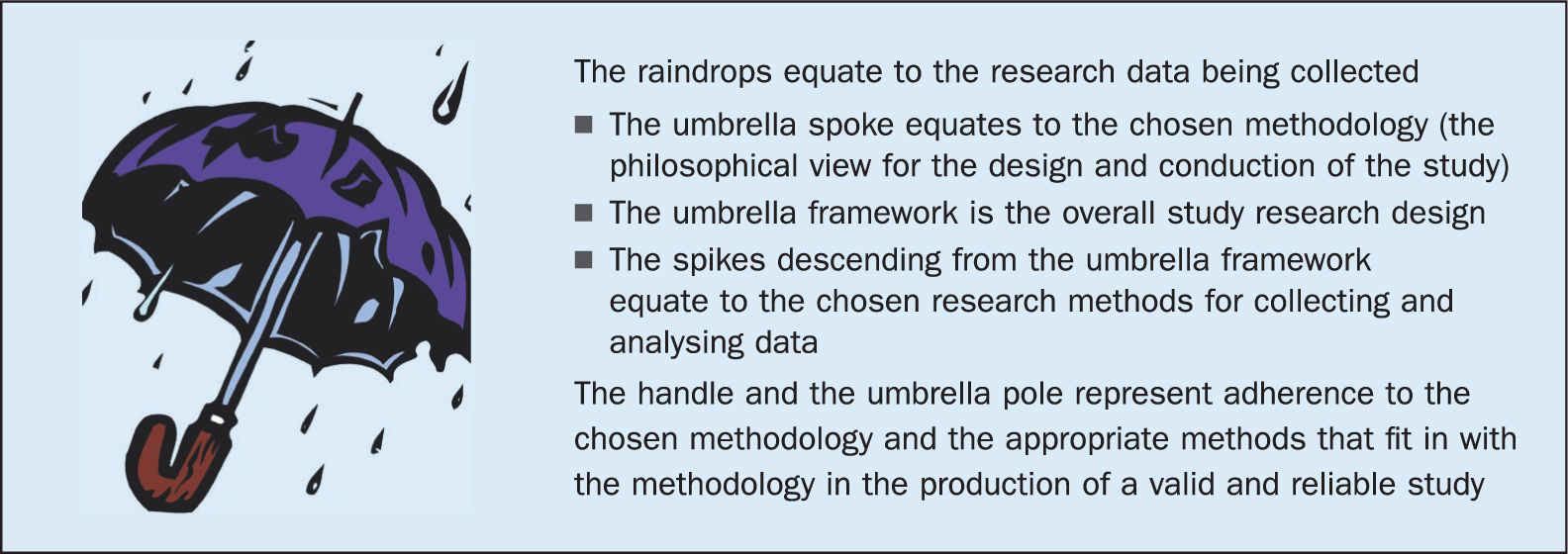
Methodology means the philosophy underpinning how the research will be conducted. It is essential for the study's research design that an appropriate methodology for the conduct and execution of the study is selected, otherwise the research will not meet the requirements of being valid and reliable. The research methods will include the design for data sampling, how recruitment into the study will be undertaken, the method/s used for the actual data collection, and the subsequent data analysis from which conclusions will be drawn (see Figure 2 ).
Quantitative, qualitative, and mixed-methods studies
A quantitative methodology is where the phenomenon lends itself to an investigation of data that can be numerically analysed using an appropriate statistical test/s. Quantitative research rests on the philosophical view that science has to be neutral and value-free, which is why precise measurement instruments are required ( Box 1 ). Quantitative research is influenced by the physical sciences such as mathematics, physics, and chemistry. The purpose of quantitative studies is to identify whether there are any causal relationships between variables present in the phenomenon. In short, a variable is an attribute that can vary and take on different values, such as the body temperature or the heart rate ( Polit and Beck, 2017 :748).
Quantitative studies can sometimes have a hypothesis. A hypothesis is a prediction of the study's outcome, and the aim of the study is to show either that the hypothesis is demonstrated as proven, or that it is not proven. Often a hypothesis is about a predicted relationship between variables. There are two types of variables, independent and dependent. An independent variable causes a change in the specific phenomenon being studied, while a dependent variable is the change in that phenomenon. The first example in Box 1 might help to clarify the difference.
An example of a hypothesis would be that older people who have a history of falls have a reduction in the incidence of falls due to exercise therapy. The causal relationship is between the independent variable— the exercise therapy—and the dependent variable—a falls reduction.
A qualitative methodology aims to explore a phenomenon with the aim of understanding the experience of the phenomenon from the perspective of those affected by it. Qualitative research is influenced by the social and not the physical sciences. Concepts and themes arise from the researcher/s interpretation of the data gained from observations and interviews. The collected data are non-numerical and this is the distinction from a quantitative study. The data collected are coded in accordance with the type of method being used in the research study, for example, discourse analysis; phenomenology; grounded theory. The researcher identifies themes from the data descriptions, and from the data analysis a theoretical understanding is seen to emerge.
A qualitative methodology rests on the philosophical view that science cannot be neutral and value-free because the researcher and the participants are part of the world that the research study aims to explore.
Unlike quantitative studies, the results of which can often be generalised due to the preciseness of the measuring instruments, qualitative studies are not usually generalisable. However, knowledge comparisons can be made between studies that have some similarity of focus. For example, the uncovering of causative or aggravating factors leading to the experiences of pain management for oncology patients, and for patients who have rheumatoid arthritis, or another long-term health problem for which pain is a characteristic feature. The validity of a qualitative study relates to the accurate representation of the data collected and analysed, and which shows that data has been saturated, meaning no new data or analysed findings are forthcoming. This is demonstrated in a clear data audit trail, and the study's findings are therefore seen as credible (see the second example in Box 1 ).
Box 1.Research study examples
- An example of a quantitative research study Kennedy and Burnett (2011) conducted a survey to determine whether there were any discernible differences in knowledge and attitudes between second- and third-year pre-registration nursing students toward hand-hygiene practices. The collected data and its subsequent analysis is presented in numerical tables and graphs, but these are supported by text explaining the research findings and how these were ascertained. For full details, see 10.1177/1757177411411124
- 2. An example of a qualitative research study Morse et al (2014) undertook an exploratory study to see what coping strategies were used by women awaiting a possible diagnosis of breast cancer. Direct quotes from the study participants appeared in the writing up of the research because it is a requirement of qualitative research that there be a transparent data audit trail. The research showed two things, both essential requirements of qualitative research. First, how the collected data were saturated to ensure that no data had been left inadequately explored, or that the data coding had been prematurely closed and, second, having captured the breadth and depth of the data findings, the researchers showed how the direct quotes were thematically coded to reveal the women's coping strategies. For full details, see 10.1188/14.ONF.350-359
- 3. An example of a mixed-methods study Lindsay-Smith et al (2018) investigated and explored the impact on elderly people's social wellbeing when they were members of a community that provided multi-activities. The study combined a quantitative survey that recorded participants' sociodemographic characteristics and measured participation in activities with a focus group study to gauge participants' perceptions of the benefits of taking part in the activities. For full details, see https://bmcgeriatr.biomedcentral.com/track/pdf/10.1186/s12877-018-0913-1.pdf
Sometimes a study cannot meet its stated research aims by using solely a quantitative or a qualitative methodology, so a mixed-methods approach combining both quantitative and qualitative methods for the collection and analysis of data are used. Cresswell (2013) explains that, depending on the aim and purpose of the study, it is possible to collect either the quantitative data first and analyse these, followed by the qualitative data and their analysis. This is an explanatory/exploratory sequence. Or the qualitative data may be collected first and analysed, followed by the quantitative; an exploratory/explanatory process. Whichever approach is used, the cumulative data analyses have to be synthesised to give a clear picture of the overall findings ( Box 1 ).
The issue of bias
Bias is a negative feature of research because it relates to either an error in the conceptualisation of the study due to the researcher/s adopting a skewed or idiosyncratic perspective, or to errors in the data analysis. Bias will affect the validity and reliability of a study, so it is important that any bias is eliminated in quantitative studies, or minimised and accounted for in qualitative studies.
Scientific and ethical approval
It should be noted that, before any research study proceeds, the research proposal for that study must have been reviewed and agreed to by a scientific and ethics committee. The purpose of a scientific and ethics committee is to see that those recruited into a study are not harmed or damaged, and that the study will contribute to the advancement of knowledge. The committee pays particular attention to whether any bias might have been introduced to a study. The researchers will have detailed the reason why the study is required, the explicit aim/s and purpose of the study, the methodology of the study, and its subsequent design, including the chosen research methods for the collection of the data (sampling and study recruitment), and what method/s will be used for data analysis.
A literature review is undertaken and the established (published) international literature on the research topic is summarised to highlight what is already known on the topic and/or to show any topic gaps that have not yet been researched. The British Educational Research Association (BERA) (2018) also gives guidance for research proposals that are deemed to be educational evaluation studies, including ‘close-practice’ research studies. Any ethical issues such as how people will be recruited into the study, the gaining of informed voluntary consent, any conflict of interest between the researcher/s and the proposed research topic, and whether the research is being funded or financially supported by a particular source will also have been considered.
Critiquing a published research paper
It is important to remember that a published paper is not the research report. It is a sample of the research report. The research author/s are presenting their research findings as a succinct summary. Only a passing mention might be made that ethical approval and voluntary informed consent were obtained. However, readers can be assured that all publications in leading journals with a good reputation are subject to an external peer review process. Any concerns about a paper's content will have been ironed out prior to publication.
It will be apparent that there are several particular research designs. The Critical Skills Appraisal Programme (CASP) provides online information to help the interpretation of each type of study, and does this by providing questions to help the reader consider and critique the paper ( CASP, 2021 ).
General points for critiquing a paper include the following:
- The paper should be readable and have explicit statements on the purpose of the research, its chosen methodology and design
- Read the paper thoroughly to get a feel for what the paper is saying
- Consider what the researcher/s says about any ethical issues and how these have been handled
- Look at how the data were collected and analysed. Are the explanations for these aspects clear? In a quantitative study, are any graphs or charts easy to understand and is there supporting text to aid the interpretation of the data? In a qualitative study, are direct quotes from the research participants included, and do the researcher/s show how data collected from interviews and observations were coded into data categories and themes?
- In a mixed-method study, how are the quantitative and qualitative analyses synthesised?
- Do the conclusions seem to fit the handling of the data's analysis?
- An important test of validity is whether the study's title relates well to the content of the paper and, conversely, whether the content reflect a corresponding match to the study's title.
Finally, remember that the research study could have been conducted using a different methodological design provided the research aims would still have been met, but a critique of the paper relates to what has been published and not what otherwise might have been done.
Your web browser is outdated and may be insecure
The RCN recommends using an updated browser such as Microsoft Edge or Google Chrome
Critical Appraisal
Use this guide to find information resources about critical appraisal including checklists, books and journal articles.
Key Resources
- This online resource explains the sections commonly used in research articles. Understanding how research articles are organised can make reading and evaluating them easier View page
- Critical appraisal checklists
- Worksheets for appraising systematic reviews, diagnostics, prognostics and RCTs. View page
- A free online resource for both healthcare staff and patients; four modules of 30–45 minutes provide an introduction to evidence based medicine, clinical trials and Cochrane Evidence. View page
- This tool will guide you through a series of questions to help you to review and interpret a published health research paper. View page
- The PRISMA flow diagram depicts the flow of information through the different phases of a literature review. It maps out the number of records identified, included and excluded, and the reasons for exclusions. View page
- A useful resource for methods and evidence in applied social science. View page
- A comprehensive database of reporting guidelines. Covers all the main study types. View page
- A tool to assess the methodological quality of systematic reviews. View page
- Borrow from RCN Library services
- Chapter 5 covers critical appraisal of the literature. View this eBook

- Chapter 6 covers assessing the evidence base. Borrow from RCN Library services
- Section 1 covers an introduction to critical appraisal. Section 3 covers appraising difference types of papers including qualitative papers and observational studies. View this eBook

- Chapter 6 covers critically appraising the literature. Borrow from RCN Library services

- View this eBook

- Chapter 8 covers critical appraisal of the evidence. View this eBook

- Chapter 18 covers critical appraisal of nursing studies. View this eBook
- Borrow from RCN Library Services

Book subject search
- Critical appraisal
Journal articles
- View article
Shea BJ and others (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions or both, British Medical Journal, 358.
- An outline of AMSTAR 2 and its use for as a critical appraisal tool for systematic reviews. View article (open access)
- View articles
Editor of this guide
RCN Library and Archive Service
Upcoming events relating to this subject guide

Know How to Search CINAHL
Learn about using the CINAHL database for literature searches at this event for RCN members.

Library Search ... in 30 minutes
Learn how RCN members can quickly and easily search for articles, books and more using our fantastic and easy to use Library Search tool.

Know How to Reference Accurately and Avoid Plagiarism
Learn how to use the Harvard refencing style and why referencing is important at this event for RCN members.

Easy referencing ... in 30 minutes
Learn how to generate quick references and citations using free, easy to use, online tools.
Page last updated - 08/02/2024
Your Spaces
- RCNi Profile
- Steward Portal
- RCN Foundation
- RCN Library
- RCN Starting Out
Work & Venue
- RCNi Nursing Jobs
- Work for the RCN
- RCN Working with us
Further Info
- Manage Cookie Preferences
- Modern slavery statement
- Accessibility
- Press office
Connect with us:
© 2024 Royal College of Nursing
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 21, Issue 4
- How to appraise quantitative research
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
This article has a correction. Please see:
- Correction: How to appraise quantitative research - April 01, 2019
- Xabi Cathala 1 ,
- Calvin Moorley 2
- 1 Institute of Vocational Learning , School of Health and Social Care, London South Bank University , London , UK
- 2 Nursing Research and Diversity in Care , School of Health and Social Care, London South Bank University , London , UK
- Correspondence to Mr Xabi Cathala, Institute of Vocational Learning, School of Health and Social Care, London South Bank University London UK ; cathalax{at}lsbu.ac.uk and Dr Calvin Moorley, Nursing Research and Diversity in Care, School of Health and Social Care, London South Bank University, London SE1 0AA, UK; Moorleyc{at}lsbu.ac.uk
https://doi.org/10.1136/eb-2018-102996
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Some nurses feel that they lack the necessary skills to read a research paper and to then decide if they should implement the findings into their practice. This is particularly the case when considering the results of quantitative research, which often contains the results of statistical testing. However, nurses have a professional responsibility to critique research to improve their practice, care and patient safety. 1 This article provides a step by step guide on how to critically appraise a quantitative paper.
Title, keywords and the authors
The authors’ names may not mean much, but knowing the following will be helpful:
Their position, for example, academic, researcher or healthcare practitioner.
Their qualification, both professional, for example, a nurse or physiotherapist and academic (eg, degree, masters, doctorate).
This can indicate how the research has been conducted and the authors’ competence on the subject. Basically, do you want to read a paper on quantum physics written by a plumber?
The abstract is a resume of the article and should contain:
Introduction.
Research question/hypothesis.
Methods including sample design, tests used and the statistical analysis (of course! Remember we love numbers).
Main findings.
Conclusion.
The subheadings in the abstract will vary depending on the journal. An abstract should not usually be more than 300 words but this varies depending on specific journal requirements. If the above information is contained in the abstract, it can give you an idea about whether the study is relevant to your area of practice. However, before deciding if the results of a research paper are relevant to your practice, it is important to review the overall quality of the article. This can only be done by reading and critically appraising the entire article.
The introduction
Example: the effect of paracetamol on levels of pain.
My hypothesis is that A has an effect on B, for example, paracetamol has an effect on levels of pain.
My null hypothesis is that A has no effect on B, for example, paracetamol has no effect on pain.
My study will test the null hypothesis and if the null hypothesis is validated then the hypothesis is false (A has no effect on B). This means paracetamol has no effect on the level of pain. If the null hypothesis is rejected then the hypothesis is true (A has an effect on B). This means that paracetamol has an effect on the level of pain.
Background/literature review
The literature review should include reference to recent and relevant research in the area. It should summarise what is already known about the topic and why the research study is needed and state what the study will contribute to new knowledge. 5 The literature review should be up to date, usually 5–8 years, but it will depend on the topic and sometimes it is acceptable to include older (seminal) studies.
Methodology
In quantitative studies, the data analysis varies between studies depending on the type of design used. For example, descriptive, correlative or experimental studies all vary. A descriptive study will describe the pattern of a topic related to one or more variable. 6 A correlational study examines the link (correlation) between two variables 7 and focuses on how a variable will react to a change of another variable. In experimental studies, the researchers manipulate variables looking at outcomes 8 and the sample is commonly assigned into different groups (known as randomisation) to determine the effect (causal) of a condition (independent variable) on a certain outcome. This is a common method used in clinical trials.
There should be sufficient detail provided in the methods section for you to replicate the study (should you want to). To enable you to do this, the following sections are normally included:
Overview and rationale for the methodology.
Participants or sample.
Data collection tools.
Methods of data analysis.
Ethical issues.
Data collection should be clearly explained and the article should discuss how this process was undertaken. Data collection should be systematic, objective, precise, repeatable, valid and reliable. Any tool (eg, a questionnaire) used for data collection should have been piloted (or pretested and/or adjusted) to ensure the quality, validity and reliability of the tool. 9 The participants (the sample) and any randomisation technique used should be identified. The sample size is central in quantitative research, as the findings should be able to be generalised for the wider population. 10 The data analysis can be done manually or more complex analyses performed using computer software sometimes with advice of a statistician. From this analysis, results like mode, mean, median, p value, CI and so on are always presented in a numerical format.
The author(s) should present the results clearly. These may be presented in graphs, charts or tables alongside some text. You should perform your own critique of the data analysis process; just because a paper has been published, it does not mean it is perfect. Your findings may be different from the author’s. Through critical analysis the reader may find an error in the study process that authors have not seen or highlighted. These errors can change the study result or change a study you thought was strong to weak. To help you critique a quantitative research paper, some guidance on understanding statistical terminology is provided in table 1 .
- View inline
Some basic guidance for understanding statistics
Quantitative studies examine the relationship between variables, and the p value illustrates this objectively. 11 If the p value is less than 0.05, the null hypothesis is rejected and the hypothesis is accepted and the study will say there is a significant difference. If the p value is more than 0.05, the null hypothesis is accepted then the hypothesis is rejected. The study will say there is no significant difference. As a general rule, a p value of less than 0.05 means, the hypothesis is accepted and if it is more than 0.05 the hypothesis is rejected.
The CI is a number between 0 and 1 or is written as a per cent, demonstrating the level of confidence the reader can have in the result. 12 The CI is calculated by subtracting the p value to 1 (1–p). If there is a p value of 0.05, the CI will be 1–0.05=0.95=95%. A CI over 95% means, we can be confident the result is statistically significant. A CI below 95% means, the result is not statistically significant. The p values and CI highlight the confidence and robustness of a result.
Discussion, recommendations and conclusion
The final section of the paper is where the authors discuss their results and link them to other literature in the area (some of which may have been included in the literature review at the start of the paper). This reminds the reader of what is already known, what the study has found and what new information it adds. The discussion should demonstrate how the authors interpreted their results and how they contribute to new knowledge in the area. Implications for practice and future research should also be highlighted in this section of the paper.
A few other areas you may find helpful are:
Limitations of the study.
Conflicts of interest.
Table 2 provides a useful tool to help you apply the learning in this paper to the critiquing of quantitative research papers.
Quantitative paper appraisal checklist
- 1. ↵ Nursing and Midwifery Council , 2015 . The code: standard of conduct, performance and ethics for nurses and midwives https://www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/nmc-code.pdf ( accessed 21.8.18 ).
- Gerrish K ,
- Moorley C ,
- Tunariu A , et al
- Shorten A ,
Competing interests None declared.
Patient consent Not required.
Provenance and peer review Commissioned; internally peer reviewed.
Correction notice This article has been updated since its original publication to update p values from 0.5 to 0.05 throughout.
Linked Articles
- Miscellaneous Correction: How to appraise quantitative research BMJ Publishing Group Ltd and RCN Publishing Company Ltd Evidence-Based Nursing 2019; 22 62-62 Published Online First: 31 Jan 2019. doi: 10.1136/eb-2018-102996corr1
Read the full text or download the PDF:
- Privacy Policy
Buy Me a Coffee

Home » Critical Analysis – Types, Examples and Writing Guide
Critical Analysis – Types, Examples and Writing Guide
Table of Contents

Critical Analysis
Definition:
Critical analysis is a process of examining a piece of work or an idea in a systematic, objective, and analytical way. It involves breaking down complex ideas, concepts, or arguments into smaller, more manageable parts to understand them better.
Types of Critical Analysis
Types of Critical Analysis are as follows:
Literary Analysis
This type of analysis focuses on analyzing and interpreting works of literature , such as novels, poetry, plays, etc. The analysis involves examining the literary devices used in the work, such as symbolism, imagery, and metaphor, and how they contribute to the overall meaning of the work.
Film Analysis
This type of analysis involves examining and interpreting films, including their themes, cinematography, editing, and sound. Film analysis can also include evaluating the director’s style and how it contributes to the overall message of the film.
Art Analysis
This type of analysis involves examining and interpreting works of art , such as paintings, sculptures, and installations. The analysis involves examining the elements of the artwork, such as color, composition, and technique, and how they contribute to the overall meaning of the work.
Cultural Analysis
This type of analysis involves examining and interpreting cultural artifacts , such as advertisements, popular music, and social media posts. The analysis involves examining the cultural context of the artifact and how it reflects and shapes cultural values, beliefs, and norms.
Historical Analysis
This type of analysis involves examining and interpreting historical documents , such as diaries, letters, and government records. The analysis involves examining the historical context of the document and how it reflects the social, political, and cultural attitudes of the time.
Philosophical Analysis
This type of analysis involves examining and interpreting philosophical texts and ideas, such as the works of philosophers and their arguments. The analysis involves evaluating the logical consistency of the arguments and assessing the validity and soundness of the conclusions.
Scientific Analysis
This type of analysis involves examining and interpreting scientific research studies and their findings. The analysis involves evaluating the methods used in the study, the data collected, and the conclusions drawn, and assessing their reliability and validity.
Critical Discourse Analysis
This type of analysis involves examining and interpreting language use in social and political contexts. The analysis involves evaluating the power dynamics and social relationships conveyed through language use and how they shape discourse and social reality.
Comparative Analysis
This type of analysis involves examining and interpreting multiple texts or works of art and comparing them to each other. The analysis involves evaluating the similarities and differences between the texts and how they contribute to understanding the themes and meanings conveyed.
Critical Analysis Format
Critical Analysis Format is as follows:
I. Introduction
- Provide a brief overview of the text, object, or event being analyzed
- Explain the purpose of the analysis and its significance
- Provide background information on the context and relevant historical or cultural factors
II. Description
- Provide a detailed description of the text, object, or event being analyzed
- Identify key themes, ideas, and arguments presented
- Describe the author or creator’s style, tone, and use of language or visual elements
III. Analysis
- Analyze the text, object, or event using critical thinking skills
- Identify the main strengths and weaknesses of the argument or presentation
- Evaluate the reliability and validity of the evidence presented
- Assess any assumptions or biases that may be present in the text, object, or event
- Consider the implications of the argument or presentation for different audiences and contexts
IV. Evaluation
- Provide an overall evaluation of the text, object, or event based on the analysis
- Assess the effectiveness of the argument or presentation in achieving its intended purpose
- Identify any limitations or gaps in the argument or presentation
- Consider any alternative viewpoints or interpretations that could be presented
- Summarize the main points of the analysis and evaluation
- Reiterate the significance of the text, object, or event and its relevance to broader issues or debates
- Provide any recommendations for further research or future developments in the field.
VI. Example
- Provide an example or two to support your analysis and evaluation
- Use quotes or specific details from the text, object, or event to support your claims
- Analyze the example(s) using critical thinking skills and explain how they relate to your overall argument
VII. Conclusion
- Reiterate your thesis statement and summarize your main points
- Provide a final evaluation of the text, object, or event based on your analysis
- Offer recommendations for future research or further developments in the field
- End with a thought-provoking statement or question that encourages the reader to think more deeply about the topic
How to Write Critical Analysis
Writing a critical analysis involves evaluating and interpreting a text, such as a book, article, or film, and expressing your opinion about its quality and significance. Here are some steps you can follow to write a critical analysis:
- Read and re-read the text: Before you begin writing, make sure you have a good understanding of the text. Read it several times and take notes on the key points, themes, and arguments.
- Identify the author’s purpose and audience: Consider why the author wrote the text and who the intended audience is. This can help you evaluate whether the author achieved their goals and whether the text is effective in reaching its audience.
- Analyze the structure and style: Look at the organization of the text and the author’s writing style. Consider how these elements contribute to the overall meaning of the text.
- Evaluate the content : Analyze the author’s arguments, evidence, and conclusions. Consider whether they are logical, convincing, and supported by the evidence presented in the text.
- Consider the context: Think about the historical, cultural, and social context in which the text was written. This can help you understand the author’s perspective and the significance of the text.
- Develop your thesis statement : Based on your analysis, develop a clear and concise thesis statement that summarizes your overall evaluation of the text.
- Support your thesis: Use evidence from the text to support your thesis statement. This can include direct quotes, paraphrases, and examples from the text.
- Write the introduction, body, and conclusion : Organize your analysis into an introduction that provides context and presents your thesis, a body that presents your evidence and analysis, and a conclusion that summarizes your main points and restates your thesis.
- Revise and edit: After you have written your analysis, revise and edit it to ensure that your writing is clear, concise, and well-organized. Check for spelling and grammar errors, and make sure that your analysis is logically sound and supported by evidence.
When to Write Critical Analysis
You may want to write a critical analysis in the following situations:
- Academic Assignments: If you are a student, you may be assigned to write a critical analysis as a part of your coursework. This could include analyzing a piece of literature, a historical event, or a scientific paper.
- Journalism and Media: As a journalist or media person, you may need to write a critical analysis of current events, political speeches, or media coverage.
- Personal Interest: If you are interested in a particular topic, you may want to write a critical analysis to gain a deeper understanding of it. For example, you may want to analyze the themes and motifs in a novel or film that you enjoyed.
- Professional Development : Professionals such as writers, scholars, and researchers often write critical analyses to gain insights into their field of study or work.
Critical Analysis Example
An Example of Critical Analysis Could be as follow:
Research Topic:
The Impact of Online Learning on Student Performance
Introduction:
The introduction of the research topic is clear and provides an overview of the issue. However, it could benefit from providing more background information on the prevalence of online learning and its potential impact on student performance.
Literature Review:
The literature review is comprehensive and well-structured. It covers a broad range of studies that have examined the relationship between online learning and student performance. However, it could benefit from including more recent studies and providing a more critical analysis of the existing literature.
Research Methods:
The research methods are clearly described and appropriate for the research question. The study uses a quasi-experimental design to compare the performance of students who took an online course with those who took the same course in a traditional classroom setting. However, the study may benefit from using a randomized controlled trial design to reduce potential confounding factors.
The results are presented in a clear and concise manner. The study finds that students who took the online course performed similarly to those who took the traditional course. However, the study only measures performance on one course and may not be generalizable to other courses or contexts.
Discussion :
The discussion section provides a thorough analysis of the study’s findings. The authors acknowledge the limitations of the study and provide suggestions for future research. However, they could benefit from discussing potential mechanisms underlying the relationship between online learning and student performance.
Conclusion :
The conclusion summarizes the main findings of the study and provides some implications for future research and practice. However, it could benefit from providing more specific recommendations for implementing online learning programs in educational settings.
Purpose of Critical Analysis
There are several purposes of critical analysis, including:
- To identify and evaluate arguments : Critical analysis helps to identify the main arguments in a piece of writing or speech and evaluate their strengths and weaknesses. This enables the reader to form their own opinion and make informed decisions.
- To assess evidence : Critical analysis involves examining the evidence presented in a text or speech and evaluating its quality and relevance to the argument. This helps to determine the credibility of the claims being made.
- To recognize biases and assumptions : Critical analysis helps to identify any biases or assumptions that may be present in the argument, and evaluate how these affect the credibility of the argument.
- To develop critical thinking skills: Critical analysis helps to develop the ability to think critically, evaluate information objectively, and make reasoned judgments based on evidence.
- To improve communication skills: Critical analysis involves carefully reading and listening to information, evaluating it, and expressing one’s own opinion in a clear and concise manner. This helps to improve communication skills and the ability to express ideas effectively.
Importance of Critical Analysis
Here are some specific reasons why critical analysis is important:
- Helps to identify biases: Critical analysis helps individuals to recognize their own biases and assumptions, as well as the biases of others. By being aware of biases, individuals can better evaluate the credibility and reliability of information.
- Enhances problem-solving skills : Critical analysis encourages individuals to question assumptions and consider multiple perspectives, which can lead to creative problem-solving and innovation.
- Promotes better decision-making: By carefully evaluating evidence and arguments, critical analysis can help individuals make more informed and effective decisions.
- Facilitates understanding: Critical analysis helps individuals to understand complex issues and ideas by breaking them down into smaller parts and evaluating them separately.
- Fosters intellectual growth : Engaging in critical analysis challenges individuals to think deeply and critically, which can lead to intellectual growth and development.
Advantages of Critical Analysis
Some advantages of critical analysis include:
- Improved decision-making: Critical analysis helps individuals make informed decisions by evaluating all available information and considering various perspectives.
- Enhanced problem-solving skills : Critical analysis requires individuals to identify and analyze the root cause of a problem, which can help develop effective solutions.
- Increased creativity : Critical analysis encourages individuals to think outside the box and consider alternative solutions to problems, which can lead to more creative and innovative ideas.
- Improved communication : Critical analysis helps individuals communicate their ideas and opinions more effectively by providing logical and coherent arguments.
- Reduced bias: Critical analysis requires individuals to evaluate information objectively, which can help reduce personal biases and subjective opinions.
- Better understanding of complex issues : Critical analysis helps individuals to understand complex issues by breaking them down into smaller parts, examining each part and understanding how they fit together.
- Greater self-awareness: Critical analysis helps individuals to recognize their own biases, assumptions, and limitations, which can lead to personal growth and development.
About the author
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

Cluster Analysis – Types, Methods and Examples

Data Collection – Methods Types and Examples

Delimitations in Research – Types, Examples and...

Discriminant Analysis – Methods, Types and...

Research Process – Steps, Examples and Tips

Research Design – Types, Methods and Examples
Critical practice in nursing care: analysis, action and reflexivity
Affiliation.
- 1 School of Nursing and Midwifery, Trinity College, Dublin. [email protected]
- PMID: 16786927
- DOI: 10.7748/ns2006.06.20.39.49.c4172
This article examines critical practice and its underlying principles: analysis, action and reflexivity. Critical analysis involves the examination of knowledge that underpins practice. Critical action requires nurses to assess their skills and identify potential gaps in need of professional development. Critical reflexivity is personal analysis that involves challenging personal beliefs and assumptions to improve professional and personal practice. Incorporating these aspects into nursing can benefit nursing practice.
Publication types
- Attitude of Health Personnel*
- Clinical Competence*
- Evidence-Based Medicine
- Health Policy
- Individuality
- Interprofessional Relations
- Negotiating
- Nurse's Role* / psychology
- Nursing Process / organization & administration*
- Nursing Research
- Nursing Theory
- Power, Psychological
- Self Efficacy
- Self-Assessment
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Fundamentals [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021.

Nursing Fundamentals [Internet].
- About Open RN
Chapter 4 Nursing Process
4.1. nursing process introduction, learning objectives.
- Use the nursing process to provide patient care
- Identify nursing diagnoses from evidence-based sources
- Describe the development of a care plan
- Prioritize patient care
- Describe documentation for each step of the nursing process
- Differentiate between the role of the PN and RN
Have you ever wondered how a nurse can receive a quick handoff report from another nurse and immediately begin providing care for a patient they previously knew nothing about? How do they know what to do? How do they prioritize and make a plan?
Nurses do this activity every shift. They know how to find pertinent information and use the nursing process as a critical thinking model to guide patient care. The nursing process becomes a road map for the actions and interventions that nurses implement to optimize their patients’ well-being and health. This chapter will explain how to use the nursing process as standards of professional nursing practice to provide safe, patient-centered care.
4.2. BASIC CONCEPTS
Before learning how to use the nursing process, it is important to understand some basic concepts related to critical thinking and nursing practice. Let’s take a deeper look at how nurses think.
Critical Thinking and Clinical Reasoning
Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.” [ 1 ] Using critical thinking means that nurses take extra steps to maintain patient safety and don’t just “follow orders.” It also means the accuracy of patient information is validated and plans for caring for patients are based on their needs, current clinical practice, and research.
“Critical thinkers” possess certain attitudes that foster rational thinking. These attitudes are as follows:
- Independence of thought: Thinking on your own
- Fair-mindedness: Treating every viewpoint in an unbiased, unprejudiced way
- Insight into egocentricity and sociocentricity: Thinking of the greater good and not just thinking of yourself. Knowing when you are thinking of yourself (egocentricity) and when you are thinking or acting for the greater good (sociocentricity)
- Intellectual humility: Recognizing your intellectual limitations and abilities
- Nonjudgmental: Using professional ethical standards and not basing your judgments on your own personal or moral standards
- Integrity: Being honest and demonstrating strong moral principles
- Perseverance: Persisting in doing something despite it being difficult
- Confidence: Believing in yourself to complete a task or activity
- Interest in exploring thoughts and feelings: Wanting to explore different ways of knowing
- Curiosity: Asking “why” and wanting to know more
Clinical reasoning is defined as, “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.” [ 2 ] To make sound judgments about patient care, nurses must generate alternatives, weigh them against the evidence, and choose the best course of action. The ability to clinically reason develops over time and is based on knowledge and experience. [ 3 ]

Inductive and Deductive Reasoning and Clinical Judgment
Inductive and deductive reasoning are important critical thinking skills. They help the nurse use clinical judgment when implementing the nursing process.
Inductive reasoning involves noticing cues, making generalizations, and creating hypotheses. Cues are data that fall outside of expected findings that give the nurse a hint or indication of a patient’s potential problem or condition. The nurse organizes these cues into patterns and creates a generalization. A generalization is a judgment formed from a set of facts, cues, and observations and is similar to gathering pieces of a jigsaw puzzle into patterns until the whole picture becomes more clear. Based on generalizations created from patterns of data, the nurse creates a hypothesis regarding a patient problem. A hypothesis is a proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring. If a “why” is identified, then a solution can begin to be explored.
No one can draw conclusions without first noticing cues. Paying close attention to a patient, the environment, and interactions with family members is critical for inductive reasoning. As you work to improve your inductive reasoning, begin by first noticing details about the things around you. A nurse is similar to the detective looking for cues in Figure 4.1 . [ 4 ] Be mindful of your five primary senses: the things that you hear, feel, smell, taste, and see. Nurses need strong inductive reasoning patterns and be able to take action quickly, especially in emergency situations. They can see how certain objects or events form a pattern (i.e., generalization) that indicates a common problem (i.e., hypothesis).
Inductive Reasoning Includes Looking for Cues
Example: A nurse assesses a patient and finds the surgical incision site is red, warm, and tender to the touch. The nurse recognizes these cues form a pattern of signs of infection and creates a hypothesis that the incision has become infected. The provider is notified of the patient’s change in condition, and a new prescription is received for an antibiotic. This is an example of the use of inductive reasoning in nursing practice.
Deductive reasoning is another type of critical thinking that is referred to as “top-down thinking.” Deductive reasoning relies on using a general standard or rule to create a strategy. Nurses use standards set by their state’s Nurse Practice Act, federal regulations, the American Nursing Association, professional organizations, and their employer to make decisions about patient care and solve problems.
Example: Based on research findings, hospital leaders determine patients recover more quickly if they receive adequate rest. The hospital creates a policy for quiet zones at night by initiating no overhead paging, promoting low-speaking voices by staff, and reducing lighting in the hallways. (See Figure 4.2 ). [ 5 ] The nurse further implements this policy by organizing care for patients that promotes periods of uninterrupted rest at night. This is an example of deductive thinking because the intervention is applied to all patients regardless if they have difficulty sleeping or not.
Deductive Reasoning Example: Implementing Interventions for a Quiet Zone Policy
Clinical judgment is the result of critical thinking and clinical reasoning using inductive and deductive reasoning. Clinical judgment is defined by the National Council of State Boards of Nursing (NCSBN) as, “The observed outcome of critical thinking and decision-making. It uses nursing knowledge to observe and assess presenting situations, identify a prioritized patient concern, and generate the best possible evidence-based solutions in order to deliver safe patient care.” [ 6 ] The NCSBN administers the national licensure exam (NCLEX) that measures nursing clinical judgment and decision-making ability of prospective entry-level nurses to assure safe and competent nursing care by licensed nurses.
Evidence-based practice (EBP) is defined by the American Nurses Association (ANA) as, “A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and patient, family, group, community, and population preferences and values.” [ 7 ]
Nursing Process
The nursing process is a critical thinking model based on a systematic approach to patient-centered care. Nurses use the nursing process to perform clinical reasoning and make clinical judgments when providing patient care. The nursing process is based on the Standards of Professional Nursing Practice established by the American Nurses Association (ANA). These standards are authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently. [ 8 ] The mnemonic ADOPIE is an easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: A ssessment, D iagnosis, O utcomes Identification, P lanning, I mplementation, and E valuation.
The nursing process is a continuous, cyclic process that is constantly adapting to the patient’s current health status. See Figure 4.3 [ 9 ] for an illustration of the nursing process.
The Nursing Process
Review Scenario A in the following box for an example of a nurse using the nursing process while providing patient care.
Patient Scenario A: Using the Nursing Process [ 10 ]

A hospitalized patient has a prescription to receive Lasix 80mg IV every morning for a medical diagnosis of heart failure. During the morning assessment, the nurse notes that the patient has a blood pressure of 98/60, heart rate of 100, respirations of 18, and a temperature of 98.7F. The nurse reviews the medical record for the patient’s vital signs baseline and observes the blood pressure trend is around 110/70 and the heart rate in the 80s. The nurse recognizes these cues form a pattern related to fluid imbalance and hypothesizes that the patient may be dehydrated. The nurse gathers additional information and notes the patient’s weight has decreased 4 pounds since yesterday. The nurse talks with the patient and validates the hypothesis when the patient reports that their mouth feels like cotton and they feel light-headed. By using critical thinking and clinical judgment, the nurse diagnoses the patient with the nursing diagnosis Fluid Volume Deficit and establishes outcomes for reestablishing fluid balance. The nurse withholds the administration of IV Lasix and contacts the health care provider to discuss the patient’s current fluid status. After contacting the provider, the nurse initiates additional nursing interventions to promote oral intake and closely monitor hydration status. By the end of the shift, the nurse evaluates the patient status and determines that fluid balance has been restored.
In Scenario A, the nurse is using clinical judgment and not just “following orders” to administer the Lasix as scheduled. The nurse assesses the patient, recognizes cues, creates a generalization and hypothesis regarding the fluid status, plans and implements nursing interventions, and evaluates the outcome. Additionally, the nurse promotes patient safety by contacting the provider before administering a medication that could cause harm to the patient at this time.
The ANA’s Standards of Professional Nursing Practice associated with each component of the nursing process are described below.
The “Assessment” Standard of Practice is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.” [ 11 ] A registered nurse uses a systematic method to collect and analyze patient data. Assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. For example, a nurse’s assessment of a hospitalized patient in pain includes the patient’s response to pain, such as the inability to get out of bed, refusal to eat, withdrawal from family members, or anger directed at hospital staff. [ 12 ]
The “Assessment” component of the nursing process is further described in the “ Assessment ” section of this chapter.
The “Diagnosis” Standard of Practice is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.” [ 13 ] A nursing diagnosis is the nurse’s clinical judgment about the client's response to actual or potential health conditions or needs. Nursing diagnoses are the bases for the nurse’s care plan and are different than medical diagnoses. [ 14 ]
The “Diagnosis” component of the nursing process is further described in the “ Diagnosis ” section of this chapter.
Outcomes Identification
The “Outcomes Identification” Standard of Practice is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.” [ 15 ] The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the patient based on their assessment data and nursing diagnoses.
The “Outcomes Identification” component of the nursing process is further described in the “ Outcomes Identification ” section of this chapter.
The “Planning” Standard of Practice is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.” [ 16 ] Assessment data, diagnoses, and goals are used to select evidence-based nursing interventions customized to each patient’s needs and concerns. Goals, expected outcomes, and nursing interventions are documented in the patient’s nursing care plan so that nurses, as well as other health professionals, have access to it for continuity of care. [ 17 ]
The “Planning” component of the nursing process is further described in the “ Planning ” section of this chapter.
NURSING CARE PLANS
Creating nursing care plans is a part of the “Planning” step of the nursing process. A nursing care plan is a type of documentation that demonstrates the individualized planning and delivery of nursing care for each specific patient using the nursing process. Registered nurses (RNs) create nursing care plans so that the care provided to the patient across shifts is consistent among health care personnel. Some interventions can be delegated to Licensed Practical Nurses (LPNs) or trained Unlicensed Assistive Personnel (UAPs) with the RN’s supervision. Developing nursing care plans and implementing appropriate delegation are further discussed under the “ Planning ” and “ Implementing ” sections of this chapter.
Implementation
The “Implementation” Standard of Practice is defined as, “The nurse implements the identified plan.” [ 18 ] Nursing interventions are implemented or delegated with supervision according to the care plan to assure continuity of care across multiple nurses and health professionals caring for the patient. Interventions are also documented in the patient’s electronic medical record as they are completed. [ 19 ]
The “Implementation” Standard of Professional Practice also includes the subcategories “Coordination of Care” and “Health Teaching and Health Promotion” to promote health and a safe environment. [ 20 ]
The “Implementation” component of the nursing process is further described in the “ Implementation ” section of this chapter.
The “Evaluation” Standard of Practice is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.” [ 21 ] During evaluation, nurses assess the patient and compare the findings against the initial assessment to determine the effectiveness of the interventions and overall nursing care plan. Both the patient’s status and the effectiveness of the nursing care must be continuously evaluated and modified as needed. [ 22 ]
The “Evaluation” component of the nursing process is further described in the “ Evaluation ” section of this chapter.
Benefits of Using the Nursing Process
Using the nursing process has many benefits for nurses, patients, and other members of the health care team. The benefits of using the nursing process include the following:
- Promotes quality patient care
- Decreases omissions and duplications
- Provides a guide for all staff involved to provide consistent and responsive care
- Encourages collaborative management of a patient’s health care problems
- Improves patient safety
- Improves patient satisfaction
- Identifies a patient’s goals and strategies to attain them
- Increases the likelihood of achieving positive patient outcomes
- Saves time, energy, and frustration by creating a care plan or path to follow
By using these components of the nursing process as a critical thinking model, nurses plan interventions customized to the patient’s needs, plan outcomes and interventions, and determine whether those actions are effective in meeting the patient’s needs. In the remaining sections of this chapter, we will take an in-depth look at each of these components of the nursing process. Using the nursing process and implementing evidence-based practices are referred to as the “science of nursing.” Let’s review concepts related to the “art of nursing” while providing holistic care in a caring manner using the nursing process.
Holistic Nursing Care
The American Nurses Association (ANA) recently updated the definition of nursing as, “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity.” [ 23 ]
The ANA further describes nursing is a learned profession built on a core body of knowledge that integrates both the art and science of nursing. The art of nursing is defined as, “Unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care.” [ 24 ]
Nurses care for individuals holistically, including their emotional, spiritual, psychosocial, cultural, and physical needs. They consider problems, issues, and needs that the person experiences as a part of a family and a community as they use the nursing process. Review a scenario illustrating holistic nursing care provided to a patient and their family in the following box.
Holistic Nursing Care Scenario
A single mother brings her child to the emergency room for ear pain and a fever. The physician diagnoses the child with an ear infection and prescribes an antibiotic. The mother is advised to make a follow-up appointment with their primary provider in two weeks. While providing discharge teaching, the nurse discovers that the family is unable to afford the expensive antibiotic prescribed and cannot find a primary care provider in their community they can reach by a bus route. The nurse asks a social worker to speak with the mother about affordable health insurance options and available providers in her community and follows up with the prescribing physician to obtain a prescription for a less expensive generic antibiotic. In this manner, the nurse provides holistic care and advocates for improved health for the child and their family.
Review how to provide culturally responsive care and reduce health disparities in the “ Diverse Patients ” chapter.
Caring and the nursing process.
The American Nurses Association (ANA) states, “The act of caring is foundational to the practice of nursing.” [ 25 ] Successful use of the nursing process requires the development of a care relationship with the patient. A care relationship is a mutual relationship that requires the development of trust between both parties. This trust is often referred to as the development of rapport and underlies the art of nursing. While establishing a caring relationship, the whole person is assessed, including the individual’s beliefs, values, and attitudes, while also acknowledging the vulnerability and dignity of the patient and family. Assessing and caring for the whole person takes into account the physical, mental, emotional, and spiritual aspects of being a human being. [ 26 ] Caring interventions can be demonstrated in simple gestures such as active listening, making eye contact, touching, and verbal reassurances while also respecting and being sensitive to the care recipient’s cultural beliefs and meanings associated with caring behaviors. [ 27 ] See Figure 4.4 [ 28 ] for an image of a nurse using touch as a therapeutic communication technique to communicate caring.
Touch as a Therapeutic Communication Technique
Review how to communicate with patients using therapeutic communication techniques like active listening in the “ Communication ” chapter.
Dr. Jean Watson is a nurse theorist who has published many works on the art and science of caring in the nursing profession. Her theory of human caring sought to balance the cure orientation of medicine, giving nursing its unique disciplinary, scientific, and professional standing with itself and the public. Dr. Watson’s caring philosophy encourages nurses to be authentically present with their patients while creating a healing environment. [ 29 ]
Read more about Dr. Watson’s theory of caring at the Watson Caring Science Institute .
Now that we have discussed basic concepts related to the nursing process, let’s look more deeply at each component of the nursing process in the following sections.
4.3. ASSESSMENT
Assessment is the first step of the nursing process (and the first Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.” This includes collecting “pertinent data related to the health and quality of life in a systematic, ongoing manner, with compassion and respect for the wholeness, inherent dignity, worth, and unique attributes of every person, including but not limited to, demographics, environmental and occupational exposures, social determinants of health, health disparities, physical, functional, psychosocial, emotional, cognitive, spiritual/transpersonal, sexual, sociocultural, age-related, environmental, and lifestyle/economic assessments.” [ 1 ]
Nurses assess patients to gather clues, make generalizations, and diagnose human responses to health conditions and life processes. Patient data is considered either subjective or objective, and it can be collected from multiple sources.
Subjective Assessment Data
Subjective data is information obtained from the patient and/or family members and offers important cues from their perspectives. When documenting subjective data stated by a patient, it should be in quotation marks and start with verbiage such as, The patient reports. It is vital for the nurse to establish rapport with a patient to obtain accurate, valuable subjective data regarding the mental, emotional, and spiritual aspects of their condition.
There are two types of subjective information, primary and secondary. Primary data is information provided directly by the patient. Patients are the best source of information about their bodies and feelings, and the nurse who actively listens to a patient will often learn valuable information while also promoting a sense of well-being. Information collected from a family member, chart, or other sources is known as secondary data . Family members can provide important information, especially for individuals with memory impairments, infants, children, or when patients are unable to speak for themselves.
See Figure 4.5 [ 2 ] for an illustration of a nurse obtaining subjective data and establishing rapport after obtaining permission from the patient to sit on the bed.
Example. An example of documented subjective data obtained from a patient assessment is, “The patient reports, ‘My pain is a level 2 on a 1-10 scale.’”
Objective Assessment Data
Objective data is anything that you can observe through your sense of hearing, sight, smell, and touch while assessing the patient. Objective data is reproducible, meaning another person can easily obtain the same data. Examples of objective data are vital signs, physical examination findings, and laboratory results. See Figure 4.6 [ 3 ] for an image of a nurse performing a physical examination.
Physical Examination
Example. An example of documented objective data is, “The patient’s radial pulse is 58 and regular, and their skin feels warm and dry.”
Sources of Assessment Data
There are three sources of assessment data: interview, physical examination, and review of laboratory or diagnostic test results.
Interviewing
Interviewing includes asking the patient questions, listening, and observing verbal and nonverbal communication. Reviewing the chart prior to interviewing the patient may eliminate redundancy in the interview process and allows the nurse to hone in on the most significant areas of concern or need for clarification. However, if information in the chart does not make sense or is incomplete, the nurse should use the interview process to verify data with the patient.
After performing patient identification, the best way to initiate a caring relationship is to introduce yourself to the patient and explain your role. Share the purpose of your interview and the approximate time it will take. When beginning an interview, it may be helpful to start with questions related to the patient’s medical diagnoses to gather information about how they have affected the patient’s functioning, relationships, and lifestyle. Listen carefully and ask for clarification when something isn’t clear to you. Patients may not volunteer important information because they don’t realize it is important for their care. By using critical thinking and active listening, you may discover valuable cues that are important to provide safe, quality nursing care. Sometimes nursing students can feel uncomfortable having difficult conversations or asking personal questions due to generational or other cultural differences. Don’t shy away from asking about information that is important to know for safe patient care. Most patients will be grateful that you cared enough to ask and listen.
Be alert and attentive to how the patient answers questions, as well as when they do not answer a question. Nonverbal communication and body language can be cues to important information that requires further investigation. A keen sense of observation is important. To avoid making inappropriate inferences , the nurse should validate any cues. For example, a nurse may make an inference that a patient is depressed when the patient avoids making eye contact during an interview. However, upon further questioning, the nurse may discover that the patient’s cultural background believes direct eye contact to be disrespectful and this is why they are avoiding eye contact. To read more information about communicating with patients, review the “ Communication ” chapter of this book.
A physical examination is a systematic data collection method of the body that uses the techniques of inspection, auscultation, palpation, and percussion. Inspection is the observation of a patient’s anatomical structures. Auscultation is listening to sounds, such as heart, lung, and bowel sounds, created by organs using a stethoscope. Palpation is the use of touch to evaluate organs for size, location, or tenderness. Percussion is an advanced physical examination technique typically performed by providers where body parts are tapped with fingers to determine their size and if fluid is present. Detailed physical examination procedures of various body systems can be found in the Open RN Nursing Skills textbook with a head-to-toe checklist in Appendix C . Physical examination also includes the collection and analysis of vital signs.
Registered Nurses (RNs) complete the initial physical examination and analyze the findings as part of the nursing process. Collection of follow-up physical examination data can be delegated to Licensed Practical Nurses/Licensed Vocational Nurses (LPNs/LVNs) , or measurements such as vital signs and weight may be delegated to trained Unlicensed Assistive Personnel (UAP) when appropriate to do so. However, the RN remains responsible for supervising these tasks, analyzing the findings, and ensuring they are documented .
A physical examination can be performed as a comprehensive, head-to-toe assessment or as a focused assessment related to a particular condition or problem. Assessment data is documented in the patient’s Electronic Medical Record (EMR) , an electronic version of the patient’s medical chart.
Reviewing Laboratory and Diagnostic Test Results
Reviewing laboratory and diagnostic test results provides relevant and useful information related to the needs of the patient. Understanding how normal and abnormal results affect patient care is important when implementing the nursing care plan and administering provider prescriptions. If results cause concern, it is the nurse’s responsibility to notify the provider and verify the appropriateness of prescriptions based on the patient’s current status before implementing them.
Types of Assessments
Several types of nursing assessment are used in clinical practice:
- Primary Survey: Used during every patient encounter to briefly evaluate level of consciousness, airway, breathing, and circulation and implement emergency care if needed.
- Admission Assessment: A comprehensive assessment completed when a patient is admitted to a facility that involves assessing a large amount of information using an organized approach.
- Ongoing Assessment: In acute care agencies such as hospitals, a head-to-toe assessment is completed and documented at least once every shift. Any changes in patient condition are reported to the health care provider.
- Focused Assessment: Focused assessments are used to reevaluate the status of a previously diagnosed problem.
- Time-lapsed Reassessment: Time-lapsed reassessments are used in long-term care facilities when three or more months have elapsed since the previous assessment to evaluate progress on previously identified outcomes. [ 4 ]
Putting It Together
Review Scenario C in the following box to apply concepts of assessment to a patient scenario.
Scenario C [5]

Ms. J. is a 74-year-old woman who is admitted directly to the medical unit after visiting her physician because of shortness of breath, increased swelling in her ankles and calves, and fatigue. Her medical history includes hypertension (30 years), coronary artery disease (18 years), heart failure (2 years), and type 2 diabetes (14 years). She takes 81 mg of aspirin every day, metoprolol 50 mg twice a day, furosemide 40 mg every day, and metformin 2,000 mg every day.
Ms. J.’s vital sign values on admission were as follows:
- Blood Pressure: 162/96 mm Hg
- Heart Rate: 88 beats/min
- Oxygen Saturation: 91% on room air
- Respiratory Rate: 28 breaths/minute
- Temperature: 97.8 degrees F orally
Her weight is up 10 pounds since the last office visit three weeks prior. The patient states, “I am so short of breath” and “My ankles are so swollen I have to wear my house slippers.” Ms. J. also shares, “I am so tired and weak that I can’t get out of the house to shop for groceries,” and “Sometimes I’m afraid to get out of bed because I get so dizzy.” She confides, “I would like to learn more about my health so I can take better care of myself.”
The physical assessment findings of Ms. J. are bilateral basilar crackles in the lungs and bilateral 2+ pitting edema of the ankles and feet. Laboratory results indicate a decreased serum potassium level of 3.4 mEq/L.
As the nurse completes the physical assessment, the patient’s daughter enters the room. She confides, “We are so worried about mom living at home by herself when she is so tired all the time!”
Critical Thinking Questions
Identify subjective data.
Identify objective data.
Provide an example of secondary data.
Answers are located in the Answer Key at the end of the book.
4.4. DIAGNOSIS
Diagnosis is the second step of the nursing process (and the second Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse analyzes assessment data to determine actual or potential diagnoses, problems, and issues.” The RN “prioritizes diagnoses, problems, and issues based on mutually established goals to meet the needs of the health care consumer across the health–illness continuum and the care continuum.” Diagnoses, problems, strengths, and issues are documented in a manner that facilitates the development of expected outcomes and a collaborative plan. [ 1 ]
Analyzing Assessment Data
After collection of assessment data, the registered nurse analyzes the data to form generalizations and create hypotheses for nursing diagnoses. Steps for analyzing assessment data include performing data analysis, clustering of information, identifying hypotheses for potential nursing diagnosis, performing additional in-depth assessment as needed, and establishing nursing diagnosis statements. The nursing diagnoses are then prioritized and drive the nursing care plan. [ 2 ]
Performing Data Analysis
After nurses collect assessment data from a patient, they use their nursing knowledge to analyze that data to determine if it is “expected” or “unexpected” or “normal” or “abnormal” for that patient according to their age, development, and baseline status. From there, nurses determine what data are “clinically relevant” as they prioritize their nursing care. [ 3 ]
Example. In Scenario C in the “Assessment” section of this chapter, the nurse analyzes the vital signs data and determines the blood pressure, heart rate, and respiratory rate are elevated, and the oxygen saturation is decreased for this patient. These findings are considered “relevant cues.”
Clustering Information/Seeing Patterns/Making Hypotheses
After analyzing the data and determining relevant cues, the nurse clusters data into patterns. Assessment frameworks such as Gordon’s Functional Health Patterns assist nurses in clustering information according to evidence-based patterns of human responses. See the box below for an outline of Gordon’s Functional Health Patterns. [ 4 ] Concepts related to many of these patterns will be discussed in chapters later in this book.
Example. Refer to Scenario C of the “Assessment” section of this chapter. The nurse clusters the following relevant cues: elevated blood pressure, elevated respiratory rate, crackles in the lungs, weight gain, worsening edema, shortness of breath, a medical history of heart failure, and currently prescribed a diuretic medication. These cues are clustered into a generalization/pattern of fluid balance, which can be classified under Gordon’s Nutritional-Metabolic Functional Health Pattern. The nurse makes a hypothesis that the patient has excess fluid volume present.
Gordon’s Functional Health Patterns [ 5 ]
Health Perception-Health Management: A patient’s perception of their health and well-being and how it is managed
Nutritional-Metabolic: Food and fluid consumption relative to metabolic need
Elimination: Excretory function, including bowel, bladder, and skin
Activity-Exercise: Exercise and daily activities
Sleep-Rest: Sleep, rest, and daily activities
Cognitive-Perceptual: Perception and cognition
Self-perception and Self-concept: Self-concept and perception of self-worth, self-competency, body image, and mood state
Role-Relationship: Role engagements and relationships
Sexuality-Reproductive: Reproduction and satisfaction or dissatisfaction with sexuality
Coping-Stress Tolerance: Coping and effectiveness in terms of stress tolerance
Value-Belief: Values, beliefs (including spiritual beliefs), and goals that guide choices and decisions
Identifying Nursing Diagnoses
After the nurse has analyzed and clustered the data from the patient assessment, the next step is to begin to answer the question, “What are my patient’s human responses (i.e., nursing diagnoses)?” A nursing diagnosis is defined as, “A clinical judgment concerning a human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group, or community.” [ 6 ] Nursing diagnoses are customized to each patient and drive the development of the nursing care plan. The nurse should refer to a care planning resource and review the definitions and defining characteristics of the hypothesized nursing diagnoses to determine if additional in-depth assessment is needed before selecting the most accurate nursing diagnosis.
Nursing diagnoses are developed by nurses, for use by nurses. For example, NANDA International (NANDA-I) is a global professional nursing organization that develops nursing terminology that names actual or potential human responses to health problems and life processes based on research findings. [ 7 ] Currently, there are over 220 NANDA-I nursing diagnoses developed by nurses around the world. This list is continuously updated, with new nursing diagnoses added and old nursing diagnoses retired that no longer have supporting evidence. A list of commonly used NANDA-I diagnoses are listed in Appendix A . For a full list of NANDA-I nursing diagnoses, refer to a current nursing care plan reference.
NANDA-I nursing diagnoses are grouped into 13 domains that assist the nurse in selecting diagnoses based on the patterns of clustered data. These domains are similar to Gordon’s Functional Health Patterns and include health promotion, nutrition, elimination and exchange, activity/rest, perception/cognition, self-perception, role relationship, sexuality, coping/stress tolerance, life principles, safety/protection, comfort, and growth/development.
Knowledge regarding specific NANDA-I nursing diagnoses is not assessed on the NCLEX. However, analyzing cues and creating hypotheses are part of the measurement model used to assess a candidate’s clinical judgment. Read more about the NCLEX and Next Generation NCLEX in the “ Scope of Practice ” chapter.
Nursing diagnoses vs. medical diagnoses.
You may be asking yourself, “How are nursing diagnoses different from medical diagnoses?” Medical diagnoses focus on diseases or other medical problems that have been identified by the physician, physician’s assistant, or advanced nurse practitioner. Nursing diagnoses focus on the human response to health conditions and life processes and are made independently by RNs. Patients with the same medical diagnosis will often respond differently to that diagnosis and thus have different nursing diagnoses. For example, two patients have the same medical diagnosis of heart failure. However, one patient may be interested in learning more information about the condition and the medications used to treat it, whereas another patient may be experiencing anxiety when thinking about the effects this medical diagnosis will have on their family. The nurse must consider these different responses when creating the nursing care plan. Nursing diagnoses consider the patient’s and family’s needs, attitudes, strengths, challenges, and resources as a customized nursing care plan is created to provide holistic and individualized care for each patient.
Example. A medical diagnosis identified for Ms. J. in Scenario C in the “Assessment” section is heart failure. This cannot be used as a nursing diagnosis, but it can be considered as an “associated condition” when creating hypotheses for nursing diagnoses. Associated conditions are medical diagnoses, injuries, procedures, medical devices, or pharmacological agents that are not independently modifiable by the nurse, but support accuracy in nursing diagnosis. The nursing diagnosis in Scenario C will be related to the patient’s response to heart failure.
Additional Definitions Used in NANDA-I Nursing Diagnoses
The following definitions of patient, age, and time are used in association with NANDA-I nursing diagnoses:
The NANDA-I definition of a “patient” includes:
- Individual: a single human being distinct from others (i.e., a person).
- Caregiver: a family member or helper who regularly looks after a child or a sick, elderly, or disabled person.
- Family: two or more people having continuous or sustained relationships, perceiving reciprocal obligations, sensing common meaning, and sharing certain obligations toward others; related by blood and/or choice.
- Group: a number of people with shared characteristics generally referred to as an ethnic group.
- Community: a group of people living in the same locale under the same governance. Examples include neighborhoods and cities. [ 8 ]
The age of the person who is the subject of the diagnosis is defined by the following terms: [ 9 ]
- Fetus: an unborn human more than eight weeks after conception, until birth.
- Neonate: a person less than 28 days of age.
- Infant: a person greater than 28 days and less than 1 year of age.
- Child: a person aged 1 to 9 years
- Adolescent: a person aged 10 to 19 years
- Adult: a person older than 19 years of age unless national law defines a person as being an adult at an earlier age.
- Older adult: a person greater than 65 years of age.
The duration of the diagnosis is defined by the following terms: [ 10 ]
- Acute: lasting less than 3 months.
- Chronic: lasting greater than 3 months.
- Intermittent: stopping or starting again at intervals
- Continuous: uninterrupted, going on without stop.
New Terms Used in 2018-2020 NANDA-I Diagnoses
The 2018-2020 edition of Nursing Diagnoses includes two new terms to assist in creating nursing diagnoses: at-risk populations and associated conditions. [ 11 ]
At-Risk Populations are groups of people who share a characteristic that causes each member to be susceptible to a particular human response, such as demographics, health/family history, stages of growth/development, or exposure to certain events/experiences.
Associated Conditions are medical diagnoses, injuries, procedures, medical devices, or pharmacological agents. These conditions are not independently modifiable by the nurse, but support accuracy in nursing diagnosis [ 12 ]
Types of Nursing Diagnoses
There are four types of NANDA-I nursing diagnoses: [ 13 ]
- Problem-Focused
- Health Promotion – Wellness
A problem-focused nursing diagnosis is a “clinical judgment concerning an undesirable human response to health condition/life processes that exist in an individual, family, group, or community.” [ 14 ] To make an accurate problem-focused diagnosis, related factors and defining characteristics must be present. Related factors (also called etiology) are causes that contribute to the diagnosis. Defining characteristics are cues, signs, and symptoms that cluster into patterns. [ 15 ]
A health promotion-wellness nursing diagnosis is “a clinical judgment concerning motivation and desire to increase well-being and to actualize human health potential.” These responses are expressed by the patient’s readiness to enhance specific health behaviors. [ 16 ] A health promotion-wellness diagnosis is used when the patient is willing to improve a lack of knowledge, coping, or other identified need.
A risk nursing diagnosis is “a clinical judgment concerning the vulnerability of an individual, family, group, or community for developing an undesirable human response to health conditions/life processes.” [ 17 ] A risk nursing diagnosis must be supported by risk factors that contribute to the increased vulnerability. A risk nursing diagnosis is different from the problem-focused diagnosis in that the problem has not yet actually occurred. Problem diagnoses should not be automatically viewed as more important than risk diagnoses because sometimes a risk diagnosis can have the highest priority for a patient. [ 18 ]
A syndrome diagnosis is a “clinical judgment concerning a specific cluster of nursing diagnoses that occur together, and are best addressed together and through similar interventions.” [ 19 ]
Establishing Nursing Diagnosis Statements
When using NANDA-I nursing diagnoses, NANDA-I recommends the structure of a nursing diagnosis should be a statement that includes the nursing diagnosis and related factors as exhibited by defining characteristics . The accuracy of the nursing diagnosis is validated when a nurse is able to clearly link the defining characteristics, related factors, and/or risk factors found during the patient’s assessment. [ 20 ]
To create a nursing diagnosis statement, the registered nurse completes the following steps. After analyzing the patient’s subjective and objective data and clustering the data into patterns, the nurse generates hypotheses for nursing diagnoses based on how the patterns meet defining characteristics of a nursing diagnosis. Defining characteristics is the terminology used for observable signs and symptoms related to a nursing diagnosis. [ 21 ] Defining characteristics are included in care planning resources for each nursing diagnosis, along with a definition of that diagnosis, so the nurse can select the most accurate diagnosis. For example, objective and subjective data such as weight, height, and dietary intake can be clustered together as defining characteristics for the nursing diagnosis of nutritional status.
When creating a nursing diagnosis statement, the nurse also identifies the cause of the problem for that specific patient. Related factors is the terminology used for the underlying causes (etiology) of a patient’s problem or situation. Related factors should not be a medical diagnosis, but instead should be attributed to the underlying pathophysiology that the nurse can treat. When possible, the nursing interventions planned for each nursing diagnosis should attempt to modify or remove these related factors that are the underlying cause of the nursing diagnosis. [ 22 ]
Creating nursing diagnosis statements has traditionally been referred to as “using PES format.” The PES mnemonic no longer applies to the current terminology used by NANDA-I, but the components of a nursing diagnosis statement remain the same. A nursing diagnosis statement should contain the problem, related factors, and defining characteristics. These terms fit under the former PES format in this manner:
Problem (P) – the patient p roblem (i.e., the nursing diagnosis)
Etiology (E) – related factors (i.e., the e tiology/cause) of the nursing diagnosis; phrased as “related to” or “R/T”
Signs and Symptoms (S) – defining characteristics manifested by the patient (i.e., the s igns and s ymptoms/subjective and objective data) that led to the identification of that nursing diagnosis for the patient; phrased with “as manifested by” or “as evidenced by.”
Examples of different types of nursing diagnoses are further explained below.
Problem-Focused Nursing Diagnosis
A problem-focused nursing diagnosis contains all three components of the PES format :
Problem (P) – statement of the patient response (nursing diagnosis)
Etiology (E) – related factors contributing to the nursing diagnosis
Signs and Symptoms (S) – defining characteristics manifested by that patient
SAMPLE PROBLEM-FOCUSED NURSING DIAGNOSIS STATEMENT
Refer to Scenario C of the “Assessment” section of this chapter. The cluster of data for Ms. J. (elevated blood pressure, elevated respiratory rate, crackles in the lungs, weight gain, worsening edema, and shortness of breath) are defining characteristics for the NANDA-I Nursing Diagnosis Excess Fluid Volume . The NANDA-I definition of Excess Fluid Volume is “surplus intake and/or retention of fluid.” The related factor (etiology) of the problem is that the patient has excessive fluid intake. [ 23 ]
The components of a problem-focused nursing diagnosis statement for Ms. J. would be:
Fluid Volume Excess
Related to excessive fluid intake
As manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, increased weight of 10 pounds, and the patient reports, “ My ankles are so swollen .”
A correctly written problem-focused nursing diagnosis statement for Ms. J. would look like this:
Fluid Volume Excess related to excessive fluid intake as manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, an increase weight of 10 pounds, and the patient reports, “My ankles are so swollen.”
Health-Promotion Nursing Diagnosis
A health-promotion nursing diagnosis statement contains the problem (P) and the defining characteristics (S). The defining characteristics component of a health-promotion nursing diagnosis statement should begin with the phrase “expresses desire to enhance”: [ 24 ]
Signs and Symptoms (S) – the patient’s expressed desire to enhance
SAMPLE HEALTH-PROMOTION NURSING DIAGNOSIS STATEMENT
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. demonstrates a readiness to improve her health status when she told the nurse that she would like to “learn more about my health so I can take better care of myself.” This statement is a defining characteristic of the NANDA-I nursing diagnosis Readiness for Enhanced Health Management , which is defined as “a pattern of regulating and integrating into daily living a therapeutic regimen for the treatment of illness and its sequelae, which can be strengthened.” [ 25 ]
The components of a health-promotion nursing diagnosis for Ms. J. would be:
Problem (P): Readiness for Enhanced Health Management
Symptoms (S): Expressed desire to “learn more about my health so I can take better care of myself.”
A correctly written health-promotion nursing diagnosis statement for Ms. J. would look like this:
Enhanced Readiness for Health Promotion as manifested by expressed desire to “learn more about my health so I can take better care of myself.”
Risk Nursing Diagnosis
A risk nursing diagnosis should be supported by evidence of the patient’s risk factors for developing that problem. Different experts recommend different phrasing. NANDA-I 2018-2020 recommends using the phrase “as evidenced by” to refer to the risk factors for developing that problem. [ 26 ]
A risk diagnosis consists of the following:
As Evidenced By – Risk factors for developing the problem
SAMPLE RISK DIAGNOSIS STATEMENT
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. has an increased risk of falling due to vulnerability from the dizziness and weakness she is experiencing. The NANDA-I definition of Risk for Falls is “increased susceptibility to falling, which may cause physical harm and compromise health.” [ 27 ]
The components of a risk diagnosis statement for Ms. J. would be:
Problem (P) – Risk for Falls
As Evidenced By – Dizziness and decreased lower extremity strength
A correctly written risk nursing diagnosis statement for Ms. J. would look like this:
Risk for Falls as evidenced by dizziness and decreased lower extremity strength.
Syndrome Diagnosis
A syndrome is a cluster of nursing diagnoses that occur together and are best addressed together and through similar interventions. To create a syndrome diagnosis, two or more nursing diagnoses must be used as defining characteristics (S) that create a syndrome. Related factors may be used if they add clarity to the definition, but are not required. [ 28 ]
A syndrome statement consists of these items:
Problem (P) – the syndrome
Signs and Symptoms (S) – the defining characteristics are two or more similar nursing diagnoses
SAMPLE SYNDROME DIAGNOSIS STATEMENT
Refer to Scenario C in the “Assessment” section of this chapter. Clustering the data for Ms. J. identifies several similar NANDA-I nursing diagnoses that can be categorized as a syndrome . For example, Activity Intolerance is defined as “insufficient physiological or psychological energy to endure or complete required or desired daily activities.” Social Isolation is defined as “aloneness experienced by the individual and perceived as imposed by others and as a negative or threatening state.” These diagnoses can be included under the the NANDA-I syndrome named Risk for Frail Elderly Syndrome. This syndrome is defined as a “dynamic state of unstable equilibrium that affects the older individual experiencing deterioration in one or more domains of health (physical, functional, psychological, or social) and leads to increased susceptibility to adverse health effects, in particular disability.” [ 29 ]
The components of a syndrome nursing diagnosis for Ms. J. would be:
– Risk for Frail Elderly Syndrome
– The nursing diagnoses of Activity Intolerance and Social Isolation
Additional related factor: Fear of falling
A correctly written syndrome diagnosis statement for Ms. J. would look like this:
Risk for Frail Elderly Syndrome related to activity intolerance, social isolation, and fear of falling
Prioritization
After identifying nursing diagnoses, the next step is prioritization according to the specific needs of the patient. Nurses prioritize their actions while providing patient care multiple times every day. Prioritization is the process that identifies the most significant nursing problems, as well as the most important interventions, in the nursing care plan.
It is essential that life-threatening concerns and crises are identified immediately and addressed quickly. Depending on the severity of a problem, the steps of the nursing process may be performed in a matter of seconds for life-threatening concerns. In critical situations, the steps of the nursing process are performed through rapid clinical judgment. Nurses must recognize cues signaling a change in patient condition, apply evidence-based practices in a crisis, and communicate effectively with interprofessional team members. Most patient situations fall somewhere between a crisis and routine care.
There are several concepts used to prioritize, including Maslow’s Hierarchy of Needs, the “ABCs” (Airway, Breathing and Circulation), and acute, uncompensated conditions. See the infographic in Figure 4.7 [30] on The How To of Prioritization .
The How To of Prioritization
Maslow’s Hierarchy of Needs is used to categorize the most urgent patient needs. The bottom levels of the pyramid represent the top priority needs of physiological needs intertwined with safety. See Figure 4.8 [31] for an image of Maslow’s Hierarchy of Needs. You may be asking yourself, “What about the ABCs – isn’t airway the most important?” The answer to that question is “it depends on the situation and the associated safety considerations.” Consider this scenario – you are driving home after a lovely picnic in the country and come across a fiery car crash. As you approach the car, you see that the passenger is not breathing. Using Maslow’s Hierarchy of Needs to prioritize your actions, you remove the passenger from the car first due to safety even though he is not breathing. After ensuring safety and calling for help, you follow the steps to perform cardiopulmonary resuscitation (CPR) to establish circulation, airway, and breathing until help arrives.
Maslow’s Hierarchy of Needs
In addition to using Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation, the nurse also considers if the patient’s condition is an acute or chronic problem. Acute, uncompensated conditions generally require priority interventions over chronic conditions. Additionally, actual problems generally receive priority over potential problems, but risk problems sometimes receive priority depending on the patient vulnerability and risk factors.
Example. Refer to Scenario C in the “Assessment” section of this chapter. Four types of nursing diagnoses were identified for Ms. J.: Fluid Volume Excess, Enhanced Readiness for Health Promotion, Risk for Falls , and Risk for Frail Elderly Syndrome . The top priority diagnosis is Fluid Volume Excess because it affects the physiological needs of breathing, homeostasis, and excretion. However, the Risk for Falls diagnosis comes in a close second because of safety implications and potential injury that could occur if the patient fell.
American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020 . Thieme Publishers New York. ↵
Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
Gordon, M. (2008). Assess notes: Nursing assessment and diagnostic reasoning. F.A. Davis Company. ↵
NANDA International. (n.d.). Glossary of terms . https://nanda .org/nanda-i-resources /glossary-of-terms / ↵
NANDA International. (n.d.). Glossary of terms . https://nanda .org/nanda-i-resources /glossary-of-terms/ ↵
NANDA International. (n.d.). Glossary of terms. https://nanda .org/nanda-i-resources /glossary-of-terms/ ↵
“The How To of Prioritization” by Valerie Palarski for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
“ Maslow's hierarchy of needs.svg ” by J. Finkelstein is licensed under CC BY-SA 3.0 ↵
4.5. OUTCOME IDENTIFICATION
Outcome Identification is the third step of the nursing process (and the third Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.” The RN collaborates with the health care consumer, interprofessional team, and others to identify expected outcomes integrating the health care consumer’s culture, values, and ethical considerations. Expected outcomes are documented as measurable goals with a time frame for attainment. [ 1 ]
An outcome is a “measurable behavior demonstrated by the patient responsive to nursing interventions.” [ 2 ] Outcomes should be identified before nursing interventions are planned. After nursing interventions are implemented, the nurse will evaluate if the outcomes were met in the time frame indicated for that patient.
Outcome identification includes setting short- and long-term goals and then creating specific expected outcome statements for each nursing diagnosis.
Short-Term and Long-Term Goals
Nursing care should always be individualized and patient-centered. No two people are the same, and neither should nursing care plans be the same for two people. Goals and outcomes should be tailored specifically to each patient’s needs, values, and cultural beliefs. Patients and family members should be included in the goal-setting process when feasible. Involving patients and family members promotes awareness of identified needs, ensures realistic goals, and motivates their participation in the treatment plan to achieve the mutually agreed upon goals and live life to the fullest with their current condition.
The nursing care plan is a road map used to guide patient care so that all health care providers are moving toward the same patient goals. Goals are broad statements of purpose that describe the overall aim of care. Goals can be short- or long-term. The time frame for short- and long-term goals is dependent on the setting in which the care is provided. For example, in a critical care area, a short-term goal might be set to be achieved within an 8-hour nursing shift, and a long-term goal might be in 24 hours. In contrast, in an outpatient setting, a short-term goal might be set to be achieved within one month and a long-term goal might be within six months.
A nursing goal is the overall direction in which the patient must progress to improve the problem/nursing diagnosis and is often the opposite of the problem.
Example. Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. had a priority nursing diagnosis of Fluid Volume Excess. A broad goal would be, “ Ms. J. will achieve a state of fluid balance. ”
Expected Outcomes
Goals are broad, general statements, but outcomes are specific and measurable. Expected outcomes are statements of measurable action for the patient within a specific time frame that are responsive to nursing interventions. Nurses may create expected outcomes independently or refer to classification systems for assistance. Just as NANDA-I creates and revises standardized nursing diagnoses, a similar classification and standardization process exists for expected nursing outcomes. The Nursing Outcomes Classification (NOC) is a list of over 330 nursing outcomes designed to coordinate with established NANDA-I diagnoses. [ 3 ]
Patient-Centered
Outcome statements are always patient-centered. They should be developed in collaboration with the patient and individualized to meet a patient’s unique needs, values, and cultural beliefs. They should start with the phrase “The patient will…” Outcome statements should be directed at resolving the defining characteristics for that nursing diagnosis. Additionally, the outcome must be something the patient is willing to cooperate in achieving.
Outcome statements should contain five components easily remembered using the “SMART” mnemonic: [ 4 ]
- M easurable
- A ttainable/Action oriented
- R elevant/Realistic
See Figure 4.9 [ 5 ] for an image of the SMART components of outcome statements. Each of these components is further described in the following subsections.
SMART Components of Outcome Statements
Outcome statements should state precisely what is to be accomplished. See the following examples:
- Not specific: “The patient will increase the amount of exercise.”
- Specific: “The patient will participate in a bicycling exercise session daily for 30 minutes.”
Additionally, only one action should be included in each expected outcome. See the following examples:
- “The patient will walk 50 feet three times a day with standby assistance of one and will shower in the morning until discharge” is actually two goals written as one. The outcome of ambulation should be separate from showering for precise evaluation. For instance, the patient could shower but not ambulate, which would make this outcome statement very difficult to effectively evaluate.
- Suggested revision is to create two outcomes statements so each can be measured: The patient will walk 50 feet three times a day with standby assistance of one until discharge. The patient will shower every morning until discharge.
Measurable outcomes have numeric parameters or other concrete methods of judging whether the outcome was met. It is important to use objective data to measure outcomes. If terms like “acceptable” or “normal” are used in an outcome statement, it is difficult to determine whether the outcome is attained. Refer to Figure 4.10 [ 6 ] for examples of verbs that are measurable and not measurable in outcome statements.
Figure 4.10
Measurable Outcomes
See the following examples:
- Not measurable: “The patient will drink adequate fluid amounts every shift.”
- Measurable: “The patient will drink 24 ounces of fluids during every day shift (0600-1400).”
Action-Oriented and Attainable
Outcome statements should be written so that there is a clear action to be taken by the patient or significant others. This means that the outcome statement should include a verb. Refer to Figure 4.11 [ 7 ] for examples of action verbs.
Figure 4.11
Action Verbs
- Not action-oriented: “The patient will get increased physical activity.”
- Action-oriented: “The patient will list three types of aerobic activity that he would enjoy completing every week.”
Realistic and Relevant
Realistic outcomes consider the patient’s physical and mental condition; their cultural and spiritual values, beliefs, and preferences; and their socioeconomic status in terms of their ability to attain these outcomes. Consideration should be also given to disease processes and the effects of conditions such as pain and decreased mobility on the patient’s ability to reach expected outcomes. Other barriers to outcome attainment may be related to health literacy or lack of available resources. Outcomes should always be reevaluated and revised for attainability as needed. If an outcome is not attained, it is commonly because the original time frame was too ambitious or the outcome was not realistic for the patient.
- Not realistic: “The patient will jog one mile every day when starting the exercise program.”
- Realistic: “The patient will walk ½ mile three times a week for two weeks.”
Time Limited
Outcome statements should include a time frame for evaluation. The time frame depends on the intervention and the patient’s current condition. Some outcomes may need to be evaluated every shift, whereas other outcomes may be evaluated daily, weekly, or monthly. During the evaluation phase of the nursing process, the outcomes will be assessed according to the time frame specified for evaluation. If it has not been met, the nursing care plan should be revised.
- Not time limited: “The patient will stop smoking cigarettes.”
- Time limited: “The patient will complete the smoking cessation plan by December 12, 2021.”
In Scenario C in Box 4.3, Ms. J.’s priority nursing diagnosis statement was Fluid Volume Excess related to excess fluid intake as manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, an increase weight of 10 pounds, and the patient reports, “My ankles are so swollen.” An example of an expected outcome meeting SMART criteria for Ms. J. is, “The patient will have clear bilateral lung sounds within the next 24 hours.”
4.6. PLANNING
Planning is the fourth step of the nursing process (and the fourth Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.” The RN develops an individualized, holistic, evidence-based plan in partnership with the health care consumer, family, significant others, and interprofessional team. Elements of the plan are prioritized. The plan is modified according to the ongoing assessment of the health care consumer’s response and other indicators. The plan is documented using standardized language or terminology. [ 1 ]
After expected outcomes are identified, the nurse begins planning nursing interventions to implement. Nursing interventions are evidence-based actions that the nurse performs to achieve patient outcomes. Just as a provider makes medical diagnoses and writes prescriptions to improve the patient’s medical condition, a nurse formulates nursing diagnoses and plans nursing interventions to resolve patient problems. Nursing interventions should focus on eliminating or reducing the related factors (etiology) of the nursing diagnoses when possible. [ 2 ] Nursing interventions, goals, and expected outcomes are written in the nursing care plan for continuity of care across shifts, nurses, and health professionals.
Planning Nursing Interventions
You might be asking yourself, “How do I know what evidence-based nursing interventions to include in the nursing care plan?” There are several sources that nurses and nursing students can use to select nursing interventions. Many agencies have care planning tools and references included in the electronic health record that are easily documented in the patient chart. Nurses can also refer to other care planning books our sources such as the Nursing Interventions Classification (NIC) system. Based on research and input from the nursing profession, NIC categorizes and describes nursing interventions that are constantly evaluated and updated. Interventions included in NIC are considered evidence-based nursing practices. The nurse is responsible for using clinical judgment to make decisions about which interventions are best suited to meet an individualized patient’s needs. [ 3 ]
Direct and Indirect Care
Nursing interventions are considered direct care or indirect care. Direct care refers to interventions that are carried out by having personal contact with patients. Examples of direct care interventions are wound care, repositioning, and ambulation. Indirect care interventions are performed when the nurse provides assistance in a setting other than with the patient. Examples of indirect care interventions are attending care conferences, documenting, and communicating about patient care with other providers.
Classification of Nursing Interventions
There are three types of nursing interventions: independent, dependent, and collaborative. (See Figure 4.12 [ 4 ] for an image of a nurse collaborating with the health care team when planning interventions.)
Figure 4.12
Collaborative nursing interventions, independent nursing interventions.
Any intervention that the nurse can independently provide without obtaining a prescription is considered an independent nursing intervention . An example of an independent nursing intervention is when the nurses monitor the patient’s 24-hour intake/output record for trends because of a risk for imbalanced fluid volume. Another example of independent nursing interventions is the therapeutic communication that a nurse uses to assist patients to cope with a new medical diagnosis.
Example. Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. was diagnosed with Fluid Volume Excess . An example of an evidence-based independent nursing intervention is, “The nurse will reposition the patient with dependent edema frequently, as appropriate.” [ 5 ] The nurse would individualize this evidence-based intervention to the patient and agency policy by stating, “The nurse will reposition the patient every 2 hours.”
Dependent Nursing Interventions
Dependent nursing interventions require a prescription before they can be performed. Prescriptions are orders, interventions, remedies, or treatments ordered or directed by an authorized primary health care provider. [ 6 ] A primary health care provider is a member of the health care team (usually a physician, advanced practice nurse, or physician’s assistant) who is licensed and authorized to formulate prescriptions on behalf of the client. For example, administering medication is a dependent nursing intervention. The nurse incorporates dependent interventions into the patient’s overall care plan by associating each intervention with the appropriate nursing diagnosis.
Example. Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. was diagnosed with Fluid Volume Excess . An example of a dependent nursing intervention is, “The nurse will administer scheduled diuretics as prescribed.”
Collaborative nursing interventions are actions that the nurse carries out in collaboration with other health team members, such as physicians, social workers, respiratory therapists, physical therapists, and occupational therapists. These actions are developed in consultation with other health care professionals and incorporate their professional viewpoint. [ 7 ]
Example. Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. was diagnosed with Fluid Volume Excess . An example of a collaborative nursing intervention is consulting with a respiratory therapist when the patient has deteriorating oxygen saturation levels. The respiratory therapist plans oxygen therapy and obtains a prescription from the provider. The nurse would document “ The nurse will manage oxygen therapy in collaboration with the respiratory therapist ” in the care plan.
Individualization of Interventions
It is vital for the planned interventions to be individualized to the patient to be successful. For example, adding prune juice to the breakfast meal of a patient with constipation will only work if the patient likes to drink the prune juice. If the patient does not like prune juice, then this intervention should not be included in the care plan. Collaboration with the patient, family members, significant others, and the interprofessional team is essential for selecting effective interventions. The number of interventions included in a nursing care plan is not a hard and fast rule, but enough quality, individualized interventions should be planned to meet the identified outcomes for that patient.
Creating Nursing Care Plans
Nursing care plans are created by registered nurses (RNs). Documentation of individualized nursing care plans are legally required in long-term care facilities by the Centers for Medicare and Medicaid Services (CMS) and in hospitals by The Joint Commission. CMS guidelines state, “Residents and their representative(s) must be afforded the opportunity to participate in their care planning process and to be included in decisions and changes in care, treatment, and/or interventions. This applies both to initial decisions about care and treatment, as well as the refusal of care or treatment. Facility staff must support and encourage participation in the care planning process. This may include ensuring that residents, families, or representatives understand the comprehensive care planning process, holding care planning meetings at the time of day when a resident is functioning best and patient representatives can be present, providing sufficient notice in advance of the meeting, scheduling these meetings to accommodate a resident’s representative (such as conducting the meeting in-person, via a conference call, or video conferencing), and planning enough time for information exchange and decision-making. A resident has the right to select or refuse specific treatment options before the care plan is instituted.” [ 8 ] The Joint Commission conceptualizes the care planning process as the structuring framework for coordinating communication that will result in safe and effective care. [ 9 ]
Many facilities have established standardized nursing care plans with lists of possible interventions that can be customized for each specific patient. Other facilities require the nurse to develop each care plan independently. Whatever the format, nursing care plans should be individualized to meet the specific and unique needs of each patient. See Figure 4.13 [ 10 ] for an image of a standardized care plan.
Figure 4.13
Standardized Care Plan
Nursing care plans created in nursing school can also be in various formats such as concept maps or tables. Some are fun and creative, while others are more formal. Appendix B contains a template that can be used for creating nursing care plans.
4.7. IMPLEMENTATION OF INTERVENTIONS
Implementation is the fifth step of the nursing process (and the fifth Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse implements the identified plan.” The RN may delegate planned interventions after considering the circumstance, person, task, communication, supervision, and evaluation, as well as the state Nurse Practice Act, federal regulation, and agency policy. [ 1 ]
Implementation of interventions requires the RN to use critical thinking and clinical judgment. After the initial plan of care is developed, continual reassessment of the patient is necessary to detect any changes in the patient’s condition requiring modification of the plan. The need for continual patient reassessment underscores the dynamic nature of the nursing process and is crucial to providing safe care.
During the implementation phase of the nursing process, the nurse prioritizes planned interventions, assesses patient safety while implementing interventions, delegates interventions as appropriate, and documents interventions performed.
Prioritizing Implementation of Interventions
Prioritizing implementation of interventions follows a similar method as to prioritizing nursing diagnoses. Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation are used to establish top priority interventions. When possible, least invasive actions are usually preferred due to the risk of injury from invasive options. Read more about methods for prioritization under the “ Diagnosis ” subsection of this chapter.
The potential impact on future events, especially if a task is not completed at a certain time, is also included when prioritizing nursing interventions. For example, if a patient is scheduled to undergo a surgical procedure later in the day, the nurse prioritizes initiating a NPO (nothing by mouth) prescription prior to completing pre-op patient education about the procedure. The rationale for this decision is that if the patient ate food or drank water, the surgery time would be delayed. Knowing and understanding the patient’s purpose for care, current situation, and expected outcomes are necessary to accurately prioritize interventions.
Patient Safety
It is essential to consider patient safety when implementing interventions. At times, patients may experience a change in condition that makes a planned nursing intervention or provider prescription no longer safe to implement. For example, an established nursing care plan for a patient states, “The nurse will ambulate the patient 100 feet three times daily.” However, during assessment this morning, the patient reports feeling dizzy today, and their blood pressure is 90/60. Using critical thinking and clinical judgment, the nurse decides to not implement the planned intervention of ambulating the patient. This decision and supporting assessment findings should be documented in the patient’s chart and also communicated during the shift handoff report, along with appropriate notification of the provider of the patient’s change in condition.
Implementing interventions goes far beyond implementing provider prescriptions and completing tasks identified on the nursing care plan and must focus on patient safety. As front-line providers, nurses are in the position to stop errors before they reach the patient. [ 2 ]
In 2000 the Institute of Medicine (IOM) issued a groundbreaking report titled To Err Is Human: Building a Safer Health System . The report stated that as many as 98,000 people die in U.S. hospitals each year as a result of preventable medical errors. To Err Is Human broke the silence that previously surrounded the consequences of medical errors and set a national agenda for reducing medical errors and improving patient safety through the design of a safer health system. [ 3 ] In 2007 the IOM published a follow-up report titled Preventing Medication Errors and reported that more than 1.5 million Americans are injured every year in American hospitals, and the average hospitalized patient experiences at least one medication error each day. This report emphasized actions that health care systems could take to improve medication safety. [ 4 ]
Read additional information about specific actions that nurses can take to prevent medication errors; go to the “Preventing Medication Errors” section of the “ Legal/Ethical” chapter of the Open RN Nursing Pharmacology textbook.
In an article released by the Robert Wood Johnson Foundation, errors involving nurses that endanger patient safety cover broad territory. This territory spans “wrong site, wrong patient, wrong procedure” errors, medication mistakes, failures to follow procedures that prevent central line bloodstream and other infections, errors that allow unsupervised patients to fall, and more. Some errors can be traced to shifts that are too long that leave nurses fatigued, some result from flawed systems that do not allow for adequate safety checks, and others are caused by interruptions to nurses while they are trying to administer medications or provide other care. [ 5 ]
The Quality and Safety Education for Nurses (QSEN) project began in 2005 to assist in preparing future nurses to continuously improve the quality and safety of the health care systems in which they work. The vision of the QSEN project is to “inspire health care professionals to put quality and safety as core values to guide their work.” [ 6 ] Nurses and nursing students are expected to participate in quality improvement (QI) initiatives by identifying gaps where change is needed and assisting in implementing initiatives to resolve these gaps. Quality improvement is defined as, “The combined and unceasing efforts of everyone – health care professionals, patients and their families, researchers, payers, planners and educators – to make the changes that will lead to better patient outcomes (health), better system performance (care), and better professional development (learning).” [ 7 ]
Delegation of Interventions
While implementing interventions, RNs may elect to delegate nursing tasks. Delegation is defined by the American Nurses Association as, “The assignment of the performance of activities or tasks related to patient care to unlicensed assistive personnel or licensed practical nurses (LPNs) while retaining accountability for the outcome.” [ 8 ] RNs are accountable for determining the appropriateness of the delegated task according to condition of the patient and the circumstance; the communication provided to an appropriately trained LPN or UAP; the level of supervision provided; and the evaluation and documentation of the task completed. The RN must also be aware of the state Nurse Practice Act, federal regulations, and agency policy before delegating. The RN cannot delegate responsibilities requiring clinical judgment. [ 9 ] See the following box for information regarding legal requirements associated with delegation according to the Wisconsin Nurse Practice Act.
Delegation According to the Wisconsin Nurse Practice Act
During the supervision and direction of delegated acts a Registered Nurse shall do all of the following:
Delegate tasks commensurate with educational preparation and demonstrated abilities of the person supervised.
Provide direction and assistance to those supervised.
Observe and monitor the activities of those supervised.
Evaluate the effectiveness of acts performed under supervision. [ 10 ]
The standard of practice for Licensed Practical Nurses in Wisconsin states, “In the performance of acts in basic patient situations, the LPN. shall, under the general supervision of an RN or the direction of a provider:
Accept only patient care assignments which the LPN is competent to perform.
Provide basic nursing care. Basic nursing care is defined as care that can be performed following a defined nursing procedure with minimal modification in which the responses of the patient to the nursing care are predictable.
Record nursing care given and report to the appropriate person changes in the condition of a patient.
Consult with a provider in cases where an LPN knows or should know a delegated act may harm a patient.
Perform the following other acts when applicable:
Assist with the collection of data.
Assist with the development and revision of a nursing care plan.
Reinforce the teaching provided by an RN provider and provide basic health care instruction.
Participate with other health team members in meeting basic patient needs.” [ 11 ]
Read additional details about the scope of practice of registered nurses (RNs) and licensed practical nurses (LPNs) in Wisconsin’s Nurse Practice Act in Chapter N 6 Standards of Practice .
Read more about the American Nurses Association’s Principles of Delegation.
Table 4.7 outlines general guidelines for delegating nursing tasks in the state of Wisconsin according to the role of the health care team member.
General Guidelines for Delegating Nursing Tasks
Documentation of Interventions
As interventions are performed, they must be documented in the patient’s record in a timely manner. As previously discussed in the “Ethical and Legal Issues” subsection of the “ Basic Concepts ” section, lack of documentation is considered a failure to communicate and a basis for legal action. A basic rule of thumb is if an intervention is not documented, it is considered not done in a court of law. It is also important to document administration of medication and other interventions in a timely manner to prevent errors that can occur due to delayed documentation time.
Coordination of Care and Health Teaching/Health Promotion
ANA’s Standard of Professional Practice for Implementation also includes the standards 5A Coordination of Care and 5B Health Teaching and Health Promotion . [ 12 ] Coordination of Care includes competencies such as organizing the components of the plan, engaging the patient in self-care to achieve goals, and advocating for the delivery of dignified and holistic care by the interprofessional team. Health Teaching and Health Promotion is defined as, “Employing strategies to teach and promote health and wellness.” [ 13 ] Patient education is an important component of nursing care and should be included during every patient encounter. For example, patient education may include teaching about side effects while administering medications or teaching patients how to self-manage their conditions at home.
Refer to Scenario C in the “Assessment” section of this chapter. The nurse implemented the nursing care plan documented in Appendix C. Interventions related to breathing were prioritized. Administration of the diuretic medication was completed first, and lung sounds were monitored frequently for the remainder of the shift. Weighing the patient before breakfast was delegated to the CNA. The patient was educated about her medications and methods to use to reduce peripheral edema at home. All interventions were documented in the electronic medical record (EMR).
4.8. EVALUATION
Evaluation is the sixth step of the nursing process (and the sixth Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.” [ 1 ] Both the patient status and the effectiveness of the nursing care must be continuously evaluated and the care plan modified as needed. [ 2 ]
Evaluation focuses on the effectiveness of the nursing interventions by reviewing the expected outcomes to determine if they were met by the time frames indicated. During the evaluation phase, nurses use critical thinking to analyze reassessment data and determine if a patient’s expected outcomes have been met, partially met, or not met by the time frames established. If outcomes are not met or only partially met by the time frame indicated, the care plan should be revised. Reassessment should occur every time the nurse interacts with a patient, discusses the care plan with others on the interprofessional team, or reviews updated laboratory or diagnostic test results. Nursing care plans should be updated as higher priority goals emerge. The results of the evaluation must be documented in the patient’s medical record.
Ideally, when the planned interventions are implemented, the patient will respond positively and the expected outcomes are achieved. However, when interventions do not assist in progressing the patient toward the expected outcomes, the nursing care plan must be revised to more effectively address the needs of the patient. These questions can be used as a guide when revising the nursing care plan:
- Did anything unanticipated occur?
- Has the patient’s condition changed?
- Were the expected outcomes and their time frames realistic?
- Are the nursing diagnoses accurate for this patient at this time?
- Are the planned interventions appropriately focused on supporting outcome attainment?
- What barriers were experienced as interventions were implemented?
- Does ongoing assessment data indicate the need to revise diagnoses, outcome criteria, planned interventions, or implementation strategies?
- Are different interventions required?
Refer to Scenario C in the “Assessment” section of this chapter and Appendix C . The nurse evaluates the patient’s progress toward achieving the expected outcomes.
For the nursing diagnosis Fluid Volume Excess , the nurse evaluated the four expected outcomes to determine if they were met during the time frames indicated:
The patient will report decreased dyspnea within the next 8 hours.
The patient will have clear lung sounds within the next 24 hours.
The patient will have decreased edema within the next 24 hours.
The patient’s weight will return to baseline by discharge.
Evaluation of the patient condition on Day 1 included the following data: “ The patient reported decreased shortness of breath, and there were no longer crackles in the lower bases of the lungs. Weight decreased by 1 kg, but 2+ edema continued in ankles and calves .” Based on this data, the nurse evaluated the expected outcomes as “ Partially Met ” and revised the care plan with two new interventions:
Request prescription for TED hose from provider.
Elevate patient’s legs when sitting in chair.
For the second nursing diagnosis, Risk for Falls , the nurse evaluated the outcome criteria as “ Met ” based on the evaluation, “ The patient verbalizes understanding and is appropriately calling for assistance when getting out of bed. No falls have occurred. ”
The nurse will continue to reassess the patient’s progress according to the care plan during hospitalization and make revisions to the care plan as needed. Evaluation of the care plan is documented in the patient’s medical record.
4.9. SUMMARY OF THE NURSING PROCESS
You have now learned how to perform each step of the nursing process according to the ANA Standards of Professional Nursing Practice. Critical thinking, clinical reasoning, and clinical judgment are used when assessing the patient, creating a nursing care plan, and implementing interventions. Frequent reassessment, with revisions to the care plan as needed, is important to help the patient achieve expected outcomes. Throughout the entire nursing process, the patient always remains the cornerstone of nursing care. Providing individualized, patient-centered care and evaluating whether that care has been successful in achieving patient outcomes are essential for providing safe, professional nursing practice.
Video Review of Creating a Sample Care Plan [ 1 ]
4.10. LEARNING ACTIVITIES
Learning activities.
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Instructions: Apply what you’ve learned in this chapter by creating a nursing care plan using the following scenario. Use the template in Appendix B as a guide.
The client, Mark S., is a 57-year-old male who was admitted to the hospital with “severe” abdominal pain that was unable to be managed in the Emergency Department. The physician has informed Mark that he will need to undergo some diagnostic tests. The tests are scheduled for the morning.
After receiving the news about his condition and the need for diagnostic tests, Mark begins to pace the floor. He continues to pace constantly. He keeps asking the nurse the same question (“How long will the tests take?”) about his tests over and over again. The patient also remarked, “I’m so uptight I will never be able to sleep tonight.” The nurse observes that the client avoids eye contact during their interactions and that he continually fidgets with the call light. His eyes keep darting around the room. He appears tense and has a strained expression on his face. He states, “My mouth is so dry.” The nurse observes his vital signs to be: T 98, P 104, R 30, BP 180/96. The nurse notes that his skin feels sweaty (diaphoretic) and cool to the touch.
Critical Thinking Activity:
Group (cluster) the subjective and objective data.
Create a problem-focused nursing diagnosis (hypothesis).
Develop a broad goal and then identify an expected outcome in “SMART” format.
Outline three interventions for the nursing diagnosis to meet the goal. Cite an evidence-based source.
Imagine that you implemented the interventions that you identified. Evaluate the degree to which the expected outcome was achieved: Met – Partially Met – Not Met.

- IV GLOSSARY
The act or process of pleading for, supporting, or recommending a cause or course of action. [ 1 ]
Unconditionally acceptance of the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care. [ 2 ]
Groups of people who share a characteristic that causes each member to be susceptible to a particular human response, such as demographics, health/family history, stages of growth/development, or exposure to certain events/experiences. [ 3 ]
Medical diagnoses, injuries, procedures, medical devices, or pharmacological agents. These conditions are not independently modifiable by the nurse, but support accuracy in nursing diagnosis. [ 4 ]
Care that can be performed following a defined nursing procedure with minimal modification in which the responses of the patient to the nursing care are predictable. [ 5 ]
A relationship described as one in which the whole person is assessed while balancing the vulnerability and dignity of the patient and family. [ 6 ]
Individual, family, or group, which includes significant others and populations. [ 7 ]
The observed outcome of critical thinking and decision-making. It is an iterative process that uses nursing knowledge to observe and access presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care. [ 8 ]
A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions. [ 9 ]
Grouping data into similar domains or patterns.
Nursing interventions that require cooperation among health care professionals and unlicensed assistive personnel (UAP).
While implementing interventions during the nursing process, includes components such as organizing the components of the plan with input from the health care consumer, engaging the patient in self-care to achieve goals, and advocating for the delivery of dignified and person-centered care by the interprofessional team. [ 10 ]
Reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow. [ 11 ]
Subjective or objective data that gives the nurse a hint or indication of a potential problem, process, or disorder.
“Top-down thinking” or moving from the general to the specific. Deductive reasoning relies on a general statement or hypothesis—sometimes called a premise or standard—that is held to be true. The premise is used to reach a specific, logical conclusion.
Observable cues/inferences that cluster as manifestations of a problem-focused, health-promotion diagnosis, or syndrome. This does not only imply those things that the nurse can see, but also things that are seen, heard (e.g., the patient/family tells us), touched, or smelled. [ 12 ]
The assignment of the performance of activities or tasks related to patient care to unlicensed assistive personnel while retaining accountability for the outcome. [ 13 ]
Interventions that require a prescription from a physician, advanced practice nurse, or physician’s assistant.
Interventions that are carried out by having personal contact with a patient.
An electronic version of the patient’s medical record.
A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and patient, family, group, community, and population preferences and values. [ 14 ]
Statements of measurable action for the patient within a specific time frame and in response to nursing interventions. “SMART” outcome statements are specific, measurable, action-oriented, realistic, and include a time frame.
An evidence-based assessment framework for identifying patient problems and risks during the assessment phase of the nursing process.
A judgment formed from a set of facts, cues, and observations.
Broad statements of purpose that describe the aim of nursing care.
Employing strategies to teach and promote health and wellness. [ 15 ]
Any intervention that the nurse can provide without obtaining a prescription or consulting anyone else.
Interventions performed by the nurse in a setting other than directly with the patient. An example of indirect care is creating a nursing care plan.
A type of reasoning that involves forming generalizations based on specific incidents.
Interpretations or conclusions based on cues, personal experiences, preferences, or generalizations.
Nurses who have had specific training and passed a licensing exam. The training is generally less than that of a Registered Nurse. The scope of practice of an LPN/LVN is determined by the facility and the state’s Nurse Practice Act.
A disease or illness diagnosed by a physician or advanced health care provider such as a nurse practitioner or physician’s assistant. Medical diagnoses are a result of clustering signs and symptoms to determine what is medically affecting an individual.
Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity. [ 16 ]
Specific documentation of the planning and delivery of nursing care that is required by The Joint Commission.
A systematic approach to patient-centered care with steps including assessment, diagnosis, outcome identification, planning, implementation, and evaluation; otherwise known by the mnemonic “ADOPIE.”
Data that the nurse can see, touch, smell, or hear or is reproducible such as vital signs. Laboratory and diagnostic results are also considered objective data.
A measurable behavior demonstrated by the patient that is responsive to nursing interventions. [ 17 ]
The format of a nursing diagnosis statement that includes:
Problem (P) – statement of the patient problem (i.e., the nursing diagnosis)
Etiology (E) – related factors (etiology) contributing to the cause of the nursing diagnosis
Signs and Symptoms (S) – defining characteristics manifested by the patient of that nursing diagnosis
Orders, interventions, remedies, or treatments ordered or directed by an authorized primary health care provider. [ 18 ]
Information collected from the patient.
Member of the health care team (usually a medical physician, nurse practitioner, etc.) licensed and authorized to formulate prescriptions on behalf of the client. [ 19 ]
The skillful process of deciding which actions to complete first, second, or third for optimal patient outcomes and to improve patient safety.
The “combined and unceasing efforts of everyone — health care professionals, patients and their families, researchers, payers, planners, and educators — to make the changes that will lead to better patient outcomes (health), better system performance (care), and better professional development (learning).” [ 20 ]
Developing a relationship of mutual trust and understanding.
A nurse who has had a designated amount of education and training in nursing and is licensed by a state Board of Nursing.
The underlying cause (etiology) of a nursing diagnosis when creating a PES statement.
Patients have the right to determine what will be done with and to their own person.
Principles and procedures in the discovery of knowledge involving the recognition and formulation of a problem, the collection of data, and the formulation and testing of a hypothesis.
Information collected from sources other than the patient.
Data that the patient or family reports or data that the nurse makes as an inference, conclusion, or assumption, such as “The patient appears anxious.”
Any unlicensed personnel trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated. [ 21 ]
Obtaining Subjective Data in a Care Relationship
Licensed under a Creative Commons Attribution 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/ .
- Cite this Page Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Fundamentals [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021. Chapter 4 Nursing Process.
- PDF version of this title (216M)
In this Page
- NURSING PROCESS INTRODUCTION
- BASIC CONCEPTS
- OUTCOME IDENTIFICATION
- IMPLEMENTATION OF INTERVENTIONS
- SUMMARY OF THE NURSING PROCESS
- LEARNING ACTIVITIES
Other titles in this collection
- Open RN OER Textbooks
Related Items in Bookshelf
- All Textbooks
Bulk Download
- Bulk download content from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Chapter 4 Nursing Process - Nursing Fundamentals Chapter 4 Nursing Process - Nursing Fundamentals
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

How to Write a Policy Analysis Paper : A Nursing/Med Student Guide

Healthcare practice has shifted to evidence-based decision-making, which nurses and other healthcare practitioners can achieve through policy analysis. Therefore, students pursuing health sciences such as nursing, pharmacy, and health sciences and medicine courses must understand the importance of evidence-based policymaking. In doing so, they are often assigned tasks where they critically appraise the policy processes and responses. Unfortunately, most students find completing a health policy document analysis paper, essay or report difficult.
The overarching purpose of a policy analysis paper is to investigate and integrate the knowledge of advanced nursing practice, scholarly research, and healthcare leadership through a critical examination of a policy at the level of clinical practice, social or public health, and healthcare systems policy.
Most policy analysis papers are above 2000 words, meaning their lower limit is 8 or 10 pages, giving you sufficient space to investigate a policy.
Writing a paper of such a scope is arduous and time-consuming. Therefore, we have compiled this ultimate guide to take you through the process and help you discover some tips for success when writing a policy analysis paper for your nursing class. But first, let's get solid on a policy analysis paper.
What is a Policy Analysis Paper?
Research shows that engaging nursing students in health policy prepare them for a holistic practice. So, if you are a medical or nursing student, expect to engage more in writing healthcare policy analysis papers or policy briefs.
Analyzing a policy helps identify the potential policy options that can sustainably, pragmatically, and feasibly address a health issue. It is a process that has evolved from a technical approach to a process that enables sharing of social meaning.
A Policy Analysis paper, sometimes referred to as a strategy paper or policy brief, is a document that entails a critical analysis of a healthcare policy at the level of clinical practice, healthcare systems, and public or social issues.
It entails in-depth research of a healthcare issue from a political perspective (analyzing a bill that touches on a healthcare issue). To better analyze a policy, it is imperative to reflect on the policy process (formulation, adoption, implementation, monitoring and evaluation). You should then consider the policy analysis framework that can be applied to nursing and health policies because they shape your policy critique paper. You can choose the analysis framework from the legal, historical, social, ethical, economic, and cultural contexts.
When analyzing a policy, you need to define the problem or issue of interest, provide background and significance, and include a well-balanced assessment of the options that policymakers can pursue to resolve the issue.
The analysis should also include recommendations for the best course of action for the policymakers.
Now that we know what a policy analysis paper or essay entails, let's focus on how it is done. What steps does one follow when writing a policy analysis paper or doing a policy analysis? We answer these questions comprehensively in the next section.
Steps for Health Policy Analysis - How to Get it Right
P olicy analysis is a systematic and disciplined application where an individual defines a problem, gathers evidence, considers alternatives, selects a criterion, predicts the outcomes, confronts tradeoffs and makes or recommends a decision .
Writing a policy analysis paper is time-consuming, stressful, and demands attention and keenness. In most cases, given the possibility of problems arising when deciding which aspect of a policy to analyze, you must be meticulous.
You must distinguish between analyzing a policy process and a document or content. If it is process analysis, focus on the policy formulation process, and if it is content analysis, base your entire analysis on the composition or substance of the policy.
Our focus in this guide is on the analysis of the policy document or the contents of a policy. Policy analysis generally entails five processes: definition, prediction, prescription, description, and evaluation. It can further be condensed into policy making, cause and consequences, and policy prescription.
Step 1: Identify the Policy Issue
The first thing you need to do when assigned to write a policy paper is to determine the policy issue of interest. For instance, choose a topic that you find interesting to handle.
You can choose to focus on health promotion, mental health problems, stigmatization, drug and substance abuse, the opioid epidemic, adult obesity, road traffic accidents, chronic diseases, use of technology in healthcare, etc. look at the health policy issue from the political, social, cultural, spiritual, national, and economic lenses. To identify a problem, focus on a literature review, environmental scan, and survey the best practices.
The main aim of this step is to contextualize the issue. Look at the issue's broad and impactful and have a rationale for choosing it.
Consider the discrepancy between the status quo and the ideal or planned situation. You can also consider the reasons for the difference and the available solutions.
Defining the health issue or problem is like a typical problem statement and must to accompanied by a citation from credible scholarly sources. The statement should describe the problem and present a diagnosis of the causes of the problem using critical statistics such as mortality rates, live births, morbidity, and other statistics.
You should understand the problem conceptually and empirically for successful policy analysis. Then, with the problem stated, you should select a policy to evaluate the many alternatives and provide a rationale. Let's see how to do that in the next step.
Step 2: Select the Policy document for analysis
After identifying the problem, go ahead and search for the relevant evidence. First, collect data about the policies meant to address the health issue. You can access the relevant healthcare policies through research on government websites and publications. Next, look at the various policy options available to address the problem. Considering different policy options can entail adding a policy action that solves the issue or forgoing a policy alternative. Policy options can be described and determined through their health impact, cost of implementation, and feasibility. You should then rank the options and select the top choice.
When considering alternative policies, your focus should be on the outcomes of the alternative. Consider a feasible, practical, and relevant policy to your healthcare issue.
Step 3: Read the policy document and take notes
After choosing a policy of interest for the analysis, you must extract data further and compile excepts from the policy document. Here is where you apply your preferred evaluation criteria.
The evaluation criteria focus on assessing the suitability of an intervention. You need to have standards to measure the projected outcomes. The criteria will hugely depend on the issue of interest. When evaluating a policy, focus on its relevance, progress, efficiency, effectiveness, and impact on the health problem.
Consider the policy background, including its historical context, available evidence, its implementation, monitoring and evaluation, and strategies for stakeholder engagement. You need to take notes that will come in handy as you write the outline and later when compiling the entire policy analysis paper.
Related reading:
- How to write a great nursing diagnosis.
- Best nursing research, essay, and term paper topics.
- Nursing theories to consider when writing nursing papers.
Step 4: Outline the Policy Analysis Paper
Given that you have defined the problem and are now conversant with the central policy of interest, the alternatives, and your evaluation criteria, it is time to outline your policy analysis report. The outline will depend on the selected framework or model for health policy analysis ( we have discussed choosing a framework/model elsewhere in this comprehensive guide ).
The outline should be based on the appropriate structure of a policy analysis paper. For example, plan what to include in the executive summary or abstract, introduction, problem statement, background information, policy alternatives, recommendations, and conclusion.
The outline is a roadmap that comes in handy as you begin to write the paper at the advanced stages of policy analysis. Remember, the focus is not on the policy but its outcomes. For instance, consider the improved health status of people with obesity after health promotion interventions versus improved knowledge of healthy lifestyle practices. Depending on its feasibility (resources, finance, human capital, etc.), you can then decide on the best policy to pursue.
Step 5: Write the Policy Analysis Paper
Assuming everything is in place, you need to take a break before resuming to write the policy paper.
When writing the paper, begin with the introduction. You can break this into separate sections as long as the underlying motivation of the report comes out clearly. For example, include the historical context and the current status quo of the healthcare problem or issue. Next, explain to your readers why you selected the problem or issue and why you settled on a specific policy option.
The next step is to write the methodology, which entails the evaluation criteria. You should also include a literature review where you contextualize the policy based o existing academic work. Next, explore the policy context or options by describing the current policy and the intervention efforts. Finally, look at case studies and best practice guidelines to get a good rationale for selecting a given policy.
Write down the policy options and recommendations before concluding the paper. Finally, include the reference pages and the appendices. When writing the first draft, focus on researching and writing. You should leave editing and proofreading for the final step.
Step 6: Review, Revise, and Polish the paper
Writing a policy analysis paper is the same task as critiquing a policy. It needs to be done in a professional and academic tone. After writing the sections of the policy paper, your next move is to edit it.
When editing, focus on the flow of information, paragraph structure, sentence structure, formatting, in-text citations, tenses, content, and the choice of words.
You should also proofread your policy analysis paper for grammar, spelling, and punctuation. You can use software such as Grammarly, Ginger, or Hemmingway Editor.
This step aims to convert the first draft into a final one you will submit to your instructor for grading. First, therefore, you must ensure that it Then, you can use the reverse outline method to uncover the inadequacies in your paper.
Check whether all the citations are represented in the reference list. Equally, ensure that the references are consistent with the selected formatting style.
You can read your paper loud so that you can spot the errors. Then, if you need further help, you can hire a proofreader and editor to check whether you omitted something or reduced the number of words but retained the message.
Structure of a Policy Analysis Paper in Nursing
When assigned to write a policy analysis paper, below is a standard structure to adopt. Note that some instructors will have a breakdown of how to do the policy analysis, but we share the standard structure here. Of course, the wording could differ depending on institutions, but these are the major sections or parts of a policy analysis paper or essay.
Contains information about yourself. Include:
- Course name and code
- Coordinator or instructor's name
- Name of your institution (i.e., nursing school or university)
- Date of submission
Abstract/Executive Summary
The abstract is a brief 200-word paragraph that condenses the entire policy analysis paper. It should elaborate on the chosen policy, its strengths and weaknesses, relevance to nursing or healthcare, implications, policy evidence, monitoring and evaluation, stakeholder engagement, the target population, how the policy addresses healthcare's social and ecological determinants, and the areas of improvement. The abstract is never indented and is presented as a whole paragraph. Some instructors will ask for an executive summary instead, a summary of your entire policy document analysis paper.
Introduction
The introduction should begin with an attention grabber or hook statement that not only attracts the readers' attention but also announces the focus or direction of the policy paper. It should also generally define and describe the policy issue of interest. It further entails a few sentences that identify the purpose of the analysis, the targeted policy level (clinical, public/social health, or healthcare systems), the policy's scope, and the topic's significance. Finally, it also identifies the questions the policy intended to address.
Background and Significance
In the background section of a policy paper, you will include the details of the issue or problem. Identify the scope of the problem and present its context, then explore relevant literature that details its history. You should also describe the existing policy that addresses the issue. Expound on the policy you are about to analyze regarding the health issue. You should also examine the enforcement implications. Explore the strengths and weaknesses of the existing policy. It should also identify and describe the major stakeholders (groups or individuals) that are or will be affected by the policies, including the reasons. The background should be supported by evidence from credible scholarly sources. Consider the fiscal impact of the policy or issue, its impact on social justice, and the recommended policy's potential barriers and unintended consequences.
Methods and Analysis
This section of the paper is where you describe the policy analysis plan. First, establish the evaluation criteria to guide your analysis and the policy selection. You can also identify the various policy alternatives to help achieve objectives and evaluate each alternative. Next, demonstrate the potential impact of the policies based on the evaluation criteria. Finally, assess the tradeoffs between the options.
Recommendations
In the recommendations section, you must identify the best policy among the alternatives to address the current problem or issue (the policy scenario). You should follow it by explaining the rationale for selecting it among the alternatives. Next, you should describe the potential strategies that can be used to implement the policy successfully. Also, explore the barriers to the implementation of the selected alternative. Finally, explain the methods to monitor and control (evaluate) the effectiveness of policy implementation.
In this section of the policy analysis paper, you must discuss the analysis and recommendations relative to the policy level and the original questions in your introduction. Further, include the limitations of the analysis and discuss the implications for practice, research, policy formulation, implementation, and education.
The conclusion summarizes the findings and recommendations of the entire analysis. It should also feature the questions addressed in future policy analyses or studies.
This is where you list all the references cited in your policy analysis paper.
The appendices can be a table displaying the results of your analysis. You can include the list of policy alternatives you considered, the criteria you use, and the degree to which each alternative meets the criteria. You can also include illustrations such as graphs, tables, images, charts, etc. be sure to cite them appropriately in either ASA, AMA, APA, or Harvard referencing formats if they are sourced from other sources.
Format of a Policy Analysis Paper in Nursing
You must follow academic and professional writing conventions in nursing and most healthcare sciences. Below are some formatting requirements you need to achieve for this assignment:
- Writing Style: Ensure that you use person-centered terminology in your analysis document. Write complete sentences and support your writing with appropriate references. Use the correct in-text citation format and limit the use of quotes. You should never include direct quotes unless asked to, so stick to the parenthetical citation.
- Paper Size: You should write or type the paper on standard A4 (210 x 297mm) paper.
- Margins. Set the margins to 1 inch or 2.0 cm around the document.
- Font. Use at least 12 points and Times New Roman or Arial.
- Line Spacing. 0 or double spacing, 1.5-line spacing, or single-spacing (1.0)
- Do not include any graphics in the body, such as pictures, graphs, and diagrams. Those should go to the appendix and should only be relevant if specified by your instructor.
- Tabulated information can be included if contained within the world limits provided by your instructor. Format, cite, and reference the tables appropriately.
- Title Page. Include your credentials, such as student name and number, instructor's name, course name and code, and institution.
- Header. Should include the relevant information as per the citation and formatting style chosen. Most instructors will prefer that it consists of the page number.
- Footer. You should include your name, student number, and page number. But this depends on your instructor or course coordinator's preferences.
Use APA, Harvard, AMA, or ASA writing format for your policy analysis paper. In most cases, health sciences and nursing use APA, Harvard, and AMA. If unsure, ask your instructor for clarification.
How to Select a Policy Analysis Framework
A policy analysis framework informs the entire policy analysis paper. Therefore, you must select a plausible policy analysis framework after determining and defining the policy. A good policy analysis paper provides in-depth, reasoned, relevant, and evaluative information about a policy in the context of a health issue or problem.
The role of the framework is to guide the evaluation process. It provides the structure of the paper, allowing you to explore a policy issue logically. When selecting a framework, consider the assignment instructions and the policy focus you will analyze. It will depend on whether the policy is prescriptive or predictive.
Nursing practice and the consumers of healthcare have a social contract. Nurses should evaluate what is best for the consumers and promote/advocate for their best interests. Engaging in the policy process helps nurses influence healthcare, solve health issues, and promote social justice. One way to develop policy acumen is through using policy analysis frameworks to analyze policies.
In broad form, the policy analysis framework includes the stages of analyzing a policy. It could be done in many stages or a few steps. One of the most popular policy analysis models or frameworks advocates for an analysis process focusing on:
- Defining the problem
- Assembling evidence
- Considering the policy alternatives
- Selecting the evaluation criteria
- Monitoring and evaluation of outcomes
- Confronting tradeoffs
- Decision making
- Dissemination
Considering that health policy analysis is a social and political activity, the best healthcare policy framework to adopt (one that considers the contexts relevant to healthcare) entails:
- Defining the context
- Statement of the problem
- Searching for evidence
- Considering the alternative policy options
- Projecting the outcomes
- Applying the evaluative criteria
- Weighing the outcomes
- Making a decision.
The above framework is similar to CDC's Policy analytical framework ( PDF) . Therefore, you can use the model to analyze and prioritize policy.
You can also consider the data-driven policy-analysis model presented in 2003 by the Agency for Healthcare Research and Quality (AHRQ) to assist in evaluating the impact of health policies. Consult your class resources to select the best policy analysis models or frameworks. Asking for instructor clarification is also highly encouraged to get everything right.
Related Reading: How to write a personal nursing philosophy.
Questions to ask yourself before and when analyzing a health policy
- What is the context of the policy? Is it regulatory, administrative, legislative, ethical, etc.?
- How does the policy work? What's its scope?
- What are the aims and objectives of the policy?
- What is the value of the policy?
- What are the short, medium, and long-term outcomes of the policy?
- What are the unforeseeable negative and positive impacts of the policy?
- Who are the stakeholders? What are their interest and values?
- What are the available resources, capacity, and technical requirements for implementing the policy?
- What time frame is needed to formulate and implement the policy?
- How does the policy address the problem or issue?
- What are the populations of interest? How are they affected? What outcomes will affect them, and how?
- How grave is the health issue of interest?
- How does the policy relate to nursing practice and profession?
- What are the cost and benefits of the policy?
- How do the costs compare to the benefits (consider ROI, cost-to-benefit ratio, costs averted, cost savings, etc.)?
- What is the distribution of the cost?
- What are the timelines for the costs and benefits?
- Can you tell if there are any gaps in the data?
- Is there available local and national empirical data to support the policy?
- A conceptual model of Nursing and health policy
- CDC's Policy Analysis Framework (Website)
- Health Policy Analysis by Wendy L. Thomson (DNP, MPH, PHN) (Demonstrative Video)
- Healthcare Policy, Analysis, and Advocacy: Policy Initiative (Website)
- Is there life after policy streams, advocacy coalitions, and punctuations: Using evolutionary theory to explain policy change?
- Policy Analysis by CDC
- Policy Analysis Examples (Issue Briefs) (Download Samples here)
- Policy Analysis Format
- Policy analysis paper Structure
- Policy analysis: A framework for nurse managers
- Putting policy theory to work: tobacco control in California
- Sample Expert Policy analysis papers (download)
- Theory and Methods in Comparative Policy Analysis Studies: Volume One
- How to write a policy paper (extended version)
Struggling with
Related Articles
Nursing Student's Ultimate Guide to Writing a Nursing Care Plan

Best Topics and Ideas for an Epidemiology Paper

How to Do a Case Conceptualization Plus an Example
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.

IMAGES
VIDEO
COMMENTS
The following steps can help you format a critical analysis: 1) Identify the purpose of the critical analysis. 2) Identify the literature that will be used in the analysis. 3) distill the information from the literature into a clear, concise, and objective statement.
This article examines how students can develop critical analysis skills to write at undergraduate degree level. It highlights some of the common errors when writing at this academic level and provides advice on how to avoid such mistakes. Nursing Standard . 23, 47, 35-40. doi: 10.7748/ns2009.07.23.47.35.c7201. [email protected]. This article ...
Critical appraisal is the assessment of research studies' worth to clinical practice. Critical appraisal—the heart of evidence-based practice—involves four phases: rapid critical appraisal, evaluation, synthesis, and recommendation. This article reviews each phase and provides examples, tips, and caveats to help evidence appraisers ...
Step 2: Select the best fitting intervention in view of client problems, situation and outcomes. The nurse selects the intervention that produces the required outcome (patient independence) and which also is affordable and realisable given the time and expertise available.
Nursing: Analysis, Synthesis, and Response Papers 3 A Process for Responding to the Information Try to suspend judgment until you have read and analyzed each article. That is, let the information inform your opinion rather than the other way around. Try to write the analysis (and synthesis) before writing your response.
The research process for conducting a critical analysis literature review has three phases ; (a) the deconstruction phase in which the individually reviewed studies are broken down into separate discreet data points or variables (e.g., breastfeeding duration, study design, sampling methods); (b) the analysis phase that includes both cross-case ...
thus making critical reading even more daunting. It is imperative in nursing that care has its foundations in sound research and it is essential that all nurses have the ability to critically appraise research to identify what is best practice. This article is a step-by step-approach to critiquing quantitative research to help nurses demystify the
Table 4.2: Critical thinking and critical writing. Critical thinking may involve: Critical writing may involve: Being curious and reflecting carefully on a topic. Having an inquiring mind by being skeptical and examining your own thinking and the thinking of others concerning a topic. Don't just accept an argument or a way of thinking.
Analysis refers to the assessment, or critique, of the literature (p. 274) The critical reflection Callahan (2014) described is simi-lar to the reflexivity required when conducting a qualitative study (Dodgson, 2019). It is not traditional for authors of literature review research to critically reflect on their assump-tions, beliefs or values ...
Abstract. When writing at degree level, nurses need to demonstrate an understanding of evidence by summarising its key elements and comparing and contrasting authors' views. Critical analysis is an important nursing skill in writing and in practice. With the advent of an all-degree profession, understanding how to develop this skill is. crucial.
Critiquing a published healthcare research paper. Research is defined as a 'systematic inquiry using orderly disciplined methods to answer questions or to solve problems' ( Polit and Beck, 2017 :743). Research requires academic discipline coupled with specific research competencies so that an appropriate study is designed and conducted ...
London: CRC Press. Section 1 covers an introduction to critical appraisal. Section 3 covers appraising difference types of papers including qualitative papers and observational studies. View this eBook. Coughlan M and Cronin P (2020) Doing a literature review in nursing, health and social care. 3rd edn.
Title, keywords and the authors. The title of a paper should be clear and give a good idea of the subject area. The title should not normally exceed 15 words 2 and should attract the attention of the reader. 3 The next step is to review the key words. These should provide information on both the ideas or concepts discussed in the paper and the ...
Below are nine organizational and writing tips to help you craft the best possible critical analysis essay. 1. Read Thoroughly and Carefully. You will need to accurately represent an author's point of view and techniques. Be sure you truly understand them before you begin the writing process.
Ensure your essay is double-spaced, with 1-inch margins and a readable 12-point font. Include your name, the date, and any other required information on the title page or header. Writing a critical analysis nursing essay is a multi-step process involving planning, research, and analysis, and writing and revising.
Concept analysis, whether using qualitative methods, critical analysis of the literature, or quantitative methods, must be based on rich and comprehensive TABLE 7. Criteria for Evaluating Rigor of ...
Abstract. The four major methodological approaches to concept analysis (Wilson-derived methods, qualitative methods, critical analysis of the literature, and quantitative methods) are compared. The authors suggest that qualitative methods and methods that critically analyze the literature may be selected according to the level of the maturity ...
When to Write Critical Analysis. You may want to write a critical analysis in the following situations: Academic Assignments: If you are a student, you may be assigned to write a critical analysis as a part of your coursework. This could include analyzing a piece of literature, a historical event, or a scientific paper.
Critical analysis involves the examination of knowledge that underpins practice. Critical action requires nurses to assess their skills and identify potential gaps in need of professional development. Critical reflexivity is personal analysis that involves challenging personal beliefs and assumptions to improve professional and personal practice.
5. Proofread and refine your work. Read through your critical analysis to ensure it sounds as professional as it should. Correct any spelling and grammatical errors and awkward phrasing when you see it. Reading your critical analysis out loud can help you identify more areas for improvement.
Critical Thinking and Clinical Reasoning. Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes "reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow." [1] Using critical thinking means that nurses take extra steps to maintain patient safety ...
Step 5: Write the Policy Analysis Paper. Assuming everything is in place, you need to take a break before resuming to write the policy paper. When writing the paper, begin with the introduction. You can break this into separate sections as long as the underlying motivation of the report comes out clearly.
A critical incident analysis and reflection. The purpose of this essay is to reflect and critically study an incident from a clinical setting whilst using a model of reflection. This will allow me to analyse and make sense of the incident and draw conclusions relating to personal learning outcomes. The significance of critical analysis and ...