Type 2 Diabetes Essay
Introduction.
Diabetes is a health condition that is developed when sugar level in the blood increases above normal levels. The two major types of diabetes are type 1 diabetes and type 2 diabetes. Type 2 diabetes is more prevalent than type 1 diabetes. This essay discusses some of the most frequently asked questions about type 2 diabetes through a sample dialogue between a patient and a doctor.

Patient: What is type 2 Diabetes and how is it developed?
Doctor: Type 2 diabetes can be described as a complication in the metabolic processes characterized by a relative shortage of insulin and high levels of glucose in the blood (Barnett, 2011). It differs from type 1 diabetes where there is a complete deficiency of insulin caused by destruction of pancreatic islet cells.
In addition, type 2 diabetes is more common in adults unlike type 1 diabetes which is prevalent amongst young people. The typical symptoms of type 2 diabetes include: recurrent urination, excessive thirst, and persistent hunger (Wilson &Mehra, 1997).
Type 2 diabetes is caused by a mixture of lifestyle and hereditary factors. Even though some factors, like nutrition and obesity, are under individual control, others like femininity, old age, and genetics are not. Sedentary lifestyle, poor nutrition and stress are the major causes of Type 2 diabetes.
Particularly, excessive consumption of sugar and fats increases the risk of infection. Genetic factors have been linked to this condition. For instance, research indicates that if one identical twin is infected, there is a 90% probability of the other twin getting infected. Nutritional condition of a mother for the period of fetal growth can as well lead to this condition. Inadequate sleep is associated with Type 2 diabetes since it affects the process of metabolism (Hawley & Zierath, 2008).
Patient: How is type 2 Diabetes transmitted?
Doctor: Type 2 diabetes cannot be transmitted from one individual to another, since it is not caused by micro-organisms that can be spread. Instead, it is a health condition where the body is unable to create sufficient insulin to maintain the blood sugar level.
Nevertheless, a child from diabetic parents is likely to develop the complication due to genetic inheritance. According to Hanas & Fox (2007), there are some genes that may result in diabetes. As in 2011, research showed that there are more than thirty-six genes that increase the risk of type 2 diabetes infection.
These genes represent 10 per cent of the entire hereditary component of the complication. For instance, a gene referred to as TCF7L2 allele, increases the probability of diabetes occurrence by 1.5 times. It is the greatest threat amongst the genetic invariants. Children from diabetic parents are, therefore, likely to get infected since genes are transferrable from parents to the offspring.
Patient: How is type 2 Diabetes treated?
Doctor: The first step in the treatment of type 2 diabetes is consumption of healthy diet. This involves avoiding excessive consumption of foods that contain sugar and fats as they are likely to increase the levels of sugar in the blood. In addition, getting involved in physical activity and losing excessive weight are also important.
These management practices are recommended because they lower insulin resistance and improve the body cells’ response to insulin. Eating healthy food and physical activity also lower the level of sugar in the blood. There are also pills and other medications that can be injected when these lifestyle changes do not regulate the blood sugar (Roper, 2006).
Type2 diabetes pills function in different ways. Some pills work by lowering insulin resistance while some raise the level of insulin in the blood or decrease the rate of food digestion. Even though the non-insulin injected medicines for this condition work in complex ways, essentially, they lower the levels of blood glucose after injection.
Insulin injection treatment basically raises the insulin level in the blood. Another treatment for type 2 diabetes is weight loss surgery that is recommended for obese people. This treatment has been proved effective since most of the patients can maintain regular levels of sugar in their blood after surgery (Codario, 2011).
Multiple prescriptions can be applied in controlling the levels of blood sugar. Actually, combination treatment is a popular remedy for Type 2 diabetes. If a single therapy is not sufficient, a health care provider may prescribe two or more different kinds of pills.
For instance, individuals with type 2 diabetes have high fat levels in the blood and high blood pressure. Therefore, doctors can prescribe medicines for treatment of these conditions at the same time. The kind of medication prescribed depends on the health condition of the patient (Ganz, 2005).
Patient: What are the chances of survival?
Doctor: Diabetes is one of the major causes of deaths in the United States each year. Statistics indicates that it contributes to approximately 100,000 deaths every year. In the United States, there are over 20 million reported cases of diabetes, the majority being Type 2 diabetes. Proper remedy including change of lifestyle and medications is known to improve the health condition of a patient. If properly used together, lifestyle changes and medication can increase the chances of survival of a patient by up to 85 per cent (Rosenthal, 2009).
Barnett, H. (2011). Type 2 diabetes. Oxford: Oxford University Press.
Codario, A. (2011). Type 2 diabetes, pre-diabetes, and the metabolic syndrome. Totowa, N.J: Humana Press.
Ganz, M. (2005). Prevention of Type 2 Diabetes . Chichester: John Wiley & Sons.
Hanas, R., & Fox, C. (2007). Type 2 diabetes in adults of all ages. London: Class Health.
Hawley, A., & Zierath, R. (2008). Physical activity and type 2 diabetes: Therapeutic effects and mechanisms of action. Champaign, IL: Human Kinetics.
Roper, R. (2006). Type 2 diabetes: The adrenal gland disease : the cause of type 2 diabetes and a nutrition program that takes control! . Bloomington, IN: AuthorHouse.
Rosenthal, S. (2009). The Canadian type 2 diabetes sourcebook. Mississauga, Ont: J. Wiley & Sons Canada.
Wilson, L., & Mehra, V. (1997). Managing the patient with type II diabetes . Gaithersburg, Md: Aspen Publishers.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2019, February 4). Type 2 Diabetes. https://ivypanda.com/essays/type-2-diabetes-2/
"Type 2 Diabetes." IvyPanda , 4 Feb. 2019, ivypanda.com/essays/type-2-diabetes-2/.
IvyPanda . (2019) 'Type 2 Diabetes'. 4 February.
IvyPanda . 2019. "Type 2 Diabetes." February 4, 2019. https://ivypanda.com/essays/type-2-diabetes-2/.
1. IvyPanda . "Type 2 Diabetes." February 4, 2019. https://ivypanda.com/essays/type-2-diabetes-2/.
Bibliography
IvyPanda . "Type 2 Diabetes." February 4, 2019. https://ivypanda.com/essays/type-2-diabetes-2/.
- Insulin Injection: Drug Properties and Injection Process
- Doctors' Reluctance to Prescribe Birth Control Pills to Early Adolescents
- Endocrine Disorders: The Diabetic
- The Diabetic Plate and Healthy Nutrition
- How to Self-Administer Insulin Injection
- The History of the Pill and Feminism
- Management of Patients With Diabetic Ketoacidosis
- Stontioum-90 in Plasma
- R-insulin: Article Critique
- Diabetic Diet and Food Restrictions
- Type I Diabetes: Pathogenesis and Treatment
- Human Body Organ Systems Disorders: Diabetes
- Informative Speech on Hyperthyroidism
- Are there Occasions in the Delivery of Health Care when Deception is Warranted?
- Xtra Mile: Roles of Medical Directors
- Reference Manager
- Simple TEXT file
People also looked at
Hypothesis and theory article, type 2 diabetes mellitus: a pathophysiologic perspective.

- Department of Medicine, Duke University, Durham, NC, United States
Type 2 Diabetes Mellitus (T2DM) is characterized by chronically elevated blood glucose (hyperglycemia) and elevated blood insulin (hyperinsulinemia). When the blood glucose concentration is 100 milligrams/deciliter the bloodstream of an average adult contains about 5–10 grams of glucose. Carbohydrate-restricted diets have been used effectively to treat obesity and T2DM for over 100 years, and their effectiveness may simply be due to lowering the dietary contribution to glucose and insulin levels, which then leads to improvements in hyperglycemia and hyperinsulinemia. Treatments for T2DM that lead to improvements in glycemic control and reductions in blood insulin levels are sensible based on this pathophysiologic perspective. In this article, a pathophysiological argument for using carbohydrate restriction to treat T2DM will be made.
Introduction
Type 2 Diabetes Mellitus (T2DM) is characterized by a persistently elevated blood glucose, or an elevation of blood glucose after a meal containing carbohydrate ( 1 ) ( Table 1 ). Unlike Type 1 Diabetes which is characterized by a deficiency of insulin, most individuals affected by T2DM have elevated insulin levels (fasting and/or post glucose ingestion), unless there has been beta cell failure ( 2 , 3 ). The term “insulin resistance” (IR) has been used to explain why the glucose levels remain elevated even though there is no deficiency of insulin ( 3 , 4 ). Attempts to determine the etiology of IR have involved detailed examinations of molecular and intracellular pathways, with attribution of cause to fatty acid flux, but the root cause has been elusive to experts ( 5 – 7 ).
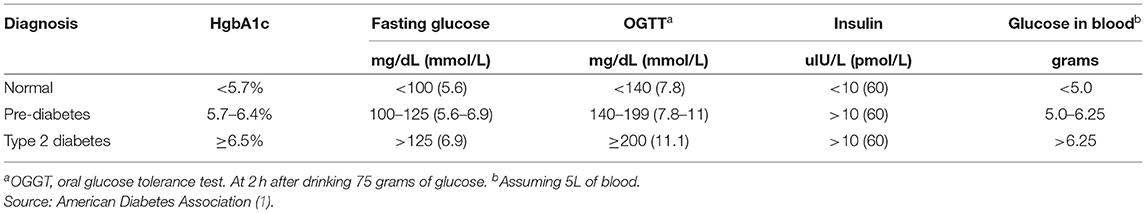
Table 1 . Definition of type 2 diabetes mellitus.
How Much Glucose Is in the Blood?
Keeping in mind that T2DM involves an elevation of blood glucose, it is important to understand how much glucose is in the blood stream to begin with, and then the factors that influence the blood glucose—both exogenous and endogenous factors. The amount of glucose in the bloodstream is carefully controlled—approximately 5–10 grams in the bloodstream at any given moment, depending upon the size of the person. To calculate this, multiply 100 milligrams/deciliter × 1 gram/1,000 milligrams × 10 deciliters/1 liter × 5 liters of blood. The “zeros cancel” and you are left with 5 grams of glucose if the individual has 5 liters of blood. Since red blood cells represent about 40% of the blood volume, and the glucose is in equilibrium, there may be an extra 40% glucose because of the red blood cell reserve ( 8 ). Adding the glucose from the serum and red blood cells totals about 5–10 grams of glucose in the entire bloodstream.
Major Exogenous Factors That Raise the Blood Glucose
Dietary carbohydrate is the major exogenous factor that raises the blood glucose. When one considers that it is common for an American in 2021 to consume 200–300 grams of carbohydrate daily, and most of this carbohydrate is digested and absorbed as glucose, the body absorbs and delivers this glucose via the bloodstream to the cells while attempting to maintain a normal blood glucose level. Thinking of it in this way, if 200–300 grams of carbohydrates is consumed in a day, the bloodstream that holds 5–10 grams of glucose and has a concentration of 100 milligrams/deciliter, is the conduit through which 200,000–300,000 milligrams (200 grams = 200,000 milligrams) passes over the course of a day.
Major Endogenous Factors That Raise the Blood Glucose
There are many endogenous contributors that raise the blood glucose. There are at least 3 different hormones that increase glucose levels: glucagon, epinephrine, and cortisol. These hormones increase glucose levels by increasing glycogenolysis and gluconeogenesis ( 9 ). Without any dietary carbohydrate, the normal human body can generate sufficient glucose though the mechanism of glucagon secretion, gluconeogenesis, glycogen storage and glycogenolysis ( 10 ).
Major Exogenous Factors That Lower the Blood Glucose
A reduction in dietary carbohydrate intake can lower the blood glucose. An increase in activity or exercise usually lowers the blood glucose ( 11 ). There are many different medications, employing many mechanisms to lower the blood glucose. Medications can delay sucrose and starch absorption (alpha-glucosidase inhibitors), slow gastric emptying (GLP-1 agonists, DPP-4 inhibitors) enhance insulin secretion (sulfonylureas, meglitinides, GLP-1 agonists, DPP-4 inhibitors), reduce gluconeogenesis (biguanides), reduce insulin resistance (biguanides, thiazolidinediones), and increase urinary glucose excretion (SGLT-2 inhibitors). The use of medications will also have possible side effects.
Major Endogenous Factors That Lower the Blood Glucose
The major endogenous mechanism to lower the blood glucose is to deliver glucose into the cells (all cells can use glucose). If the blood glucose exceeds about 180 milligrams/deciliter, then loss of glucose into the urine can occur. The blood glucose is reduced by cellular uptake using glut transporters ( 12 ). Some cells have transporters that are responsive to the presence of insulin to activate (glut4), others have transporters that do not require insulin for activation. Insulin-responsive glucose transporters in muscle cells and adipose cells lead to a reduction in glucose levels—especially after carbohydrate-containing meals ( 13 ). Exercise can increase the glucose utilization in muscle, which then increases glucose cellular uptake and reduce the blood glucose levels. During exercise, when the metabolic demands of skeletal muscle can increase more than 100-fold, and during the absorptive period (after a meal), the insulin-responsive glut4 transporters facilitate the rapid entry of glucose into muscle and adipose tissue, thereby preventing large fluctuations in blood glucose levels ( 13 ).
Which Cells Use Glucose?
Glucose can used by all cells. A limited number of cells can only use glucose, and are “glucose-dependent.” It is generally accepted that the glucose-dependent cells include red blood cells, white blood cells, and cells of the renal papilla. Red blood cells have no mitochondria for beta-oxidation, so they are dependent upon glucose and glycolysis. White blood cells require glucose for the respiratory burst when fighting infections. The cells of the inner renal medulla (papilla) are under very low oxygen tension, so therefore must predominantly use glucose and glycolysis. The low oxygen tension is a result of the countercurrent mechanism of urinary concentration ( 14 ). These glucose-dependent cells have glut transporters that do not require insulin for activation—i.e., they do not need insulin to get glucose into the cells. Some cells can use glucose and ketones, but not fatty acids. The central nervous system is believed to be able to use glucose and ketones for fuel ( 15 ). Other cells can use glucose, ketones, and fatty acids for fuel. Muscle, even cardiac muscle, functions well on fatty acids and ketones ( 16 ). Muscle cells have both non-insulin-responsive and insulin-responsive (glut4) transporters ( 12 ).
Possible Dual Role of an Insulin-Dependent Glucose-Transporter (glut4)
A common metaphor is to think of the insulin/glut transporter system as a key/lock mechanism. Common wisdom states that the purpose of insulin-responsive glut4 transporters is to facilitate glucose uptake when blood insulin levels are elevated. But, a lock serves two purposes: to let someone in and/or to keep someone out . So, one of the consequences of the insulin-responsive glut4 transporter is to keep glucose out of the muscle and adipose cells, too, when insulin levels are low. The cells that require glucose (“glucose-dependent”) do not need insulin to facilitate glucose entry into the cell (non-insulin-responsive transporters). In a teleological way, it would “make no sense” for cells that require glucose to have insulin-responsive glut4 transporters. Cells that require glucose have glut1, glut2, glut3, glut5 transporters—none of which are insulin-responsive (Back to the key/lock metaphor, it makes no sense to have a lock on a door that you want people to go through). At basal (low insulin) conditions, most glucose is used by the brain and transported by non-insulin-responsive glut1 and glut3. So, perhaps one of the functions of the insulin-responsive glucose uptake in muscle and adipose to keep glucose OUT of the these cells at basal (low insulin) conditions, so that the glucose supply can be reserved for the tissue that is glucose-dependent (blood cells, renal medulla).
What Causes IR and T2DM?
The current commonly espoused view is that “Type 2 diabetes develops when beta-cells fail to secrete sufficient insulin to keep up with demand, usually in the context of increased insulin resistance.” ( 17 ). Somehow, the beta cells have failed in the face of insulin resistance. But what causes insulin resistance? When including the possibility that the environment may be part of the problem, is it possible that IR is an adaptive (protective) response to excess glucose availability? From the perspective that carbohydrate is not an essential nutrient and the change in foods in recent years has increased the consumption of refined sugar and flour, maybe hyperinsulinemia is the cause of IR and T2DM, as cells protect themselves from excessive glucose and insulin levels.
Insulin Is Already Elevated in IR and T2DM
Clinical experience of most physicians using insulin to treat T2DM over time informs us that an escalation of insulin dose is commonly needed to achieve glycemic control (when carbohydrate is consumed). When more insulin is given to someone with IR, the IR seems to get worse and higher levels of insulin are needed. I have the clinical experience of treating many individuals affected by T2DM and de-prescribing insulin as it is no longer needed after consuming a diet without carbohydrate ( 18 ).
Diets Without Carbohydrate Reverse IR and T2DM
When dietary manipulation was the only therapy for T2DM, before medications were available, a carbohydrate-restricted diet was used to treat T2DM ( 19 – 21 ). Clinical experience of obesity medicine physicians and a growing number of recent studies have demonstrated that carbohydrate-restricted diets reverse IR and T2DM ( 18 , 22 , 23 ). Other methods to achieve caloric restriction also have these effects, like calorie-restricted diets and bariatric surgery ( 24 , 25 ). There may be many mechanisms by which these approaches may work: a reduction in glucose, a reduction in insulin, nutritional ketosis, a reduction in metabolic syndrome, or a reduction in inflammation ( 26 ). Though there may be many possible mechanisms, let's focus on an obvious one: a reduction in blood glucose. Let's assume for a moment that the excessive glucose and insulin leads to hyperinsulinemia and this is the cause of IR. On a carbohydrate-restricted diet, the reduction in blood glucose leads to a reduction in insulin. The reduction in insulin leads to a reduction in insulin resistance. The reduction in insulin leads to lipolysis. The resulting lowering of blood glucose, insulin and body weight reverses IR, T2DM, AND obesity. These clinical observations strongly suggest that hyperinsulinemia is a cause of IR and T2DM—not the other way around.
What Causes Atherosclerosis?
For many years, the metabolic syndrome has been described as a possible cause of atherosclerosis, but there are no RCTs directly targeting metabolic syndrome, and the current drug treatment focuses on LDL reduction, so its importance remains controversial. A recent paper compared the relative importance of many risk factors in the prediction of the first cardiac event in women, and the most powerful predictors were diabetes, metabolic syndrome, smoking, hypertension and BMI ( 27 ). The connection between dietary carbohydrate and fatty liver is well-described ( 28 ). The connection between fatty liver and atherosclerosis is well-described ( 29 ). It is very possible that the transport of excess glucose to the adipose tissue via lipoproteins creates the particles that cause the atherosclerotic damage (small LDL) ( Figure 1 ) ( 30 – 32 ). This entire process of dietary carbohydrate leading to fatty liver, leading to small LDL, is reversed by a diet without carbohydrate ( 26 , 33 , 34 ).
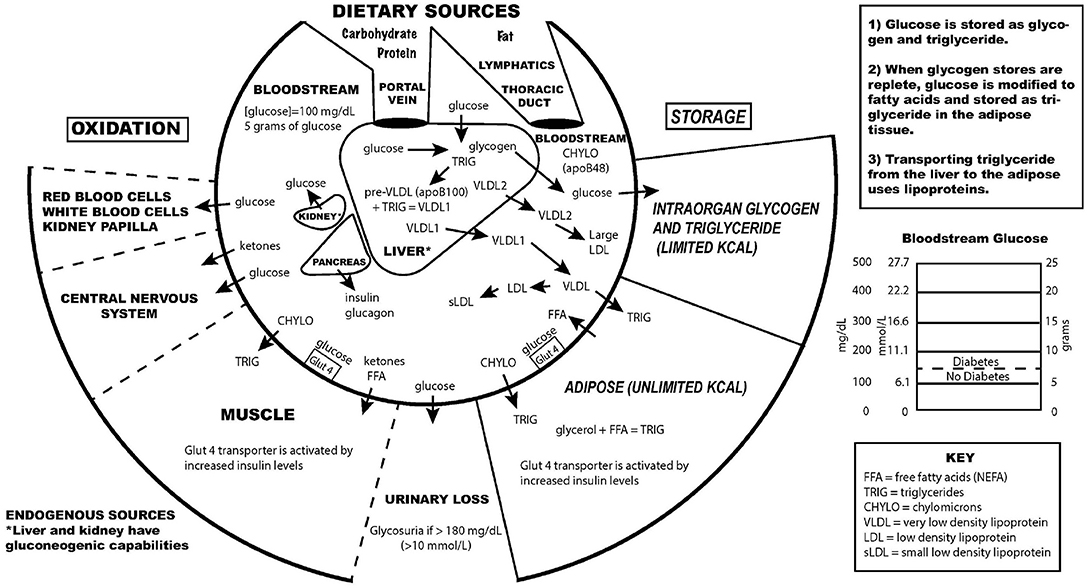
Figure 1 . Key aspects of the interconnection between glucose and lipoprotein metabolism.
Reducing dietary carbohydrate in the context of a low carbohydrate, ketogenic diet reduces hyperglycemia and hyperinsulinemia, IR and T2DM. In the evaluation of an individual for a glucose abnormality, measure the blood glucose and insulin levels. If the insulin level (fasting or after a glucose-containing meal) is high, do not give MORE insulin—instead, use an intervention to lower the insulin levels. Effective ways to reduce insulin resistance include lifestyle, medication, and surgical therapies ( 23 , 35 ).
The search for a single cause of a complex problem is fraught with difficulty and controversy. I am not hypothesizing that excessive dietary carbohydrate is the only cause of IR and T2DM, but that it is a cause, and quite possibly the major cause. How did such a simple explanation get overlooked? I believe it is very possible that the reductionistic search for intracellular molecular mechanisms of IR and T2DM, the emphasis on finding pharmaceutical (rather than lifestyle) treatments, the emphasis on the treatment of high total and LDL cholesterol, and the fear of eating saturated fat may have misguided a generation of researchers and clinicians from the simple answer that dietary carbohydrate, when consumed chronically in amounts that exceeds an individual's ability to metabolize them, is the most common cause of IR, T2DM and perhaps even atherosclerosis.
While there has historically been a concern about the role of saturated fat in the diet as a cause of heart disease, most nutritional experts now cite the lack of evidence implicating dietary saturated fat as the reason for lack of concern of it in the diet ( 36 ).
The concept of comparing medications that treat IR by insulin-sensitizers or by providing insulin itself was tested in the Bari-2D study ( 37 ). Presumably in the context of consuming a standard American diet, this study found no significant difference in death rates or major cardiovascular events between strategies of insulin sensitization or insulin provision.
While lifestyle modification may be ideal to prevent or cure IR and T2DM, for many people these changes are difficult to learn and/or maintain. Future research should be directed toward improving adherence to all effective lifestyle or medication treatments. Future research is also needed to assess the effect of carbohydrate restriction on primary or secondary prevention of outcomes of cardiovascular disease.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of Interest
EW receives royalties from popular diet books and is founder of a company based on low-carbohydrate diet principles (Adapt Your Life, Inc.).
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. American Diabetes Association. Classification and diagnosis of diabetes. Diabetes Care . (2016) 39 (Suppl. 1):S13–22. doi: 10.2337/dc16-S005
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Bogardus C, Lillioja S, Howard BV, Reaven G, Mott D. Relationships between insulin secretion, insulin action, and fasting plasma glucose concentration in nondiabetic and noninsulin-dependent diabetic subjects. J Clin Invest. (1984) 74:1238–46. doi: 10.1172/JCI111533
3. Reaven GM. Compensatory hyperinsulinemia and the development of an atherogenic lipoprotein profile: the price paid to maintain glucose homeostasis in insulin-resistant individuals. Endocrinol Metab Clin North Am. (2005) 34:49–62. doi: 10.1016/j.ecl.2004.12.001
4. DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. (1991) 14:173–94. doi: 10.2337/diacare.14.3.173
5. Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. (2005) 365:1415–28. doi: 10.1016/S0140-6736(05)66378-7
6. Yaribeygi H, Farrokhi FR, Butler AE, Sahebkar A. Insulin resistance: review of the underlying molecular mechanisms. J Cell Physiol. (2019) 234:8152–61. doi: 10.1002/jcp.27603
7. Shulman GI. Cellular mechanisms of insulin resistance. J Clin Invest. (2000) 106:171–6. doi: 10.1172/JCI10583
8. Guizouarn H, Allegrini B. Erythroid glucose transport in health and disease. Pflugers Arch. (2020) 472:1371–83. doi: 10.1007/s00424-020-02406-0
9. Petersen MC, Vatner DF, Shulman GI. Regulation of hepatic glucose metabolism in health and disease. Nat Rev Endocrinol. (2017) 13:572–87. doi: 10.1038/nrendo.2017.80
10. Tondt J, Yancy WS, Westman EC. Application of nutrient essentiality criteria to dietary carbohydrates. Nutr Res Rev. (2020) 33:260–70. doi: 10.1017/S0954422420000050
11. Colberg SR, Hernandez MJ, Shahzad F. Blood glucose responses to type, intensity, duration, and timing of exercise. Diabetes Care. (2013) 36:e177. doi: 10.2337/dc13-0965
12. Mueckler M, Thorens B. The SLC2 (GLUT) family of membrane transporters. Mol Aspects Med. (2013) 34:121–38. doi: 10.1016/j.mam.2012.07.001
13. Bryant NJ, Govers R, James DE. Regulated transport of the glucose transporter GLUT4. Nat Rev Mol Cell Biol. (2002) 3:267–77. doi: 10.1038/nrm782
14. Epstein FH. Oxygen and renal metabolism. Kidney Int. (1997) 51:381–5. doi: 10.1038/ki.1997.50
15. Cahill GF. Fuel metabolism in starvation. Annu Rev Nutr. (2006) 26:1–22. doi: 10.1146/annurev.nutr.26.061505.111258
16. Murashige D, Jang C, Neinast M, Edwards JJ, Cowan A, Hyman MC, et al. Comprehensive quantification of fuel use by the failing and nonfailing human heart. Science. (2020) 370:364–8. doi: 10.1126/science.abc8861
17. Skyler JS, Bakris GL, Bonifacio E, Darsow T, Eckel RH, Groop L, et al. Differentiation of diabetes by pathophysiology, natural history, and prognosis. Diabetes. (2017) 66:241–55. doi: 10.2337/db16-0806
18. Westman EC, Yancy WS, Mavropoulos JC, Marquart M, McDuffie JR. The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutr Metab. (2008) 5:36. doi: 10.1186/1743-7075-5-36
CrossRef Full Text | Google Scholar
19. Allen F. The treatment of diabetes. Boston Med Surg J. (1915) 172:241–7. doi: 10.1056/NEJM191502181720702
20. Osler W, McCrae T. The Principles and Practice of Medicine . 9th ed. New York and London: Appleton & Company (1923).
21. Lennerz BS, Koutnik AP, Azova S, Wolfsdorf JI, Ludwig DS. Carbohydrate restriction for diabetes: rediscovering centuries-old wisdom. J Clin Invest. (2021) 131:e142246. doi: 10.1172/JCI142246
22. Steelman GM, Westman EC. Obesity: Evaluation and Treatment Essentials . 2nd ed. Boca Raton: CRC Press, Taylor & Francis Group (2016). 340 p.
23. Athinarayanan SJ, Adams RN, Hallberg SJ, McKenzie AL, Bhanpuri NH, Campbell WW, et al. Long-term effects of a novel continuous remote care intervention including nutritional ketosis for the management of type 2 diabetes: a 2-year non-randomized clinical trial. Front Endocrinol. (2019) 10:348. doi: 10.3389/fendo.2019.00348
24. Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia. (2011) 54:2506–14. doi: 10.1007/s00125-011-2204-7
25. Isbell JM, Tamboli RA, Hansen EN, Saliba J, Dunn JP, Phillips SE, et al. The importance of caloric restriction in the early improvements in insulin sensitivity after Roux-en-Y gastric bypass surgery. Diabetes Care. (2010) 33:1438–42. doi: 10.2337/dc09-2107
26. Bhanpuri NH, Hallberg SJ, Williams PT, McKenzie AL, Ballard KD, Campbell WW, et al. Cardiovascular disease risk factor responses to a type 2 diabetes care model including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: an open label, non-randomized, controlled study. Cardiovasc Diabetol. (2018) 17:56. doi: 10.1186/s12933-018-0698-8
27. Dugani SB, Moorthy MV, Li C, Demler OV, Alsheikh-Ali AA, Ridker PM, et al. Association of lipid, inflammatory, and metabolic biomarkers with age at onset for incident coronary heart disease in women. JAMA Cardiol. (2021) 6:437–47. doi: 10.1001/jamacardio.2020.7073
28. Duwaerts CC, Maher JJ. Macronutrients and the adipose-liver axis in obesity and fatty liver. Cell Mol Gastroenterol Hepatol. (2019) 7:749–61. doi: 10.1016/j.jcmgh.2019.02.001
29. Zhang L, She Z-G, Li H, Zhang X-J. Non-alcoholic fatty liver disease: a metabolic burden promoting atherosclerosis. Clin Sci Lond Engl. (1979) 134:1775–99. doi: 10.1042/CS20200446
30. Horton TJ, Drougas H, Brachey A, Reed GW, Peters JC, Hill JO. Fat and carbohydrate overfeeding in humans: different effects on energy storage. Am J Clin Nutr. (1995) 62:19–29. doi: 10.1093/ajcn/62.1.19
31. Packard C, Caslake M, Shepherd J. The role of small, dense low density lipoprotein (LDL): a new look. Int J Cardiol. (2000) 74 (Suppl. 1):S17–22. doi: 10.1016/S0167-5273(99)00107-2
32. Borén J, Chapman MJ, Krauss RM, Packard CJ, Bentzon JF, Binder CJ, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: pathophysiological, genetic, and therapeutic insights: a consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. (2020) 41:2313–30. doi: 10.1093/eurheartj/ehz962
33. Yancy WS, Olsen MK, Guyton JR, Bakst RP, Westman EC. A low-carbohydrate, ketogenic diet versus a low-fat diet to treat obesity and hyperlipidemia: a randomized, controlled trial. Ann Intern Med. (2004) 140:769. doi: 10.7326/0003-4819-140-10-200405180-00006
34. Tendler D, Lin S, Yancy WS, Mavropoulos J, Sylvestre P, Rockey DC, et al. The effect of a low-carbohydrate, ketogenic diet on nonalcoholic fatty liver disease: a pilot study. Dig Dis Sci. (2007) 52:589–93. doi: 10.1007/s10620-006-9433-5
35. Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. (1995) 222:339–50. doi: 10.1097/00000658-199509000-00011
36. Astrup A, Magkos F, Bier DM, Brenna JT, de Oliveira Otto MC, Hill JO, et al. Saturated fats and health: a reassessment and proposal for food-based recommendations: JACC state-of-the-art review. J Am Coll Cardiol. (2020) 76:844–57. doi: 10.1016/j.jacc.2020.05.077
37. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med . (2009) 360:2503–15. doi: 10.1056/NEJMoa0805796
Keywords: type 2 diabetes, insulin resistance, pre-diabetes, carbohydrate-restricted diets, hyperinsulinemia, hyperglycemia
Citation: Westman EC (2021) Type 2 Diabetes Mellitus: A Pathophysiologic Perspective. Front. Nutr. 8:707371. doi: 10.3389/fnut.2021.707371
Received: 09 May 2021; Accepted: 20 July 2021; Published: 10 August 2021.
Reviewed by:
Copyright © 2021 Westman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eric C. Westman, ewestman@duke.edu
This article is part of the Research Topic
Carbohydrate-restricted Nutrition and Diabetes Mellitus
Essay on Diabetes for Students and Children
500+ words essay on diabetes.
Diabetes is a very common disease in the world. But people may never realize, how did they get diabetes and what will happen to them and what will they go through. It may not be your problem but you have to show respect and care for the one who has diabetes. It can help them and also benefited you to know more about it and have a better understanding of it. Diabetes is a metabolic disorder which is identified by the high blood sugar level. Increased blood glucose level damages the vital organs as well as other organs of the human’s body causing other potential health ailments.

Types of Diabetes
Diabetes Mellitus can be described in two types:
Description of two types of Diabetes Mellitus are as follows
1) Type 1 Diabetes Mellitus is classified by a deficiency of insulin in the blood. The deficiency is caused by the loss of insulin-producing beta cells in the pancreas. This type of diabetes is found more commonly in children. An abnormally high or low blood sugar level is a characteristic of this type of Diabetes.
Most patients of type 1 diabetes require regular administration of insulin. Type 1 diabetes is also hereditary from your parents. You are most likely to have type 1 diabetes if any of your parents had it. Frequent urination, thirst, weight loss, and constant hunger are common symptoms of this.
2) Type 2 Diabetes Mellitus is characterized by the inefficiency of body tissues to effectively respond to insulin because of this it may be combined by insulin deficiency. Type 2 diabetes mellitus is the most common type of diabetes in people.
People with type 2 diabetes mellitus take medicines to improve the body’s responsiveness to insulin or to reduce the glucose produced by the liver. This type of diabetes mellitus is generally attributed to lifestyle factors like – obesity, low physical activity, irregular and unhealthy diet, excess consumption of sugar in the form of sweets, drinks, etc.
Get the huge list of more than 500 Essay Topics and Ideas
Causes of Diabetes
By the process of digestion, food that we eat is broken down into useful compounds. One of these compounds is glucose, usually referred to as blood sugar. The blood performs the job of carrying glucose to the cells of the body. But mere carrying the glucose to the cells by blood isn’t enough for the cells to absorb glucose.
This is the job of the Insulin hormone. Pancreas supply insulin in the human body. Insulin acts as a bridge for glucose to transit from blood to the body cells. The problem arises when the pancreas fails to produce enough insulin or the body cells for some reason do not receive the glucose. Both the cases result in the excess of glucose in the blood, which is referred to as Diabetes or Diabetes Mellitus.
Symptoms of Diabetes
Most common symptoms of diabetes are fatigue, irritation, stress, tiredness, frequent urination and headache including loss of strength and stamina, weight loss, increase in appetite, etc.
Levels of Diabetes
There are two types of blood sugar levels – fasting blood sugar level and postprandial blood sugar level. The fasting sugar level is the sugar level that we measure after fasting for at least eight hours generally after an overnight fast. Blood sugar level below 100 mg/dL before eating food is considered normal. Postprandial glucose level or PP level is the sugar level which we measure after two hours of eating.
The PP blood sugar level should be below 140 mg/dL, two hours after the meals. Though the maximum limit in both the cases is defined, the permissible levels may vary among individuals. The range of the sugar level varies with people. Different people have different sugar level such as some people may have normal fasting sugar level of 60 mg/dL while some may have a normal value of 90 mg/dL.
Effects of Diabetes
Diabetes causes severe health consequences and it also affects vital body organs. Excessive glucose in blood damages kidneys, blood vessels, skin resulting in various cardiovascular and skin diseases and other ailments. Diabetes damages the kidneys, resulting in the accumulation of impurities in the body.
It also damages the heart’s blood vessels increasing the possibility of a heart attack. Apart from damaging vital organs, diabetes may also cause various skin infections and the infection in other parts of the body. The prime cause of all type of infections is the decreased immunity of body cells due to their inability to absorb glucose.
Diabetes is a serious life-threatening disease and must be constantly monitored and effectively subdued with proper medication and by adapting to a healthy lifestyle. By following a healthy lifestyle, regular checkups, and proper medication we can observe a healthy and long life.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App


- Previous Article
- Next Article

Acknowledgments
Connected content.
In a special series of the ADA Journals' podcast Diabetes Core Update , host Dr. Neil Skolnik interviews special guests and authors of this clinical compendium issue. Listen now at Special Podcast Series: Focus on Diabetes or view the interviews on YouTube at A Practice Guide to Diabetes-Related Eye Care .
Summary and Conclusion
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Thomas W. Gardner; Summary and Conclusion. ADA Clinical Compendia 1 July 2022; 2022 (3): 20. https://doi.org/10.2337/db20223-20
Download citation file:
- Ris (Zotero)
- Reference Manager
Diabetes is a multifactorial disease process, and its long-term management requires the active involvement of people with diabetes and their families, as well as a large multidisciplinary care team to ensure optimal health, quality of life, and productivity. Keeping up with new medications, emerging technology, and evolving treatment recommendations can be challenging, and the language and care processes commonly used by practitioners in one discipline may be less familiar to other diabetes care professionals.
In the realm of diabetes-related eye care, our ability to prevent the progression of diabetes-related retinal disease and thereby preserve vision has never been greater. However, far too many people with diabetes still are not receiving appropriate screening to identify eye disease early and ensure its timely treatment.
It is our hope that this compendium has provided information and guidance to improve communication and encourage collaboration between eye care professionals and other diabetes health care professionals and allow them to more effectively cooperate to reduce barriers to care and improve both the ocular and systemic health of their shared patients.
Editorial and project management services were provided by Debbie Kendall of Kendall Editorial in Richmond, VA.
Dualities of Interest
B.A.C. is a consultant for Genentech and Regeneron. S.A.R. is a speaker for Allergan, Inc., and VSP Vision Care. No other potential conflicts of interest relevant to this compendium were reported.
Author Contributions
All authors researched and wrote their respective sections. Lead author T.W.G. reviewed all content and is the guarantor of this work.
The opinions expressed are those of the authors and do not necessarily reflect those of VSP Vision Care, Regeneron, or the American Diabetes Association. The content was developed by the authors and does not represent the policy or position of the American Diabetes Association, any of its boards or committees, or any of its journals or their editors or editorial boards.
Email alerts
- Online ISSN 2771-6880
- Print ISSN 2771-6872
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Home — Essay Samples — Nursing & Health — Diabetes — The Type 1 and Type 2 Diabetes
The Type 1 and Type 2 Diabetes
- Categories: Diabetes
About this sample

Words: 454 |
Published: Jan 29, 2019
Words: 454 | Page: 1 | 3 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 912 words
6 pages / 2514 words
1 pages / 548 words
2 pages / 909 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Diabetes
Type 2 diabetes is a chronic health condition that affects millions of people worldwide. It is characterized by the body's inability to properly utilize insulin, leading to high blood sugar levels. This essay will explore the [...]
Diabetes is a chronic condition that affects millions of people worldwide, leading to serious health complications if not managed properly. This essay aims to delve into the various aspects of diabetes, including its causes, [...]
Type 2 diabetes, also known as adult-onset diabetes, is a chronic condition that affects the way the body processes blood sugar (glucose). It is a growing concern worldwide, with approximately 463 million adults living with [...]
Gestational diabetes (also referred to as gestational diabetes mellitus, or GDM), is a form of diabetes occurring during pregnancy. The condition usually goes away after the pregnancy. Gestational diabetes is diagnosed when [...]
Diabetes mellitus is a disease of metabolic dysregulation, most notably abnormal glucose metabolism, accompanied by characteristic long-term complications. The complications that are specific to diabetes include retinopathy, [...]
Diabetes is a general term that refers to any of various disorders that are characterized by excessive urination, also known as polyuria. When used alone it refers to Diabetes Mellitus (DM). There are several types of Diabetes, [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Type 2 diabetes.
Rajeev Goyal ; Mayank Singhal ; Ishwarlal Jialal .
Affiliations
Last Update: June 23, 2023 .
- Continuing Education Activity
Diabetes mellitus (DM) is a chronic metabolic disorder characterized by persistent hyperglycemia. It may be due to impaired insulin secretion, resistance to peripheral actions of insulin, or both. Chronic hyperglycemia in synergy with the other metabolic aberrations in patients with diabetes mellitus can cause damage to various organ systems, leading to the development of disabling and life-threatening health complications, most prominent of which are microvascular (retinopathy, nephropathy, and neuropathy) and macrovascular complications leading to a 2-fold to 4-fold increased risk of cardiovascular diseases. This activity reviews the pathophysiology of DM and highlights the role of the interprofessional team in its management.
- Describe the etiologies of diabetes mellitus.
- Review the pathophysiology of diabetes mellitus.
- Summarize the treatment options for diabetes mellitus.
- Review the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by diabetes mellitus type 2.
- Introduction
Diabetes mellitus (DM) is a chronic metabolic disorder characterized by persistent hyperglycemia. It may be due to impaired insulin secretion, resistance to peripheral actions of insulin, or both. According to the International Diabetes Federation (IDF), approximately 415 million adults between the ages of 20 to 79 years had diabetes mellitus in 2015. [1] DM is proving to be a global public health burden as this number is expected to rise to another 200 million by 2040. [1] Chronic hyperglycemia in synergy with the other metabolic aberrations in patients with diabetes mellitus can cause damage to various organ systems, leading to the development of disabling and life-threatening health complications, most prominent of which are microvascular (retinopathy, nephropathy, and neuropathy) and macrovascular complications leading to a 2-fold to 4-fold increased risk of cardiovascular diseases. In this review, we provide an overview of the pathogenesis, diagnosis, clinical presentation, and principles of management of diabetes.
DM is broadly classified into three types by etiology and clinical presentation, type 1 diabetes, type 2 diabetes, and gestational diabetes (GDM). Some other less common types of diabetes include monogenic diabetes and secondary diabetes. [2] [3] [4] [5]
Type 1 Diabetes Mellitus (T1DM)
Type 1 diabetes mellitus (T1DM) accounts for 5% to 10% of DM and is characterized by autoimmune destruction of insulin-producing beta cells in the islets of the pancreas. As a result, there is an absolute deficiency of insulin. A combination of genetic susceptivity and environmental factors such as viral infection, toxins, or some dietary factors have been implicated as triggers for autoimmunity. T1DM is most commonly seen in children and adolescents though it can develop at any age.
Type 2 Diabetes Mellitus
Type 2 diabetes mellitus (T2DM) accounts for around 90% of all cases of diabetes. In T2DM, the response to insulin is diminished, and this is defined as insulin resistance. During this state, insulin is ineffective and is initially countered by an increase in insulin production to maintain glucose homeostasis, but over time, insulin production decreases, resulting in T2DM. T2DM is most commonly seen in persons older than 45 years. Still, it is increasingly seen in children, adolescents, and younger adults due to rising levels of obesity, physical inactivity, and energy-dense diets.
Gestational Diabetes Mellitus
Hyperglycaemia, which is first detected during pregnancy, is classified as gestational diabetes mellitus (GDM), also known as hyperglycemia in pregnancy. Although it can occur anytime during pregnancy, GDM generally affects pregnant women during the second and third trimesters. According to the American Diabetes Association (ADA), GDM complicates 7% of all pregnancies. Women with GDM and their offspring have an increased risk of developing type 2 diabetes mellitus in the future.
GDM can be complicated by hypertension, preeclampsia, and hydramnios and may also lead to increased operative interventions. The fetus can have increased weight and size (macrosomia) or congenital anomalies. Even after birth, such infants may have respiratory distress syndrome and subsequent childhood and adolescent obesity. Older age, obesity, excessive gestational weight gain, history of congenital anomalies in previous children, or stillbirth, or a family history of diabetes are risk factors for GDM.
Monogenic Diabetes
A single genetic mutation in an autosomal dominant gene causes this type of diabetes. Examples of monogenic diabetes include conditions like neonatal diabetes mellitus and maturity-onset diabetes of the young (MODY). Around 1 to 5% of all diabetes cases are due to monogenic diabetes. MODY is a familial disorder and usually presents under the age of 25 years.
Secondary Diabetes
Secondary diabetes is caused due to the complication of other diseases affecting the pancreas (for example, pancreatitis), hormone disturbances (for example, Cushing disease), or drugs (for example, corticosteroids).
- Epidemiology
Diabetes is a worldwide epidemic. With changing lifestyles and increasing obesity, the prevalence of DM has increased worldwide. The global prevalence of DM was 425 million in 2017. According to the International Diabetes Federation (IDF), in 2015, about 10% of the American population had diabetes. Of these, 7 million were undiagnosed. With an increase in age, the prevalence of DM also increases. About 25% of the population above 65 years of age has diabetes. [5]
- Pathophysiology
In T1DM, there is cellular-mediated, autoimmune destruction of pancreatic beta cells. T1DM has a strong genetic predisposition. The major histocompatibility complex (MHC), also known as human leukocyte antigens (HLA), is reported to account for approximately 40 to 50% of the familial aggregation of T1DM. The significant determinants are polymorphisms of class II HLA genes encoding DQ and DR4-DQ8, with DR3-DQ2, found in 90% of T1DM patients.
Another form of T1DM is latent autoimmune diabetes of adults (LADA). It occurs in adulthood, often with a slower course of onset.
The rate of destruction is generally rapid in children and faster in adults. Autoantibodies against islet cells, insulin, glutamic acid decarboxylase-65 (GAD-65), and zinc transporter 8 (Zn T8) may be detected in the serum of such patients. These antibodies wane over time and do not have sufficient diagnostic accuracy to be used routinely for diagnosis, especially after the first year. With the progressive destruction of beta cells, there is little or no secretion of insulin. These patients are generally not obese. They are more prone to develop other autoimmune disorders such as Addison disease, Graves disease, Hashimoto thyroiditis, and celiac disease. A subset of T1DM not associated with insulin autoimmunity and not associated with the above HLA is termed idiopathic T1DM. It is more common in African and Asians and presents with episodic diabetic ketoacidosis (DKA).
T2DM is an insulin-resistance condition with associated beta-cell dysfunction. Initially, there is a compensatory increase in insulin secretion, which maintains glucose levels in the normal range. As the disease progresses, beta cells change, and insulin secretion is unable to maintain glucose homeostasis, producing hyperglycemia. Most of the patients with T2DM are obese or have a higher body fat percentage, distributed predominantly in the abdominal region. This adipose tissue itself promotes insulin resistance through various inflammatory mechanisms, including increased FFA release and adipokine dysregulation. Lack of physical activity, prior GDM in those with hypertension or dyslipidemia also increases the risk of developing T2DM. Evolving data suggest a role for adipokine dysregulation, inflammation, abnormal incretin biology with decreased incretins such as glucagon-like peptide-1 (GLP-I) or incretin resistance, hyperglucagonemia, increased renal glucose reabsorption, and abnormalities in gut microbiota.
- History and Physical
Patients with diabetes mellitus most commonly present with increased thirst, increased urination, lack of energy and fatigue, bacterial and fungal infections, and delayed wound healing. Some patients can also complain of numbness or tingling in their hands or feet or with blurred vision.
These patients can have modest hyperglycemia, which can proceed to severe hyperglycemia or ketoacidosis due to infection or stress. T1DM patients can often present with ketoacidosis (DKA) coma as the first manifestation in about 30% of patients.
The height, weight, and body mass index (BMI) of patients with diabetes mellitus should be recorded. Retinopathy needs to be excluded in such patients by an ophthalmologist. All pulses should be palpated to examine for peripheral arterial disease. Neuropathy should be ruled out by physical examination and history.
Persons older than 40 years of age should be screened annually. More frequent screening is recommended for individuals with additional risk factors for diabetes. [6] [7] [8] [9] [10]
- Certain races/ethnicities (Native American, African American, Hispanics, or Asian American, Pacific Islander),
- Overweight or obese persons with a BMI greater than or equal to 25 kg/m2 or 23 kg/m2 in Asian Americans,
- First-degree relative with diabetes mellitus
- History of cardiovascular disease or hypertension
- Low HDL-cholesterol or hypertriglyceridemia,
- Women with polycystic ovarian syndrome
- Physical inactivity
- Conditions associated with insulin resistance, for example, Acanthosis nigricans.
Women diagnosed with gestational diabetes mellitus (GDM) should have lifelong testing at least every three years. For all other patients, testing should begin at age 45 years, and if results are normal, patients should be tested at a minimum of every 3-years.
The same tests are used to both screen for and diagnose diabetes. These tests also detect individuals with prediabetes.
Diabetes can be diagnosed either by the hemoglobin A1C criteria or plasma glucose concentration (fasting or 2-hour plasma glucose).
Fasting Plasma Glucose (FPG)
A blood sample is taken after an 8 hour overnight fast. As per ADA, fasting plasma glucose (FPG) level of more than 126 mg/dL (7.0 mm/L) is consistent with the diagnosis.
Two-Hour Oral Glucose Tolerance Test (OGTT)
In this test, the plasma glucose level is measured before and 2 hours after the ingestion of 75 gm of glucose. DM is diagnosed if the plasma glucose (PG) level in the 2-hour sample is more than 200 mg/dL (11.1 mmol/L). It is also a standard test but is inconvenient and more costly than FPG and has major variability issues. Patients need to consume a diet with at least 150 g per day of carbohydrates for 3 to 5 days and not take any medications that can impact glucose tolerance, such as steroids and thiazide diuretics.
Glycated Hemoglobin (Hb) A1C
This test gives an average of blood glucose over the last 2 to 3 months. Patients with a Hb A1C greater than 6.5% (48 mmol/mol) are diagnosed as having DM. Hb A1C is a convenient, rapid, standardized test and shows less variation due to pre-analytical variables. It is not much affected by acute illness or stress.
Hb A1C is costly and has many issues, as discussed below, including lower sensitivity. Hb A1C should be measured using the National Glycohemoglobin Standardization Program (NGSP) certified method standardized to Diabetes Control and Complications Trial (DCCT) assay. It is affected by numerous conditions such as sickle cell disease, pregnancy, hemodialysis, blood loss or transfusion, or erythropoietin therapy. It has not been well validated in non-white populations.
Anemia due to deficiency of iron or vitamin B12 leads to spurious elevation of Hb A1C, limiting its use in countries with a high prevalence of anemia. Also, in children and the elderly, the relation between Hb A1C and FPG is suboptimal.
For all of the above tests, if the person is asymptomatic, testing should be repeated later to make a diagnosis of diabetes mellitus.
In patients with classic symptoms of hyperglycemia (increased thirst, increased hunger, increased urination), random plasma glucose more than 200 mg/dL is also sufficient to diagnose DM.
FPG, 2-hour PG during 75-g GTT, and Hb A1C are equally appropriate for the diagnosis of DM. There is no concordance between the results of these tests.
Diagnosis of Gestational Diabetes Mellitus
Pregnant women not previously known to have diabetes should be tested for GDM at 24 to 28 weeks of gestation. ADA and American College of Obstetrics and Gynecology (ACOG) recommend using either a 1-step or 2-step approach for diagnosing GDM.
One-Step Strategy
75 gm OGTT is performed after an overnight fast. Blood samples are collected at fasting for 1 hour and 2 hours. GDM is diagnosed if fasting glucose meet or exceed 92 mg/dl (5.1 mmol/l), 1-hour serum glucose of 180 mg/dl (10.0 mmol/l) or 2-hour serum glucose of 153 mg/dl (8.5 mmol/l).
Two-Step Strategy
- Step one: Perform a 50-gram glucose challenge test irrespective of the last meal. If PG at 1-hour after the load is greater than or equal to 140mg/dl (7.8 mmol/l), proceed to step 2.
- Step 2: 100 g glucose OGTT is performed after overnight fasting. Cut off values are fasting PG 95 or 105 mg/dl (5.5/5.8 mmol/l), 1-hour PG of 180 or 190 mg/dl (10.0/10.6 mmol/l), 2-hour PG of 155 or 165 mg/dl (8.6/9.2 mmol/l) or 3-hour PG of 140 or 145 mg/dl (7.8/8.0 mmol/l). GDM is diagnosed if two or more PG levels equal to or exceed these cutoffs.
- Treatment / Management
For both T1DM and T2DM, the cornerstone of therapy is diet and exercise. [11] [12] [13]
A diet low in saturated fat, refined carbohydrates, high fructose corn syrup, and high in fiber and monounsaturated fats needs to be encouraged. Aerobic exercise for a duration of 90 to 150 minutes per week is also beneficial. The major target in T2DM patients, who are obese, is weight loss.
If adequate glycemia cannot be achieved, metformin is the first-line therapy. Following metformin, many other therapies such as oral sulfonylureas, dipeptidyl peptidase-4 (DPP-4) inhibitors. Glucagon-like peptide-1 (GLP-I) receptor agonists, Sodium-glucose co-transporter-2 (SGLT2) inhibitors, pioglitazone, especially if the patient has fatty liver disease, alpha-glucosidase inhibitors, and insulin, are available. Recent studies have shown that the SGLT2 inhibitor, empagliflozin (EMPA), and the GLP-1 receptor agonist, liraglutide, reduce significant cardiovascular (CV) events and mortality. Hence, in patients with CV disease, these drugs should be considered next. For patients with T1DM, a regime of basal-bolus insulin is the mainstay of therapy. Also, insulin pump therapy is a reasonable choice. Since hypoglycemia portends increased mortality, preference should be given to therapies that do not induce hypoglycemia, for example, DPP-4 Inhibitors, SGLT-2 inhibitors, GLP-I receptor agonists, and pioglitazone with metformin. The other advantages of SGLT-2 inhibitors and GLP-I receptor agonists are a reduction in body weight, blood pressure (BP), and albuminuria.
To reduce microvascular complications in the majority, the goal Hb A1C should be less than 7%. Also, the BP goal should be less than 130/85 mmHg with a preference for angiotensin-converting enzyme (ACE)/angiotensin receptor blocker (ARB) therapy. Fundal exams should be undertaken as proposed by guidelines and urine albumin excretion at least twice a year.
For the lipid panel, the goal should be an LDL-C less than 100 mg/dl if no atherosclerotic cardiovascular disease (ASCVD) or less than 70 mg/dl if ASCVD present. The drug of choice is a statin since these drugs reduce CV events and CV mortality. Consider adding ezetimibe and PCSK9 inhibitors for patients with ASCVD who are not at goal.
Since the different complications and therapies have been detailed in other StatPearls review articles, we have outlined only the principles of therapy. [14] [15]
- Differential Diagnosis
The list of differential diagnosis of diabetes mellitus consists of various conditions that would exhibit similar signs and symptoms: [16] [17]
- Drug-induced signs and symptoms due to corticosteroids, neuroleptics, pentamidine, etc.
- Genetic aberrations in beta-cell function and insulin action
- Metabolic syndrome (syndrome X) [18]
- Endocrinopathies such as acromegaly, Cushing disease, pheochromocytoma, hypothyroidism, etc. [19]
- Complications of iron overload (hemochromatosis)
- Conditions affecting the exocrine part of the pancreas such as pancreatitis, cystic fibrosis, etc. [20]
DM is associated with increased atherosclerotic cardiovascular disease (ASCVD) and treating blood pressure, statin use, regular exercise, and smoking cessation are of great importance in ameliorating risk. The overall excess mortality in those with T2DM is around 15% higher but varies widely. The prevalence of vision-threatening diabetic retinopathy in the United States is about 4.4% among adults with diabetes, while it is 1% for end-stage renal disease. Today, with pharmacotherapy for hyperglycemia, as well as lowering LDL cholesterol and managing blood pressure with ACE/ARB therapy, with other antihypertensive medications and aspirin in secondary prevention, vascular complications can be managed adequately, resulting in a reduction in morbidity and mortality. [21] [22]
- Complications
Persistent hyperglycemia in uncontrolled diabetes mellitus can cause several complications, both acute and chronic. Diabetes mellitus is one of the leading causes of cardiovascular disease (CVD), blindness, kidney failure, and amputation of lower limbs. Acute complications include hypoglycemia, diabetic ketoacidosis, hyperglycemic hyperosmolar state, and hyperglycaemic diabetic coma. Chronic microvascular complications are nephropathy, neuropathy, and retinopathy, whereas chronic macrovascular complications are coronary artery disease (CAD), peripheral artery disease (PAD), and cerebrovascular disease. It is estimated that every year 1.4 to 4.7% of middle-aged people with diabetes have a CVD event. [23] [24]
- Deterrence and Patient Education
Patients must be educated about the importance of blood glucose management to avoid complications associated with DM. Stress must be given on lifestyle management, including diet control and physical exercise. Self-monitoring of blood glucose is an important means for patients to take responsibility for their diabetes management. Regular estimation of glucose, glycated hemoglobin, and lipid levels is necessary.
Healthcare professionals should educate patients about the symptoms of hypoglycemia (such as tachycardia, sweating, confusion) and required action (ingestion of 15 to 20 gm of carbohydrate).
Patients should be motivated to stop smoking. Emphasis is required on regular eye check-ups and foot care.
- Pearls and Other Issues
- T1DM is characterized by the autoimmune destruction of pancreatic beta cells in the majority.
- T2DM is caused due to duel defects in insulin resistance and insulin secretion.
- Gestational diabetes is associated with maternal as well as fetal complications.
- Exercise and a healthy diet are beneficial in both type 1 and type 2 diabetes mellitus.
- Novel therapies, such as GLP-1 receptor agonists and SGLT2 inhibitors, are safer since they do not cause hypoglycemia, are weight neutral or result in weight loss and blood pressure and impact vascular complications favorably.
- Enhancing Healthcare Team Outcomes
The diagnosis and management of type 2 diabetes mellitus are with an interprofessional team. These patients need an appropriate referral to the ophthalmologist, nephrologist, cardiologist, and vascular surgeon. Also, patients need to be educated about lifestyle changes that can help lower blood glucose. All obese patients should be encouraged to lose weight, exercise, and eat a healthy diet. The primary care provider and the diabetic nurse must encourage all people with diabetes to stop smoking and abstain from drinking alcohol. The complications of diabetes mellitus are limb and life-threatening and seriously diminish the quality of life. [25] [26] [27]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Rajeev Goyal declares no relevant financial relationships with ineligible companies.
Disclosure: Mayank Singhal declares no relevant financial relationships with ineligible companies.
Disclosure: Ishwarlal Jialal declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Goyal R, Singhal M, Jialal I. Type 2 Diabetes. [Updated 2023 Jun 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Impact of excluding hyperglycemia from international diabetes federation metabolic syndrome diagnostic criteria on prevalence of the syndrome and its association with microvascular complications, in adult patients with type 1 diabetes. [Endocrine. 2022] Impact of excluding hyperglycemia from international diabetes federation metabolic syndrome diagnostic criteria on prevalence of the syndrome and its association with microvascular complications, in adult patients with type 1 diabetes. Lecumberri E, Nattero-Chávez L, Quiñones Silva J, Alonso Díaz S, Fernández-Durán E, Dorado Avendaño B, Escobar-Morreale HF, Luque-Ramírez M. Endocrine. 2022 Jun; 76(3):601-611. Epub 2022 Mar 28.
- Report of the Committee on the classification and diagnostic criteria of diabetes mellitus. [Diabetes Res Clin Pract. 2002] Report of the Committee on the classification and diagnostic criteria of diabetes mellitus. Kuzuya T, Nakagawa S, Satoh J, Kanazawa Y, Iwamoto Y, Kobayashi M, Nanjo K, Sasaki A, Seino Y, Ito C, et al. Diabetes Res Clin Pract. 2002 Jan; 55(1):65-85.
- Review FreeStyle Libre Flash Glucose Self-Monitoring System: A Single-Technology Assessment [ 2017] Review FreeStyle Libre Flash Glucose Self-Monitoring System: A Single-Technology Assessment Bidonde J, Fagerlund BC, Frønsdal KB, Lund UH, Robberstad B. 2017 Aug 21
- Guidelines on the management and prevention of prediabetes. [Acta Med Indones. 2014] Guidelines on the management and prevention of prediabetes. Indonesian Diabetes Association. Acta Med Indones. 2014 Oct; 46(4):348-59.
- Review How dysregulation of the immune system promotes diabetes mellitus and cardiovascular risk complications. [Front Cardiovasc Med. 2022] Review How dysregulation of the immune system promotes diabetes mellitus and cardiovascular risk complications. Girard D, Vandiedonck C. Front Cardiovasc Med. 2022; 9:991716. Epub 2022 Sep 29.
Recent Activity
- Type 2 Diabetes - StatPearls Type 2 Diabetes - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

ESSAY SAUCE
FOR STUDENTS : ALL THE INGREDIENTS OF A GOOD ESSAY
Essay: Type 2 Diabetes (T2DM)
Essay details and download:.
- Subject area(s): Health essays
- Reading time: 12 minutes
- Price: Free download
- Published: 13 June 2021*
- File format: Text
- Words: 3,323 (approx)
- Number of pages: 14 (approx)
- Tags: Diabetes essays
Text preview of this essay:
This page of the essay has 3,323 words. Download the full version above.
American Diabetes Association (2015) describes “Diabetes as a group of metabolic diseases characterized by hyperglycaemia resulting from defects in insulin secretion, insulin action, or both. Type 2 Diabetes(T2DM), the most prevalent form of the disease is caused by a series of metabolic disorders which results from insulin resistance in muscles and tissues, unrestricted glucose secretion, reduced insulin secretion from the pancreas and or declining beta cell function. which lead to elevated levels of sugar in the blood (Talachai et al 2012). Diabetes of all types can lead to complications in many parts of the body, increasing the overall risk of dying prematurely (Lind 2013). Complications include heart attack, stroke, kidney failure, leg amputation, vision loss and nerve damage. In pregnancy, poorly controlled diabetes increases the risk of fatal death and other complications (Diabetes UK 2015). Both Diabetes UK (2015) and WHO (2016) makes us aware of the substantial economic loss diabetes and its complication can bring to people with diabetes, their families, health systems and national economies through direct medical costs, loss of work and wages. Because of the huge burden of mortality and morbidity attributed to diabetes through micro and macro vascular completion (Lind 2013), people with diabetes require access to systematic, ongoing, and structured care delivered by a team of competent healthcare professionals (NICE 2017).The U.K. prospective diabetes study group UKPDS (1998) had indicated that this was necessary in order to achieve strict glucose control, blood pressure and cholesterol which can reduce the risk of diabetes related complication. Diabetic care in the primary care involves the use of medication, health education, counselling, consistent follow up and periodic referral for specialist services (Long 2011) in accordance with National Institute of Clinical Excellence (NICE) (2017) guidelines for managing diabetes. The initial recommendation is to follow a healthy diet and exercise regime and usually followed with one or more hypoglycaemic agents to prevent micro and macrovascular complication (American Diabetes Association 2015). Despite the benefit of medication, numerous studies have indicated that that recommended glycaemic targets are not achieved by majority of patients. America Diabetic Association (2015) makes us aware that about 50% of patients with type 2 diabetes fail to achieve glycaemic control that is HBA1c less than 7%. As a result, two third of patients die prematurely of cardiovascular diseases (Bailey and Kodack 2011). Edege et al (2016) further believes that the problem is due to poor patient adherence to prescribed medication. Particularly In primary care population. Anecdotal evidence from practice, gathered from HBA1c results suggest that even with the wide range of oral pharmacological available to patients, achieving recommended glycaemic control among adult patients’ groups on oral medication is a challenge. This results in a greater number of patients remaining at risk of long term complication, premature mortality, and increased healthcare cost. It well documented that reasons for non-adherent may be difficult to modify, partly due to factors beyond patient control such as demographic and healthcare structures (Luis Emilio et al 2013). Never the less, Salker (2016) believes if primary care nurses understand the barriers to medicine adherence, they will be able to intervene to increase adherence and improve patient outcome. Pathophysiology of Type 2 Diabetes The characterises hyperglycaemia associated with Type two diabetes is caused by a series of metabolic disorders which results from insulin resistance in muscles and tissues, unrestricted glucose secretion, reduced insulin secretion from the pancreas and or declining beta cell function (Ruso et al 2014) Talachi et al (2012) further explains that, although beta cell disfunction may be partly due to genetics, it can also be caused by inflammation, obesity, insulin resistance, overconsumption of saturated fats and free fatty acid. Beta cell disfunction is characterized by impairment in the first phase of insulin secretion during glucose stimulation followed by the inability of the pancreas to compensate for insulin resistance. This leads to hyperglycemia and the onset of diabetes with symptoms as tiredness, polyphagia, polyuria, polydipsia, blurred vision, slow healing wounds, loss of muscle mass and thrush (Barr, Myslinksi, & Scarborough, 2008). Russo et al (2014) further comments, it is the β-cell dysfunction along with glucotoxicity, lipid toxicity, and other inflammatory agents on pancreatic insulin production all play a contributing role in the development of type 2 diabetes mellitus. Tissue resistance to glucose uptake is also recognized as a major cause of DMT2.Cerf (2013) explains that tissue resistance is linked to elevated levels of pro-inflammatory cytokines which trigger endothelial cell dysfunction leading to vascular abnormalities. These mechanisms may also lead to atherosclerosis and coagulation tendencies which can also be present with DMT2. Although these causes are not linked to diabetes alone, they are found in other chronic diseases such as dyslipidemia and hypertension which are known risk factors of diabetes. (Cerf 2013). Incidence of Type 2 diabetes Global incidence of diabetes is on the rise (World Health Organization (WHO) (2016). Similarly, International Diabetes Federation (IDF) (2015) predict the cases of type 2 diabetes are set to double particularly in US, Australia, and Europe, by 2040 making type 2 diabetes the seventh-biggest cause of death worldwide (Long 2011, WHO 2016). Type 2 diabetes in United Kingdom is estimated to double by 2040, causing 16% of deaths (Diabetes UK 2011, Basu et al 2014, IDF 2015). As the UK’s fifth-biggest cause of death, it accounts for one tenth of NHS expenditure (Paulweber et al 2010, Hex et al 2012, WHO 2016). The incidence of type 2 diabetes in a locality in outer London borough is not an isolated case. Of the 15000 active patients within the health facility 810 do suffer from type 2 diabetics. Type 2 diabetes affect more men than women and affect people from black and south Asian ethnic minority groups (PHE 2011). The increase in T2DM is associated with the increases in obesity, and an increasingly elderly population (PHE 2011) Management of type two diabetes and Quality and outcome framework NICE (2017) guideline NG28 provides evidence-based management system for the management of type 2 diabetes in primary care. This is based on the intervening to promote and support healthy lifestyle, pharmacological control of hyperglycaemia, hypertension, and hyperlipidaemia regular exam for early detection of cardiovascular risk and standard criteria for referral of patients to specialist care The guideline is supported by Quality and Outcomes Framework (QOF) introduced in 2004 and provides financial incentives to general practices for the provision of high-quality care Diabetes UK (2018). Contrary to the limited evidence of improving healthcare quality (PRUComm 2016, NHS 2017), diabetic outcomes and care process under QOF has improved according to National Diabetic Audit Report (2017) Poor Medicine adherence and Glycaemic control The suggestion that people are achieving the recommended target for glycaemic control (NDA 2017) is debatable. Indeed, some practices may be achieving recommended targets according to QOF (NDA 2017), yet poor glycaemic control remains a problem among patient groups (Hendelsman et al 2015). Hendelsman et al (2015) further argue that, the present high morbidity and mortality associated with the disease and its associated high healthcare bill is attributed to poor glycaemic control which is a result of poor medicine adherence among patients ((DiBonaventura et al 2014) Medicine adherence is crucial if the recommended glycaemic control, essential to prevent long term micro and macro vascular complication of the disease is to be achieved (American diabetic association 2013). Aside poor glycaemic control, Poor medicine adherence is also associated with increased healthcare costs (Nasseh et al 2012), and higher morbidity and mortality rates (Currie et al 2012). Improved medication adherence has the potential to reduce healthcare related with care T2DM (Jha et al 2012) and improve patient outcomes (Egede et al 2014.) it is obvious that therefore that improving medicine adherence in patients with T2DM offers real opportunity for improving outcomes as well as reducing health care costs. Numerous studies have evidence non-adherence in patients on one or more to oral hypoglycaemic medications, all with wide variation the in actual occurrences. An extensive study of electronic records on patients on oral hypoglycaemic agents revealed that only 39.6 % of patients filled their prescription after two years although 53% had HBA1C over 7 % (Karter et al 2009). A retrospective analysis of health records of patients who had recently initiated oral diabetic medication showed an overall adherence of 81% (Garzia-Perez et al 2013) Similarly, a recent meta-analysis of 40 studies in which patients taking oral antidiabetic drugs found that medication adherence rates were suboptimal, with only 67.9% of patients showing an overall adherence of about 80% (Iglay et 2105).all studies recognize the scope of the problems and its key contributors. Factors influencing adherence to oral antiglycaemics Studies have been conducted in attempt to identify the factors that influence patients’ adherence to prescribed medication (Houston et al 1997, Ho et al 2006 and Maningat et al 2013). Most of the factors identified. include relationship between patient and healthcare professional, healthcare systems and environment. Hsu et al (2014) explains the factors as lack of education about treatment regimes, lack of support to help patients establish a routine for taking their medicine and poor communication between healthcare professionals as the major barriers to medication adherence. Experience from practice also reveals four major reasons of non-adherence among the patient groups. These include medication side effect, complexity of regime, beliefs about diabetic medication and communication between patients and healthcare professionals These are explored. Medication side effects The first line of treatment in type 2 diabetes are lifestyle modification and metformin Bartolomeo et al (2010). If glycaemic control is not achieved and or is contraindicated, a second drug such as sulphanylureas, meglitinide thiazolidines, alpha-glucosidase inhibitors incretin mimetics and incretin enhancer are used (Bartolomeo et al 2010) However, patients’ knowledge of and or experience of side effects of medication can prevent them from adhering to medication especially when the side effect(s) is/are not communicated to healthcare professionals. Side effect associated with oral medication includes bloating or diarrhoea, weight loss or weight gain, feeling sick and swollen ankles (NHS 2017), erectly dysfunction and hypoglycaemia (Garcia-Pérez et al 2013). For example, the link between obesity and type 2 diabetes is known (Russo et al 2014), so if patients who are overweight or obese are gaining weight because of side effects of medication, and do not report for medication review, they are likely not to adhere to the medication Garcia-Pérez et al (2013) and Skyler et al (2009) evidence this, that obese or severely obese patients and patient who have experience symptoms hypoglycaemia are more likely to have low or moderate low compliance to medication as compared to non-obese individuals. Also, contrary to the assertion that Intensive treatment of hyperglycaemia reduce HBA1C levels and reduce in cardiovascular events (Mannuci et al 2009), Terry et al (2012) makes us aware that, intensive glucose control does not reduce macrovascular diseases in older patients with long standing diabetes but may be associated with increased mortality. Which way, if patients have knowledge or have experience side effects of medication and do not report the side effects for appropriate intervention, they are more likely not to take their medication Perceived complexity and inconvenience Type 2 diabetes mellitus is a chronic complex disease which implies patients will not only have to be on medication for life but also faced the reality of doses and types of medication increasing over time. For example, the progressive nature of the disease may mean that at oral therapies may over time not be effective in achieving the recommended HbA1c levels, and most patients over time are eventually prescribed injectables which further reduce adherence (cook et al 2010) Furthermore, Medication for T2DM and related complication can involve up to 10 tablets per day (Gaede et al 2003).This has a profound influence on adherence It has been observed in practice that non adherence to medication tend to be more prevalent when the number of prescribed doses per day increases and more so where patients indicates the treatment was complex and/or inconvenience .Hauber et al ( 2006 )put this in context; that, the number of prescribed dosed in a day is inversely associated with medication adherence with mean adherence decreasing sharply from 79% on once daily dose to 51% on four times daily dose. Adding to the effect of dose regime, de Vires et al (2014) further Comment that where treatment regime has been viewed as complex, adherence ifs further reduced. Medication beliefs The perceptions of patients’ effectiveness of medication and fear of the long-term risks associated with diabetic medication contributes to non-adherence to medication in patient groups. Mann et al (2009) indicates that when patients hold negative beliefs or hold sceptical beliefs about their prescribed medications, often fearing that the long-term risks outweigh any benefits. They are more likely not to adhere to prescribed medication and this will be indicated in HBAIc results Although the general believe that when patients view medications as necessary, they are more likely to adhere to prescribed medication, it is equally valid too that patients’ concerns about their medications are more strongly linked to adherence than their beliefs in the necessity of those same medications (Foot et al 2016) .Particularly In patients with T2DM,Mann et al (2009) makes us aware that concerns, about the possible negative impact of medications are associated with poor adherence including reluctance to starting new medications Communication between Healthcare Professionals and Patients Communication between patients suffering from type 2 diabetes and their healthcare providers can have a profound impact on adherence. In practice, where a good rapport has been established and patients understand very well their diseases and the need for medication, adherence is good. Likewise, where effective communication has not been established adherence is poor. Tiv et al (2012) evidence this; that good adherence is associated with good relationship between patients and health professionals whiles poor relationship between patient and healthcare professional is observed in patients with poor adherence to medication and glucose monitoring which is associated with higher HBA1C levels Rubin et al (2006) goes further comment that where there is not only a good relationship between patient and healthcare provider but also have a diabetic specialist nurse at the premises, adherence to both medication and lifestyle is improved. Effective communication between patients and healthcare providers resolves patient distress, patients become aware of treatment options and decisions which leads to patients becoming empowered to self-care. this improves adherence and glycaemic control Improving adherence Nurses owe duty of care to their patient in accordance with the requirements of Nurse and Midwifery (NMC) 2015 code. General practice nurses remain crucial in screening, maintaining, and supporting people with diabetes (Royal College of Nursing 2017). This is because it they are privileged to meet patient at least on annual basis and hence best placed to identify incidences on non-adherence and positively influence the patients. General practice nurses provide the crucial supportive role by providing information (Hick 2010) and developing patients knowledge to be able to take ownership of their care process, through this process patients, can overcome barriers and modify their lifestyles to attain a better quality of life, Evidence evaluating the long-term impact of interventions to improve adherence is limited and results from existing studies are inconsistence (Newman et al (2013), however where there is evidence, the suggestion is that interventions to improve adherence may be beneficial (Sapkota et al 2015). Which way, the case for nurse intervention in improving adherence to diabetic medication is firmly held (Farmer et al 2006). Farmer A et al (2012) recommend that interventions targeted at improving adherence in patients with chronic conditions such as Type 2 diabetes could help to reduce the burden of the disease. Although Farmer et al (2006) and Hick (2010) continues to make the case for improving medicine adherence, Gorter et al (2011) makes the case that healthcare professionals including general practice nurse often do not prepare patient well enough to take responsibility of their care. This leads to misunderstanding between the two parties. The lack of effective communication inhibits partnership building and results in limitation of patients sense of ownership in the care process and adhering to medication. There is therefore the need for general practice nurses to build effective partnership with patients diagnosed with type 2 diabetes right form the onset of the care process, to earn patients trust to empower patients to own the treatment process (Garcia-Perez et al 2013). Patient empowerment is a predictor of self-care behaviours and HBAIc (Yang et al 2015). Therefore, intervening to enhance and promote empowerment must be key in diabetic education programs to improve self-behaviour including medicine adherence for glycaemic control. (Yang et al 2015). Yang et al (2015) even challenges the notion of medicine adherence as a dysfunctional concept in diabetes care which must replace by collaboration between patients and healthcare professional. In all, patients will only attain growth and personal maturity if healthcare professional not only tailor relationships but also help them to reflect on their lives and formulate new meaning in their modified lives. The complex nature of T2DM and real possibility of increase in medication types and doses have been noted, (Bartolomeo et al 2013), this requires that patients are armed with coping skills to deal with the complexities of living with T2DM.Here practice nurse can make a difference by early referral for intervention when that challenge has been identified. Garter et al (2010) notes that although patients with higher education may have the capacity to cope with complexities associated with diabetes medication regime, those with lower education may not. Referrals can be made to both commissioned services as well as voluntary services available within the practice locality. It requires adequate knowledge of commissioned services as well as a voluntary service that are available to patients. There is robust evidence that early referral and engagement with diabetic services result in significant decrease in HBA1c levels (Chrvala et al 2016), yet the experience is sometimes some patient may be seen for several times without referral to structured education program or when the referrals have been made, it had not been followed through Also, Patients ability to cope can be adversely affected if they feel thay have little or no imput regarding decision about their care (Dutton et al 2012). The notion of patient centred care is further stressed in diabetes care (Inzucchi et al 2012). Primarily general practice nurse not only promote health but also facilitate the care of individuals within their practice population.it will therefore self-defeating for general practice nurse to accept or even to be inclined to think that they have no contribution to make to help people develop coping strategies and that a patient ability to cope is down to the person individual characteristics. Schulman-Green et al (2012) point out that often healthcare professionals focus on management of illness through improved medication adherence rather than focussing on the emotional aspects of having the diseases and the impact the emotional aspects plays in the patient’s medicine adherence. Obviously, general practice nurses can positively influence adherence when they pay greater attention to patient’s emotions too rather than focusing on the illness alone in efforts to improve adherence. General practice nurses (GPNs) provide knowledge and skill training, facilitate problem solving, motivate for lifestyle adaptation, developing coping skills to achieve goals. Patients including those suffering from T2DM relies on the services of general practice nurses for health and well-being of themselves and family (Madan 2016). General practice nurses, therefore, need to be confident and capable of providing evidence-based information that will instil confidence in patients and carers. This requires a personal commitment to improving practice for better patients’ outcomes thorough ongoing personal and professional development such as attending conferences supervision and regular updates. It is an also worth noting that although GPNs are well placed to be health promotions champion in their communities, let us not forget the challenges they also face which could affect their ability to effect the much-needed changes in patients within their practice community. GPNs are faced with increased patients’ demand, an ageing population, increase in number of people suffering from long term conditions including T2DM, (Cumings 2017) against the backdrop of a shrinking workforce and this is likely to impact on care patients receive. This calls for a need for nurses including customary practices nurses involved in diabetic care to be well supported and recognized. (While 2004) The need to develop and support GPN workforce is widely acknowledged (NHS 2016) Although it may be too early to realize its impact, it has provided an opportunity to develop the much-needed confidence, capability, and capacity to support general practice nurses to effect changes that will ensure that will ensure better outcomes for patients suffering fromT2DM
...(download the rest of the essay above)
Discover more:
- Diabetes essays
Recommended for you
- Existing methodologies and techniques for early diagnosis of diabetes mellitus
- Manage Type 2 Diabetes with Lifestyle Modification: Benefits, Drawbacks and Future
- Is gastric bypass surgery a viable option for weight loss to improve Diabetes Mellitus Type 2?
About this essay:
If you use part of this page in your own work, you need to provide a citation, as follows:
Essay Sauce, Type 2 Diabetes (T2DM) . Available from:<https://www.essaysauce.com/health-essays/type-2-diabetes-t2dm/> [Accessed 08-04-24].
These Health essays have been submitted to us by students in order to help you with your studies.
* This essay may have been previously published on Essay.uk.com at an earlier date.
Essay Categories:
- Accounting essays
- Architecture essays
- Business essays
- Computer science essays
- Criminology essays
- Economics essays
- Education essays
- Engineering essays
- English language essays
- Environmental studies essays
- Essay examples
- Finance essays
- Geography essays
- Health essays
- History essays
- Hospitality and tourism essays
- Human rights essays
- Information technology essays
- International relations
- Leadership essays
- Linguistics essays
- Literature essays
- Management essays
- Marketing essays
- Mathematics essays
- Media essays
- Medicine essays
- Military essays
- Miscellaneous essays
- Music Essays
- Nursing essays
- Philosophy essays
- Photography and arts essays
- Politics essays
- Project management essays
- Psychology essays
- Religious studies and theology essays
- Sample essays
- Science essays
- Social work essays
- Sociology essays
- Sports essays
- Types of essay
- Zoology essays

How do you get diabetes? Causes of Type 1 and Type 2, according to an expert.
D iabetes affects 37 million people in the U.S. The Centers for Disease Control and Prevention estimates another 96 million people – or 1 in 3 adults – have prediabetes , a condition where blood sugar levels are higher than normal but not high enough to be diagnosed with Type 2.
Most people know of Type 1 and Type 2 diabetes, but not all know how their causes differ. We asked Dr. Rodica Busui, the president of Medicine and Science at the American Diabetes Association. Here’s what you need to know.
What causes diabetes?
Start the day smarter. Get all the news you need in your inbox each morning.
Diabetes is a chronic health condition. With Type 1 diabetes, your body can’t produce enough insulin and with Type 2 diabetes, it doesn’t use it properly.
But even beyond the two types, the effects and treatment associated with diabetes are different from person to person. It can also have serious complications if left untreated. This is why educating the public about diabetes is so crucial, says Busui.
“It can affect every single part of one body, and that’s important to understand – it cannot be taken lightly,” Busui says.
How to prevent diabetes: Here are tips to control the condition, according to a doctor
What causes Type 1 diabetes?
Type 1 diabetes is an autoimmune disease where beta cells, a hormone located in the pancreas that creates insulin, are destroyed, Busui says. This destruction may happen quickly or over some time until a “critical mass” of beta cells is lost and the individual cannot survive without insulin from external sources. This is why many Type 1 diabetics undergo regular insulin injections .
“It’s like your own body creates antibodies against your own structures, in this case, the beta cells,” Busui says.
Type 1 diabetes is more commonly diagnosed in children than Type 2. It can occur at any age – Busui says she’s diagnosed patients in their mid-60s with Type 1 and recent data suggests more than half of new Type 1 cases occur in adulthood.
Anyone can get Type 1 diabetes, Busui says. Type 1 symptoms , which include increased thirst and hunger, frequent urination, fatigue, blurry vision, slow-healing cuts and bruises and weight loss, often come on quicker than Type 2 diabetes.
What causes Type 2 diabetes?
Type 2 diabetes is the more common form of diabetes. In Type 2, beta cell dysfunction has multiple, complex causes, including weight gain, lifestyle changes and lack of exercise. Family history, ethnicity and age can also play a role.
These changes cause your body to stop using the insulin it makes properly. This is called insulin resistance – it’s harder for your body to bring blood glucose levels down.
“The more we are insulin resistant … the more insulin is needed to take the same amount of glucose from the blood inside the cell to produce energy,” Busui says. “And because of that, the beta cells have to work overtime constantly, working nonstop. Eventually, they get exhausted and they cannot produce as much insulin.”
This can cause changes in the brain and warp your sense of satiety, or how full you are. Busui says this causes a “vicious cycle,” for those who dealing with obesity and diabetes.
Doctors are diagnosing more children with Type 2 diabetes than ever, an impact of the obesity epidemic in the U.S. and food insecurity, where many children don’t have access to fresh, healthy food. Children can also develop complications from Type 2 diabetes, Busui says.
The Diabetes Dilemma: American can prevent (and control) Type 2 diabetes. So why aren’t we doing it?
Not everyone who has Type 2 diabetes needs insulin from an external source – many Type 2 diabetics’ bodies can still produce insulin. This is why early diagnosis is key and can help patients make lifestyle changes or start on medication to prevent further complications. But because Type 2 diabetes symptoms are much more subtle than Type 1, they may not be taken seriously enough to seek care.
“If people ignore (high blood glucose levels) saying ‘Well, I don’t have a pain, I don’t want to do anything,’ then there is a progressive decrease,” Busui says. “The higher blood glucose then generates some changes in the body metabolism that will lead to all these toxic radicals that actually have an additional effect on the beta cells to make them less and less functional.”
The Diabetes Dilemma: Managing Type 2 diabetes is complicated.
Can eating too much sugar cause diabetes?
Consumption of sugary drinks is associated with a higher risk of Type 2 diabetes , studies show. But there are other risk factors including family history, age and ethnicity. Sugar-sweetened beverages are the largest source of added sugar in American diets.
The American Diabetes Association recommends avoiding sugar-sweetened beverages and switching to water. The Dietary Guidelines for Americans advise no more than 10% of daily caloric intake be from added sugar.
Diabetes is one of the leading causes of death and disability in the country, but Busui says she has a “glass half full” outlook on where diabetes care and research are today. Part of that is providing greater education and access to care, especially for high-risk, historically underserved populations .
“It’s truly remarkable how much progress we have made in discovering effective strategies, medications, technologies,” Busui says.
The Diabetes Dilemma: Solutions exist to end the Type 2 diabetes dilemma but too few get the help they need
Diabetes treatment can be costly: The biggest cost is (surprisingly) not insulin
Just Curious for more? We've got you covered
USA TODAY is exploring the questions you and others ask every day. From "What is the healthiest bread?" to "How to treat dog flu" to "How much do nurses make?" , we're striving to find answers to the most common questions you ask every day. Head to our Just Curious section to see what else we can answer for you.
Read more on diabetes in America
Diabetes runs deep in rural Mississippi: Locals have taken to growing their own solutions.
A diabetes disparity: Why Colorado's healthy lifestyle brand isn't shared by all
The steep cost of Type 2: When diabetes dragged her down, she chose to fight
More: America can prevent (and control) Type 2 diabetes. So why aren’t we doing it?
More: Solutions exist to end the Type 2 diabetes dilemma but too few get the help they need
This article originally appeared on USA TODAY: How do you get diabetes? Causes of Type 1 and Type 2, according to an expert.


IMAGES
VIDEO
COMMENTS
The typical symptoms of type 2 diabetes include: recurrent urination, excessive thirst, and persistent hunger (Wilson &Mehra, 1997). Type 2 diabetes is caused by a mixture of lifestyle and hereditary factors. Even though some factors, like nutrition and obesity, are under individual control, others like femininity, old age, and genetics are not.
Type 2 diabetes (T2D) is a highly dominant and long-lasting metabolic disorder (Mukherjee 439). WHO suspects that by the year of 2025 up to 200-300 million people worldwide will have developed type 2 diabetes (Hussain 318). Approximately half of the risk factor for individuals with type 2 diabetes is due to environmental contact and to genetics ...
Introduction. Insulin resistance and β-cell dysfunction are the 2 major hallmarks of type 2 diabetes mellitus (T2DM) that appear as the result of disturbed homeostasis [].Failure of β-cells (∼80% of their β-cell function) and insulin resistance in muscles and the liver is a vicious triumvirate responsible for the core physiological defects.
Global and regional trends from 1990 to 2017 of type 2 diabetes for all ages were compiled. Forecast estimates were obtained using the SPSS Time Series Modeler. In 2017, approximately 462 million individuals were affected by type 2 diabetes corresponding to 6.28% of the world's population (4.4% of those aged 15-49 years, 15% of those aged ...
The aim of this essay is to explore the psychological implications for a person suffering from type 2 diabetes and others involved in the experience of that illness. Type 2 diabetes, is caused as the result of reduced secretion of insulin and to peripheral resistance to the action of insulin; that is, the insulin in the body does not have its ...
Type 2 diabetes has emerged as a major public health and economic burden of the 21st century. Recent statistics from the Centers for Disease Control and Prevention suggest that diabetes affects 29.1 million people in the United States, 1 and the International Diabetes Federation estimates diabetes effects 366 million people worldwide. 2 As these shocking numbers continue to increase, the cost ...
Type 2 Diabetes Mellitus (T2DM) is characterized by chronically elevated blood glucose (hyperglycemia) and elevated blood insulin (hyperinsulinemia). When the blood glucose concentration is 100 milligrams/deciliter the bloodstream of an average adult contains about 5-10 grams of glucose. Carbohydrate-restricted diets have been used effectively to treat obesity and T2DM for over 100 years ...
Type 2 diabetes is the most common form of the disease. Diabetes mellitus is where the body cells cannot use glucose properly for lack of or resistance to the hormone insulin, which is produced by the pancreas. Diabetes can lead to serious complications over time if left untreated. The high blood sugar levels from uncontrolled diabetes can ...
Diabetes Mellitus can be described in two types: 1) Type 1. 2) Type 2. Description of two types of Diabetes Mellitus are as follows. 1) Type 1 Diabetes Mellitus is classified by a deficiency of insulin in the blood. The deficiency is caused by the loss of insulin-producing beta cells in the pancreas. This type of diabetes is found more commonly ...
A diet high in processed foods, sugar, and saturated fats can lead to weight gain and insulin resistance, increasing the risk of developing diabetes (Hu, 2011). Moreover, sedentary behavior and lack of physical activity are significant risk factors for type 2 diabetes. Regular exercise has been shown to improve insulin sensitivity, reduce blood ...
Analytical Essay : Type 2 Diabetes Mellitus. Diabetes mellitus is a metabolic disease that is characterised by hyperglycaemia. This is a result from a deficiency in insulin action and secretion. Symptoms of hyperglycaemia include polyuria, polydipsia, weight loss, blurred vision and on some occasions, polyphagia.
Two review papers address the complications that are non-traditionally linked to type 2 diabetes, although currently under exhaustive research: bone health and non-alcoholic fatty liver disease [9,10]. The multifaceted nature of type 2 diabetes is clearly visualized owing to the holistic angle used by these approaches.
Diabetes Type Analysis of Type 2 Diabetes Local and National Statistics Compared Incidences and Prevalence According to data seen from 1994 through 1998 at the three university-based diabetes centers in Florida, 92 were classified with Type 2 diabetes. The proportion of patients increased over the five years from 9.4% in 1994 to 20.0% in 1998. From 1994 through 1998, there was a significant ...
Summary and Conclusion. Diabetes is a multifactorial disease process, and its long-term management requires the active involvement of people with diabetes and their families, as well as a large multidisciplinary care team to ensure optimal health, quality of life, and productivity. Keeping up with new medications, emerging technology, and ...
Type 1 diabetes is always treated with insulin. Meal planning also helps with keeping blood sugar at the right levels. Type 1 diabetes also includes latent autoimmune diabetes in adults (LADA), the term used to describe the small number of people with type 2 diabetes who appear to have immune-mediated loss of pancreatic beta cells. Type 2 ...
Type 2 diabetes is the most common form of the disease. Diabetes mellitus is where the body cells cannot use glucose properly for lack of or resistance to the hormone insulin, which is produced by the pancreas. Diabetes can lead to serious complications over time if left untreated. The high blood sugar levels from uncontrolled diabetes can ...
Type 2 Diabetes Mellitus. Type 2 diabetes mellitus (T2DM) accounts for around 90% of all cases of diabetes. In T2DM, the response to insulin is diminished, and this is defined as insulin resistance. During this state, insulin is ineffective and is initially countered by an increase in insulin production to maintain glucose homeostasis, but over ...
Type 2 Diabetes (T2DM), the most prevalent form of the disease is caused by a series of metabolic disorders which results from insulin resistance in muscles and tissues, unrestricted glucose secretion, reduced insulin secretion from the pancreas and or declining beta cell function. which lead to elevated levels of sugar in the blood (Talachai ...
Anyone can get Type 1 diabetes, Busui says. , which include increased thirst and hunger, frequent urination, fatigue, blurry vision, slow-healing cuts and bruises and weight loss, often come on ...