89 Postpartum Depression Essay Topic Ideas & Examples
🏆 best postpartum depression topic ideas & essay examples, 👍 most interesting postpartum depression topics to write about, ⭐ good research topics about postpartum depression, ❓ postpartum depression research questions.
- Activity During Pregnancy and Postpartum Depression Studies have shown that women’s mood and cardiorespiratory fitness improve when they engage in moderate-intensity physical activity in the weeks and months after giving birth to a child.
- Complementary Therapy for Postpartum Depression in Primary Care Thus, the woman faced frustration and sadness, preventing her from taking good care of the child, and the lack of support led to the emergence of concerns similar to those in the past. We will write a custom essay specifically for you by our professional experts 808 writers online Learn More
- Technology to Fight Postpartum Depression in African American Women I would like to introduce the app “Peanut” the social network designed to help and unite women exclusively, as a technology aimed at fighting postpartum depression in African American Women.
- The Postpartum Depression in Afro-Americans Policy The distribution of the funds is managed and administered on the state level. Minnesota and Maryland focused on passing the legislation regulating the adoption of Medicaid in 2013.
- Breastfeeding and Risk of Postpartum Depression The primary goal of the research conducted by Islam et al.was to analyze the correlation between exclusive breastfeeding and the risk of postpartum depression among new mothers.
- Postpartum Depression in African American Women As far as African American women are concerned, the issue becomes even more complex due to several reasons: the stigma associated with the mental health of African American women and the mental health complications that […]
- Postpartum Depression Among the Low-Income U.S. Mothers Mothers who take part in the programs develop skills and knowledge to use the existing social entities to ensure that they protect themselves from the undesirable consequences associated with the PPD and other related psychological […]
- In-Vitro Fertilization and Postpartum Depression The research was conducted through based on professional information sources and statistical data collected from the research study used to further validate the evidence and outcome of this study.
- Postpartum Depression and Its Impact on Infants The goal of this research was “to investigate the prevalence of maternal depressive symptoms at 5 and 9 months postpartum in a low-income and predominantly Hispanic sample, and evaluate the impact on infant weight gain, […]
- Postpartum Depression: Statistics and Methods of Diagnosis The incorporation of the screening tools into the existing electronic medical support system has proved to lead to positive outcomes for both mothers and children.
- Postpartum Psychosis: Impact on Family By the ties of kinship, the extended families of both parents are often intricately involved in the pregnancy and maybe major sources of support for the pregnant woman.
- Postpartum Depression: Treatment and Therapy It outlines the possible treatment and therapy methods, as well as the implications of the condition. A 28-year-old patient presented in the office three weeks after giving birth to her first son with the symptoms […]
- A Review of Postpartum Depression and Continued Post Birth Support In the first chapter – the introduction – the problem statement, background, purpose, and nature of the project are mentioned. The purpose of the project is to explain the significance of managing postpartum depression by […]
- Postpartum Depression: Understanding the Needs of Women This article also emphasizes the need to consider and assess the needs of the mother, infant as well as family members during the treatment of PPD.
- Postpartum Depression and Acute Depressive Symptoms It is hypothesized that the authors of the study wished to establish, with certainty, the effect of the proposed predictors for the development of PPD.
- Postpartum Depression and Its Peculiarities The major peculiarity of PPD in terms of its adverse effects is that it is detrimental to both the mother and the newborn child.
- Supporting the Health Needs of Patients With Parkinson’s, Preeclampsia, and Postpartum Depression The medical history of the patient will help the doctor to offer the best drug therapy. Members of the family might also be unable to cope with the disorder.
- Postpartum Depression and Comorbid Disorders For example, at a public hospital in Sydney, Australia, the psychiatrists used a Routine Comprehensive Psychosocial Assessment tool to study the chances of ‘low risk’ women developing the postpartum symptoms.
- Correlation Between Multiple Pregnancies and Postpartum Depression or Psychosis In recognition of the paucity of information on the relationship between multiple pregnancies and postpartum depression, the paper reviews the likely relationship by understanding the two variables, multiple pregnancies and postpartum depression, in terms of […]
- Acknowledging Postpartum Depression: Years Ago, There Was
- Postpartum Depression and Crime: The Case of Andrea Yates
- Baby Blues, Postpartum Depression, and Postpartum Psychosis
- Postpartum Depression and Parent-Child Relationships
- Cheryl Postpartum Depression Theory Analysis
- Cognitive Therapy for Postpartum Depression
- Postpartum Depression: An Important Issue in Women’s Health
- The Relationships Between Depression and Postpartum Depression
- Postpartum Depression: Causes and Treatments
- How Postpartum Depression Predicts Emotional and Cognitive Difficulties in 11-Year-Olds
- Economic and Health Predictors of National Postpartum Depression Prevalence
- Postpartum Depression (PPD): Symptoms, Causes, and Treatment
- Fathers Dealing With Postpartum Depression
- Postpartum Depression and the Birth of a New Baby
- Risk of Postpartum Depression in Women Without Depression in Pregnancy
- Intimate Partner Violence During Pregnancy and Postpartum Depression in Japan
- Managing Postpartum Depression Through Medications and Therapy
- Early Identification Essential to Treat Postpartum Depression
- Screening for Postpartum Depression and Associated Factors Among Women in China
- Postpartum Depression and Anxiety Disorders in Women
- Postpartum Depression and Child Development
- Association Between Family Members and Risk of Postpartum Depression in Japan
- Postpartum Depression and Its Effects on Mental Health
- Baby Blues, the Challenges of Postpartum Depression
- How Postpartum Depression Affects Employment
- Postpartum Depression During the Postpartum Period
- Evidence-Based Interventions of Postpartum Depression
- Proposed Policy for Postpartum Depression Screening and Treatment
- Sleep Deprivation and Postpartum Depression
- The Causes and Effects of Postpartum Depression
- The Main Facts About Postpartum Depression
- The Postpartum Depression and Crime Relations
- Sleep Quality and Mothers With Postpartum Depression
- Postpartum Depression and Its Effects on Early Brain
- Fetal Gender and Postpartum Depression in a Cohort of Chinese Women
- Postpartum Depression and Postnatal Depression Psychology
- The Problem of Postpartum Depression Among Canadian Women
- Postpartum Depression and Its Effect on the Family Experience
- Mothers With Postpartum Depression for Breastfeeding Success
- Postpartum Depression and Analysis of Treatments and Health Determinants
- How Are Neuroactive Steroids Related to Major Depressive Disorder and Postpartum Depression?
- What Are the Emotional and Behavioral Changes During Postpartum Depression?
- Does Postpartum Depression Affect the Child’s Development?
- When Does Postpartum Depression Lead to Psychosis?
- How to Recognize Postpartum Depression?
- What Is the Role of the Mother, Child, and Partner in Postpartum Depression?
- Is There an Association Between Family Members and the Risk of Postpartum Depression in Japan?
- What Are the Most Common Signs of Postpartum Depression?
- How Does Postpartum Depression Affect Parent-Child Relationships?
- What Type of Therapy Is Most Widely Used for a Person Suffering from Postpartum Depression?
- Can Postpartum Depression Cause Autism?
- What Is a Gender Perspective on Postpartum Depression and the Social Construction of Motherhood?
- How Are Postpartum Depression and Related Factors Screened Among Women in China?
- What Are the Economic and Medical Projections of the Prevalence of Postpartum Depression?
- Is There a Difference Between Postnatal and Postpartum Depression?
- What Is the Biggest Risk Factor for Postpartum Depression?
- How Are Fetal Gender and Postpartum Depression Related in a Cohort of Chinese Women?
- What Factors Contribute to the Development of Postpartum Depression?
- Is Postpartum Depression a Long-Term Disability?
- What Are the Causes and Consequences of Postpartum Depression?
- How Is Postpartum Depression Diagnosed?
- What Is Postpartum Depression and How Does It Affect Newborns and Mothers?
- Is Psychotherapy the Best Treatment for Postpartum Depression?
- What Should Be the Knowledge of Nurses in the Diagnosis of Postpartum Depression?
- How Does Postpartum Depression Affect the Family Experience?
- What Is the Relationship Between Sleep Quality and Postpartum Depression in Mothers?
- Can Postpartum Depression Be Managed with Medication and Therapy?
- What Treatment Options Are Available for People with Postpartum Depression?
- How Long After Childbirth Can Postpartum Depression Occur?
- Are Physical Activity Interventions Effective in the Treatment of Postpartum Depression?
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2023, September 20). 89 Postpartum Depression Essay Topic Ideas & Examples. https://ivypanda.com/essays/topic/postpartum-depression-essay-topics/
"89 Postpartum Depression Essay Topic Ideas & Examples." IvyPanda , 20 Sept. 2023, ivypanda.com/essays/topic/postpartum-depression-essay-topics/.
IvyPanda . (2023) '89 Postpartum Depression Essay Topic Ideas & Examples'. 20 September.
IvyPanda . 2023. "89 Postpartum Depression Essay Topic Ideas & Examples." September 20, 2023. https://ivypanda.com/essays/topic/postpartum-depression-essay-topics/.
1. IvyPanda . "89 Postpartum Depression Essay Topic Ideas & Examples." September 20, 2023. https://ivypanda.com/essays/topic/postpartum-depression-essay-topics/.
Bibliography
IvyPanda . "89 Postpartum Depression Essay Topic Ideas & Examples." September 20, 2023. https://ivypanda.com/essays/topic/postpartum-depression-essay-topics/.
- Parenting Research Topics
- Motherhood Ideas
- Mental Health Essay Ideas
- Stress Titles
- Depression Essay Topics
- Suicide Topics
- Cognitive Therapy Essay Topics
- Mental Disorder Essay Topics
- Abnormal Psychology Paper Topics
- Childhood Essay Topics
- Family Problems Questions
- Cognitive Psychology Topics
- Infant Research Topics
- Gender Stereotypes Essay Titles
- Psychoanalysis Essay Topics

434 Depression Essay Titles & Research Topics: Argumentative, Controversial, and More
Depression is undeniably one of the most prevalent mental health conditions globally, affecting approximately 5% of adults worldwide. It often manifests as intense feelings of hopelessness, sadness, and a loss of interest in previously enjoyable activities. Many also experience physical symptoms like fatigue, sleep disturbances, and appetite changes. Recognizing and addressing this mental disorder is extremely important to save lives and treat the condition.
In this article, we’ll discuss how to write an essay about depression and introduce depression essay topics and research titles for students that may be inspirational.
- 🔝 Top Depression Essay Titles
- ✅ Essay Prompts
- 💡 Research Topics
- 🔎 Essay Titles
- 💭 Speech Topics
- 📝 Essay Structure
🔗 References
🔝 top 12 research titles about depression.
- How is depression treated?
- Depression: Risk factors.
- The symptoms of depression.
- What types of depression exist?
- Depression in young people.
- Differences between anxiety and depression.
- The parents’ role in depression therapy.
- Drugs as the root cause of depression.
- Dangerous consequences of untreated depression.
- Effect of long-term depression.
- Different stages of depression.
- Treatment for depression.
✅ Prompts for Essay about Depression
Struggling to find inspiration for your essay? Look no further! We’ve put together some valuable essay prompts on depression just for you!
Prompt for Personal Essay about Depression
Sharing your own experience with depression in a paper can be a good idea. Others may feel more motivated to overcome their situation after reading your story. You can also share valuable advice by discussing things or methods that have personally helped you deal with the condition.
For example, in your essay about depression, you can:
- Tell about the time you felt anxious, hopeless, or depressed;
- Express your opinion on depression based on the experiences from your life;
- Suggest a way of dealing with the initial symptoms of depression ;
- Share your ideas on how to protect mental health at a young age.
How to Overcome Depression: Essay Prompt
Sadness is a common human emotion, but depression encompasses more than just sadness. As reported by the National Institute of Mental Health, around 21 million adults in the United States, roughly 8.4% of the total adult population , faced at least one significant episode of depression in 2020. When crafting your essay about overcoming depression, consider exploring the following aspects:
- Depression in young people and adolescents;
- The main causes of depression;
- The symptoms of depression;
- Ways to treat depression;
- Help from a psychologist (cognitive behavioral therapy or interpersonal therapy ).
Postpartum Depression: Essay Prompt
The birth of a child often evokes a spectrum of powerful emotions, spanning from exhilaration and happiness to apprehension and unease. It can also trigger the onset of depression. Following childbirth, many new mothers experience postpartum “baby blues,” marked by shifts in mood, bouts of tears, anxiety, and sleep disturbances. To shed light on the subject of postpartum depression, explore the following questions:
- What factors may increase the risk of postpartum depression?
- Is postpartum depression predictable?
- How to prevent postpartum depression?
- What are the symptoms of postpartum depression?
- What kinds of postpartum depression treatments exist?
Prompt for Essay about Teenage Depression
Teenage depression is a mental health condition characterized by sadness and diminishing interest in daily activities. It can significantly impact a teenager’s thoughts, emotions, and behavior, often requiring long-term treatment and support.
By discussing the primary symptoms of teenage depression in your paper, you can raise awareness of the issue and encourage those in need to seek assistance. You can pay attention to the following aspects:
- Emotional changes (feelings of sadness, anger, hopelessness, guilt, etc.);
- Behavioral changes (loss of energy and appetite , less attention to personal hygiene, self-harm, etc.);
- New addictions (drugs, alcohol, computer games, etc.).
💡 Research Topics about Depression
- The role of genetics in depression development.
- The effectiveness of different psychotherapeutic interventions for depression.
- Anti-depression non-pharmacological and medication treatment .
- The impact of childhood trauma on the onset of depression later in life.
- Exploring the efficacy of antidepressant medication in different populations.
- The impact of exercise on depression symptoms and treatment outcomes.
- Mild depression: pharmacotherapy and psychotherapy .
- The relationship between sleep disturbances and depression.
- The role of gut microbiota in depression and potential implications for treatment.
- Investigating the impact of social media on depression rates in adolescents.
- Depression, dementia, and delirium in older people .
- The efficacy of cognitive-behavioral therapy in preventing depression relapse.
- The influence of hormonal changes on depression risk.
- Assessing the effectiveness of self-help and digital interventions for depression.
- Herbal and complementary therapies for depression .
- The relationship between personality traits and vulnerability to depression.
- Investigating the long-term consequences of untreated depression on physical health.
- Exploring the link between chronic pain and depression.
- Depression in the elderly male .
- The impact of childhood experiences on depression outcomes in adulthood.
- The use of ketamine and other novel treatments for depression.
- The effect of stigma on depression diagnosis and treatment.
- The conducted family assessment: cases of depression .
- The role of social support in depression recovery.
- The effectiveness of online support groups for individuals with depression.
- Depression and cognitive decline in adults.
- Depression: PICOT question component exploration .
- Exploring the impact of nutrition and dietary patterns on depression symptoms.
- Investigating the efficacy of art-based therapies in depression treatment.
- The role of neuroplasticity in the development and treatment of depression.
- Depression among HIV-positive women .
- The influence of gender on depression prevalence and symptomatology.
- Investigating the impact of workplace factors on depression rates and outcomes.
- The efficacy of family-based interventions in reducing depression symptoms in teenagers.
- Frontline nurses’ burnout, anxiety, depression, and fear statuses .
- The role of early-life stress and adversity in depression vulnerability.
- The impact of various environmental factors on depression rates.
- Exploring the link between depression and cardiovascular health .
- Depression detection in adults in nursing practice .
- Virtual reality as a therapeutic tool for depression treatment.
- Investigating the impact of childhood bullying on depression outcomes.
- The benefits of animal-assisted interventions in depression management.
- Depression and physical exercise .
- The relationship between depression and suicidal behavior .
- The influence of cultural factors on depression symptom expression.
- Investigating the role of epigenetics in depression susceptibility.
- Depression associated with cognitive dysfunction .
- Exploring the impact of adverse trauma on the course of depression.
- The efficacy of acceptance and commitment therapy in treating depression.
- The relationship between depression and substance use disorders .
- Depression and anxiety among college students .
- Investigating the effectiveness of group therapy for depression.
- Depression and chronic medical conditions .
Psychology Research Topics on Depression
- The influence of early attachment experiences on the development of depression.
- The impact of negative cognitive biases on depression symptomatology.
- Depression treatment plan for a queer patient .
- Examining the relationship between perfectionism and depression.
- The role of self-esteem in depression vulnerability and recovery.
- Exploring the link between maladaptive thinking styles (e.g., rumination, catastrophizing) and depression.
- Investigating the impact of social support on depression outcomes and resilience.
- Identifying depression in young adults at an early stage .
- The influence of parenting styles on the risk of depression in children and adolescents.
- The role of self-criticism and self-compassion in depression treatment.
- Exploring the relationship between identity development and depression in emerging adulthood.
- The role of learned helplessness in understanding depression and its treatment.
- Depression in the elderly .
- Examining the connection between self-efficacy beliefs and depression symptoms.
- The influence of social comparison processes on depression and body image dissatisfaction .
- Exploring the impact of trauma-related disorders on depression.
- The role of resilience factors in buffering against the development of depression.
- Investigating the relationship between personality traits and depression.
- Depression and workplace violence .
- The impact of cultural factors on depression prevalence and symptom presentation.
- Investigating the effects of chronic stress on depression risk.
- The role of coping strategies in depression management and recovery.
- The correlation between discrimination/prejudice and depression/anxiety .
- Exploring the influence of gender norms and societal expectations on depression rates.
- The impact of adverse workplace conditions on employee depression.
- Investigating the effectiveness of narrative therapy in treating depression.
- Cognitive behavior and depression in adolescents .
- Childhood emotional neglect and adult depression.
- The influence of perceived social support on treatment outcomes in depression.
- The effects of childhood bullying on the development of depression.
- The impact of intergenerational transmission of depression within families.
- Depression in children: symptoms and treatments .
- Investigating the link between body dissatisfaction and depression in adolescence.
- The influence of adverse life events and chronic stressors on depression risk.
- The effects of peer victimization on the development of depression in adolescence.
- Counselling clients with depression and addiction .
- The role of experiential avoidance in depression and its treatment.
- The impact of social media use and online interactions on depression rates.
- Depression management in adolescent .
- Exploring the relationship between emotional intelligence and depression symptomatology.
- Investigating the influence of cultural values and norms on depression stigma and help-seeking behavior.
- The effects of childhood maltreatment on neurobiological markers of depression.
- Psychological and emotional conditions of suicide and depression .
- Exploring the relationship between body dissatisfaction and depression.
- The influence of self-worth contingencies on depression vulnerability and treatment response.
- The impact of social isolation and loneliness on depression rates.
- Psychology of depression among college students .
- The effects of perfectionistic self-presentation on depression in college students.
- The role of mindfulness skills in depression prevention and relapse prevention.
- Investigating the influence of adverse neighborhood conditions on depression risk.
- Personality psychology and depression .
- The impact of attachment insecurity on depression symptomatology.
Postpartum Depression Research Topics
- Identifying risk factors for postpartum depression.
- Exploring the role of hormonal changes in postpartum depression.
- “Baby blues” or postpartum depression and evidence-based care .
- The impact of social support on postpartum depression.
- The effectiveness of screening tools for early detection of postpartum depression.
- The relationship between postpartum depression and maternal-infant bonding .
- Postpartum depression educational program results .
- Identifying effective interventions for preventing and treating postpartum depression.
- Examining the impact of cultural factors on postpartum depression rates.
- Investigating the role of sleep disturbances in postpartum depression.
- Depression and postpartum depression relationship .
- Exploring the impact of a traumatic birth experience on postpartum depression.
- Assessing the impact of breastfeeding difficulties on postpartum depression.
- Understanding the role of genetic factors in postpartum depression.
- Postpartum depression: consequences .
- Investigating the impact of previous psychiatric history on postpartum depression risk.
- The potential benefits of exercise on postpartum depression symptoms.
- The efficacy of psychotherapeutic interventions for postpartum depression.
- Postpartum depression in the twenty-first century .
- The influence of partner support on postpartum depression outcomes.
- Examining the relationship between postpartum depression and maternal self-esteem.
- The impact of postpartum depression on infant development and well-being.
- Maternal mood symptoms in pregnancy and postpartum depression .
- The effectiveness of group therapy for postpartum depression management.
- Identifying the role of inflammation and immune dysregulation in postpartum depression.
- Investigating the impact of childcare stress on postpartum depression.
- Postpartum depression among low-income US mothers .
- The role of postnatal anxiety symptoms in postpartum depression.
- The impact of postpartum depression on the marital relationship.
- The influence of postpartum depression on parenting practices and parental stress.
- Postpartum depression: symptoms, role of cultural factors, and ways to support .
- Investigating the efficacy of pharmacological treatments for postpartum depression.
- The impact of postpartum depression on breastfeeding initiation and continuation.
- The relationship between postpartum depression and post-traumatic stress disorder .
- Postpartum depression and its identification .
- The impact of postpartum depression on cognitive functioning and decision-making.
- Investigating the influence of cultural norms and expectations on postpartum depression rates.
- The impact of maternal guilt and shame on postpartum depression symptoms.
- Beck’s postpartum depression theory: purpose, concepts, and significance .
- Understanding the role of attachment styles in postpartum depression vulnerability.
- Investigating the effectiveness of online support groups for women with postpartum depression.
- The impact of socioeconomic factors on postpartum depression prevalence.
- Perinatal depression: research study and design .
- The efficacy of mindfulness-based interventions for postpartum depression.
- Investigating the influence of birth spacing on postpartum depression risk.
- The role of trauma history in postpartum depression development.
- The link between the birth experience and postnatal depression .
- How does postpartum depression affect the mother-infant interaction and bonding ?
- The effectiveness of home visiting programs in preventing and managing postpartum depression.
- Assessing the influence of work-related stress on postpartum depression.
- The relationship between postpartum depression and pregnancy-related complications.
- The role of personality traits in postpartum depression vulnerability.
🔎 Depression Essay Titles
Depression essay topics: cause & effect.
- The effects of childhood trauma on the development of depression in adults.
- The impact of social media usage on the prevalence of depression in adolescents.
- “Predictors of Postpartum Depression” by Katon et al.
- The effects of environmental factors on depression rates.
- The relationship between academic pressure and depression among college students.
- The relationship between financial stress and depression.
- The best solution to predict depression because of bullying .
- How does long-term unemployment affect mental health ?
- The effects of unemployment on mental health, particularly the risk of depression.
- The impact of genetics and family history of depression on an individual’s likelihood of developing depression.
- The relationship between depression and substance abuse .
- Child abuse and depression .
- The role of gender in the manifestation and treatment of depression.
- The effects of chronic stress on the development of depression.
- The link between substance abuse and depression.
- Depression among students at Elon University .
- The influence of early attachment styles on an individual’s vulnerability to depression.
- The effects of sleep disturbances on the severity of depression.
- Chronic illness and the risk of developing depression.
- Depression: symptoms and treatment .
- Adverse childhood experiences and the likelihood of experiencing depression in adulthood.
- The relationship between chronic illness and depression.
- The role of negative thinking patterns in the development of depression.
- Effects of depression among adolescents .
- The effects of poor body image and low self-esteem on the prevalence of depression.
- The influence of social support systems on preventing symptoms of depression.
- The effects of child neglect on adult depression rates.
- Depression caused by hormonal imbalance .
- The link between perfectionism and the risk of developing depression.
- The effects of a lack of sleep on depression symptoms.
- The effects of childhood abuse and neglect on the risk of depression.
- Social aspects of depression and anxiety .
- The impact of bullying on the likelihood of experiencing depression.
- The role of serotonin and neurotransmitter imbalances in the development of depression.
- The impact of a poor diet on depression rates.
- Depression and anxiety run in the family .
- The effects of childhood poverty and socioeconomic status on depression rates in adults.
- The impact of divorce on depression rates.
- The relationship between traumatic life events and the risk of developing depression.
- The influence of personality traits on susceptibility to depression.
- The impact of workplace stress on depression rates.
- Depression in older adults: causes and treatment .
- The impact of parental depression on children’s mental health outcomes.
- The effects of social isolation on the prevalence and severity of depression.
- The role of cultural factors in the manifestation and treatment of depression.
- The relationship between childhood bullying victimization and future depressive symptoms.
- The impact of early intervention and prevention programs on reducing the risk of postpartum depression.
- Treating mood disorders and depression .
- How do hormonal changes during pregnancy contribute to the development of depression?
- The effects of sleep deprivation on the onset and severity of postpartum depression.
- The impact of social media on depression rates among teenagers.
- The role of genetics in the development of depression.
- The impact of bullying on adolescent depression rates.
- Mental illness, depression, and wellness issues .
- The effects of a sedentary lifestyle on depression symptoms.
- The correlation between academic pressure and depression in students.
- The relationship between perfectionism and depression.
- The correlation between trauma and depression in military veterans.
- Anxiety and depression during childhood and adolescence .
- The impact of racial discrimination on depression rates among minorities.
- The relationship between chronic pain and depression.
- The impact of social comparison on depression rates among young adults.
- The effects of childhood abuse on adult depression rates.
Depression Argumentative Essay Topics
- The role of social media in contributing to depression among teenagers.
- The effectiveness of antidepressant medication: an ongoing debate.
- Depression treatment: therapy or medications ?
- Should depression screening be mandatory in schools and colleges?
- Is there a genetic predisposition to depression?
- The stigma surrounding depression: addressing misconceptions and promoting understanding.
- Implementation of depression screening in primary care .
- Is psychotherapy more effective than medication in treating depression?
- Is teenage depression overdiagnosed or underdiagnosed: a critical analysis.
- The connection between depression and substance abuse: untangling the relationship.
- Humanistic therapy of depression .
- Should ECT (electroconvulsive therapy) be a treatment option for severe depression?
- Where is depression more prevalent: in urban or rural communities? Analyzing the disparities.
- Is depression a result of chemical imbalance in the brain? Debunking the myth.
- Depression: a serious mental and behavioral problem .
- Should depression medication be prescribed for children and adolescents?
- The effectiveness of mindfulness-based interventions in managing depression.
- Should depression in the elderly be considered a normal part of aging?
- Is depression hereditary? Investigating the role of genetics in depression risk.
- Different types of training in managing the symptoms of depression .
- The effectiveness of online therapy platforms in treating depression.
- Should psychedelic therapy be explored as an alternative treatment for depression?
- The connection between depression and cardiovascular health: Is there a link?
- The effectiveness of cognitive-behavioral therapy in preventing depression relapse.
- Depression as a bad a clinical condition .
- Should mind-body interventions (e.g., yoga , meditation) be integrated into depression treatment?
- Should emotional support animals be prescribed for individuals with depression?
- The effectiveness of peer support groups in decreasing depression symptoms.
- The use of antidepressants: are they overprescribed or necessary for treating depression?
- Adult depression and anxiety as a complex problem .
- The effectiveness of therapy versus medication in treating depression.
- The stigma surrounding depression and mental illness: how can we reduce it?
- The debate over the legalization of psychedelic drugs for treating depression.
- The relationship between creativity and depression: does one cause the other?
- Cognitive-behavioral therapy for generalized anxiety disorder and depression .
- The role of childhood trauma in shaping adult depression: Is it always a causal factor?
- The debate over the medicalization of sadness and grief as forms of depression.
- Alternative therapies, such as acupuncture or meditation, are effective in treating depression.
- Depression as a widespread mental condition .
Controversial Topics about Depression
- The existence of “chemical imbalance” in depression: fact or fiction?
- The over-reliance on medication in treating depression: are alternatives neglected?
- Is depression overdiagnosed and overmedicated in Western society?
- Measurement of an individual’s level of depression .
- The role of Big Pharma in shaping the narrative and treatment of depression.
- Should antidepressant advertisements be banned?
- The inadequacy of current diagnostic criteria for depression: rethinking the DSM-5.
- Is depression a biological illness or a product of societal factors?
- Literature review on depression .
- The overemphasis on biological factors in depression treatment: ignoring environmental factors.
- Is depression a normal reaction to an abnormal society?
- The influence of cultural norms on the perception and treatment of depression.
- Should children and adolescents be routinely prescribed antidepressants?
- The role of family in depression treatment .
- The connection between depression and creative genius: does depression enhance artistic abilities?
- The ethics of using placebo treatment for depression studies.
- The impact of social and economic inequalities on depression rates.
- Is depression primarily a mental health issue or a social justice issue?
- Depression disassembling and treating .
- Should depression screening be mandatory in the workplace?
- The influence of gender bias in the diagnosis and treatment of depression.
- The controversial role of religion and spirituality in managing depression.
- Is depression a result of individual weakness or societal factors?
- Abnormal psychology: anxiety and depression case .
- The link between depression and obesity: examining the bidirectional relationship.
- The connection between depression and academic performance : causation or correlation?
- Should depression medication be available over the counter?
- The impact of internet and social media use on depression rates: harmful or beneficial?
- Interacting in the workplace: depression .
- Is depression a modern epidemic or simply better diagnosed and identified?
- The ethical considerations of using animals in depression research.
- The effectiveness of psychedelic therapies for treatment-resistant depression.
- Is depression a disability? The debate on workplace accommodations.
- Polysubstance abuse among adolescent males with depression .
- The link between depression and intimate partner violence : exploring the relationship.
- The controversy surrounding “happy” pills and the pursuit of happiness.
- Is depression a choice? Examining the role of personal responsibility.
Good Titles for Depression Essays
- The poetic depictions of depression: exploring its representation in literature.
- The melancholic symphony: the influence of depression on classical music.
- Moderate depression symptoms and treatment .
- Depression in modern music: analyzing its themes and expressions.
- Cultural perspectives on depression: a comparative analysis of attitudes in different countries.
- Contrasting cultural views on depression in Eastern and Western societies.
- Diagnosing depression in the older population .
- The influence of social media on attitudes and perceptions of depression in global contexts.
- Countries with progressive approaches to mental health awareness.
- From taboo to acceptance: the evolution of attitudes towards depression.
- Depression screening tool in acute settings .
- The Bell Jar : analyzing Sylvia Plath’s iconic tale of depression .
- The art of despair: examining Frida Kahlo’s self-portraits as a window into depression.
- The Catcher in the Rye : Holden Caulfield’s battle with adolescent depression.
- Music as therapy: how jazz artists turned depression into art.
- Depression screening tool for a primary care center .
- The Nordic paradox: high depression rates in Scandinavian countries despite high-quality healthcare.
- The Stoic East: how Eastern philosophies approach and manage depression.
- From solitude to solidarity: collective approaches to depression in collectivist cultures.
- The portrayal of depression in popular culture: a critical analysis of movies and TV shows.
- The depression screening training in primary care .
- The impact of social media influencers on depression rates among young adults.
- The role of music in coping with depression: can specific genres or songs help alleviate depressive symptoms?
- The representation of depression in literature: a comparative analysis of classic and contemporary works.
- The use of art as a form of self-expression and therapy for individuals with depression.
- Depression management guidelines implementation .
- The role of religion in coping with depression: Christian and Buddhist practices.
- The representation of depression in the video game Hellblade: Senua’s Sacrifice .
- The role of nature in coping with depression: can spending time outdoors help alleviate depressive symptoms?
- The effectiveness of dance/movement therapy in treating depression among older adults.
- The National Institute for Health: depression management .
- The portrayal of depression in stand-up comedy: a study of comedians like Maria Bamford and Chris Gethard.
- The role of spirituality in coping with depression: Islamic and Hindu practices .
- The portrayal of depression in animated movies : an analysis of Inside Out and The Lion King .
- The representation of depression by fashion designers like Alexander McQueen and Rick Owens.
- Depression screening in primary care .
- The portrayal of depression in documentaries: an analysis of films like The Bridge and Happy Valley .
- The effectiveness of wilderness therapy in treating depression among adolescents.
- The connection between creativity and depression: how art can help heal.
- The role of Buddhist and Taoist practices in coping with depression.
- Mild depression treatment research funding sources .
- The portrayal of depression in podcasts: an analysis of the show The Hilarious World of Depression .
- The effectiveness of drama therapy in treating depression among children and adolescents.
- The representation of depression in the works of Vincent van Gogh and Edvard Munch.
- Depression in young people: articles review .
- The impact of social media on political polarization and its relationship with depression.
- The role of humor in coping with depression: a study of comedians like Ellen DeGeneres.
- The portrayal of depression in webcomics: an analysis of the comics Hyperbole and a Half .
- The effect of social media on mental health stigma and its relationship with depression.
- Depression and the impact of human services workers .
- The masked faces: hiding depression in highly individualistic societies.
💭 Depression Speech Topics
Informative speech topics about depression.
- Different types of depression and their symptoms.
- The causes of depression: biological, psychological, and environmental factors.
- How depression and physical issues are connected .
- The prevalence of depression in different age groups and demographics.
- The link between depression and anxiety disorders .
- Physical health: The effects of untreated depression.
- The role of genetics in predisposing individuals to depression.
- What you need to know about depression .
- How necessary is early intervention in treating depression?
- The effectiveness of medication in treating depression.
- The role of exercise in managing depressive symptoms.
- Depression in later life: overview .
- The relationship between substance abuse and depression.
- The impact of trauma on depression rates and treatment.
- The effectiveness of mindfulness meditation in managing depressive symptoms.
- Enzymes conversion and metabolites in major depression .
- The benefits and drawbacks of electroconvulsive therapy for severe depression.
- The effect of gender and cultural norms on depression rates and treatment.
- The effectiveness of alternative therapies for depression, such as acupuncture and herbal remedies .
- The importance of self-care in managing depression.
- Symptoms of anxiety, depression, and peritraumatic dissociation .
- The role of support systems in managing depression.
- The effectiveness of cognitive-behavioral therapy in treating depression.
- The benefits and drawbacks of online therapy for depression.
- The role of spirituality in managing depression.
- Depression among minority groups .
- The benefits and drawbacks of residential treatment for severe depression.
- What is the relationship between childhood trauma and adult depression?
- How effective is transcranial magnetic stimulation (TMS) for treatment-resistant depression?
- The benefits and drawbacks of art therapy for depression.
- Mood disorder: depression and bipolar .
- The impact of social media on depression rates.
- The effectiveness of dialectical behavior therapy (DBT) in treating depression.
- Depression in older people .
- The impact of seasonal changes on depression rates and treatment options.
- The impact of depression on daily life and relationships, and strategies for coping with the condition.
- The stigma around depression and the importance of seeking help.
Persuasive Speech Topics about Depression
- How important is it to recognize the signs and symptoms of depression ?
- How do you support a loved one who is struggling with depression?
- The importance of mental health education in schools to prevent and manage depression.
- Social media: the rise of depression and anxiety .
- Is there a need to increase funding for mental health research to develop better treatments for depression?
- Addressing depression in minority communities: overcoming barriers and disparities.
- The benefits of including alternative therapies , such as yoga and meditation, in depression treatment plans.
- Challenging media portrayals of depression: promoting accurate representations.
- Two sides of depression disease .
- How social media affects mental health: the need for responsible use to prevent depression.
- The importance of early intervention: addressing depression in schools and colleges.
- The benefits of seeking professional help for depression.
- There is a need for better access to mental health care, including therapy and medication, for those suffering from depression.
- Depression in adolescents and suitable interventions .
- How do you manage depression while in college or university?
- The role of family and friends in supporting loved ones with depression and encouraging them to seek help.
- The benefits of mindfulness and meditation for depression.
- The link between sleep and depression, and how to improve sleep habits.
- How do you manage depression while working a high-stress job?
- Approaches to treating depression .
- How do you manage depression during pregnancy and postpartum?
- The importance of prioritizing employee mental health and providing resources for managing depression in the workplace.
- How should you manage depression while caring for a loved one with a chronic illness?
- How to manage depression while dealing with infertility or pregnancy loss.
- Andrew Solomon: why we can’t talk about depression .
- Destigmatizing depression: promoting mental health awareness and understanding.
- Raising funds for depression research: investing in mental health advances.
- The power of peer support: establishing peer-led programs for depression.
- Accessible mental health services: ensuring treatment for all affected by depression.
- Evidence-based screening for depression in acute care .
- The benefits of journaling for mental health: putting your thoughts on paper to heal.
- The power of positivity: changing your mindset to fight depression .
- The healing power of gratitude in fighting depression.
- The connection between diet and depression: eating well can improve your mood.
- Teen depression and suicide in Soto’s The Afterlife .
- The benefits of therapy for depression: finding professional help to heal.
- The importance of setting realistic expectations when living with depression.
📝 How to Write about Depression: Essay Structure
We’ve prepared some tips and examples to help you structure your essay and communicate your ideas.
Essay about Depression: Introduction
An introduction is the first paragraph of an essay. It plays a crucial role in engaging the reader, offering the context, and presenting the central theme.
A good introduction typically consists of 3 components:
- Hook. The hook captures readers’ attention and encourages them to continue reading.
- Background information. Background information provides context for the essay.
- Thesis statement. A thesis statement expresses the essay’s primary idea or central argument.
Hook : Depression is a widespread mental illness affecting millions worldwide.
Background information : Depression affects your emotions, thoughts, and behavior. If you suffer from depression, engaging in everyday tasks might become arduous, and life may appear devoid of purpose or joy.
Depression Essay Thesis Statement
A good thesis statement serves as an essay’s road map. It expresses the author’s point of view on the issue in 1 or 2 sentences and presents the main argument.
Thesis statement : The stigma surrounding depression and other mental health conditions can discourage people from seeking help, only worsening their symptoms.
Essays on Depression: Body Paragraphs
The main body of the essay is where you present your arguments. An essay paragraph includes the following:
- a topic sentence,
- evidence to back up your claim,
- explanation of why the point is essential to the argument;
- a link to the next paragraph.
Topic sentence : Depression is a complex disorder that requires a personalized treatment approach, comprising both medication and therapy.
Evidence : Medication can be prescribed by a healthcare provider or a psychiatrist to relieve the symptoms. Additionally, practical strategies for managing depression encompass building a support system, setting achievable goals, and practicing self-care.
Depression Essay: Conclusion
The conclusion is the last part of your essay. It helps you leave a favorable impression on the reader.
The perfect conclusion includes 3 elements:
- Rephrased thesis statement.
- Summary of the main points.
- Final opinion on the topic.
Rephrased thesis: In conclusion, overcoming depression is challenging because it involves a complex interplay of biological, psychological, and environmental factors that affect an individual’s mental well-being.
Summary: Untreated depression heightens the risk of engaging in harmful behaviors such as substance abuse and can also result in negative thought patterns, diminished self-esteem, and distorted perceptions of reality.
We hope you’ve found our article helpful and learned some new information. If so, feel free to share it with your friends. You can also try our free online topic generator !
- Pain, anxiety, and depression – Harvard Health | Harvard Health Publishing
- Depression-related increases and decreases in appetite reveal dissociable patterns of aberrant activity in reward and interoceptive neurocircuitry – PMC | National Library of Medicine
- How to Get Treatment for Postpartum Depression – The New York Times
- What Is Background Information and What Purpose Does It Serve? | Indeed.com
- Thesis | Harvard College Writing Center
- Topic Sentences: How Do You Write a Great One? | Grammarly Blog
725 Research Proposal Topics & Title Ideas in Education, Psychology, Business, & More
414 proposal essay topics for projects, research, & proposal arguments.
Home — Essay Samples — Nursing & Health — Neurology & Nervous System Diseases — Postpartum Depression
Essay Examples on Postpartum Depression
Postpartum depression and anxiety disorders in women, suffering in silence: the development of postpartum depression, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Jane's Postpartum Depression in The Yellow Wallpaper by Charlotte Perkins Gilman
The factors of postpartum depression, the effects of postpartum depression in the poem the yellow wallpaper by charlotte perkins gilman, postpartum depression among canadian women, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Bond Between Mother and Child: Postpartum Depression in Immigrants
Relevant topics.
- Post Traumatic Stress Disorder
- Sleep Deprivation
- Drug Addiction
- Breast Cancer
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

KATHRYN P. HIRST, MD, AND CHRISTINE Y. MOUTIER, MD
A more recent article on peripartum depression is available.
Am Fam Physician. 2010;82(8):926-933
Patient information: See related handout on postpartum depression , written by the authors of this article.
Author disclosure: Nothing to disclose.
Postpartum major depression is a disorder that is often unrecognized and must be distinguished from “baby blues.” Antenatal depressive symptoms, a history of major depressive disorder, or previous postpartum major depression significantly increase the risk of postpartum major depression. Screening with the Edinburgh Postnatal Depression Scale may be appropriate. Some women with postpartum major depression may experience suicidal ideation or obsessive thoughts of harming their infants, but they are reluctant to volunteer this information unless asked directly. Psychotherapy or selective serotonin reuptake inhibitors may be used to treat the condition. In patients with moderate to severe postpartum major depression, psychotherapy may be used as an adjunct to medication. No evidence suggests that one antidepressant is superior to others. Antidepressants vary in the amount secreted into breast milk. If left untreated, postpartum major depression can lead to poor mother-infant bonding, delays in infant growth and development, and an increased risk of anxiety or depressive symptoms in the infant later in life.
The term “postpartum depression” commonly includes major and minor depression, which differ in severity and prognosis, and have a combined incidence of 7 to 15 percent in the first three months postpartum. 1 The overall incidence of postpartum major depression is 5 to 7 percent in the first three months, suggesting that postpartum women have rates of major depression similar to those in the general population. 1 However, specific risk factors significantly increase rates of postpartum major depression for a subset of women. The strongest risk factor is a history of postpartum major depression with a previous pregnancy. Studies report that 25 to 50 percent of women who experience postpartum major depression will have a recurrence after a subsequent pregnancy. 2 – 4 Other important risk factors include antenatal depressive symptoms (relative risk [RR] = 5.6), a history of major depressive disorder (RR = 4.5), poor social support (RR = 2.6), major life events or stressors during pregnancy (RR = 2.5), and a family history of postpartum major depression (RR = 2.4). 5 – 7 Women with gestational diabetes 8 and who give birth to multiples may also be at higher risk of postpartum major depression. 9 Socioeconomic status and obstetric complications have not been shown consistently to be risk factors for postpartum major depression. 10
The etiology of postpartum major depression remains unclear. Some women may be sensitive to hormonal changes during reproductive events, specifically menses, pregnancy, and menopause. 11 The drop in hormone levels after delivery may play a role. 12 , 13 An association between cortisol levels and depressive symptoms during pregnancy and postpartum has been reported. 14 Major depression may also begin during pregnancy and continue into the postpartum period.
According to the American College of Obstetricians and Gynecologists, screening for antepartum or postpartum depression should be strongly considered, although evidence is lacking to support a recommendation for universal screening. 15 Patients with identified risk factors may be selected for screening. Preparation for postpartum care and consideration of prophylactic treatment have been recommended in these women. 16 Prophylactic treatment may involve psychotherapy beginning in the third trimester or medication offered immediately postpartum. Sertraline (Zoloft) has been shown to decrease the recurrence of postpartum major depression when started immediately after delivery. 3 The most commonly used validated screening tool for postpartum depression is the Edinburgh Postnatal Depression Scale ( Figure 1 ) . 16 – 19 The scale has 10 questions, including a question on suicidal ideation. Each question is scored on a scale from zero to three. In women without a history of postpartum major depression, a score above 12 has a sensitivity of 86 percent and specificity of 78 percent for postpartum major depression. 17 One study reported that 80 percent of women with a history of postpartum major depression who relapsed within one year of a subsequent delivery scored above nine at four weeks postpartum. 20
Screening can be performed at the four- to six-week postpartum visit or the two-month well-child visit. 20 , 21 The Edinburgh Postnatal Depression Scale is completed by the patient and can be quickly scored by office staff. It is available in several languages and may be downloaded free from multiple sources, including the University of California, San Francisco, Fresno, Web site ( http://www.fresno.ucsf.edu/pediatrics/downloads/edinburghscale.pdf ).
A diagnosis of major depressive disorder requires the presence of five key symptoms that last at least two weeks and impair normal function. Depressed mood or anhedonia must be present ( Table 1 22 ) . The Diagnostic and Statistical Manual of Mental Disorders, 4th ed., text revision, does not distinguish between postpartum major depression and major depressive disorder, but does provide a postpartum onset specifier for major depressive disorder, defined as onset within four weeks of delivery. 22 Many experts extend this to the first 12 months postpartum. 23
Postpartum major depression is differentiated from “baby blues” by the severity and duration of symptoms ( Table 2 ) . Baby blues begins during the first two to three days after delivery and resolves within 10 days. Symptoms include brief crying spells, irritability, poor sleep, nervousness, and emotional reactivity. Suicidal ideation is not present. Although baby blues was previously considered benign, increasing evidence suggests that women with these symptoms are at risk of progression to postpartum major depression. 24 The diagnosis of postpartum major depression should be strongly considered in women who score above 12 on the Edinburgh Postnatal Depression Scale, experience symptoms that cause moderate to severe social dysfunction, report any suicidal ideation, or experience symptoms for more than 10 days.
Symptoms of postpartum major depression may differ from nonpostpartum major depression. 25 Women with postpartum major depression are less likely to report feeling sad, 26 but have notable feelings of guilt or worthlessness, and a lack of enjoyment or interest in pleasurable activities. Decreased energy and disrupted sleep related to infant care may be difficult to differentiate from symptoms of depression. Asking a mother whether she can sleep when her infant sleeps at night may provide clarification, because many women with postpartum major depression have difficulty falling or staying asleep. 27 Although sleep disruptions can also lead to mild transient problems in memory and concentration, persistent difficulty with concentration or cognitive tasks is indicative of a mood disorder. 28 Changes in appetite are unreliable in making a diagnosis. 24
Many women with postpartum major depression have no psychiatric history and may be reluctant to volunteer symptoms or to seek help. It is important to discuss symptoms, such as obsessive thoughts and suicidal ideation, with these women. Up to 60 percent of women with postpartum major depression have obsessive thoughts focusing on aggression toward the infant. 29 These thoughts are intrusive and similar to those in obsessive-compulsive disorder. They do not represent a desire to hurt the infant but over time can lead to avoidance of the infant in an effort to minimize the thoughts. The shame and guilt associated with these intrusive images or thoughts can reduce the likelihood of divulging this symptom. Physicians should ask about these symptoms as part of the diagnosis of postpartum major depression. Nonjudgmental phrases include: “Many women with postpartum major depression have thoughts or images of hurting their baby. Has this happened to you? What did you do in response to them?” By acknowledging that these symptoms are part of postpartum major depression, physicians can help women understand their experiences and seek treatment.
Because suicide is a leading cause of maternal death, physicians should ask women suspected of having postpartum major depression about suicidal ideation. 30 Many physicians are familiar with asking about active suicidal ideation, which involves a plan to end one's life. However, women with mild to moderate postpartum major depression may have passive suicidal ideation, defined as a desire to die but no plan. One useful question is, “Have you wished you would go to sleep and not wake up?” A woman with active or passive suicidal ideation may cite her infant or family as a reason not to harm herself. However, as depression worsens, she may view herself as a bad mother and believe that her child would be better off without her. A woman who has active suicidal ideation or thoughts that her child or family would benefit from her death requires emergent psychiatric evaluation and possible hospitalization.
The diagnosis of postpartum major depression should also include asking patients about past manic episodes. 31 A history of mania or hypomania may indicate bipolar disorder, requiring specific pharmacologic treatment. Bipolar disorder is also associated with a higher risk of mood episode postpartum. 32 Two questions that are recommended for screening for past manic episodes are (1) “Have you ever had four continuous days when you were feeling so good, high, excited, or hyper that other people thought you were not your normal self or you got into trouble?” and (2) “Have you experienced four continuous days when you were so irritable that you found yourself shouting at people or starting fights or arguments?” Positive responses require referral to a psychiatrist. 16
Laboratory Testing
Because hypothyroidism may also cause depressive symptoms, physicians should measure thyroid-stimulating hormone levels in women with suspected postpartum major depression. 16 About 8 percent of women develop postpartum autoimmune thyroiditis, which can mimic many symptoms of postpartum major depression. 33 Blood loss during delivery can lead to anemia and considerable fatigue, but does not cause depressed mood or anhedonia.
NONPHARMACOLOGIC TREATMENT
Individual or group psychotherapy is an effective treatment for mild to moderate postpartum major depression. 34 Psychotherapy can also be used as adjunct therapy with medication in moderate to severe postpartum major depression. The most commonly used psychotherapy modalities are interpersonal therapy and cognitive behavior therapy. Both modalities have been shown to be effective in individual and group settings for treating postpartum major depression. 35 – 38
Light therapy has not been shown to be effective in patients with postpartum major depression. 39 Acupuncture, yoga, and exercise have not been studied sufficiently. 40 However, exercise, adequate exposure to morning light, and support from others are encouraged by many physicians as adjuncts to other treatments for women with postpartum major depression. A postpartum depression action plan is available at https://familydoctor.org/familydoctor/en/diseases-conditions/postpartum-depression.html .
PHARMACOLOGIC TREATMENT
Selective serotonin reuptake inhibitors have become the mainstay of treatment for moderate to severe postpartum major depression because of their favorable adverse effect profiles and relative safety in overdose compared with tricyclic antidepressants 16 ( Figure 2 ) . Table 3 lists the most commonly used antidepressants, adverse effect profiles, and starting and target dosages. 16 No evidence suggests that one antidepressant is superior to others in treating postpartum major depression.
For breastfed infants of mothers treated for postpartum major depression, a pooled analysis of available data found that infant serum levels of sertraline, paroxetine (Paxil), and nortriptyline (Pamelor) were usually undetectable. 41 Detectable levels of fluoxetine (Prozac) and citalopram (Celexa) have been found in infant serum, but the milk-to-plasma ratio remains well below the standard acceptable ratio of 0.1. 41 Case reports cite adverse effects in some breastfed infants of mothers taking fluoxetine, citalopram, or bupropion (Wellbutrin), but overall evidence of harm to infants is lacking. 42 Measurement of medication levels in infant serum or breast milk is not currently recommended. 43
Before prescribing an agent for postpartum major depression, physicians should consider the patient's experience with antidepressants. If the patient has previously responded well to a specific agent, that medication should be the first choice unless there is evidence of potential harm. 16 , 44 Although breastfed infants are unlikely to experience adverse effects from antidepressant medications, infants should be monitored for symptoms, such as persistent irritability, decreased feeding, or poor weight gain. Maternal depression or problems within the mother-infant dyad can also be associated with these symptoms. 45 , 46 Formula feeding should be considered in women with severe postpartum major depression that requires medication implicated in adverse effects for the infant. LactMed is an online, peer-reviewed resource that provides information on the safety of medications in mothers who breastfeed ( http://toxnet.nlm.nih.gov/cgi-bin/sis/htmlgen?LACT ).
Because postpartum women may have increased sensitivity to adverse effects of medications, a reasonable strategy is to start at low dosages for the first four days and then titrate up. 3 , 16 The Edinburgh Postnatal Depression Scale can be used to monitor progress over time. After symptoms are in remission, treatment is typically continued for six to nine months of euthymia before tapering the medication. Tapering over two weeks, especially for paroxetine, extended-release venlafaxine (Effexor XR), and extended-release desvenlafaxine (Pristiq), can prevent the influenza-like symptoms of discontinuation syndrome.
Estrogen therapy has been studied as a treatment for postpartum major depression. Three studies have reported positive results, but each has had notable limitations. 47 – 49 Although estrogen therapy is not currently recommended for postpartum major depression, further research is needed. 49 , 50
Risks and Benefits of Treatment
Women who are pregnant or breastfeeding may be reluctant to start medication for fear of harming their child. A thorough risk-benefit discussion with each patient is essential before deciding on treatment for postpartum major depression. With the physician's help, the patient should be encouraged to make a list of the potential benefits of treatment. This will allow her to envision her own recovery and set appropriate goals. The physician should then explain the risks of pharmacologic treatment, such as the penetrance of medication into breast milk (if applicable for the medication selected), as well as the risks of persistent depressive symptoms, such as infant sleep disturbance, 51 poor mother-infant bonding, delays in infant growth and IQ, and an increased risk of anxiety or depressive symptoms for the infant later in life. 52
Gaynes BN, Gavin N, Meltzer-Brody S, et al. Perinatal depression: prevalence, screening accuracy, and screening outcomes. Evidence Report/Technology Assessment No. 119. (Prepared by the RTI–University of North Carolina Evidence-based Practice Center, under Contract No. 290-02-0016.) AHRQ Publication No. 05-E006-2. Rockville, Md.: Agency for Healthcare Research and Quality. February 2005.
Cooper PJ, Murray L. Course and recurrence of postnatal depression. Evidence for the specificity of the diagnostic concept. Br J Psychiatry. 1995;166(2):191-195.
Wisner KL, Perel JM, Peindl KS, Hanusa BH, Piontek CM, Findling RL. Prevention of postpartum depression: a pilot randomized clinical trial. Am J Psychiatry. 2004;161(7):1290-1292.
Wisner KL, Perel JM, Peindl KS, Hanusa BH, Findling RL, Rapport D. Prevention of recurrent postpartum depression: a randomized clinical trial. J Clin Psychiatry. 2001;62(2):82-86.
Milgrom J, Gemmill AW, Bilszta JL, et al. Antenatal risk factors for postnatal depression: a large prospective study. J Affect Disord. 2008;108(1–2):147-157.
Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26(4):289-295.
Forty L, Jones L, Macgregor S, et al. Familiality of postpartum depression in unipolar disorder: results of a family study. Am J Psychiatry. 2006;163(9):1549-1553.
Kozhimannil KB, Pereira MA, Harlow BL. Association between diabetes and perinatal depression among low-income mothers. JAMA. 2009;301(8):842-847.
Choi Y, Bishai D, Minkovitz CS. Multiple births are a risk factor for postpartum maternal depressive symptoms. Pediatrics. 2009;123(4):1147-1154.
Johnstone S, Boyce PM, Hickey AR, Morris-Yatees AD, Harris MG. Obstetric risk factors for postnatal depression in urban and rural community samples. Aust N Z J Psychiatry. 2001;35(1):69-74.
Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, Rubinow DR. Effects of gonadal steroids in women with a history of postpartum depression. Am J Psychiatry. 2000;157(6):924-930.
Green AD, Barr AM, Galea LA. Role of estradiol withdrawal in ‘anhedonic’ sucrose consumption: a model of postpartum depression. Physiol Behav. 2009;97(2):259-265.
Suda S, Segi-Nishida E, Newton SS, Duman RS. A postpartum model in rat: behavioral and gene expression changes induced by ovarian steroid deprivation. Biol Psychiatry. 2008;64(4):311-319.
Yim IS, Glynn LM, Dunkel-Schetter C, Hobel CJ, Chicz-DeMet A, Sandman CA. Risk of postpartum depressive symptoms with elevated corticotropin- releasing hormone in human pregnancy. Arch Gen Psychiatry. 2009;66(2):162-169.
American College of Obstetricians and Gynecologists. Committee on Obstetric Practice. Committee opinion no. 453: screening for depression during and after pregnancy. Obstet Gynecol. 2010;115(2 pt 1):394-395.
Wisner KL, Parry BL, Piontek CM. Clinical practice. Postpartum depression. N Engl J Med. 2002;347(3):194-199.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782-786.
Eberhard-Gran M, Eskild A, Tambs K, Schei B, Opjordsmoen S. The Edinburgh Postnatal Depression Scale: validation in a Norwegian community sample. Nord J Psychiatry. 2001;55(2):113-117.
Adouard F, Glangeaud-Freudenthal NM, Golse B. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in a sample of women with high-risk pregnancies in France. Arch Womens Ment Health. 2005;8(2):89-95.
Peindl KS, Wisner KL, Hanusa BH. Identifying depression in the first postpartum year: guidelines for office-based screening and referral. J Affect Disord. 2004;80(1):37-44.
Sheeder J, Kabir K, Stafford B. Screening for postpartum depression at well-child visits: is once enough during the first 6 months of life?. Pediatrics. 2009;123(6):e982-e988.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders . 4th ed., text revision. Washington, DC: American Psychiatric Association; 2000.
O'Hara MW, Swain AM. Rates and risk of postpartum depression: a meta-analysis. Int Rev Psychiatry. 1996;8(1):37-54.
Henshaw C, Foreman D, Cox J. Postnatal blues: a risk factor for postnatal depression. J Psychosom Obstet Gynaecol. 2004;25(3–4):267-272.
Kammerer M, Marks MN, Pinard C, et al. Symptoms associated with the DSM IV diagnosis of depression in pregnancy and post partum. Arch Womens Ment Health. 2009;12(3):135-141.
Bernstein IH, Rush AJ, Yonkers K, et al. Symptom features of postpartum depression: are they distinct?. Depress Anxiety. 2008;25(1):20-26.
Goyal D, Gay C, Lee K. Fragmented maternal sleep is more strongly correlated with depressive symptoms than infant temperament at three months postpartum. Arch Womens Ment Health. 2009;12(4):229-237.
Swain AM, O'Hara MW, Starr KR, Gorman LL. A prospective study of sleep, mood, and cognitive function in postpartum and nonpostpartum women. Obstet Gynecol. 1997;90(3):381-386.
Wisner KL, Peindl KS, Gigliotti T, Hanusa BH. Obsessions and compulsions in women with postpartum depression. J Clin Psychiatry. 1999;60(3):176-180.
Mander R, Smith GD. Saving mothers' lives (formerly why mothers die): reviewing maternal deaths to make motherhood safer 2003–2005. Midwifery. 2008;24(1):8-12.
Sharma V, Khan M, Corpse C, Sharma P. Missed bipolarity and psychiatric comorbidity in women with postpartum depression. Bipolar Disord. 2008;10(6):742-747.
Munk-Olsen T, Laursen TM, Mendelson T, Pedersen CB, Mors O, Mortensen PB. Risks and predictors of readmission for a mental disorder during the postpartum period. Arch Gen Psychiatry. 2009;66(2):189-195.
Nicholson WK, Robinson KA, Smallridge RC, Ladenson PW, Powe NR. Prevalence of postpartum thyroid dysfunction: a quantitative review. Thyroid. 2006;16(6):573-582.
Dennis CL, Hodnett E. Psychosocial and psychological interventions for treating postpartum depression. Cochrane Database Syst Rev. 2007(4):CD006116.
Grote NK, Swartz HA, Geibel SL, Zuckoff A, Houck PR, Frank E. A randomized controlled trial of culturally relevant, brief interpersonal psychotherapy for perinatal depression. Psychiatr Serv. 2009;60(3):313-321.
Chabrol H, Teissedre F, Saint-Jean M, Teisseyre N, Rogé B, Mullet E. Prevention and treatment of post-partum depression: a controlled randomized study on women at risk. Psychol Med. 2002;32(6):1039-1047.
Appleby L, Warner R, Whitton A, Faragher B. A controlled study of fluoxetine and cognitive-behavioural counselling in the treatment of postnatal depression. BMJ. 1997;314(7085):932-936.
Crockett K, Zlotnick C, Davis M, Payne N, Washington R. A depression preventive intervention for rural low-income African-American pregnant women at risk for postpartum depression. Arch Womens Ment Health. 2008;11(5–6):319-325.
Corral M, Wardrop AA, Zhang H, Grewal AK, Patton S. Morning light therapy for postpartum depression. Arch Womens Ment Health. 2007;10(5):221-224.
Dennis CL, Allen K. Interventions (other than pharmacological, psychosocial or psychological) for treating antenatal depression. Cochrane Database Syst Rev. 2008(4):CD006795.
Weissman AM, Levy BT, Hartz AJ, et al. Pooled analysis of antidepressant levels in lactating mothers, breast milk, and nursing infants. Am J Psychiatry. 2004;161(6):1066-1078.
Sit DK, Wisner KL. Identification of postpartum depression. Clin Obstet Gynecol. 2009;52(3):456-468.
ACOG Committee on Practice Bulletins–Obstetrics. ACOG Practice Bulletin: clinical management guidelines for obstetrician-gynecologists number 92, April 2008 (replaces practice bulletin number 87, November 2007). Use of psychiatric medications during pregnancy and lactation. Obstet Gynecol. 2008;111(4):1001-1020.
Payne JL. Antidepressant use in the postpartum period: practical considerations. Am J Psychiatry. 2007;164(9):1329-1332.
O'Brien LM, Heycock EG, Hanna M, Jones PW, Cox JL. Postnatal depression and faltering growth: a community study. Pediatrics. 2004;113(5):1242-1247.
McGrath JM, Records K, Rice M. Maternal depression and infant temperament characteristics. Infant Behav Dev. 2008;31(1):71-80.
Gregoire AJ, Kumar R, Everitt B, Henderson AF, Studd JW. Transdermal oestrogen for treatment of severe postnatal depression. Lancet. 1996;347(9006):930-933.
Ahokas A, Kaukoranta J, Wahlbeck K, Aito M. Estrogen deficiency in severe postpartum depression: successful treatment with sublingual physiologic 17beta-estradiol: a preliminary study. J Clin Psychiatry. 2001;62(5):332-336.
Sichel DA, Cohen LS, Robertson LM, Ruttenberg A, Rosenbaum JF. Prophylactic estrogen in recurrent postpartum affective disorder. Biol Psychiatry. 1995;38(12):814-818.
Moses-Kolko EL, Berga SL, Kalro B, Sit DK, Wisner KL. Transdermal estradiol for postpartum depression: a promising treatment option. Clin Obstet Gynecol. 2009;52(3):516-529.
Armitage R, Flynn H, Hoffmann R, Vazquez D, Lopez J, Marcus S. Early developmental changes in sleep in infants: the impact of maternal depression. Sleep. 2009;32(5):693-696.
Brand SR, Brennan PA. Impact of antenatal and postpartum maternal mental illness: how are the children?. Clin Obstet Gynecol. 2009;52(3):441-455.
Continue Reading
More in AFP
More in pubmed.
Copyright © 2010 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

Research Topic Starters
- Aggressive/Distracted Driving
- Climate Change
- Depression & Postpartum Depression
- E-Cigarettes and Vaping
- Freedom of Speech
- Gender Equity
- Gun Control
- Prescription Medication Abuse
- Psychological Disorders
- Systemic Racism
- Trigger Warnings
NEW: All STCC students, faculty & staff are now automatically registered in the library system!
>help with accessing library resources., ask a librarian..., >email: [email protected].
>Call a librarian: (413)755-4549
Staff available during library hours
- Academic Search Complete This link opens in a new window A good starting point for a database search. - provides full text articles to many journals and magazines, including peer-reviewed or scholarly titles
- MedlinePlus This link opens in a new window Produced by the National Library of Medicine, it brings you information about diseases, conditions, and wellness issues in language you can understand.
- Psychology & Behavioral Sciences Collection This link opens in a new window More advanced database - covering topics in emotional and behavioral characteristics, psychiatry & psychology, mental processes.
Resources on Depression & Postpartum Depression
- Search Terms
- Citation Aids
Depression is a serious medical illness. It's more than just a feeling of being sad or "blue" for a few days. If you are one of the more than 19 million teens and adults in the United States who have depression, the feelings do not go away. They persist and interfere with your everyday life. Symptoms can include
- Feeling sad or "empty"
- Loss of interest in favorite activities
- Overeating, or not wanting to eat at all
- Not being able to sleep, or sleeping too much
- Feeling very tired
- Feeling hopeless, irritable, anxious, or guilty
- Aches or pains, headaches, cramps, or digestive problems
- Thoughts of death or suicide
Depression is a disorder of the brain. There are a variety of causes, including genetic, biological, environmental, and psychological factors.
>Taken from MedlinePlus and produced by the National Institute of Health, a United States Government Agency.
______________________________________________________________________________________________
Postpartum Depression : The birth of a baby can trigger a jumble of powerful emotions, from excitement and joy to fear and anxiety. But it can also result in something you might not expect — depression.
Most new moms experience postpartum "baby blues" after childbirth, which commonly include mood swings, crying spells, anxiety and difficulty sleeping. Baby blues typically begin within the first two to three days after delivery, and may last for up to two weeks.
Postpartum depression isn't a character flaw or a weakness. If you have postpartum depression, prompt treatment can help you manage your symptoms and help you bond with your baby.
>Taken from the Mayo Clinic Website , a prominent health care provider.
Some search terms to try when searching databases for Depression:
Mental Depression
Clinical Depression
Major Depressive Disorder (MDD)
Unipolar Depression
Bipolar Depression
Antidepressants
Persistent depressive disorder
Note: Using just the search term 'depression' in non-medical databases can lead to returns on an economic depression. It is best to use more than one search term to optimize search returns.
Some search terms to try when searching databases for Postpartum Depression:
Postpartum Depression (PPD)
Baby Blues S yndrome
Postpartum Anxiety
Postpartum Psychosis
Postnatal Complications,
Note It is best to use more than one search term to optimize search returns
General Background - Depression
- Depression - also called: Clinical depression, Dysthymic disorder, Major depressive disorder, Unipolar depression From MedlinePlus. Good starting point and introduction to the brain disease.
- Depression Basics Background information on Depression from the National Institute of Mental Health, A United States Government agency..
General Background - Postpartum Depression
- Postpartum Depression- also called: Post-pregnancy depression Starting point article from MedlinePlus - Many women have the baby blues after childbirth and may have mood swings, feel sad, anxious or overwhelmed, have crying spells, lose your appetite, or have trouble sleeping.
- Postpartum Depression Introduction from the Mayo Clinic. Good background and starting point to begin your research.
- Postpartum depression. - Research Starter Magill’s Medical Guide (Online Edition), 2019
Scholarly Peer Reviewed Articles on Depression
- Major Depression Disorder in Adults: A Review of Antidepressants. Major Depressive Disorder (MDD) is the "most common mood disorder having at least one single major depressive episode." The purpose of this paper is to discuss and review current drugs and treatment for MDD.
- General practitioners' perspectives on barriers to depression care: development and validation of a questionnaire. General practitioners (GPs) regularly feel challenged by the care of depressed patients and may encounter several barriers in providing best management. The aim of this study was to develop and validate a questionnaire assessing barriers to depression care
- The Association of Diet and Depression: An Analysis of Dietary Measures in Depressed, Non-depressed, and Healthy Youth The authors designed this study to assess the association between dietary patterns and depression using four dietary measures previously studied in children and adolescents.
Scholarly Peer Reviewed Articles on Postpartum Depression
- The Effect of Social Support on Pregnancy and Postpartum Depression. Introduction: Recent researches show us the given social support to the mother during pregnancy, birth and in postpartum peroid effects positively the adaptation to the role of motherhood, increases sensitivity to the baby and helps to relations with the relatives.
- Postpartum depression screening in primary care: How to make it a success. The article discusses the conduct of postpartum depression (PPD) screening in primary care to identify, support, and refer mothers for appropriate mental health treatment in 2019.
- Tracking Postpartum Depression In Young Women Objective: to track postpartum depression among young women who are in the second week and in the sixth month postpartum.
- Diagnosing Depression Signs and symptoms of depression are spelled out, and multimodal treatment through psychotherapy, medication, support groups, and aerobic exercise is discussed
- Understanding Depression Dr. Andrew Leuchter, Director of Adult Psychiatry at UCLA, explains that depression is an illness not a weakness, and that real, physical changes in brain neurochemistry or in horm...
- Women and Depression Clinical depression affects 19 million Americans, of whom two-thirds are women. This program from The Doctor Is In addresses the good news about depression: it is a diagnosable and treatable illness. From Films on Demand. Login Required
STCC Library Citation Handouts
- 2020 APA Citation Handout 7th edition
- 2020 MLA Citation Handout
MyBib Plug in your source information and MyBib will create a citation for you!
- << Previous: Climate Change
- Next: E-Cigarettes and Vaping >>
- Last Updated: Jan 19, 2024 11:23 AM
- URL: https://libguides.stcc.edu/ResearchStarter
- Infertility
- Miscarriage & Loss
- Pre-Pregnancy Shopping Guides
- Diapering Essentials
- Bedtime & Bathtime
- Baby Clothing
- Health & Safety
- First Trimester
- Second Trimester
- Third Trimester
- Pregnancy Products
- Baby Names By Month
- Popular Baby Names
- Unique Baby Names
- Labor & Delivery
- Birth Stories
- Fourth Trimester
- Parental Leave
- Postpartum Products
- Sleep Guides & Schedules
- Feeding Guides & Schedules
- Milestone Guides
- Learn & Play
- Beauty & Style Shopping Guides
- Meal Planning & Shopping
- Entertaining
- Personal Essays
- State of Motherhood
- Home Shopping Guides
- Work & Motherhood
- Family Finances & Budgeting
- Viral & Trending
Celebrity News
- Women’s Health
- Children’s Health
- It’s Science
- Mental Health
- Health & Wellness Shopping Guide
- What To Read
- What To Watch
- Women’s History Month
- St. Patrick’s Day
- Single Parenting
- Blended Families
- Community & Friendship
- Marriage & Partnerships
- Grandparents & Extended Families
- Stretch Mark Cream
- Pregnancy Pillows
- Maternity Pajamas
- Maternity Workout Clothes
- Compression Socks
- All Pregnancy Products
- Pikler Triangles
- Toddler Sleep Sacks
- Toddler Scooters
- Water Tables
- All Toddler Products
- Breastmilk Coolers
- Postpartum Pajamas
- Postpartum Underwear
- Postpartum Shapewear
- All Postpartum Products
- Kid Pajamas
- Play Couches
- Kids’ Backpacks
- Kids’ Bikes
- Kids’ Travel Gear
- All Child Products
- Baby Swaddles
- Eco-Friendly Diapers
- Baby Bathtubs
- All Baby Products
- Pregnancy-safe Skincare
- Diaper Bags
- Maternity Jeans
- Matching Family Swimwear
- Mama Necklaces
- All Beauty and Style Products
- All Classes
- Free Classes By Motherly
- Parenting & Family Topics
- Toddler Topics
- TTC & Pregnancy
- Wellness & Fitness
- Please wait..
Stop telling me I won’t have PPD again
I'm pregnant again, and some of my friends and family have decided to tell me that “this time will be different.” More specifically, that this time around I won’t have postpartum depression.
By Erin Bagwell February 25, 2022

Erin Bagwell
Content warning: Discussion of suicidal ideation ahead.
Hi! My name is Erin Bagwell and I’m a documentary filmmaker, postpartum depression survivor , and mother of two girls: a 3-year-old and a 1-month-old.
I had debilitating postpartum depression with my first daughter three years ago. I was suicidal, crying multiple times a day, and felt like I was trapped under an excruciating wave of depression and anxiety for the first few months of my daughter’s life. So much so that I thought I made a mistake. Maybe I didn’t have what it takes to be a mom.
I found a PMAD therapist (perinatal mood and anxiety disorder) and joined a PMAD support group where I learned I was wrong: I not only had what it takes to be a mom, but I was experiencing something, that according to The Motherhood Center 1 in 5 birthing people struggle with when they become mothers. Being able to name my postpartum depression (PPD) allowed me to understand that what I was experiencing wasn’t what motherhood was supposed to feel like. It gave me the tools and the hope to explore the narrative I had around what it meant to be a mother, and to start the healing process. I even made a 30 minute documentary about the process called Year One about identity, coming through the other side of PPD, and my first year of motherhood.
You can watch Year One here.
After my daughter turned 1, my mental health began to improve, and little by little, I began to feel happier than I had been in a long time. Coming through the other side of something so painful felt liberating. Every good day I felt more confident in myself and more joyful. I started to regain my sense of self and rebuild my identity as a mother. And after weathering the first year of the pandemic, my husband and I started talking about what it would look like to have another baby.
We went back and forth on the pros and cons and what it would be like to potentially experience PPD again. And despite the pain of experiencing PPD, I felt like I was strong enough to try again. Especially since I had a great PMAD therapist to guide me through this pregnancy, and the experience of knowing when something might be wrong.
So I got pregnant.
But I’ve noticed that during this pregnancy, some of my friends and family have decided to tell me that “this time will be different.” More specifically, that this time around I won’t have postpartum depression.
PPD doesn’t discriminate based on how together your life is.
And to be fair: this time will be different. Lots of things in my life are different. My family moved out of our one-bedroom apartment in Brooklyn and into a house closer to my parents. I have more support and my toddler is in a part-time childcare program. My parenting life is much easier than it was when my family lived in New York City. But having great support doesn’t guarantee perfect mental health. Look no further than some of our favorite celebrities like Adele , Cardi B , and Reese Witherspoon , who all suffered from PMADs. Or the patron saint of postpartum depression, Alanis Morrisette , who had PPD with all three of her children. One could assume all of these women had first-class postpartum support, but having support doesn’t negate the life-altering matrescence a person goes through to become a mother.
One of the biggest misconceptions about depression is that it can’t affect put-together people. In fact, my PMAD therapist told me the people who are often hit the hardest are the Type-A overachievers who like to stick to a plan and know how to do things well. But what I’ve learned through my parenting experience is that motherhood wasn’t something I did “well” off the bat. It was a struggle, a process, a learning—one that can be quite infuriating.
My own grandmother had postpartum depression twice when she was pregnant with my dad and aunt, and she’s the toughest woman I know. PPD doesn’t discriminate based on how together your life is. It doesn’t care if you live in a one-bedroom apartment or if you can sell out the Hollywood Bowl with Oprah singing along to your songs.
The idea that it “will be better this time” actually puts the responsibility on the mother: the one person who doesn’t really need to take on the pressure of meeting others’ expectations about her own mental health. Instead, if you have a friend who is going through the postpartum journey again, maybe it would be better to just say, “I’m here to support you, no matter what.” Even just an honest “how are you doing?” can be quite effective; you’d be surprised how many people are afraid to ask the simple questions when it comes to mental health .
Part of my mental health journey has been about giving myself permission to talk about it more openly, and not feel shame around admitting that I’m struggling.
Because at the end of the day, that’s the real reason for how “it will be different this time.” It’s going to be different because hopefully your village will show up and be there with you in the discomfort. And if they won’t, you don’t have to take that on either. That’s what a great PMAD therapist is for. Your journey is yours alone, and you don’t owe anyone anything other than taking care of yourself and your own family.
I’ve been battling with suicidal thoughts and depression since I was about 17 years old. It’s been a hard topic to discuss with my family, especially with my mom, who I feel comfortable sharing the good parts of my life with, but not always the bad. Part of my mental health journey has been about giving myself permission to talk about it more openly, and not feel shame around admitting that I’m struggling.
This past week on Instagram I posted a photo of a candle on my stories that read, “lighting an evening candle is really helping my seasonal depression.” A few hours later my mom called to inform me she had been gifted about a million holiday candles from school and that I could have a couple if I wanted to help fight my seasonal depression. She was being sincere with a hint of sarcasm, and it was perfect. It was the first time we talked about my depression casually, without any strings, and without me feeling any shame. It just was.
As I enter into the first few weeks postpartum I’ll be thinking about Cardi B, my nanny, my best friend Molly, and all those who’ve experienced PPD and survived. Who’ve gone on to work through their depression, become excellent mothers, and grow from their postpartum journeys. Parents who have taught me to hope, and love, and given me the courage to bring another child into the world again.
It will be better this time.
If you or someone you know is struggling with suicidal thoughts, call the National Suicide Prevention Lifeline at 800-273-8255 or text HOME to the Crisis Text Line at 741741.
Related Stories

4 simple things you can do to have a better hospital birth

10 celebrities who have shared their postpartum depression stories
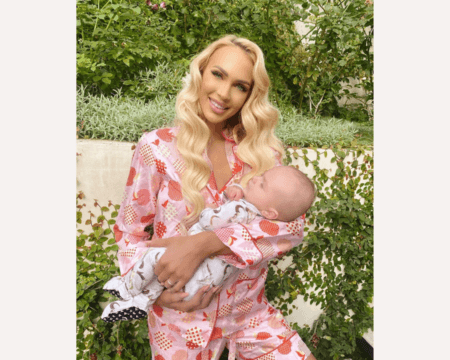
‘Selling Sunset’ star Christine Quinn says she had PPD while filming
Our editors also recommend....


My 10-year-old daughter asked if she was fat, and it gutted me

Toddler Health
To the worried mama whose child won’t eat enough—let go of expectations.

Mother’s Day without a mom is hard, but I don’t regret breaking up with my toxic mom

Real Feeding Stories from Real Mamas
Breastfeeding is a marathon and women’s bodies pay the price.

Motherly Stories
Having a second baby healed me.
The Concept of Postpartum Depression
Introduction, predisposing factors.
Postpartum depression (PPD) is a range of emotional and physical changes that the majority of new mothers go through. Immediately after delivery, mothers experience a sharp drop in hormones, and this chemical change may cause depression. Additionally, social and psychological changes that occur after getting a baby may cause this condition. One in every 10 new mothers experiences PPD (Chojenta, Lucke, Forder, & Loxton, 2016). Postpartum depression is a common condition involving psychological, emotional, social, and physical changes that many new mothers experience immediately after giving birth, but it is easily treated using medications and therapy. Postpartum depression is a common condition involving psychological, emotional, social, and physical changes that many new mothers experience immediately after giving birth, but it is easily treated using medications and therapy.
The common form of PPD is “baby blues,” which is mild and it affects almost every new mother. Normally, after delivery, new mothers are likely to experience sudden moods, which may lead to irritability, anxiety, loneliness, restlessness, and sadness. These changes may last for two weeks. PPD is prolonged and frequent baby blues’ symptoms with depressive characteristics, and it can occur several weeks or months after delivery. A new mother suffering from depressive symptoms should visit a health practitioner for treatment using medication and therapy. Postpartum psychosis is a severe form of PPD with full-blown symptoms of depression. New mothers suffering from this condition lose touch with reality together with having delusions, hallucinations, insomnia, agitation, and restlessness. Treatment is recommended using therapy and medications.
The common symptoms include mood changes, loss of appetite, and extreme fatigue, which are common signs after delivery. Other new mothers may experience loneliness, restlessness, agitation, and anxiety. In extreme cases where postpartum psychosis is involved, some individuals may experience symptoms such as suicidal thoughts, feelings of despair, and ineptitude, which are pointers to depression.
A new mother with a history of depression even before pregnancy is highly likely to suffer from PPD. Additionally, having many children may cause depression in new mothers, especially in cases where there is not enough financial support to take care of the kids (Chojenta et al., 2016). Young age at the time of pregnancy predisposes new mothers to PPD as they figure out how to deal with their new status. Finally, marital conflict and limited social or family support are risk factors because new mothers under such conditions lack the requisite backup that they need to deal with motherhood (Ghaedrahmati, Kazemi, Kheirabadi, Ebrahimi, & Bahrami, 2017).
Treatment depends on the type and severity of the condition. Psychotherapy is used to guide the patient on how to cope and overcome their depression and other related conditions. The commonly used drugs are antidepressants to alleviate depressive symptoms. In cases of psychosis, a patient may be admitted to a hospital, and antipsychotic drugs are used for treatment (Ghaedrahmati et al., 2017). Social support is also recommended as a coping mechanism.
Postpartum depression is a common condition affecting one in every ten new mothers, and it comes in different forms such as baby blues, PPD, and postpartum psychosis. Symptoms differ depending on the type of PPD being experienced. The main predisposing factors include a history of depression, age, marital conflict, and lack of social support. Treatment is done through psychotherapy and antidepressant medications. Antipsychotic drugs are used in cases of postpartum psychosis.
Chojenta, C. L., Lucke, J. C., Forder, P. M., & Loxton, D. J. (2016). Maternal health factors as risks for postnatal depression: A prospective longitudinal study. PLoS ONE, 11 (1), 1-9. Web.
Ghaedrahmati, M., Kazemi, A., Kheirabadi, G., Ebrahimi, A., & Bahrami, M. (2017). Postpartum depression risk factors: A narrative review. Journal of Education and Health Promotion, 6 (60), 1-21. Web.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2021, June 19). The Concept of Postpartum Depression. https://studycorgi.com/the-concept-of-postpartum-depression-essay/
"The Concept of Postpartum Depression." StudyCorgi , 19 June 2021, studycorgi.com/the-concept-of-postpartum-depression-essay/.
StudyCorgi . (2021) 'The Concept of Postpartum Depression'. 19 June.
1. StudyCorgi . "The Concept of Postpartum Depression." June 19, 2021. https://studycorgi.com/the-concept-of-postpartum-depression-essay/.
Bibliography
StudyCorgi . "The Concept of Postpartum Depression." June 19, 2021. https://studycorgi.com/the-concept-of-postpartum-depression-essay/.
StudyCorgi . 2021. "The Concept of Postpartum Depression." June 19, 2021. https://studycorgi.com/the-concept-of-postpartum-depression-essay/.
This paper, “The Concept of Postpartum Depression”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: June 19, 2021 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.

General Information:
The postpartum period.
During the postpartum period, about 85% of women experience some type of mood disturbance. For most the symptoms are mild and short-lived; however, 10 to 15% of women develop more significant symptoms of depression or anxiety. Postpartum psychiatric illness is typically divided into three categories: (1) postpartum blues (2) postpartum depression and (3) postpartum psychosis. It may be useful to conceptualize these disorders as existing along a continuum, where postpartum blues is the mildest and postpartum psychosis the most severe form of postpartum psychiatric illness.
Postpartum Blues
It appears that about 50 to 85% of women experience postpartum blues during the first few weeks after delivery. Given how common this type of mood disturbance is, it may be more accurate to consider the blues as a normal experience following childbirth rather than a psychiatric illness. Rather than feelings of sadness, women with the blues more commonly report mood lability, tearfulness, anxiety or irritability. These symptoms typically peak on the fourth or fifth day after delivery and may last for a few hours or a few days, remitting spontaneously within two weeks of delivery. While these symptoms are unpredictable and often unsettling, they do not interfere with a woman’s ability to function. No specific treatment is required; however, it should be noted that sometimes the blues heralds the development of a more significant mood disorder, particularly in women who have a history of depression. If symptoms of depression persist for longer than two weeks, the patient should be evaluated to rule out a more serious mood disorder.
Postpartum Depression
PPD typically emerges over the first two to three postpartum months but may occur at any point after delivery. Some women actually note the onset of milder depressive symptoms during pregnancy. Postpartum depression is clinically indistinguishable from depression occurring at other times during a woman’s life. The symptoms of postpartum depression include:
- Depressed or sad mood
- Tearfulness
- Loss of interest in usual activities
- Feelings of guilt
- Feelings of worthlessness or incompetence
- Sleep disturbance
- Change in appetite
- Poor concentration
- Suicidal thoughts
Significant anxiety symptoms may also occur. Generalized anxiety is common, but some women also develop panic attacks or hypochondriasis. Postpartum obsessive-compulsive disorder has also been reported, where women report disturbing and intrusive thoughts of harming their infant. Especially with milder cases, it may be difficult to detect postpartum depression because many of the symptoms used to diagnose depression (i.e., sleep and appetite disturbance, fatigue) also occur in postpartum women in the absence of depression. The Edinburgh Postnatal Depression Scale is a 10-item questionnaire that may be used to identify women who have PPD. On this scale, a score of 12 or greater or an affirmative answer on question 10 (presence of suicidal thoughts) raise concern and indicate a need for more thorough evaluation.
Postpartum Psychosis
Postpartum psychosis is the most severe form of postpartum psychiatric illness. It is a rare event that occurs in approximately 1 to 2 per 1000 women after childbirth. Its presentation is often dramatic, with onset of symptoms as early as the first 48 to 72 hours after delivery. The majority of women with puerperal psychosis develop symptoms within the first two postpartum weeks.
It appears that in most cases, postpartum psychosis represents an episode of bipolar illness; the symptoms of puerperal psychosis most closely resemble those of a rapidly evolving manic (or mixed) episode. The earliest signs are restlessness, irritability, and insomnia. Women with this disorder exhibit a rapidly shifting depressed or elated mood, disorientation or confusion, and erratic or disorganized behavior. Delusional beliefs are common and often center on the infant. Auditory hallucinations that instruct the mother to harm herself or her infant may also occur. Risk for infanticide, as well as suicide, is significant in this population.
Depression and Obsessive Compulsive Symptoms During the Postpartum Period
Despite several studies which have begun to demonstrate that maternal anxiety during pregnancy can negatively affect offspring neurodevelopment, little attention has been given to postpartum maternal anxiety both by clinicians and researchers. This may be because of the clinical overlap between depression and anxiety symptoms. Routine postpartum screening generally includes assessing symptoms of depression but anxiety disorders are often masked. Educating clinicians about postpartum anxiety can be very helpful for patients.
Recent studies show pregnancy and childbirth are frequently associated with the onset of the Obsessive Compulsive Disorder (OCD), one type of anxiety disorder. Some women do not have OCD but are bothered by obsessive-compulsive symptoms.
Miller and colleagues aimed to shed light on postpartum depression and anxiety, with and without obsessions, in their two recent studies (Miller, Hoxha, Wisner, & Gossett, 2015a , 2015b ).
A prospective cohort study of 461 women was performed to examine the phenomenology and the most common obsessive and compulsive symptoms present in postpartum women without a diagnosis of obsessive compulsive disorder (OCD). Of the 461 women included, 11.2% screened positive for OCD at 2 weeks postpartum, while 37.5% reported experiencing subclinical obsessions or compulsions. Both at 2 and 6 weeks, among the women who screened negative for OCD, the most commonly reported obsessions were aggression and contamination, and the most common compulsions were cleaning/washing, checking. Women with compulsions, with aggressive, religious and somatic obsessions and obsessions with symmetry were more likely to screen positive for OCD . Miller and colleagues’ data also showed that women with subclinical obsessions or compulsions were much more likely to be experiencing depression, as nearly 25% of these women also screened positive for depression.
In a secondary analysis of their prospective cohort study , Miller and colleagues examined the clinical course of postpartum anxiety and they confirmed the clinical overlap between postpartum anxiety and depression. A large number of women with postpartum depression had anxiety symptoms and obsessive-compulsive symptoms in the immediate postpartum period. At 2 weeks postpartum 19.9% of women with depression were more likely to experience comorbid state-trait anxiety, compared to 1.3% women who screened negative for depression. At both at 2 and 6 weeks postpartum, women with depression were more likely to report obsessions and compulsions compared to women without depression. While state-trait anxiety symptoms tended to resolve with time, obsessive-compulsive symptoms persisted. By 6 months postpartum, there were no differences in anxiety symptoms in women with and without depression, but the difference in obsessive-compulsive symptoms persisted (p=0.017). All this means severe distress for women and therapeutic implications for clinicians.
Given the potential adverse effects of untreated mood and anxiety symptoms on both the mother and child, careful screening and early recognition of anxiety symptoms during the postpartum period is recommended.
What Causes Postpartum Depression?
The postpartum period is characterized by a rapid shift in the hormonal environment. Within the first 48 hours after delivery, estrogen and progesterone concentrations fall dramatically. As these gonadal steroids modulate neurotransmitter systems involved in the regulation of mood, many investigators have proposed a role for these hormonal shirts in the emergence of postpartum affective illness. While it appears that there is no consistent correlation between serum levels of estrogen, progesterone, cortisol, or thyroid hormones and the occurrence of postpartum mood disturbance, some investigators hypothesize that there is a subgroup of women who are particularly sensitive to the hormonal changes that take place after delivery. This population of women may be more vulnerable to PPD and to other hormonally driven mood disturbances, such as those occurring during the premenstrual phase of the menstrual cycle or during the perimenopause.
Other factors may play a role in the etiology of PPD. One of the most consistent findings is that among women who report marital dissatisfaction and/or inadequate social supports, postpartum depressive illness is more common. Several investigators have also demonstrated that stressful life events occurring either during pregnancy or near the time of delivery appear to increase the likelihood of postpartum depression.
While all of these factors may act together to cause PPD, the emergence of this disorder probably reflects an underlying vulnerability to affective illness. Women with histories of major depression or bipolar disorder are more vulnerable to PPD, and women who develop PPD will often go on to have recurrent episodes of depression unrelated to pregnancy or childbirth.
Who is at Risk for Postpartum Depression?
All women are vulnerable to postpartum depression, regardless of age, marital status, education level, or socioeconomic status. While it is impossible to predict who will develop PPD, certain risk factors for PPD have been identified, including:
- Previous episode of PPD
- Depression during pregnancy
- History of depression or bipolar disorder
- Recent stressful life events
- Inadequate social supports
- Marital problem
Click here to read a 2005 blog post on risk factors for PPD.
Click here to read about obesity linked to postpartum risk.
Treatment for Postpartum Illness
Postpartum depression presents along a continuum, and the type of treatment selected is based on the severity and type of symptoms present. However, before initiating psychiatric treatment, medical causes for mood disturbance (e.g., thyroid dysfunction, anemia) must be excluded. Initial evaluation should include a thorough history, physical examination, and routine laboratory tests.
Non-pharmacological therapies are useful in the treatment of postpartum depression. In a randomized study it was demonstrated that short-term cognitive-behavioral therapy (CBT) was as effective as treatment with fluoxetine in women with postpartum depression. Interpersonal therapy (IPT) has also been shown to be effective for the treatment of women with mild to moderate postpartum depression. Not only is IPT effective for treating the symptoms of depression, women who receive IPT also benefit from significant improvements in the quality of their interpersonal relationships. Read this 2004 blog post and this 2007 post to learn more about CBT as a treatment option.
These non-pharmacological interventions may be particularly attractive to those patients who are reluctant to use psychotropic medications (e.g., women who are breast-feeding) or for patients with milder forms of depressive illness. Women with more severe postpartum depression may choose to receive pharmacological treatment, either in addition to or instead of these non-pharmacological therapies.
To date, only a few studies have systematically assessed the pharmacological treatment of postpartum depression. Conventional antidepressant medications (fluoxetine, sertraline, fluvoxamine, and venlafaxine) have shown efficacy in the treatment of postpartum depression. In all of these studies, standard antidepressant doses were effective and well tolerated. The choice of an antidepressant should be guided by the patient’s prior response to antidepressant medication and a given medication’s side effect profile. Specific serotonin reuptake inhibitors (SSRIs) are ideal first-line agents, as they are anxiolytic, non-sedating, and well tolerated. For women who cannot tolerate SSRIs, bupropion (Wellbutrin) may be an alternative; although one pilot study suggests bupropion may not be as effective as SSRIs. Tricyclic antidepressants (TCAs) are frequently used and, because they tend to be more sedating, may be more appropriate for women who present with prominent sleep disturbance. Given the prevalence of anxiety symptoms in this population, adjunctive use of a benzodiazepine (e.g., clonazepam, lorazepam) may be very helpful.
Puerperal psychosis is considered a psychiatric emergency that typically requires inpatient treatment. Acute treatment with either typical or atypical anti-psychotic medications is indicated. Given the well-established relationship between puerperal psychosis and bipolar disorder, postpartum psychosis should be treated as an affective psychosis and a mood stabilizer is indicated. Electroconvulsive therapy (ECT) is well tolerated and rapidly effective for severe postpartum depression and psychosis.
Using Medications While Breastfeeding
The nutritional, immunologic and psychological benefits of breastfeeding have been well documented. Women who plan to breastfeed must be informed that all psychotropic medications, including antidepressants, are secreted into the breast milk. Concentrations in the breast milk appear to vary widely. The amount of medication to which an infant is exposed depends on several factors, including dosage of medication, rate of maternal drug metabolism, and frequency and timing of feedings (Llewelyn and Stowe).
Over the past five years, data have accumulated regarding the use of various antidepressants during breastfeeding (reviewed in Newport et al 2002). Available data on the tricyclic antidepressants, fluoxetine, paroxetine, and sertraline during breastfeeding have been encouraging and suggest that significant complications related to neonatal exposure to psychotropic drugs in breast milk appear to be rare. While less information is available on other antidepressants, there have been no reports of serious adverse events related to exposure to these medications.
For women with bipolar disorder, breastfeeding may be more problematic. First is the concern that on-demand breastfeeding may significantly disrupt the mother’s sleep and thus may increase her vulnerability to relapse during the acute postpartum period. Second, there have been reports of toxicity in nursing infants related to exposure to various mood stabilizers, including lithium and carbamazepine, in breast milk. Lithium is excreted at high levels in the mother’s milk, and infant serum levels are relatively high, about one-third to one-half of the mother’s serum levels, increasing the risk of neonatal toxicity. Exposure to carbamazepine and valproic acid in the breast milk has been associated with hepatotoxicity in the nursing infant.
Learn more in our Breastfeeding and Psychiatric Medication specialty area.
How to Prevent PPD
Although it is difficult to reliably predict which women in the general population will experience postpartum mood disturbance, it is possible to identify certain subgroups of women (i.e., women with a history of mood disorder) who are more vulnerable to postpartum affective illness. Current research indicates that prophylactic interventions may be instituted near or at the time of delivery to decrease the risk of postpartum illness. Several studies demonstrate that women with histories of bipolar disorder or puerperal psychosis benefit from prophylactic treatment with lithium instituted either prior to delivery (at 36 weeks gestation) or no later than the first 48 hours postpartum. For women with histories of postpartum depression, several studies have described a beneficial effect of prophylactic antidepressant (either TCAs or SSRIs) administered after delivery. Patients with postpartum psychiatric illness are offered a variety of services by clinicians with particular expertise in this area:
- Clinical evaluation for postpartum mood and anxiety disorders
- Medication management
- Consultation regarding breastfeeding and psychotropic medications
- Recommendations regarding non-pharmacological treatments
- Referral to support services within the community
Click here to read a blog post on the prevention of PPD.
For the latest information on postpartum psychiatric disorders, please visit our blog .
How do I get an appointment?
Consultations regarding treatment options can be scheduled by calling our intake coordinator at 617-724-7792.
If you are pregnant or planning pregnancy, you may be interested in enrolling in the National Pregnancy Registry. You may find more information on this registry here . To view the list of our other active studies please visit our research page .
References:
Miller ES, Hoxha D, Wisner KL, Gossett DR.The impact of perinatal depression on the evolution of anxiety and obsessive-compulsive symptoms. Arch Womens Ment Health . 2015
Miller ES, Hoxha D, Wisner KL, Gossett DR. Obsessions and compulsions in postpartum women without obsessive compulsive disorder. J Womens Health (Larchmt). 2015
Share This Post, Choose Your Platform!

PARTICIPATE IN RELATED RESEARCH
The national pregnancy registry for psychiatric medications:.

All pregnant women between the ages of 18-45 with a history of psychiatric illness are eligible to enroll in the registry.
The Postpartum Psychosis Project

Recruiting individuals who have experienced a psychotic episode within 6 months of a live birth, still birth, or Intrauterine Fetal Death that occurred within the past 10 years
MGHPDS Mobile App
Are you pregnant? Do you own a smart phone? Get the MGH Perinatal Depression Scale app.
RECENT RELATED POSTS

Allison Baker, MD on the Specialized Care of Pregnant and Postpartum Women with ADHD
MGH Center for Women's Mental Health 2024-02-29T08:58:53-04:00 February 28th, 2024 |
To better care for pregnant and postpartum mothers with ADHD, clinicians should understand the unique facets of ADHD in women, how symptoms change during pregnancy and the postpartum period, and how to help new parents make decisions around medication use and ADHD symptom management.

What is Dexmedetomidine? And Does it Prevent Postpartum Depression?
MGH Center for Women's Mental Health 2024-02-07T20:23:16-04:00 February 7th, 2024 |
Dexmedetomidine, an α2-adrenergic receptor agonist, shows promise in preventing postpartum depression, reducing symptoms and improving sleep and pain control in women with prenatal depression.

Is Postpartum Depression More Common in Women with Sensitivity to Hormonal Contraceptive?
MGH Center for Women's Mental Health 2024-02-05T19:00:48-04:00 February 6th, 2024 |
A history of hormonal contraception-associated depression may be associated with a higher risk for postpartum depression.

Validated Questionnaire May Improve Identification of Postpartum Women with Childbirth-Associated PTSD
MGH Center for Women's Mental Health 2024-01-08T16:28:02-04:00 January 9th, 2024 |
Childbirth-related PTSD is relatively common; routine screening with a survey of PTSD symptoms may identify women in need of specific PTSD interventions.

New Oral Drug Zuranolone (Zurzuvae) for Postpartum Depression is Now Available
MGH Center for Women's Mental Health 2023-12-28T10:16:03-04:00 December 28th, 2023 |
The FDA approves zuranolone, a new option for the treatment of PPD, a rapidly acting antidepressant with a good safety profile.

New Oral PPD Treatment Zuranolone Will Soon Hit the Market as Zurzuvae
MGH Center for Women's Mental Health 2023-11-12T20:34:27-04:00 November 13th, 2023 |
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Educ Health Promot
Postpartum depression risk factors: A narrative review
Maryam ghaedrahmati.
Reproductive Health Department Student Research Committee, School of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran
Ashraf Kazemi
1 Women's Health Research Center, School of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran
Gholamreza Kheirabadi
2 Behavioral Sciences Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
Amrollah Ebrahimi
Masood bahrami.
3 Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran
Postpartum depression is a debilitating mental disorder with a high prevalence. The aim of this study was review of the related studies. In this narrative review, we report studies that investigated risk factors of postpartum depression by searching the database, Scopus, PubMed, ScienceDirect, Uptodate, Proquest in the period 2000-2015 published articles about the factors associated with postpartum depression were assessed in Farsi and English. The search strategy included a combination of keywords include postpartum depression and risk factors or obstetrical history, social factors, or biological factors. Literature review showed that risk factors for postpartum depression in the area of economic and social factors, obstetrical history, and biological factors, lifestyle and history of mental illness detected. Data from this study can use for designing a screening tools for high-risk pregnant women and for designing a prevention programs.
Introduction
Postpartum depression is a debilitating mental disorder with a prevalence between 5% and 60.8% worldwide.[ 1 ] The intensity of feeling inability in suffering mothers is so high that some mothers with postpartum depression comment life as the death swamp[ 2 ] while nondepressed mothers see their baby's birth as the happiest stage of their life.[ 3 ] The disease manifests as sleep disorders, mood swings, changes in appetite, fear of injury, serious concerns about the baby, much sadness and crying, sense of doubt, difficulty in concentrating, lack of interest in daily activities, thoughts of death and suicide.[ 4 , 5 ] Feelings of hopelessness in severe cases of illness can threaten life and lead to suicide;[ 6 ] it is a factor that causes 20% of maternal deaths in the course after giving birth.[ 7 ] In addition, issues such as fear of harming the baby (36%), weak attachment to the baby (34%) and even, in extreme cases, child suicide attempts have been reported.[ 8 , 9 ] These symptoms have serious effects on family health.[ 10 ] Therefore, susceptible people need to be identified before delivery to receive proper care measures. However, the development of screening programs as well as designing evidence-based prevention programs requires principled collection of scientific documentations. However, systematic reviews were seen in the review of some available studies that have assessed the resources in explaining the therapeutic effects of selective serotonin reuptake inhibitors on postpartum depression[ 11 ] and cognitive behavioral therapies.[ 12 ] Review studies seem to be inadequate, which evaluate the social factors besides addressing biological and psychological factors, while for achieving sufficient knowledge to design screening and preventing programs, all the factors associated with postpartum depression need be evaluated together. Thus, this study aimed to evaluate risk factors for postpartum depression during pregnancy and afterward.
Materials and Methods
This was a review (narrative) study, in which literature in English and Farsi was evaluated using electronic search in databases of Scopus, PubMed, ScienceDirect, UpToDate, and Proquest in the time range returns between 2000 and 2015. Searching in the databases was made using key words of “postpartum depression” and “risk factors” or “predisposing factors” or “predictive factors” and “biological agents” or “social factors” or “pathophysiology” or “hormonal factors” or “lifestyle” and “pregnancy.” In assessing in the PubMed database, the keywords were selected in accordance with the MeSH system. Those articles were included in the study that had done research on risk factors and predisposing factors of postpartum depression, which were of cross-sectional, cohort, case–control, interventional, and review article types. In addition, the illness diagnosis basis in these articles was the diagnosis of depression within 4 weeks after giving birth to 1 year after delivery. The articles improper regarding the adequacy of sample size, research design, and statistical methods were excluded from the study.
In the initial evaluation of the articles titles, 200 paper abstracts were extracted and evaluated by two members of the research team in terms of inclusion criteria after removal the authors’ names. In case of nonagreement on the presence if inclusion criteria between the two evaluators, the articles abstract was given to the third evaluator whose opinion was determinant to include the article in the review. According to the articles arbitration, 74 papers were detected appropriate. Then, the full-texts of available articles were prepared. In case of articles with unavailable full text, correspondence was done with the authors to request them for sending the article's full text after explaining the purpose of the survey.
The articles were evaluated by three team members of the research in terms of inclusion criteria. In case of meeting the inclusion criteria, the article was reviewed and contents related to the subject were extracted. Thus, the main results of each study with the article's specifications under the relevant title were noted. After collecting, the material and content were categorized based on scientific content in their respective area subsets.
Results and Discussion
Articles’ assessment showed that the factors associated with postpartum depression can be classified in five domains of risk factors for psychiatric, obstetric risk factors, biological and hormonal risk factors, social risk factors, and lifestyle risk factors.
Psychological factors
Previous history of depression and anxiety is among the factors that are associated with a higher risk of postpartum depression. The relationship between postpartum depression and prior onset of depression has been reported in many studies,[ 13 , 14 ] which has been referred to as powerful factors in postpartum depression.[ 15 , 16 ] The occurrence of mental health disorders such as depression during pregnancy is a powerful factor in predicting postpartum depression.[ 17 ]
There is evidence in explaining these relationships suggesting that women with a positive history of depression are more susceptible to hormonal changes.[ 18 ] In support of this finding, it has reported that a history of moderate to severe premenstrual syndrome (PMS) is a factors affecting the onset of postpartum depression.[ 19 ] In women with severe PMS, the serotonin transport system will change while the serotonin transporter polymorphism area is associated with major depression.[ 20 ] High serotonin polymorphism may lead to tryptophan depletion and induction of postpartum major depression.[ 21 ]
In addition to previous depression history, negative attitude toward the recent pregnancy, number of life events,[ 18 ] and a history of sexual abuse in the past[ 22 ] were as predisposing risk factors of postpartum depression. Furthermore, the reluctance of the baby gender[ 13 ] and having low self-esteem with the impact on parenting stress[ 22 ] are factors that contribute in the development of postpartum depression.
Obstetric risk factors
Assessment the relationship between the number of delivery and postpartum depression has been associated with conflicting results. Mayberry et al . have reported postpartum depression is more prevalent in multiparous women than in nulliparous women[ 23 ] while the results of another study indicate a higher prevalence of the disease in nulliparous women.[ 16 ] Furthermore, in a study conducted by Matsin in 2013, on 86 participants within 6 weeks after delivery, it was found that having two or more children due to higher psychological burden is more likely to be associated with the occurrence of depression.[ 10 ] The discrepancies between the results of these studies suggest that the number of childbirth alone is not an independent factor for developing postpartum depression and the development of pathological conditions for the occurrence of the illness is caused by psychosocial conditions that the multiplicity of delivery creates for the women.
Risky pregnancy is also associated with an increased risk of postpartum depression. These risks include conditions that lead to performing emergency cesarean section or hospitalization during pregnancy. Postpartum complications[ 22 , 24 ] are also effective on the incidence of postpartum depression as much as during labor complications such as meconium passage, umbilical cord prolapse, and obstetric hemorrhages.[ 10 ] Mothers with the birth of an infant with a weight <1500 g are 4–18 times at risk for postpartum depression[ 25 ] more than others.
A mismatch between the expectations of mother and pregnancy events is as factors that affect the occurrence of depression. It has been reported that women with strong desire to have natural childbirth during the perinatal period whose delivery are done by caesarean section are more prone to risk for postpartum depression than others.[ 26 ] Spending the course of pregnancy in a natural state away from the excitements due to complications during pregnancy and preparedness for the delivery seem to be as conditions effective in the prevention of postpartum depression. Since it has been reported that the use of epidural anesthesia during childbirth, attending in childbirth preparation classes during pregnancy, and continued breastfeeding after childbirth were associated with a reduced risk of postpartum depression.[ 27 ] However, insomnia during pregnancy can lead to the risk of recurrent postpartum depression in women with a previous history of the disease.[ 28 ]
The inverse association between breastfeeding and postpartum depression shows that breastfeeding is associated with a reduction in the rate of postpartum depression. It has been reported that women exclusively breastfeed their infants in the first 3 months after childbirth show lower values of Edinburgh Postnatal Depression Scale.[ 29 ] In a study conducted by Hamdan and Tamim, it was found that breastfeeding during the first 4 months after delivery reduces the risk of postpartum depression.[ 30 ] Although no causal relationship has been established for the relationship between breastfeeding and postpartum depression, breastfeeding increases the interaction between mother and baby[ 31 , 32 ] and thereby may affect the health of the mother.
A relationship has been observed between low hemoglobin concentration at day 7 after delivery (<120 g/L) and postpartum depressive symptoms at day 28 after childbirth.[ 3 ] Furthermore, an effective correlation has been seen between homocysteinemia in the 1 st week and 6 weeks after delivery and depression. However, there is not enough evidence in this regard that postpartum anemia can cause postpartum depression or complications of pregnancy period associated with the postpartum anemia may lead to increased risk of the disease.
Biological factors
Young age during pregnancy increases the risk of depression. The highest level of depression has been reported in mothers aged 13–19 years[ 33 ] while the lowest rate has been seen in women with the age range of 31–35-year-old.[ 34 ] In a study conducted by Abdollahi et al . on 1950 women at 2–12 weeks after giving birth, it was found that increasing maternal age and maternal self-efficacy are associated with a reduced risk of postpartum depression.[ 35 ]
Studies show that glucose metabolism disorders during pregnancy are also as predisposing factors for postpartum depression so that it has been observed that women with higher blood glucose levels (mean of 120 vs. 114 mg/dl) after an hour after performing the glucose challenge test with 50 g of glucose were more at risk of postpartum depression than others.[ 36 ]
Serotonin and tryptophan levels in the blood are also known factors effective on depression. A study has shown a relationship between different serotonin transporter gene alleles and serotonin receptors with mood disorders and depression.[ 37 ] Serotonin is a monoamine neurotransmitter that is synthesized during an enzymatic route from amino acid tryptophan.[ 38 ] The amount of serotonin directly depends on the individual diet. The consumption of foods rich in protein reduces the amounts of tryptophan and serotonin in the brain while a carbohydrate snack has reverse effects.[ 38 ] In nutritional deficiencies, reduced brain tryptophan (a precursor of serotonin) up to 15% leads to increased depression scale rate of postpartum depression.[ 21 ]
Oxytocin also plays a key role in regulating emotions, social interactions, and emotional responses.[ 39 ] Higher levels of oxytocin in midpregnancy have been predictors of postpartum depression within less than the first 2 weeks after delivery.[ 40 ] Recent evidence suggests that oxytocin induces the activity of serotonin receptors[ 41 ] and reduces the response to stress. The intranasal oxytocin spraying has increased the duration of positive behaviors such as eye contact and possibility of emotions and feelings both in women and men.[ 42 ]
The role of estrogen has been also evaluated in the incidence of postpartum depression. Studies on animal models have shown that steroid and estrogen hormones are modulators of transcription from nervous neurotransmitters[ 43 ] and adjust the function of serotonin receptors.[ 44 ] This hormone causes the renewal of the generation of damaged neurons in brain and leads to the production of brain neurotransmitters.[ 45 ] In hypothalamus, estrogen also affects the neurotransmitters and regulates sleep and temperature. It has been observed that the fluctuations in this hormone or its absence is associated with depression.[ 45 ]
The role of corticotropin-releasing hormone in the regulation of steroid hormones and depression has been studied as well. In addition to hypothalamus, this hormone is also produced during pregnancy in placenta, uterus, and ovaries and regulates the pituitary-hypothalamus-adrenal axis for production of steroid hormones.[ 46 ] After delivery and expulsion of the placenta, dramatic drop of this hormone leads to reduced production of steroid hormones such as estrogen and leads to increased susceptibility to depression in the first 12 weeks after childbirth.[ 47 ] In addition to steroid hormones, some evidence has been reported suggesting the inverse association of free thyroxine levels and total serum thyroxine concentrations with symptoms of postpartum depression.[ 48 ]
Although the relationship between thyroid dysfunction and postpartum depression has not been certainly established, the disorder may cause postpartum depression in a subgroup of women.[ 18 ] According to a report, a positive thyroid peroxidase antibody test at 32 weeks of pregnancy will increase the risk of postpartum depression as 2–3 times.[ 49 ]
In addition to the association of some endogenous hormones with postpartum depression, cytokine network and inflammatory responses have been observed to be involved in the pathophysiology of depression as well.[ 50 ] Administration of cytokines such as interferon alpha and cytokine inducers such as lipopolysaccharides and typhoid vaccines have caused behavioral changes such as mood disorders, anorexia, fatigue, sleep disorders, and other temperamental mood swings, which overlap with depression symptoms.[ 51 ] Depressed women may develop postpartum psychoneuroimmunological disorder, which is caused by inflammatory response turmoil in the normal course of labor and delivery.[ 52 ] Some evidence of changes in the regulators of T-cells has also been observed in depressed women before delivery.[ 53 ] The mechanism of explaining the changes in T-cells in depression is unknown. However, it is observed that the T-cells develop apoptosis in depressed patients. One of the possible mechanisms of explaining T-cells apoptosis in depression is the increased activity of the immune system, especially depletion of their tryptophan. Tryptophan is an essential component for the proliferation of T-cells, and in an environment free of tryptophan, the T-cells undergo apoptosis process.[ 51 ]
In depressed patients, increased apoptosis in the T-cells along with decreased response to glucocorticoids will lead to decreased available T-cells and reduced the capacity of the brain in response to immunological stimuli.[ 51 ]
Social factors
Social support refers to emotional support, financial support, intelligence support, and empathy relations.[ 54 ] The role of social support in reducing postpartum depression has been demonstrated.[ 55 ] Reducing social support is the most important environmental factor in the onset of depression and anxiety disorders.[ 56 ] At the International Conference on Population and Development of the year, decision-making power at home and increased support of the partner have been considered as the most important solution to promote women's reproductive health.[ 57 ] The spouse sexual violence and other forms of domestic violence during pregnancy are seen as factors contributing to the incidence of postpartum depression.[ 58 ]
In addition to the women's relationship with family members and community, behaviors such as smoking during prenatal period, is of social factors associated with increased incidence of postpartum depression as 1.7 times.[ 59 ]
The simultaneous relationship between smoking and socioeconomic level and the relationship between socioeconomic level with depression complicate the association between smoking and postpartum depression. However, the physiological changes of pregnancy may seem as a stressful event for some mothers and lead to the onset of depression symptoms and start of smoking.[ 60 ]
Another social factor is employment status, especially professional careers, which have been associated with a reduced risk of postpartum depression.[ 61 ] However, education and low income are associated with the risk of postpartum depression.[ 36 , 62 ]
Among the factors related to lifestyle, factors of food intake patterns, sleep status, exercise, and physical activities may affect postpartum depression. It was observed that sufficient consumption of vegetables, fruits, legumes, seafood, milk and dairy products, olive oil, and a variety of nutritious may reduce postpartum depression as 50%.[ 63 ]
Vitamin B6 is effective in the production of serotonin from tryptophan as a cofactor. Therefore, the reduction of this vitamin may be involved in the process of postpartum depression.[ 64 ] In a study, the positive relation between the level of vitamin B2 absorption at week 21 of pregnancy and postpartum depression has been reported.[ 37 ] The results of an ecological study from 23 countries found that increased seafood consumption is associated with reduced risk of postpartum depression.
The results of an ecological study on 23 countries indicated that high docosahexaenoic acid levels and increased seafood consumption have been associated with reduced risk of postpartum depression.[ 65 , 66 ] This compound is found in fish oil.
Among the micronutrients, reduced intake of zinc and selenium is linked with the incidence of postpartum depression.[ 67 ] It was reported in a study that zinc applies its antidepressant by influencing the serotonin reuptake.[ 68 ] Selenium deficiency is likely to affect the postpartum depression by developing thyroid dysfunction.[ 69 ] Zinc is specifically found in red meat, grains, meat, and fish.
In addition to nutritional status, sleep status is among the factors influencing the risk of depression. Evidence shows that there is a relationship between less sleep and postpartum depression.[ 20 , 70 ] Furthermore, an effective relationship has been observed between the rate of fatigue and depression levels in days after delivery. Periods of severe sleep deprivation have been reported in depressed women after delivery.[ 20 ] Chronic sleep deprivation affects glucose metabolism, inflammatory processes, social communications, mental health, and the quality of life.[ 71 ] In addition, acute episodes of sleep deprivation affect the immune system and increase inflammatory markers such as interleukin-6 and tumor necrosis factor while these inflammatory factors have been seen more in women with postpartum depression.
There is also some evidence to suggest that exercise and physical activity have significant benefits in reducing depression symptoms, which are comparable with medicinal benefits.[ 72 ] Moderate physical activity in the third trimester of pregnancy has lowered the postpartum depression scale at 6 weeks after the delivery.[ 73 ]
A possible mechanism is the effect of exercise on mental conditions of women by increasing the endogenous opioids and endorphins, which improve the mental health. Exercise also increases self-confidence and will eliminate negative self-assessments caused by depression. In addition, exercise will help women focusing on the environment around and solving their problems.[ 74 ]
Biological factors and social factors create intertwined rings that each makes women prone to postpartum depression by affecting each other. According to the findings of this study, many biological and environmental factors, such as lifestyle-related factors, are involved in the incidence or prevention of postpartum depression through direct and indirect impact on the level of serotonin in the brain and its function. Furthermore, many environmental factors such as socioeconomic factors cause crisis conditions and postpartum depression through influencing the mental health during pregnancy. Therefore, postpartum depression prevention programs need to focus on individuals interpersonal relationships to reduce domestic violence and increase social protection in addition to modify the women's lifestyle and increase their ability to cope with the crisis conditions. Moreover, based on the results of this research, the postpartum depression predictor tools should focus on social factors and lifestyle in addition to physical health conditions of individuals.
Financial support and sponsorship
This study was supported by Isfahan University of Medical Sciences (Grant Number: 394313).
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This study is part of a research thesis proposal approved by the Isfahan University of Medical Sciences which was performed with financial support of the Research Council of the University.
Graduate Thesis Or Dissertation
Postpartum depression among adolescent mothers: examining and treating low-income adolescents with symptoms of postpartum depression public deposited.

- Postpartum depression (PPD) among adult women is a prevalent and impairing problem, with evidence suggesting risk of adverse consequences for mothers and their infants. Few studies have investigated the problems of PPD among adolescents; however, both the emergence during adolescence of increased risk for depression among girls compared to boys and the prevalence of adolescent pregnancy suggest that this is a topic worthy of increased attention. The present thesis examines correlates of adolescent PPD, as well as an intervention for low-income adolescent mothers with symptoms of PPD. Study 1 investigated the relationship between depressive symptom severity and potential individual vulnerability and social context factors among a sample of adolescent mothers (N=102). Results indicate that adolescent PPD symptoms are associated with the number of negative life events, perceived discrimination, deficits in social support, anxiety symptom severity, perceived stress, impaired bonding and deficits in interpersonal effectiveness and emotion regulation. The best fitting model from the stepwise regression analyses indicated that perceived stress and anxiety symptom severity were the best predictors of adolescent PPD symptom severity. Study 2 examined the feasibility and preliminary outcomes of a behavioral skills training group intervention, based on Dialectical Behavioral Therapy (DBT), among adolescents with PPD (N=24) recruited from both a public health parent education program and a specialty obstetrics clinic for adolescent mothers. Findings suggest the intervention was both feasible and associated with improvement in mental health and functional domains. Together these studies indicate that a number of domains are related to adolescent PPD symptoms, particularly anxiety symptom severity and perceived stress, and a DBT skills group may be effective in reducing symptoms of PPD, as well as other areas of difficulty for adolescent mothers.
- Kleiber, Blair Vinson
- Psychology and Neuroscience
- Dimidjian, Sona
- Park, Bernadette
- Arch, Joanna
- Mollborn, Stefanie
- University of Colorado Boulder
- perceived stress
- Dialectical Behavioral Therapy
- intervention
- behavioral skills
- Dissertation
- In Copyright
- English [eng]
Relationships
Call or Text the Maternal Mental Health Hotline
Parents: don’t struggle alone
The National Maternal Mental Health Hotline provides free, confidential mental health support. Pregnant people, moms, and new parents can call or text any time, every day.
Start a call: 1-833-TLC-MAMA (1-833-852-6262)
Text now: 1-833-TLC-MAMA (1-833-852-6262)
Use TTY: Use your preferred relay service or dial 711 , then 1-833-852-6262 .
Learn more about the Hotline
- Programs & Impact
- Focus Areas
- Maternal Health
- Strengthening Black Maternal Health
A Journey Through Postpartum Depression
Nicole Barnett's journey through postpartum depression demonstrates the strength to seek help and break down the stigma surrounding maternal mental health.
After welcoming her third child, Nicole Barnett found herself in a fog of exhaustion that seemed unshakeable. Parenting three children—a 5-year-old, a 3-year-old, and a newborn—was already difficult enough. But now she felt like she was walking underwater with a blindfold on and one hand tied behind her back. This was different—and this was unshakeable.

Nicole had been through the newborn stage before. She knew it would be hard, but something just didn’t feel right. She reached out to her obstetrician’s office and described what was going on. They immediately explained she might be going through postpartum depression, and could give her some medication to make her feel better.
“I just did not want to hear the phrase ‘postpartum depression.’ I was a clinical social worker and I knew, generally, what that meant—but it just sounded like a failure label to me in that moment. I just didn’t want to receive it. I felt like surely it was something else.”
Reluctant to accept the possibility of postpartum depression, she chose not to seek help. She feared not only stigma, but also worried that medication would prevent her from breastfeeding. As the weeks passed, Nicole’s condition worsened, and she went into a deeper level of depression and anxiety. The panic attacks and overwhelming sense of failure consumed her. She struggled to fulfill even the simplest tasks and started withdrawing from daily life. Once the fear of how this could interfere with her children's safety set in, she realized she needed help. With the support of her husband, she took the courageous step of seeking professional help, including medication. She also participated in therapy and a support group.
“I was afraid the medication was going to make me feel a false sense of happiness or a false me, but the nurse said, ‘It’s not going to make you feel false. It’s going to put you on an even keel. One day, you’re going to notice. You’re going to suddenly realize ‘oh, I’m back to myself again.’” I didn’t really believe her when she said it at that time. But it was true, I remember it happening clearly. I was at my oldest daughter’s kindergarten graduation, and I was so happy when I realized I was fully myself again. I was fully present, and the fog was gone, and I wasn’t in that constant state of sadness…and that was the beginning of my recovery.”

Looking back, she wishes she had not allowed fear and stigma to delay her recovery. Her journey through postpartum depression has taught her that strength lies not in suffering alone, but in reaching out for help when we need it most. She describes, “Not reaching out for help is simply hoping things will get better. Reaching out for help is actually taking the first step to make things better.”
Now, as a counselor for the National Maternal Mental Health Hotline , Nicole strives to impart this wisdom to others, particularly women of color who face unique challenges in getting mental health resources. Through her pain, she discovered her purpose in life: to offer hope and support to those navigating the rough waters of motherhood, one conversation at a time.

“My wish for other moms, especially for women of color, is to not let the stigma of depression, anxiety, or any type of mental health label keep you from getting the help that you need.” She continued, “You may be just experiencing stress. It may be just a pit in your stomach—like something just isn’t feeling quite right. If you want someone to talk to, reach out to the Hotline. The counselors will be able to speak with you, listen to your concerns, and share resources. You don’t have to have a diagnosed mental health condition to call the Hotline. We are there for pregnant and parenting people, their loved ones, their family members.”
Behavioral health conditions can affect us across our lives. And, according to data from Maternal Mortality Review Committees in 36 states, mental health conditions are the leading cause of pregnancy-related death. In 2021, 12.7% of women experienced postpartum depression symptoms following birth.
You’re not alone. It's normal to feel sad, anxious, tired, or overwhelmed during pregnancy and after childbirth. However, if these feelings last more than two weeks and affect daily tasks like self-care, it could be a sign of postpartum depression. The National Maternal Mental Health Hotline offers immediate support and can be reached by calling or texting 1-833-TLC-MAMA (1-833-852-6262) . TTY users can connect through 711 followed by the hotline number. The hotline provides free, confidential assistance 24/7, connecting callers with counselors who offer real-time help, information, and referrals in English, Spanish, and 60 other languages, ensuring everyone receives culturally sensitive support.
Be brave and reach out if you or a loved one needs help!

IMAGES
COMMENTS
Activity During Pregnancy and Postpartum Depression. Studies have shown that women's mood and cardiorespiratory fitness improve when they engage in moderate-intensity physical activity in the weeks and months after giving birth to a child. Complementary Therapy for Postpartum Depression in Primary Care. Thus, the woman faced frustration and ...
Postpartum depression is widely recognized as a significant health threat to the mother and the rest of the family, and thus to society, but the biggest threat is to the lifetime health prospects of the newborn infant. Given the health significance of postpartum depression, recent research about the risk factors for this condition, and ...
1. Our Experts. can deliver a custom essay. for a mere 11.00 9.35/page 304 qualified. specialists online Learn more. Depression is undeniably one of the most prevalent mental health conditions globally, affecting approximately 5% of adults worldwide. It often manifests as intense feelings of hopelessness, sadness, and a loss of interest in ...
This essay analyzes a clinical research article "Improving care for depression in obstetrics and gynecology: A randomized controlled trial" by Melville et al. Postpartum Depression, Prevention and Treatment. Postpartum depression is a common psychiatric condition in women of the childbearing age.
Essay grade: Excellent. 3 pages / 1375 words. Imagine being locked in a room, with no outside interaction, except for the rare conversations with a housemaid or husband. Add in a bout of postpartum depression and an overbearing husband to have the story of Jane, a woman in nineteenth-century America.
Postpartum depression occurs after a mother gives birth and her body changes mentally and physically (Prevatt & Desmarais, 2018). After a mother has given birth to her offspring, she begins to experience postpartum anxiety (Baylor, 2019). This often includes being easily irritated, poor diet, and some explosive emotions (Baylor, 2019).
A more recent article on peripartum depression is available.. Am Fam Physician. 2010;82(8):926-933 Patient information: See related handout on postpartum depression, written by the authors of this ...
Most new moms experience postpartum "baby blues" after childbirth, which commonly include mood swings, crying spells, anxiety and difficulty sleeping. Baby blues typically begin within the first two to three days after delivery, and may last for up to two weeks. Postpartum depression isn't a character flaw or a weakness.
Students and educators currently depend on technology to enhance and improve learning, how they engage, communicate, and interact with the instructors. E-Advising is one of the…. Postpartum Depression essay example for your inspiration. ️ 1023 words. Read and download unique samples from our free paper database.
Etiology. PPD can occur in females having depression and anxiety in any trimester of pregnancy. Risk Factors. Psychological: History of depression and anxiety, premenstrual syndrome (PMS), Negative attitude towards the baby, the reluctance of baby's gender, and history of sexual abuse are perpetual factors for developing postpartum depression. Obstetric risk factors: Risky pregnancy, which ...
Andrea Yates 'Postpartum Depression' By Andrea Yates. Postpartum Depression In 2001, Andrea Yates, a Texas mother, was accused of drowning her five children, (aged seven, five, three, two, and six months) in her bathtub. The idea of a mother drowning all of her children puzzled the nation. Her attorney argued that it was Andrea Yates' untreated ...
It will be better this time. If you or someone you know is struggling with suicidal thoughts, call the National Suicide Prevention Lifeline at 800-273-8255 or text HOME to the Crisis Text Line at 741741. In this postpartum depression essay, a mother shares her struggles with PPD with her first and second baby while pregnant with her second child.
Results: A total of 122 studies (out of 3712 references retrieved from bibliographic databases) were included in this systematic review. The results of the studies were synthetized into three categories: (a) the maternal consequences of postpartum depression, including physical health, psychological health, relationship, and risky behaviors; (b) the infant consequences of postpartum depression ...
Postpartum depression (PPD) is a range of emotional and physical changes that the majority of new mothers go through. Immediately after delivery, mothers experience a sharp drop in hormones, and this chemical change may cause depression. Additionally, social and psychological changes that occur after getting a baby may cause this condition.
Postpartum Depression has many underlying causes and cannot be narrowed down to one single factor. However, mental and physical changes after birth can definitely make an impact on the manifestation of PPD. Every woman experiences changes in their body after giving birth. However, the body changes come with hormone changes, and the hormones ...
Postnatal depression is also known as postpartum or perinatal depression. It is a more serious type of depression than the "baby blues". The baby blues, unless persistent, usually do not require treatment and are normal reactions to the hormonal changes and stress after delivery. It is thought that postnatal depression can occur at any time ...
The Postpartum Period. During the postpartum period, about 85% of women experience some type of mood disturbance. For most the symptoms are mild and short-lived; however, 10 to 15% of women develop more significant symptoms of depression or anxiety. Postpartum psychiatric illness is typically divided into three categories: (1) postpartum blues ...
Postpartum depression is a type of depression that happens after having a baby. It affects up to 15% of people. People with postpartum depression experience emotional highs and lows, frequent crying, fatigue, guilt, anxiety and may have trouble caring for their baby. Postpartum depression can be treated with medication and counseling.
Postpartum depression is a debilitating mental disorder with a high prevalence. The aim of this study was review of the related studies. In this narrative review, we report studies that investigated risk factors of postpartum depression by searching the database, Scopus, PubMed, ScienceDirect, Uptodate, Proquest in the period 2000-2015 published articles about the factors associated with ...
Few studies have investigated the problems of PPD among adolescents; however, both the emergence during adolescence of increased risk for depression among girls compared to boys and the prevalence of adolescent pregnancy suggest that this is a topic worthy of increased attention.
In 2021, 12.7% of women experienced postpartum depression symptoms following birth. You're not alone. It's normal to feel sad, anxious, tired, or overwhelmed during pregnancy and after childbirth. However, if these feelings last more than two weeks and affect daily tasks like self-care, it could be a sign of postpartum depression.
Postpartum depression is a major mental health disorder that can negatively affect both mother and baby. In addition, the COVID-19 pandemic associated with extreme measures of the lockdown had profound effects on humanity, increasing the rates of anxiety and depression, especially among women in the postpartum period. The aim of this study was threefold: to determine the prevalence of ...