- Search by keyword
- Search by citation
Page 1 of 41

Competency scale of quality and safety for greenhand nurses: instrument development and psychometric test
Guaranteeing nursing service safety and quality is a prioritized issue in the healthcare setting worldwide. However, there still lacks a valid scale to measure the quality and safety competencies of newly grad...
- View Full Text
Status and content of outpatient preoperative education for rectal cancer patients undergoing stoma surgery provided by Japanese wound, ostomy, and continence nurses: a cross-sectional study
Preoperative education can improve postoperative quality of life in patients undergoing stoma surgery. However, the prevalence and when, where, and how preoperative education is implemented are unclear. Theref...
Effects of nurses-led multidisciplinary-based psychological management in spinal surgery: a retrospective, propensity-score-matching comparative study
Patients in spine surgery often have emotional disorders which is caused by multi-factors. Therefore, a multidisciplinary and multimodal intervention program is required to improve emotional disorders during t...
Nurses’ perceptions of how their professional autonomy influences the moral dimension of end-of-life care to nursing home residents– a qualitative study
Over the years, caring has been explained in various ways, thus presenting various meanings to different people. Caring is central to nursing discipline and care ethics have always had an important place in nu...
Challenges of home care: a qualitative study
Despite countless benefits of home care, unfortunately, the variety and quality of services provided by homecare centers are uncertain. This study was conducted to explore of home care challenges.
A closer look: obsessive-compulsive symptoms among intern nurses amidst COVID-19 pandemic
The distinctive circumstances and socio-cultural context in Egypt make it crucial to explore the psychological well-being of intern nurses amid the COVID-19 pandemic, with a specific focus on obsessive-compuls...
Digital stress perception among German hospital nurses and associations with health-oriented leadership, emotional exhaustion and work-privacy conflict: a cross-sectional study
The use of digital information and communication technologies (ICT) can be accompanied by increased technostress for nursing staff, which in turn can be associated with health consequences. In addition, the us...
Dual mediating effects of anxiety to use and acceptance attitude of artificial intelligence technology on the relationship between nursing students’ perception of and intention to use them: a descriptive study
Artificial intelligence (AI)-based healthcare technologies are changing nurses’ roles and enhancing patient care. However, nursing students may not be aware of the benefits, may not be trained to use AI-based ...
Health characteristics and factors associated with transition shock in newly graduated registered nurses: a latent class analysis
Transition shock occurs at a vulnerable time in newly graduated registered nurses’ careers and has a clear impact on both newly graduated registered nurses’ productivity and patient recovery outcomes. Identify...
Nursing students’ attitudes toward intimate partner violence and its relationship with self-esteem and self-efficacy
Understanding nursing students’ attitudes toward Intimate Partner Violence (IPV) is pivotal because it may impact the care and support, they provide victims. This study aimed to explore nursing students’ attit...
A multi-country mixed-method study identifying the association between perceived ethical work climate and problems among critical care nurses
Given the grave ethical tension and dilemmas posed continuously which are aggravated in the intensive care unit context and its related caregiving provision, combined with their impact on critical care nurses’...
Radiation safety compliance awareness among healthcare workers exposed to ionizing radiation
In recent years, there has been a marked growth in the use of ionizing radiation in medical imaging for both diagnosis and therapy, which in turn has led to increased radiation exposure among healthcare workers.
Exploring nurses’ experiences of providing spiritual care to cancer patients: a qualitative study
This study aims to explore nurses’ experiences of delivering spiritual care in an oncology setting.
Development and effects of advanced cardiac resuscitation nursing education program using web-based serious game: application of the IPO model
The significant rise in cardiac arrest cases within hospitals, coupled with a low survival rate, poses a critical health issue. And in most situations, nurses are the first responders. To develop nursing stude...
Nurses’ perceptions, experience and knowledge regarding artificial intelligence: results from a cross-sectional online survey in Germany
Nursing faces increasing pressure due to changing demographics and a shortage of skilled workers. Artificial intelligence (AI) offers an opportunity to relieve nurses and reduce pressure. The perception of AI ...
Determination of nurses’ happiness, hope, future expectations, and the factors influencing them: a descriptive study that can guide policy development to prevent nurse migration*
The happiness and hopefulness of nurses are not only known that contribute to their emotional well-being but also professional creativity, improve the quality of nursing services and organizational performance...
Evaluation of a new concept to improve and organize clinical practice in nursing education: a pilot-study
Nursing students may experience clinical practice as unsafe due to the interactions with patients, fear of making mistakes, lack of clinical experience and supervision, which results in anxiety and stress. Thu...
Variability of clinical practice in the care of the second stage of labor among midwives in Spain
There are recommendations based on scientific evidence on care in the second stage of labor, but it is not known to what degree the professionals comply with these recommendations.
Study protocol for the development, trial, and evaluation of a strategy for the implementation of qualification-oriented work organization in nursing homes
Staffing ratios in nursing homes vary among the federal states of Germany, but there are no rational grounds for these variations. In a previous study, a new instrument for the standardized calculation of staf...
Outcomes of professional misconduct by nurses: a qualitative study
Professional misconduct by nurses is a critical challenge in providing safe quality care, which can lead to devastating and extensive outcomes. Explaining the experiences of clinical nurses and nursing manager...
Face-to-face versus 360° VR video: a comparative study of two teaching methods in nursing education
The practical sessions during skills laboratory simulation or clinical simulation are cores of nursing education. For this, different modalities have been devised to facilitate psychomotor skills learning. One...
Evaluating person-centered care in neurological outpatient care: a mixed-methods content validity study
Person-centered care (PCC) is gaining increased attention. PCC concerns the whole person behind the disease and can improve care for people with long-term conditions such as multiple sclerosis (MS) and Parkins...
Relationship between medication burden and medication experience in stable patients with schizophrenia: the mediating effect of medication belief
Individuals with schizophrenia require prolonged antipsychotic medication treatment. But more than 50% of individuals with schizophrenia experience adverse medication experiences during their antipsychotic tre...
Enhancing feedback by health coaching: the effectiveness of mixed methods approach to long-term physical activity changes in nurses. An intervention study
Although knowledge of the barriers and motivators to physical activity participation among nurses is increasing, the factors influencing motivation methods’ effectiveness are not completely defined. This study...
Individual and organizational interventions to promote staff health and well-being in residential long-term care: a systematic review of randomized controlled trials over the past 20 years
Staff in residential long-term care (RLTC) experience significant physical and mental work demands. However, research on specific interventions to promote staff health and well-being in RLTC facilities is limi...
Thriving at work as a mediator of the relationship between psychological resilience and the work performance of clinical nurses
This study aims to investigate the relationship between psychological resilience, thriving at work, and work performance among nurses, as well as analyse the mediating role of thriving at work in the relations...
The relationship between organizational dehumanization and work engagement: the mediating effect of nurses’ work stress
Organizational dehumanization has detrimental consequences for nurses’ wellbeing and leads to a stressful work environment. Moreover, it is very destructive to work engagement.
Job crafting, positive psychological capital, and social support as predictors of job embeddedness on among clinical nurses- a structural model design
This study establishes the relationships among role conflict, positive psychological capital, social support, job crafting, and job embeddedness among clinical nurses. The results are expected to provide a bas...
Inductive process of moral distress development in viewpoints from surgical nurses: a mixed-method study
Moral distress is a multifactorial and complex phenomenon influenced by various individual, cultural, and systemic factors. This study aimed to investigate the frequency and intensity of nurses’ moral distress...
Assessment of preventive practices towards hepatitis B infection among nursing students in Bangladesh: role of knowledge, attitudes and sociodemographic factors
Globally, hepatitis B infection (HBI) poses a substantial public health concern and healthcare workers, including nursing students, are at a higher risk of contracting this disease. Thus, the study aimed to as...
Assessment of patient safety culture in Moroccan primary health care: a multicentric study
Promoting patient safety is a critical concern for developing-countries health systems like Morocco. There is an increasing acknowledgment of the need to create a patient-centered culture with the aim to decre...
Stressors, emotions, and social support systems among respiratory nurses during the Omicron outbreak in China: a qualitative study
Respiratory nurses faced tremendous challenges when the Omicron variant spread rapidly in China from late 2022 to early 2023. An in-depth understanding of respiratory nurses’ experiences during challenging tim...
Analysis of cybersickness in virtual nursing simulation: a German longitudinal study
Innovative educational approaches such as simulation-based nursing education using virtual reality (VR) technologies provide new opportunities for nursing education. However, there is a lack of information on ...
Prevalence and characters of post-acute COVID-19 syndrome in healthcare workers in Kashan/Iran 2023: a cross-sectional study
Post-acute COVID-19 syndrome that is called long COVID-19 consists of the symptoms that last more than 12 weeks with no other explanation. The present study aimed to determine the prevalence, frequency of symp...
Exploring advanced clinical practitioner perspectives on training, role identity and competence: a qualitative study
Advanced Clinical Practitioners (ACPs) are a new role that have been established to address gaps and support the existing medical workforce in an effort to help reduce increasing pressures on NHS services. ACP...

Improvement and implementation of central sterile supply department training program based on action research
This study aimed to improve and implement the central sterile supply department (CSSD) training program through action research and to evaluate its effect.
Translation and psychometric evaluation of the Persian version of the nurses’ quality of life scale: a validation study in Iran
The quality of life for nurses can be significantly impacted by various occupational factors that Influence their working conditions and professional performance. The current study aimed to translate and valid...
Cultural sensitivity and associated factors among nurses in southwest Ethiopia: a cross-sectional study
Because of the rapidly rising cultural diversity, the ability to recognize cultural diversity is extremely important to all healthcare professionals, especially to nurses. However, there is a paucity of inform...
Nurses’ motivation for performing cardiopulmonary resuscitation: a cross-sectional study
Nurse motivation can have a significant impact on the quality of cardiopulmonary resuscitation and the patients’ survival. Therefore, the present study aimed to examine nurses’ motivation for performing cardio...
The biosafety incident response competence scale for clinical nursing staff: a development and validation study
This study was designed to develop a biosafety incident response competence scale and evaluate its validity and reliability among clinical nurses.
Acceptance of a robotic system for nursing care: a cross-sectional survey with professional nurses, care recipients and relatives
The end-users’ acceptance is a core concept in the development, implementation and evaluation of new systems like robotic systems in daily nursing practice. So far, studies have shown various findings concerni...
Mediating effect of psychological capital on the relationship between mental health literacy and coping styles among newly recruited nurses
Newly recruited nurses face multiple sources of stress and their coping styles need to be focused on to ensure good mental health. This study aimed to examine the relationship among mental health literacy, psy...
Challenges to the delivery and utilisation of child healthcare services: a qualitative study of the experiences of nurses and caregivers in a rural district in Ghana
Sub-Saharan Africa has one of the poorest child health outcomes in the world. Children born in this region face significant health challenges that jeopardise their proper growth and development. Even though th...
Pharmacological labour pain interventions: South African midwives’ perspective
Women of childbearing age feel great about giving birth, but the pain could be excruciating depending on their pain tolerances. Midwives requires obstetrical knowledge and skills such as pain management during...
Prevalence of medication errors and its related factors in Iranian nurses: an updated systematic review and meta-analysis
Nurses may make medication errors during the implementation of therapeutic interventions, which initially threaten the patient’s health and safety and prolong their hospital stay. These errors have always been...
The impact of mentorship program on the level of anxiety and pre-internship exam scores among Iranian senior nursing students
Mentorship involves a voluntary, collaborative, and non-hierarchical relationship where an experienced individual shares knowledge with a less-experienced individual. This study aimed to evaluate the effects o...
Compassionate care during the COVID-19 pandemic
There was a substantial documented call for healthcare professionals to provide compassionate care during the COVID-19 pandemic and significant criticism voiced when it was lacking. This study aimed to explore...
Measuring the quality of transitional care based on elderly patients’ experiences with the partners at care transitions measure: a cross-sectional survey
The quality of transitional care is closely related to the health outcomes of patients, and understanding the status of transitional care for patients is crucial to improving the health outcomes of patients. T...
Knowledge, attitudes, and practices toward Patient Safety among nurses in health centers
To assess knowledge, attitudes, and practices (KAPs) toward patient safety among nurses working at primary and comprehensive health care centers in Jordan; to identify factors that predict KAPs among nurses.
Missed nursing care and its relationship with nurses’ moral sensitivity: a descriptive-analytical study
Missed care rates are an indicator of healthcare quality. Missed nursing care can reduce patient safety and lead to adverse events. Moral sensitivity enables nurses to interpret and respond to clients’ needs a...
Important information
Editorial board
For authors
For editorial board members
For reviewers
- Manuscript editing services
Annual Journal Metrics
2022 Citation Impact 3.2 - 2-year Impact Factor 3.6 - 5-year Impact Factor 1.428 - SNIP (Source Normalized Impact per Paper) 0.769 - SJR (SCImago Journal Rank)
2023 Speed 26 days submission to first editorial decision for all manuscripts (Median) 161 days submission to accept (Median)
2023 Usage 3,633,213 downloads 785 Altmetric mentions
- More about our metrics
Peer-review Terminology
The following summary describes the peer review process for this journal:
Identity transparency: Single anonymized
Reviewer interacts with: Editor
Review information published: Review reports. Reviewer Identities reviewer opt in. Author/reviewer communication
More information is available here
- Follow us on Twitter
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

Answers: Health Sciences Library
How can i find a scholarly article written by a nurse.
Using CINAHL Complete (click the word Database under the title to access CINAHL), there are four ways to limit your results to scholarly articles written by nurse(s):
1) First Author is Nurse *
2) Any Author is Nurse *
If those do not work, try the Journal Subset **, or the Author Affiliation AF .**
1) First Author is Nurse * limiter is available in the Limit Your Results menu beneath the Advanced Search screen. To use, simply tick the First Author is Nurse box, enter your search terms at the top, and click the Search button.
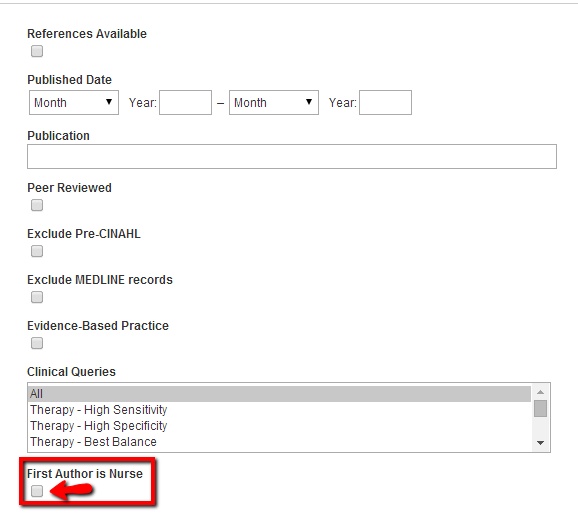
The first author is generally the person claiming most responsibility for the research in most scientific publishing. So, an article in which the first-named author is a nurse has a higher probability of reflecting nursing research interests.
*The written by a nurse limiter applies to records from November 2009 - present. Credentials include RN, BSN, MSN, or appropriate degree. For non-U.S. journals, the credentials include licensed nurse or appropriate nursing degree in the particular country.
2) The Any Author is Nurse * limiter is also located in the Limit Your Results menu. Simply tick the Any Author is Nurse box, enter your search terms in the search box, and click the Search button.
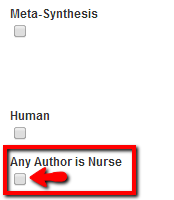
The Journal Subset ** is located immediately below the Any Author is Nurse limiter. Scroll through the list of journal subsets; find and select the Nursing subset. Enter your search terms and click the Search button.
Journal Subset restricts your search to the nursing databases, filtering out other allied health discipline journals. We're assuming that nursing authors will likely publish more in nursing journals than other health science disciplines. This strategy will give you broader results than limiting by nurse author(s).
**While the logic is sound, the assumption is not foolproof. Verify the author's nursing credentials by checking the author information in the article.
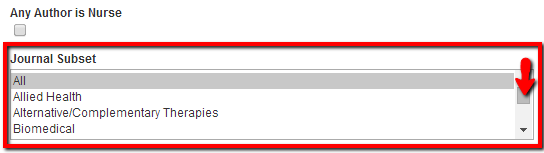
AF Author Affiliation** is available in the dropdown menu next to the search box.
To search by AF Author Affiliation , click the Select a Field (optional) dropdown menu next to the first search box. Find and select AF Author Affiliation . Type nurs* into the adjacent search box, enter your specific keywords in the search box below, then click the Search button.
Many nurse scholars teach at or are associated with departments of nursing in institutions of higher learning, and the word "nursing" is frequently included in the department heading. In most cases, the affiliated author will be a nurse.
**The assumption is not foolproof. Verify the author's nursing credentials by checking the author information in the article.
Links & Files
- Nursing Research Guide
- Last Updated May 10, 2018
- Answered By Kenneth Haggerty
FAQ Actions
- Share on Facebook
Comments (0)
Finding Research Articles in PubMed and CINAHL
Finding nursing authors in cinahl plus, finding son authors in pubmed.
To find articles authored by nurses in CINAHL Complete :
After entering your search topic, under Limit Your Results, click on either:
- First Author is Nurse: If you apply this limit, you will only retrieve records where it is confirmed that the first author of an article is a nurse, according to credentials noted in the article.
- Any Author is Nurse: If you apply this limit, you will only retrieve records where at least one author is a nurse, according to the credentials noted in the article.
NOTE: The written by a nurse limiters apply only to records from November 2009 and forward.
To find articles authored by University of Washington nurses:
After entering your search topic, in the second Search box enter University of Washington and change the drop-down menu to: AF Author Affiliation.
When checking your Results, look at the Affiliation field to see if author is from the UW School of Nursing.
To find articles authored by University of Washington School of Nursing faculty in PubMed :
Use the AD Address field.
Add the following to your search topic: nursing [ad] AND "university of washington" [ad]
Example: irritable bowel syndrome AND nursing [ad] AND "university of washington" [ad]
- << Previous: CINAHL
- Next: APA Style >>
- Last Updated: Jun 22, 2023 1:19 PM
- URL: https://guides.lib.uw.edu/hsl/nmeth403
Be boundless
1959 NE Pacific Street | T334 Health Sciences Building | Box 357155 | Seattle, WA 98195-7155 | 206-543-3390
© 2024 University of Washington | Seattle, WA

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int Wound J
- v.15(1); 2018 Feb
Wound care evidence, knowledge and education amongst nurses: a semi‐systematic literature review
1 School of Health, Nursing and Midwifery, University of the West of Scotland, Paisley Scotland
The aims of this study were to determine the knowledge and skills of nurses involved in wound care, to provide a critical overview of the current evidence base underpinning wound care and to determine the extent of utilisation of existing evidence by nurses involved in the management of wounds in practice.
A semi‐systematic review of the literature was undertaken on Cinahl, Medline Science Direct and Cochrane using the search terms: wound, tissue viability, education, nurse, with limitations set for dates between 2009 and 2017 and English language.
Shortfalls were found in the evidence base underpinning wound care and in links between evidence and practice, prevalence of ritualistic practice and in structured education at pre‐ and post‐registration levels.
The evidence underpinning wound care practice should be further developed, including the conduction of independent studies and research of qualitative design to obtain rich data on both patient and clinician experiences of all aspects of wound management. More structured wound care education programmes, both at pre‐registration/undergraduate and professional development levels, should be established.
Introduction/background
The presence of a wound represents a considerable burden in terms of economic cost to health and social care providers and impact on patient quality of life (QoL). This is notably so for chronic wounds, the definition of which has not been universally agreed upon but is generally accepted to refer to wounds that do not follow the normal stages of healing and in which healing is consequently delayed 1 . Whilst chronic wounds were previously estimated to cost the National Health Service (NHS) between £2·5 and £3 billion p/a 2 , more recent data propose that the annual cost to manage wounds and associated comorbidities is between £4·5 and £5·1 billion 3 . In addition, Augustin et al. 4 found living with a wound to have a negative multifactorial impact on psychosocial health and well‐being. This impact is recognised to be worsening with changing demographics and a population that is living longer with multiple comorbidities and chronic conditions 5 . In the UK, the increasing decentralisation of health and social care means that the majority of the burden lies within the community setting where district nurses (DNs) and other community health and social care providers are responsible for wound management 6 . Indeed, wound care represents between 35% and 65% of community nurses' caseloads ( 7 , 8 ), which has significant implications for an increasingly overstretched and pressurised DN work force 6 , 9 , 10 .
The effective management of chronic wounds is complex, and in order to maximise outcomes for patients, it is recommended that those involved in their care and treatment should have the appropriate knowledge and skills (European Wound Management Association 11 , 12 . This includes an understanding of the anatomy and physiology of tissue repair and aetiology and also knowledge pertaining to the selection of appropriate products and interventions to support the achievement of positive outcomes. The most obvious of these is wound closure, which is reflected in the frequency with which it is measured in studies 12 ; however, those relating to patient QoL are increasingly regarded with equal importance as wounds negatively impact all aspects of an individual's life, and complete closure is not always the ultimate goal of care (e.g., in palliative care patients for whom maximisation of comfort and dignity often takes precedence over healing) 13 . Despite this, little is known about nurses' knowledge and skills in wound care, both in relation to formal evidence and education and that which is from gleaned from experiential learning and clinical practice 14 , 15 . There is also debate surrounding the quality of evidence, which seeks to confirm the proposed effectiveness of particular types of wound treatments and products and factors influencing their selection 5 , 16 . A significant shortfall of this evidence is that it is largely driven and funded by industry, which may have potential methodological and ethical implications. It is therefore crucial that a more developed understanding of the evidence base underpinning the care of wounds and its role in shaping nurses' knowledge, education and clinical practice is achieved so that outcomes can be maximised.
The aim of this literature review is to provide a critical overview of the current evidence base underpinning wound care and the extent of utilisation of existing evidence by nurses involved in the management of wounds in practice. It will also seek to determine the knowledge and skills of nurses in relation to wound care and the sources from which it arises, including those that are formal (i.e. empirical evidence and structured education) and those that are informal (i.e. experiential, clinical practice and knowledge gleaned from colleagues).
Search strategy
An initial literature search was carried out in February 2017 on health care and scientific databases, including Cinahl, Medline, Cochrane,; Science Direct and PubMed, with the following key words singularly and in various combinations: Wound*, knowledge, nurs*, tissue viability, evidence, education.
Inclusion criteria were as follows: original research studies with no restrictions on design or methodology, English language, date of publication between 2009 and 2017 to source contemporary literature and all age groups.
Exclusion criteria were as follows: review papers, publications in languages other than English, date of publication before 2009, publications not fitting specified methodologies, publications focusing upon specialist or novel approaches to wound management, studies published with industry support and funding and studies focussing on specific or specialist wound care skills and practice.
The original search yielded 201 papers, which were filtered to 193 with the removal of duplicates; 193 papers were screened, with 104 excluded by title and abstract, and a further 84 excluded following review of full text and reference lists. An additional search on Google Scholar was carried out, but no further studies were identified. Saved searches were re‐run on a weekly basis until March 2017, but no new studies were identified, leaving a final total of five papers that fit the inclusion criteria (Figure (Figure1 1 ).

Search strategy algorithm. PRISMA 35 .
To assist with structured methodological appraisal, a summary table was used (Table (Table1). 1 ). An appraisal tool was adapted from the Critical Appraisal Skills Programme (CASP) for quantitative studies to support the critique of each study using the checklist approach that is recommended by the Centre for Reviews and Dissemination 17 .
Summary appraisal table
Key findings
The findings of the literature review highlighted a number of shortfalls and limitations pertaining to wound care knowledge and practice, with the following common sub‐themes emerging:
- Limitations in the evidence base pertaining to wound care, including the domination of studies published for corporate interest;
- Poorly developed links between evidence and wound care in practice;
- Recognition of insufficient wound care knowledge amongst nurses;
- The frequency of ritualistic and historic practice;
- Recognition of the need for more structured wound care education programmes for nurses at pre‐ and post‐registration levels.
A number of generic ontological and methodological limitations were identified with the evidence sourced – most notably that all studies took a similar post‐positivist approach, adopting descriptive and quantitative methodologies. A key and significant flaw is, therefore, the absence of studies underpinned by a constructivist or interpretivist paradigm and an overlooking of knowledge formation from contextual, individualistic and socially developed perspectives 18 . This might be contested to particularly misalign with the ethos of the nursing profession, which is embedded in person centeredness and holism 19 . The absence of studies adopting a qualitative design also overlooks the importance of rich contextual data, for example, that pertaining to nurses' views on their wound care knowledge and patients' lived experiences of having a wound 18 . The uniform choice of questionnaire and survey design methods considerably limit the variety of data that shape the resulting evidence base and may not accurately represent wound care in the practice setting, particularly because all studies relied upon data that was self‐reported.
In terms of methodological weakness, only one study utilised a validated tool to collate data, whilst a number of the sample sizes were small, with only one study completing a power calculation and others having relatively poor participant response rates. For the majority of studies, the approach to sampling was convenience, which may not have led to results reflective of wider nursing practice. No studies declared whether researchers had been previously known to participants and in what capacity, which could have contributed to a researcher effect 20 . This is considered to be an important factor in maintaining reliability in studies of positivist, realist and, to a lesser degree, post‐positivist ontology as contextual factors, including relationships between researchers and participants, should be highly controlled 20 . Finally, four of the studies used participants from only acute clinical settings, which limits the generalisability of the findings to wider areas of practice. This is particularly relevant in the UK where the majority of wound care is carried out in the community setting and may consequently account for community nurses having more developed skills in wound management 6 . However, the representation of wound care practice in a variety of geographical settings might be argued to shape a global perspective and enable useful comparisons to be made.
Each of the emergent themes will now be explored in succession.
Evidence in wound care
Nursing has been historically criticised for the absence of a distinct profession‐specific evidence base, instead borrowing on those from professions such as medicine and the social sciences 21 . To some extent, the academisation and move from an apprenticeship model to a higher education model has raised the profile of the profession in this capacity; however, there is still a reluctance amongst nurses to fully embrace evidence‐based practice (EBP), most notably within the clinical context 22 . This trend has been particularly visible within wound care, which has been argued to lag behind other areas of practice due to the lack of robust empirical evidence 23 . All five of the publications reviewed acknowledged this shortfall and the need to establish a more scientific evidence base 23 , 24 , 25 , 26 , 27 . Whilst national clinical guidelines, such as those produced by National Centre for Health and Care Excellence (NICE) in the UK, employ strict criteria for development (e.g., the underpinning of empirical evidence that is high on the hierarchy of evidence such as clinical trials), it was also recognised that, within wound care, nurses often rely upon evidence that is lower on the traditional hierarchy to shape practice 26 . This was particularly noted in relation to a lack of evidence supporting the efficacy of specific dressings 26 . However, although empirical evidence was widely agreed to be a crucial component of EBP in relation to wound care, additional types of knowledge, such as that gleaned from informal sources (i.e., experience, clinical practice and learning through colleagues), were also recognised to be important 23 , 24 , 25 , 26 , 27 . Indeed, the Centres for Disease Prevention and Control [CDC] in the USA applies a combination of empirical evidence, theoretical knowledge and contextual knowledge to shape each of its recommendations 26 , which supports an increasing awareness of the role of informal sources of knowledge in EBP. Dugdall and Watson 23 additionally recognised shortfalls in evidence pertaining to the management of wounds for specific patient groups (e.g. paediatrics and neonates) and a subsequent need to adopt evidence from studies conducted on adults to shape practice. However, it should be noted that this challenge is not unique to wound care as it is ethically problematic to carry out trials using paediatric and neonatal participants in all areas of practice 28 . A final factor is that much wound care research is supported by industry, leading to potential conflicts of interest in relation to overall corporate aim and the opportunity for ethical misconduct.
Poorly developed links between evidence and practice
All five of the studies either directly or indirectly identified poor links or barriers to the implementation of EBP. Although McCluskey and McCarthy 27 recognised the importance of informal sources of knowledge, such as experiential learning and intuition, in shaping competence in wound care practice, the lack of a structured approach and barriers to the implementation of EBP were also identified. As such, nurses' knowledge was, in some cases, found to be sufficient, but poor application negatively affected competence in practice. Gillespie et al . 26 also recognised the role of experiential knowledge but found gaps between knowledge and practice and a failure of nurses to apply recommendations made by national clinical guidelines, whilst a high number of respondents in deFaria et al . 24 and Ferreira et al . 25 reported a lack of awareness of the existence of local protocols or guidelines pertaining to wound care in their clinical area at all. Dugdall and Watson 23 found statistically significant correlations between positive attitudes to EBP and a specific tissue viability role ( P = 0·002), a first degree ( P = 0·001) and a formal tissue viability qualification ( P = 0·001), which suggests that EBP is more positively received by those with structured education. However, shortfalls in partnerships and integration between higher education/academic institutions and clinical sectors were also noted, which are also recognised to negatively affect the implementation of EBP in the practice setting 23 , 24 .
Inadequate wound care knowledge amongst nurses
Nurses' knowledge in wound care was addressed by five of the studies, all of which acknowledged an insufficiency to some degree. deFaria et al . 24 and Ferreira et al . 25 noted a clear deficit in knowledge in a number of areas pertaining to wound care (e.g. pressure ulcer grading, awareness of clinical guidelines/protocols, dressing selection etc.), although it should be noted that both studies were conducted in the same acute hospital in Brazil, which may identify shortfalls pertaining to the particular setting rather than to nursing in the wider sense. McCluskey and McCarthy 27 found that whilst wound care knowledge was sufficient to inform practice overall and somewhat better than reported in a number of previous studies, this was distinct from competence, which was often negatively affected by nurses' poor application of knowledge in the clinical setting. This was supported by Gillespie et al . 26 who found that despite having a good theoretical knowledge of wound assessment, Australian nurses working in the acute sector demonstrated similar poor links between knowledge and practice and poor application of clinical guidelines. Dugdall and Watson 23 was the only study that did not explicitly explore knowledge; however, they did identify a link between higher and specialist wound care education and a positive attitude to EBP, which subsequently led to better wound care practice. Although findings from some of the studies also suggested that nurses often lack product‐specific knowledge, which is required to make evidence‐based decisions in the selection of dressings 24 , 26 , in other studies, some participants reported a degree of confidence in product selection 25 . deFaria et al . 24 found that 70% of respondents attested that there were no wound care guidelines or standards in their area of practice, whilst a further 6% were unable to respond due to lack of information. When questioned about their level of professional autonomy in the selection of wound care products, 63% also stated that authorisation from the doctor was required in this capacity. This is in contrast to the UK where nurses historically take the lead in the management of wounds; however, although this might be argued to be reflective of differences in the organisational and professional hierarchies in health care, nurses from those studies carried out in other areas also reported some lack of knowledge, which reveals a potential deficit in a range of geographical settings 26 , 27 . Finally, only McCluskey and McCarthy 27 explored the nature and types of knowledge nurses apply to shape wound care practice, including those that are empirical, formal and explicit and also those that are tacit, informal and contextual, the latter of which were perceived to be linked to competence and experiential learning in practice.
Ritualistic and historic practice in wound care
Four of the studies attributed much wound care practice to derive from historic and ritualistic practices ( 23 , 24 , 25 , 26 ). Ferreira et al . 25 reported that wound care practice was rooted in tradition and myth; with Gillespie et al . 26 using the concept of the “sterile field” as an example of wound care practice, which is ritualistic rather than underpinned by evidence. Gillespie et al . 26 and McCluskey and McCarthy 27 both acknowledged the contextual and individualised nature of knowledge applied to wound care practice and a lack of standardisation that varied both within and between organisations. Dugdall and Watson 23 attributed this partly to the increasing availability of wound care products and nurses' reluctance to change the types of dressings used in case it appeared that they were challenging colleagues, whilst Gillespie et al . 26 attested that the selection of product can also be limited by contextual factors such as senior clinician preference and stock availability. McCluskey and McCarthy 27 also recognised the increasing complexity of wound aetiologies as a potential factor affecting ritualistic practice, whilst Ferreira et al . 25 and deFaria et al . 24 acknowledged challenges associated with accessing updated information about wound care and reliance upon colleagues' knowledge and experience as a means to address this. This was echoed by Gillespie et al . 26 , who reported that 75% of respondents obtained wound care information from informal sources, such as local specialists, rather than from scientific journals. Although learning from colleagues may be argued to present an opportunity for the maintenance of historic and ritualistic practice, in contrast, McCluskey and McCarthy 27 found that wound care competence in practice improved in accordance with length of clinician experience, which supports a positive link between contextual learning and competence in wound management.
Shortfalls in wound education
Dugdall and Watson 23 acknowledged the need for better education in EBP and research and also specifically recognised shortfalls in tissue viability content in undergraduate nursing education. This was echoed by Ferreira et al . 25 and deFaria et al . (2016) 24 , who found that 71·4% and 67·3% of respondents, respectively, reported to having insufficient formal wound care education, and McCluskey and McCarthy 27 , who recommended the implementation of better wound care education programmes for nurses working in acute setting. Gillespie et al . 26 did not specifically comment on the existence or effectiveness of formal wound care education or that accrued in practice but did acknowledge the existence of a positive relationship between higher education or specific tissue viability training and favourable attitudes towards EBP, which suggest that education improves practice. This may be argued to be of particular importance within the primary care sector as in a number of areas (e.g. across the UK), complex care is increasingly delivered in the community, and ineffective wound management would have a significant impact 6 .
It is clear from the findings of this review and from additional studies that the existence of high‐quality evidence pertaining to wound management is limited. This was found to be the case both in the generic sense but also in more specific areas of wound care practice (e.g. paediatrics) and was particularly notable in relation to the perceived effectiveness of specific products. This has been proposed to be related to a number of potential factors, notable of which may be that wound care practice has been traditionally led by the nursing profession rather than the medical profession, the latter of whom are historically regarded as the dominant health care professional 29 . As such, this may lead to their domination of competing research activity and resources but also to a failure to prioritise wound care and continually regard it as being of lesser importance than many clinical activities traditionally associated with doctors. It may also be linked to the lesser overall production of nursing research as nurses are recognised for their lesser engagement and reluctance to participate in scholarly activity in comparison to their medical counterparts. All of the publications acknowledged the need to establish a more scientific evidence base; however; despite attempts to gain legitimacy by aligning itself with the post‐positivist approach favoured by medicine 20 , nursing might be argued to be more ontologically in tune with the interpretivist/relativist/constructionist paradigms, which continue to be regarded with lesser scientific value amongst academic and research bodies than both the positivist and post‐positivist paradigms 30 . A further consideration is the links between wound care research and industry, although this has been addressed to some extent by the development of ethical codes of conduct for those employed by public sector and industry 31 , 32 .
Although empirical evidence was recognised to be a key component of practice [e.g. shaping national clinical wound care guidelines, such as those produced by the Scottish Intercollegiate Guidelines Network (SIGN) in the UK], nurses were also found to rely on evidence that is lower on the traditional hierarchy, with additional types of knowledge gleaned from informal sources (i.e. experience, clinical practice and learning through colleagues) also being recognised as important in all five studies. However, all studies also identified barriers to the implementation of EBP, including poor application of knowledge, failure to apply recommendations made by clinical guidelines or lack of awareness of protocols and guidelines altogether. Shortfalls in partnerships and integration between higher education/academic institutions and clinical sectors were also recognised to negatively affect the implementation of EBP in the practice setting 23 , 24 .
One of the shortfalls pertaining to the application of wound care theory to practice was the deficit in structured tissue viability education, both at an undergraduate level and that accredited by continuing professional development, which may be linked to the lack of prioritisation of wound care in comparison to other areas of practice and a consequential failure to organise and deliver sufficient education programmes. A further issue may be the increasing complexity of health demographics, which has led to a call in some circles for the preference of the term complex wounds rather than chronic wounds as the latter is defined by an association with time whilst the former recognises the growing underlying comorbidities that have a more multifactorial impact on wound healing 33 . This highlights an additional challenge for clinicians who are ultimately accountable for ensuring correct diagnosis, treatment pathways and responsible use of resources; however, this may be further limited by local systems and protocols impacting product availability in particular clinical areas (i.e. local wound care formularies). Additionally, the reduction of funding in CPD courses by NHS England in the UK may have a detrimental impact on access for those nurses wishing to undertake tissue viability courses, a development that is likely to filter out to other areas of the UK over time 34 .
A final point to note is that the majority of research pertaining to wound care is of quantitative design, and there is a noted absence of qualitative studies exploring either patients' or nurses' views, experiences and knowledge surrounding wounds and their management. Although the formal evidence base pertaining to wound care is unwaveringly limited, evidence and knowledge from less formal sources were more challenging to define. This was reflected in mixed evidence amongst the studies supporting the use of experiential and tacit learning in the practice setting and the conflicting results that emerged (i.e. learning from colleagues but also passing on ritualistic practices); however, experiential knowledge has been long recognised to be an important component of nursing practice, and there is no theoretical reason to believe this to be any less so in the field of wound care 14 , 15 .
This work reviewed literature pertaining to wound management to determine the current evidence base underpinning wound care, the extent of utilisation of existing evidence by nurses involved in the management of wounds and the knowledge and skills of nurses in relation to wound care. The evidence base pertaining to wound care practice was found to be limited, with weak links between EBP and practice‐heavy reliance upon industry support and funding, which may have potential ethical implications. Nurses were found to rely upon both formal and informal sources of knowledge to shape wound care practice; however, this contributed to the culture of ritualistic practice that withstands the clinical setting. A further impacting factor was found to be the inadequacy of wound care education at all levels.
Recommendations for practice
- The commitment to the conduction of independent studies in an effort to build the evidence base on all aspects of wound management;
- The commitment to the conduction of wound care research of qualitative design to obtain rich data on both patient and clinician experiences of all aspects of wound management;
- The development of more structured wound care education programmes at both pre‐registration/undergraduate and professional development levels;
- The commitment from nurse leaders and managers to support innovation and best practice through ongoing governance and audit activity.
Acknowledgements
The authors acknowledge Professor Ruth Deery, School of Health, Nursing and Midwifery, University of the West of Scotland, Dr Stephen Day, Assistant Dean, School of Education, University of the West of Scotland, Dr Vivian Crispin, Lecturer, School of Health, Nursing and Midwifery, University of the West of Scotland.
No conflicts of interest declared.

IMAGES
VIDEO
COMMENTS
AJN is pleased to announce the 2023 Nurse Faculty Scholars/AJN Mentored Writing Award, an annual program to promote mentorship and develop scholarly writing skills among nurses. The program is open to all RNs. Each candidate, working with a mentor, will develop and submit a paper to AJN; an awards committee will choose the winning paper.The winner will receive a $500 award.
The research showed that out of a total of 75 nurses, 38 (50.7%) had a good safety culture quality, while 37 (49.3%) were in the poor category. 20 This is evidenced by the high level of awareness of nurses in ensuring patient safety. This study shows that the longer a person works in a certain unit, the better the patient safety culture's ...
Exploring nurses' experiences of providing spiritual care to cancer patients: a qualitative study. This study aims to explore nurses' experiences of delivering spiritual care in an oncology setting. Huda A. Anshasi, Mirna Fawaz, Yousef M. Aljawarneh and Ja'far M. Alkhawaldeh. BMC Nursing 2024 23 :207. Research Published on: 27 March 2024.
The nursing profession has never been more visible, thrust into the spotlight of the COVID-19 pandemic. This focus has not only brought gratitude and fleeting displays of public support for so-called health-care heroes, but also vulnerability for patients and nurses alike.1 The importance of a competent, confident, and credentialled nurse has never been more crucial, yet in many settings, a ...
The Executive Vice President and Chief Nursing Officer for CommonSpirit Health discusses challenges nurses are facing during the Covid-19 pandemic, predominantly in terms of staffing, burnout, and compassion fatigue and PTSD; how burnout has been a problem in nursing for decades; and involving nurses in the vision for the future of health care delivery.
Depression and Nursing. Owing to the chaos and exhaustion caused by the COVID-19 pandemic, I have mentally felt less-than-optimal over the last few months. I was intrigued by the July Reflections article, "Acceptance Was the Key," in which Andy Marmion discussed suffering from depression as a nurse—and how a fellow nurse, Anne, helped him ...
Journal of Research in Nursing publishes quality research papers on healthcare issues that inform nurses and other healthcare professionals globally through linking policy, research and development initiatives to clinical and academic excellence. View full journal description. This journal is a member of the Committee on Publication Ethics (COPE).
Canadian Journal of Nursing Research (CJNR), Canada's leading journal in nursing research and scholarship publishes original research and scholarly manuscripts that are of special interest to nursing clinicians, educators, leaders, policy makers, and researchers, as well as other health care providers.CJNR is intended to serve both Canada and the international nursing community as a forum ...
The reasons for exclusion were lack of evidence of authors' affiliation with nursing, articles were published in a non-English language, or the full-text of the articles were unavailable. Through this search strategy, the authors identified 108 publications consisting of articles (90%, 97 of 108), reports (5%, 5 of 108), websites (5%, 5 of ...
Announcing. MCN The American Journal of Maternal Child Nursing Editorial Fellowship for 2024! For more information, please read this ann oucement. 2023 Research Article of the Year. Marliese Dion Nist, PhD, RNC-NIC, Audrey Robinson, BSN, RN, and Rita H. Pickler, PhD, RN, FAAN. Published in the March / April 2023 issue of MCN.
Introduction. Hand hygiene (HH) is the simplest and most effective measure for preventing healthcare-associated infections (HAIs).[] Despite the simplicity of this procedure and advances made in infection control, hospital health care workers' compliance to HH recommendations is generally low.[] Nurses have the most frequent patient care interactions, and thus more opportunities to practice ...
Our nursing publications include: • More than 60 credible, authoritative, peer-reviewed journals published by Lippincott Williams and Wilkins. • A library of more than 6,000 nursing articles. • Hundreds of Books and eBooks . • Free nursing eNewsletters. • The Focus On series, which are specially priced topical collections of articles ...
The official journal of the American Nurses Association (ANA), and rated as a highly valuable benefit of membership by ANA members, American Nurse Journal is read by 175,000 nursing professionals. Every edition features peer-reviewed features and articles written to keep nurses abreast of the latest developments in health care, and supply them ...
Bingham (2014) sees all of these actions as "sharing the wisdom of nursing" (p. 523) and describes the process of sharing knowledge through communication in peer-reviewed journals or through other professional outlets. Generally scholarly publications are peer reviewed or are part of scholarly publication and could include book reviews or ...
Journal of Cardiovascular Nursing is one of the leading journals for advanced practice nurses in cardiovascular care, providing thorough coverage of timely topics and information that is extremely practical for daily, on-the-job use. Each issue addresses the physiologic, psychologic, and social needs of cardiovascular patients and their families in a variety of environments.
Using CINAHL Complete (click the word Database under the title to access CINAHL), there are four ways to limit your results to scholarly articles written by nurse(s):. 1) First Author is Nurse* 2) Any Author is Nurse* If those do not work, try the Journal Subset**, or the Author Affiliation AF.**. 1) First Author is Nurse* limiter is available in the Limit Your Results menu beneath the ...
Background. A previous review on compassion in healthcare (1988-2014) identified several empirical studies and their limitations. Given the large influx and the disparate nature of the topic within the healthcare literature over the past 5 years, the objective of this study was to provide an update to our original scoping review to provide a current and comprehensive map of the literature to ...
Nurse Faculty Scholars / AJN Mentored Writing Award; Reprints; Rights and Permissions; Subscription Services; Nurses: Submit Your Photos! Advanced Search. October 2019 - Volume 119 - Issue 10 Previous Article; Next Article Letters, etc. Nursing and Aging. Stephany, Theresa MSN, RN ...
NOTE: The written by a nurse limiters apply only to records from November 2009 and forward. To find articles authored by University of Washington nurses: After entering your search topic, in the second Search box enter University of Washington and change the drop-down menu to: AF Author Affiliation.
Whereas nurses do have a specific language about their observations, our study showed that the specific day‐to‐day articulation about pressure ulcers is missing out. There is a tendency in health care that the written observations and reflections diminish when using a computer system where ticking off is an easy option (Iedema et al., 2011 ...
What is the relationship between nurses' attitude to evidence based practice and the selection of wound care procedures? Journal of Clinical Nursing. Non‐experimental, retrospective cross‐sectional postal survey. To investigate qualified nurses' views towards evidence‐based practice (EBP) and whether this influenced dressing selection ...